Professional Documents
Culture Documents
Antiplatelet Medications Mechanism Atf
Uploaded by
Amir mohammad moori MohammadiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antiplatelet Medications Mechanism Atf
Uploaded by
Amir mohammad moori MohammadiCopyright:
Available Formats
Last edited: 9/25/2021
1. ANTI-PLATELET MEDICATIONS
Anti-platelet Medications | Mechanism of Action, Medical Editor: Abigail S. Xu, RPh
Indications, Adverse Reactions, Contraindications
OUTLINE
(A) TXA2 SYNTHESIS INHIBITORS
I) MECHANISM OF ACTION
II) INDICATIONS
III) ADVERSE DRUG REACTIONS (ADRS)
IV) CONTRAINDICATIONS
V) REVIEW QUESTIONS
VI) REFERENCES
I) MECHANISM OF ACTION
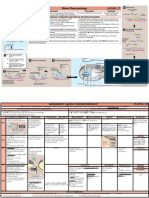
Hemostasis Overview
Endothelial Cells
● line the inner portion of blood vessels
● release chemicals such as PGI2 and Nitric Oxide (NO) Figure 2. TXA2 Synthesis
that inactivate platelets to keep blood antithrombotic
● damaged vessel lining → ↓PGI2 and NO → ↓inhibition of TXA2 Roles
platelet → ↑platelet that attach to endothelial lining ● Activate Gq pathway → activate Phospholipase C (PLC)
→ break down PIP2 into IP3 and DAG
von Willebrand Factor (vWF)
Inositol Triphosphate (IP3)
● proteins that attach to the exposed collagen following o Binds to endoplasmic reticulum-like network and
endothelial damage stimulate protein channel to shuttle out Ca2+
● made by endothelial cells and platelets o Shuttled out Ca2+ stimulates degranulation →
release of ADP, 5HT, Ca2+, TXA2 → ↑platelet
Glycoprotein Ib (GPIb) aggregation
● binds platelet to VWF Diacylglycerol (DAG)
o activate Protein Kinase C (PKC) → stimulate GP
Delta/ Dense granules
IIb/IIIa → stabilize platelet plug
● release platelet aggregation agents that call other
platelets to the injured site Drug that Inhibits TXA2 Synthesis
o Serotonin (5HT) Aspirin (ASA)
o ADP
o Ca2+ ● irreversibly inhibits cyclooxygenase (COX) 1 and 2 that
o Thromboxane A2 (TXA2) are responsible for the conversion of arachidonic acid to
PGG2, ultimately leading to decrease in TXA2 production
Glycoprotein IIb/IIIa (GP IIb/IIIa) → ↓platelet aggregation & ↓stability of platelet plug
● protein complex on the surface of platelets [Trevor, Katzung, & (B) ADP RECEPTOR INHIBITORS
Kruidering-Hall, 2015]
● when activated, aggregates platelets by binding to fibrin ADP Roles
[Trevor, Katzung, & Kruidering-Hall, 2015]
a. bind to P2Y12 receptor on platelet surface → activate
Gi pathway → inhibit adenylate cyclase (AC) →↓ATP
→↓cAMP → ↓PKA → ↓phosphorylation of VASP into
inactive form → ↑active VASP → ↑stimulation of GP
IIb/IIIa → ↑platelet plug stability
Adenylate cyclase
o responsible for the conversion of ATP into cyclic
AMP (cAMP); cAMP will then activate protein
kinase A (PKA) that will phosphorylate active
vasodilator stimulatory protein (VASP) into the
inactive VASP-P
VASP (active)
o stimulate GP IIb/IIIa → ↑platelet plug stability
Figure 1. Summary of Thrombus Formation and Mechanism of b. bind to P2Y12 receptor on platelet surface → activate
Action of Antiplatelet Medications Gq pathway → activate Phospholipase C (PLC) →
[Trevor, Katzung, & Kruidering-Hall, 2015, p. 281, Fig. 34-3] break down PIP2 into IP3 and DAG (see discussion on
Gq in TXA2)
anti-platelet medications CARDIOVASCULAR PHARMACOLOGY: Note #1. 1 of 4
Drugs that block ADP receptor Potency of drugs (Most potent to least potent)
● block P2Y12 receptor leading to inhibition of Gi and Gq Abciximab
pathways, ultimately leading to decreased platelet o only give to high-risk patients
aggregation and inhibition of GPIIb/IIIa o not commonly given since GPIIb/IIIa Inhibitors has the
● Thienopyridine Derivatives highest bleeding risk
o Converted in the liver to active metabolites that Prasugrel
irreversibly inhibit ADP receptor [Trevor, Katzung, & Kruidering- o black box warning for bleeding
Ticagrelor
Hall, 2015]
o Clopidogrel (Plavix) o commonly used
o Prasugrel (Effient) Clopidogrel
o Ticlopidine – not commonly used anymore due to o commonly used
adverse drug reactions (ADRs) o has risk of Thrombotic Thrombocytopenic Purpura
(TPP)
● Non-thienopyridine o some individuals may be poor metabolizers due to
o Does not require activation and reversibly inhibit ADP CYP2C19 mutation
receptor [Trevor, Katzung, & Kruidering-Hall, 2015] Aspirin
o Ticagrelor (Brilinta) o Least bleeding risk
(C) GPIIB/IIIA INHIBITORS Usual drug combos used in Percutaneous Coronary
● Inhibit GP IIb/IIIa interaction → ↓stability of platelet plug Intervention (PCI)
o Abciximab o Long-term/ Post-PCI: ASA + Clopidogrel
o Pre-PCI: ASA + Ticagrelor
o Tirofiban
o High-Risk Patients Pre-PCI: ASA + Abciximab
o Eptifibatide
(D) PHOSPHODIESTERASE-3 (PDE-3) INHIBITORS (B) CEREBROVASCULAR ACCIDENTS (CVA)
● Inhibit PDE-3 (enzyme that breaks down cAMP) ● Blood clots in brain, stroke
o ↓cAMP breakdown → ↑cAMP → ↑PKA → ● ASA + Clopidogrel (given 3-4.5 hours post-CVA)
↑phosphorylation of VASP →↓VASP active →
Important!
inhibition of GPIIb/IIIa During first 3-4.5 hours of CVA
o Cilostazol o give tPA (tissue plasminogen activator)
o Dipyridamole
(C) CAROTID ARTERY STENTING (PRE AND POST)
Other Mechanism and Use of PDE-3 Inhibitors
● Drug Combination: ASA + Clopidogrel
● cause smooth muscle relaxation → dilate blood vessel →
↑ blood flow (D) CORONARY ARTERY DISEASE PROPHYLAXIS
● Use: Peripheral Artery Disease
● ASA can prevent another MI or CVA
● Mechanism:
o Normal Physiology (E) GIANT CELL ARTERITIS
In smooth muscles, adenosine binds to its
● Inflammation of temporal arteries (vasculitis) increases
receptor and activate Gs → activates AC, which
risk of developing clots that can block the temporal artery
converts ATP to cAMP → activate PKA →
branches, such as ophthalmic artery and arteries that
phosphorylate myosin light chain kinase (MLCK)
supply muscles for mastication, leading to pain in
to its inactivated form MLCK-P → no smooth
temples, vision loss, or jaw claudication
muscle contraction
● Drug: ASA
o Cilostazol and Dipyridamole
inhibit PDE-3 → ↓ cAMP breakdown → ↑ cAMP → (F) PERIPHERAL ARTERY DISEASE (PAD)
↑PKA →↑phosphorylation of MLCK → inhibition of
● Plaques or clots in the vessels of the leg occlude blood
smooth muscle contraction → smooth muscle
flow to the surrounding muscles leading to development
relaxation → blood vessel dilation
of ulcers, gangrene, or claudication due to decreased
II) INDICATIONS oxygen supply
● Drug Combination: ASA + Cilostazol
(A) ACUTE CORONARY SYNDROME (ACS)
(G) PROPHYLAXIS OF COLORECTAL CANCER
● Thrombus or blockade in the myocardial blood vessels (LYNCH SYNDROME)
● Types of ACS
● ASA decrease risk of Colorectal cancer (especially Lynch
Unstable Angina
Syndrome)
Non-ST Elevated Myocardial Infarction (NSTEMI)
● Lynch Syndrome: tumors that form in different parts of
ST Elevated Myocardial Infarction (STEMI)
body (colorectal, endometrial, ovarian, renal, pancreatic)
Drug Combinations for ACS
(H) STRESS TEST
● ASA + Clopidogrel/ Prasugrel/ Ticagrelor/
● Assessment of myocardial perfusion in CAD is usually
*Abciximab (*only for high-risk patients)
done by exercise-induced stress test. If the patient
cannot exercise, Dipyridamole can be used.
High-risk patients ● Dipyridamole dilates myocardial vessels to see perfusion
o >75 y/o via imaging techniques. Dipyridamole increases blood
o Diabetic flow of normal vessels, but stenotic vessels are not
o ST segment deviations
dilated.
o ↑↑Troponin
o Left Ventricular Ejection Fraction (LVEF) <40% Important Dosage to Remember:
o Pulmonary Edema ASA
o ACS: 325mg ASA chewed then swallowed
o CAD Prophylaxis: 80mg ASA/ day
Clopidogrel
o Loading dose of 300 mg, then 75mg/day
2 of 4 CARDIOVASCULAR PHARMACOLOGY: Note #1. . anti-platelet medications
III) ADVERSE DRUG REACTIONS (ADRS) ● If Salicylates (i.e., ASA) are given to patient:
o Salicylates get metabolized by enzymes in the hepatic
(A) BLEEDING mitochondria, producing metabolites that inhibit β-
oxidation, leading to ↓Acetyl-CoA → ↓NADH and
Anterior Epistaxis – nosebleed
FADH2 → ↓ATP production
Gingival bleeding – bleeding in gums
Bleeding indications on skin ● Viral infections:
a. Petechiae – pinpoint hemorrhage on skin o Viruses increase metabolism of salicylates →
b. Purpura – larger pinpoint hemorrhaging ↑salicylate metabolites → ↑ inhibition of β-oxidation →
c. Ecchymosis – large bruising → → ↓ATP → ↓cell function → cell death
Hematemesis- vomiting blood ● Detoxification in Liver
Melena – upper GI bleed – dark or black feces o Amino Acids can be degraded in the liver, forming
Hematochezia – lower GI bleed – red stool ammonia (NH3) as a product.
Excessive Vaginal/Uterine Bleeding o NH3 is then metabolized and excreted via the Urea
cycle in the hepatic mitochondria.
Monitoring patients o If there is liver failure (i.e., due to giving salicylates
● Look for signs of bleeding (physical exam) during viral infections), the liver would not be able to
● CBC to check for anemia metabolize ammonia via the Urea cycle.
● Hemoccult to check for GI bleed ↑ NH3 in blood → NH3 into CNS → NH3 converts
glutamate into glutamine in the astrocytes →
(B) THROMBOTIC THROMBOCYTOPENIC PURPURA astrocytes become osmotically active → swelling
(TTP) → Encephalopathy
● Syndrome characterized by formation of small thrombi, Signs and Symptoms of Encephalopathy
platelet consumption and thrombocytopenia [Trevor, Katzung, & o Vomiting
Kruidering-Hall, 2015] o Fatigue
● Associated with Ticlopidine and Clopidogrel use o Seizures
o Coma
Mechanism: o Delirium
● Normal Physiology: VWF monomers fuse together
Reye Syndrome Triad
forming multimers. Multimers can be broken down again
into monomers via ADAMS T13 enzyme. ● <19y/o, febrile (possibly due to viral infection)
● Effect of Anti-platelets (i.e., Ticlopidine and Clopidogrel) ● Liver Damage (↑AST/ALT)
o ↓ ADAMS T13 level → ↑VWF multimers → platelets ● Signs of Encephalopathy
will stick to the multimers → ↑clots and ↓platelets
Remember:
(since they are consumed in the formation of clots) Aspirin increases the risk for Reye’s syndrome, so giving
Conditions or Medications that ↓ADAMS T13 ASA to <19y/o febrile patients is contraindicated.
o Antiplatelet medications (Ticlopidine, Clopidogrel)
o Lupus
o Chemotherapy (Gemcitabine, Cyclosporine) (B) THROMBOCYTOPENIA
Signs and Symptoms of TTP (“FAT-RN”) ● Low platelet count (<100,000)
● Fever (> 100.4 ⁰F) ● Contraindicated especially in GPIIb/IIIa inhibitors i.e.,
● Hemolytic Anemia due to breakdown of RBC Abciximab
o ↑LDH, ↑Bilirubin, ↓Haptoglobin (C) UNCONTROLLED BLOOD PRESSURE/
● Thrombocytopenia ↓platelets AORTIC DISSECTION
● Renal damage ● High BP can tear tunica intima of blood vessels → aortic
o Basic Metabolic Panel (BMP) ↑Creatinine, ↑BUN dissection → ↑ bleeding risk
● Neurological Damage
(D) BLEEDING
o Headache
o Confusion ● GI bleed, perforated peptic ulcer
● Subarachnoid hemorrhage
Treatment of TTP
(E) TRAUMA/ SURGERY
● Plasmapheresis: clean blood by removing different
substances V) REVIEW QUESTIONS
● Steroids to ↓inflammatory response
● Rituximab Which of the following is a GP IIb/IIIa inhibitor?
a. Clopidogrel
IV) CONTRAINDICATIONS b. Aspirin
c. Ticlopidine
(A) <19Y/O + FEVER d. Abciximab
RISK OF DEVELOPING REYE SYNDROME
● Never give ASA Which drug can be used in cardiac stress test?
Mechanism: a. Tirofiban
b. Dipyridamole
● Normal Physiology: c. Prasugrel
o Hepatic mitochondria break down free fatty acids into d. Eptifibatide
acetyl-CoA via β-oxidation. Acetyl-CoA goes into the
Krebs Cycle forming NADH and FADH2 that
stimulates the electron transport chain (ETC) to make What is the mechanism of action of Aspirin?
ATP. a. Inhibits PDE-3
b. Blocks P2Y12 receptor
c. Inhibits COX-1 and COX-2
d. Inhibit GP IIb/IIIa
anti-platelet medications CARDIOVASCULAR PHARMACOLOGY: Note #1. 3 of 4
What enzyme metabolizes Clopidogrel?
a. CYP2C19
b. ADAMS T13
c. PDE-3
d. Adenylyl cyclase
What is given to patients suffering from CVA during
the first 3 to 4.5 hours?
a. Aspirin
b. Clopidogrel
c. tPA
d. Ticlopidine
Which enzyme is responsible for the conversion of
ATP into cAMP?
a. Phospholipase C
b. Adenylate Cyclase
c. PDE-3
d. Protein Kinase A
Which drug is contraindicated in children with fever
since it increases the risk of developing Reye’s
syndrome?
a. Clopidogrel
b. Paracetamol
c. Aspirin
d. Tylenol
Which of the following is given only in high-risk ACS
patients?
a. Aspirin
b. Clopidogrel
c. Abciximab
d. Cilostazol
Loading dose of Clopidogrel
a. 325 mg
b. 300 mg
c. 80 mg
d. 75 mg
Which can be used for Peripheral Artery Disease?
a. Cilostazol
b. Abciximab
c. Tirofiban
d. Clopidogrel
CHECK YOUR ANSWERS
VI) REFERENCES
● Trevor, A., Katzung, B., & Kruidering-Hall, M. (2015). Katzung &
Trevor’s Pharmacology Examination & Board Review. McGraw Hill
Education
4 of 4 CARDIOVASCULAR PHARMACOLOGY: Note #1. . anti-platelet medications
You might also like
- httpsstatic1.squarespace.comstatic58e8b95bf5e231a18a2c2907t5a518d200d9297f9a5825cfb1515293993746Anticoagulants.pdfDocument10 pageshttpsstatic1.squarespace.comstatic58e8b95bf5e231a18a2c2907t5a518d200d9297f9a5825cfb1515293993746Anticoagulants.pdfNav ThiranNo ratings yet
- Blood Thinners: Maher Khdour Clinical Pharmacy, BSC, MSC, PHDDocument68 pagesBlood Thinners: Maher Khdour Clinical Pharmacy, BSC, MSC, PHDYousef JafarNo ratings yet
- Anticoagulants: BY: Saleema Allana MSCN, AkusonamDocument35 pagesAnticoagulants: BY: Saleema Allana MSCN, AkusonamDanial HassanNo ratings yet
- Vasodilation: Vasodilation Is The Widening of Blood VesselsDocument8 pagesVasodilation: Vasodilation Is The Widening of Blood VesselsNTA UGC-NETNo ratings yet
- AnticoagulantsDocument47 pagesAnticoagulantsTyler Lawrence Coye100% (1)
- Blood Pharmacology 27-34Document8 pagesBlood Pharmacology 27-34ahmedsalah565vvvNo ratings yet
- L P 4 Blood Pharmacology - Final-2022Document26 pagesL P 4 Blood Pharmacology - Final-2022Zakria Al-HadadNo ratings yet
- Anti-Platelet DrugsDocument10 pagesAnti-Platelet DrugsGoodone OneNo ratings yet
- Endo - PhysiologyDocument22 pagesEndo - PhysiologyTauseef AfridiNo ratings yet
- Anticoagulants affecting the cardiovascular systemDocument14 pagesAnticoagulants affecting the cardiovascular system백지원 (소네트리)No ratings yet
- Hemost. & Coag - PhysiologyDocument71 pagesHemost. & Coag - PhysiologyariniNo ratings yet
- Platelet Activation PathwayDocument15 pagesPlatelet Activation PathwayLe_redd21No ratings yet
- Ticlopidine (Ticlid™) and Clopidogrel (Plavix™)Document11 pagesTiclopidine (Ticlid™) and Clopidogrel (Plavix™)DhenokNo ratings yet
- Hematology - BNBDocument4 pagesHematology - BNBAndleeb ImranNo ratings yet
- Ticlopidine ClopidogrelDocument11 pagesTiclopidine ClopidogrelDhenokNo ratings yet
- Biochem SuperTable PDFDocument2 pagesBiochem SuperTable PDFPrincess MarielleNo ratings yet
- 9 Anti PlateletDocument15 pages9 Anti PlateletHely PatelNo ratings yet
- 3 - Vascular Endothelium IMBS 2023Document18 pages3 - Vascular Endothelium IMBS 2023Francisco HenriquezNo ratings yet
- Coagulation DrugsDocument1 pageCoagulation Drugsmed testNo ratings yet
- Table 4-2. Mechanism of Action of Selected Nonpeptide NeurotransmittersDocument1 pageTable 4-2. Mechanism of Action of Selected Nonpeptide NeurotransmittersaustinchenNo ratings yet
- Hematologi Pharmacolog: Hemostasis and Blood Coagulation CascadeDocument19 pagesHematologi Pharmacolog: Hemostasis and Blood Coagulation CascadeDivina ArenaNo ratings yet
- NIH Public Access: Platelet Aggregation PathwayDocument10 pagesNIH Public Access: Platelet Aggregation PathwaygabrimarteNo ratings yet
- Literature Review Anti Platelet, Anti Koagulan, Anti IskemikDocument53 pagesLiterature Review Anti Platelet, Anti Koagulan, Anti IskemikahrarsyamNo ratings yet
- Biochem SuperTableDocument2 pagesBiochem SuperTablePrincess MarielleNo ratings yet
- Regulation of Hemostasis MechanismsDocument55 pagesRegulation of Hemostasis MechanismsMJ PutraNo ratings yet
- Hema2 Lec Week-3Document7 pagesHema2 Lec Week-3Reyn CrisostomoNo ratings yet
- How Aspirin Works: Inhibiting Prostaglandin SynthesisDocument29 pagesHow Aspirin Works: Inhibiting Prostaglandin SynthesisNarasimha MurthyNo ratings yet
- Hemostatic Physiology: Regulation and MechanismsDocument65 pagesHemostatic Physiology: Regulation and MechanismsShibaNo ratings yet
- Jurnal Agregasi TrombositDocument21 pagesJurnal Agregasi Trombositnovi aprianiNo ratings yet
- Platelet Activation and Coagulation CascadeDocument9 pagesPlatelet Activation and Coagulation CascaderekanihlaNo ratings yet
- Pros Tag Land InsDocument16 pagesPros Tag Land InsTinaxNo ratings yet
- LMR - Biochemistry: CarbohydratesDocument6 pagesLMR - Biochemistry: CarbohydratesYuku BabyNo ratings yet
- Mekanisme Hemostasis & Koagulasi (Prof. Dr. Mansyur Arif, PH.D, SP - PK (K) )Document55 pagesMekanisme Hemostasis & Koagulasi (Prof. Dr. Mansyur Arif, PH.D, SP - PK (K) )ikram hanafiNo ratings yet
- Prostaglandins Synthesis and Inhibition by NSAIDsDocument29 pagesProstaglandins Synthesis and Inhibition by NSAIDsQamar QamarNo ratings yet
- Antiplatelet Pada ACSDocument22 pagesAntiplatelet Pada ACSRidyah Ning TyasNo ratings yet
- Obat Yang Mempengaruhi Pembekuan Darah: Dr.i Made Jawi, M.Kes Bagian Farmakologi FK UnudDocument42 pagesObat Yang Mempengaruhi Pembekuan Darah: Dr.i Made Jawi, M.Kes Bagian Farmakologi FK UnudChie ZhumieNo ratings yet
- 1.02 - Hemostasis, Surgical Bleeding and TransfusionsDocument11 pages1.02 - Hemostasis, Surgical Bleeding and TransfusionsPhilip Patrick LeeNo ratings yet
- Novel Aspects of Platelet Aggregation: Y. M. Roka-Moya, V. L. Bilous, D. D. Zhernossekov, T. V. GrinenkoDocument6 pagesNovel Aspects of Platelet Aggregation: Y. M. Roka-Moya, V. L. Bilous, D. D. Zhernossekov, T. V. GrinenkoАнна ШаповаловаNo ratings yet
- Eicosanoids & Their FunctionsDocument44 pagesEicosanoids & Their Functionsdevesh.hsNo ratings yet
- 13 HemostasisDocument38 pages13 HemostasissiratelNo ratings yet
- Carbohydrate Metabolism Week 2Document38 pagesCarbohydrate Metabolism Week 2shadaalnaas657No ratings yet
- 13 08045 Askandar 0840Document9 pages13 08045 Askandar 0840Fadhil Muhammad AwaluddinNo ratings yet
- 108 - Neurology Physiology) Adrenergic ReceptorsDocument9 pages108 - Neurology Physiology) Adrenergic ReceptorsvsugumaranNo ratings yet
- 347 - Hematology Physiology) Hemostasis Coagulation CascadeDocument6 pages347 - Hematology Physiology) Hemostasis Coagulation Cascadehasanatiya41No ratings yet
- Drugs in Blood DisordersDocument1 pageDrugs in Blood DisordersSantosh patelNo ratings yet
- Coagulation Disorders Disease 1° Bleeding Disorders Hemophilia A HemophiliaDocument2 pagesCoagulation Disorders Disease 1° Bleeding Disorders Hemophilia A HemophiliamcwnotesNo ratings yet
- Primary hemostatic plug components and their rolesDocument1 pagePrimary hemostatic plug components and their rolesC CNo ratings yet
- Glurs - Metabotropic Glutamate Receptors: Mglurs: L-Glutamine (Via Glutaminase) L-Glutamate (Mitochondrial)Document35 pagesGlurs - Metabotropic Glutamate Receptors: Mglurs: L-Glutamine (Via Glutaminase) L-Glutamate (Mitochondrial)jttodayNo ratings yet
- Acs - Sindroma Koroner Akut (Ska)Document55 pagesAcs - Sindroma Koroner Akut (Ska)Daniel VictorNo ratings yet
- AnticoagulantsDocument3 pagesAnticoagulantsDarNo ratings yet
- ReceptorsDocument9 pagesReceptorsAlexandra AlexaNo ratings yet
- Hematology: Coagulation, Platelets, and Clotting DisordersDocument78 pagesHematology: Coagulation, Platelets, and Clotting DisordersJaankiNo ratings yet
- Komplikasi DMDocument53 pagesKomplikasi DMpurwandinyNo ratings yet
- AspirinDocument11 pagesAspirinBindira MaharjanNo ratings yet
- BDS/MBBS Thrombolytics and Antiplatelet DrugsDocument33 pagesBDS/MBBS Thrombolytics and Antiplatelet DrugsDr.U.P.Rathnakar.MD.DIH.PGDHMNo ratings yet
- منار كمDocument61 pagesمنار كمFemale calmNo ratings yet
- NeurochemDocument17 pagesNeurochemJoseph WangNo ratings yet
- 9 - Anti-Platelet DrugsDocument12 pages9 - Anti-Platelet DrugsGoodone OneNo ratings yet
- Physiology for General Surgical Sciences Examination (GSSE)From EverandPhysiology for General Surgical Sciences Examination (GSSE)S. Ali MirjaliliNo ratings yet
- Warfarin's mechanism of action and indicationsDocument4 pagesWarfarin's mechanism of action and indicationsAmir mohammad moori MohammadiNo ratings yet
- Aortic Dissection AtfDocument8 pagesAortic Dissection AtfAmir mohammad moori MohammadiNo ratings yet
- Alpha Blockers Mechanism of Action AtfDocument5 pagesAlpha Blockers Mechanism of Action AtfAmir mohammad moori Mohammadi0% (1)
- Arrhythmias Types, Pathophysiology AtfDocument9 pagesArrhythmias Types, Pathophysiology AtfAmir mohammad moori MohammadiNo ratings yet
- ACE I & ARBs Mechanism of Action AtfDocument3 pagesACE I & ARBs Mechanism of Action AtfAmir mohammad moori MohammadiNo ratings yet
- Cerebrospinal Fluid - AUBFDocument9 pagesCerebrospinal Fluid - AUBFMitch IbayNo ratings yet
- Alkaloids and Its AdulterantsDocument1 pageAlkaloids and Its AdulterantsSAIDALAVI KMNo ratings yet
- Bio ChemistryDocument16 pagesBio ChemistryDamini MandhoryaNo ratings yet
- Psychology Paper 1 TZ1 HLSL MarkschemeDocument10 pagesPsychology Paper 1 TZ1 HLSL MarkschemeWanna One HatsuneNo ratings yet
- Unit 7 Urinary SystemDocument5 pagesUnit 7 Urinary SystemSiraj ShiferawNo ratings yet
- Carbohydrates Metabolism 3 Glycolysis ISUDocument25 pagesCarbohydrates Metabolism 3 Glycolysis ISUsjs6r8wwv9No ratings yet
- Module 11, Chapter 27:: University of Cebu-BaniladDocument10 pagesModule 11, Chapter 27:: University of Cebu-BaniladSuzanne Kyla CabuenasNo ratings yet
- Science: Modified Strategic Intervention MaterialsDocument24 pagesScience: Modified Strategic Intervention MaterialsRoxanne Manaloto100% (1)
- NATS-08 (NEET-2020 (Code-G5) )Document19 pagesNATS-08 (NEET-2020 (Code-G5) )gohilsumit5050No ratings yet
- Disorder of The Neuromuscular Junction: Courtesy . DR - Syeda Afsheen Hasnain DPT/MSPT NeuroloicalDocument16 pagesDisorder of The Neuromuscular Junction: Courtesy . DR - Syeda Afsheen Hasnain DPT/MSPT NeuroloicalCHANGEZ KHAN SARDAR100% (1)
- Prof. N. Syabbalo: MB., CHB., PHD., FCCP., FRS., Fiba Professor of Physiology & MedicineDocument50 pagesProf. N. Syabbalo: MB., CHB., PHD., FCCP., FRS., Fiba Professor of Physiology & MedicineHomeground entertainmentNo ratings yet
- Marma and Marma TherapyDocument14 pagesMarma and Marma TherapysunithaNo ratings yet
- Introduction to Biocatalysis and Classification of EnzymesDocument29 pagesIntroduction to Biocatalysis and Classification of EnzymesAudryan PradiptaNo ratings yet
- Ans 201 Anatomy and Physiology of Farm AnimalsDocument33 pagesAns 201 Anatomy and Physiology of Farm AnimalsAdewaleNo ratings yet
- ENGLISH Tìm từ sai-TOEFL- Bài số 1Document5 pagesENGLISH Tìm từ sai-TOEFL- Bài số 1iey ranaNo ratings yet
- Specific Objectives: Marjoriechiong001@deped - Gov.phDocument7 pagesSpecific Objectives: Marjoriechiong001@deped - Gov.phAnnejhel Mae PoralanNo ratings yet
- The Meaning of My GemstonesDocument10 pagesThe Meaning of My GemstonesAngelBaby38No ratings yet
- Immune System KriyasDocument6 pagesImmune System KriyasClaireNo ratings yet
- Understanding Sars-Cov-2-Induced Systemic Amyloidosis: BiorxivDocument4 pagesUnderstanding Sars-Cov-2-Induced Systemic Amyloidosis: BiorxivAntonisNo ratings yet
- Physiology RAASDocument3 pagesPhysiology RAASAulia Mahya FaradisaNo ratings yet
- 3 PracticalDocument47 pages3 PracticalT NNo ratings yet
- Jurnal UtamaDocument9 pagesJurnal UtamarekaNo ratings yet
- Zen Masters TherapyDocument14 pagesZen Masters Therapysayyoni johriNo ratings yet
- NSSCH Specimen Bio Apr2006Document54 pagesNSSCH Specimen Bio Apr2006AngelNo ratings yet
- Physiology Biochemistry Gen Surgery AnswersDocument7 pagesPhysiology Biochemistry Gen Surgery AnswersSanNo ratings yet
- Laboratory Activity No. 10: Frog Circulatory and Excretory SystemDocument5 pagesLaboratory Activity No. 10: Frog Circulatory and Excretory SystemMaricris GuillermoNo ratings yet
- Developmental Biology GametogenesisDocument14 pagesDevelopmental Biology Gametogenesispragyamaharjan2No ratings yet
- Mitigating Abiotic Stress: Microbiome Engineering For Improving Agricultural Production and Environmental SustainabilityDocument34 pagesMitigating Abiotic Stress: Microbiome Engineering For Improving Agricultural Production and Environmental SustainabilityNisrinaNo ratings yet
- Torehj 6 1 PDFDocument20 pagesTorehj 6 1 PDFSaifuddin HaswareNo ratings yet
- Organisation FTDocument18 pagesOrganisation FTjane byersNo ratings yet