Professional Documents
Culture Documents
Weight Stigma in Children and Adolescents
Uploaded by
Victoria VDOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Weight Stigma in Children and Adolescents
Uploaded by
Victoria VDCopyright:
Available Formats
2.
0
ANCC CONTACT HOURS
RAIHANA ASRAL /SHUTTERSTOCK
Weight stigma in children
and adolescents:
Recommendations for practice and policy
BY KARYN J. ROBERTS, PhD, RN, CHSE, AND MICHELE L. POLFUSS, PhD, RN, CPNP-AC/PC
Abstract: Weight stigma is the devaluation Obesity in children and adolescents ics.2 The oversimplistic assumption
of a person because of excess body weight. is the most prevalent chronic con- that obesity is a choice and can be
Individuals who experience stigmatization dition in the US. Over 19% of chil- “fixed” by moving more and eating
are at increased risk for adverse physical dren ages 2-19 years have obesity, less is outdated and inaccurate in
and psychological health outcomes. This which is defined as a body mass the current science of obesity.3 Over
article provides an overview of weight stig-
index (BMI) greater than or equal the last 20 years, researchers have
ma and the implications for nursing practice
to the 95th percentile on the CDC begun to shed light on the multifac-
and policy.
growth chart.1 Obesity is a complex eted complexity of obesity. Physi-
Keywords: obesity, pediatric health, weight physiologic condition influenced by ologically, adolescents with obesity
stigma genetics, hormones, sleep, environ- have an increased risk of develop-
ment, cultural norms, and econom- ing adverse health outcomes such
www.Nursing2022.com June l Nursing2022 l 17
Copyright © 2022 Wolters Kluwer Health, Inc. All rights reserved.
NSG0622_NCPD_WeightStigma_Ramakant.indd 17 29/04/22 3:27 PM
Noting the high prevalence of obe-
Key terms in weight stigma7 sity in children and adolescents, rec-
ognizing and reducing internalized
Weight-based stereotypes: Generalizations that persons with overweight or weight stigma must be prioritized in
obesity are lazy, gluttonous, and incompetent; lack will power and self-discipline; healthcare.
are unmotivated to improve their health and noncompliant with medical treatment;
and are solely to blame for their weight.
Manifestations of stigma
Explicit weight bias: Overt, consciously held negative attitudes that can be Weight stigma is manifested in
measured by self-report. various ways. The most com-
Weight stigma: The social devaluation and denigration of a person because of mon expressions of weight stigma
their excess body weight. Can lead to negative attitudes, stereotypes, prejudice, and in children and adolescents are
discrimination. weight-based teasing, bullying, and
Weight discrimination: Overt forms of weight-based prejudice and unfair treat- victimization. Weight-based teasing
ment toward persons with obesity, such as being denied employment. involves name-calling, derogatory
Implicit weight bias: Automatic, negative attributions and stereotypes existing remarks, or being made the object
outside of the conscious awareness of an individual. of ridicule.16 Weight-based bullying
can also involve physical actions
of hitting, kicking, pushing, or
as type 2 diabetes, hypertension, inaccurate assumptions are preva- shoving.16 Children and adoles-
elevated serum cholesterol and lent in the United States and held cents with overweight and obesity
triglyceride levels, respiratory dis- by individuals, healthcare provid- are more likely to be bullied than
orders such as asthma, and joint ers, educators, parents, media, and their peers with healthy weight,
problems.4 Psychologically, they policymakers.8,9 Weight stigma and and these experiences can begin at
have been shown to have increased its manifestations have been used to very young ages.16 Weight-based
rates of anxiety, depression, low shame and “motivate” people with victimization includes social exclu-
self-esteem, body image dissatisfac- obesity to “comply” with recommen- sion, being ignored, avoided, or
tion, and decreased quality of life.5,6 dations.10 made the target of rumors.17 It may
Additionally, youth with obesity Weight stigmatization is prevalent be clear to see how these explicit
are at increased risk of experienc- in children and adolescents regard- forms of weight bias and stigma
ing weight bias and stigma, which less of their socioeconomic and are harmful; however, implicit bias
often exacerbate and perpetuate the demographic characteristics. Adoles- may be just as harmful. Implicit
cycle of adverse physiologic and cents, regardless of gender, are more bias among parents, educators,
psychological consequences.7 By likely to be bullied for their weight and healthcare providers has been
understanding the pervasiveness or physical appearance than for their shown to impact the perceptions
of weight stigma and its negative race, ethnicity, disability status, or of children and adolescents con-
consequences, nurses must lead the sexual orientation.11 Recent estimates cerning their physical, social, and
prevention and cessation of weight report nearly 25%-50% of youth academic abilities.18-21 Over time,
stigma. This article discusses weight have been bullied for their weight, such implicit bias may contribute
stigma and its implications for clin- and 13%-32% report they have been to adverse health outcomes in this
ical practice and healthcare policy. discriminated against based on their population.18-21
weight.5,11-13 Youth who experience weight
Key terms and definitions Weight stigma contributes to the stigma may internalize these expe-
Weight stigma is the social devalua- current obesity epidemic because riences. This could result in weight
tion and denigration of a person be- individuals who experience stigma- bias internalization wherein one
cause of excess body weight.7 Weight tization such as weight-based teas- directs stigma and negative ste-
stigma can lead to negative attitudes, ing, bullying, and victimization have reotypes at oneself due to weight-
stereotypes, prejudice, discrimi- increased risks for adverse health biased beliefs and attitudes.14
nation, and includes explicit and outcomes. Individuals may internal- Studies have shown that children
implicit weight bias (see Key terms ize stigmatization, decreasing their with overweight and obesity who
in weight stigma). Weight stigma per- overall quality of life.14,15 Public have experienced teasing by peers
petuates the view that obesity is the health policy aimed at reducing and or who have lower self-esteem
fault of the individual due to poor preventing weight stigma may aid in have higher weight bias internal-
diet and exercise patterns.7 These improving global obesity rates. ization.22
18 l Nursing2022 l Volume 52, Number 6 www.Nursing2022.com
Copyright © 2022 Wolters Kluwer Health, Inc. All rights reserved.
NSG0622_NCPD_WeightStigma_Ramakant.indd 18 29/04/22 3:27 PM
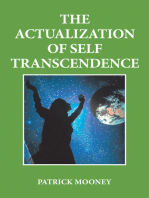
Negative feedback loop in pediatric obesity
Pediatric Obesity
Weight Stigmatization
Decreased
• Teasing
Physical Activity
NEGATIVE • Bullying
• Victimization
FEEDBACK
LOOP
Physiological Stress
Eating Behaviors Psychosocial Problems
• Increased risk of • Depression
eating disorders • Low self-esteem
• Increased caloric intake • Social isolation
• Impaired academic performance
Source and attributions: Modified from Haqq, et al.18; Icons made by www.freepik.com from https://www.flaticon.com/. Icons made by www.flaticon.com/authors/
smashicons and altered by College of Nursing UWM.
Physical consequences of Decreased physical activity ing to cope with stress, and restricted
weight stigma Perceived weight discrimination has eating.13,31,32 These disordered eating
Physiologic stress, weight gain been associated with higher odds of behaviors may be overlooked due
The mechanism resulting from being inactive in adults.27 In persons to the assumption that children and
experiences of weight stigma is a seeking treatment for weight man- adolescents with obesity cannot expe-
negative emotional stressor that agement, those with higher levels of rience consequences of restricted eat-
initiates a cascade of behavioral, weight stigma were more likely to ing patterns or binging and purging.
emotional, and physiologic re- avoid exercise and be less physically Furthermore, individuals who experi-
sponses.23 Though evidence is lim- active.28 Less is known about the ence weight stigma have demonstrated
ited in how experiences of weight impact of weight stigma on physical increased use of emotional eating and
stigma impact the body’s response activity in children and adolescents. higher caloric consumption overall.33
to stress in children and adoles- However, researchers have reported
cents, adult population research decreased physical activity, physical Psychosocial problems
has demonstrated physiologic fitness, and exercise efficacy in chil- Weight stigma has several short- and
consequences of weight stigma in- dren and adolescents experiencing long-term effects on children and ado-
cluding higher circulating levels of weight stigma.29,30 lescents. Children and adolescents who
inflammatory markers (C-reactive experience weight stigma have been
protein) and cortisol.23-26 Cortisol Psychological consequences shown to have increased anxiety and
is a stress hormone, which when of weight stigma depression, decreased self-esteem, in-
elevated, drives hunger urges, Unhealthy eating patterns creased rates of suicidal thoughts, and
stress-induced eating, and causes Weight-based teasing, regardless reports of loneliness.34 Other research
weight gain.23 Pearl et al.14 report- of the source, has been associated has described how blame, weight bias
ed weight bias internalization as a with unhealthy weight management internalization, and strained family
risk factor for metabolic syndrome, behaviors. Youth who internalize relationships add to these adverse psy-
which can lead to comorbidities weight stigma are more susceptible chological consequences experienced
such as diabetes, heart disease, to disordered eating behaviors such by children and adolescents with obe-
and stroke. as binge eating, eating in secret, eat- sity and their caregivers.14,35,36
www.Nursing2022.com June l Nursing2022 l 19
Copyright © 2022 Wolters Kluwer Health, Inc. All rights reserved.
NSG0622_NCPD_WeightStigma_Ramakant.indd 19 29/04/22 3:27 PM
Reduced quality of life and academic per- more likely to be bullied than their environment rather than the child’s
formance healthy-weight peers.16 In addition, abilities.41,49,50
Health-related quality of life and these youth experience higher lev-
academic performance have been els of weight-based teasing, verbal Society and media
reported to be negatively impacted threats, physical harassment, negative Though our society has worked to
by experiences of weight stigma rumors, ignoring, avoiding, and so- address many forms of stigma and
in children and adolescents with cial exclusion.16,44 Children and ado- discrimination (such as race, dis-
obesity. Researchers have reported lescents are perceived as less popular, ability, and gender), a person’s body
children experiencing weight-based attractive, and athletic; more sensi- weight is one area where bias and
teasing have decreased health-related tive, and less likely to be identified as stigma continue to be acceptable in
quality of life.37 Poorer academic per- friends as their weight increases.44 society at large. In popular media,
formance among youth with obesity children with larger bodies are often
as compared with peers with healthy Family depicted as aggressive, unpopular,
weight has been reported in the lit- Weight bias among family members and unhealthy.51 They are often the
erature, though this is likely due to of children and adolescents with target of ridicule and insults specifi-
a stigmatizing environment and not obesity is common and can be both cally about body size.51 Researchers
caused by excess weight.38-40 implicit and explicit. Researchers found over 50% of the content of
report implicit and explicit biases movies and TV for children and ado-
Additional weight gain held by parents, though parents with lescents had weight stigmatizing sub-
The complex physiologic and psy- obesity have less bias than parents ject matter as compared with shows
chological mechanisms which occur of healthy weight.19 Implicit and targeting general audiences.51,52 Ad-
with experiences of weight stigma explicit weight bias by mothers to- ditionally, significant associations be-
can produce a negative feedback ward their adolescents significantly tween greater media exposure among
loop, which ultimately can lead to predicts higher weight bias inter- children and adolescents have been
additional weight gain (see Nega- nalization in these adolescents.45 shown to influence increased expres-
tive feedback loop in pediatric obesity). Siblings, parents, and extended sions of weight stigma toward peers
Stress hormones produced by family members have been reported with overweight and obesity.22
stigmatizing experiences can drive to tease, bully, and place blame on Social media has been found to
hunger and cause the body to store children and adolescents for their have a more significant impact on
fat.22,41 This stress response can also weight.35,46,47 In addition, conflict the promotion of weight stigma than
lead to increased anxiety, depres- and blame between biological par- other forms of media. Cyberbully-
sion, social isolation, and trigger ents about their child’s weight and ing has been documented to occur
unhealthy coping such as disordered how to approach weight manage- on social media due to increased
eating behaviors and lack of engage- ment adds to family discord and anonymity and lack of real conse-
ment in physical activity. stress and increases feelings of dis- quences.53 Body comparison among
tress and helplessness for the child peers and exposure to unrealistic im-
Sources of stigma experiencing stigmatization.35,46-48 ages on social media with its popular
Peers filter features have been reported to
The most prevalent source of weight Teachers promote body dissatisfaction, eating
stigma in children and adolescents Weight bias among teachers has disorders, and self-harm.53 People
is from peers.34 Studies have shown been documented in the literature with obesity may also be portrayed
children as young as age 4 hold- as prevalent in school settings and in stigmatizing ways such as being
ing negative biases and judgments includes both implicit and explicit unintelligent or undisciplined.53 So-
toward peers with higher weight.34 biases.34,44 Research indicates that cial media increases negative messag-
These negative biases continue some physical education teachers ing about weight, which promotes
through middle childhood into harbor assumptions that children individual blame that leads to nega-
adolescence and can be influenced and adolescents with high weight tive self-perception and internalized
by stigmatizing media content.42,43 have less general endurance com- weight bias.53
Researchers examining relationships pared with their peers.41,49 Educators
among children and adolescents have reported to believe obesity is Healthcare providers
with overweight and obesity and associated with impaired school per- Healthcare providers in a variety of
their peers have demonstrated youth formance, but as noted this is likely disciplines, including those provid-
with overweight and obesity are secondary to the stigmatizing school ing obesity care, have been found
20 l Nursing2022 l Volume 52, Number 6 www.Nursing2022.com
Copyright © 2022 Wolters Kluwer Health, Inc. All rights reserved.
NSG0622_NCPD_WeightStigma_Ramakant.indd 20 29/04/22 3:27 PM
Best practices for avoiding weight stigmatization11,22
Avoid oversimplifying obesity Address weight bias in healthcare Treat the child, adolescent, or
and consider all potential settings to improve patient parent with dignity, respect, and
causes. experience. empathy.
• Recognize that obesity is a • Consider and confront implicit and • Consider the multifactorial nature of
multifactorial disease which often explicit biases toward individuals with weight management, and explore
requires lifelong management. obesity. alternative factors that contribute to
• Challenge stereotypes about obesity • Support evidence-based care (such higher BMI.
as a lifestyle choice. as medications and metabolic • Commit to treating patients with
• Incorporate evidence-based obesity surgery). dignity and respect, regardless of their
and weight bias content in healthcare • During visits, maintain focus on the BMI.
curriculum. patient’s primary issue (which may or • Ask permission to discuss weight
may not be weight-related). during healthcare interactions.
• Advocate for and educate colleagues • Adopt people-first language; say child
on reducing weight stigma in practice or adolescent with higher BMI rather
settings. than “obese” child or adolescent.
to hold implicit and explicit weight viders, content surrounding the have the opposite effect, resulting
biases toward adults and youth with complex etiology and physiology in exercise avoidance, unhealthy
obesity.54 These biases can increase of obesity should be integrated into diets, and increased sedentary be-
patient stress and mistrust of health- the curriculum.21 Concurrently, fac- haviors that lead to worse physical
care providers, negatively influence ulty need education about the prev- and mental health, increased weight
patient engagement, motivation, alence of weight stigma and how to gain, and decreased quality of life.6
adherence, prevent timely access to negate stereotypes when instructing It is critical that public health ef-
care, and reduce the quality of care future healthcare providers.55,58 Re- forts to promote healthy weight and
provided.55-57 Youth with obesity searchers have shown that when an weight management behaviors are
and their parents have reported in- obesity curriculum was implement- nonstigmatizing.
teractions with healthcare providers ed for pediatric residents, there
which have ranged from overt blame were significant improvements in Recommendations for practice
to name-calling of the child.35,36 In their weight bias scores.58 Simi- Nursing is the largest healthcare
addition, parents have reported feel- larly, nursing students’ attitude and profession in the US and has been
ing blamed or stigmatized by health- support of patients with obesity ranked the most trusted profession
care providers for their perceived improved after they participated in for 20 years in a row.60 This posi-
role in their child’s weight.35 This simulations designed to assist them tions nurses to advocate for children
further diminishes the building of a in understanding the daily experi- and adolescents with obesity, lead
trusting relationship with the health- ence of living with obesity.18 in reducing the stigma, and improve
care provider. holistic health for this vulnerable
Implicit and explicit weight Public health initiatives population (see Best practices for
bias among healthcare providers Public health campaigns have ne- avoiding weight stigmatization). Nurs-
and medical students has been glected to consider stigma as a bar- es in pediatric healthcare settings
documented. One study found that rier in the effort to prevent and treat can begin by advocating for and
medical students exhibited greater obesity or have perpetuated weight providing weight-neutral approach-
explicit bias against people with stigma through their use of images es to care. For example, consider
obesity than against racial minori- that perpetuate negative obesity whether a visit requires the patient
ties, gays and lesbians, and people stereotypes.59 Some public health to get weighed. Though pediatric
who are poor.21 In addition, nurs- campaigns have suggested that medication dosing is weight-based
ing students have been reported openly shaming people with obesity for patients less than 40 kg, con-
to have negative attitudes toward will motivate them to change their sider reviewing the patient’s medical
patients with obesity.18 To reduce diet and exercise habits, thus per- record for the reason for the visit
weight bias among healthcare pro- petuating stigma.7,10 These strategies and the timing of previous visits pri-
www.Nursing2022.com June l Nursing2022 l 21
Copyright © 2022 Wolters Kluwer Health, Inc. All rights reserved.
NSG0622_NCPD_WeightStigma_Ramakant.indd 21 29/04/22 3:27 PM
or to weighing the patient.62 Placing consequences of weight stigma on
scales in a private space or room if patients’ physical and mental health,
available and paying attention to quality of life, and their motiva-
patient and parent cues can reduce tion to engage in healthy behaviors
stress, stigma, and the anxiety of is another area for advocacy. Much
being weighed. Providing furniture like addressing the stigma associated
in waiting rooms and other spaces, with mental health and substance
and equipment such as BP cuffs that use disorders, it is important to cor-
are adequately sized for persons rect inaccurate assumptions, com-
with obesity can promote a weight- munication, and behaviors. Nurses,
inclusive environment. regardless of practice area, can advo-
Nurses can also educate others Nurses can also educate cate for improved care for children
by modeling weight-inclusive words others by modeling and adolescents with obesity and
and behaviors and respectfully weight-inclusive words their families. Unlike treatment tied
bringing attention to overt stigma- to substance use disorders, one can-
tizing words and actions. Examples
and behaviors and not simply stop eating because food
include listening to the patient and respectfully bringing is necessary for sustaining life, is a
caregiver and not making the child’s attention to overt source of pleasure, and is central to
weight the focus of any visit un- stigmatizing words and most cultures and family traditions.
less given permission to discuss or Nurses can also partner with
if their weight is directly related to
actions. schools and communities as they
the reason for the visit. Consider- address bullying among youth by
ation for the language used when sharing that weight is the number
discussing weight is an important one reason that children are bullied.
area of advocacy. Using people-first obesity and positively impact the By highlighting this, nurses can bring
language is critical to decreasing bias culture of healthcare. attention to the implicit and explicit
and stigma. Referring to people as bias educators and other community
obese can influence how they feel Recommendations for policy members may have about children
about their weight as well as how Nurses should be leaders in advocat- and adolescents with obesity. Em-
and when they seek healthcare.63 ing for changes in health policy in powering youth to participate in
People-first language places the their institutions, communities, and both education and advocacy to
person first, not the condition (such society at large. This advocacy work reduce bullying and weight stigma
as “child with obesity” rather than begins with an awareness of one’s is an example of how nurses can
“obese child”) and helps to reduce own implicit bias regarding children engage in their communities and
weight stigma experienced while and adolescents with obesity. Implicit society at large by seeking out and
accessing healthcare.63 In a survey of bias is often a result of a lack of un- partnering with existing organiza-
adolescents with obesity (50% girls, derstanding of the complex physiol- tions.65
50% boys) and asking their prefer- ogy of obesity. Increased adipose tis-
ences for words that healthcare pro- sue, weight loss, and food restriction Conclusion
viders use to refer to their weight, all activate the body’s compensatory Understanding the prevalence and
adolescents preferred words like mechanisms and make weight loss negative impact of weight stigma
“weight,” “weight problem,” “BMI,” and maintenance extremely difficult in society and healthcare systems is
and “plus size” as opposed to pro- to sustain with only lifestyle modi- crucial to providing bias-free and
viders using the words “fat,” “large,” fications (such as diet and exercise). high-quality care to children and
“curvy,” “obese,” and “extremely Nurses should educate themselves youth with obesity and their families.
obese.”64 Healthcare providers and advocate for continuing educa- Nurses can begin by considering
should use non-stigmatizing com- tion across disciplines on the physi- their own implicit biases related to
munication, assess for teasing and ology of obesity. This knowledge weight and identify explicit weight
bullying, and educate families about will hopefully translate into reduced bias in their practice setting. Nurses
weight stigma in the home and implicit bias and increased empathy are in a strategic position to advo-
school settings.34 These behaviors for youth with obesity. cate, educate, and begin to reframe
will improve healthcare encounters Educating oneself, colleagues, the context of healthcare for children
for children and adolescents with patients, and their families on the and youth with obesity. ■
22 l Nursing2022 l Volume 52, Number 6 www.Nursing2022.com
Copyright © 2022 Wolters Kluwer Health, Inc. All rights reserved.
NSG0622_NCPD_WeightStigma_Ramakant.indd 22 29/04/22 3:27 PM
REFERENCES 17. Pont SJ, Puhl R, Cook SR, Slusser W. Stigma 33. Araiza AM, Wellman JD. Weight stigma
1. Fryar CD, Carroll MD, Afful JA. Prevalence of experienced by children and adolescents with predicts inhibitory control and food selection in
overweight, obesity, and severe obesity among obesity. Pediatrics. 2017;140(6):1-11. response to the salience of weight discrimination.
children and adolescents aged 2–19 years: United 18. Hunter J, Rawlings-Anderson K, Lindsay T, Appetite. 2017;114:382-390. doi:10.1016/j.
States, 1963–1965 through 2017–2018. 2020. Bowden T, Aitken LM. Exploring student nurses’ appet.2017.04.009.
www.cdc.gov/nchs/data/hestat/obesity-child-17-18/ attitudes towards those who are obese and whether 34. Puhl RM, Lessard LM. Weight stigma in youth:
overweight-obesity-child-H.pdf. these attitudes change following a simulated prevalence, consequences, and considerations for
2. Hruby A, Hu FB. The epidemiology of obesity: activity. Nurse Educ Today. 2018;65:225-231. clinical practice. Curr Obes Rep. 2020;9(4):402-411.
a big picture. Pharmacoeconomics. 2015;33(7):673- doi:10.1016/j.nedt.2018.03.013. doi:10.1007/s13679-020-00408-8.
689. doi:10.1007/s40273-014-0243-x. 19. Lydecker JA, O’Brien E, Grilo CM. Parents have 35. Roberts KJ, Polfuss ML, Marston EC, Davis
3. Ludwig DS, Aronne LJ, Astrup A, et al. The both implicit and explicit biases against children RL. Experiences of weight stigma in adolescents
carbohydrate-insulin model: a physiological with obesity. J Behav Med. 2018;41(6):784-791. with severe obesity and their families. J Adv Nurs.
perspective on the obesity pandemic. Am J Clin doi:10.1007/s10865-018-9929-4. 2021;77(10):4184-4194. doi:10.1111/jan.15012.
Nutr. 2021;114(6):1873-1885. doi:10.1093/ajcn/ 20. Lynagh M, Cliff K, Morgan PJ. Attitudes and 36. Zenlea IS, Thompson B, Fierheller D, et al.
nqab270. beliefs of nonspecialist and specialist trainee health Walking in the shoes of caregivers of children with
4. Skinner AC, Perrin EM, Moss LA, Skelton and physical education teachers toward obese obesity: supporting caregivers in paediatric weight
JA. Cardiometabolic risks and severity of children: evidence for “anti-fat” bias. J Sch Health. management. Clin Obes. 2017;7(5):300-306.
obesity in children and young adults. N Engl 2015;85(9):595-603. doi:10.1111/josh.12287.
37. Guardabassi V, Mirisola A, Tomasetto C. How
J Med. 2015;373(14):1307-1317. doi:10.1056/ 21. Phelan SM, Dovidio JF, Puhl RM, et al. is weight stigma related to children’s health-related
NEJMoa1502821. Implicit and explicit weight bias in a national quality of life? A model comparison approach. Qual
5. Juvonen J, Lessard LM, Schacter HL, Suchilt sample of 4,732 medical students: the medical Life Res. 2018;27(1):173-183. doi:10.1007/s11136-
L. Emotional implications of weight stigma student CHANGES study. Obesity (Silver Spring). 017-1701-7.
across middle school: the role of weight-based 2014;22(4):1201-1208. doi:10.1002/oby.20687.
38. Wu N, Chen Y, Yang J, Li F. Childhood obesity
peer discrimination. J Clin Child Adolesc Psychol. 22. Fields LC, Brown C, Skelton JA, Cain KS, and academic performance: the role of working
2017;46(1):150-158. doi:10.1080/15374416.2016. Cohen GM. Internalized weight bias, teasing, memory. Front Psychol. 2017;8:611. doi:10.3389/
1188703. and self-esteem in children with overweight or fpsyg.2017.00611.
6. Puhl R, Suh Y. Health consequences of weight obesity. Child Obes. 2021;17(1):43-50. doi:10.1089/
39. Asirvatham J, Thomsen MR, Nayga RM Jr.
stigma: implications for obesity prevention and chi.2020.0150.
Childhood obesity and academic performance
treatment. Curr Obes Rep. 2015;4(2):182-190. 23. Tomiyama AJ, Epel ES, McClatchey TM, et among elementary public school children. Educ
doi:10.1007/s13679-015-0153-z. al. Associations of weight stigma with cortisol Res. 2019;61(1):1-21. doi:10.1080/00131881.2019
7. Rubino F, Puhl RM, Cummings DE, et al. Joint and oxidative stress independent of adiposity. .1568199.
international consensus statement for ending Health Psychol. 2014;33(8):862-867. doi:10.1037/
40. Guardabassi V, Tomasetto C. Weight status
stigma of obesity. Nat Med. 2020;26(4):485-497. hea0000107.
or weight stigma? Obesity stereotypes-not excess
doi:10.1038/s41591-020-0803-x. 24. Sutin AR, Stephan Y, Luchetti M, Terracciano weight-reduce working memory in school-aged
8. Lawrence BJ, Kerr D, Pollard CM, et al. Weight A. Perceived weight discrimination and C-reactive children. J Exp Child Psychol. 2020;189:104706.
bias among health care professionals: a systematic protein. Obesity (Silver Spring). 2014;22(9):1959- doi:10.1016/j.jecp.2019.104706.
review and meta-analysis. Obesity (Silver Spring). 1961. doi:10.1002/oby.20789.
41. Tomiyama AJ, Carr D, Granberg EM, et
2021;29(11):1802-1812. doi:10.1002/oby.23266. 25. Himmelstein MS, Incollingo Belsky AC, al. How and why weight stigma drives the
9. Palad CJ, Yarlagadda S, Stanford FC. Weight Tomiyama AJ. The weight of stigma: cortisol obesity ‘epidemic’ and harms health. BMC Med.
stigma and its impact on paediatric care. Curr reactivity to manipulated weight stigma. Obesity 2018;16(1):123. doi:10.1186/s12916-018-1116-5.
Opin Endocrinol Diabetes Obes. 2019;26(1):19-24. (Silver Spring). 2015;23(2):368-374. doi:10.1002/
42. Karsay K, Schmuck D. “Weak, sad, and lazy
doi:10.1097/med.0000000000000453. oby.20959.
fatties”: adolescents’ explicit and implicit weight
10. Callahan D. Children, stigma, and obesity. 26. Schvey NA, Puhl RM, Brownell KD. The stress bias following exposure to weight loss reality TV
JAMA Pediatr. 2013;167(9):791-792. doi:10.1001/ of stigma: exploring the effect of weight stigma on shows. Media Psychol. 2019;22(1):60-81. doi:10.108
jamapediatrics.2013.2814. cortisol reactivity. Psychosom Med. 2014;76(2):156- 0/15213269.2017.1396903.
162. doi:10.1097/psy.0000000000000031.
11. Bucchianeri MM, Gower AL, McMorris 43. Rex-Lear M, Jensen-Campbell LA, Lee S. Young
BJ, Eisenberg ME. Youth experiences with 27. Pearl RL, Wadden TA, Jakicic JM. Is weight and biased: children’s perceptions of overweight
multiple types of prejudice-based harassment. stigma associated with physical activity? A peers. J Appl Biobehav Res. 2019;24(2):e12161.
J Adolesc. 2016;51:68-75. doi:10.1016/j. systematic review. Obesity (Silver Spring). doi:10.1111/jabr.12161.
adolescence.2016.05.012. 2021;29(12):1994-2012. doi:10.1002/oby.23274.
44. Nutter S, Ireland A, Alberga AS, et al. Weight
12. Haqq AM, Kebbe M, Tan Q, Manco M, 28. Han S, Agostini G, Brewis AA, Wutich A. bias in educational settings: a systematic review.
Ramos Salas X. Complexity and stigma of Avoiding exercise mediates the effects of internalized Curr Obes Rep. 2019;8(2):185-200. doi:10.1007/
pediatric obesity. Child Obes. 2021;17(4):229-240. and experienced weight stigma on physical activity s13679-019-00330-8.
doi:10.1089/chi.2021.0003. in the years following bariatric surgery. BMC Obes.
45. Puhl RM, Himmelstein MS. Weight bias
2018;5:18. doi:10.1186/s40608-018-0195-3.
13. Puhl RM, Wall MM, Chen C, Bryn Austin S, internalization among adolescents seeking weight
Eisenberg ME, Neumark-Sztainer D. Experiences 29. Greenleaf C, Petrie TA, Martin SB. Relationship loss: implications for eating behaviors and parental
of weight teasing in adolescence and weight-related of weight-based teasing and adolescents’ communication. Front Psychol. 2018;9:2271.
outcomes in adulthood: a 15-year longitudinal psychological well-being and physical health. J Sch doi:10.3389/fpsyg.2018.02271.
study. Prev Med. 2017;100:173-179. doi:10.1016/j. Health. 2014;84(1):49-55. doi:10.1111/josh.12118.
46. Eisenberg ME, Puhl R, Watson RJ. Family
ypmed.2017.04.023. 30. Ievers-Landis CE, Dykstra C, Uli N, O’Riordan weight teasing, LGBTQ attitudes, and well-being
14. Pearl RL, Puhl RM. Weight bias internalization MA. Weight-related teasing of adolescents among LGBTQ adolescents. Fam Community
and health: a systematic review. Obes Rev. who are primarily obese: roles of sociocultural Health. 2020;43(1):17-25. doi:10.1097/
2018;19(8):1141-1163. doi:10.1111/obr.12701. attitudes towards appearance and physical fch.0000000000000239.
activity self-efficacy. Int J Environ Res Public Health.
15. Pearl RL, Puhl RM, Himmelstein MS, Pinto 47. Pearlman AT, Schvey NA, Neyland MKH, et al.
2019;16(9):1540. doi:10.3390/ijerph16091540.
AM, Foster GD. Weight stigma and weight-related Associations between family weight-based teasing,
health: associations of self-report measures 31. Himmelstein MS, Puhl RM, Watson RJ. eating pathology, and psychosocial functioning
among adults in weight management. Ann Behav Weight-based victimization, eating behaviors, among adolescent military dependents. Int J Environ
Med. 2020;54(11):904-914. doi:10.1093/abm/ and weight-related health in sexual and gender Res Public Health. 2019;17(1):24. doi:10.3390/
kaaa026. minority adolescents. Appetite. 2019;141:104321. ijerph17010024.
doi:10.1016/j.appet.2019.104321.
16. Puhl RM, Himmelstein MS, Pearl RL. Weight 48. Roberts KJ, Gallo AM, Patil CL, Vincent
stigma as a psychosocial contributor to obesity. 32. Vartanian LR, Porter AM. Weight stigma and C, Binns HJ, Koenig MD. Family management
Am Psychol. 2020;75(2):274-289. doi:10.1037/ eating behavior: a review of the literature. Appetite. of severe obesity in adolescents. J Pediatr Nurs.
amp0000538. 2016;102:3-14. doi:10.1016/j.appet.2016.01.034. 2021;60:181-189. doi:10.1016/j.pedn.2021.06.016.
www.Nursing2022.com June l Nursing2022 l 23
Copyright © 2022 Wolters Kluwer Health, Inc. All rights reserved.
NSG0622_NCPD_WeightStigma_Ramakant.indd 23 29/04/22 3:27 PM
49. Kenney EL, Redman MT, Criss S, Sonneville 55. Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt 62. Matson KL, Horton ER, Capino AC. Medication
KR, Austin SB. Are K-12 school environments WL, Griffin JM, van Ryn M. Impact of weight bias dosage in overweight and obese children.
harming students with obesity? A qualitative and stigma on quality of care and outcomes for J Pediatr Pharmacol Ther. 2017;22(1):81-83.
study of classroom teachers. Eat Weight Disord. patients with obesity. Obes Rev. 2015;16(4):319- doi:10.5863/1551-6776-22.1.81.
2017;22(1):141-152. doi:10.1007/s40519-016- 326. doi:10.1111/obr.12266. 63. Obesity Action Coalitian. People-First Language
0268-6. 56. Alberga AS, Pickering BJ, Alix Hayden K, et for Obesity. 2021. www.obesityaction.org/
50. Lessard LM, Puhl RM. Reducing educators’ al. Weight bias reduction in health professionals: wp-content/uploads/1033162_FirstPersonOne-
weight bias: the role of school-based anti-bullying a systematic review. Clin Obes. 2016;6(3):175-188. Pager01_041921.pdf.
policies. J School Health. 2021;91(10):796-801. doi:10.1111/cob.12147. 64. Puhl RM, Himmelstein MS. Adolescent
doi:10.1111/josh.13068. 57. Jachyra P, Anagnostou E, Knibbe TJ, et al. preferences for weight terminology used by health
51. Eisenberg ME, Carlson-McGuire A, Gollust SE, Weighty conversations: caregivers’, children’s, care providers. Pediatr Obes. 2018;13(9):533-540.
Neumark-Sztainer D. A content analysis of weight and clinicians’ perspectives and experiences of doi:10.1111/ijpo.12275.
stigmatization in popular television programming discussing weight-related topics in healthcare 65. 10-8 InService. 2021. https://10-8inservice.org/.
for adolescents. Int J Eat Disord. 2015;48(6):759- consultations. Autism Res. 2018;11(11):1500-1510.
766. doi:10.1002/eat.22348. doi:10.1002/aur.2017.
52. Throop EM, Skinner AC, Perrin AJ, Steiner 58. Rincon-Subtirelu M. Education as a tool
Karyn J. Roberts is an adjunct assistant professor at
MJ, Odulana A, Perrin EM. Pass the popcorn: to modify anti-obesity bias among pediatric Northwestern University Feinberg School of Medi-
“obesogenic” behaviors and stigma in children’s residents. Int J Med Educ. 2017;8:77-78. doi:10.5116/ cine-Department of Pediatrics in Chicago, Ill. and a
movies. Obesity (Silver Spring). 2014;22(7):1694- ijme.58b1.46e3. clinical assistant professor at the University of Wis-
1700. doi:10.1002/oby.20652. 59. Johnstone G, Grant SL. Weight stigmatisation consin-Milwaukee (UW-Milwaukee) College of Nurs-
ing in Milwaukee, Wis., where Michele L. Polfuss is
53. Clark O, Lee MM, Jingree ML, et al. Weight in antiobesity campaigns: the role of images. Health an associate professor. She’s also the Joint Research
stigma and social media: evidence and public Promot J Austr. 2019;30(1):37-46. doi:10.1002/ Chair in the Nursing of Children at UW-Milwaukee
health solutions. Front Nutr. 2021;8:739056. hpja.183. and Children’s Hospital of Wisconsin.
doi:10.3389/fnut.2021.739056. 60. American Association of Colleges of Nursing.
54. Garcia JT, Amankwah EK, Hernandez RG. Nursing Fact Sheet. 2019. www.aacnnursing.org/
Assessment of weight bias among pediatric news-Information/fact-sheets/nursing-fact-sheet. The authors and planners have disclosed no potential
nurses and clinical support staff toward 61. Gaines K. Nurses ranked most trusted conflicts of interest, financial or otherwise.
obese patients and their caregivers. J Pediatr profession 19 years in a row. 2021. https://
Nurs. 2016;31(4):e244-e251. doi:10.1016/j. nurse.org/articles/nursing-ranked-most-honest-
pedn.2016.02.004. profession/. DOI-10.1097/01.NURSE.0000829904.57766.58
> For 207 additional continuing professional development articles related to
Pediatrics topics, go to nursingcenter.com/CE. >
NCPD Nursing Continuing
Professional Development
INSTRUCTIONS
Weight stigma in children and adolescents: Recommendations for practice and policy
TEST INSTRUCTIONS PROVIDER ACCREDITATION
• Read the article. The test for this nursing continuing professional Lippincott Professional Development will award 2.0 contact hours
development (NCPD) activity is to be taken online at www.nursing for this nursing continuing professional development activity.
center.com/CE/nursing. Tests can no longer be mailed or faxed. Lippincott Professional Development is accredited as a provider
• You'll need to create an account (it's free!) and log in to access My of nursing continuing professional development by the American
Planner before taking online tests. Your planner will keep track of all Nurses Credentialing Center's Commission on Accreditation.
your Lippincott Professional Development online NCPD activities This activity is also provider approved by the California Board
for you. of Registered Nursing, Provider Number CEP 11749 for 2.0 contact
• There's only one correct answer for each question. A passing score hours. Lippincott Professional Development is also an approved
for this test is 7 correct answers. If you pass, you can print your provider of continuing nursing education by the District of
certificate of earned contact hours and access the answer key. If you Columbia, Georgia, West Virginia, New Mexico, South Carolina,
fail, you have the option of taking the test again at no additional cost. and Florida, CE Broker #50-1223. Your certificate is valid in all states.
• For questions, contact Lippincott Professional Development: Payment: The registration fee for this test is $21.95.
1-800-787-8985.
• Registration deadline is June 6, 2025.
24 l Nursing2022 l Volume 52, Number 6 www.Nursing2022.com
Copyright © 2022 Wolters Kluwer Health, Inc. All rights reserved.
NSG0622_NCPD_WeightStigma_Ramakant.indd 24 29/04/22 3:27 PM
You might also like
- Facilitator Guide A Class DividedDocument8 pagesFacilitator Guide A Class Dividedbmorris777No ratings yet
- Prejudice and DiscriminationDocument27 pagesPrejudice and DiscriminationAnonymous DqeRReNo ratings yet
- HomelessDocument13 pagesHomelessapi-409521281No ratings yet
- The Psychological Impact of AusterityDocument16 pagesThe Psychological Impact of AusterityThe Centre for Welfare Reform100% (2)
- Sample Literature Review - PsychologyDocument9 pagesSample Literature Review - Psychologyapi-242012614No ratings yet
- 1 Official Synthesis EssayDocument9 pages1 Official Synthesis Essayapi-461616923No ratings yet
- Microaggressions in The ClassroomDocument2 pagesMicroaggressions in The Classroomapi-388641000No ratings yet
- Parent Stress Index With Instructions - 11-28-11Document2 pagesParent Stress Index With Instructions - 11-28-11Sumit SinghNo ratings yet
- PrejudiceDocument14 pagesPrejudiceReinaNo ratings yet
- Dummy ReportDocument29 pagesDummy ReportnaquiahoNo ratings yet
- Eating Disorders 1Document46 pagesEating Disorders 1Heba_Al_KhozaeNo ratings yet
- Smashing Stigma: Dismantling Stereotypes, Prejudice, and DiscriminationFrom EverandSmashing Stigma: Dismantling Stereotypes, Prejudice, and DiscriminationNo ratings yet
- Psych 575 Disorder PSYCH 575 WEEK 5 DISORDER PAPER Select A Neurological, Psychological, or Neurodevelopmental Disorder. THE DISORDER FOR THIS PAPER IS PARKINSON'S DIESESEDocument13 pagesPsych 575 Disorder PSYCH 575 WEEK 5 DISORDER PAPER Select A Neurological, Psychological, or Neurodevelopmental Disorder. THE DISORDER FOR THIS PAPER IS PARKINSON'S DIESESEWrite This Way (R)100% (1)
- Skills For Care Presentation Web Version Standard 4Document11 pagesSkills For Care Presentation Web Version Standard 4Georgiana GeorgyNo ratings yet
- Promoting Healthy Aging by Confronting AgeismDocument7 pagesPromoting Healthy Aging by Confronting AgeismJuanito MaravillasNo ratings yet
- Interview Questions 5Document5 pagesInterview Questions 5api-502274542No ratings yet
- Borderline Clients Tend To Show: The TAT and Borderline, Narcissistic, and Psychotic PatientsDocument2 pagesBorderline Clients Tend To Show: The TAT and Borderline, Narcissistic, and Psychotic Patientsaastha jainNo ratings yet
- The Effects of Gender Role Socialization On Self-Expression of Female Students in Secondary School The Case of Fasil-DeseDocument10 pagesThe Effects of Gender Role Socialization On Self-Expression of Female Students in Secondary School The Case of Fasil-DesearcherselevatorsNo ratings yet
- NEUROPSYCHOLOGY of AGING PDFDocument74 pagesNEUROPSYCHOLOGY of AGING PDFLisa DottiNo ratings yet
- Research Final DefenseDocument67 pagesResearch Final DefenseNellyWataNo ratings yet
- Lo3 Artifact - Micro-Counseling Skills Midterm ReflectionDocument6 pagesLo3 Artifact - Micro-Counseling Skills Midterm Reflectionapi-543749170No ratings yet
- The Emotionally Abused and Neglected Child: Identification, Assessment and Intervention: A Practice HandbookFrom EverandThe Emotionally Abused and Neglected Child: Identification, Assessment and Intervention: A Practice HandbookNo ratings yet
- Old Age Consists of Ages Nearing or Surpassing The Average Life Span of HumanDocument13 pagesOld Age Consists of Ages Nearing or Surpassing The Average Life Span of HumanVarun JainNo ratings yet
- Developing Mental Health Nursing Practice - Edited.edited - Edited.editedDocument17 pagesDeveloping Mental Health Nursing Practice - Edited.edited - Edited.editedakolom samuelNo ratings yet
- Senior Project PresentationDocument13 pagesSenior Project Presentationapi-535239899No ratings yet
- TransYouth Clinic Presentation To LAUSDDocument40 pagesTransYouth Clinic Presentation To LAUSDDaily Wire Investigations TeamNo ratings yet
- Trauma-Informed CareDocument18 pagesTrauma-Informed Careapi-384358306100% (1)
- Sda 5910 03 Praxis PaperDocument9 pagesSda 5910 03 Praxis Paperapi-665859469No ratings yet
- SLCS RDocument2 pagesSLCS RdanieljohnarboledaNo ratings yet
- Autism Research Paper - Samantha MiglioreDocument11 pagesAutism Research Paper - Samantha Miglioreapi-456361087No ratings yet
- Adolescent Development: Physical and Emotional DevelopmentDocument14 pagesAdolescent Development: Physical and Emotional DevelopmentAoi Sora100% (1)
- Pyschology PaperDocument53 pagesPyschology Paperapi-500458080No ratings yet
- WorldpovertyDocument9 pagesWorldpovertyapi-318228418No ratings yet
- Challenge The Status QuoDocument49 pagesChallenge The Status QuoChris StewartNo ratings yet
- Daddy Dearest? Active Fatherhood and Public PolicyDocument90 pagesDaddy Dearest? Active Fatherhood and Public PolicyIPPRNo ratings yet
- Muscle DysmorphiaDocument4 pagesMuscle DysmorphiaFarfoosh Farfoosh FarfooshNo ratings yet
- Harm to Others: The Assessment and Treatment of DangerousnessFrom EverandHarm to Others: The Assessment and Treatment of DangerousnessNo ratings yet
- Research Essay Final WeeblyDocument12 pagesResearch Essay Final Weeblyapi-519040910No ratings yet
- The Abrasive PatientDocument149 pagesThe Abrasive Patientmaruan_trascu5661No ratings yet
- Historical Perspective On The Study of Aging - BASA, ULAHDocument29 pagesHistorical Perspective On The Study of Aging - BASA, ULAHDebayn CandidatoNo ratings yet
- Gender IssuesDocument55 pagesGender Issuessija-ekNo ratings yet
- Guia - AdolescentesDocument6 pagesGuia - AdolescentesCentro De Psicoterapia Condesa100% (1)
- Social Determinants of Health: Why Is There Such A Gap Between Our Knowledge and Its Implementation?Document77 pagesSocial Determinants of Health: Why Is There Such A Gap Between Our Knowledge and Its Implementation?Avinash KumarNo ratings yet
- Application Assignment 1Document12 pagesApplication Assignment 1api-595939801No ratings yet
- Louis Russo Life Story Through The Prism of Older Adult Developmental TheoriesDocument18 pagesLouis Russo Life Story Through The Prism of Older Adult Developmental TheoriesDaniel R. Gaita, MA, LMSWNo ratings yet
- Social StigmaDocument32 pagesSocial StigmaDavi MarquesNo ratings yet
- Community PsychologyDocument20 pagesCommunity PsychologyMaePornelaGomezNo ratings yet
- Exploratory Essay Draft 2Document3 pagesExploratory Essay Draft 2api-358044397No ratings yet
- Critical Reflection EssayDocument7 pagesCritical Reflection EssaykjdwcNo ratings yet
- H.4 Borderline PowerPoint Revised 2015Document31 pagesH.4 Borderline PowerPoint Revised 2015Ptrc Lbr LpNo ratings yet
- The AgedDocument14 pagesThe AgeddexminiNo ratings yet
- LGBTQ ArticlesDocument4 pagesLGBTQ ArticlesAnonymous Qn8AvWvxNo ratings yet
- Build Emotional Muscle For More Productive and Satisfying LivesFrom EverandBuild Emotional Muscle For More Productive and Satisfying LivesNo ratings yet
- EriksonDocument8 pagesEriksonNungs Ainul InungNo ratings yet
- Person Perception: Forming Impressions of OthersDocument65 pagesPerson Perception: Forming Impressions of OthersgprasadatvuNo ratings yet
- What Is CompassionDocument4 pagesWhat Is Compassionapi-508026516No ratings yet
- Endodontic Pain: Paul A. RosenbergDocument24 pagesEndodontic Pain: Paul A. RosenbergArturo Trejo VeraNo ratings yet
- BR IER December 2023Document7 pagesBR IER December 2023Jed A. MartirNo ratings yet
- Distribution of ABO and RH-D Blood Group Antigens Among Blood Donors in The Amhara Regional State, EthiopiaDocument11 pagesDistribution of ABO and RH-D Blood Group Antigens Among Blood Donors in The Amhara Regional State, EthiopiaSely wulan widya ningsihNo ratings yet
- Effect of Custom-Made Footwear On Foot Ulcer Recurrence in DiabetesDocument8 pagesEffect of Custom-Made Footwear On Foot Ulcer Recurrence in DiabetesJosé MorenoNo ratings yet
- How To Write An Essay From An InterviewDocument5 pagesHow To Write An Essay From An Interviewafibzfwdkaesyf100% (2)
- Tutorial Material For Mandatory Basic Safety Training Course (Construction Work)Document22 pagesTutorial Material For Mandatory Basic Safety Training Course (Construction Work)Nirajan MarwaitNo ratings yet
- Pineal GlandDocument2 pagesPineal GlandYolisNo ratings yet
- Physical and Chemical Restraint (An Update)Document15 pagesPhysical and Chemical Restraint (An Update)Alifvia IntanNo ratings yet
- Desi1219 DossierDocument82 pagesDesi1219 DossierJuy HuyNo ratings yet
- Case Study MiDocument23 pagesCase Study Mianamika sharma100% (7)
- Preventing and Managing Breast EngorgementDocument3 pagesPreventing and Managing Breast EngorgementAlifaNo ratings yet
- Osteoarthritis: Epidemiology, Risk Factors, and PathophysiologyDocument10 pagesOsteoarthritis: Epidemiology, Risk Factors, and PathophysiologyMaryama AflahaNo ratings yet
- EnglishInAction3 Keyword Unit6Document2 pagesEnglishInAction3 Keyword Unit6Băng Di TrầnNo ratings yet
- Summary MIT Document - Edited For SLTribDocument23 pagesSummary MIT Document - Edited For SLTribThe Salt Lake TribuneNo ratings yet
- Hipertensión SitémicaDocument12 pagesHipertensión SitémicaIván Alejandro Trejo ValdiviezoNo ratings yet
- Autoimmune Disorders - AgungDocument40 pagesAutoimmune Disorders - AgungalgutNo ratings yet
- Solar PlexusDocument8 pagesSolar PlexusEbyug AkhilNo ratings yet
- 6 - Hand Deformities, Fractures, and PalsyDocument57 pages6 - Hand Deformities, Fractures, and PalsyKarthiga RajooNo ratings yet
- Kav It HaDocument158 pagesKav It HaRuthraaadi RameshkumarNo ratings yet
- CASE STUDY ABRUPTIO PLACENTA BSN 2 H For Printing NA FINAL NAaaaaaaDocument36 pagesCASE STUDY ABRUPTIO PLACENTA BSN 2 H For Printing NA FINAL NAaaaaaaisaacdarylNo ratings yet
- 3 Behavioral Neurology and Psychiatry (045-075)Document31 pages3 Behavioral Neurology and Psychiatry (045-075)Eliana NataliaNo ratings yet
- Psychotherapeutic Agents: They Are Used To Treat Psychoses-Perceptual and Behavioral DisordersDocument26 pagesPsychotherapeutic Agents: They Are Used To Treat Psychoses-Perceptual and Behavioral DisordersJustin Ahorro-DionisioNo ratings yet
- Lec Framework Care of MotherDocument27 pagesLec Framework Care of MotherRica ParcasioNo ratings yet
- Final Burtons SummaryDocument53 pagesFinal Burtons SummaryJessabelle Ramos100% (1)
- Brenner and Stevens, Pharmacology 3 © 2010Document5 pagesBrenner and Stevens, Pharmacology 3 © 2010PharAwayNo ratings yet
- Dietary Lipids For Healthy Brain FunctionDocument247 pagesDietary Lipids For Healthy Brain FunctionLaudry Fanthera100% (1)
- AAPC Module 1 - Introduction To Artificial IntelligenceDocument18 pagesAAPC Module 1 - Introduction To Artificial Intelligencetami.albertNo ratings yet
- 2008 Curcumin AD - Hong Kong StudyDocument22 pages2008 Curcumin AD - Hong Kong StudysandyedamanaNo ratings yet
- Artículo Aparato de Golgi - Liu Et Al. 2021Document14 pagesArtículo Aparato de Golgi - Liu Et Al. 2021MARIA SOL MONTALVO LALALEONo ratings yet
- Cardiovascular Complications of Respiratory DisordersDocument334 pagesCardiovascular Complications of Respiratory DisordersDani CapiNo ratings yet