Professional Documents
Culture Documents
NCP Assessment Fluid Deficit
Uploaded by
Basema Hashhash0 ratings0% found this document useful (0 votes)
9 views2 pagesThe patient was experiencing nausea, dysuria, and fever, resulting in decreased urine output and risk for deficient fluid volume. The nurse's interventions were to monitor the patient's vital signs and intake/output, maintain IV fluid replacement to correct the fluid deficit, and ensure the patient maintained adequate fluid volume within 8 hours as evidenced by normal urinary output and vital signs. The rationale included addressing factors that influence fluid needs like fever and nausea, using weight to assess possible fluid imbalance, and replacing fluid loss from vomiting to prevent dehydration.
Original Description:
Original Title
NCP-BASEMA
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentThe patient was experiencing nausea, dysuria, and fever, resulting in decreased urine output and risk for deficient fluid volume. The nurse's interventions were to monitor the patient's vital signs and intake/output, maintain IV fluid replacement to correct the fluid deficit, and ensure the patient maintained adequate fluid volume within 8 hours as evidenced by normal urinary output and vital signs. The rationale included addressing factors that influence fluid needs like fever and nausea, using weight to assess possible fluid imbalance, and replacing fluid loss from vomiting to prevent dehydration.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
9 views2 pagesNCP Assessment Fluid Deficit
Uploaded by
Basema HashhashThe patient was experiencing nausea, dysuria, and fever, resulting in decreased urine output and risk for deficient fluid volume. The nurse's interventions were to monitor the patient's vital signs and intake/output, maintain IV fluid replacement to correct the fluid deficit, and ensure the patient maintained adequate fluid volume within 8 hours as evidenced by normal urinary output and vital signs. The rationale included addressing factors that influence fluid needs like fever and nausea, using weight to assess possible fluid imbalance, and replacing fluid loss from vomiting to prevent dehydration.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
NCP
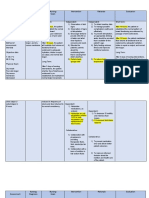
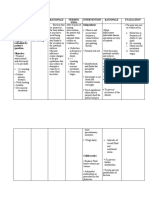
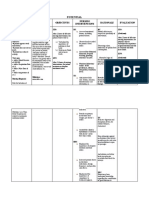
Assessment Explanation Of The Problem Objective Intervention Rationale Evaluation
Subjective: STO: Dx STO:
Deficient FluidVolume Within 30 minutes to 1. Monitor and record 1. Febrile states Within 30 minutes
Related to nausea , one hour of effective vital signs. Especially decrease body to 1 hour of
Objective: dysuria,and fever, nursing interventions: the temperature. fluids by effective nursing
Nausea evidenced by decreased Patient X will perspiration and interventions the
Fever urine output . verbalizes increased patients X
Dysuria awareness of 2. Record intake respiration. This is verbalized
Reference: causative factors and output. known as insensible awareness of
Doenges, M., Moorhouse, and behaviors water loss. causative factors
M., & Murr, A., (2012). essential to correct 3. Note presence of and behaviors
Nurse’s Pocket Guide p. fluid deficit. nausea, vomiting 2. To determine fluid essential to correct
Diagnosis: 413-417 and fever. balance . fluid deficit.
Risk for deficient fluid
volume related to LTO:
fever and nausea. . Tx 3. These factors Within 8 hours of
1. Weigh daily with influence intake, effective nursing
same scale, and fluid needs, and interventions,
preferably at the route of patient
LTO: same time of day. replacement. maintained fluid
Within 8 hours of volume at a
effective nursing 1. Weight is the best functional level as
interventions: assessment data evidenced by
2. Monitor active fluid for possible fluid individually
loss from vomiting; volume imbalance. adequate urinary
maintain accurate An increased in 2 output with normal
input and output lbs a week is specific gravity,
record. consider normal. stable vital signs,
Patient X will 2. Fluid loss from moist mucous
Maintain fluid volume 3. Maintain IV fluid vomiting cause membranes, good
at a functional level as replacement as decreased fluid skin turgor, and
evidenced by ordered to volume and can prompt capillary
individually adequate maintain. lead to refill.
urinary output with EDX dehydration. GOAL MET.
normal specific gravity, 1. Emphasize
stable vital signs, moist importance of oral 3. Dehydrated
mucous membranes, hygiene. patients may be
good skin turgor, and weak and unable
prompt capillary refill. to meet prescribed
intake
2. Encourage patient independently.
to increase fluid
Intake.
1. Fluid deficit can
3.encourage to eat cause a dry, sticky
foods with high fluid mouth. Attention to
content such as mouth care
watermelon and promotes interest in
grapes. drinking and
reduces discomfort
of dry mucous
membranes.
2. To replace fluid
lost and prevent
dehydration.
3. For hydration.
You might also like
- Nursing Care Plan for Fluid Volume DeficitDocument3 pagesNursing Care Plan for Fluid Volume Deficitnj_pink08179456% (9)
- Injera Production and Export Business PlanDocument50 pagesInjera Production and Export Business PlanTumim84% (44)
- MisOr Division Template in Action ResearchDocument14 pagesMisOr Division Template in Action ResearchAmorEmbone100% (2)
- NCP Peptic Ulcer DsDocument4 pagesNCP Peptic Ulcer Dsplug0650% (10)
- ASSESSMENT OUTCOMES INTERVENTIONS RATIONALE EVALUATIONDocument4 pagesASSESSMENT OUTCOMES INTERVENTIONS RATIONALE EVALUATIONArian May Marcos100% (1)
- Drug Study OmeprazoleDocument2 pagesDrug Study OmeprazoleGilianne Jimenea60% (5)
- Written Assignment Week 4Document5 pagesWritten Assignment Week 4Thai50% (2)
- Vibrational Behaviour of The Turbo Generator Stator End Winding in CaseDocument12 pagesVibrational Behaviour of The Turbo Generator Stator End Winding in Casekoohestani_afshin50% (2)
- Ayurveda Fact Sheet AustraliaDocument2 pagesAyurveda Fact Sheet AustraliaRaviNo ratings yet
- Assessment Explanation of The Problem Objective Intervention Rationale Evaluation Subjective: Objective: Sto: DX StoDocument2 pagesAssessment Explanation of The Problem Objective Intervention Rationale Evaluation Subjective: Objective: Sto: DX StoBasema HashhashNo ratings yet
- Assessment Explanation of The Problem Objective Intervention Rationale Expected Outcome Subjective: Objective: Sto: DX Sto: (Goal Met)Document2 pagesAssessment Explanation of The Problem Objective Intervention Rationale Expected Outcome Subjective: Objective: Sto: DX Sto: (Goal Met)Basema HashhashNo ratings yet
- Deficient Fluid Volume (AGEDocument2 pagesDeficient Fluid Volume (AGENursesLabs.com83% (6)
- NCP - AgeDocument5 pagesNCP - Ageunsp3akabl386% (7)
- NCP Deficit Fluid VolumeDocument4 pagesNCP Deficit Fluid VolumeKingJayson Pacman06No ratings yet
- Volume 1Document2 pagesVolume 1roxybiscanteNo ratings yet
- Nursing Diagnosis and InterventionsDocument4 pagesNursing Diagnosis and InterventionsChe SalveronNo ratings yet
- Risk NCP - PESCADERO 4CDocument1 pageRisk NCP - PESCADERO 4COrlando VillanuevaNo ratings yet
- Subjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Document5 pagesSubjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Erle Gray CadangenNo ratings yet
- Nursing Care PlansDocument31 pagesNursing Care PlansCyril Jane Caanyagan AcutNo ratings yet
- NCP Case Analysis GastritisDocument7 pagesNCP Case Analysis GastritisSteffi GolezNo ratings yet
- Gastroenteritis NCPDocument6 pagesGastroenteritis NCPKaguraNo ratings yet
- Nursing Assessment, Planning, Intervention and Evaluation for GastroenteritisDocument2 pagesNursing Assessment, Planning, Intervention and Evaluation for GastroenteritisgeorgiaNo ratings yet
- Actual and potential NCP peptic ulcerDocument3 pagesActual and potential NCP peptic ulcerAdepoju IyinoluwaNo ratings yet
- Assessment/ Cues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale EvaluationDocument6 pagesAssessment/ Cues Nursing Diagnosis Background Knowledge Goal and Objectives Nursing Interventions and Rationale EvaluationimnasNo ratings yet
- Fluid Volume Deficit Related To Loose Watery Stool Diarrhea)Document2 pagesFluid Volume Deficit Related To Loose Watery Stool Diarrhea)Jesse James Advincula Edjec100% (15)
- Hydration and Constipation ManagementDocument3 pagesHydration and Constipation ManagementCharissa de LeonNo ratings yet
- Assessment Nursing Diagnosis Objectives Interventions Rationale EvaluationDocument12 pagesAssessment Nursing Diagnosis Objectives Interventions Rationale EvaluationMaria LeeNo ratings yet
- Cues Nursing Diagnosis Background and Knowledge Goals and Objectives Nursing Intervention and Rationale EvaluationDocument3 pagesCues Nursing Diagnosis Background and Knowledge Goals and Objectives Nursing Intervention and Rationale EvaluationKristiene Kyle AquinoNo ratings yet
- Prado NCPDocument4 pagesPrado NCPalleah pradoNo ratings yet
- Deficient Fluid Volume (Vanene)Document7 pagesDeficient Fluid Volume (Vanene)jajalerNo ratings yet
- Patient Verbalizes Understanding of Causative Factors and Purpose of Individual Therapeutic Interventions and MedicationsDocument3 pagesPatient Verbalizes Understanding of Causative Factors and Purpose of Individual Therapeutic Interventions and MedicationsSheenaGuinoCullaNo ratings yet
- Prio NCP NG Dka ByeDocument5 pagesPrio NCP NG Dka ByeMARIA HILARY TABLANTENo ratings yet
- Risk For Deficient Fluid VolumeDocument3 pagesRisk For Deficient Fluid VolumeALEKS MONTECINO JIMENEZNo ratings yet
- Nursing Assessment and Intervention for DehydrationDocument3 pagesNursing Assessment and Intervention for DehydrationKristil ChavezNo ratings yet
- Assessment Nursing Diagnosis Nursing Goals Intervention Rationale EvaluationDocument5 pagesAssessment Nursing Diagnosis Nursing Goals Intervention Rationale EvaluationKobe ManuelNo ratings yet
- Ninda Komplementer Mual MuntahDocument12 pagesNinda Komplementer Mual MuntahanisaNo ratings yet
- Nursing Care Plan: Assessment Diagnosis Goals Intervention Rationale EvaluationDocument2 pagesNursing Care Plan: Assessment Diagnosis Goals Intervention Rationale EvaluationLeizel ApolonioNo ratings yet
- Nursing care plan for dehydrated child with acute gastroenteritisDocument3 pagesNursing care plan for dehydrated child with acute gastroenteritisRhos Antonette GuimbanNo ratings yet
- Ate Gabs Nyo Pagod NaDocument3 pagesAte Gabs Nyo Pagod NaGabrielle EvangelistaNo ratings yet
- Final Nursing Care PlanDocument7 pagesFinal Nursing Care PlanKatherine BellezaNo ratings yet
- Diabetes Mellitus Nursing Care PlanDocument7 pagesDiabetes Mellitus Nursing Care PlanSheenaGuinoCullaNo ratings yet
- Nursing Care Plan: Assessment Nursing Diagnosis Scientific Background Planning Implementation Rationale EvaluationDocument3 pagesNursing Care Plan: Assessment Nursing Diagnosis Scientific Background Planning Implementation Rationale EvaluationMelrhean GraceNo ratings yet
- Nursing Care Plan: Cues Nursing Diagnosi S Analysis GOAL and Objectives Intervention Rationale EvaluationDocument5 pagesNursing Care Plan: Cues Nursing Diagnosi S Analysis GOAL and Objectives Intervention Rationale EvaluationMark Allison BuenaventuraNo ratings yet
- Managing Overweight through Diet and ExerciseDocument17 pagesManaging Overweight through Diet and ExerciseMarie Ashley CasiaNo ratings yet
- Ncp.-Fluid Volume DeficitDocument1 pageNcp.-Fluid Volume DeficitAdia Cavrinni De JesusNo ratings yet
- Managing Fluid and Electrolyte Imbalances in Older AdultsDocument3 pagesManaging Fluid and Electrolyte Imbalances in Older AdultsLacangan, Thea YvonneNo ratings yet
- CS5 (AGE) Acute Gastroenteritis NCPDocument2 pagesCS5 (AGE) Acute Gastroenteritis NCPAudrie Allyson GabalesNo ratings yet
- NCP1 3Document3 pagesNCP1 3Mary Grace VillegasNo ratings yet
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument7 pagesAssessment Nursing Diagnosis Planning Intervention Rationale EvaluationpamelaideaNo ratings yet
- NCP Post PartumDocument2 pagesNCP Post PartumsteffiNo ratings yet
- Nursing Care Plan for AmebiasisDocument4 pagesNursing Care Plan for AmebiasiskristennemarieNo ratings yet
- ROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPDocument6 pagesROSABIA, Micaela Pauline J. .-BSN-2A-ISDH-GS-NURSERY-NCPkimberly quitonNo ratings yet
- Dengue NCPDocument3 pagesDengue NCPingridNo ratings yet
- Duty RequirementsDocument13 pagesDuty RequirementsRey Jean GarciaNo ratings yet
- MS Soapie #1Document2 pagesMS Soapie #1Fatima KateNo ratings yet
- Assessment Explanation of The Problem Objectives Nursing Interventions Rationale Evaluation Subjective: Sto: DX: Sto: (Goal Met)Document5 pagesAssessment Explanation of The Problem Objectives Nursing Interventions Rationale Evaluation Subjective: Sto: DX: Sto: (Goal Met)Bea Marie A. ValdezNo ratings yet
- Assessing and Treating Acute Gastroenteritis and DehydrationDocument2 pagesAssessing and Treating Acute Gastroenteritis and DehydrationvicenteturasNo ratings yet
- NCP LeptospirosisDocument6 pagesNCP LeptospirosisJean Marie DavidNo ratings yet
- NCP-Fluid Volume DeficitDocument2 pagesNCP-Fluid Volume Deficitanon_207994234100% (1)
- Nursing Care Plan for Fluid Volume DeficitDocument3 pagesNursing Care Plan for Fluid Volume DeficitDan Dan ManaoisNo ratings yet
- Nursing Care Plan for Fluid Volume DeficitDocument7 pagesNursing Care Plan for Fluid Volume DeficitDan Dan ManaoisNo ratings yet
- Nursing Care Plan 1Document2 pagesNursing Care Plan 1Denise GabatoNo ratings yet
- Short Term: Independent: Independent: Short TermDocument2 pagesShort Term: Independent: Independent: Short TermAndre ImperialNo ratings yet
- Freedom from Constipation: Natural Remedies for Digestive HealthFrom EverandFreedom from Constipation: Natural Remedies for Digestive HealthNo ratings yet
- Intestinal Ills Chronic Constipation, Indigestion, Autogenetic Poisons, Diarrhea, Piles, Etc. Also Auto-Infection, Auto-Intoxication, Anemia, Emaciation, Etc. Due to Proctitis and ColitisFrom EverandIntestinal Ills Chronic Constipation, Indigestion, Autogenetic Poisons, Diarrhea, Piles, Etc. Also Auto-Infection, Auto-Intoxication, Anemia, Emaciation, Etc. Due to Proctitis and ColitisNo ratings yet
- Revision FileDocument14 pagesRevision FileBasema HashhashNo ratings yet
- Journal-Of-18 MicuDocument1 pageJournal-Of-18 MicuBasema HashhashNo ratings yet
- Risperidone Drug StudyDocument2 pagesRisperidone Drug StudyBasema HashhashNo ratings yet
- Dosage and Nursing Responsibilities for OlanzapineDocument1 pageDosage and Nursing Responsibilities for OlanzapineBasema HashhashNo ratings yet
- Renal McqsDocument13 pagesRenal McqsShahabuddin Shaikh100% (1)
- Budgeting Your TimeDocument1 pageBudgeting Your TimeBasema HashhashNo ratings yet
- Depression, Bipolar Disorder Chronic Pain InsomniaDocument4 pagesDepression, Bipolar Disorder Chronic Pain InsomniaBasema HashhashNo ratings yet
- Processrecording EnglishDocument5 pagesProcessrecording EnglishBasema HashhashNo ratings yet
- Hashhash, Abtisam Review MoiveDocument2 pagesHashhash, Abtisam Review MoiveBasema HashhashNo ratings yet
- Alalag, Elsie: "The Impact of Access To Immunization Information On Vaccine Acceptance in Three Countries"Document4 pagesAlalag, Elsie: "The Impact of Access To Immunization Information On Vaccine Acceptance in Three Countries"Basema HashhashNo ratings yet
- B - Laroco James C.Document5 pagesB - Laroco James C.Basema HashhashNo ratings yet
- Fdar 22-24 2Document1 pageFdar 22-24 2Basema HashhashNo ratings yet
- BGH August 28 Oct1Document28 pagesBGH August 28 Oct1Basema HashhashNo ratings yet
- OR QuizDocument1 pageOR QuizBasema HashhashNo ratings yet
- Drug Study 1Document13 pagesDrug Study 1Basema HashhashNo ratings yet
- Journal-Of-18 MicuDocument1 pageJournal-Of-18 MicuBasema HashhashNo ratings yet
- JournalDocument32 pagesJournalBasema HashhashNo ratings yet
- HASHHASH, Journal CommunityDocument1 pageHASHHASH, Journal CommunityBasema HashhashNo ratings yet
- MidazolamDocument2 pagesMidazolamDesireemae Riosa-Candaroma100% (6)
- ED Nursing Management of Orthopedic FracturesDocument2 pagesED Nursing Management of Orthopedic FracturesBasema HashhashNo ratings yet
- Body Weakness NCPDocument1 pageBody Weakness NCPArnold Christian QuilonNo ratings yet
- Morphine pain relief side effectsDocument6 pagesMorphine pain relief side effectsBasema HashhashNo ratings yet
- NCP - BasemaDocument2 pagesNCP - BasemaBasema HashhashNo ratings yet
- NCP 1 HyperthermiaDocument3 pagesNCP 1 HyperthermiaBasema HashhashNo ratings yet
- Ncp-Potential-Fernandez Hashhash Navarro PaitDocument3 pagesNcp-Potential-Fernandez Hashhash Navarro PaitBasema HashhashNo ratings yet
- Med Ward JournalDocument2 pagesMed Ward JournalBasema HashhashNo ratings yet
- NCP Impaired Physical MobilityDocument6 pagesNCP Impaired Physical MobilityBasema HashhashNo ratings yet
- College Nursing Drug StudyDocument19 pagesCollege Nursing Drug StudyBasema HashhashNo ratings yet
- Journal Psych WardDocument2 pagesJournal Psych WardBasema HashhashNo ratings yet
- Google in China - A Case StudyDocument11 pagesGoogle in China - A Case StudymyschoolworkNo ratings yet
- Soil MechanicsDocument117 pagesSoil MechanicsChiranjaya HulangamuwaNo ratings yet
- Demand for E-ZPass and Gas GuzzlersDocument11 pagesDemand for E-ZPass and Gas GuzzlersYonn Me Me KyawNo ratings yet
- Work Permit ManualDocument20 pagesWork Permit ManualRoni EnjelaniNo ratings yet
- Professional EthicsDocument2 pagesProfessional EthicsKoushik MeduriNo ratings yet
- Explaining organizational structure based on 5 contingency factorsDocument5 pagesExplaining organizational structure based on 5 contingency factorsdkrirayNo ratings yet
- Cognitive Neuroscience of MusicDocument13 pagesCognitive Neuroscience of MusicMitkoNo ratings yet
- Admin Case DigestDocument8 pagesAdmin Case DigestlenvfNo ratings yet
- UConn Criminal Information SummaryDocument2 pagesUConn Criminal Information SummaryEllyn SantiagoNo ratings yet
- Basic Principles of Cancer ChemotherapyDocument2 pagesBasic Principles of Cancer ChemotherapyGerardLum100% (2)
- Farm, George Orwell: Examples of AlliterationDocument4 pagesFarm, George Orwell: Examples of Alliterationruel_spideyNo ratings yet
- ART. Dworkin - in Praise of Theory PDFDocument16 pagesART. Dworkin - in Praise of Theory PDFmaiasilva70No ratings yet
- DWDM On: Dense Wavelength Division Multiplexing Optical NetworkDocument81 pagesDWDM On: Dense Wavelength Division Multiplexing Optical NetworkNataša Mihić BoskovićNo ratings yet
- Pre-Lab: Ahnaf Habib Khan 40079665 TJ-XDocument2 pagesPre-Lab: Ahnaf Habib Khan 40079665 TJ-XAhnafHabibKhanNo ratings yet
- The Abington Journal 04-20-2011Document28 pagesThe Abington Journal 04-20-2011The Times LeaderNo ratings yet
- People V Pugay DigestDocument2 pagesPeople V Pugay DigestSecret SecretNo ratings yet
- Repaso 5to Grado 3°trimestreDocument25 pagesRepaso 5to Grado 3°trimestreFany BalderramaNo ratings yet
- Prosthetics OrthoticsDocument9 pagesProsthetics OrthoticsSameeha AbbassNo ratings yet
- The Role and Capabilities of The Executive SponsorDocument8 pagesThe Role and Capabilities of The Executive Sponsorkatty_domínguez_8No ratings yet
- Restorative Justice and The Prison MinistryDocument15 pagesRestorative Justice and The Prison MinistrypfipilipinasNo ratings yet
- Smu02b v300r002c02 User Manual 02Document248 pagesSmu02b v300r002c02 User Manual 02Jaime Andres Niño100% (2)
- Success Factors For Augmented Reality Business ModelsDocument36 pagesSuccess Factors For Augmented Reality Business ModelsAsutosh GuptaNo ratings yet
- Conditions of Contract For: ConstructionDocument30 pagesConditions of Contract For: Constructionvladimir100% (2)
- Excel 2003 - CompleteDocument387 pagesExcel 2003 - CompleteRazvan PetrariuNo ratings yet
- Fractured Root Tips During Dental Extractions and Retained Root Fragments. A Clinical Dilemma?Document7 pagesFractured Root Tips During Dental Extractions and Retained Root Fragments. A Clinical Dilemma?Siti Ulfah NesiaNo ratings yet