Professional Documents
Culture Documents
Pediatrics Rotation 1 - Airway Clearance for Pneumonia
Uploaded by
Frauline GagaracruzOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pediatrics Rotation 1 - Airway Clearance for Pneumonia
Uploaded by
Frauline GagaracruzCopyright:
Available Formats
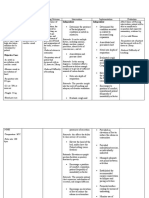
Rotation 1- Pediatrics
NCP
ASSESSMENT NURSING PLANNING IMPLEMENTATION EVALUATION
DIAGNOSIS
OBJECTIVE OF CARE INTERVENTION RATIONALE
CUES:
Ineffective After 8 hours of nursing The goal was met when the patient was
Subjective: airway clearance intervention the patient able to:
The mother related to will be able to:
difficulty of - Maintain patent airway with clear
verbalized that
breathing and - Maintain patent - Assess the rate, - Tachypnea, shallow respirations - At 10 am, for every 2 hours, breath sounds, absence of dyspnea,
her child has:
greenish airway with clear rhythm, depth of and asymmetric chest movement I assessed the patients rate, negative crackles and cleared
- Cough
secretion. breath sounds, respiration, chest are frequently present because of rhythm, depth of respiration, secretions after following doctors
- Colds
absence of movement and use of the discomfort of moving chest chest movement and the use advice.
with dyspnea and accessory muscles wall due to a compensatory of accessory muscles.
greenish - Demonstrate behaviors to achieve
effectively every 2 hours. response to airway obstruction.
secretion airway clearance by doing deep-
clearing secretions.
s for 2 breath exercises using bubble, stuff
weeks - HR and BP increases if fever - At 10:15 am, for every 4
toys and such.
- Develope - Assess vital signs rises. hours, I assessed the
d fever & every 4 hours to see patients vital sign.
- chills changes.
Objective: - Coughing is the most effective - At 10:30am, I checked the
- Assess cough way to remove secretions. cough effectiveness and
Weight: 26.5 lbs
effectiveness and Pneumonia may cause thick and productivity of the patient.
(12kg)
productivity. tenacious secretions in patients.
Vital Signs: - After endorsement for the
Temp: 38.6 C - Follows progress and effects and patient, the next nurse will
PP: 160 bpm extent of pneumonia. Oxygen monitor the chest x-ray,
RP: 60 bpm - Monitor chest x-rays,
saturation should be maintained ABG and pulse oximetry.
O2 Sat: 94% at ABG, Pulse oximetry
at 90% or greater. Imbalances in
room air readings
PaCO2 and Pa02 may indicate
respiratory fatigue. - I administer the medication
Lab Results:
- elevated prescribed by the physician
RBC following the prescribed
5.57x10/ - Administer medication - Medications used to facilitate time and date
- Demonstrate as indicated. respiration by dilating the
L
behaviors to airways.
(Polycyth
achieve airway - Elevate the head of the
emia) - I encouraged the mother of
clearance. bed, change position - Doing so would lower the
- elevated the patient to always elevate
frequently. diaphragm and promote chest
WBC the head of the bed or
expansion, aeration of lung
19.61 elevate the head of the
segments, mobilization, and
- (indicates patient to aid in chest
expectoration of secretions.
infection) expansion.
- Teach and assist
Urinalysis patient and the mother - Taught the patient and
- Facilitates maximum expansion
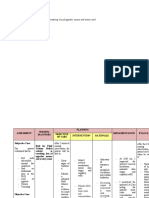
ASSESSMENT NURSING PLANNING IMPLEMENTATION EVALUATION
DIAGNOSIS
OBJECTIVE OF INTERVENTION RATIONALE
CARE
CUES: After 8 hours of to do proper deep of lungs, removes secretions and encouraged the mother to The goal was met when the
- + pus Anxiety related to nursing interventionbreathing exercises. patient and family members were
change in reduces chest discomfort. join by using bubbles,
Subjective:
cells the patient will be stuffed toys, pin wheel. able to reduce anxiety and fear
The mother environment as able to: upon the change in environment
Lung X-rayverbalized that her evidenced by fear - Maintain - adequate
Assess child’s and - Provides information - - At 10: 30am, I assessed
Encouraged mother to assist and hospitalization.
upon seeing the - reduce parents’
warm level of about sources and level the
Film: child has: hydration of
- Fluids aidofinanxiety
the mobilization thepatient
patientand guardian’s
in drinking warm
Lung - Cough nurse staff anxiety and fluids to at anxiety,
least 2 –child’s
4 associatedand
to level of anxiety,
fluids every after meal and
fear upon cups. developmental level, expectoration of secretions.
illness and developmental level,
inflammation- Colds with small sips in between.
right upper lobe greenish seeing understanding of hospitalization; sources understanding of illness
consolidation secretions hospital staff illness, and reason of anxiety and and reason for
for 2 weeks specifically for hospitalization, responses differ with hospitalization.
- has - Developed nurses and and responses to this age of child and
difficultyfever & doctor. and prior include separation, pain
of hospitalizations and bodily injury, loss
- chills
breathing during admission. of control, enforced
Objective:
- febrile dependence, fear of
- sweating
Weight: 26.5 lbs - Reduce the unknown, fear of
- lethargic
(12kg) anxiety and equipment, unfamiliar
- decrease fear of environment and
d Vital
breathSigns: family routines, guilt, fear and
sounds &38.6 C
Temp: members concern for child’s
- + PP: 160 bpm recovery, feelings of
- I encouraged the guardian
RP: 60 bpm
crackles powerlessness.
O2 Sat: 94% at - Allow verbalization to assist the patient and to
room air of feelings and voice out their opinion
concerns about - Provides an upon doing my rounds.
Lab Results: condition and opportunity to express
- elevated procedures and feelings and fears to
RBC listen individually to lessen anxiety and
(Polycythem child and parents. promote adjustment to - I encouraged the patient to
ia) hospitalization. share what he feels by
- Allow the child to asking him using a soft
- elevated
play out feelings. tone voice like where does
WBC - Allows the child to
Accept feelings and it hurt?
(indicates reveal feelings without
responses expressed
infection) fear of punishment.
by the child.
Urinalysis - had a fun talk with the
- + pus cells patient explaining that I
- Provide consistent will be his nurse until my
same personnel in - Promotes continuity shift ends.
Lung X-ray Film:
handling written and uniformity of care
Lung inflammation
care plan, care for to sustain a trusting
right upper lobe
child; schedule relationship.
consolidation
personal contact
- has with the child within - Played and talked with the
difficulty of workday. patient to build raport.
breathing
- Interact child in a - Develops rapport and
- sweating
positive approach; trust and maintains
- lethargic
use child’s proper identity.
- decreased name; avoid
breath communicating,
sounds & either verbally or
+ crackles - I encouraged the parents to
nonverbally, any minimize visitors and loud
rejection, judgments, noises to ease the anxiety
or negativism. of the patient.
- Decrease stimuli that
You might also like
- Planning 3 NCPSDocument5 pagesPlanning 3 NCPSCuttie Anne GalangNo ratings yet
- Nursing Care Plan: Assessment Nursing DX Planning Intervention Planning EvaluationDocument2 pagesNursing Care Plan: Assessment Nursing DX Planning Intervention Planning EvaluationJustine M. BellezaNo ratings yet
- NCP (Monreal)Document5 pagesNCP (Monreal)Karen Joy MonrealNo ratings yet
- Nursing Care Plan: Lipa City CollegesDocument13 pagesNursing Care Plan: Lipa City CollegesVincent Maralit MaterialNo ratings yet
- UntitledDocument12 pagesUntitledJoanna Marie PacanoNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanRachelleNo ratings yet
- Ineffective Airway Clearance: Fowler'sDocument3 pagesIneffective Airway Clearance: Fowler'sMarissa AsimNo ratings yet
- Assessing Airway Clearance for Improved RespirationDocument2 pagesAssessing Airway Clearance for Improved RespirationNica PinedaNo ratings yet
- medication and nursing care planDocument4 pagesmedication and nursing care planRubina MasihNo ratings yet
- Ineffective Airway Clearance: Fowler'sDocument3 pagesIneffective Airway Clearance: Fowler'sCake ManNo ratings yet
- NCP Drug StudyDocument3 pagesNCP Drug StudySofia NunagNo ratings yet
- Nursing Care Plan for Ineffective Airway ClearanceDocument2 pagesNursing Care Plan for Ineffective Airway ClearanceKenj Pereña100% (1)
- Dnrle Covid NCPDocument3 pagesDnrle Covid NCPEna RodasNo ratings yet
- Maintaining Clear AirwaysDocument2 pagesMaintaining Clear AirwaysBasema HashhashNo ratings yet
- Impaired Gas Exchange Assessment, Diagnosis, Planning, Intervention, EvaluationDocument2 pagesImpaired Gas Exchange Assessment, Diagnosis, Planning, Intervention, EvaluationDYNA GISELLE ROMERONo ratings yet
- NCP On Ineffective Airway Clearance Nursing Diagnosi S Planning Nursing Interventions Implementatio N Evaluation Subjective: IndependentDocument10 pagesNCP On Ineffective Airway Clearance Nursing Diagnosi S Planning Nursing Interventions Implementatio N Evaluation Subjective: IndependentSheryhan Tahir BayleNo ratings yet
- NCP of PnuemoniaDocument13 pagesNCP of PnuemoniaFrando kenneth100% (1)
- NCP For CKDDocument4 pagesNCP For CKDMinhwa KimNo ratings yet
- Airway Clearance StrategiesDocument4 pagesAirway Clearance Strategiescammel ramos100% (1)
- NCP For Nuchal CordDocument6 pagesNCP For Nuchal CordAubrey Marie GuerreroNo ratings yet
- Nursing care plan for community acquired pneumoniaDocument5 pagesNursing care plan for community acquired pneumoniaAubrey Marie GuerreroNo ratings yet
- NCP FinalDocument5 pagesNCP FinalVenus BonglayNo ratings yet
- Nursing care plan for anxiety-induced breathing issuesDocument2 pagesNursing care plan for anxiety-induced breathing issuesAbbyNo ratings yet
- Scenario 4 - NCPDocument15 pagesScenario 4 - NCPVian RiveraNo ratings yet
- NCP-FORMAT-Fernando-Legaspi-MalubayDocument3 pagesNCP-FORMAT-Fernando-Legaspi-MalubayGave gonzalesNo ratings yet
- Nursing Care Plan For A Premature InfantDocument3 pagesNursing Care Plan For A Premature InfantVillablanca Michelle84% (102)
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument9 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationthegoodreaderNo ratings yet
- Nursing Care Plan: Lopez, Maria Sofia B. 9/29/2020 3-BSN-B Prof. ZoletaDocument5 pagesNursing Care Plan: Lopez, Maria Sofia B. 9/29/2020 3-BSN-B Prof. ZoletaSofiaLopezNo ratings yet
- Lopez, Maria Sofia B. 10/07/2020 3-BSN-B Prof. Zoleta: Nursing Care Plan: PneumoniaDocument9 pagesLopez, Maria Sofia B. 10/07/2020 3-BSN-B Prof. Zoleta: Nursing Care Plan: PneumoniaSofia Lopez100% (2)
- PNEUMONIADocument8 pagesPNEUMONIARica ParcasioNo ratings yet
- Asthma NCPDocument3 pagesAsthma NCPjaijai magbanuaNo ratings yet
- NCP AlsDocument1 pageNCP AlsAlyssa Rose MacasiebNo ratings yet
- NCP and Drug StudyDocument7 pagesNCP and Drug StudyKirsty Marie SupranesNo ratings yet
- Nursing Care PlanDocument7 pagesNursing Care PlanDickson,Emilia Jade100% (3)
- Lumunok at Huminga, Nabibilaukan Din Ako Madalas" AsDocument4 pagesLumunok at Huminga, Nabibilaukan Din Ako Madalas" AsPatricia Ortega100% (1)
- Nursing Diagnosis, Interventions, and OutcomesDocument5 pagesNursing Diagnosis, Interventions, and OutcomesNur SetsuNo ratings yet
- Nursing Care Plan 3Document2 pagesNursing Care Plan 3Fiona Xandra San JuanNo ratings yet
- Nursing Care Plan: Assessm ENT Nursing Diagnos IS Planning Intervention Rationale Evaluati ON Subjectiv eDocument4 pagesNursing Care Plan: Assessm ENT Nursing Diagnos IS Planning Intervention Rationale Evaluati ON Subjectiv eJ. TSNo ratings yet
- Nursing Care Plan: Assessment Nursing Diagnosis Nursing Analysis Planning Nursing Interventions Rationale EvaluationDocument4 pagesNursing Care Plan: Assessment Nursing Diagnosis Nursing Analysis Planning Nursing Interventions Rationale EvaluationElla EvangelistaNo ratings yet
- NCP Ineffective Tissue PerfusionDocument2 pagesNCP Ineffective Tissue PerfusionYasminGianneDeOcampoBarizoNo ratings yet
- Ineffective Airway Clearance - PTBDocument2 pagesIneffective Airway Clearance - PTBIrish Eunice FelixNo ratings yet
- Ineffective Airway ClearanceDocument9 pagesIneffective Airway ClearanceMarissa AsimNo ratings yet
- Name: Mr. M AGE: 62 Years Old SEX: Male CC: Persistent Cough Admitting/Working Diagnosis: PnuemoniaDocument3 pagesName: Mr. M AGE: 62 Years Old SEX: Male CC: Persistent Cough Admitting/Working Diagnosis: PnuemoniaMae Therese B. MAGNONo ratings yet
- UntitledDocument4 pagesUntitledPie CanapiNo ratings yet
- Assessing and Managing Ineffective BreathingDocument3 pagesAssessing and Managing Ineffective BreathingEdem LeeNo ratings yet
- Assessment Nursing Diagnosis Plan of Care Expected Outcome Evaluation Subjective: Independent: Short Term Goal: Goals MetDocument2 pagesAssessment Nursing Diagnosis Plan of Care Expected Outcome Evaluation Subjective: Independent: Short Term Goal: Goals Metapi-3828211No ratings yet
- Nursing Care PlanDocument5 pagesNursing Care PlanWinsly BautistaNo ratings yet
- Cues Diagnosi S Desired Outcome Interventions Rationale EvaluationDocument2 pagesCues Diagnosi S Desired Outcome Interventions Rationale EvaluationYamete KudasaiNo ratings yet
- Jade R. Dinolan BSN-4 Case Study On A Patient With Pulmonary TuberculosisDocument8 pagesJade R. Dinolan BSN-4 Case Study On A Patient With Pulmonary TuberculosisJhade RelletaNo ratings yet
- Nursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisDocument19 pagesNursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisRiza Angela BarazanNo ratings yet
- Nursing Care Plan & Drug Study Set #1: PneumoniaDocument6 pagesNursing Care Plan & Drug Study Set #1: PneumoniaBakushidoNo ratings yet
- Difficulty of BreathingDocument4 pagesDifficulty of BreathingNur SetsuNo ratings yet
- Assessment Subjective: "Apat Na Araw Na SiyangDocument2 pagesAssessment Subjective: "Apat Na Araw Na Siyangmarlon_taycoNo ratings yet
- Nursing Care Plan for Labor Pain ManagementDocument8 pagesNursing Care Plan for Labor Pain ManagementDickson,Emilia Jade100% (1)
- NCP Ineffective Breathing PatternDocument4 pagesNCP Ineffective Breathing PatternSeika SouiNo ratings yet
- Tuberculosis Nursing Care Plan Ineffective Airway Clearance PDFDocument2 pagesTuberculosis Nursing Care Plan Ineffective Airway Clearance PDFPratiksha AmbedkarNo ratings yet
- NCP PaquidingDocument8 pagesNCP PaquidingGwyneth PaquidingNo ratings yet
- Explanation of The Problem Objective Nursing Intervention Rational EvaluationDocument4 pagesExplanation of The Problem Objective Nursing Intervention Rational EvaluationmeteabNo ratings yet
- Assessment Nursing Diagnosis Planning Interventions EvaluationsDocument2 pagesAssessment Nursing Diagnosis Planning Interventions EvaluationsAjay SupanNo ratings yet
- Cellular AbrasionDocument3 pagesCellular AbrasionFrauline GagaracruzNo ratings yet
- ASTHMADocument4 pagesASTHMAFrauline GagaracruzNo ratings yet
- ASTHMADocument4 pagesASTHMAFrauline GagaracruzNo ratings yet
- Surgical Procedure and Instruments Used (FOR OPERATING ROOM ONLY ONLY)Document7 pagesSurgical Procedure and Instruments Used (FOR OPERATING ROOM ONLY ONLY)Frauline GagaracruzNo ratings yet
- Metaclopramide: 4. Drug StudyDocument8 pagesMetaclopramide: 4. Drug StudyFrauline GagaracruzNo ratings yet
- Alternative Learning System Related Learning Experience Operating RoomDocument4 pagesAlternative Learning System Related Learning Experience Operating RoomFrauline GagaracruzNo ratings yet
- Als 2Document7 pagesAls 2Frauline GagaracruzNo ratings yet
- Risk for Fluid Volume Deficit and Acute PainDocument8 pagesRisk for Fluid Volume Deficit and Acute PainFrauline GagaracruzNo ratings yet
- "World Community"Document3 pages"World Community"Frauline GagaracruzNo ratings yet
- ASTHMADocument4 pagesASTHMAFrauline GagaracruzNo ratings yet
- Pathophysiology, Mapping and Differentiation of CancerDocument3 pagesPathophysiology, Mapping and Differentiation of CancerFrauline GagaracruzNo ratings yet
- NCMB 312 Lect Final NotesDocument16 pagesNCMB 312 Lect Final NotesAngie BaylonNo ratings yet
- SCH - HLTH 6002 Rehabilitation Assessment 1 Case StudyDocument17 pagesSCH - HLTH 6002 Rehabilitation Assessment 1 Case StudyHimanshu Sappal100% (2)
- Drug Study Hep BDocument4 pagesDrug Study Hep BSawada TsunayoshiNo ratings yet
- Jurnal 2 Scalloped TongueDocument3 pagesJurnal 2 Scalloped TonguestephanieNo ratings yet
- Oratio ImperataDocument1 pageOratio ImperataMark BinghayNo ratings yet
- Coronavirus Disease - by Slidesgo 2Document14 pagesCoronavirus Disease - by Slidesgo 2ZareefNo ratings yet
- Nidaan Swasthya Bima Policy BrochureDocument10 pagesNidaan Swasthya Bima Policy Brochureimpbithin96No ratings yet
- The Pathophysiology of Virulence of The COVID-19Document31 pagesThe Pathophysiology of Virulence of The COVID-19Glaneisia MitchellNo ratings yet
- Spontaneous Spondylodiscitis 2017Document7 pagesSpontaneous Spondylodiscitis 2017Paolo ContrerasNo ratings yet
- Cervical Stenotic Myelopathy in HorsesDocument7 pagesCervical Stenotic Myelopathy in HorsesKmii TspNo ratings yet
- Infection Control: Tel: SnleprometricDocument14 pagesInfection Control: Tel: SnleprometricSami MdNo ratings yet
- Spotting PSMDocument60 pagesSpotting PSMAmanNo ratings yet
- Trauma Thesis - Medical and LiteraryDocument290 pagesTrauma Thesis - Medical and Literarysadeyes_19No ratings yet
- Postural DrainageDocument7 pagesPostural DrainagemohtishimNo ratings yet
- Abdominal RadiologyDocument14 pagesAbdominal Radiologyfrancu60No ratings yet
- Report EmpyemaDocument32 pagesReport EmpyemaMylah CruzNo ratings yet
- CMVH PDFDocument199 pagesCMVH PDFFajriah SaraswatiNo ratings yet
- Imaging Features of Pediatric Musculoskeletal Tuberculosis: Pictorial EssayDocument15 pagesImaging Features of Pediatric Musculoskeletal Tuberculosis: Pictorial EssayMarwin JouleNo ratings yet
- Reflexology New Patient FormDocument7 pagesReflexology New Patient FormOana Iftimie100% (2)
- Conversion DisorderDocument18 pagesConversion Disorderrebecca wanjiruNo ratings yet
- Print NCLEX Study - Mark Klimek Blue BookDocument17 pagesPrint NCLEX Study - Mark Klimek Blue Booklento1990No ratings yet
- Krok 1 - 2006 (General Medicine) - EneutronDocument58 pagesKrok 1 - 2006 (General Medicine) - EneutronHarsh NimavatNo ratings yet
- 13 Matriks (Hal 104)Document2,003 pages13 Matriks (Hal 104)desti suci wulandariNo ratings yet
- Lepto Spiros IsDocument2 pagesLepto Spiros IsKBDNo ratings yet
- Tiotropium Bromide: Spiriva Handihaler, Spiriva RespimatDocument9 pagesTiotropium Bromide: Spiriva Handihaler, Spiriva RespimatAssem Ashraf KhidhrNo ratings yet
- RENR MOCK EXAMINATION 2 2018. Question SheetDocument24 pagesRENR MOCK EXAMINATION 2 2018. Question SheetSasha UterNo ratings yet
- Routledge International Handbook of Critical Mental HealthDocument308 pagesRoutledge International Handbook of Critical Mental HealthAdriánSánchez100% (2)
- Dystonia Fact Sheet: Causes, Symptoms & TreatmentsDocument7 pagesDystonia Fact Sheet: Causes, Symptoms & Treatmentsepiipo91No ratings yet
- Epidemiology of InfluenzaDocument12 pagesEpidemiology of InfluenzaSamwel KangyNo ratings yet
- Gynecological Oncology PDFDocument226 pagesGynecological Oncology PDFlula gestiana taufanNo ratings yet