Professional Documents
Culture Documents
PT31LEC - 5 Exercise and Physical Activity For Older Adults
Uploaded by
Althea DionaldoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PT31LEC - 5 Exercise and Physical Activity For Older Adults
Uploaded by
Althea DionaldoCopyright:
Available Formats
PT31 LEC - Geriatric PT EXERCISE AND PHYSICAL ACTIVITY FOR OLDER ADULTS
Exercise Role of Physical Activity (cont.)
- the single most efficacious intervention for older adults used - Accelerated Loss of Strength
by physical therapists - end result of inactivity
- known to simultaneously impact and mediate chronic disease, - Ultimate Goal of Exercise/Activity
many impairments, functional deficits, quality of life, and - to improve mobility and function and thereby decrease
cognition and prevent the negative sequelae associated with the patient’s mobility disability
sedentary lifestyles - Mobility/Disability
- an inability to walk one quarter of a mile and to climb a
Physical Activity flight of stairs
- any bodily movement that involves skeletal muscle - Study of Simonsick et al:
contraction and that substantially increases energy - 23% achieve the CDC’s physical activity
expenditure recommendations
- leisurely activity, requires little to no supervision, is of lower - 12% participate in strengthening exercises
intensity (3 to 6 METs) than exercise, and may be thought of
as usual activity The Slippery Slope of Aging
- 10,000 steps/day ○ Age-related Loss of Strength
○ CDC Recommendations for Older Adults: - one of the most critical factors contributing to mobility
- 150 minutes of moderate-intensity physical disability
activity/week ⬞ 10% per decade
- Strengthening exercise (2 or more days/week)(major - decrease in strength (30 y/o)
muscle groups) ⬞ 15% per decade
- decrease in strength (60 y/o)
Role of Physical Activity ○ Fun
○ CDC Physical Activity Guidelines for Older Adults - the physical ability to do whatever one wants,
⬞ Option 1 whenever one desires, for as long as desired
- 2 hours 30 minutes (150 minutes) of ○ Function
moderate-intensity aerobic activity every week - represents those who have to make choices about their
- muscle strengthening exercise on 2 or more days activities based on some decreased physical capacity
a week: all major muscle groups - represents those who are at risk for mobility
⬞ Option 2 disability or have some degree of mobility
- 1 hour 15 minutes (75 minutes) of disability
vigorous-intensity aerobic activity every week ○ Frail
- muscle strengthening exercise on 2 or more days - those who require help with IADLs and BADLs
a week: all major muscle groups ○ Failure
⬞ Option 3 - those who are completely dependent and often
- an equivalent mix of moderate- and bedbound
vigorous-intensity aerobic activity ⬞ 24% of baseline strength
- muscle strengthening exercise on 2 or more days - required for walking
a week: all major muscle groups ⬞ Leg strength
○ Common Chronic Health Conditions due to Physical Inactivity: - the single most important predictor of subsequent
⬞ Heart disease institutionalization, and it is more important than
⬞ Cancer: breast, colon, prostate, and pancreatic physiological markers or disease
⬞ Congestive heart disease
○ Criteria for Frailty as a Clinical Syndrome (Fried)
⬞ Depression
⬞ Hypertension
- Unintentional weight loss of 10 lb or more in the past
⬞ Cognitive disease year
⬞ Type 2 diabetes - Self-reported exhaustion
⬞ Obesity - Muscle weakness (grip strength in lowest 20%: <23 lb
⬞ Osteoporosis for women; <32 lb for men)
⬞ Peripheral vascular disease Physical frailty
- Walking speed in the lowest 20% (<0.8 m/sec)
⬞ Sleep apnea
⬞ Osteoarthritis
- Low level of activity (kcal/week–lowest 20%: 270
⬞ Stroke kcal/wk for women; 383 kcal/wk for men equivalent to
⬞ Balance problems and falls sitting quietly and/ or lying down for the vast majority
○ Physical Inactivity Increases the Risk of Disability in of the day)
Individuals with Various Chronic Health Conditions including: ⬞ frail if he or she meets 3 of these 5 frailty criteria
⬞ Chronic back pain ⬞ prefrail if he or she meets one or two of these frailty
⬞ Balance problems and falls criteria
⬞ Stroke
⬞ Arthritis
⬞ Frailty
⬞ Debilitating illness
⬞ Long-term chemotherapy
⬞ Total joint arthroplasties
⬞ Lower extremity fracture
⬞ Parkinson’s disease
PT31 LEC - Geriatric PT EXERCISE AND PHYSICAL ACTIVITY FOR OLDER ADULTS
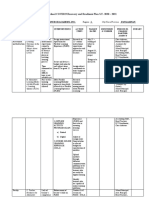
The Slippery Slope of Aging (cont.) Elements of an Exercise Prescription
○ Estimated Values for Functional Markers ○ Overload
⬞ critical parameter needed to extend the limits of
Fun Function Frail Failure
muscular performance
⬞ Intensity of exercise
Gait Speed >1.5m/sec 0.8-1.5m/sec 0.3-0.8m/sec <0.3m/sec
- needed to achieve high levels of function
Six-minute >500m 350-500m 200-350m <200m ⬞ 60% of the muscle’s maximum force
walk test - improve muscle force
⬞ Dose-response relationship
Chair rise 30 >15 reps 8-15 reps <8 reps unable - the greater the stimulus, the greater the
sec w/o hands
improvement
Stair climbing <10 sec 10-30 sec 30-50 sec unable
⬞ Intensity of 80% of a 1RM
10 stairs without rails with or with rails - to obtain optimal result
without rails ⬞ Assessment of Overload Stimulus
- determining the appropriate overload stimulus to
Floor transfer <10 sec 10-30 sec >30 sec with unable
without assist with or assist achieve an adaptive response requires knowledge
without assist of thresholds for adaptation for the aerobic and
muscular systems
- VO2 max
Strengthening Exercise
- 1 RM
○ Thomas DeLorme (strengthening)
- RPE
- progressive sets of each exercise based on a 10RM
- Modified scale of perceived exertion
○ ACSM (cardiac fitness and body composition)
- Talk test
○ Fiatarone (strengthening in older adults)
○ Specificity
- 80% of 1RM
- specificity is achieved by prescribing exercises that
○ Evans (strength training for older adults)
match the type of muscle contraction, the speed of
- high-intensity exercise
contraction, and consideration of the functional
movement inherent in the desired outcome
Physical Stress Theory
- functional strengthening
- foundation of exercise prescription
⬞ Overloading the patient’s gait
- the predictable response of tissues, organs, and systems to
- challenge their speed of walking
mechanical and physiological stressors
- ambulate on unlevel surfaces
- explains the effect of overload or insufficient load on tissues,
- incorporating head turns while walking
organs or systems, as well as the lack of change in tissues,
- carry a large object that blocks direct vision of the
organs, and systems if a “usual” stress is applied consistently
patient’s feet or have the patient move through an
○ The ability of tissue to absorb and dissipate forces is
obstacle course
dependent on many variables:
⬞ Functional Movement
⬞ time over which the stressor is applied
○ Bed mobility
⬞ direction, magnitude, and combination of stressors
⬝ Key Muscles
applied
- abdominals
⬞ physiological condition of the tissue, organ, or system
- erector spinae
⬞ frequency of the application of a stressor and length of
- gluteus maximus
time between the applications
⬝ Exercises
⬞ psychological state of the person and the “environment”
- Bridge progression
in which the stressor is applied
- Sit backs
- Plank (modified and full)
Physical Stress Theory
- Prone hip extension (single and
Too much stress (>100% of maximum) Injury or tissue death double)
- Side plank (regular and modified)
Appropriate (60% to 100% of Strengthening ○ Transfers and squats
overload maximum) ⬝ Key Muscles
- gluteus maximus, medius
Usual stress (40% to 60% of maximum) No change in tissue - obturator externus
- piriformis
Too little stress (<40% of maximum) Atrophy - quadriceps
⬝ Exercises
No stress (0% of maximum) Loss of ability to adapt (death) - sit to stand
- squats with knees abducted and hips
externally rotated
- leg press, wall slides
PT31 LEC - Geriatric PT EXERCISE AND PHYSICAL ACTIVITY FOR OLDER ADULTS
Elements of an Exercise Prescription ○ Functional Training (cont.)
○ Specificity - can be used for balance and strengthening
⬞ Functional Movement (cont.) - can be incorporated into gait training
○ Ambulation and stair climbing ⬞ Speed and Power
⬝ Key Muscles ⬝ Power
- abdominals - time rate of force development
- ES - loss of speed and power is associated with frailty,
- Gmax and Gmed falls, and slow gait speed; slow gait speed is
- Ob Ext predictive of loss of ADL ability and future
- piriformis institutionalization
- quads ⬝ Slowness of movements and gait occurs with
- TA aging:
- gastroc-soleus - loss of type II or fast-twitch muscle fibers
⬝ Exercises ○ Types of Contractions
- Bridge progression ○ Motor Learning
- Sit backs ○ Frequency
- Plank (modified and full) - number of exercise sessions per week that are
- Prone hip extension (single and necessary or advisable to obtain optimum results
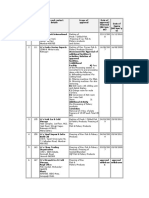
double) Recommended Frequency for Types of Exercise
- Step ups (varied heights)
Activity Frequency
○ Floor transfers
⬝ Key Muscles
- abdominals Aerobic (cardiovascular 3–5 times per week
- ES conditioning) With higher intensity, frequency
- Gmax and Gmed can be decreased
- Ob Ext
- piriformis Skills (motor learning) Daily
- quads and balance
- gastroc-soleus
⬝ Exercises Stretching 5–7 times per week
- kneeling with trunk rotations
- extension Strengthening 2–3 times per week for each
- UE movements muscle group
- quadruped trunk rotations and hip
extensions
○ Fast gait and jumping ○ Sets
⬝ Key Muscles - one set of each exercise are effective for the first 3
- Gastroc-soleus months of training, in untrained and novice weight
- Gmax and Gmed lifters, and in older adults
- quads ○ Duration
⬝ Exercises - amount of time of each exercise bout or the length of
- skipping time of an exercise session
- fast foot placement on target - skill and balance activities are practiced 20 to 30
- hopping minutes per session
- fast walking and jogging for short - aerobic exercise durations are 30 minutes, with short
distances periods of 5 to 10 minutes of warm-up and cool-down
○ Functional Training ⬞ Stretching exercise:
- overloading the movement or activity of interest to - 30 seconds in younger people
challenge the whole neuromuscular system rather than - four repetitions of 60 seconds in older adults
simply challenging a muscle ⬞ Strengthening exercise:
- muscular and articular systems - 10RM
- proprioceptive and cutaneous sensory systems
- vestibular and visual systems
⬞ Progression of a functional exercise program is
obtained by moving from:
⬝ simple movements to more complex movements
⬝ normal speed to either quicker or slower
movements
⬝ stable surfaces to unstable or compliant surfaces
⬝ eyes open to eyes closed
⬝ an emphasis on form to an emphasis on intensity
and the working over from base of support to
working outside the base of support
PT31 LEC - Geriatric PT EXERCISE AND PHYSICAL ACTIVITY FOR OLDER ADULTS
Types of Exercises for Older Adults ○ Strengthening Exercise
○ Aerobic Exercise ⬞ Measurement
⬞ Measurement ⬞ MMT
⬞ Target HR ⬞ Muscle dynamometry
⬞ RPE: subjective measure of exercise intensity ⬞ Isokinetic dynamometers
⬞ Clinical Functional Measures of Aerobic Capacity ⬞ RM test
⬞ 6MWT ⬞ 60% of 1RM
⬞ 400-m walk test - minimum training stimulus for strengthening
⬞ 60%-80% exercise stimulus: to achieve CV exercise
adaptation and fitness ⬞ Leg Press
⬞ Measurement - body weight
- THR = 60% to 80% X [220 - age] ⬞ Indications for Strengthening Exercise
- Karvonen method of THR = ⬞ insidious loss of strength with age
([60% to 80% x (220 - age - resting HR)] + resting HR) ⬞ to add reserve to provide a protective effect in the
⬞ Measurement event that the person has a period of enforced
⬞ Subjective Measures of Perceived Exertion bed rest
- RPE: tool to monitor exercise intensity has ⬞ SLOWNESS OF MOVEMENT: hallmark of frailty
been validated in older adults, and is (strength and power training)
particularly useful in those who may have a ⬞ Contraindications and Safety for Strengthening Exercise
blunted heart rate response, such as those ⬞ use proper form and avoid holding breath
taking b-blockers
⬞ Exercise Stress Test ○ Stretching Exercise
- gold standard for determining readiness to - stretching is indicated to promote adaptation of
exercise shortened muscles to a more lengthened position to
⬞ 6MWT achieve better posture and movement patterns
- useful objective baseline measure and has ⬞ 30-second hold - younger adult
normative results and minimal clinically ⬞ 60 seconds hold - adults age 65 years or older
important differences established for a range ⬞ four repetitions of a 60-second hold performed
of older individuals regularly, 5 to 7 days a week
⬞ Measurement ⬞ slow static stretching
⬞ 400-m Walk Test ⬞ Measurement
⬞ Indications for Aerobic Exercise ⬞ ROM
- indicated for patients who lack the ability to ⬞ Functional ranges
sustain activity for a desired period of time ⬞ Indications for Stretching Exercise
because of decreased cardiovascular efficiency ⬞ pain syndromes, painful postures, abnormal
⬞ Contraindications and Safety for Aerobic Exercise movement patterns, and loss of function
⬞ resting heart rate greater than 100 bpm ⬞ future painful conditions and loss of function
⬞ systolic blood pressure higher than 200 mmHg ⬞ Typical muscles requiring stretching in older
⬞ diastolic blood pressure higher than 120 mmHg adults:
⬝ Suboccipital muscles
○ Aquatic Exercise ⬝ Pectoralis minor and downward rotators
- the buoyancy of the water allows a deconditioned and protractors of the shoulder girdle
individual or an individual with significant joint ⬝ Extensors of the lumbar spine
pathology to exercise by decreasing the forces needed ⬝ Hip flexors and external rotators
to move and decreasing the forces on the joint ⬝ Ankle plantar flexors
⬞ Indications for Aquatic Exercise ⬞ Contraindications and Safety for Stretching Exercise
⬞ patients who have painful joints in weight bearing ⬞ presence of joint instability
to exercise
⬞ patients who have osteoarthritis, who are ○ Plyometrics
overweight, or who have recently undergone - plyometric exercise is an attempt to use the stretch re-
surgery may initially benefit from this form of flex of the muscle spindle and the elastic energy that is
exercise stored in a stretched muscle to enhance an immediate
⬞ patients who have significant balance disorders or reciprocal contraction in that muscle
a fear of falling - eccentric and concentric
⬞ Contraindications and Safety for Aquatic Exercise ⬞ Measurement
⬞ same with aerobic exercise - Isokinetic dynamometer
⬞ individual with open wounds - Functional testing
- Rose’s Fullerton balance test
⬞ Indications for Plyometrics
- Loss of power
- Decreasing fall risk
- Increasing UE power
PT31 LEC - Geriatric PT EXERCISE AND PHYSICAL ACTIVITY FOR OLDER ADULTS
○ Tai Chi
- fall risk benefits
- involves learning multiple poses that are linked
together with slow movements that emphasize control
and balance.
- the focus required to complete the movements and
postures and recalling the sequence of postures has
been credited with both the mental calm and the
cognitive benefits associated with Tai Chi
⬞ Indications for Tai Chi
⬞ mediates the effects of chronic conditions such as
arthritis, cancer, CVD, and DM
⬞ decreases stress
⬞ lessens depression
⬞ improves mental health and cognitive function
while improving balance and fitness
⬞ decreasing falls and lessening fall risks
You might also like
- ESC-GASTPE School COVID19 Recovery and Readiness Plan S.Y. 2020 - 2021Document5 pagesESC-GASTPE School COVID19 Recovery and Readiness Plan S.Y. 2020 - 2021Jubylyn Aficial100% (3)
- Geriatrics Eval Management Tool For FrailtyDocument2 pagesGeriatrics Eval Management Tool For FrailtyDaulat JosuaNo ratings yet
- Benefits of Exercise and Physical Activity: Why Workout? Why Exercise? Why Be Physically Active?Document5 pagesBenefits of Exercise and Physical Activity: Why Workout? Why Exercise? Why Be Physically Active?Justine MainNo ratings yet
- Pathfit02 Prelims ReviewerDocument3 pagesPathfit02 Prelims ReviewerowenbacatancorporalNo ratings yet
- Peh 12 1ST Sem-1st Quarter ReviewerDocument15 pagesPeh 12 1ST Sem-1st Quarter ReviewerRalph Louis RosarioNo ratings yet
- Be Active 2008-Factsheet ProfessionalsDocument2 pagesBe Active 2008-Factsheet ProfessionalsLaurencia LenyNo ratings yet
- Fitness - Physical ActivityDocument22 pagesFitness - Physical ActivityZizo AboshadiNo ratings yet
- Articulo Salud PublicaDocument18 pagesArticulo Salud PublicaCatherinne Quiñonez GutierrezNo ratings yet
- PATHFITT 2 - HandoutsDocument14 pagesPATHFITT 2 - HandoutsDona Caballejo- ArcenaNo ratings yet
- Exercise Prescription For Healthy Populations With Special Considerations FormattedDocument49 pagesExercise Prescription For Healthy Populations With Special Considerations Formattedashlyn granthamNo ratings yet
- Exercise Prescription in Primary Care SettingDocument34 pagesExercise Prescription in Primary Care Settingdr.gunturadwiNo ratings yet
- OKK 2 - Leo - Yunia - Exercise To Increase The Components of Physical FitnessDocument43 pagesOKK 2 - Leo - Yunia - Exercise To Increase The Components of Physical FitnessAna NurfaizahNo ratings yet
- Fitness Exercise Fitt 2Document16 pagesFitness Exercise Fitt 2darillpabilando09No ratings yet
- FITTDocument7 pagesFITTAllona VillarinNo ratings yet
- Answer Yes or No: Pre-TestDocument7 pagesAnswer Yes or No: Pre-TestNabi BratzchNo ratings yet
- Lifestyle and Weight ManagementDocument2 pagesLifestyle and Weight ManagementcashieentanNo ratings yet
- MBR 2019 - Rehab Med HandoutsDocument4 pagesMBR 2019 - Rehab Med HandoutsRgm UyNo ratings yet
- Class Presentation - Effects of Exercise On Physiologic AgingDocument26 pagesClass Presentation - Effects of Exercise On Physiologic AgingTruman ChiuNo ratings yet
- PEH1Document8 pagesPEH1Jana De LiñaNo ratings yet
- Functional Exercise To Improve Fitness Balance & AgilityDocument70 pagesFunctional Exercise To Improve Fitness Balance & Agilityhadyahmed0318No ratings yet
- Aktivitas Fisik Pada Dewasa Dan GeriatriDocument20 pagesAktivitas Fisik Pada Dewasa Dan GeriatriAdinda Suci MaghfiraNo ratings yet
- Presented By: DR - Shilpa K PrajapatiDocument46 pagesPresented By: DR - Shilpa K PrajapatijothiNo ratings yet
- Wollo University College of Natural & Computational Science Course Name Health and Physical Fitness Abebaw W. (MSC in S. Medicine) Feb.2021Document68 pagesWollo University College of Natural & Computational Science Course Name Health and Physical Fitness Abebaw W. (MSC in S. Medicine) Feb.2021abebawNo ratings yet
- Exercise For Fitness: (Shs-Videolecture-1 & 2 Week)Document18 pagesExercise For Fitness: (Shs-Videolecture-1 & 2 Week)Mark Joshua MandaniNo ratings yet
- Weebly Questions Week NineDocument4 pagesWeebly Questions Week Nineapi-459697337No ratings yet
- PE 02 Chapter-1Document9 pagesPE 02 Chapter-1Milk BrotherNo ratings yet
- Hubs2503 Lecture NotesDocument150 pagesHubs2503 Lecture NotesSruthi SruthiNo ratings yet
- Day 3 Principles of Rehabilitation in Elderly The NewestDocument43 pagesDay 3 Principles of Rehabilitation in Elderly The NewestaniendyawijayaNo ratings yet
- GRADE 11 PE Chapter 1 DoneDocument30 pagesGRADE 11 PE Chapter 1 DoneBananaNo ratings yet
- PA in Stroke - Chutima Aug1,2020Document25 pagesPA in Stroke - Chutima Aug1,2020ridaimroNo ratings yet
- An Introduction To Physical Activity: Study Guide For Module No. 2Document6 pagesAn Introduction To Physical Activity: Study Guide For Module No. 2MC BlancoNo ratings yet
- DISABILITYDocument8 pagesDISABILITYahmedNo ratings yet
- Fitness Training: Danish LatifDocument26 pagesFitness Training: Danish LatifShimmering MoonNo ratings yet
- Promoting Physical Activity To PatientsDocument7 pagesPromoting Physical Activity To PatientsAlexander OchoaNo ratings yet
- Presentation 2Document16 pagesPresentation 2Mohammad Ajmal MadniNo ratings yet
- Week 1 Slides Aug 31 Final StudentsDocument39 pagesWeek 1 Slides Aug 31 Final StudentsMaude GohierNo ratings yet
- Fisiologi SenamDocument4 pagesFisiologi SenamFatin FatinNo ratings yet
- Lifestyle, Fitness and WellnessDocument275 pagesLifestyle, Fitness and WellnessCaldwellNo ratings yet
- Exercise Prescription: Exercise Recommenda2ons For Persons With Special NeedsDocument29 pagesExercise Prescription: Exercise Recommenda2ons For Persons With Special NeedsThe Health Therapist AcademyNo ratings yet
- Hope 1Document4 pagesHope 1Sea are YellowNo ratings yet
- TE Chapter 1Document45 pagesTE Chapter 1tooba khanNo ratings yet
- Pathfi Module 1: Movement: C. Manipulative SkillsDocument4 pagesPathfi Module 1: Movement: C. Manipulative SkillsAndrea Gail UlitinNo ratings yet
- PE ReviewerDocument2 pagesPE ReviewerGeorgette Princess Yvonne R. GatdulaNo ratings yet
- The Benefits of ExerciseDocument3 pagesThe Benefits of ExerciseAtet KurniadiNo ratings yet
- Nutrition and Exercise Physiology 1st-1Document23 pagesNutrition and Exercise Physiology 1st-1Dawat E Islam.No ratings yet
- 10-Lecture 13 - HAN - Physical Fitness and HealthDocument24 pages10-Lecture 13 - HAN - Physical Fitness and HealthSuleiman AbdallahNo ratings yet
- WardDocument41 pagesWardSuman DeyNo ratings yet
- Fitness Tests Management For Sustainable HealthDocument5 pagesFitness Tests Management For Sustainable HealthkyleNo ratings yet
- Ronai 2013 Inespecific Low Back PainDocument4 pagesRonai 2013 Inespecific Low Back PainivanNo ratings yet
- Care of Older Adult Finals IlgDocument77 pagesCare of Older Adult Finals IlgMiden AlbanoNo ratings yet
- WELLNESSDocument2 pagesWELLNESScessyriveracruzNo ratings yet
- 2008 Physical Activity Guidelines: National Council On Strength & FitnessDocument2 pages2008 Physical Activity Guidelines: National Council On Strength & FitnessPaulo ZulluNo ratings yet
- Ch01.Intro To Phys Fit WellDocument24 pagesCh01.Intro To Phys Fit WellDREAM UPNo ratings yet
- Movement Enhancement 1: Module 7: Moderate and Vigorous Physical ActivitiesDocument8 pagesMovement Enhancement 1: Module 7: Moderate and Vigorous Physical ActivitiesMarjorie PolinarNo ratings yet
- Female Athlete TriadDocument29 pagesFemale Athlete TriadShimmering MoonNo ratings yet
- Exercise Testing and Prescription in Older AdultsDocument19 pagesExercise Testing and Prescription in Older Adultspushplata.19770No ratings yet
- Pe Lecture NotesDocument7 pagesPe Lecture NotesAnonymous LJrX4dzNo ratings yet
- The Benefits of Physical Activity UploadDocument17 pagesThe Benefits of Physical Activity UploadDorart IsmajliNo ratings yet
- Exercise and Cardiovascular HealthDocument2 pagesExercise and Cardiovascular HealthsynysterbraveNo ratings yet
- Exercise Prescription Certificate Course: Exercise Recommenda2ons For Persons With Special NeedsDocument59 pagesExercise Prescription Certificate Course: Exercise Recommenda2ons For Persons With Special NeedsThe Health Therapist AcademyNo ratings yet
- Dry Lab Exercise 4 EndocrineDocument4 pagesDry Lab Exercise 4 Endocrine06Fajrian RidhatunnisaNo ratings yet
- AAAAA - Family Developmental TaskDocument2 pagesAAAAA - Family Developmental TaskMaevan BacolNo ratings yet
- EU Approved Units EIA - MaharashtraDocument7 pagesEU Approved Units EIA - MaharashtragibinkumarNo ratings yet
- Container Data UtilizationDocument2,910 pagesContainer Data UtilizationCege Wa NjorogeNo ratings yet
- AVTC 5 - 09 - Group 3 - Business PlanDocument9 pagesAVTC 5 - 09 - Group 3 - Business Planda zelNo ratings yet
- TFN Reviewer PrelimsDocument8 pagesTFN Reviewer PrelimsCUBILLAS, JASMIN G.No ratings yet
- Alumunium Chlorohydrate: Material Safety Data SheetDocument4 pagesAlumunium Chlorohydrate: Material Safety Data Sheethinur awaNo ratings yet
- Mine? ? ??Document16 pagesMine? ? ??Samskruthi ChallaNo ratings yet
- QuestionDocument5 pagesQuestionJavy mae masbateNo ratings yet
- 4 Van Der Linden Et Al. (2020) Inoculating Against Fake NewsDocument7 pages4 Van Der Linden Et Al. (2020) Inoculating Against Fake Newsegenaz tunçdemirNo ratings yet
- Pe9 - q1 - Mod1 - Physical Activity and Physical Fitness Assessments - v3Document11 pagesPe9 - q1 - Mod1 - Physical Activity and Physical Fitness Assessments - v3JaysonMananquilLabsanNo ratings yet
- Benzofurano-Isatins: Search For Antimicrobial Agents: Arabian Journal of ChemistryDocument8 pagesBenzofurano-Isatins: Search For Antimicrobial Agents: Arabian Journal of Chemistrylucian_lovNo ratings yet
- Meaning of Self-Esteem: by Dr. Ranjit Singh MalhiDocument2 pagesMeaning of Self-Esteem: by Dr. Ranjit Singh Malhieva pandanaNo ratings yet
- Boys Simplified Field Tables Weight For Length 2 To 5 Years (Percentiles)Document4 pagesBoys Simplified Field Tables Weight For Length 2 To 5 Years (Percentiles)Gabrielly LopesNo ratings yet
- CMR 00062-17Document78 pagesCMR 00062-17pokhara144No ratings yet
- Material Safety Data Sheet Avades 100Document4 pagesMaterial Safety Data Sheet Avades 100fs1640No ratings yet
- Tatalaksana Oftalmia Neonatorum Ec Infeksi Gonokokal Dengan Ikterik Neonatorum - Viora Rianda PiscalokaDocument12 pagesTatalaksana Oftalmia Neonatorum Ec Infeksi Gonokokal Dengan Ikterik Neonatorum - Viora Rianda Piscalokasupaidi97No ratings yet
- List of Empanelled Hospitals & Diagnostic Centres DGEHSDocument33 pagesList of Empanelled Hospitals & Diagnostic Centres DGEHSaaryan0% (2)
- ABI Worksheet: Patient Name: Patient ID: DateDocument2 pagesABI Worksheet: Patient Name: Patient ID: Datezaqqi ubaidillahNo ratings yet
- Print Boarding PassDocument2 pagesPrint Boarding PassAshu SinghNo ratings yet
- Các Thì C A Đ NG TDocument3 pagesCác Thì C A Đ NG TThanh TuyếtNo ratings yet
- Cumulative Adversity As A Correlate of Posttraumatic GrowthDocument20 pagesCumulative Adversity As A Correlate of Posttraumatic GrowthLorena RodríguezNo ratings yet
- E-Cigarette Wholesale Distributor in USA - Vape Supplier in USADocument10 pagesE-Cigarette Wholesale Distributor in USA - Vape Supplier in USAAnjum JohnNo ratings yet
- Ca1 PrelimDocument60 pagesCa1 PrelimAira EspleguiraNo ratings yet
- TESTS DISEASES OF BLOOD AND ENDOCRINE SYSTEM Methodical Manual For The 5 Year PDFDocument152 pagesTESTS DISEASES OF BLOOD AND ENDOCRINE SYSTEM Methodical Manual For The 5 Year PDFMayur WakchaureNo ratings yet
- Citizens Civil Complaint Against Pittsfield, Cell TowerDocument65 pagesCitizens Civil Complaint Against Pittsfield, Cell ToweriBerkshires.comNo ratings yet
- Common Errors in Dental RadiographyDocument48 pagesCommon Errors in Dental RadiographyDarwin D. J. LimNo ratings yet
- Administering Intradermal InjectionDocument17 pagesAdministering Intradermal InjectionPattNo ratings yet
- Green Gradient Monotone Minimalist Presentation TemplateDocument20 pagesGreen Gradient Monotone Minimalist Presentation TemplateJo-ann AguirreNo ratings yet