Professional Documents
Culture Documents
Jurnal Rehab 1
Uploaded by
Sanyuki KhoirunnisaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jurnal Rehab 1
Uploaded by
Sanyuki KhoirunnisaCopyright:
Available Formats
Am J Transl Res 2021;13(7):8316-8322
www.ajtr.org /ISSN:1943-8141/AJTR0129430
Original Article
Effect of early partial weight-bearing rehabilitative
exercise on postoperative functional recovery
of sanders IV calcaneal fractures
Yu Li1*, Lin Xie2*, Wei Li2
1
Department of Traumatic Orthopedicss, Yantai Shan Hospital, Yantai 264000, Shandong, China; 2Department of
Rehabilitation Medicine, Yantai Yuhuangding Hospital, Yantai 264000, Shandong, China. *Equal contributors.
Received January 1, 2021; Accepted February 7, 2021; Epub July 15, 2021; Published July 30, 2021
Abstract: Objectives: This research explored and analyzed the effects of early partial weight-bearing rehabilitative
exercise on postoperative recovery after Sanders IV calcaneal fractures. Methods: 86 patients hospitalized with
Sanders IV calcaneal fracture from April 2018 to January 2020 were selected as the research participants. The
patients were randomly divided into the observation group (n=44) and the control group (n=42). The control group
carried out the conventional rehabilitative exercise, and the observation group underwent early partial weight-bear-
ing rehabilitative exercise. The foot function between the two groups was compared after 24 weeks of treatment.
Results: The foot function of the observation group after 24 weeks of treatment was notably superior to that of the
control group (P<0.05). The Maryland foot function scores of the two groups 6 weeks, 12 weeks and 24 weeks
post-operation were critically higher than those before treatment (P<0.05), and the score of the observation group
was substantially higher than that of the control group (P<0.05). The AOFAS score of patients in the two groups 6
weeks, 12 weeks and 24 weeks post-operation increased apparently than that before treatment (P<0.05), and the
scores of observation group was evidently higher than that of control group (P<0.05). In addition, the comparison
of Angle B’hler and Angle Gissane between the two groups of patients 24 weeks postoperation showed statistically
insignificant difference (P>0.05). Conclusion: The early partial weight-bearing rehabilitative exercise can effectively
promote the postoperative functional recovery of patients with Sander IV calcaneal fractures, and at the same time
it has no impact on internal fixation and calcaneus shape of patients, which is worthy popularizing in clinic.
Keywords: Early partial weight-bearing rehabilitative exercise, sanders IV calcaneal fractures, postoperative, func-
tional recovery
Introduction results in unsatisfactory therapeutic effects [2,
3]. Studies have shown [4] that about 75% of
There are a total of seven tarsal bones in patients have experienced foot dysfunction,
human body. Among which, calcaneus is the and for those with severely injured the disa-
largest tarsal bone, and bears about 40% of bility rate is as high as 30%. Many patients
the body weight when walking and loading [1]. had good surgical reduction, but failed for the
Calcaneal fractures are particularly common in recovery of foot function due to the lack of
clinical work, and it accounts for 60% of tarsal effective postoperative functional exercise.
fractures and 2% of total body fractures. The Besides, there still exist controversies about
anatomical structure of calcaneus is special postoperative weight-bearing functional exer-
and complex, and the mechanism of calcaneal cise [5]. In order to further improve the postop-
injury and fracture types are numerous. In addi- erative recovery of foot function after Sanders
tion, as the foot function is connected with a IV calcaneal fracture, we explored and analyzed
variety of factors such as the shape, anatomi- the effects of early partial weight-bearing reha-
cal angle and the relative position, it is difficult bilitative exercise exerted to the disease. The
to achieve anatomical reduction, and usually details are stated as follows:
Postoperative exercise for sanders type IV calcaneal fracture
Materials and methods postoperation. They underwent joint mobiliza-
tion of subtalar joint, calcaneocubic joint, and
Research objects talar navicular joint, and passively moved the
subtalar joint to gradually restore the range of
86 patients, hospitalized with Sanders IV calca- motion for the three joints. Meanwhile, we
neal fracture from April 2018 to January 2020, adopted the unarmed resistant technique to
were selected as the research participants. perform isometric exercises on patients’ poste-
They were randomly divided into the observa- rior tibial muscle, tibial anterior muscle, and
tion group (n=44) and the control group (n=42) tibial long brevis muscle in order to strengthen
according to random number table. The study the patients’ muscles strength around their
was approved by the ethics committee of our ankle joints. (4) According to fracture degree,
hospital. the patients performed the partial weight-bear-
ing standing or walking in the 13th to 24th
Inclusive criteria
weeks after surgery, and gradually increased
(1) The diagnostic criteria of patients were in the exercise intensity to full weight-bearing.
accordance with Sanders IV calcaneal fracture The proprioceptive training of patients was car-
in Bone and Joint Injury, and the type was fresh ried out by shaking board, so that the patients’
simple fracture [6]; (2) All patients had under- proprioceptive system of ankle and foot can be
gone open reduction and internal fixation (ORIF) recovered; For gait training, it started by shift-
with steel plate; (3) Patients aged between ing the center of gravity left/right and front/
18-60 years; (4) Patients had voluntarily signed back between the legs; For walking practice,
informed consent. the patients were required to reach the equal
support of both feet and same extent in swing
Exclusive criteria phase, until the normal walking gait can be
restored.
(1) Patients with Sanders I, II, III calcaneal frac-
tures; (2) Patients with injuries of vital nerves, The observation group conducted the partial
blood vessels or ligaments; (3) Patients with weight-bearing rehabilitative exercise, and the
immune system diseases, endocrine system specific training program was as follows: The
diseases, etc.; (4) Patients with dysfunctions of rehabilitative trainings for joint activity, muscle
heart, brain, liver or kidney; or (5) Patients with strength and proprioception were the same as
mental disorders. those conducted by the control group. While
starting from the 4th week postoperatively,
Methods these patients received partial weight-bearing
training as well. The patients held the parallel
The control group carried out the regular reha- rod with both hands, and put the mass measur-
bilitation exercises, and the specific process ing instrument under feet to experience the
were as follows: (1) The main treatment from loading weight they can tolerate. The patient’s
the first day to the second week after surgery initial loading weight was 25% of his body
was to reduce swelling. The patient raised the mass, which ranged from 10 to 20 kg, and then
injured foot and began to perform passive toe increased progressively. The patients looked
movements 24 hours after operation. The straight and walked with crutches in a three-
exercise was required to perform in maximum point manner, and started to stand or walk with
range, 3-5 times/group and 6 groups a day. (2) full weight 13 weeks after surgery.
In the 3rd to 6th week after the operation, the
patients continued the above exercises and Observation of indexes
conducted gentle active and passive ex-
ercises of ankle and subtalar joints. The The Maryland foot function scores, including
patients were asked to extend their back or pain and function, were compared between the
plantar flexion as long as they can tolerate, and two groups before surgery, and 6 weeks, 12
maintained for 20 seconds. The exercise was weeks, and 24 weeks after surgery [7]. The
set by 3 to 5 times/group, and 6 groups per scale has a full score of 100 points, and the
day. (3) The patients continued to expand the higher score referred to the better foot func-
range of motion in ankle joint during 2-7 weeks tion. For the earned score, 90-100 is consid-
8317 Am J Transl Res 2021;13(7):8316-8322
Postoperative exercise for sanders type IV calcaneal fracture
Table 1. Comparison of clinical data between the two groups of patients
Number of Gender _ _ Injured part
Group Age (years old, x ± sd) BMI (kg/m2, x ± sd)
cases Male Female Left Right
Observation group 44 25 19 39.18±7.30 23.27±3.10 21 23
Control group 42 22 20 38.75±8.33 23.49±2.71 19 23
t/χ2 - 0.171 0.255 0.350 0.054
P - 0.680 0.799 0.727 0.817
Table 2. Comparison of foot function between the two groups at 24 Comparison of foot func-
weeks after operation [n (%)] tion between two groups
Number of patients 24 weeks after
Group Excellent Good Acceptable Poor treatment
of cases
Observation group 44 26 (59.9) 9 (20.45) 5 (11.36) 4 (9.09)
Control group 42 13 (20.95) 12 (28.57) 8 (19.05) 9 (21.43)
In observation group, there
were 26 cases with excel-
Z - -2.653
lent foot function (59.9%),
P - 0.008
9 cases with good foot
function (20.45%), 5 cases
ered as excellent foot function, 75-89 as good, with fair foot function (11.36%), and 4 cases
50-74 as fair, and <50 as poor foot function. with poor performance (9.09%). The proportion
of patients in control group were 13 (20.95%),
The AOFAS scores of the two groups before sur- 12 (28.57%), 8 (19.05%) and 9 (21.43%). The
gery, and 6 weeks, 12 weeks and 24 weeks foot function of the observation group 24
after surgery were compared [8]. The AOFAS weeks after treatment was notably superior to
score includes the dimensions of daily activity that of the control group (P<0.05), as shown in
function, pain and imaging that comprehen- Table 2.
sively evaluate the patient’s ankle function
recovery, and the full score is 100 points. The Comparison of Maryland foot function score
higher AOFAS score of patients reflects the bet- between the two groups before and after treat-
ter ankle functions. ment
The differences of Angle B’hler and Gissane There was no significant difference in scores of
between the two groups 24 weeks postopera- Maryland foot function before treatment
tion were compared. between the two groups (P>0.05). The scores
Statistical analysis of the two groups 6 weeks, 12 weeks and 24
weeks postoperation were critically higher than
The analysis of data was processed by SPSS those before treatment (P<0.05), and the
22.0. The comparison of measurement data observation group had substantially higher
was done by t-test, enumeration data by χ2 test, scores than the control group (P<0.05) (Table 3
and ordinal data by Kruskal-Wallis test. The sta- and Figure 1A).
tistically significant difference was set by
Comparison of AOFAS scores between the two
P<0.05. The graphic software adopted was
groups before and after treatment
Graphpad prism.
Results There was no significant difference in AOFAS
scores before treatment between the two
Clinical data groups (P>0.05). The score of both groups of
patients 6 weeks, 12 weeks and 24 weeks
There was insignificant difference in clinical postoperation increased apparently than those
data between the two groups (P>0.05), as before treatment (P<0.05), and the observa-
shown in Table 1. tion group had evidently higher score than the
8318 Am J Transl Res 2021;13(7):8316-8322
Postoperative exercise for sanders type IV calcaneal fracture
Table 3. Comparison
_ of Maryland foot function score between the two groups before and after treat-
ment (points, x ± sd)
Number of Before 6 weeks 12 weeks 24 weeks
Group
cases treatment postoperatively postoperatively postoperatively
Observation group 44 14.28±3.11 41.26±5.49* 61.73±8.11* 89.74±10.23*
Control group 42 13.97±2.98 36.58±4.85* 53.03±7.52* 81.29±9.52*
t - 0.472 4.182 5.152 3.961
P - 0.638 <0.001 <0.001 <0.001
Note: *P<0.05 compared with the same group before treatment.
control group (P<0.05), as shown in Table 4
and Figure 1B.
Comparison of Angle B’hler and Gissane be-
tween the two groups 24 weeks after opera-
tion
The difference of Angle B’hler and Angle
Gissane between the two groups of patients 24
weeks after operation was statistically insignifi-
cant (P>0.05) (Table 5).
Discussion
Calcaneus fracture is one of the most common
types of tarsal fractures. Most calcaneal frac-
tures are caused by a fall from a height or a
vertical impact on the heel after the foot hits
the ground. Orthopedic clinicians have con-
ducted in-depth researches on the types of
calcaneal fractures, operation timing, incision
positioning, and internal fixation, but there are
still patients who have not achieved good reha-
bilitative results. In recent years, an increasing
number of scholars have focused on the post-
operative rehabilitative exercise on foot func-
tion recovery of patients with calcaneal
fractures [9, 10]. Wound complications and
postoperative recovery of joint function are
two major problems in the treatment of calca-
neal fractures. As we all know, anatomical
reduction and rigid internal fixation are the
basis for achieving ideal treatment effect, and
the active rehabilitation exercise after surgery
is also a crucial part that impacts the re-
covery of joint function [11]. The articular sur-
faces of calcaneus and talus, anterior, middle
and heel constitute the special structure of the
Figure 1. Comparison of Maryland foot function score subtalar joint. After calcaneal fracture, the
and AOFAS scores between the two groups before anastomosis with the surrounding small joints
and after treatment. Note: (A) Maryland foot function
score; (B) AOFAS scores. *P<0.05 compared with the will be affected, and varying degrees of ankle
same group before treatment; #P<0.05 compared dysfunction in ankle joint will be caused [12,
with the control group. 13]. The prolonged immobilization during peri-
8319 Am J Transl Res 2021;13(7):8316-8322
Postoperative exercise for sanders type IV calcaneal fracture
_
Table 4. Comparison of AOFAS scores between the two groups before and after treatment (points, x
± sd)
Number of Before 6 weeks 12 weeks 24 weeks
Group
cases treatment postoperatively postoperatively postoperatively
Observation group 44 10.25±2.17 37.69±5.47 57.84±8.95 83.42±8.54
Control group 42 10.96±2.58 33.21±4.36 51.06±6.08 76.42±7.03
t - 1.384 4.188 4.090 4.139
P - 0.170 <0.001 <0.001 <0.001
Table 5. Angle B’hler angle and Gissane at 24 weeks Sanders IV calcaneal fractures were ana-
postoperatively between the two groups lyzed.
Number The study demonstrated that the foot
Group B’hler Gissane
of cases
function of the observation group was
Observation group 44 30.28±3.16 131.57±6.38 remarkably superior to that of the control
Control group 42 30.97±2.98 130.89±5.37 group after 24 weeks of treatment. The
t - 1.041 0.534 improvement of Maryland foot function
P - 0.301 0.595 scores and the AOFAS scores of the ob-
servation group 6 weeks, 12 weeks and
24 weeks after operation were substan-
operative period may lead to capsular contrac- tially better than those of the control group.
ture, muscle atrophy and osteoporosis, and These results are consistent with the findings
result in ankle stiffness, foot pain and discom- of other scholars [22, 23], suggesting that
fort [14]. Studies reported by other scholars early partial weight-bearing rehabilitative exer-
[15, 16] revealed that early rehabilitative exer- cise can effectively promote the rehabilitation
cise could effectively reduce the postoperative of patients. The exercise is beneficial to the
wound infection and promote the recovery of recovery of muscle strength and body circula-
ankle joint function. In addition, studies have tion, and is also beneficial to enhancing
shown that effective postoperative rehabilita- patients’ confidence in recovery of body func-
tion exercise can promote the regression of tion. In addition, the difference of Angle B’hler
body swelling, and accelerate the absorption and Angle Gissane between the two groups of
of inflammatory factors. Meanwhile, the active patients 24 weeks postoperation was statisti-
rehabilitation exercise can avoid the arthrogry- cally insignificant, indicating that the early
posis of Achilles tendon, and the injuries to the partial weight-bearing rehabilitative exercise
motion range of important adjacent joints in brings no impact to the fracture internal fix-
each axis caused by adhesion of ankle joint, ation and calcaneus shape of patients with
and provide a good basis for the recovery of calcaneal fractures.
patient’s postoperative functions [17, 18].
To conclude, the early partial weight-bearing
In recent years, there is still a great contro- rehabilitative exercise can effectively promote
versy about whether to carry out early weight- the postoperative functional recovery of pati-
bearing rehabilitative exercise for calcaneal ents with Sander IV calcaneal fractures, and at
fractures with articular surface damage. Some the same time has no impact on internal fixa-
scholars held that early weight-bearing exer- tion and calcaneus shape of patients, which is
cise after calcaneal fracture may increase the worthy popularizing in clinic.
risk of collapse of the subtalar articular sur-
face. Others shared that early weight-bearing Disclosure of conflict of interest
exercise will not cause the displacement of
fractures and affect the stability of internal None.
fixation, but can promote the postoperative
functional recovery of patients and reduce the Address correspondence to: Wei Li, Department
risk of osteoporosis [19-21]. In this research, of Rehabilitation Medicine, Yantai Yuhuangding
the effects of early partial weight-bearing reha- Hospital, No. 20 Yuhuangding East Road, Zhifu
bilitative exercise on postoperative recovery of District, Yantai 264000, Shandong, China. Tel: +86-
8320 Am J Transl Res 2021;13(7):8316-8322
Postoperative exercise for sanders type IV calcaneal fracture
0535-6691999-83613; E-mail: liwei13053542- [11] Magaziner J, Mangione KK, Orwig D, Baumgar-
572@163.com ten M, Magder L, Terrin M, Fortinsky RH, Gru-
ber-Baldini AL, Beamer BA, Tosteson ANA,
References Kenny AM, Shardell M, Binder EF, Koval K,
Resnick B, Miller R, Forman S, McBride R and
[1] Nerz C, Schwickert L, Becker C, Studier-Fischer Craik RL. Effect of a multicomponent home-
S, Müßig JA and Augat P. Effectiveness of ro- based physical therapy intervention on ambu-
bot-assisted training added to conventional lation after hip fracture in older adults: the CAP
rehabilitation in patients with humeral fracture randomized clinical trial. JAMA 2019; 322:
early after surgical treatment: protocol of a 946-956.
randomised, controlled, multicentre trial. Trials [12] Uda K, Matsui H, Fushimi K and Yasunaga H.
2017; 18: 589. Intensive in-hospital rehabilitation after hip
[2] Su B, Newson R, Soljak H and Soljak M. Asso- fracture surgery and activities of daily living in
ciations between post-operative rehabilitation patients with dementia: retrospective analysis
of hip fracture and outcomes: national data- of a nationwide inpatient database. Arch Phys
base analysis (90 characters). BMC Musculo- Med Rehabil 2019; 100: 2301-2307.
skelet Disord 2018; 19: 211. [13] Asplin G, Carlsson G, Zidén L and Kjellby-
[3] Lee SY, Yoon BH, Beom J, Ha YC and Lim JY. Wendt G. Early coordinated rehabilitation in
Effect of lower-limb progressive resistance ex- acute phase after hip fracture - a model for in-
ercise after hip fracture surgery: a systematic creased patient participation. BMC Geriatr
review and meta-analysis of randomized con- 2017; 17: 240.
trolled studies. J Am Med Dir Assoc 2017; 18: [14] Büker N, Şavkın R and Ök N. Comparison of
1096. supervised exercise and home exercise after
[4] Caforio M and Maniscalco P. The importance ankle fracture. J Foot Ankle Surg 2019; 58:
of early rehabilitation in proximal humeral frac- 822-827.
ture: a clinical trial of efficacy and safety of a
[15] Kristensen MT, Öztürk B, Röck ND, Ingeman A,
new endomedullary nail. J Back Musculoskelet
Palm H and Pedersen AB. Regaining pre-frac-
Rehabil 2017; 30: 195-202.
ture basic mobility status after hip fracture
[5] Quadlbauer S, Pezzei C, Jurkowitsch J,
and association with post-discharge mortality
Rosenauer R, Kolmayr B, Keuchel T, Simon D,
and readmission-a nationwide register study in
Beer T, Hausner T and Leixnering M. Rehabili-
Denmark. Age Ageing 2019; 48: 278-284.
tation after distal radius fractures: is there a
[16] Williamson M, Iliopoulos E, Jain A, Ebied W and
need for immobilization and physiotherapy?
Trompeter A. Immediate weight bearing after
Arch Orthop Trauma Surg 2020; 140: 651-
plate fixation of fractures of the tibial plateau.
663.
Injury 2018; 49: 1886-1890.
[6] Lee SY, Jung SH, Lee SU, Ha YC and Lim JY. Ef-
fect of balance training after hip fracture sur- [17] Berggren M, Karlsson Å, Lindelöf N, Englund U,
gery: a systematic review and meta-analysis of Olofsson B, Nordström P, Gustafson Y and
randomized controlled studies. J Gerontol A Stenvall M. Effects of geriatric interdisciplinary
Biol Sci Med Sci 2019; 74: 1679-1685. home rehabilitation on complications and re-
[7] Dehghan N, Mitchell SM and Schemitsch EH. admissions after hip fracture: a randomized
Rehabilitation after plate fixation of upper and controlled trial. Clin Rehabil 2019; 33: 64-73.
lower extremity fractures. Injury 2018; 49: [18] Lahtinen A, Leppilahti J, Vähänikkilä H, Har-
S72-S77. mainen S, Koistinen P, Rissanen P and
[8] Diong J, Allen N and Sherrington C. Structured Jalovaara P. Costs after hip fracture in inde-
exercise improves mobility after hip fracture: a pendently living patients: a randomised com-
meta-analysis with meta-regression. Br J parison of three rehabilitation modalities. Clin
Sports Med 2016; 50: 346-355. Rehabil 2017; 31: 672-685.
[9] Fischer K, Trombik M, Freystätter G, Egli A, [19] Pils K. Physical medical aspects of early reha-
Theiler R and Bischoff-Ferrari HA. Timeline of bilitation after proximal femoral fractures. Z
functional recovery after hip fracture in seniors Gerontol Geriatr 2018; 51: 711-721.
aged 65 and older: a prospective observation- [20] Henkelmann R, Schneider S, Müller D, Gahr R,
al analysis. Osteoporos Int 2019; 30: 1371- Josten C and Böhme J. Outcome of patients
1381. after lower limb fracture with partial weight
[10] Kraus TM, Abele C, Freude T, Ateschrang A, bearing postoperatively treated with or without
Stöckle U, Stuby FM and Schröter S. Duration anti-gravity treadmill (alter G) during six weeks
of incapacity of work after tibial plateau frac- of rehabilitation - a protocol of a prospective
ture is affected by work intensity. BMC Muscu- randomized trial. BMC Musculoskelet Disord
loskelet Disord 2018; 19: 281. 2017; 18: 104.
8321 Am J Transl Res 2021;13(7):8316-8322
Postoperative exercise for sanders type IV calcaneal fracture
[21] Monticone M, Ambrosini E, Brunati R, Capone [23] Rexiti P, Zhang TC, Batuer C and Cao L. Ortho-
A, Pagliari G, Secci C, Zatti G and Ferrante S. pedic treatment for open fracture of lower ex-
How balance task-specific training contributes tremities and soft tissue defects in young chil-
to improving physical function in older subjects dren and rapid rehabilitation after operation.
undergoing rehabilitation following hip frac- Phys Sportsmed 2020; 48: 161-164.
ture: a randomized controlled trial. Clin Reha-
bil 2018; 32: 340-351.
[22] Hasebe K, Momosaki R, Sawabe M, Chono M,
Sawaguchi A, Kasuga S, Asanuma D, Suzuki S,
Miyauchi N and Abo M. Effectiveness of week-
end physical rehabilitation for functional recov-
ery in geriatric patients with hip fracture. Geri-
atr Gerontol Int 2018; 18: 1143-1146.
8322 Am J Transl Res 2021;13(7):8316-8322
You might also like
- Principles of Manual Medicine for Sacroiliac Joint Dysfunction: Arthrokinematic Approach-Hakata MethodFrom EverandPrinciples of Manual Medicine for Sacroiliac Joint Dysfunction: Arthrokinematic Approach-Hakata MethodShigehiko KatadaNo ratings yet
- Aust JPhysiotherv 51 I 1 ShawDocument9 pagesAust JPhysiotherv 51 I 1 ShawPrime PhysioNo ratings yet
- 10 1155@2019@1694695Document8 pages10 1155@2019@1694695DATO13No ratings yet
- The Long-Term Effect of 2 PostoperativeDocument9 pagesThe Long-Term Effect of 2 Postoperativeahmed K.Abd el SaterNo ratings yet
- Effects On Lower Extremity Neuromuscular Control Exercises On Knee PDFDocument7 pagesEffects On Lower Extremity Neuromuscular Control Exercises On Knee PDFEva MartinezNo ratings yet
- Gunnarsson 2011Document5 pagesGunnarsson 2011dwimellyndaNo ratings yet
- 27 Sankarlingam EtalDocument4 pages27 Sankarlingam EtaleditorijmrhsNo ratings yet
- Choi Et. Al. (2005) - Exercício IsoladDocument9 pagesChoi Et. Al. (2005) - Exercício IsoladFrancieleNo ratings yet
- Effects of Distally Fixated Versus Nondistally Fixated Leg Extensor Resistance Training On Knee Pain in The Early Period After Anterior Cruciate Ligament ReconstructionDocument9 pagesEffects of Distally Fixated Versus Nondistally Fixated Leg Extensor Resistance Training On Knee Pain in The Early Period After Anterior Cruciate Ligament ReconstructionMirna Vasquez MacayaNo ratings yet
- Alfredson AchillesDocument7 pagesAlfredson AchillesTonyNo ratings yet
- Ijos - Acl PaperDocument5 pagesIjos - Acl Paperavinashrao39No ratings yet
- Aust JPhysiotherv 50 I 2 HayesDocument7 pagesAust JPhysiotherv 50 I 2 HayesAnderson Landim MilletusNo ratings yet
- Effects of Scapular Stabilization Exercise Training OnDocument12 pagesEffects of Scapular Stabilization Exercise Training OnNajoua SalomaoNo ratings yet
- 1 s2.0 S1607551X09703614 MainDocument8 pages1 s2.0 S1607551X09703614 MainAchenk BarcelonistaNo ratings yet
- 1651171792jmpas April 2022Document3 pages1651171792jmpas April 2022matiaspenrozvaldiviaNo ratings yet
- ArticuloDocument10 pagesArticuloYucely BermudezNo ratings yet
- 2009 Ericsson Et Al-2009-Scandinavian Journal of Medicine & Science in SportsDocument10 pages2009 Ericsson Et Al-2009-Scandinavian Journal of Medicine & Science in SportsLuis MiguelNo ratings yet
- 10 1111@sms 13853Document17 pages10 1111@sms 13853Cintia BeatrizNo ratings yet
- Jpts 27 2621Document4 pagesJpts 27 2621vvNo ratings yet
- Hooper Et Al. - 2002 - Gait Analysis 6 and 12 Months After Anterior Cruciate Ligament Reconstruction SurgeryDocument11 pagesHooper Et Al. - 2002 - Gait Analysis 6 and 12 Months After Anterior Cruciate Ligament Reconstruction SurgeryAwatef FituriNo ratings yet
- Difference in Balance Measures Between Patients With Chronic Ankle Instability and Patients After An Acute Ankle Inversion TraumaDocument17 pagesDifference in Balance Measures Between Patients With Chronic Ankle Instability and Patients After An Acute Ankle Inversion TraumaAbu MishalNo ratings yet
- Use of A Static Progressive Stretch Orthosis To Treat Post-Traumatic Ankle StiffnessDocument5 pagesUse of A Static Progressive Stretch Orthosis To Treat Post-Traumatic Ankle StiffnessNararyo anantoNo ratings yet
- 27 PDFDocument7 pages27 PDFMunni KNo ratings yet
- JurnalDocument8 pagesJurnalSelingan SenjaNo ratings yet
- Efficacy of Sot in FemalesDocument7 pagesEfficacy of Sot in FemalesDenise MathreNo ratings yet
- Research Article: Effects of Low-Level Laser Therapy and Eccentric Exercises in The Treatment of Patellar TendinopathyDocument7 pagesResearch Article: Effects of Low-Level Laser Therapy and Eccentric Exercises in The Treatment of Patellar TendinopathyAlvin JulianNo ratings yet
- CMJ2009 - 7 (2) E4Document5 pagesCMJ2009 - 7 (2) E4sulis tiyowatiNo ratings yet
- Perturbation Training Prior To ACL Reconstruction Improves Gait Asymmetries in Non-CopersDocument6 pagesPerturbation Training Prior To ACL Reconstruction Improves Gait Asymmetries in Non-CopersMario Peraza MurilloNo ratings yet
- Pain, Trunk Muscle Strength, Spine Mobility and Disability Following Lumbar Disc SurgeryDocument5 pagesPain, Trunk Muscle Strength, Spine Mobility and Disability Following Lumbar Disc Surgerye7choevaNo ratings yet
- C Rioter ApyDocument6 pagesC Rioter ApyDanNy ClaudiuNo ratings yet
- Return Sport Post Atroskopi SholdrDocument8 pagesReturn Sport Post Atroskopi SholdrFarhan JustisiaNo ratings yet
- 0269215511423557Document10 pages0269215511423557Jose Maria DominguezNo ratings yet
- Comparison of Effect of Hip Joint Mobilization and Hip Joint Muscle Strengthening Exercises With Knee Osteoarthritis A. Tanvi, R. Amrita, R. Deepak, P. Kopal Srji Vol 3-Issue 1 Year 2014Document13 pagesComparison of Effect of Hip Joint Mobilization and Hip Joint Muscle Strengthening Exercises With Knee Osteoarthritis A. Tanvi, R. Amrita, R. Deepak, P. Kopal Srji Vol 3-Issue 1 Year 2014Dr. Krishna N. Sharma100% (1)
- The Immediate Effects of Lumbar Rotational Mobilization On Trunk Control and Gait Parameter in Patients With StrokeDocument7 pagesThe Immediate Effects of Lumbar Rotational Mobilization On Trunk Control and Gait Parameter in Patients With Stroke林良駿No ratings yet
- Evaluation of The Lateral Instability of The Ankle by Inversion Simulation Device and Assessment of The Rehabilitation ProgramDocument13 pagesEvaluation of The Lateral Instability of The Ankle by Inversion Simulation Device and Assessment of The Rehabilitation ProgramZzDel VerdeNo ratings yet
- ArticuloDocument9 pagesArticuloPARA PASAR VIDEOSNo ratings yet
- The Timing of Rehabilitation Commencement After Reconstruction of The Anterior Cruciate LigamentDocument5 pagesThe Timing of Rehabilitation Commencement After Reconstruction of The Anterior Cruciate LigamentQuiroprácticaParaTodosNo ratings yet
- Quadriceps Muscle Function After Rehabilitation With Cryotherapy in Patients With Anterior Cruciate Ligament ReconstructionDocument7 pagesQuadriceps Muscle Function After Rehabilitation With Cryotherapy in Patients With Anterior Cruciate Ligament ReconstructionMarco Antonio Silva RiveraNo ratings yet
- Critical Time Period For Recovery of Functional Range of Motion After Surgical Treatment of Complex Elbow Instability: Prospective Study On 76 PatientsDocument7 pagesCritical Time Period For Recovery of Functional Range of Motion After Surgical Treatment of Complex Elbow Instability: Prospective Study On 76 PatientsMutiara Rachmawati ViorhaNo ratings yet
- Extension LagDocument5 pagesExtension LagjeremyjlNo ratings yet
- JSR Article p335Document11 pagesJSR Article p335MarianoNo ratings yet
- Colgan 2016Document6 pagesColgan 2016Wahyu InsanNo ratings yet
- Bodkin - Time Between RTP Assessments To Achieve Strength Gains post-ACLR - 2019Document8 pagesBodkin - Time Between RTP Assessments To Achieve Strength Gains post-ACLR - 2019krayfieldNo ratings yet
- DONEDocument7 pagesDONEpashaNo ratings yet
- Pzac 056Document9 pagesPzac 056ganesh goreNo ratings yet
- 28 - Jpts 2016 190Document6 pages28 - Jpts 2016 190alsyafarinoorNo ratings yet
- Mobility Training After Hip FractureDocument7 pagesMobility Training After Hip FracturewirasenaNo ratings yet
- Anterior Cruciate Ligament Injury-Who Succeeds WitDocument9 pagesAnterior Cruciate Ligament Injury-Who Succeeds WitNura Eky VNo ratings yet
- Hamstring Muscle Strain Treated by Mobilizing The Sacroiliac JointDocument4 pagesHamstring Muscle Strain Treated by Mobilizing The Sacroiliac JointKarthik BhashyamNo ratings yet
- Effectiveness of Hallux Valgus' Correction To Improve Triple Jump and Long Jump Performance of A Female Athlete: A Case ReportDocument3 pagesEffectiveness of Hallux Valgus' Correction To Improve Triple Jump and Long Jump Performance of A Female Athlete: A Case ReportajmrdNo ratings yet
- Effects of The Bad Ragaz Ring Method On Muscle Activation of The Lower Limbs and Balance Ability in Chronic Stroke: A Randomised Controlled TrialDocument7 pagesEffects of The Bad Ragaz Ring Method On Muscle Activation of The Lower Limbs and Balance Ability in Chronic Stroke: A Randomised Controlled TrialDianaNo ratings yet
- Heavy-Load Eccentric Calf Muscle Training For The Treatment of Chronic Achilles TendinosisDocument8 pagesHeavy-Load Eccentric Calf Muscle Training For The Treatment of Chronic Achilles TendinosisburgoschileNo ratings yet
- Imagenes PBODocument13 pagesImagenes PBOPaulina CelisNo ratings yet
- Effects of 4 Weeks of Elastic-Resistance Training On Ankle-Evertor Strength and LatencyDocument17 pagesEffects of 4 Weeks of Elastic-Resistance Training On Ankle-Evertor Strength and LatencyUpender YadavNo ratings yet
- Evaluation of Gait Kinematics and Symmetry During The First Two Stages of Physiotherapy After Anterior Cruciate Ligament ReconstructionDocument10 pagesEvaluation of Gait Kinematics and Symmetry During The First Two Stages of Physiotherapy After Anterior Cruciate Ligament ReconstructionZaro AnitaNo ratings yet
- X Xdonghwan Park, XX X Xji-Hyun Lee, XX X Xtae-Woo Kang, XX and X Xheon-Seock Cynn, XXDocument9 pagesX Xdonghwan Park, XX X Xji-Hyun Lee, XX X Xtae-Woo Kang, XX and X Xheon-Seock Cynn, XXRay HannaNo ratings yet
- EJHM - Volume 89 - Issue 2 - Pages 6617-6621Document5 pagesEJHM - Volume 89 - Issue 2 - Pages 6617-6621emad ahmedNo ratings yet
- Open Kinetic Chain Exercises in A Restricted Range of Motion After Anterior Cruciate Ligament Reconstruction - Fukuda2013Document8 pagesOpen Kinetic Chain Exercises in A Restricted Range of Motion After Anterior Cruciate Ligament Reconstruction - Fukuda2013Adriano SantosNo ratings yet
- Neurorobotics Presentation 3Document8 pagesNeurorobotics Presentation 3Hamza MinhasNo ratings yet
- Case 12749: Spontaneous Pneumothorax: A Complication of TuberculosisDocument8 pagesCase 12749: Spontaneous Pneumothorax: A Complication of TuberculosisSanyuki KhoirunnisaNo ratings yet
- Penurunan Kesadaran (Decreased of Consiousness)Document26 pagesPenurunan Kesadaran (Decreased of Consiousness)Sanyuki KhoirunnisaNo ratings yet
- Introduksi Chest X RayDocument64 pagesIntroduksi Chest X RaySanyuki KhoirunnisaNo ratings yet
- Pharmacon: Nony L. Poana, Weny I. Wiyono, Deby A. MpilaDocument10 pagesPharmacon: Nony L. Poana, Weny I. Wiyono, Deby A. MpilaSanyuki KhoirunnisaNo ratings yet
- 01 Pregnancy To 0 11 MonthsDocument12 pages01 Pregnancy To 0 11 MonthsSanyuki KhoirunnisaNo ratings yet
- Squirrel Cage Induction Motor Preventive MaintenaceDocument6 pagesSquirrel Cage Induction Motor Preventive MaintenaceNishantPareekNo ratings yet
- Continue: Rudolf Bultmann Theology of The New Testament PDFDocument3 pagesContinue: Rudolf Bultmann Theology of The New Testament PDFpishoi gerges0% (1)
- QA/QC Checklist - Installation of MDB Panel BoardsDocument6 pagesQA/QC Checklist - Installation of MDB Panel Boardsehtesham100% (1)
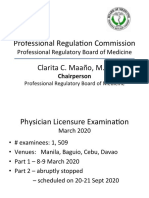
- Professional Regula/on Commission: Clarita C. Maaño, M.DDocument31 pagesProfessional Regula/on Commission: Clarita C. Maaño, M.Dmiguel triggartNo ratings yet
- Properties of Moist AirDocument11 pagesProperties of Moist AirKarthik HarithNo ratings yet
- 18 - PPAG-100-HD-C-001 - s018 (VBA03C013) - 0 PDFDocument1 page18 - PPAG-100-HD-C-001 - s018 (VBA03C013) - 0 PDFSantiago GarciaNo ratings yet
- 06-Apache SparkDocument75 pages06-Apache SparkTarike ZewudeNo ratings yet
- Tivoli Performance ViewerDocument4 pagesTivoli Performance ViewernaveedshakurNo ratings yet
- Employees' Pension Scheme, 1995: Form No. 10 C (E.P.S)Document4 pagesEmployees' Pension Scheme, 1995: Form No. 10 C (E.P.S)nasir ahmedNo ratings yet
- Topic 4: Mental AccountingDocument13 pagesTopic 4: Mental AccountingHimanshi AryaNo ratings yet
- STM - Welding BookDocument5 pagesSTM - Welding BookAlvin MoollenNo ratings yet
- Manufacturing StrategyDocument31 pagesManufacturing Strategyrajendra1pansare0% (1)
- Cam Action: Series: Inch StandardDocument6 pagesCam Action: Series: Inch StandardVishwa NNo ratings yet
- M2 Economic LandscapeDocument18 pagesM2 Economic LandscapePrincess SilenceNo ratings yet
- 1SXP210003C0201Document122 pages1SXP210003C0201Ferenc SzabóNo ratings yet
- Separation PayDocument3 pagesSeparation PayMalen Roque Saludes100% (1)
- Blade Torrent 110 FPV BNF Basic Sales TrainingDocument4 pagesBlade Torrent 110 FPV BNF Basic Sales TrainingMarcio PisiNo ratings yet
- Are Groups and Teams The Same Thing? An Evaluation From The Point of Organizational PerformanceDocument6 pagesAre Groups and Teams The Same Thing? An Evaluation From The Point of Organizational PerformanceNely Noer SofwatiNo ratings yet
- Brochure Ref 670Document4 pagesBrochure Ref 670veerabossNo ratings yet
- Lea 4Document36 pagesLea 4Divina DugaoNo ratings yet
- Algorithmique Et Programmation en C: Cours Avec 200 Exercices CorrigésDocument298 pagesAlgorithmique Et Programmation en C: Cours Avec 200 Exercices CorrigésSerges KeouNo ratings yet
- 21st Bomber Command Tactical Mission Report 178, OcrDocument49 pages21st Bomber Command Tactical Mission Report 178, OcrJapanAirRaidsNo ratings yet
- Zelio Control RM35UA13MWDocument3 pagesZelio Control RM35UA13MWSerban NicolaeNo ratings yet
- Aisladores 34.5 KV Marca Gamma PDFDocument8 pagesAisladores 34.5 KV Marca Gamma PDFRicardo MotiñoNo ratings yet
- The Effectiveness of Risk Management: An Analysis of Project Risk Planning Across Industries and CountriesDocument13 pagesThe Effectiveness of Risk Management: An Analysis of Project Risk Planning Across Industries and Countriesluisbmwm6No ratings yet
- Vinera Ewc1201Document16 pagesVinera Ewc1201josue1965No ratings yet
- Brand Positioning of PepsiCoDocument9 pagesBrand Positioning of PepsiCoAbhishek DhawanNo ratings yet
- RevisionHistory APFIFF33 To V219Document12 pagesRevisionHistory APFIFF33 To V219younesNo ratings yet
- Electrical ConnectorsDocument5 pagesElectrical ConnectorsRodrigo SantibañezNo ratings yet
- Role of The Government in HealthDocument6 pagesRole of The Government in Healthptv7105No ratings yet