Professional Documents
Culture Documents
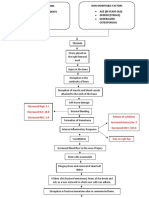
Modifiable Factors Non-Modifiable Factors
Uploaded by
kim cortezOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Modifiable Factors Non-Modifiable Factors
Uploaded by
kim cortezCopyright:
Available Formats
Modifiable Factors
Non-Modifiable Factors
Coping Skills
Substance Abuse Previous Traumatic Experiences (Sailing
Low Self-Esteem Accident)
Life stressors Family History of PTSD or Depression
History of Abuse
Psychiatric Comorbidities
Traumatic Event
(Death of a loved one, Lack of
control, Feelings of helplessness)
Intense peri-traumatic emotional response
(Fear, helplessness, nightmares)
Post-Traumatic Stress
Disorder / Depression
Neurochemical abnormalities Disrupted cognitive
Changes in cortisol, GABA, Dopamine processes
Emotional Increased Increased reactivity Development of Disruptions to
hyper-arousal Anxiety
in amygdala negative cognitive prefrontal cortex
(Attentional bias and behavioral thought
towards threat cues) patterns suppression
Hyper- Exaggerated Trouble
vigilance startle reflex Concentrating
Re-experiencing the Ruminative and Avoidance and
Insomnia Irritability trauma event worry thought numbing
(Flashbacks, nightmares) patterns (people, places,
feelings)
Low energy and
low appetite Social isolation
and inter-
personal
challenges
Clinically significant distress, or impaired functioning
Causes
Signs and Symptoms
Post-traumatic stress disorder symptoms may start within one month of a traumatic
event, but sometimes symptoms may not appear until years after the event. These
symptoms cause significant problems in social or work situations and in relationships.
They can also interfere with your ability to go about your normal daily tasks.
PTSD symptoms are generally grouped into four types: intrusive memories, avoidance,
negative changes in thinking and mood, and changes in physical and emotional
reactions. Symptoms can vary over time or vary from person to person.
Intrusive memories
Symptoms of intrusive memories may include:
Recurrent, unwanted distressing memories of the traumatic event
Reliving the traumatic event as if it were happening again (flashbacks)
Upsetting dreams or nightmares about the traumatic event
Severe emotional distress or physical reactions to something that reminds
you of the traumatic event
Avoidance
Symptoms of avoidance may include:
Trying to avoid thinking or talking about the traumatic event
Avoiding places, activities or people that remind you of the traumatic event
Negative changes in thinking and mood
Symptoms of negative changes in thinking and mood may include:
Negative thoughts about yourself, other people or the world
Hopelessness about the future
Memory problems, including not remembering important aspects of the
traumatic event
Difficulty maintaining close relationships
Feeling detached from family and friends
Lack of interest in activities you once enjoyed
Difficulty experiencing positive emotions
Feeling emotionally numb
Changes in physical and emotional reactions
Symptoms of changes in physical and emotional reactions (also called arousal
symptoms) may include:
Being easily startled or frightened
Always being on guard for danger
Self-destructive behavior, such as drinking too much or driving too fast
Trouble sleeping
Trouble concentrating
Irritability, angry outbursts or aggressive behavior
Overwhelming guilt or shame
Depression
-Trouble concentrating, remembering details, and making
decisions
Feelings of guilt, worthlessness, and helplessness
-Insomnia,
-Low energy, low appetite
-Suicidal thoughts
Pessimism and hopelessness
Diagnosis
A doctor can rule out other conditions that may cause depression with a
physical examination, a personal interview, and lab tests. The doctor
will also do a complete diagnostic evaluation, discussing any family
history of depression or other mental illness.
After reviewing the information from your appointment, including the
signs and symptoms, patient history, family history, and physician exam
The CAPS is widely considered to be the "gold standard" in PTSD assessment. It is a
structured interview providing a categorical diagnosis, as well as a measure of the severity of
PTSD symptoms as defined by DSM-IV. It can be administered by any trained person and takes
30-60 minutes.
CAPS-5
The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) is a standard test used to diagnose
PTSD.3 This is a 30-item questionnaire that clinicians use to better understand the patient’s
experience with PTSD.
The goal of CAPS-5 is to establish whether a person can be diagnosed with PTSD. It is also used to
assess whether this condition has been present throughout a person’s life or within the past month.
Additionally, this assessment is used to assess symptoms as the patient has experienced them over
the previous week.
Specifically, these questions explore:
The onset and duration of symptoms
The impact of symptoms on social relationships and work functioning
Overall severity of PTSD symptoms
Presence of dissociative subtype, like depersonalization and derealization
This interview takes roughly an hour to complete, follows a detailed scoring system, and determines
to what extent the severity of the symptoms impacts an individual’s daily life.
Treatment-Outcome Post Traumatic Stress Disorder Scale
(TOP-8)
The TOP-8 is also an interview-based assessment tool that uses the DSM-5 to understand and
evaluate symptoms. This scale includes eight questions drawn from the core symptom groups
associated with PTSD, which include intrusion, avoidance, and numbing.
PTSD Symptom Scale Interview (PSS-I and PSS-I-5)
The PSS-I is a 17-item assessment tool that asks patients to identify a singular traumatic event that
they believe is causing their symptoms. Symptoms from the past two weeks are identified and
assessed as they relate to the DSM-5 diagnosis criteria.
The PSS-I-5 contains 24 questions, with 20 focusing on symptoms and four focusing on symptom
distress, interference, onset, and duration.
The Davidson Trauma Scale (DTS)
The Davidson Trauma Scale (DTS) is a self-assessment that people can use to screen themselves for
PTSD. This test uses a four-item scale called SPAN that looks at four key areas involved in PTSD:
startle, physiological arousal, anger, and emotional numbness. This test has 17 items and asks the
person taking it to rate the severity of each symptom across the SPAN categories.
PTSD Checklist for DSM-5 (PCL-5)
Patients can also use the PTSD Checklist for DSM-5, or PCL-5, to assess their
symptoms.4 Composed of 20 questions, this report was created by the National Center for PTSD of
the Department of Veterans Affairs and is used widely because it can offer support throughout a
person’s PTSD journey.
In addition to supporting self-assessment with PTSD, it can also be used after a diagnosis to monitor
symptoms. Therefore, it acts both as a tool for diagnosis and one for assessing symptoms to
understand improvement.
Short PTSD Rating Interview (SPRINT)
The Short PTSD Rating Interview, or SPRINT, can be used to assess main PTSD symptoms. 5 It looks
at eight proven PTSD symptom categories, including intrusion, avoidance, numbing, arousal, somatic
malaise, stress vulnerability, and role and social impairment.
This assessment is best used when a person is first interested in seeking care for PTSD, and it is
considered a more preliminary approach for people who aren’t sure whether they have PTSD. The
test uses a five-point scale, asking patients to rank their symptoms from 0 to 4. If a person’s results
are positive, meaning they rated at least one question above 0, they need further assessment by a
professional.
Beck Depression Inventory
The Beck Depression Inventory (BDI) is made up of 21 self-reported depression
questions. They are designed to help mental health professionals assess the
mood, symptoms, and behaviors of people who are depressed. Each answer is
given a score of zero through three to indicate severity of symptoms.
Hamilton Depression Rating Scale
The Hamilton Depression Rating Scale (HDRS) is a questionnaire designed to
help healthcare professionals determine the severity of depression in people who
have already been diagnosed. It also consists of 21 questions. Each relates to a
particular sign or symptom of depression. Multiple-choice answers are given a
score of zero through four. Higher total scores indicate more severe depression.
Treatment
Post-traumatic stress disorder treatment can help you regain a sense of control over
your life. The primary treatment is psychotherapy, but can also include medication.
Combining these treatments can help improve your symptoms by:
Teaching you skills to address your symptoms
Helping you think better about yourself, others and the world
Learning ways to cope if any symptoms arise again
Treating other problems often related to traumatic experiences, such as
depression, anxiety, or misuse of alcohol or drugs
Psychotherapy
Several types of psychotherapy, also called talk therapy, may be used to treat children
and adults with PTSD. Some types of psychotherapy used in PTSD treatment include:
Cognitive therapy. This type of talk therapy helps you recognize the ways
of thinking (cognitive patterns) that are keeping you stuck — for example,
negative beliefs about yourself and the risk of traumatic things happening
again. For PTSD, cognitive therapy often is used along with exposure
therapy.
Exposure therapy. This behavioral therapy helps you safely face both
situations and memories that you find frightening so that you can learn to
cope with them effectively. Exposure therapy can be particularly helpful for
flashbacks and nightmares. One approach uses virtual reality programs that
allow you to re-enter the setting in which you experienced trauma.
Eye movement desensitization and reprocessing (EMDR). EMDR
combines exposure therapy with a series of guided eye movements that
help you process traumatic memories and change how you react to them.
Medications
Several types of medications can help improve symptoms of PTSD:
Antidepressants. These medications can help symptoms of depression and
anxiety. They can also help improve sleep problems and concentration. The
selective serotonin reuptake inhibitor (SSRI) medications sertraline (Zoloft) and
paroxetine (Paxil) are approved by the Food and Drug Administration (FDA) for
PTSD treatment.
Anti-anxiety medications. These drugs can relieve severe anxiety and related
problems. Some anti-anxiety medications have the potential for abuse, so they are
generally used only for a short time.
Prazosin. While several studies indicated that prazosin (Minipress) may reduce or
suppress nightmares in some people with PTSD, a more recent study showed no
benefit over placebo. But participants in the recent study differed from others in
ways that potentially could impact the results. Individuals who are considering
prazosin should speak with a doctor to determine whether or not their particular
situation might merit a trial of this drug.
o
You might also like
- BEHS Disorders ChartDocument7 pagesBEHS Disorders ChartAndrew PatelNo ratings yet
- Mental Status Exam: Component Elements To Assess Potential Illnesses Sample QuestionsDocument8 pagesMental Status Exam: Component Elements To Assess Potential Illnesses Sample QuestionsLa LangNo ratings yet
- Post-Traumatic Stress Disorder Workbook: Practical Help and Information for PTSDFrom EverandPost-Traumatic Stress Disorder Workbook: Practical Help and Information for PTSDRating: 4.5 out of 5 stars4.5/5 (6)
- Pshciatry in BriefDocument18 pagesPshciatry in BriefSelim TarekNo ratings yet
- PsychologyDocument52 pagesPsychologySandra ManzanoNo ratings yet
- Cognitive Behaviour TherapyDocument49 pagesCognitive Behaviour TherapyTidita Ahmetaga-AbdurrahmaniNo ratings yet
- Safety Organisation & Safety Committee MeetingDocument6 pagesSafety Organisation & Safety Committee MeetingVishu SharmaNo ratings yet
- Employee Safety Training Matrix Template ExcelDocument79 pagesEmployee Safety Training Matrix Template Excelشاز إياسNo ratings yet
- Psych HX MSE DMHBS PGMI 2020Document7 pagesPsych HX MSE DMHBS PGMI 2020Mariana B.No ratings yet
- Intro Psychological DisordersDocument39 pagesIntro Psychological DisordersMary Jo LegaspiNo ratings yet
- Essentials of Neurology 2Document153 pagesEssentials of Neurology 2prahul2588100% (7)
- AP Psychology Module 66+67Document5 pagesAP Psychology Module 66+67kyuuNo ratings yet
- Profit and Loss Statement TemplateDocument2 pagesProfit and Loss Statement TemplateAlisa VisanNo ratings yet
- Overcoming PTSD: The workbook designed to help you understand and overcome post-traumatic stress disorderFrom EverandOvercoming PTSD: The workbook designed to help you understand and overcome post-traumatic stress disorderNo ratings yet
- Psychiatry Disorders in ElderlyDocument25 pagesPsychiatry Disorders in ElderlyIndah Sandy SimorangkirNo ratings yet
- PTSD and Cognitive Processing Therapy Presented by Patricia A. Resick, PHD, AbppDocument28 pagesPTSD and Cognitive Processing Therapy Presented by Patricia A. Resick, PHD, AbppDardo Arreche100% (2)
- HEALTH TALK Care of Depression PatientDocument17 pagesHEALTH TALK Care of Depression PatientAmit RanjanNo ratings yet
- NCP For Adjustment DisordersDocument18 pagesNCP For Adjustment Disordersshaider119100% (1)
- Anxiety DisordersDocument34 pagesAnxiety DisordersGafaranga Jean PierreNo ratings yet
- Psychological DisordersDocument46 pagesPsychological DisordersanNo ratings yet
- Manufacturing Process of Plastic BottlesDocument19 pagesManufacturing Process of Plastic BottlesAparna Samuel87% (23)
- Sleep E Book Power of SleepDocument36 pagesSleep E Book Power of Sleepstrgates34100% (1)
- Part 3 - Mental Illness - Psychological Health and WellbeingDocument24 pagesPart 3 - Mental Illness - Psychological Health and Wellbeingapi-642709499No ratings yet
- Trauma HandoutsDocument8 pagesTrauma HandoutsDawn Farm100% (1)
- Retaining Wall Design-REVDocument34 pagesRetaining Wall Design-REVzaheer0406100% (1)
- Auraton 2005Document24 pagesAuraton 2005Muhidin KozicaNo ratings yet
- Trauma Survivor's Guide to Coping with Panic Attacks: Focusing on Panic Associated with PTSD and cPTSDFrom EverandTrauma Survivor's Guide to Coping with Panic Attacks: Focusing on Panic Associated with PTSD and cPTSDNo ratings yet
- Effective CommunicationDocument19 pagesEffective Communicationkim cortezNo ratings yet
- Module Tests: Expert PTEA Testmaster B2 Answer KeyDocument5 pagesModule Tests: Expert PTEA Testmaster B2 Answer KeyRyan MathProNo ratings yet
- DepressionDocument28 pagesDepressionDr.M HanifNo ratings yet
- Trauma and Stress Related Disorder For PGY 1Document28 pagesTrauma and Stress Related Disorder For PGY 1AbelNo ratings yet
- Case Analysis OcdDocument3 pagesCase Analysis OcdAjay SupanNo ratings yet
- Psyc1002-Ch.14 Lec NotesDocument4 pagesPsyc1002-Ch.14 Lec NotesNadya B.No ratings yet
- Mental Illness Types, Risk Factors, and TreatmentDocument1 pageMental Illness Types, Risk Factors, and TreatmentMediBuddyNo ratings yet
- PTSD ReportDocument21 pagesPTSD ReportDana LabusonNo ratings yet
- Physiological DisordersDocument38 pagesPhysiological Disordersreview notesNo ratings yet
- Introduction-: Post Traumatic Stress Disorder (PTSD)Document10 pagesIntroduction-: Post Traumatic Stress Disorder (PTSD)preeti sharmaNo ratings yet
- Clinical Psychology: Mood Disorders: What Is Abnormality?Document6 pagesClinical Psychology: Mood Disorders: What Is Abnormality?Alexandra Adina RădescuNo ratings yet
- Mental Disorders 2Document36 pagesMental Disorders 2Iraide GarcésNo ratings yet
- Trauma and The LifespanDocument39 pagesTrauma and The LifespanRegina PhalangeNo ratings yet
- Educational Brochure (Abnormal Psychology)Document7 pagesEducational Brochure (Abnormal Psychology)Leonardo YsaiahNo ratings yet
- 1-01 Psychiatric History and Mental Status Examination Appendix CIC v1Document5 pages1-01 Psychiatric History and Mental Status Examination Appendix CIC v1Dane Mikhael CalicaNo ratings yet
- 6 DepressionDocument42 pages6 DepressionEIorgaNo ratings yet
- Day 3 Mood Disorders RV Rushed 2018Document28 pagesDay 3 Mood Disorders RV Rushed 2018api-433532127No ratings yet
- ABPG1103 - Topic 12 - Psychological Disorder - 222Document21 pagesABPG1103 - Topic 12 - Psychological Disorder - 222nureryani bathowiNo ratings yet
- Major Depression - Dysthymic DisorderDocument27 pagesMajor Depression - Dysthymic DisorderCay SevillaNo ratings yet
- Week6 Disorderspart1Document20 pagesWeek6 Disorderspart1reyeslucasmat4No ratings yet
- Neouropsychiatric AssessmentDocument21 pagesNeouropsychiatric AssessmentKopano'Gucci'ModisenyaneNo ratings yet
- 08.06 Abnormal Psychology-Revised NotesDocument6 pages08.06 Abnormal Psychology-Revised NotesJesusa Angelika IlustreNo ratings yet
- Rit Aec26 Unit 1 Lecture 2Document56 pagesRit Aec26 Unit 1 Lecture 2pshashank138No ratings yet
- Major Depression - Dysthymic DisorderDocument28 pagesMajor Depression - Dysthymic Disorderapi-3797941No ratings yet
- Farmakoterapi DepresiDocument46 pagesFarmakoterapi DepresiPrinss AntyyNo ratings yet
- Clinical Assessment Part 2 2 SlidesDocument34 pagesClinical Assessment Part 2 2 SlidesKresna Surya WNo ratings yet
- Psychological Analysis FinalDocument7 pagesPsychological Analysis FinaldrcalypsojellyfingerNo ratings yet
- Midterm - Chapter 7Document6 pagesMidterm - Chapter 7mark OrpillaNo ratings yet
- Mar 28 - 30 - 31 StudentDocument20 pagesMar 28 - 30 - 31 StudentpaulamvillahermosaNo ratings yet
- ABPSY Finals ReviewerDocument48 pagesABPSY Finals ReviewerMary Grace AngelesNo ratings yet
- PSYCHIATRYDocument12 pagesPSYCHIATRYSavanthi Carmaline de SilvaNo ratings yet
- Farmakoterapi Sistem Organ II-DepresiDocument73 pagesFarmakoterapi Sistem Organ II-DepresiDISKA YUNIAROHIMNo ratings yet
- Psychodynamic and Psychopathology (Compatibility Mode) PDFDocument27 pagesPsychodynamic and Psychopathology (Compatibility Mode) PDFMade Satria PawitraNo ratings yet
- PPP Training Module 3 FINAL - JanDocument41 pagesPPP Training Module 3 FINAL - JanMary Ann MejiaNo ratings yet
- PresentationDocument14 pagesPresentationAndrius GorodeckisNo ratings yet
- Cluster C Personality DisordersDocument3 pagesCluster C Personality DisordersCake ManNo ratings yet
- PPP Training Module 3 DownloadDocument46 pagesPPP Training Module 3 DownloadNafiu AbdullateefNo ratings yet
- Prelim ReviewerDocument8 pagesPrelim ReviewerAGNER JASMIN ROSE L.No ratings yet
- Mental Disorder: Cretoiu StefanDocument8 pagesMental Disorder: Cretoiu StefanStefanCretoiuNo ratings yet
- Reviewer Mental HeathDocument3 pagesReviewer Mental HeathChelca Angela RamosNo ratings yet
- Psychological First Aid YET FinalDocument49 pagesPsychological First Aid YET FinalJultrin Ganso KiiskiNo ratings yet
- Conversion Disorder Hysterical NeurosisDocument4 pagesConversion Disorder Hysterical NeurosisrianachuNo ratings yet
- 1868-Article Text-5360-1-10-20201204Document22 pages1868-Article Text-5360-1-10-20201204kim cortezNo ratings yet
- The Impact of Social Media Exposure and Interpersonal Discussion On Intention of COVID-19 Vaccination Among NursesDocument13 pagesThe Impact of Social Media Exposure and Interpersonal Discussion On Intention of COVID-19 Vaccination Among Nurseskim cortezNo ratings yet
- Decreased HGB: 9.1 Decreased HCT: 28.8 Decreased RBC: 2.8 Release of Cytokines Increased Monocytes: 9 Decreased MCV: 103.6Document3 pagesDecreased HGB: 9.1 Decreased HCT: 28.8 Decreased RBC: 2.8 Release of Cytokines Increased Monocytes: 9 Decreased MCV: 103.6kim cortezNo ratings yet
- Fetal AssessmentDocument57 pagesFetal Assessmentkim cortezNo ratings yet
- Appointment RecieptDocument1 pageAppointment Recieptaqil faizanNo ratings yet
- Balancing ActDocument5 pagesBalancing ActAnonymous AMmNGgPNo ratings yet
- 2018 - Shiau - Evaluation of A Flipped Classroom Approach To Learning Introductory EpidemiologyDocument9 pages2018 - Shiau - Evaluation of A Flipped Classroom Approach To Learning Introductory EpidemiologySocorro Moreno LunaNo ratings yet
- G3520 Lehe2832 02 PDFDocument6 pagesG3520 Lehe2832 02 PDFCostas Aggelidis100% (1)
- Chapter 4 Scintillation Detectors: 4.1. Basic Principle of The ScintillatorDocument10 pagesChapter 4 Scintillation Detectors: 4.1. Basic Principle of The ScintillatorbbkanilNo ratings yet
- Organic Food Business in India A Survey of CompaniDocument19 pagesOrganic Food Business in India A Survey of CompaniShravan KemturNo ratings yet
- Identify The Letter of The Choice That Best Completes The Statement or Answers The QuestionDocument18 pagesIdentify The Letter of The Choice That Best Completes The Statement or Answers The QuestionCeline YoonNo ratings yet
- Supply, Elasticity of SupplyDocument4 pagesSupply, Elasticity of SupplySaurabhNo ratings yet
- Sa Bref 0505Document469 pagesSa Bref 0505tc5440No ratings yet
- IP Rating ChartDocument3 pagesIP Rating ChartMayur MNo ratings yet
- Turnstile Design SheetDocument6 pagesTurnstile Design SheetArmstrongMasengaNo ratings yet
- DP27, DP27E, DP27R and DP27Y Pilot Operated Pressure Reducing ValvesDocument36 pagesDP27, DP27E, DP27R and DP27Y Pilot Operated Pressure Reducing ValvesAntonio FedatoNo ratings yet
- Pregnancy in Dental TreatmentDocument62 pagesPregnancy in Dental TreatmentChinar HawramyNo ratings yet
- Bonpak Catalogue 2011Document18 pagesBonpak Catalogue 2011George TowerNo ratings yet
- Reservoir Design and OperationDocument66 pagesReservoir Design and OperationUssamaLatifNo ratings yet
- 2019 IWA WDCE SriLanka Programme-Book Website PDFDocument75 pages2019 IWA WDCE SriLanka Programme-Book Website PDFPradeep KumaraNo ratings yet
- Solar Direct-Drive Vaccine Refrigerators and Freezers: The Need For Off-Grid Cooling OptionsDocument10 pagesSolar Direct-Drive Vaccine Refrigerators and Freezers: The Need For Off-Grid Cooling OptionsRolando mendozaNo ratings yet
- Pleskac - 2008 - Decision Making and Learning While Taking SequentiDocument20 pagesPleskac - 2008 - Decision Making and Learning While Taking SequentiDurgesh Haribhau SalunkheNo ratings yet
- Deltaweld 453 MilDocument40 pagesDeltaweld 453 MilHugo RodriguezNo ratings yet
- BancassuranceDocument53 pagesBancassuranceSonali Chaubey0% (1)
- Food WebDocument12 pagesFood WebShaurya ChauhanNo ratings yet