Professional Documents
Culture Documents
1fca PDF
Uploaded by
Halim SudonoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
1fca PDF
Uploaded by
Halim SudonoCopyright:
Available Formats
Neonatal and Adult ICU Ventilators to Provide Ventilation in
Neonates, Infants, and Children: A Bench Model Study
Laurence Vignaux PhD, Lise Piquilloud MD, Pierre Tourneux MD,
Philippe Jolliet MD, and Peter C Rimensberger MD
BACKGROUND: Using a bench test model, we investigated the hypothesis that neonatal and/or
adult ventilators equipped with neonatal/pediatric modes currently do not reliably administer
pressure support (PS) in neonatal or pediatric patient groups in either the absence or presence of
air leaks. METHODS: PS was evaluated in 4 neonatal and 6 adult ventilators using a bench model
to evaluate triggering, pressurization, and cycling in both the absence and presence of leaks.
Delivered tidal volumes were also assessed. Three patients were simulated: a preterm infant (re-
sistance 100 cm H2O/L/s, compliance 2 mL/cm H2O, inspiratory time of the patient [TI] 400 ms,
inspiratory effort 1 and 2 cm H2O), a full-term infant (resistance 50 cm H2O/L/s, compliance
5 mL/cm H2O, TI 500 ms, inspiratory effort 2 and 4 cm H2O), and a child (resistance 30 cm H2O/L/s,
compliance 10 mL/cm H2O, TI 600 ms, inspiratory effort 5 and 10 cm H2O). Two PS levels were
tested (10 and 15 cm H2O) with and without leaks and with and without the leak compensation
algorithm activated. RESULTS: Without leaks, only 2 neonatal ventilators and one adult ventilator
had trigger delays under a given predefined acceptable limit (1/8 TI). Pressurization showed high
variability between ventilators. Most ventilators showed TI in excess high enough to seriously
impair patient-ventilator synchronization (> 50% of the TI of the subject). In some ventilators,
leaks led to autotriggering and impairment of ventilation performance, but the influence of leaks
was generally lower in neonatal ventilators. When a noninvasive ventilation algorithm was avail-
able, this was partially corrected. In general, tidal volume was calculated too low by the ventilators
in the presence of leaks; the noninvasive ventilation algorithm was able to correct this difference in
only 2 adult ventilators. CONCLUSIONS: No ventilator performed equally well under all tested
conditions for all explored parameters. However, neonatal ventilators tended to perform better in
the presence of leaks. These findings emphasize the need to improve algorithms for assisted ventilation
modes to better deal with situations of high airway resistance, low pulmonary compliance, and the
presence of leaks. Key words: mechanical ventilators; ventilatory support; neonatal; pediatrics; inten-
sive care units; equipment safety; respiration; artificial; models. [Respir Care 2014;59(10):1463–1475.
© 2014 Daedalus Enterprises]
Introduction children are prone to respiratory failure and possibly re-
quire respiratory support via mechanical ventilation de-
Because of anatomic characteristics (small airway di-
spite their youth. Using assisted ventilation modes (during
ameter) and specific respiratory mechanics (high resis-
which the patient is given the opportunity to trigger the
tance and low compliance) and because they often suffer
ventilator) is effective in increasing patients’ comfort1 and
from infectious airway diseases, neonates, infants, and small
Dr Vignaux is affiliated with the Cardio-Respiratory Physiotherapy Unit, Geneva, Switzerland. Drs Piquilloud and Jolliet are affiliated with the
Hôpital de La Tour, Meyrin, Switzerland. Drs Vignaux and Tourneux are Adult Intensive Care and Burn Unit, University Hospital of Lausanne,
affiliated with Peritox, EA 4284-Unité Mixte I01, L’Institut National de Lausanne, Switzerland. Dr Tourneux is also affiliated with the Pedi-
l’Environnement Industriel et des Risques, Université de Picardie Jules atric Intensive Care Unit, University Hospital North, Amiens, France.
Verne, Amiens, France. At the time of this study, Dr Vignaux was Dr Rimensberger is affiliated with the Neonatal and Pediatric Intensive
affiliated the Adult Intensive Care Unit, University Hospital of Geneva, Care Unit, University Hospital of Geneva, Geneva, Switzerland.
RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10 1463
ICU VENTILATORS FOR NEONATES, INFANTS, AND CHILDREN
limiting ventilator-induced diaphragmatic dysfunction2
compared with controlled ventilation modes. Assisted ven- QUICK LOOK
tilation modes, particularly pressure support ventilation Current knowledge
(PSV), have been increasingly used as an alternative to
controlled mechanical ventilation. This change of practice Mechanical ventilation of the neonate is complicated by
is encouraged by the results of a meta-analysis showing the requirement for small-diameter uncuffed endotra-
that using various modes of assisted ventilation compared cheal tubes and the presence of a variable leak. The
with pure controlled mechanical ventilation in neonates performance of ventilators in the pressure support mode
was associated with a shorter duration of mechanical ven- in this scenario is a technical challenge.
tilation.3
What this paper contributes to our knowledge
Neonatal ventilators performed better in the presence of
high resistance, low compliance, and leaks than venti-
SEE THE RELATED EDITORIAL ON PAGE 1606 lators capable of adult and neonatal ventilation. No one
ventilator performed optimally under all the test con-
ditions. The use of the noninvasive algorithms on adult
However, a major difficulty using assisted ventilation ventilators improved performance in this scenario ex-
and especially PSV in small children (related to the use of cept for one device.
uncuffed endotracheal tubes) is the presence of air leaks,
which, as reported previously in adult studies,4,5 can be
related to poor patient-ventilator synchrony. Specifically,
significant air leaks are present in ⬃70% of invasively Methods
ventilated neonates and are responsible for frequent auto-
triggering during assisted ventilation in this patient popu- Ventilators
lation.6 Ten ICU ventilators, commonly available in Europe to
It was reported previously that during assisted pressure ventilate neonates and small children, were tested in the
controlled ventilation (patient-triggered, pressure-targeted, Mechanical Ventilation Research Laboratory in the Adult
time-cycled), adult ventilators equipped with a neonatal Intensive Care Unit of the University Hospital of Geneva.
mode responded faster and more efficiently to a patient’s Among these ventilators, there were 4 neonatal ventilators
effort compared with a specific neonatal ventilator, the (SLE 5000, SLE Ltd, South Croydon, United Kingdom;
Babylog 8000 (Dräger, Lübeck, Germany).7 As differences Leoni Plus, Heinen ⫹ Löwenstein, Bad Ems, Germany;
in ventilator technical performance can influence patient- Babylog VN500, Dräger; Fabian, Acutronic Medical Sys-
ventilator synchrony during PSV, a better understanding tems AG, Hirzel, Switzerland) and 6 adult ventilators
of these differences would influence daily pediatric clini- equipped with a neonatal/pediatric option (Servo-i, Ma-
cal practice regarding mechanical ventilation. Addition- quet, Wayne, New Jersey; Evita XL NeoFlow, Dräger;
ally, this knowledge could be of major interest when com- Engström Carestation, GE Healthcare, Madison, Wiscon-
paring improved patient-ventilator synchrony documented sin; PB840, Covidien, Mansfield, Massachusetts; Avea,
with neurally adjusted ventilatory assist.8,9 CareFusion, San Diego, California; G5, Hamilton Medi-
The purpose of this study was to investigate, using a cal, Reno, Nevada). The main characteristics of these ven-
bench model, the hypothesis that neonatal and/or adult tilators are summarized (see the supplementary materials
ventilators equipped with neonatal/pediatric modes cur- at http://www.rcjournal.com).
rently do not reliably administer pressure support (PS) in
the absence or presence of air leaks. Bench Model
A bench model derived from the one we used in our
previous bench studies10-12 adapted to simulate specific neo-
Supplementary material related to this paper is available at http:// natal, infant, and pediatric respiratory mechanics was used
www.rcjournal.com. for this study (Fig. 1). Briefly, the model (Adult/Infant
The authors have disclosed no conflicts of interest. Training and Test Lung, Michigan Instruments, Grand
Rapids, Michigan) consisted of 2 separate chambers
Correspondence: Laurence Vignaux PhD, Cardio-Respiratory Physiother- linked by a rigid metal strip. The first chamber was con-
apy Department, Hôpital de La Tour, 3 Avenue JD Maillard, 1217 Mey-
rin, Switzerland. E-mail: laurence.vignaux@latour.ch. nected to a driver ventilator (Evita 4, Dräger), which sim-
ulates patient inspiratory effort.10-12 The second chamber,
DOI: 10.4187/respcare.02540 a neonatal/pediatric compartment, was connected to the
1464 RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10
ICU VENTILATORS FOR NEONATES, INFANTS, AND CHILDREN
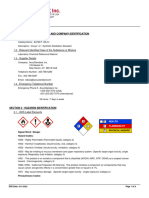
Fig. 1. Experimental setup. A neonatal/pediatric lung model was ventilated by a tested ventilator and triggered by a driver ventilator. Tidal
volume was measured by the ventilator at the Y-piece and by a pneumotachograph at the lung compartment model. Different endotracheal
tube leaks were simulated by open tubes of different lengths. Data were acquired online via an analog-to-digital converter and stored in a
laptop computer for subsequent analysis.
ventilator being tested using a ventilator circuit equipped product at 300 ms (PTP300) to assess global pressuriza-
with a system designed to create intentional leaks (leak tion capacity, and inspiratory time in excess (TIex) to assess
generator). Its total lung capacity was 200 mL, its residual cycling off. Delivered tidal volumes (VT) were also mea-
volume was 70 mL, and its compliance could be adjusted sured and compared with VT displayed by the machines.
from 1 to 15 mL/cm H2O. The rigid metal strip placed PTP300 was expressed as a percentage of an ideal PTP300
between the 2 chambers allowed the transmission of the (illustrated in Fig. 2), defined as the PTP300 that would
inspiratory effort from the first chamber to the second. have been delivered if the delivered pressurization had
The second chamber was free during expiration. The in- immediately reached its maximum value (ie, no trigger
spiratory effort generated by the driver ventilator was de- delay and no rise time).
tected by the ventilator being tested, which, in response, A maximum trigger delay of 100 ms,13,14 corresponding
initiated pressurization according to the chosen settings. to ⬃12.5% of the mean TI of 800 ms,4,15-17 is usually
To perform the measurements, 3 flow sensors and pressure considered as acceptable in adult patients. In this study,
transducers (Hamilton Medical) were inserted in the cir- inspiratory times of 400, 500, and 600 ms to simulate a
cuit between the driver ventilator and the lung model, preterm neonate, a full-term neonate, and a child were
between the lung model and the leak system, and between used, respectively (hereafter referred to as patient type).
the leak system and the ventilator being tested. Data were Therefore, we considered trigger delays of 50, 60, and
recorded online using an analog-to-digital converter 70 ms as acceptable upper limits for the 3 simulated pa-
(MP100, Biopac Systems, Goleta, California), sampled at tient types, respectively.
500 Hz, and stored in a laptop computer for subsequent
analysis (AcqKnowledge software, Biopac Systems). All Leaks
measurements were performed at an FIO2 of 0.21.
Leaks were generated by using open silicone tubes
Measured Parameters (1.5-mm inner diameter) of 3 different lengths (one spe-
cific length for each simulated patient type) attached to a
The various parameters commonly used to assess ven- 3-way stopcock inserted between the Y-piece of the ven-
tilator performance during PSV were measured from the tilator circuit and the lung model. The amount of leakage
recorded curves (for detailed explanations, see the supple- obtained was computed by subtracting the flow measured
mentary materials at http://www.rcjournal.com)12: trigger after leak generation from the flow measured before it.12
delay to assess the ventilator response time, pressure-time The leak flows obtained with a continuous PEEP of
RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10 1465
ICU VENTILATORS FOR NEONATES, INFANTS, AND CHILDREN
inspiratory efforts 5 and 10 cm H2O (R30C10). As the
amplitude of inspiratory efforts varies in children in gen-
eral18,19 and can, under some circumstances such as during
sleep or with small infants, be very low,20-22 we chose to
simulate this as well. Neonatal options of the Fabian and
Evita XL NeoFlow ventilators were tested with R100C2,
and R50C5; pediatric options of the same ventilators were
tested with R50C5 and R30C10.
Each ventilator was tested in PSV mode with the fol-
lowing settings: maximum sensitivity inspiratory flow trig-
ger while avoiding autotriggering, PEEP 5 cm H2O, PS
levels 10 and 15 cm H2O, backup ventilation deactivated,
expiratory trigger setting (ETS) at 15% of the peak in-
Fig. 2. Measured parameters. Trigger delay (Td) is the time be- spiratory flow (except the Leoni Plus ventilator, which has
tween the beginning of the inspiratory effort and the minimum a non-modifiable ETS of 25%). If adjustable, the maxi-
value measured on the pressure curve during the triggering phase.
The pressure-time product at 300 ms (PTP300) is expressed as a mum TI was set to the highest value possible to avoid
percentage of the ideal PTP, which corresponds to the PTP300 time-based cycling.
that would have been delivered if the pressurization delivered had To test the influence of the leaks on ventilation perfor-
immediately reached its maximum value (ie, no trigger delay and mance, tests were carried out while applying the 3 follow-
no rise time), and is represented by the rectangle. TI ⫽ inspiratory
time of the patient (duration of inspiration by the patient [driver ing leakage scenarios: (1) in the absence of leaks and with
ventilator]). TIex ⫽ TI in excess (duration of pressurization by the the ventilator leak compensation algorithm or noninvasive
ventilator in excess of patient inspiratory duration). P aw ⫽ airway ventilation (NIV) algorithm deactivated, (2) in the pres-
pressure. ence of leaks and with the NIV algorithm (which should
theoretically compensate for the presence of leaks) deac-
tivated, and (3) in the presence of leaks and with the NIV
algorithm activated. For each tested condition (patient type
5 cm H2O for the 3 tested patient types were 0.6 L/min plus leakage scenario), 2 min were recorded. Between 2
(0.01 L/s) for a resistance of 100 cm H2O/L/s and a com- different conditions, a washout period of 2 min was ob-
pliance of 2 mL/cm H2O with a tube of 343 cm, 1.2 L/min served.
(0.02 L/s) for a resistance of 50 cm H2O/L/s and a com-
pliance of 5 mL/cm H2O with a tube of 172 cm, and
2.4 L/min (0.04 L/s) for a resistance of 30 cm H2O/L/s and Statistical Analysis
a compliance of 10 mL/cm H2O with a tube of 95 cm.
For each tested condition, 10 consecutive, interpretable,
Experiment Protocol and triggered respiratory cycles (starting from the second
recorded cycle) were considered for the analyses. All re-
The driver ventilator was set in airway pressure release sults are expressed as mean ⫾ SD.
ventilation mode. Thus, the inspiratory effort generated For each simulated patient type, the measured parame-
was equal to the set pressure above PEEP.10-12 The base-
ters were compared between the different respiration sce-
line breathing frequency was 20 breaths/min. In the case of
narios (with or without leaks and with or without the NIV
air trapping related to delayed cycling, the breathing fre-
algorithm activated) by repeated measures analysis of vari-
quency was decreased to allow complete expiration, which
ance, followed by a pairwise multiple comparison proce-
was assessed using visualization of the flow curve (expi-
ration was considered complete when the flow curve came dure for post hoc analysis (Student-Newman-Keuls
back to 0 before the start of the next inspiratory effort). method) when analysis of variance was statistically sig-
The various ventilators were tested with the 3 simulated nificant.
patient types. Preterm infant settings were: resistance All statistical analyses were performed using SigmaStat 2.0
100 cm H2O/L/s, compliance 2 mL/cm H2O, TI 400 ms, (Systat, San Jose, California). P ⬍ .05 was considered
inspiratory efforts 1 and 2 cm H2O (R100C2). Full-term statistically significant. Only data that had a difference of
infant settings were: resistance 50 cm H2O/L/s, compli- ⬎ 10% in absolute value was considered clinically rele-
ance 5 mL/cm H2O, TI 500 ms, inspiratory efforts 2 and vant. Only clinically relevant and statistically significant
4 cm H2O (R50C5). Child settings were: resistance data are provided in the tables and figures and considered
30 cm H2O/L/s, compliance 10 mL/cm H2O, TI 600 ms, for discussion.
1466 RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10
ICU VENTILATORS FOR NEONATES, INFANTS, AND CHILDREN
Fig. 3. Trigger delay with the 10 ventilators tested with 3 different types of patients: a preterm infant (resistance 100 cm H2O/L/s, compliance
2 mL/cm H2O, inspiratory time [TI] 400 ms, inspiratory effort 1 and 2 cm H2O [R100C2]), a full-term infant (resistance 50 cm H2O/L/s,
compliance 5 mL/cm H2O, TI 500 ms, inspiratory effort 2 and 4 cm H2O [R50C5]), and a child (resistance 30 cm H2O/L/s, compliance
10 mL/cm H2O, TI 600 ms, inspiratory effort 5 and 10 cm H2O [R30C10]). Two pressure support levels (10 and 15 cm H2O) were tested;
results are pooled. Histogram bars are mean ⫾ SD.
Results effort increasing). Except for the G5 and Engström Care-
station, PTP300 values were clearly below 50% of the
Ventilation Performance in the Absence of Leaks ideal PTP300 in at least one of the 3 simulated patient
types.
Triggering: Trigger Delays. For simulated neonatal ven-
tilation, 3 neonatal ventilators (Leoni Plus, SLE 5000, and Cycling: TIex. Most ventilators had a very high TIex (ie,
Fabian) and one adult ventilator (Avea) had trigger delays ⬎ 50% of the patient’s TI). The TIex sometimes varied a lot
below the predefined acceptable limit (Fig. 3). For simu- for a single ventilator between various simulated patient
lated child ventilation, 2 neonatal ventilators (Leoni Plus types (Fig. 5). Three ventilators (Babylog VN500, G5, and
and SLE 5000) and one adult ventilator (G5) had trigger Servo-i) had a clearly lower TIex compared with the others.
delays below the predefined acceptable limits. For some In contrast, 4 ventilators (SLE 5000, Fabian in neonatal
ventilators, trigger delays were very different between the mode, PB840, and Avea) had a TIex that was ⬎ 100% of
various simulated patient types. the TI, meaning that the ventilator-delivered pressurization
lasted more than twice the patient’s TI, in at least one of
Pressurization: PTP300. Pressurization capacities were the simulated patient types.
very different depending on the ventilator and simulated
patient type, ranging from 15% (PB840) to 70% (Eng- Influence of Leaks
ström Carestation and Fabian in neonatal mode) of ideal
PTP300 (Fig. 4). The highest global PTP300 values were Autotriggering. Introducing a leak into the circuit led to
achieved by 2 adult ventilators (Engström Carestation and autotriggering in almost all ventilators except the Babylog
Avea) and one neonatal ventilator (Fabian). Most of the VN500 and Fabian. For the Leoni Plus and G5, increasing
ventilators, with the exception of Babylog VN500, Servo-i, the inspiratory trigger only slightly (from 0.1 to 0.2 L/min
and PB840, showed reduced pressurization capacity when and from 0.5 to 1 L/min, respectively) solved the problem.
the simulated patient type’s age was increased (ie, com- Activating the NIV algorithm when available also cor-
pliance increasing, resistance decreasing, and inspiratory rected the problem, except for the Avea.
RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10 1467
ICU VENTILATORS FOR NEONATES, INFANTS, AND CHILDREN
Fig. 4. Pressure-time product at 300 ms (PTP300) with the 10 ventilators tested with 3 different patient types: a preterm infant (resistance
100 cm H2O/L/s, compliance 2 mL/cm H2O, inspiratory time [TI] 400 ms, inspiratory effort 1 and 2 cm H2O [R100C2]), a full-term infant
(resistance 50 cm H2O/L/s, compliance 5 mL/cm H2O, TI 500 ms, inspiratory effort 2 and 4 cm H2O [R50C5]), and a child (resistance
30 cm H2O/L/s, compliance 10 mL/cm H2O, TI 600 ms, inspiratory effort 5 and 10 cm H2O [R30C10]). Two pressure support levels (10 and
15 cm H2O) were tested; results are pooled. The limit of 100 ms is generally recommended in adults4,17 for a mean TI of 800 ms. Histogram
bars are mean ⫾ SD.
Trigger Delay. Introducing a leak substantially increased was performed, this ventilator was not approved to venti-
trigger delay for the Leoni Plus, Evita XL NeoFlow, Eng- late children ⬍ 3 kg of body weight.
ström Carestation, and Avea, namely, for one neonatal
ventilator and 4 adult ventilators (Fig. 6). Activation of the Cycling. The presence of leaks increased the TIex in all
NIV algorithm allowed complete or partial compensation ventilators except the Fabian in neonatal mode, Babylog
for the impairment in only 2 adult ventilators (Evita XL VN500, and Evita XL NeoFlow in neonatal mode (Fig. 8).
NeoFlow with pediatric mode and Engström Carestation). The TIex was clearly ⬎ 100% in 3 adult ventilators (Eng-
Activating the Servo-i NIV algorithm induced a major ström Carestation, PB840, and Avea) and one neonatal
increase in trigger delay (26%). ventilator (SLE 5000) in the presence of leaks. The only 2
ventilators for which the TIex was ⬍ 50% in the presence of
Pressurization. No PTP300% variation was noted with leaks were the Evita XL NeoFlow and Babylog VN500.
the 4 neonatal ventilators tested when a leak was added in Using the NIV algorithm reduced the impairment of TIex
the circuit (Fig. 7). In contrast, 2 adult ventilators showed only for the Engström Carestation (partial correction),
a significant reduction in PTP300% (Evita XL NeoFlow Servo-i (partial correction), and PB840 (total correction).
with pediatric mode and Avea). The NIV algorithm com-
pensated for the pressurization loss only for the Evita XL
Volumes
NeoFlow. Additionally, the pressurization capacity was
significantly lower in the presence of leaks and with the
NIV algorithm activated for the Servo-i and PB840 com- In the absence of leaks, the difference between the dis-
pared with the scenarios of (1) in the absence of leaks and played and measured VT was in the range of ⫾ 10% for all
with the ventilator leak compensation algorithm or NIV tested ventilators except the Evita XL NeoFlow in neona-
algorithm deactivated and (2) in the presence of leaks and tal mode, Avea, and Servo-i (Table 1). Concerning the
with the NIV algorithm deactivated. No variations of pres- technological characteristics of the ventilators (see the sup-
surization capacity between the simulated patient types plementary materials at http://www.rcjournal.com), our
were observed for the G5. Note that the G5 was not tested measurements showed no differences in VT accuracy be-
for the R100C2 simulation, as, at the time this bench test tween ventilators equipped or not with a proximal flow
1468 RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10
ICU VENTILATORS FOR NEONATES, INFANTS, AND CHILDREN
Fig. 5. Inspiratory time in excess with the 10 ventilators tested with 3 different patient types : a preterm infant (resistance 100 cm H2O/L/s,
compliance 2 mL/cm H2O, inspiratory time [TI] 400 ms, inspiratory effort 1 and 2 cm H2O [R100C2]), a full-term infant (resistance 50 cm H2O/
L/s, compliance 5 mL/cm H2O, TI 500 ms, inspiratory effort 2 and 4 cm H2O [R50C5]), and a child (resistance 30 cm H2O/L/s, compliance
10 mL/cm H2O, TI 600 ms, inspiratory effort 5 and 10 cm H2O [R30C10]). Two pressure support levels (10 and 15 cm H2O) were tested;
results are pooled. The limit of 100 ms is generally recommended in adults4,17 for a mean TI of 800 ms. Note that the Leoni Plus could be
tested only with an expiratory trigger setting of 25%. Histogram bars are mean ⫾ SD.
sensor. Also, we saw no relevant differences in flow mea- well in one or two of the measured parameters, but unfor-
surement accuracy between flow sensors using the hotwire tunately, we could not identify one or several optimal
or pressure differential technique. In the presence of leaks, ventilators that performed well for all the tested criteria.
this difference between the displayed and measured VT This was particularly true when the ventilators’ perfor-
became much more important. In this case, most of the mance was assessed in the presence of leaks.
ventilators displayed a value that was too low for the mea- On the basis of our measurements, we could not find
sured VT. any solid argument that would speak against the use of
Activation of the NIV algorithm did not correct the common adult ventilators in the neonatal field. However,
differences between the measured and displayed VT for several items have to be discussed in more detail.
the Evita XL NeoFlow and G5. In contrast, activating the
NIV mode efficiently corrected the problem for both the Ventilation Performance in the Absence of Leaks
Engström Carestation and PB840. Under some conditions,
the PB840 and Servo-i displayed a value that was too high Trigger. A prolonged trigger delay results in a large
for the effective VT when the NIV algorithm was acti- amount of time during which the patient does not receive
vated. ventilator-delivered assistance. Prolonged trigger delays
observed with some of the tested ventilators might be of
Discussion major concern for neonatal and pediatric ventilation. In a
previous bench study,7 a trigger delay ⬍ 100 ms was re-
Our results show that, during the PS mode, under dif- ported for 6 tested ventilators, with values close to 60 ms
ferent bench testing conditions, the performance of the for 2 ventilators (Avea and Engström Carestation). Our
various ventilators differed drastically with regard to trig- results obtained under similar respiratory mechanics test
ger delay, pressurization capacity, and cycling. This ap- conditions simulating a preterm infant (R100C2) are in
plied to ventilators designed primarily for neonates and line with these findings. In our bench test, the new Baby-
children as well as adult ventilators adapted to ventilate log VN500 had a trigger delay of 110 ⫾ 30 ms. This value
small children. Some of the ventilators tested performed is similar to the trigger delays found by Marchese et al7 in
RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10 1469
ICU VENTILATORS FOR NEONATES, INFANTS, AND CHILDREN
Fig. 6. Trigger delays and leaks. Inspiratory time with the 10 ventilators tested under 3 conditions: in the absence of leaks and with the
noninvasive ventilation (NIV) algorithm deactivated (L0NIV0), in the presence of leaks and with the NIV algorithm deactivated (L⫹NIV0), and
in the presence of leaks and with the NIV algorithm activated (L⫹NIV⫹). All results are pooled. Histogram bars are mean ⫾ SD. * P ⬍ .05
vs L0NIV0; † P ⬍ .05 vs L⫹NIV0 (analysis of variance).
Fig. 7. Pressure-time product at 300 ms (PTP300) and leaks. Trigger delay with the 10 ventilators tested under 3 conditions: in the absence
of leaks and with the NIV algorithm deactivated (L0NIV0), in the presence of leaks and with the NIV algorithm deactivated (L⫹NIV0), and
in the presence of leaks and with the NIV algorithm activated (L⫹NIV⫹). All results are pooled. Histogram bars mean ⫾ SD. * P ⬍ .05 vs
L0NIV0; † P ⬍ .05 vs L⫹NIV0 (analysis of variance).
1470 RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10
ICU VENTILATORS FOR NEONATES, INFANTS, AND CHILDREN
Fig. 8. Inspiratory time in excess (TIex) with the 10 ventilators tested under 3 conditions: in the absence of leaks and with the NIV algorithm
deactivated (L0NIV0), in the presence of leaks and with the NIV algorithm deactivated (L⫹NIV0), and in the presence of leaks and with the
NIV algorithm activated (L⫹NIV⫹). All results are pooled. Histogram bars mean ⫾ SD. * P ⬍ .05 vs L0NIV0; † P ⬍ .05 vs L⫹NIV0 (analysis
of variance). Note that the Leoni Plus could be tested only with an expiratory trigger setting of 25%.
similar simulated patient types with the Babylog 8000. In leaks.25 On the other hand, the occurrence of premature
contrast, a shorter trigger delay of 75 ms was reported cycling decreases the time available to deliver respiratory
when the Babylog 8000 was used in neonates.23 This might assistance, which might lead, at a given level of PS, to a
suggest that our bench test could have slightly underesti- lower VT than expected. Both conditions might increase a
mated the ventilation performance of the ventilators tested, patient’s work of breathing.26 Optimizing ETS should the-
possibly because of the difficulty in accurately simulating oretically reduce the occurrence of cycling asynchronies.
real pediatric patients’ inspiratory efforts. However, in our However, ETS optimization can be difficult at the bedside,
bench test, the trigger delays measured for the Servo-i as the respiratory mechanics might change rapidly depend-
were in line with the values reported in clinical settings.8,9,24 ing on the deterioration or improvement of the patient’s
condition, and as the intermittent occurrence of a leak can
Pressurization. In the pediatric literature, there are a strik- influence expiratory asynchrony. This calls the use of cy-
ing lack of data on the possible clinical impact of pressur- cling criteria in daily practice into question.
ization capacities of mechanical ventilators. Theoretically, It must also be emphasized that the relatively good re-
limited pressurization capacities might be responsible for a sults regarding cycling (TIex ⱕ 50%) observed with 4 of
discrepancy between a patient’s inspiratory demand and the ventilators (Babylog VN500, Evita XL NeoFlow in
the pressure delivered by the machine, which could be pediatric mode, G5, and Servo-i) might be counterbal-
responsible for an increased work of breathing or for gen- anced by an increased risk of unwanted premature cycling,
erating patient-ventilator asynchronies. However, no clin- as reported previously by Beck et al23 for the Babylog
ical data are currently available concerning this topic in 8000 and by our group for the Servo-i.24
the pediatric population.
Ventilation Performance in the Presence of Leaks
Cycling. In the presence of late cycling, patients often
fight against their ventilators and actively recruit their ex- Trigger. Similar to what was reported previously in adult
piratory muscles, thus increasing the risk of significant bench tests,12,15 NIV algorithms significantly reduced au-
RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10 1471
1472
Table 1. Difference Between Measured and Displayed Expired VT for the 10 Ventilators Tested in the Presence and Absence of Leaks and With and Without the NIV Algorithm
R100C2 R50C5 R30C10
Measured Displayed Expired Displayed Expired Displayed Expired
Expired Expired
Ventilator Expired VT ⫺ Measured VT ⫺ Measured VT ⫺ Measured
VT VT
VT Expired VT (cc) Expired VT (cc) Expired VT (cc)
L0NIV0 L0NIV0 L⫹NIV0 L⫹NIV⫹ L0NIV0 L0NIV0 L⫹NIV0 L⫹NIV⫹ L0NIV0 L0NIV0 L⫹NIV0 L⫹NIV⫹
Leoni Plus 19.5 ⫾ 3.2 ⫺0.6 ⫾ 0.4 ⫺4.6 ⫾ 0.7* 58.5 ⫾ 16.5 ⫺3.2 ⫾ 1.8 ⫺15.5 ⫾ 3.5* 91.0 ⫾ 35.1 ⫺8.3 ⫾ 4.8 ⫺16.8 ⫾ 5.6*
SLE 5000 18.3 ⫾ 4.0 ⫺1.9 ⫾ 1.4 ⫺5.7 ⫾ 0.8* 62.3 ⫾ 17.8 ⫺4.4 ⫾ 2.1 ⫺10.7 ⫾ 3.5* 102.9 ⫾ 26.0 ⫺3.1 ⫾ 6.6 ⫺25.2 ⫾ 17.2*
Fabian in neonatal 11.4 ⫾ 2.8 ⫺0.6 ⫾ 2.6 ⫺0.5 ⫾ 2.4 53.3 ⫾ 14.7 ⫺2.1 ⫾ 5.0 ⫺6.5 ⫾ 1.9* 105.2 ⫾ 27.3 13.6 ⫾ 7.8* 11.6 ⫾ 5.8
ICU VENTILATORS
mode
Fabian in pediatric 50.8 ⫾ 16.8 ⫺2.3 ⫾ 5.1 ⫺9.4 ⫾ 4.3* 92.0 ⫾ 44.2 9.5 ⫾ 1.0 13.0 ⫾ 3.3*
FOR
mode
Babylog VN500 20.0 ⫾ 2.1 1.6 ⫾ 1.7 ⫺4.8 ⫾ 0.8* 41.3 ⫾ 7.8 ⫺0.8 ⫾ 2.2 ⫺15.5 ⫾ 4.8* 80.0 ⫾ 34.9 ⫺6 ⫾ 12.8 ⫺16.8 ⫾ 6.3*
Evita NeoFlow in 22.0 ⫾ 2.9 ⫺2.5 ⫾ 0.0* ⫺9.0 ⫾ 1.2* ⫺9.0 ⫾ 1.2* 58.8 ⫾ 19.3 ⫺0.8 ⫾ 2.6 ⫺7.5 ⫾ 1.7* ⫺8.5 ⫾ 1.7 115.9 ⫾ 32.3 2.8 ⫾ 0.9 ⫺22.5 ⫾ 9.9* ⫺23.5 ⫾ 10.0*
neonatal mode
Evita XL NeoFlow 49.8 ⫾ 14.1 2.4 ⫾ 2.4 ⫺6.2 ⫾ 3.9* ⫺6.0 ⫾ 4.0 106.3 ⫾ 22.8 5.5 ⫾ 2.1 ⫺13.0 ⫾ 4.9* ⫺18.0 ⫾ 0.8*
in pediatirc mode
Engström 15.0 ⫾ 3.5 ⫺0.7 ⫾ 0.5 ⫺4.2 ⫾ 0.6* 0.1 ⫾ 0.3 58.9 ⫾ 15.9 0.5 ⫾ 3.0 ⫺2.6 ⫾ 3.4 0.1 ⫾ 1.3 114.0 ⫾ 24.4 ⫺9.0 ⫾ 4.6 ⫺42.1 ⫾ 7.8* ⫺9.0 ⫾ 2.0
Carestation
Avea 17.4 ⫾ 3.3 ⫺2.5 ⫾ 0.3* ⫺7.5 ⫾ 1.1* ⫺8.0 ⫾ 1.1* 54.1 ⫾ 17.1 ⫺5.3 ⫾ 1.5 ⫺7.0 ⫾ 2.6* ⫺7.1 ⫾ 1.4 122.5 ⫾ 30.0 ⫺7.0 ⫾ 2.9 ⫺10.8 ⫾ 1 ⫺10.8 ⫾ 2.5
NEONATES, INFANTS,
Servo-i 14.2 ⫾ 1.5 1.8 ⫾ 2.1* ⫺2.0 ⫾ 1.7* NA 52.3 ⫾ 14.9 1.1 ⫾ 3.1 ⫺13.0 ⫾ 1.9* ⫺17.5 ⫾ 1.6* 90.4 ⫾ 25.2 4.4 ⫾ 8.9 ⫺24.6 ⫾ 4.6 23.7 ⫾ 7.4
G5 47.8 ⫾ 12.7 5.7 ⫾ 6.1* ⫺1.5 ⫾ 1.9 20.8 ⫾ 6.7* 75.8 ⫾ 28.1 4.4 ⫾ 8.9 ⫺1.3 ⫾ 8.6 ⫺24.3 ⫾ 4.6
AND
PB840 12.6 ⫾ 3.9 0.1 ⫾ 0.6 ⫺11.8 ⫾ 3.3* 0.8 ⫾ 0.9 60.8 ⫾ 20.2 ⫺3.8 ⫾ 5.2 ⫺49.6 ⫾ 7.7* 0.0 ⫾ 1.2 115.0 ⫾ 28.9 ⫺10.8 ⫾ 4.4 ⫺40.8 ⫾ 2.1* 8.3 ⫾ 3.6
With the 3 different patient types: a preterm infant (resistance 100 cm H2O/L/s, compliance 2 mL/cm H2O, inspiratory time 关TI兴 400 ms, inspiratory effort 1 and 2 cm H2O 关R100C2兴), a full-term infant (resistance 50 cm H2O/L/s, compliance 5 mL/cm H2O, TI
500 ms, inspiratory effort 2 and 4 cm H2O 关R50C5兴), and a child (resistance 30 cm H2O/L/s, compliance 10 mL/cm H2O, TI 600 ms, inspiratory effort 5 and 10 cm H2O 关R30C10兴). Two pressure support levels are reported (10 and 15 cm H2O); values are
pooled. Values are expressed in mean ⫾ SD.
CHILDREN
* P ⬍ .05 and value ⬎ 10% than the expired tidal volume (VT) during L0NIV0.
L0NIV0 ⫽ in the absence of leaks and with the noninvasive ventilation (NIV) algorithm deactivated
L⫹NIV0 ⫽ in the presence of leaks and with the NIV algorithm deactivated
L⫹NIV⫹ ⫽ in the presence of leaks and with the NIV algorithm activated
NA ⫽ not applicable
RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10
ICU VENTILATORS FOR NEONATES, INFANTS, AND CHILDREN
totriggering related to leaks. Interestingly, of the neonatal showed no differences in VT accuracy between different
ventilators, only the SLE 5000 required a significant in- flow measurement techniques (distal or proximal flow sen-
crease in the flow trigger threshold (less sensitive trigger) sor, hotwire or pressure differential technique). However,
to overcome this phenomenon. This can probably be ex- this may possibly not be applicable to cases with very
plained by the fact that a leak compensation algorithm is severe compliance impairment or high airway resistance,
activated by default in neonatal devices (see the supple- as these formed no part of our bench test.
mentary materials at http://www.rcjournal.com).
In adult bench tests, it was reported previously that the Presence of Leaks. Globally, in the presence of leaks
trigger delay increased to unacceptable values in the pres- and with the NIV algorithm deactivated, the ventilators
ence of leaks.12,15 In contrast, in our neonatal/pediatric tested tended to display a value that was too low for the VT
bench test, this increase in trigger delay was globally lower effectively delivered to the patient, which could lead to the
and not systematic. Leaks did not cause major trigger de- delivery of a higher assist than expected and even to sit-
lay increases in neonatal ventilators or in 2 of the adult uations of overassistance. Most (but not all) NIV algo-
ventilators. When considering adult ventilators, in the pres- rithms corrected this problem. As leaks are often present
ence of leaks, 3 ventilators showed a significant increase during neonatal and pediatric invasive ventilation, activa-
in trigger delays (Evita XL NeoFlow, Engström Care- tion of NIV algorithms is suggested, provided that the
station, and Avea) compared with the absence of leaks. algorithm of the ventilator performs well.
Among these 3 ventilators, activating the NIV mode cor-
rected the impairment in only 2 of the ventilators (Evita
Clinical Implications
XL NeoFlow and Engström Carestation). Surprisingly, but
as reported previously in an adult bench test,12 the Servo-i
showed a higher trigger delay when activating the NIV Our bench test suggests that the ventilators used to de-
algorithm in the presence of leaks. The measured trigger liver PSV to the pediatric population do not perform well
delay in this scenario (in the presence of leaks and with the in all circumstances regarding trigger delays, pressuriza-
NIV algorithm activated) is similar to values reported pre- tion capacities, cycling, and VT accuracy, especially in the
viously in a clinical study performed in infants and chil- presence of leaks. These observations might put the ratio-
dren by our group.24 nale of using PSV in the pediatric population into question
and might also give insight into why the introduction of
Pressurization. For some adult ventilators, pressuriza- assisted ventilation modes did not show major advantages
tion was impaired in the presence of leaks either with or in terms of improved outcomes compared with controlled
without the NIV algorithm activated. We hypothesize that modes.25,30 Additionally, the poor ventilation performance
this could lead to situations of underassistance when adult documented with the currently available ventilators and
ventilators are used to ventilate small infants. In contrast, the absence of an optimal ventilator for delivering PSV to
no change in pressurization was observed in the presence small children must be taken into account when new ven-
of leaks for the 4 neonatal ventilators tested. tilatory modes, such as Neurally Adjusted Ventilatory As-
sist, are compared with standard PSV. More specifically,
Cycling. In our bench test, as found previously in other the improved patient-ventilator synchrony documented
studies,17,27 we found that the TIex was higher in the pres- with Neurally Adjusted Ventilatory Assist in recent stud-
ence of leaks. As an increased TIex is associated with an ies8,9,31-33 could have been enhanced by the non-optimal
increased incidence of late cycling and of ineffective ef- ventilation performance of the ventilator used for PSV.
forts,5,18 a TIex that is ⬎ 100% of the TI, as we observed in As optimizing the ETS criterion is difficult at the bed-
one neonatal and 3 adult ventilators, is worrying. The spe- side, especially because respiratory mechanics and the
cific NIV algorithm, included by default, in neonatal ven- amount of leakage often vary over time, ventilators should
tilators is of interest, although it showed poor ventilation offer reliable tools to measure resistance and dynamic com-
performance in one ventilator (Avea). pliance (eg, by single-occlusion technique34) during ongo-
ing mechanical ventilation and automatically adjust ETS
Volume Measurement Accuracy based on this information. As NIV was shown to improve
short-term outcomes in children,35 the use of this ventila-
Absence of Leaks. In baseline respiration scenarios, for tion modality is probably going to increase in the near
all ventilators in almost all simulated patient types, there future, and ventilators must offer NIV algorithms that ef-
were no significant differences between the displayed and ficiently deal with the presence of leaks. Given the cir-
measured VT. To accurately measure VT, especially in cumstances, it might be preferable to use time-cycled pres-
neonates, proximal flow sensors have been strongly advo- sure modes to deliver NIV to small children, although
cated for many years.28,29 Interestingly, our measurements these modes seem to increase trigger delay slightly.8
RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10 1473
ICU VENTILATORS FOR NEONATES, INFANTS, AND CHILDREN
Concerning the pediatric and neonatal modes avail- results if higher inspiratory demands had been used. Fi-
able on 2 of the ventilators tested (Fabian and Evita XL nally, we did not evaluate all operational aspects of the
NeoFlow), we observed only a slight difference in trigger ventilators, such as the user friendliness or the alarm set-
delays, but no significant differences in pressurization or tings, and their interaction with ventilation parameters.
cycling. Theoretically, the difference between the 2 These important aspects should be the aim of a future
modes is a different maximum peak inspiratory flow. There- study.
fore, we do not have any explanation for this small dif-
ference. Advantages may be seen only with higher inspira- Conclusions
tory efforts.
Relying on the VT displayed by the machine in the In our pediatric bench test, no ventilator performed
presence of leaks when the NIV mode is not activated equally well in all tested patient types and all tested leak-
might be misleading and could cause the clinician to un- age scenarios for all explored parameters (triggering, pres-
derestimate the delivered VT. This could lead to the de- surization, cycling, and VT measurement accuracy), and
livery of a higher assist than expected and even to a situ- we were not able to identify an optimal ventilator to de-
ation of overassistance. This issue can be considered as a liver PSV in all tested situations to neonates and children.
missing security feature for both neonatal and adult ven- However, neonatal ventilators tended to perform better in
tilators when used in neonates. the presence of air leaks.
There are several limitations of this study. First, a bench As adult ventilators globally performed better in the
test can simulate only a few well-defined and stable con- presence of air leaks when NIV algorithms were activated,
ditions, but cannot reflect the extent and complexity of turning these algorithms on is suggested when these ven-
true clinical scenarios, such as the variability of patients’ tilators are used to deliver PSV through uncuffed tubes to
efforts, which change almost breath by breath.9 However, neonates and young children. However, this recommenda-
bench tests allow comparison between ventilators due to tion is not valid for the Servo-i, as this ventilator per-
the reproducible conditions. Second, a fixed ETS cannot formed poorly when its NIV algorithm was activated. In
be optimal for various clinical situations, and it could be summary, we conclude that our findings emphasize the
argued that the value chosen for this study (15%) was need to improve algorithms for assisted ventilation modes
arbitrary. However, almost no data on an optimal cycling to better deal with situations of high airway resistance, low
criterion in the pediatric setting are available in the liter- pulmonary compliance, and the presence of leaks.
ature. In our pediatric ICU, 10% is the most frequently
used ETS during invasive ventilation.24 Interestingly, when
ACKNOWLEDGMENTS
a higher value of 25% (interquartile range of 21–29) was
used during NIV, many premature cycling events were We thank Mr Vincent Mathes (Chur, Switzerland) for proofreading.
documented, suggesting that this threshold was too high
even in the presence of leaks. As the Babylog VN500, a REFERENCES
typical neonatal ventilator, has a non-modifiable ETS of
1. Betensley AD, Khalid I, Crawford J, Pensler RA, DiGiovine B.
only 15%, we decided to use this same value to test all
Patient comfort during pressure support and volume controlled-con-
ventilators to allow comparisons between the machines. tinuous mandatory ventilation. Respiratory care 2008;53(7):897-902.
Of course, this choice can influence the TIex we measured 2. Futier E, Constantin JM, Combaret L, Mosoni L, Roszyk L, Sapin V,
and the occurrence of late cycling documented in our bench et al. Pressure support ventilation attenuates ventilator-induced pro-
test. Additionally, as the Leoni Plus has a non-modifiable tein modifications in the diaphragm. Crit Care 2008;12(5):R116.
3. Greenough A, Dimitriou G, Prendergast M, Milner AD. Synchro-
ETS of 25%, this ventilator could not be tested under the
nized mechanical ventilation for respiratory support in newborn in-
same conditions as the other ventilators, which means that fants. Cochrane Database Syst Rev 2008;(1):CD000456.
the TIex results reported for this ventilator must be consid- 4. Vignaux L, Tassaux D, Carteaux G, Roeseler J, Piquilloud L, Bro-
ered with caution. Third, the inspiratory times we used in chard L, Jolliet P. Performance of noninvasive ventilation algorithms
our bench tests were slightly higher than the values re- on ICU ventilators during pressure support: a clinical study. Inten-
sive Care Med 2010;36(12):2053-2059.
ported previously, especially for premature infants. How-
5. Vignaux L, Vargas F, Roeseler J, Tassaux D, Thille AW, Kossowsky
ever, as all ventilators were tested with the same inspira- MP, et al. Patient-ventilator asynchrony during non-invasive venti-
tory times, and as these values were not very different lation for acute respiratory failure: a multicenter study. Intensive
from those reported previously, in our opinion, this should Care Med 2009;35(5):840-846.
not have significantly influenced our bench test results. 6. Bernstein G, Knodel E, Heldt GP. Airway leak size in neonates and
autocycling of three flow-triggered ventilators. Crit Care Med 1995;
Fourth, to take into account the low amplitude efforts oc-
23(10):1739-1744.
curring during sleep in small infants, we chose to simulate 7. Marchese AD, Chipman D, de la Oliva P, Kacmarek RM. Adult ICU
low inspiratory efforts in our bench test. As a consequence, ventilators to provide neonatal ventilation: a lung simulator study.
we cannot conclude that we would have found the same Intensive Care Med 2009;35(4):631-638.
1474 RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10
ICU VENTILATORS FOR NEONATES, INFANTS, AND CHILDREN
8. Bordessoule A, Emeriaud G, Morneau S, Jouvet P, Beck J. Neurally 23. Beck J, Reilly M, Grasselli G, Mirabella L, Slutsky AS, Dunn MS,
adjusted ventilatory assist improves patient-ventilator interaction in Sinderby C. Patient-ventilator interaction during neurally adjusted
infants compared to conventional ventilation. Pediatr Res 2012;72(2): ventilatory assist in low birth weight infants. Pediatr Res 2009;65(6):
194-202. 663-668.
9. de la Oliva P, Schüffelmann C, Gómez-Zamora A, Villar J, Kac- 24. Vignaux L, Grazioli S, Piquilloud L, Bochaton N, Karam O, Jaecklin
marek RM. Asynchrony, neural drive, ventilatory variability and T, et al. Optimizing patient-ventilator synchrony during invasive
COMFORT: NAVA versus pressure support in pediatric patients. A ventilator assist in children and infants remains a difficult task. Pe-
non-randomized cross-over trial. Intensive Care Med 2012;38(5): diatr Crit Care Med 2013;14(7):e316-e325.
838-846. 25. Greenough A. Comparison between intermittent mandatory and syn-
10. Battisti A, Tassaux D, Janssens JP, Michotte JB, Jaber S, Jolliet P. chronized intermittent mandatory ventilation with pressure in chil-
Performance characteristics of 10 home mechanical ventilators in
dren. J Pediatr 2009;85(1):1-3.
pressure-support mode: a comparative bench study. Chest 2005;
26. Tokioka H, Tanaka T, Ishizu T, Fukushima T, Iwaki T, Nakamura Y,
127(5):1784-1792.
Kosogabe Y. The effect of breath termination criterion on breathing
11. Tassaux D, Strasser S, Fonseca S, Dalmas E, Jolliet P. Comparative
patterns and the work of breathing during pressure support ventila-
bench study of triggering, pressurization, and cycling between the
home ventilator VPAP II and three ICU ventilators. Intensive Care tion. Anesth Analg 2001;92(1):161-165.
Med 2002;28(9):1254-1261. 27. Calderini E, Confalonieri M, Puccio PG, Francavilla N, Stella L,
12. Vignaux L, Tassaux D, Jolliet P. Performance of noninvasive ven- Gregoretti C. Patient-ventilator asynchrony during noninvasive ven-
tilation modes on ICU ventilators during pressure support: a bench tilation: the role of expiratory trigger. Intensive Care Med 1999;
model study. Intensive Care Med 2007;33(8):1444-1451. 25(7):662-667.
13. Aslanian P, El Atrous S, Isabey D, Valente E, Corsi D, Harf A, et al. 28. Jaecklin T, Morel DR, Rimensberger PC. Volume-targeted modes of
Effects of flow triggering on breathing effort during partial ventila- modern neonatal ventilators: how stable is the delivered tidal vol-
tory support. Am J Respir Crit Care Med 1998;157(1):135-143. ume? Intensive Care Med 2007;33(2):326-335.
14. Whitelaw WA, Derenne JP, Milic-Emili J. Occlusion pressure as a 29. Mahmoud RA, Fischer HS, Proquitté H, Shalaby HM, Schmalisch G.
measure of respiratory center output in conscious man. Respir Physiol Relationship between endotracheal tube leakage and under-reading
1975;23(2):181-199. of tidal volume in neonatal ventilators. Acta Paediatr 2009;98(7):
15. Carteaux G, Lyazidi A, Cordoba-Izquierdo A, Vignaux L, Jolliet P, 1116-1122.
Thille AW, et al. Patient-ventilator asynchrony during noninvasive 30. Moraes MA, Bonatto RC, Carpi MF, Ricchetti SM, Padovani CR,
ventilation: a bench and clinical study. Chest 2012;142(2):367-376. Fioretto JR. Comparison between intermittent mandatory ventilation
16. Piquilloud L, Tassaux D, Bialais E, Lambermont B, Sottiaux T, and synchronized intermittent mandatory ventilation with pressure
Roeseler J, et al. Neurally adjusted ventilatory assist (NAVA) im- support in children. J Pediatr 2009;85(1):15-20.
proves patient-ventilator interaction during non-invasive ventilation 31. Alander M, Peltoniemi O, Pokka T, Kontiokari T. Comparison of
delivered by face mask. Intensive Care Med 2012;38(10):1624-1631. pressure-, flow-, and NAVA-triggering in pediatric and neonatal
17. Vignaux L, Tassaux D, Jolliet P. Evaluation of the user-friendliness ventilatory care. Pediatr Pulmonol 2012;47(1):76-83.
of seven new generation intensive care ventilators. Intensive Care
32. Breatnach C, Conlon NP, Stack M, Healy M, O’Hare BP. A pro-
Med 2009;35(10):1687-1691.
spective crossover comparison of neurally adjusted ventilatory assist
18. Fauroux B, Leroux K, Desmarais G, Isabey D, Clément A, Lofaso F,
and pressure-support ventilation in a pediatric and neonatal intensive
Louis B. Performance of ventilators for noninvasive positive-pres-
care unit population. Pediatr Crit Care Med 2010;11(1):7-11.
sure ventilation in children. Eur Respir J 2008;31(6):1300-1307.
33. Clement KC, Thurman TL, Holt SJ, Heulitt MJ. Neurally triggered
19. Harikumar G, Moxham J, Greenough A, Rafferty GF. Measurement
of maximal inspiratory pressure in ventilated children. Pediatr Pul- breaths reduce trigger delay and improve ventilator response times in
monol 2008;43(11):1085-1091. ventilated infants with bronchiolitis. Intensive Care Med 2011;37(11):
20. Honma Y, Wilkes D, Bryan MH, Bryan AC. Rib cage and abdominal 1826-1832.
contributions to ventilatory response in CO2 in infants. J Appl Physiol 34. Katier N, Uiterwaal CS, de Jong BM, Kimpen JL, van der Ent CK.
Respir Environ Exerc Physiol 1984;56(5):1211-1216. Feasibility and variability of neonatal and infant lung function mea-
21. Curzi-Dascalova L, Peirano P, Morel-Kahn F. Development of sleep surement using the single occlusion technique. Chest 2005;128(3):
states in normal premature and full-term newborns. Dev Psychobiol 1822-1829.
1988;21(5):431-444. 35. Najaf-Zadeh A, Leclerc F. Noninvasive positive pressure ventilation
22. Nicolai T. Mini-symposium: lung physiology. The physiological ba- for acute respiratory failure in children: a concise review. Ann In-
sis of respiratory support. Pedriatr Respir Rev 2006;7(2):97-102. tensive Care 2011;1(1):15.
This article is approved for Continuing Respiratory Care Education
credit. For information and to obtain your CRCE
(free to AARC members) visit
www.rcjournal.com
RESPIRATORY CARE • OCTOBER 2014 VOL 59 NO 10 1475
You might also like
- Gas Mask Buyer's Guide BreakdownDocument42 pagesGas Mask Buyer's Guide Breakdownlakanbastonero100% (1)
- Crossvent-2+: Operation & Service ManualDocument102 pagesCrossvent-2+: Operation & Service Manualginalimartinezmu100% (2)
- BLS Study Guide and PretestDocument47 pagesBLS Study Guide and PretestRicha AbcedeNo ratings yet
- Chemical Hazard Bulletin: OPT D 1127Document1 pageChemical Hazard Bulletin: OPT D 1127HaleemUrRashidBangashNo ratings yet
- Pneumonia PamphletDocument2 pagesPneumonia PamphletMairiz Jem Santos100% (6)
- Clinical Worksheet Kenneth Bronson Jasgou1752Document2 pagesClinical Worksheet Kenneth Bronson Jasgou1752Jasmyn Rose100% (1)
- Airport Emergency Plan TemplateDocument21 pagesAirport Emergency Plan Templatehmltninfante100% (2)
- Crossvent-3+: Operation & Service ManualDocument102 pagesCrossvent-3+: Operation & Service ManualIngenieria NemoconNo ratings yet
- Novel Forms of Ventilation in Neonates Neurally Adjusted VentilatoryDocument16 pagesNovel Forms of Ventilation in Neonates Neurally Adjusted VentilatorydocsaravananNo ratings yet
- Advances in Emergent Airway Management in PediatricsDocument19 pagesAdvances in Emergent Airway Management in PediatricsJpmspoonNo ratings yet
- Advances in Emergent Airway Management in PediatricsDocument19 pagesAdvances in Emergent Airway Management in PediatricsLuis Miguel VillanuevaNo ratings yet
- Mechanical Ventilation of The Premature NeonateDocument16 pagesMechanical Ventilation of The Premature NeonateHaitham HafezNo ratings yet
- Ventilating The Newborn and Child. Garcia-Fernandez JDocument8 pagesVentilating The Newborn and Child. Garcia-Fernandez JAyelen GaldeanoNo ratings yet
- Weaning Infants From Mechanical Ventilation: Clinics in Perinatology September 2012Document21 pagesWeaning Infants From Mechanical Ventilation: Clinics in Perinatology September 2012MALIK MANASRAHNo ratings yet
- Volume-Targeted Modes of Modern Neonatal Ventilators: How Stable Is The Delivered Tidal Volume?Document10 pagesVolume-Targeted Modes of Modern Neonatal Ventilators: How Stable Is The Delivered Tidal Volume?DawoodNo ratings yet
- Modes of Ventilation For Pediatric Patients Under Anesthesia A ProDocument7 pagesModes of Ventilation For Pediatric Patients Under Anesthesia A ProManigoldo CamelaNo ratings yet
- Neoreviews 2013 Keszler E237 51Document17 pagesNeoreviews 2013 Keszler E237 51Gun HawkNo ratings yet
- New Modes of Neonatal Ventilation MMV Et Al Mammel 2005 ConclusionsDocument2 pagesNew Modes of Neonatal Ventilation MMV Et Al Mammel 2005 ConclusionsOsmanyNo ratings yet
- Modes and Strategies For Providing Conventional Mechanical Ventilation in NeonatesDocument6 pagesModes and Strategies For Providing Conventional Mechanical Ventilation in Neonatesbig023296No ratings yet
- Clinical Controversies in Aerosol Therapy For Infants and ChildrenDocument23 pagesClinical Controversies in Aerosol Therapy For Infants and Childrencelma44No ratings yet
- Wormald2009kandidat 2Document4 pagesWormald2009kandidat 2adeNo ratings yet
- In Support of Pressure Support: Subrata Sarkar, MD, Steven M. Donn, MDDocument12 pagesIn Support of Pressure Support: Subrata Sarkar, MD, Steven M. Donn, MDSiska LesnussaNo ratings yet
- Comparison of Devices For Newborn Ventilation in The Delivery RoomDocument9 pagesComparison of Devices For Newborn Ventilation in The Delivery RoomRaja SekarNo ratings yet
- Care of neonates on respiratory supportDocument40 pagesCare of neonates on respiratory supportsyedNo ratings yet
- Pediatric Noninvasive Ventilation: Cathy HautDocument7 pagesPediatric Noninvasive Ventilation: Cathy HautsiputamaliaputriNo ratings yet
- Management of Rare Causes of Pediatric Chronic Respiratory FailureDocument16 pagesManagement of Rare Causes of Pediatric Chronic Respiratory FailureISABEL SOFIA CABARCAS COGOLLONo ratings yet
- Ventilator Settings: For Newborn InfantsDocument6 pagesVentilator Settings: For Newborn InfantsRomeo DevNo ratings yet
- Comparative Study Between Hydrostatic and Pneumatic Reduction For Early Intussusception in PediatricsDocument6 pagesComparative Study Between Hydrostatic and Pneumatic Reduction For Early Intussusception in PediatricsMostafa MosbehNo ratings yet
- Neonatal Noninvasive Ventilation Techniques: Do We Really Need To Intubate?Document25 pagesNeonatal Noninvasive Ventilation Techniques: Do We Really Need To Intubate?sing terriblyNo ratings yet
- A Framework For The Management of The Pediatric AirwayDocument23 pagesA Framework For The Management of The Pediatric AirwayDaniel GallegoNo ratings yet
- Volume Targeted VentilationDocument28 pagesVolume Targeted VentilationhosnameskarNo ratings yet
- Expected Difficult Airway in Children: ReviewDocument6 pagesExpected Difficult Airway in Children: ReviewAlma ChamuNo ratings yet
- Anesthetic Management of Thoracoscopic Resection of Lung Lesions in Small ChildrenDocument8 pagesAnesthetic Management of Thoracoscopic Resection of Lung Lesions in Small ChildrenburhanNo ratings yet
- Hfo 3Document8 pagesHfo 3markus_danusantosoNo ratings yet
- Pediatric Anesthesia - 2022 - Weatherall - Developing An Extubation Strategy For The Difficult Pediatric Airway Who WhenDocument8 pagesPediatric Anesthesia - 2022 - Weatherall - Developing An Extubation Strategy For The Difficult Pediatric Airway Who WhenPamela Mamani FloresNo ratings yet
- PILLOW 2012_Innovation in Surfactant Therapy II-surfactant Administration by Aerosolization.Document8 pagesPILLOW 2012_Innovation in Surfactant Therapy II-surfactant Administration by Aerosolization.Rafael JustinoNo ratings yet
- In Vitro Evaluation of Aerosol Delivery - Complementaria - Semana 3Document7 pagesIn Vitro Evaluation of Aerosol Delivery - Complementaria - Semana 3natalia muñozNo ratings yet
- Pediatric Rapid Sequence Intubation - An In-Depth ReviewDocument12 pagesPediatric Rapid Sequence Intubation - An In-Depth ReviewDiego LatorreNo ratings yet
- Paediatric Mechanical Ventilation in The Intensive Care UnitDocument5 pagesPaediatric Mechanical Ventilation in The Intensive Care UnitImmakulata LovinaNo ratings yet
- 2019 A Phase II randomized controlled trial for lung and diaphragm protective ventilationDocument7 pages2019 A Phase II randomized controlled trial for lung and diaphragm protective ventilationwilsonmauriciolozanoNo ratings yet
- Conti 2016Document7 pagesConti 2016Dwi Putri SekariniNo ratings yet
- Neonate Vs Adult VentilationDocument2 pagesNeonate Vs Adult VentilationtkAcuNNo ratings yet
- Lauder 2019Document12 pagesLauder 2019Julio AltamiranoNo ratings yet
- RSI - Children 2 PDFDocument6 pagesRSI - Children 2 PDFAbdul RachmanNo ratings yet
- 693 FullDocument12 pages693 FullGilmer alvarez floresNo ratings yet
- Use of High-Flow Nasal Cannula Oxygen Therapy To Prevent Desaturation During Tracheal Intubation of Intensive Care Patients With Mild-to-Moderate HypoxemiaDocument10 pagesUse of High-Flow Nasal Cannula Oxygen Therapy To Prevent Desaturation During Tracheal Intubation of Intensive Care Patients With Mild-to-Moderate HypoxemiaLingga AniNo ratings yet
- Paula2010b PDFDocument6 pagesPaula2010b PDFAldi AhmadNo ratings yet
- Pham - Esophageal ManometryDocument21 pagesPham - Esophageal ManometryAbraham HaneineNo ratings yet
- In Preterm Infants Recovering From Respiratory Failure Effects of Volume-Guaranteed Synchronized Intermittent Mandatory VentilationDocument7 pagesIn Preterm Infants Recovering From Respiratory Failure Effects of Volume-Guaranteed Synchronized Intermittent Mandatory VentilationIkayulianiNo ratings yet
- Invasive and Noninvasive Pediatric Mechanical Ventilation: Ira M Cheifetz MD FAARCDocument17 pagesInvasive and Noninvasive Pediatric Mechanical Ventilation: Ira M Cheifetz MD FAARCAhmed Rizk AhmedNo ratings yet
- Non Invasive Versus Invasive Respiratory Support in Preterm InfantsDocument25 pagesNon Invasive Versus Invasive Respiratory Support in Preterm InfantshosnameskarNo ratings yet
- Evidence-based role of high-frequency ventilation in neonatal respiratory failureDocument16 pagesEvidence-based role of high-frequency ventilation in neonatal respiratory failureSiska LesnussaNo ratings yet
- Sop Senam LBPDocument7 pagesSop Senam LBPFaisal HarisNo ratings yet
- Shortacting-sedativeanalgesic-drugs-protect-against-development-of-ventilatorassociated-events-in-children-Secondary-analysis-of-the-EUVAE-study_2021_American-Association-for-Respiratory-CareDocument8 pagesShortacting-sedativeanalgesic-drugs-protect-against-development-of-ventilatorassociated-events-in-children-Secondary-analysis-of-the-EUVAE-study_2021_American-Association-for-Respiratory-CareevyNo ratings yet
- Paediatric Mechanical Ventilation in The Intensive Care UnitDocument5 pagesPaediatric Mechanical Ventilation in The Intensive Care UnitdmallozziNo ratings yet
- Volume-Targeted Ventilation 2021Document17 pagesVolume-Targeted Ventilation 2021Vladimir FloresNo ratings yet
- FasdfyDocument8 pagesFasdfyzuliamNo ratings yet
- NakatoIJP Volume6 Issue9 Pages8215-8223Document9 pagesNakatoIJP Volume6 Issue9 Pages8215-8223Siti HumairahNo ratings yet
- A Retrospective Study of Success, Failure, and Time Needed To Perform Awake IntubationDocument10 pagesA Retrospective Study of Success, Failure, and Time Needed To Perform Awake IntubationnadaNo ratings yet
- A Pilot Prospective Study On Closed Loop Controlled Ventilation and Oxygenation in Ventilated Children During The Weaning PhaseDocument9 pagesA Pilot Prospective Study On Closed Loop Controlled Ventilation and Oxygenation in Ventilated Children During The Weaning PhaseSiti HumairahNo ratings yet
- Difficult or Impossible Facemask Ventilation in Children With DifficultDocument10 pagesDifficult or Impossible Facemask Ventilation in Children With Difficultema moralesNo ratings yet
- Developing A Neonatal Unit Ventilation Protocol For The Preterm BabyDocument6 pagesDeveloping A Neonatal Unit Ventilation Protocol For The Preterm BabyMALIK MANASRAHNo ratings yet
- Airway Management - StatPearls - NCBI BookshelfDocument7 pagesAirway Management - StatPearls - NCBI BookshelfClarithq LengguNo ratings yet
- LMA Use in Prone Position: An Updated ReviewDocument7 pagesLMA Use in Prone Position: An Updated ReviewAhmad Arif WibowoNo ratings yet
- Paediatric Mechanical Ventilation in The Intensive Care UnitDocument5 pagesPaediatric Mechanical Ventilation in The Intensive Care UnitAndres RiveraNo ratings yet
- Intraoperative Protective Mechanical Ventilation Fact or FictionDocument3 pagesIntraoperative Protective Mechanical Ventilation Fact or Fictionema moralesNo ratings yet
- Lung Recruitment Using Oxygenation during HFVDocument7 pagesLung Recruitment Using Oxygenation during HFVGustavo Carhuamaca RoblesNo ratings yet
- v2.0 11+endgültig+12612787 PDFDocument2 pagesv2.0 11+endgültig+12612787 PDFFadil ElbarcaNo ratings yet
- 134 2020 6048 Moesm12 EsmDocument2 pages134 2020 6048 Moesm12 EsmHalim SudonoNo ratings yet
- 2020 02 13-JMV-Potential-Interventions-for-Novel-Coronavirus-in-China-A-Systemic-ReviewDocument36 pages2020 02 13-JMV-Potential-Interventions-for-Novel-Coronavirus-in-China-A-Systemic-ReviewFrancisco29No ratings yet
- CopyrightDocument2 pagesCopyrightmudasir61No ratings yet
- 134 2020 6048 Moesm12 EsmDocument2 pages134 2020 6048 Moesm12 EsmHalim SudonoNo ratings yet
- 06 - Bryant - Pediatric CPR and Post Arrest Care HandoutDocument10 pages06 - Bryant - Pediatric CPR and Post Arrest Care HandoutHalim SudonoNo ratings yet
- 0007 0012 PDFDocument6 pages0007 0012 PDFHalim SudonoNo ratings yet
- Nutrition Support Critically Ill Pediatrics Aspen 2017Document37 pagesNutrition Support Critically Ill Pediatrics Aspen 2017Lucía González RamírezNo ratings yet
- Toxoplasmic Encephalitis in AIDSDocument12 pagesToxoplasmic Encephalitis in AIDSHalim SudonoNo ratings yet
- Spinal Ropivacaine For Cesarean Section: A Dose-Finding StudyDocument5 pagesSpinal Ropivacaine For Cesarean Section: A Dose-Finding StudyHalim SudonoNo ratings yet
- New Doc 2019-03-04 16.36.41 - 4Document1 pageNew Doc 2019-03-04 16.36.41 - 4Halim SudonoNo ratings yet
- Efficacy of Adductor Canal Block in Total Knee Arthroplasty: A Systematic ReviewDocument10 pagesEfficacy of Adductor Canal Block in Total Knee Arthroplasty: A Systematic ReviewHalim SudonoNo ratings yet
- Your Citilink e-boarding passes from BDO to HLP and HLP to SUBDocument2 pagesYour Citilink e-boarding passes from BDO to HLP and HLP to SUBHalim SudonoNo ratings yet
- Hemodynamic Effects of Lidocaine in Heart PatientsDocument8 pagesHemodynamic Effects of Lidocaine in Heart PatientsHalim SudonoNo ratings yet
- 0051 05 PDFDocument21 pages0051 05 PDFHalim SudonoNo ratings yet
- Evidence Based NSAID PDFDocument16 pagesEvidence Based NSAID PDFmchyusufNo ratings yet
- Confirmation - Check-InDocument2 pagesConfirmation - Check-InHalim SudonoNo ratings yet
- Piis0003497506011143 PDFDocument8 pagesPiis0003497506011143 PDFHalim SudonoNo ratings yet
- Confirmation - Check-In PDFDocument2 pagesConfirmation - Check-In PDFHalim SudonoNo ratings yet
- The Effectiveness of Video Technology As An Adjunct To Teach and Evaluate Epidural Anesthesia Performance SkillsDocument5 pagesThe Effectiveness of Video Technology As An Adjunct To Teach and Evaluate Epidural Anesthesia Performance SkillsHalim SudonoNo ratings yet
- Traumatic Diaphragmatic Hernia Anaesthetic ConsideDocument3 pagesTraumatic Diaphragmatic Hernia Anaesthetic ConsideHalim SudonoNo ratings yet
- TripCase - Print Your ItineraryDocument1 pageTripCase - Print Your ItineraryHalim SudonoNo ratings yet
- Anesthesiologist Perspectives For The Transoral ApproachDocument6 pagesAnesthesiologist Perspectives For The Transoral ApproachHalim SudonoNo ratings yet
- Traumatic Diaphragmatic Hernia Anaesthetic ConsideDocument3 pagesTraumatic Diaphragmatic Hernia Anaesthetic ConsideHalim SudonoNo ratings yet
- Hydrocortisone Vitamin C and Thiamine For The Treatment of SeverDocument37 pagesHydrocortisone Vitamin C and Thiamine For The Treatment of SeverNeelabh SangwanNo ratings yet
- Review Article Intrathecal Drug Spread: G. Hocking and J. A. W. WildsmithDocument11 pagesReview Article Intrathecal Drug Spread: G. Hocking and J. A. W. WildsmithHalim SudonoNo ratings yet
- Pi Is 0007091217439080Document8 pagesPi Is 0007091217439080Halim SudonoNo ratings yet
- Preventing perioperative myocardial ischemiaDocument7 pagesPreventing perioperative myocardial ischemiaHalim SudonoNo ratings yet
- 1600 - Friday - PFT and CPET Case Studies - Marciniuk PDFDocument64 pages1600 - Friday - PFT and CPET Case Studies - Marciniuk PDFtechang1No ratings yet
- Customer Health Checklist for SpasDocument1 pageCustomer Health Checklist for SpaskablasNo ratings yet
- IdentifyDocument40 pagesIdentifyLeonard Kenshin LianzaNo ratings yet
- MSDS WD 40-AerosolDocument5 pagesMSDS WD 40-AerosolYogiNo ratings yet
- The Effectiveness of Workshop and Multimedia Training Methods On The Nurses ' Decision-Making Skills Regarding Weaning From Mechanical VentilationDocument10 pagesThe Effectiveness of Workshop and Multimedia Training Methods On The Nurses ' Decision-Making Skills Regarding Weaning From Mechanical VentilationGlauber CavalcanteNo ratings yet
- IP Lab 6 Respiratory Protocols UPDATEDDocument7 pagesIP Lab 6 Respiratory Protocols UPDATEDstormigirl017No ratings yet
- PNEUMONIADocument8 pagesPNEUMONIARica ParcasioNo ratings yet
- National Neonatal Care Protocol: Prepare BEFORE Delivery - Equipment, Warmth, Getti NG HelpDocument7 pagesNational Neonatal Care Protocol: Prepare BEFORE Delivery - Equipment, Warmth, Getti NG HelpShandy BNo ratings yet
- FELTP Progress Report 2020Document53 pagesFELTP Progress Report 2020ehsanlarikNo ratings yet
- En-Msds-Ea1 - 1903 Supresor de PolvoDocument4 pagesEn-Msds-Ea1 - 1903 Supresor de PolvoAaron Ley QuirozNo ratings yet
- Comprehensive Exam on Professional CaregivingDocument4 pagesComprehensive Exam on Professional CaregivingBitoy AlarconNo ratings yet
- Quick Relaxation StrategiesDocument2 pagesQuick Relaxation Strategiesaahlada srividyaNo ratings yet
- General Safety Instruction - AmmoniaDocument5 pagesGeneral Safety Instruction - AmmoniaVăn Phú PhạmNo ratings yet
- 0 Material Safety Data Sheet: Sodium Diphenylamine Sulphonate MSDSDocument5 pages0 Material Safety Data Sheet: Sodium Diphenylamine Sulphonate MSDSSreenath Menon KNo ratings yet
- Houghton Hocut 795 - BDocument5 pagesHoughton Hocut 795 - BErwinNo ratings yet
- TCCC Skill Set Level 2024Document4 pagesTCCC Skill Set Level 2024Reza Devianto HambaliNo ratings yet
- Technical Drawing FundamentalsDocument14 pagesTechnical Drawing FundamentalsAssortativeRainNo ratings yet
- Safety Data Sheet Linx Fast-Drying Solvent 1512Document5 pagesSafety Data Sheet Linx Fast-Drying Solvent 1512Anselmo SanchezNo ratings yet
- High Blood: Activity #4. Topic: Effects of SmokingDocument2 pagesHigh Blood: Activity #4. Topic: Effects of SmokingRenzo Formanes100% (1)
- SDS - Astm P 126 01Document6 pagesSDS - Astm P 126 01Omar SaaedNo ratings yet
- ATOT Day1Document91 pagesATOT Day1Carl Jaylord CastillanoNo ratings yet
- Hubungan Tungau Debu Rumah Terhadap Angka Kejadian Rinitis Alergi Yang Berobat Di Poli THT Rsud Bangli TAHUN 2019Document12 pagesHubungan Tungau Debu Rumah Terhadap Angka Kejadian Rinitis Alergi Yang Berobat Di Poli THT Rsud Bangli TAHUN 2019RiskaaNo ratings yet
- GHS Label TemplatesDocument1 pageGHS Label TemplatesMariel Louise TanNo ratings yet