Professional Documents
Culture Documents
In Vitro Evaluation of Aerosol Delivery - Complementaria - Semana 3
Uploaded by
natalia muñozOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
In Vitro Evaluation of Aerosol Delivery - Complementaria - Semana 3
Uploaded by
natalia muñozCopyright:
Available Formats
In Vitro Evaluation of Aerosol Delivery by
Different Nebulization Modes in Pediatric and
Adult Mechanical Ventilators
Gwo-Hwa Wan PhD, Hui-Ling Lin MSc RRT RN FAARC, James B Fink PhD RRT FAARC,
Yen-Hey Chen MSc, Wei-Jhen Wang RRT, Yu-Chun Chiu RRT,
Yu-Yao Kao RRT, and Chia-Jung Liu RRT
BACKGROUND: Aerosol delivery through mechanical ventilation is influenced by the type of
aerosol generator, pattern of nebulization, and a patient’s breathing pattern. This study compares
the efficiency of pneumatic nebulization modes provided by a ventilator with adult and pediatric
in vitro lung models. METHODS: Three pneumatic nebulization modes (inspiratory intermittent
[IIM], continuous [CM], and expiratory intermittent [EIM]) provided by the Galileo Gold venti-
lator delivered medical aerosol to collection filters distal to an endotracheal tube with adult and
pediatric test lungs. A unit dose of 5 mg/2.5 mL albuterol was diluted into 4 mL with distilled water
and added to a jet nebulizer. The nebulizer was placed proximal to the ventilator, 15 cm from the
inlet of the heated humidifier chamber with a T-piece and corrugated aerosol tubing and powered
by gas from the ventilator in each of the 3 modes. Time for nebulization was recorded in minutes.
Albuterol samples collected in the inhalation filter, nebulizer, T-piece, and corrugated tubing were
eluted with distilled water and analyzed with a spectrophotometer. RESULTS: The inhaled drug,
as a percentage of total dose in both lung models, was 5.1–7.5%, without statistical significance
among the 3 modes. Median nebulization times for IIM, CM, and EIM were 38.9, 14.3, and
17.7 min, respectively, and nebulization time for the 3 modes significantly differed (P < .001). The
inhaled drug mass for the 3 modes with the adult lung model was similar to that with the pediatric
lung model (7.39 ⴞ 0.76 vs 6.27 ⴞ 0.69%, P ⴝ .77). CONCLUSIONS: Aerosol drug delivery with
a jet nebulizer placed proximal to the ventilator was not dependent on nebulization mode during
simulated pediatric and adult conventional mechanical ventilation. Use of expiratory intermittent
mode and continuous nebulization should be considered to reduce treatment time. Key words:
aerosol drug delivery; bronchodilator; small-volume nebulizer; endotracheal tube; mechanical ventila-
tion; nebulization mode. [Respir Care 2014;59(10):1494 –1500. © 2014 Daedalus Enterprises]
Introduction conditions. The jet nebulizer is frequently used to admin-
ister bronchodilators and other agents during mechanical
Aerosolized bronchodilators are commonly used to treat ventilation.
mechanically ventilated patients with airway disease and
Department of Respiratory Therapy, Chang Gung Memorial Hospital-
Linko Branch, Taoyuan, Taiwan.
Dr Wan, Ms Lin, and Ms Chen are affiliated with the Department of
Respiratory Therapy, College of Medicine, Chang Gung University, Ms Lin presented a version of this paper at the Open Forum of the AARC
Taoyuan, Taiwan. Dr Fink is affiliated with the Division of Respiratory Congress 2012, held November 10–13, 2012, in New Orleans, Louisiana.
Therapy, Georgia State University, Atlanta, Georgia. Ms Wang is affil-
iated with the Department of Respiratory Therapy, National Taiwan Uni- Dr Fink is a consultant to Aerogen, Bayer, Boehringer Ingelheim, Cubist
versity Hospital, Taipei, Taiwan. Ms Chiu is affiliated with the Graduate Pharmaceuticals, Dance Biopharm, Novartis, ONY, Parion, Aridis Phar-
Institute of Pharmacology, College of Medicine, National Taiwan Uni- maceuticals, and the World Health Organization. The other authors have
versity, Taipei, Taiwan. Mr Kao and Ms Liu are affiliated with the disclosed no conflicts of interest.
1494 RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10
AEROSOL DELIVERY BY DIFFERENT VENTILATOR NEBULIZATION MODES
The efficiency of drug delivery through mechanical ven-
tilation in adults is enhanced by many factors, including QUICK LOOK
CPAP, mode (spontaneous breathing),1 longer duty cycle Current knowledge
and inspiratory time,2 lower inspiratory flow,3 and lower
bias flow.1,2,4-6 Aerosol delivery varies with different Aerosol delivery during mechanical ventilation can be
types of aerosol generators, brands of nebulizer used, influenced by the aerosol generator, pattern of nebuli-
and their position in the ventilator circuit.6-8 Other authors zation, presence of humidification, ventilator settings,
reported that the higher the peak inspiratory flow, the and patient breathing pattern. The pattern of nebuliza-
greater the impact of inspiratory waveform on aerosol tion includes continuous, synchronized with inspiration,
delivery.5 and during expiration.
Furthermore, factors improving aerosol delivery through
What this paper contributes to our knowledge
mechanical ventilation in pediatric patients include larger
endotracheal tubes (ETTs), use of metered-dose inhalers In a lung model study, aerosolized drug delivery with a
with spacers, synchronization with inspiration, use of he- jet nebulizer placed proximal to the ventilator was not
liox (80:20 helium-oxygen mixture) as a gas power source, affected by the pattern of nebulization. However, syn-
and positioning a jet nebulizer distal to the ventilator cir- chronized inspiratory nebulization required a 3-fold lon-
cuit.8-12 ger nebulization time.
More recently, researchers have reported greater aerosol
delivery with a continuous jet nebulizer placed proximal to
the ventilator and before the humidifier in both adult and
pediatric lung models.11,13 A number of benefits have been
proposed to placing jet nebulizers proximal to the venti- from a jet nebulizer synchronized with inspiration com-
lator rather than in the more conventional placement in the pared with continuous nebulization reported a nearly 2-fold
inspiratory limb or at the Y-piece near the patient. Place- increase in delivery with jet nebulizer placement at the
ment of the nebulizer in the inspiratory limb of the venti- Y-piece, but only 15% greater compared with placement
lator circuit proximal to the ventilator allows the nebulizer in the middle of the inspiratory limb (or manifold posi-
to be oriented in an optimal position that does not change tion).14 In contrast, a reduction with synchronized nebuli-
with turning the patient and eliminates the weight of the zation at the manifold position has been reported.15 Early
nebulizer near the patient airway. Placement at the inlet of in vivo deposition studies reported ⬍ 3% deposition uti-
the humidifier reduces access of patient secretions and lizing jet nebulization synchronized with inspiration.16 A
condensate in the inspiratory limb of the ventilator circuit study by Miller et al6 compared breath-actuated nebuliza-
to contaminate the nebulizer. In addition, passing aerosol tion by 2 different ventilators (PB7200, Puritan Bennett,
through the humidifier allows larger particles to rain out, Pleasanton, California; and Dräger, Lübeck, Germany).
reducing the mass of aerosol that might deposit on a sensor
They reported substantial improvements with synchronized
placed between the ventilator circuit and the patient air-
versus continuous nebulization with the nebulizer placed
way as well as condensate that might form in the inspira-
in the inspiratory limb at the Y-piece.
tory limb.
Di Paolo et al17 and Sidler-Moix et al18 compared dif-
With those potential benefits in mind, it is important to
ferent nebulization modes in an infant bench model and
quantify aerosol drug delivery distal to the ETT with all
modes. Two basic aerosol generation scenarios have been reported better aerosol delivery with nebulization synchro-
described with adult mechanical ventilation: generating nized during expiration compared with inspiration or con-
aerosol only during inspiration and generating aerosol con- tinuously throughout the cycle. They reported that a jet
tinuously throughout the respiratory cycle. Some ventila- nebulizer delivered more efficiently with intermittent ex-
tors provide a nebulization function that synchronizes aero- piratory mode on a ventilator (Galileo, Hamilton Medical,
sol generation during mechanical ventilation. Over the last Bonaduz, Switzerland).
20 y, reports of benefits with synchronized over continu- This in vitro study compares the influence of 3 pneu-
ous nebulization have been mixed, depending on the place- matic nebulization modes of a ventilator using adult and
ment of the nebulizer. A study comparing aerosol delivery pediatric ventilator parameters and lung models. We hy-
pothesized that aerosol generated with the 3 modes during
mechanical ventilation would deliver a similar drug dose
to the distal end of an ETT. We also hypothesized that
Correspondence: Hui-Ling Lin MSc RRT RN FAARC. E-mail:
huilingrrt@gmail.com.
aerosol delivery would be greater with adult than pediatric
settings. The study was performed in the Respiratory Ther-
DOI: 10.4187/respcare.02999 apy Research Laboratory at Chang Gung University.
RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10 1495
AEROSOL DELIVERY BY DIFFERENT VENTILATOR NEBULIZATION MODES
Methods
Lung Model
Figure 1 shows the experimental apparatus of the lung
model. A ventilator (Galileo Gold, Hamilton Medical) was
set to deliver adult parameters (tidal volume [VT] of 600 mL,
breathing frequency of 16 breaths/min, PEEP 5 cm H2O,
and inspiration-expiration ratio [I:E] 1:2.5) and pediatric
parameters (VT 160 mL, breathing frequency of 25 breaths/
min, PEEP 5 cm H2O, and I:E 1:2). A 120-cm ventilator
circuit connected the ventilator to a test lung (TTL, Mich-
igan Instruments, Grand Rapids, Michigan) via an ETT
(7.5-mm [adult] and 5.0-mm [pediatric] inner diameter) Fig. 1. Diagram of experimental apparatus. A jet nebulizer (E) pow-
positioned distal to a Y-piece and a flow sensor. Adult ered by the ventilator nebulization function was placed in the ven-
(22-mm inner diameter) and pediatric (15-mm inner diam- tilator outlet 15 cm from the heater, and a filter for aerosol collec-
tion (A) was placed distal to the endotracheal tube (B). Also shown
eter) ventilator circuits were used during the experiments.
are the flow sensor (C) and the Y-piece (D).
A jet nebulizer (GaleMed Corp, Taipei, Taiwan) was placed
proximal to the ventilator 15 cm from the inlet of a heated
pass-over humidifier (MR850, Fisher & Paykel Health-
Statistical Analysis
care, Auckland, New Zealand) operated at 37°C. Aerosols
were collected distal to the ETT by a hydrophobic bacte-
rial filter (GaleMed Corp). Statistical analyses were performed using SPSS 18.0
(SPSS, Chicago, Illinois). Figures were constructed with
Prism 5.0 (GraphPad Software, San Diego, California).
Formulation and Aerosol Delivery Significance was set at P ⫽ .05. Descriptive statistics were
analyzed, and eluted drug amounts were converted to per-
A unit dose of salbutamol (known as albuterol and Ven- centage of total dose. One-way analysis of variance with
tolin Nebules [5 mg/2.5 mL], GlaxoSmithKline, Philadel- Bonferroni post hoc comparisons for normally distributed
phia, Pennsylvania) was diluted with distilled water to a data was used to assess the magnitude of group differences
total fill volume of 4 mL. The nebulizer was powered by for continuous variables. The Kruskal-Wallis test and
the ventilator in 3 nebulization modes: (1) inspiratory in- Mann-Whitney U test for non-normally distributed data
termittent nebulization mode (IIM) synchronized with in- were used to identify group differences in nebulization
spiration phase, (2) continuous nebulization mode (CM), time.
and (3) expiratory intermittent nebulization mode (EIM)
during the expiration phase. Albuterol delivery from the Results
nebulizer was stopped 5 breathing cycles after the onset of
sputter. Six new nebulizers were used for testing with each Drug Delivery
scenario.
With the adult model, drug delivery on the inhalation
Sample Measurement filter distal to the ETT expressed as a percentage of total
dose was between 7.7 and 7.0% of the charged dose in 3
nebulization pattern modes (P ⫽ .99) (Fig. 2A). In con-
Albuterol deposited on the filters, T-pieces, and corru- trast, with the pediatric model, drug delivered by IIM
gated tubing between the nebulizer and heater, as well as trended higher than CM and EIM, without achieving sta-
the residual dose in nebulizers at the end of dosing, was tistical significance (P ⫽ .40) (Fig. 2B). The average per-
eluted with distilled water and analyzed by a spectropho- centage of inhaled dose was similar with all 3 nebulization
tometer (BioMate 3S UV-visible, Thermo Fisher Scien- modes with both adult and pediatric lung models
tific, Waltham, Massachusetts) at 276 nm to quantify drug (7.39 ⫾ 0.76 and 6.27 ⫾ 0.69%, respectively, P ⫽ .77).
mass, which was reported as a percentage of total initial Comparing the drug deposited on the inhaled filter among
dose placed in the nebulizer. Nebulization time from ini- the 3 modes in the pediatric and adult lung models, there
tiation of aerosol generation to 5 breaths after onset of were no significant differences (P ⫽ .2 for IIM, P ⫽ .67
sputter was recorded in minutes. for EIM, and P ⫽ .09 for CM).
1496 RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10
AEROSOL DELIVERY BY DIFFERENT VENTILATOR NEBULIZATION MODES
Table 1. Drug as Percentage of Total Dose Deposited in Nebulizer
and Ventilator Accessory Tubing at End of Aerosol
Administration With 3 Nebulization Modes During
Mechanical Ventilation With Adult and Pediatric
Lung Models
Mode
Deposition IIM CM EIM P
(n ⫽ 6) (n ⫽ 6) (n ⫽ 6)
Adult lung model
Nebulizer, % 40.7 ⫾ 1.8 40.3 ⫾ 1.6 41.6 ⫾ 1.9 .89
Accessory tubes, 9.6 ⫾ 0.1 6.3 ⫾ 0.4* 5.6 ⫾ 0.7† ⬍ .001
%
Pediatric lung model
Nebulizer, % 36.3 ⫾ 6.2 41.9 ⫾ 2.5 40.5 ⫾ 2.3 .66
Accessory tubes, 6.1 ⫾ 0.7 4.7 ⫾ 0.6 4.4 ⫾ 0.4 .11
%
Values are mean ⫾ SD.
* P ⬍ .05, comparison between IIM and CM
† P ⬍ .05, comparison between IIM and EIM
IIM ⫽ inspiratory intermittent mode
CM ⫽ continuous mode
EIM ⫽ expiratory intermittent mode
CM, and 18.8 (IQR 17.5–22.0) min for EIM (P ⬍ .001)
(Fig. 3B). Additionally, nebulization times with the adult
lung model (23.2 ⫾ 2.7 min) and pediatric lung model
(23.4 ⫾ 2.6 min, P ⫽ .79) were similar.
Discussion
Fig. 2. Comparison of inhaled drug mass among 3 modes of neb-
Our results demonstrated similar aerosol delivery effi-
ulization. A: In an adult lung model. B: In a pediatric lung model. ciency for all 3 nebulization modes from a jet nebulizer
placed proximal to the ventilator during mechanical ven-
tilation with both adult and pediatric models. With similar
Table 1 lists the residual drug in nebulizers and on the drug delivery in all 3 modes with the adult model and only
accessory tubes (T-pieces and corrugated tubing) expressed marginally greater delivery with IIM in the pediatric model,
as a percentage of total drug dose (mean ⫾ SD) for the it appears that all modes should be considered viable for
adult and pediatric lung models. The drug deposited on aerosol administration. However, the much longer nebuli-
accessory tubes was greater in IIM than in CM or EIM zation time with IIM for both adult and pediatric models is
(P ⬍ .001 and P ⫽ .04, respectively). In contrast, in the of interest and may be of clinical importance.
pediatric lung model, no statistical difference existed in Our findings are consistent with those of Berlinski and
the amount of albuterol deposited in the nebulizer and on Willis,11 who evaluated delivery of albuterol from jet neb-
the accessory tubes in any mode. ulizers operated continuously at the ventilator (prehumidi-
fier) ranging from 3.6 to 7% compared with ⬍ 2% with
Nebulization Time placement near the patient airway. Using a pediatric model
of mechanical ventilation, Ari et al13 reported deposition at
The median nebulization times were 37.0 (interquartile the ventilator of 4.1–5.2 versus 3.8 – 4.2% at the Y-piece,
range [IQR], 33.3– 42.7) min for IIM, 14.0 (IQR 11.7– with a range of 4.7–5.2 versus 4.0 – 4.7% in the adult model.
14.6) min for CM, and 17.7 (IQR 16.1–22.4) min for EIM Sidler-Moix et al18 evaluated the influences of jet neb-
with the adult lung model. A clear difference existed in ulizer brands and nebulization modes and positions pro-
nebulization time among the 3 modes in the adult lung vided by the Galileo ventilator with the humidification
model (P ⬍ .001) (Fig. 3A). Additionally, in the pediatric system off during nebulization in pediatric lung models.
lung model, median nebulization times were 34.8 (IQR They reported a 3-fold greater drug delivery in EIM (⬃6%)
33.0 – 44.8) min for IIM, 13.84 (IQR 11.8 –15.2) min for with the aerosol generator placed proximal to the ventila-
RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10 1497
AEROSOL DELIVERY BY DIFFERENT VENTILATOR NEBULIZATION MODES
inner diameter), possibly resulting in the trend for higher
delivery with IIM in the pediatric model compared with
the adult model. The actual aerosol generation time is
similar in each mode between the adult and pediatric mod-
els. The lower circuit volume with the pediatric model
likely acts to reduce the reservoir effect with the contin-
uous gas flow through the nebulizer. The dynamics of the
fate of aerosol are different between modes but appear
consistent in each mode for the same time frames of aero-
sol generation.
The compressor of the Galileo ventilator generates a
pressure of 900 mbar during each nebulization. Di Paolo
et al,17 who assessed the pressure-flow relationship, found
that IIM was the least efficient, with lower maximum pres-
sure and lower flow than CM or EIM. They tested flows
provided to a jet nebulizer, which varied between 5.5 and
8.7 L/min. Additionally, they confirmed that the high in-
ternal resistance of the nebulizer used resulted in pro-
longed time to achieve the recommended flow of 5 L/min.
One nebulizer took 0.55 s to reach 5 L/min when the
inspiratory time was set at 0.8 s; thus, the nebulization
time of each breath was as short as 0.25 s. The pediatric
lung model in this study was set to 25 breaths/min with an
inspiratory time of 0.8 s. These settings resulted a median
nebulization time of 34.8 min. Because of the differences
in the breathing frequency between pediatric and adult
models, the calculated inspiratory times were 20 and 17.6 s,
respectively, with expiratory times per min of 40 and 43 s,
respectively. This may explain the similar inhaled dose
between models within each mode of nebulization in both
breathing patterns.
Fig. 3. Comparison of nebulization time among 3 modes of neb-
ulization. A: In an adult lung model. B: In a pediatric lung model.
Goode et al12 placed a jet nebulizer (AeroTech II at
The inspiratory intermittent modes had P ⬍ .001 among the 3 neb- 6 L/min) in the inspiratory limb of an adult ventilator
ulization modes. Whiskers show maximums and minimums, the circuit, with only one set of ventilator parameters used.
center box represents the interquartile range, and the center line Aerosol was administered with continuous jet nebuliza-
denotes the 50th percentile. tion, resulting in delivery efficiencies of 1.2–2.4% with O2
and HeO2, respectively. Ari et al13 reported deposition of
tor compared with IIM (2%) and CM (4%) with the neb- 3.6% from the jet nebulizer placed in the inspiratory limb
ulizer placed near the patient. Their similar inspiratory of a humidified circuit using a nebulizer (Airlife Misty-
time of 0.8 s and expiratory time of 1.6 s (I:E 1:2) pro- Neb, Allegiance Healthcare Corp, McGaw Park, Illinois)
vided 2-fold more time available to generate aerosol dur- operated continuously at 8 L/min gas, VT 500 mL, breath-
ing expiration, which served to charge the ventilator cir- ing frequency of 15 breaths/min, and peak inspiratory flow
cuit, resulting in more aerosol inhaled. They compared of 60 L/min, with deposition increasing to ⬃6% when the
different types of nebulizers as well as different positions jet nebulizer was moved proximal to the ventilator. Our
with those 3 nebulization modes and reported that drug study, with a VT 600 mL, breathing frequency of 16 breaths/
delivery was negatively correlated to the time required to min, and I:E 1:2.5, using an adult circuit and a different
reach the recommended gas flow for a nebulizer.18 Al- nebulizer produced results similar to those obtained by Ari
though we found similar levels of albuterol deposited in et al13 in the proximal position. None of the 3 studies
the inspiratory filter during EIM (⬃6%) with the aerosol isolated I:E as a variable. Different nebulizers, ventilator
generator proximal to the ventilator, IIM and CM deposi- parameters, and measurements in the past 30 y can impact
tion was greater with the proximal position than with place- quantification of delivery efficiency.
ment near the airway. Clinically, as nebulizer treatment time increases, the
The pediatric ventilator circuit (15-mm inner diameter) likelihood that aerosolized drug therapy will be interrupted
has a smaller internal volume than the adult circuit (22-mm by other clinical practices increases. IIM delivered a sim-
1498 RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10
AEROSOL DELIVERY BY DIFFERENT VENTILATOR NEBULIZATION MODES
ilar inhaled drug mass compared with the other 2 nebuli- patients would help establish whether these in vitro results
zation modes, yet drug delivery by IIM required a much are clinically relevant.
longer nebulization time. The use of CM and EIM can be This study was limited to one brand and model of ven-
used for routine nebulization treatment for mechanically tilator. Variations between ventilators may yield different
ventilated patients in hospitals. If time of administration is results. However, based on our finding, unless proven oth-
considered a valued resource, CM and EIM nebulization erwise, paying extra to have a ventilator that allows syn-
would be preferable to IIM. chronized nebulization might not be worth the expense.
The nebulizer in this study was placed 15 cm proximal Clinically, nebulization is terminated either at onset of
to the inlet of the heated humidifier chamber, similar to sputtering or when no aerosols are generated.20 Sputter is
that in previous studies.8,11,13,19 Recently, Berlinski and usually detected via audible and/or visual perceptions,
Willis11 demonstrated that placing a jet nebulizer proximal which may differ among health professionals. We termi-
to the ventilator circuit, both before and after the humid- nated nebulization at 5 breaths post-onset of sputter. Al-
ifier, increases drug delivery in a pediatric circuit. though reports suggest that minimum additional aerosol is
We were surprised to find such similar deposition in all delivered post-onset of sputter, this method may result in
3 modes in both the adult and pediatric models. Our study underestimation of absolute dose if nebulization was run
indicates that the inhaled mass was similar for the adult to dryness; however, because the determination of sputter
and pediatric lung models in all modes studied, likely was applied across all nebulization modes, the relative
because both models had a large internal circuit volume differences in inhaled dose should remain relevant.
acting as a reservoir, including the ventilator circuit and
heated humidification chamber. Thus, we suggest placing Conclusions
a jet nebulizer far from the Y-piece of a ventilator circuit
to decrease its influence on aerosol delivery. Aerosol drug delivery with a jet nebulizer placed prox-
The total inspiratory and expiratory times with both imal to the ventilator was not dependent on nebulization
lung models were similar, resulting in similar inhaled doses. mode provided by the Galileo ventilator during simulated
A considerable amount of aerosol generated in all 3 modes conventional pediatric and adult subject ventilation. The
resides in the inspiratory limb and heater reservoir be- synchronized inspiratory nebulization mode provided sim-
tween breaths. The smaller volume of the pediatric circuit ilar drug delivered distal to the ETT compared with the
would allow the same nebulizer gas flow to wash a greater other 2 modes but required a 3-fold longer nebulization
proportion of the generated aerosol through the circuit, time. Use of EIM and CM nebulization should be consid-
resulting in similar delivery between the 2 models. ered to reduce treatment time.
Analytical results show that drug deposition on the T-
piece and corrugated tubing by IIM was clearly higher REFERENCES
than that by the other 2 modes. The T-piece is the first 1. Coleman DM, Kelly HW, McWilliams BC. Determinants of aero-
impaction site when aerosols are generated by a jet neb- solized albuterol delivery to mechanically ventilated infants. Chest
ulizer. During the inspiratory phase, the aerosol clouds 1996;109(6):1607-1613.
meet the gas flow at the T-piece and corrugated tubing. 2. Dhand R, Tobin MJ. Bronchodilator delivery with metered-dose in-
halers in mechanically-ventilated patients. Eur Respir J 1996;9(3):
The gas flow enhances first impaction; consequently,
585-595.
drug delivery was highest with IIM. During the experi- 3. Fink JB, Dhand R, Grychowski J, Fahey PJ, Tobin MJ. Reconciling
ment, the ventilator waveform showed that the inspiratory in vitro and in vivo measurements of aerosol delivery from a me-
flows were approximately 34 L/min for the adult lung tered-dose inhaler during mechanical ventilation and defining effi-
model and 12 L/min for the pediatric lung model. Higher ciency-enhancing factors. Am J Respir Crit Care Med 1999;159(1):
63-68.
amounts of albuterol were deposited in the T-piece and 4. Fink JB, Dhand R, Duarte AG, Jenne JW, Tobin MJ. Aerosol de-
corrugated tubing in the adult lung model than in the pe- livery from a metered-dose inhaler during mechanical ventilation.
diatric lung model. An in vitro model. Am J Respir Crit Care Med 1996;154(2):382-387.
A limitation of this study is that we compared only one 5. Hess DR, Dillman C, Kacmarek RM. In vitro evaluation of aerosol
bronchodilator delivery during mechanical ventilation: pressure-con-
set of ventilator parameters for both adult and pediatric
trol vs. volume control ventilation. Intensive Care Med 2003;29(7):
lung models (based on physiologic parameters). Further 1145-1150.
evaluation with a broader range of ventilator modes and 6. Miller DD, Amin MM, Palmer LB, Shah AR, Smaldone GC. Aerosol
parameters and types of nebulizers was beyond the scope delivery and modern mechanical ventilation: in vitro/in vivo evalu-
of this study but would add greater insight on the impact ation. Am J Respir Crit Care Med 2003;168(10):1205-1209.
7. O’Riordan TG, Weinstein MD, Mao Y. Bench testing of nebulizers:
of nebulization modes. Further investigations with various a comparison of three methods. J Aerosol Med 1999;12(2):59-66.
breathing patterns are warranted. Because this was an 8. Ari A, Atalay OT, Harwood R, Sheard MM, Aljamhan EA, Fink JB.
in vitro study, clinical studies of mechanically ventilated Influence of nebulizer type, position, and bias flow on aerosol drug
RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10 1499
AEROSOL DELIVERY BY DIFFERENT VENTILATOR NEBULIZATION MODES
delivery in simulated pediatric and adult lung models during me- 15. Quinn WW. Effect of a new nebulizer position on aerosol delivery
chanical ventilation. Respir Care 2010;55(7):845-851. during mechanical ventilation: a bench study. Respir Care 1992;
9. Garner SS, Wiest DB, Bradley JW. Albuterol delivery by metered- 37(5):423-431.
dose inhaler with a pediatric mechanical ventilatory circuit model. 16. MacIntyre NR, Silver RM, Miller CW, Schuler F, Coleman RE.
Pharmacotherapy 1994;14(2):210-214. Aerosol delivery in intubated, mechanically ventilated patients. Crit
10. Pelkonen AS, Nikander K, Turpeinen M. Jet nebulization of budes- Care Med 1985;13(2):81-84.
onide suspension into a neonatal ventilator circuit: synchronized versus 17. Di Paolo ER, Pannatier A, Cotting J. In vitro evaluation of broncho-
continuous nebulizer flow. Pediatr Pulmonol 1997;24(4):282-286. dilator drug delivery by jet nebulization during pediatric mechanical
11. Berlinski A, Willis JR. Albuterol delivery by 4 different nebulizers ventilation. Pediatr Crit Care Med 2005;6(4):462-469.
placed in 4 different positions in a pediatric ventilator in vitro model. 18. Sidler-Moix AL, Dolci U, Berger-Gryllaki M, Pannatier A, Cotting
Respir Care 2013;58(7):1124-1133. J, Di Paolo ER. Albuterol delivery in an in vitro pediatric ventilator
12. Goode ML, Fink JB, Dhand R, Tobin MJ. Improvement in aerosol lung model: comparison of jet, ultrasonic, and mesh nebulizers. Pe-
delivery with helium-oxygen mixtures during mechanical ventila- diatr Crit Care Med 2013;14(2):e98–e102.
tion. Am J Respir Crit Care Med 2001;163(1):109-114. 19. Moraine JJ, Truflandier K, Vandenbergen N, Berré J, Mélot C, Vincent
13. Ari A, Areabi H, Fink JB. Evaluation of aerosol generator devices at JL. Placement of the nebulizer before the humidifier during mechanical
3 locations in humidified and non-humidified circuits during adult ventilation: effect on aerosol delivery. Heart Lung 2009;38(5):435-439.
mechanical ventilation. Respir Care 2010;55(7):837-844. 20. Dolovich MB, Ahrens RC, Hess DR, Anderson P, Dhand R, Rau JL, et
14. Hughes JM, Saez J. Effects of nebulizer mode and position in a al. Device selection and outcomes of aerosol therapy: evidence-based
mechanical ventilator circuit on dose efficiency. Respir Care 1987; guidelines: American College of Chest Physicians/American College of
32(12):1131-1135. Asthma, Allergy, and Immunology. Chest 2005;127(1):335-371.
This article is approved for Continuing Respiratory Care Education
credit. For information and to obtain your CRCE
(free to AARC members) visit
www.rcjournal.com
1500 RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10
You might also like
- Jurnal Nebulizer VentilatorDocument10 pagesJurnal Nebulizer VentilatorDessyani WulandariNo ratings yet
- 3D Lung Models for Regenerating Lung TissueFrom Everand3D Lung Models for Regenerating Lung TissueGunilla Westergren-ThorssonNo ratings yet
- Vibrating Mesh Nebulisers - Can Greater Drug DelivDocument11 pagesVibrating Mesh Nebulisers - Can Greater Drug DelivShabilah Novia SNo ratings yet
- Monitoring Mechanical Ventilation Using Ventilator WaveformsFrom EverandMonitoring Mechanical Ventilation Using Ventilator WaveformsNo ratings yet
- Aerosol TherapyDocument10 pagesAerosol Therapy04lubna_869632400No ratings yet
- 1 s2.0 S2590156723000117 MainDocument10 pages1 s2.0 S2590156723000117 MainArpad FarkasNo ratings yet
- Jerath2020_Article_InhalationalVolatile-basedSedaDocument4 pagesJerath2020_Article_InhalationalVolatile-basedSedasncr.gnyNo ratings yet
- Newer Modes of Ventilation2Document9 pagesNewer Modes of Ventilation2Saradha PellatiNo ratings yet
- Effects of High-Flow Nasal Cannula On End-Expiratory Lung Impedance in Semi-Seated Healthy SubjectsDocument8 pagesEffects of High-Flow Nasal Cannula On End-Expiratory Lung Impedance in Semi-Seated Healthy SubjectsJulieta EvangelistaNo ratings yet
- Lung Function Assessment by ImpulseDocument12 pagesLung Function Assessment by Impulsethiago gibsonNo ratings yet
- High Frequency Ventilation NeorevDocument16 pagesHigh Frequency Ventilation NeorevLuis Adolfo Gonzalez GomezNo ratings yet
- Airway Management During Upper GI Endoscopic Procedures2016Document9 pagesAirway Management During Upper GI Endoscopic Procedures2016jcarl_20063003No ratings yet
- Asynchrony Consequences and ManagementDocument17 pagesAsynchrony Consequences and ManagementLexNo ratings yet
- Mechanical VentilationDocument5 pagesMechanical VentilationCherry Kris Caperig SuarezNo ratings yet
- Cánula Asimétrica en Paciente HipoxémicoDocument12 pagesCánula Asimétrica en Paciente HipoxémicoEdgar PandoNo ratings yet
- 1 s2.0 S0196070922003945 MainDocument8 pages1 s2.0 S0196070922003945 MainJose Miguel CastellonNo ratings yet
- Hfo 3Document8 pagesHfo 3markus_danusantosoNo ratings yet
- Asynchrony Consequences and ManagementDocument17 pagesAsynchrony Consequences and ManagementAna MariaNo ratings yet
- Effect of Nebulized Suctioning With 3% Hypertonic Saline For Mechanically Ventilated Patient On Airway ClearanceDocument5 pagesEffect of Nebulized Suctioning With 3% Hypertonic Saline For Mechanically Ventilated Patient On Airway ClearanceInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Jet Ultrasonic and Mesh Nebulizers - An Evaluation of NebulizersDocument8 pagesJet Ultrasonic and Mesh Nebulizers - An Evaluation of NebulizersEsan DermawanNo ratings yet
- 1fca PDFDocument13 pages1fca PDFHalim SudonoNo ratings yet
- Applsci 09 02842 PDFDocument13 pagesApplsci 09 02842 PDFFelicia SutarliNo ratings yet
- Wang 2022Document11 pagesWang 2022Carlos Daniel AliagaNo ratings yet
- Intraoperative Mechanical Ventilation Strategies in Patients Undergoing One-Lung Ventilation: A Meta-AnalysisDocument12 pagesIntraoperative Mechanical Ventilation Strategies in Patients Undergoing One-Lung Ventilation: A Meta-AnalysisdrvmkamathNo ratings yet
- In Support of Pressure Support: Subrata Sarkar, MD, Steven M. Donn, MDDocument12 pagesIn Support of Pressure Support: Subrata Sarkar, MD, Steven M. Donn, MDSiska LesnussaNo ratings yet
- Astma in ICUDocument16 pagesAstma in ICUkillingeyes177No ratings yet
- Mojoli 2023 Tidal Lung Hysteresis To Interpret PEEP-induced Changes in Compliance in ARDS PatientsDocument10 pagesMojoli 2023 Tidal Lung Hysteresis To Interpret PEEP-induced Changes in Compliance in ARDS PatientsKhanh Ha NguyenNo ratings yet
- Mechanical Ventilation Dyssynchrony Types and ManagementDocument17 pagesMechanical Ventilation Dyssynchrony Types and ManagementjuanNo ratings yet
- WWW Minervamedica It@r02y2016n01a0058Document11 pagesWWW Minervamedica It@r02y2016n01a0058Gonzalo Venegas RojasNo ratings yet
- Modes of Mechanical Ventilation For The Operating Room BestPracResAnest 2015 PDFDocument15 pagesModes of Mechanical Ventilation For The Operating Room BestPracResAnest 2015 PDFRicardoNo ratings yet
- Novel Forms of Ventilation in Neonates Neurally Adjusted VentilatoryDocument16 pagesNovel Forms of Ventilation in Neonates Neurally Adjusted VentilatorydocsaravananNo ratings yet
- Anestesiologi EmergencyDocument12 pagesAnestesiologi EmergencyJodhy MaulanaNo ratings yet
- Research Proposal: MPT (Cardio Respiratory Disorders)Document14 pagesResearch Proposal: MPT (Cardio Respiratory Disorders)permanaNo ratings yet
- Volume-Targeted Modes of Modern Neonatal Ventilators: How Stable Is The Delivered Tidal Volume?Document10 pagesVolume-Targeted Modes of Modern Neonatal Ventilators: How Stable Is The Delivered Tidal Volume?DawoodNo ratings yet
- Tradition of Excellence: Use of Suction in Mechanically Ventilated ICU PatientsDocument7 pagesTradition of Excellence: Use of Suction in Mechanically Ventilated ICU PatientsnandaavistaNo ratings yet
- Research Paper VapDocument14 pagesResearch Paper Vapapi-401343496No ratings yet
- CNAF Post ExtubacionDocument10 pagesCNAF Post ExtubacionpelaojaegerNo ratings yet
- Ventilación Del Pulmón Sano CC Current 20Document5 pagesVentilación Del Pulmón Sano CC Current 20Silvia Lorena Mireles GonzálezNo ratings yet
- Short Term Effect of An Active Heat and Moisture Exchanger During Invasive VentilationDocument7 pagesShort Term Effect of An Active Heat and Moisture Exchanger During Invasive VentilationekaNo ratings yet
- Respiratory Disorders Pressure Support Ventilation Reduces Added Work of BreathingDocument8 pagesRespiratory Disorders Pressure Support Ventilation Reduces Added Work of BreathingAli Mohamed AbdallaNo ratings yet
- Med 9780199600830 Chapter 97Document7 pagesMed 9780199600830 Chapter 97Kiki Sri Rejeki AgisinaNo ratings yet
- En - Paper Bias FlowDocument2 pagesEn - Paper Bias FlowBryan MaldonadoNo ratings yet
- Nasal high-frequency ventilation overviewDocument22 pagesNasal high-frequency ventilation overviewdragajojicNo ratings yet
- Bertoni 2019Document10 pagesBertoni 2019MISSAEL ESPINOZANo ratings yet
- Future Options For Aerosol Delivery To Children: Allergy February 1999Document8 pagesFuture Options For Aerosol Delivery To Children: Allergy February 1999Suada HalimiNo ratings yet
- Applsci 09 02007Document18 pagesApplsci 09 02007DevasyaNo ratings yet
- Closed Vs Open SuctionDocument5 pagesClosed Vs Open SuctionKhushboo DurejaNo ratings yet
- Modes and Strategies For Providing Conventional Mechanical Ventilation in NeonatesDocument6 pagesModes and Strategies For Providing Conventional Mechanical Ventilation in Neonatesbig023296No ratings yet
- LISTA 2012_Surfactant and mechanical ventilationDocument3 pagesLISTA 2012_Surfactant and mechanical ventilationRafael JustinoNo ratings yet
- Do Commonly Used Ventilator SettingsDocument6 pagesDo Commonly Used Ventilator Settingsnatalia muñozNo ratings yet
- Comparative Efficacy of SPONTANEOUS BREATHING TRIAL Techniques in Mechanically Ventilated Adult Patients A ReviewDocument6 pagesComparative Efficacy of SPONTANEOUS BREATHING TRIAL Techniques in Mechanically Ventilated Adult Patients A ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Evidence-based role of high-frequency ventilation in neonatal respiratory failureDocument16 pagesEvidence-based role of high-frequency ventilation in neonatal respiratory failureSiska LesnussaNo ratings yet
- Lavorini Et Al Respiration 2014Document14 pagesLavorini Et Al Respiration 2014Miriam BlejerNo ratings yet
- Is Mechanical Power An Under-Recognised Entity WitDocument8 pagesIs Mechanical Power An Under-Recognised Entity WitManoj kumar DasariNo ratings yet
- Jurnal ALFIA NOFITASARI (200902027)Document7 pagesJurnal ALFIA NOFITASARI (200902027)Gede Kevin Adhitya SaputraNo ratings yet
- Articulo Effect of Flashlight Guidance On Manual Ventilation Performance in Cardiopulmonary Resuscitation A Randomized Controlled Simulation StudyDocument11 pagesArticulo Effect of Flashlight Guidance On Manual Ventilation Performance in Cardiopulmonary Resuscitation A Randomized Controlled Simulation StudyCindy Katherine LlanosNo ratings yet
- HFOV (Book)Document37 pagesHFOV (Book)sajjad alhajjiNo ratings yet
- Aerosol Drug Delivery Developments in Device Design andDocument14 pagesAerosol Drug Delivery Developments in Device Design andEdgard Eduardo Azañero EstradaNo ratings yet
- Hfo 2Document9 pagesHfo 2markus_danusantosoNo ratings yet
- Reviews: Cardiogenic Shock: Failure of Oxygen Delivery and Oxygen UtilizationDocument7 pagesReviews: Cardiogenic Shock: Failure of Oxygen Delivery and Oxygen Utilizationhana haniNo ratings yet
- Arterial Blood Gases and Oxygen Content in Climbers On Mount EverestDocument10 pagesArterial Blood Gases and Oxygen Content in Climbers On Mount EveresthendersonNo ratings yet
- Do Commonly Used Ventilator SettingsDocument6 pagesDo Commonly Used Ventilator Settingsnatalia muñozNo ratings yet
- Heat Andmoisture Exchangers Versus Heated HumidifierDocument73 pagesHeat Andmoisture Exchangers Versus Heated Humidifiernatalia muñozNo ratings yet
- RedactedDocument24 pagesRedactedJohn HarrisNo ratings yet
- Fi & EiDocument3 pagesFi & EiPrasanna S Kulkarni100% (1)
- Oxygen Concentrator SpecificationsDocument3 pagesOxygen Concentrator Specificationsmino pharmNo ratings yet
- ON Code (Aci 318-77) : Commentary Building Requirements For Reinforced ConcreteDocument132 pagesON Code (Aci 318-77) : Commentary Building Requirements For Reinforced ConcreteAzmi BazazouNo ratings yet
- Water Spray Nozzle: Fire Fighting Equipment Data SheetDocument7 pagesWater Spray Nozzle: Fire Fighting Equipment Data SheetJosef MadronaNo ratings yet
- Enzyme ActivityDocument3 pagesEnzyme ActivityNabindra Ruwali100% (2)
- Shadows On The Moon by Zoe Marriott ExtractDocument20 pagesShadows On The Moon by Zoe Marriott ExtractWalker Books100% (1)
- Catalogo Tecnico Gb-S v07Document29 pagesCatalogo Tecnico Gb-S v07farou9 bmzNo ratings yet
- Marketing 5 0Document23 pagesMarketing 5 0gmusicestudioNo ratings yet
- Waste Management in Vienna. MA 48Document12 pagesWaste Management in Vienna. MA 484rtttt4ttt44No ratings yet
- Accepted Manuscript: Process Safety and Environment ProtectionDocument51 pagesAccepted Manuscript: Process Safety and Environment Protectionimran shaukatNo ratings yet
- Airway Management in The Critically Ill: ReviewDocument9 pagesAirway Management in The Critically Ill: ReviewQuarmina HesseNo ratings yet
- Kant On Religion and ScienceDocument21 pagesKant On Religion and ScienceEduardo CharpenelNo ratings yet
- Iodine Summaryupdate 2016Document26 pagesIodine Summaryupdate 2016FrankNo ratings yet
- ZTE UMTS KPI Optimization Analysis Guide V1 1 1Document62 pagesZTE UMTS KPI Optimization Analysis Guide V1 1 1GetitoutLetitgo100% (1)
- Determine PH by PH Indicator and Universal IndicatorDocument3 pagesDetermine PH by PH Indicator and Universal IndicatorhaleelNo ratings yet
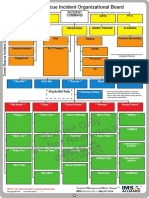
- Sample Only Do Not Reproduce: Trench Rescue Incident Organizational BoardDocument1 pageSample Only Do Not Reproduce: Trench Rescue Incident Organizational BoardLuis Diaz CerdanNo ratings yet
- How To Attract Love and Powerful Soul ConnectionsDocument5 pagesHow To Attract Love and Powerful Soul Connectionskinzaali71916No ratings yet
- Ac+lic Lab Manual 2018-19Document76 pagesAc+lic Lab Manual 2018-19Samanvi SaatviNo ratings yet
- Material ManagementDocument106 pagesMaterial ManagementRomi AfriansyahNo ratings yet
- Column FootingDocument57 pagesColumn Footingnuwan01100% (7)
- Beneficiation of Cassiterite From Primary Tin OresDocument11 pagesBeneficiation of Cassiterite From Primary Tin OresSULMAGNo ratings yet
- LEEA-036 (B) - Academy ITS Practical Training Courses Jan - June 2020 Version 1 October 2019Document18 pagesLEEA-036 (B) - Academy ITS Practical Training Courses Jan - June 2020 Version 1 October 2019kaito kurabaNo ratings yet
- 16 Balance TestDocument15 pages16 Balance Testelga saniNo ratings yet
- 21st Century Science - Summer 2011 - The Universe Is CreativeDocument84 pages21st Century Science - Summer 2011 - The Universe Is CreativeMatthew EhretNo ratings yet
- DesignDocument2 pagesDesignAmr AbdalhNo ratings yet
- Solar Collectors Final WordDocument14 pagesSolar Collectors Final WordVaibhav Vithoba NaikNo ratings yet
- Whirlpool - Service Information Frontloader Washing Machine AWO/D 43115Document53 pagesWhirlpool - Service Information Frontloader Washing Machine AWO/D 43115amandialopes50% (2)
- Mathematical Structures of The UniverseDocument228 pagesMathematical Structures of The UniverseMaki MajomNo ratings yet
- Lab ReportDocument9 pagesLab ReportQi Yi TanNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (15)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)