Professional Documents
Culture Documents
Ortho Supplemental Notes
Uploaded by
MARIA ANGELIKA DEL ROSARIO0 ratings0% found this document useful (0 votes)
27 views5 pagesOriginal Title
ORTHO-SUPPLEMENTAL-NOTES
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
27 views5 pagesOrtho Supplemental Notes
Uploaded by
MARIA ANGELIKA DEL ROSARIOCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 5
TRACTION - Assess back of the knee for pressure
- The act of pulling associated with sores
counterpull - Check for signs and symptoms of
PURPOSES thrombophlebitis
1. Reduce/immobilize fractures 3. Bryant Traction
2. Relieve muscle pain/spasm - Both legs raised at 90 degree angle to
3. Relieve pain bed because the weight of the child is not
4. Prevent/correct deformities adequate to provide countertraction
- Used for children under 2 years and
TYPES OF TRACTION
A. Skin traction – uses elastic bandages and 30 pounds to treat fractures of the femur and
adhesives hip dislocation
– is used to control muscle spasms and to - Buttocks must be slightly off the
immobilize an area before surgery mattress to enhance efficacy of the weight as
- Is accomplished by using a weight to pull countertraction
on traction tape or on a foam boot - Knees slightly flexed to prevent
attached to the skin hyperextension deformity
- The amount of weight applied must not 4. Cervical Traction
exceed the tolerance of the skin - Cervical head halter attached to
1. Buck’s Traction weights that hang over head of bed
- to temporary immobilize the leg in - Used for soft tissue damage or
patient with a fractured hip degenerative disc disease of cervical spine to
- shock blocks at the foot of the bed to reduce muscle spasm and maintain
produce counter traction and to prevent the alignment
patient from sliding down in bed - Usually intermittent traction, elevate
- turn towards unaffected side, with 2 head of bed to provide countertraction
pillows in between legs - Do not shave beard for better
- check for pressure sore at the heel of anchorage of halter
the feet and signs and symptoms of 5. Pelvic Traction
thrombophlebitis - Pelvic girdle with extension straps
2. Russell’s Traction attached to ropes and weights used for low
- Knee is suspended in a sling attached back to reduce muscle spasm and maintain
to a rope and pulley on a Balkan frame, alignment
creating upward pull from the knee - Usually intermittent, patient in semi-
- Weights are attached to the foot of Fowler’s position with knee gatched 20-30
the bed creating horizontal traction degrees angle, secure pelvic girdle around
- Used to treat fracture of the femur iliac crests
- Allows patient to move about in bed - Encourage to use overhead trapeze
more freely and permits bending of the knee -
joint B. SKELETAL TRACTION
- Hip should be flexed at 20 degrees; 1. Balanced Suspension Traction
foot of bed usually elevated by shock blocks - Produced by a counterforce other
to provide countertraction than the patient’s weight
- Extremity floats or balances in the 5. Turn the client as indicated.
traction apparatus 6. Avoid friction.
- Patient may change position without 7. Pin site care for skeletal traction:
disturbing the line of traction - Cleanse and apply antibiotic ointment.
2. Thomas Splint with Pearson attachment - Do neurovascular check.
- Used with skeletal traction in - Prevent complications of immobility.
fractures of the femur, hip should be flexed
at 20˚
- Use footplate to prevent footdrop CASTING MATERIALS
TYPES:
- Check pressure at the inguinal area
1. Nonplaster (synthetic)
(groin)
- Generally referred to as fiberglass casts
- Because upward traction is required,
which have the versatility of plaster but
an overbed frame is used
are lighter in weight, stronger, water-
3. Dunlop traction - horizontal traction to
resistant and durable
align fractures of the humerus; vertical
- Reach full rigid strength in minutes
traction maintains the forearm in proper
- Are porous and therefore diminish skin
alignment
problems
4. 90® – 90® Traction – for femoral fractures
- Do not soften when wet which allows the
in children
use of hydrotherapy
NOTE: Only skeletal traction has pin site care to - When wet, dry with a hair drier on a cool
avoid development of osteomyelitis. setting; dry thoroughly to prevent skin
breakdown
- Indication: used for nondisplaced
PRINCIPLES IN THE CARE OF THE CLIENT WITH fractures with minimal swelling and for
TRACTION long-term wear
1. Traction must be continuous to be effective
in reducing and immobilizing fractures. 2. Plaster
2. Skeletal traction is never interrupted. - Rolls of plaster bandage wet in cool water
3. Weights are not removed unless intermittent applied smoothly to the body
traction is prescribed. - A crystallizing reaction can occur and heat
4. Any factor that might reduce the effective is given off which can be uncomfortable,
pull or alter in resultant line of pull must be therefore, nurse should inform patient
eliminated: about the sensation of increasing warmth
a. The patient must be in good body so patient does not become alarmed
alignment in the center of the bed when - Cast needs to be exposed to allow
traction is applied. maximum dissipation of the heat and that
b. Ropes must be unobstructed. most casts cool after about 15 minutes
c. Weights must hang free and not rest on - It does not have its full strength until dry
the bed or floor. - When wet, cast can be dented, therefore,
d. Knots in the rope or the footplate must it must be handled with the palms of the
not touch the pulley or the foot of the hand and not allowed to rest on hard
bed. surfaces or sharp edges
- Requires 24 to 72 hours to dry completely try to dorsiflex (peroneal nerve =
- Freshly applied cast should be exposed to damage causes footdrop) and plantarflex
circulating air to dry and should not be (tibial nerve) the ankles and flex and
covered with clothing or bed linens extend the toes.
- Wet plaster cast: appears dull and gray, Pulse: If an upper extremity is involved,
sounds dull on percussion, feels damp, brachial, radial, ulnar, and digital pulses
and smells musty should be checked. If a lower extremity is
- Dry plaster cast: white and shiny, involved, femoral, popliteal, posterior
resonant, odorless, and firm tibial, and dorsalis pedis pulses should be
monitored.
CARE OF THE CLIENT WITH CAST Pain: Any sign of pain should be noted
1. Carry with palms of the hand, not the fingers and the exact area determined
to prevent indentation and pressure. 11. Windowing – to facilitate observation under
2. Do not insert anything into the cast. the cast if infected
3. Use blower to relieve itchiness inside the 12. . Bivalving – done for casts that are too tight
cast. to prevent compartment syndrome.
4. Elevate with pillow support for the first 24-48
hours to prevent edema.
5. Expose to air to dry.
6. Keep clean and dry.
7. Observe “hot spots” & musty odor. These
are signs and symptoms of infection.
8. Maintain skin integrity – “petalling”
9. Do isometric exercises on the affected
extremity and active ROM on unaffected
extremity.
10. Do neurovascular checks:
Skin color: Check the extremity and the
nail beds distal to the site of the fracture
for color. Pallor, discoloration, and
coldness indicate circulatory impairment HIP REPLACEMENT
Skin temperature: “hot spots” (areas
warm to touch) or any elevation of AVOIDING HIP DISLOCATION AFTER
temperature must be noted, documented REPLACEMENT SURGERY
and reported needed until 4 months after surgery
Sensation: Check for any diminished or 1. Maintain abduction of the affected leg at all
absent sensation or for numbness or times with abductor splint or 2 pillows
tingling between legs.
Mobility: Check hand function by having 2. Prevent external rotation by placing
the patient try to hyperextend the thumb trochanter rolls along hip.
or wrist, oppose the thumb and little 3. Use abductor splint or 2 pillows when turning
finger, and adduct all fingers. Check or lying on side.
function of the foot by having the patient 4. Keep the knees apart at all times.
5. Put a pillow between the legs when sleeping. Providing activity to the client decreases
6. Never cross the legs when seated. The knees phantom limb pain
should be lower than the hip. Stump desensitization by kneading massage
7. Avoid bending forward when seated in a brings relief
chair. Hip should not bend more than 90˚ 2. If prescribed, during the first 24 hours,
8. Do not elevate the head of the bed more elevate the foot of the bed to reduce edema;
than 60°. then keep the bed flat to prevent hip flexion
9. Avoid bending forward to pick up an object contractures
on the floor. 3. Do not elevate the stump itself but raise the
10. Use a high-seated chair and a raised toilet entire foot of the bed because elevation can
seat. cause flexion contracture of the hip joint.
11. Do not flex the hip to put on clothing such as 4. After 24 and 48 hours postoperatively,
pants, stockings, socks, or shoes. position the client prone for 20-30 minutes 2-
12. For use of the fracture bedpan, flex the 3x/day if prescribed, to stretch the muscles
unaffected hip and use the trapeze to lift the and prevent flexion contractures of hip
pelvis onto the bed pan. Never flex the 5. In the prone position, place a pillow under
affected hip. the abdomen and stump and keep the legs
13. Do not sleep on the affected extremity. close together to prevent abduction
14. Affected leg should not cross the center of 6. Maintain application of an Ace wrap or elastic
the body. stump shrinker
15. Affected leg should not turn inward while Wrap from distal to proximal
lying down. If it falls off, nurse must immediately wrap
F If prosthesis becomes dislocated, the residual limb to prevent severe edema
immediately notify the surgeon to reduce 7. Wash the stump with mild soap and water
and stabilize hip promptly to prevent and apply lanolin to the skin if prescribed
circulatory and nerve damage. 8. Massage the skin toward the suture line to
increase circulation
9. Encourage the client to look at the stump
SIGNS OF DISLOCATION OF
10. Encourage verbalization regarding loss of the
PROSTHESIS body part
1. Popping sensation of the hip.
2. Pain and swelling at the groin. Above the Knee Amputation
3. Shortening of the affected leg. 1. prevent edema – ace wrap
4. Loss of function of the affected leg. 2. do not allow the stump to hang over the
5. Abnormal internal or external rotation of the edge of the bed – prevent flexion
affected leg. contractures
3. do not allow the client to sit for long periods
of time, to prevent contractures
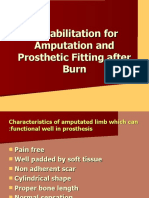
Care for Clients after Limb Amputation Below the Knee Amputation
1. Evaluate for phantom limb sensation and 1. Prevent internal or external rotation of the
pain; explain sensation and pain to the client, limb
and medicate the client as prescribed.
2. Place a sandbag or rolled towel along the
outside of the thigh to prevent rotation
Note: A large tourniquet in plain sight at bedside
must be on hand for hemorrhage
You might also like
- Ortho Supplemental NotesDocument6 pagesOrtho Supplemental Notestanya merdeNo ratings yet
- 1 CastDocument47 pages1 CastLuayon FrancisNo ratings yet
- TractionDocument16 pagesTractionMaulina AyuNo ratings yet
- Romero, Deinielle Ingird M. (BST Assignment 2)Document14 pagesRomero, Deinielle Ingird M. (BST Assignment 2)Deinielle Magdangal RomeroNo ratings yet
- Buck Docbuck Docbuck Docbuck Docbuck DocbuckDocument7 pagesBuck Docbuck Docbuck Docbuck Docbuck DocbucksabisiNo ratings yet
- TRACTIONSDocument29 pagesTRACTIONSRoeder CuerdaNo ratings yet
- Splints and Tractions in OrthopaedicsDocument56 pagesSplints and Tractions in OrthopaedicsNinaNo ratings yet
- Fracture MegDocument3 pagesFracture MegJhonny pingolNo ratings yet
- Skeletal and Skin TractionDocument38 pagesSkeletal and Skin TractionCORROS JASMIN MARIENo ratings yet
- Care of Patients With Traction NewDocument17 pagesCare of Patients With Traction Newjohnpantinople100% (18)
- NCP Self Care DeficitDocument15 pagesNCP Self Care DeficitSkye M. PetersNo ratings yet
- Kin Traction - Lower Extremity: MethodDocument11 pagesKin Traction - Lower Extremity: MethodMary Joy AntolinNo ratings yet
- TRACTIONDocument10 pagesTRACTIONKimberly SungaNo ratings yet
- Orthopedic NursingDocument2 pagesOrthopedic NursingMichelle TamorNo ratings yet
- Traction MethodsDocument11 pagesTraction MethodsalcaponeNo ratings yet
- Traction 9 PDF FreeDocument22 pagesTraction 9 PDF FreeJa DimasNo ratings yet
- Ortho AssignmentDocument18 pagesOrtho AssignmentSean Derick Cariño MercadoNo ratings yet
- Care of Patients With TractionDocument25 pagesCare of Patients With Tractionmftaganas100% (1)
- Types of Traction An CareDocument1 pageTypes of Traction An CarePrincess Faniega SugatonNo ratings yet
- TractionDocument22 pagesTraction紅玉練67% (3)
- Traction, Etc...... IDocument12 pagesTraction, Etc...... IJolo Q. Bilaos67% (3)
- TractionDocument11 pagesTractionDenalyn Ann TormoNo ratings yet
- TractionDocument20 pagesTractionCharinelle MolinaNo ratings yet
- 3.1 AmputationDocument4 pages3.1 AmputationDiana CalderonNo ratings yet
- TractionDocument4 pagesTractionGly MtgNo ratings yet
- Skeletal and Skin TractionDocument16 pagesSkeletal and Skin TractionJam Corros100% (2)
- Practical Splints and Slings - BCCH Emergency Department Resource PackDocument7 pagesPractical Splints and Slings - BCCH Emergency Department Resource PackMuhammad asif samiNo ratings yet
- Musculoskeletal Care ModalitiesDocument53 pagesMusculoskeletal Care ModalitiesJona Kristin EnclunaNo ratings yet
- An Orthopedic Treatment That Involves Placing On A Limb, Bone or Muscle Group Using Variety ofDocument22 pagesAn Orthopedic Treatment That Involves Placing On A Limb, Bone or Muscle Group Using Variety oflemuel_que100% (2)
- Orthopedic Nursing: TractionDocument2 pagesOrthopedic Nursing: TractionGhee EvangelistaNo ratings yet
- UntitledDocument5 pagesUntitledHUTALLA CezanneNo ratings yet
- TractionDocument14 pagesTractionRukshana Balakrishnan100% (1)
- Rehab. Following AmputationDocument27 pagesRehab. Following Amputationyosra adamNo ratings yet
- Types of Traction An CareDocument1 pageTypes of Traction An CarePrincess Faniega SugatonNo ratings yet
- Positioning ClientsDocument12 pagesPositioning ClientsGrace UyNo ratings yet
- Rangeen ChandranDocument40 pagesRangeen Chandranabhi2871995No ratings yet
- Slings - SprainsDocument1 pageSlings - Sprainsxiled59546No ratings yet
- Name: Bontilao, Jimnah Rhodrick M. Level: 3-B Instructor in Charge: MRS. AISSA CARLIT Date Materials Checked: Date PerformedDocument7 pagesName: Bontilao, Jimnah Rhodrick M. Level: 3-B Instructor in Charge: MRS. AISSA CARLIT Date Materials Checked: Date PerformedJimnah Rhodrick BontilaoNo ratings yet
- Ortho LecDocument7 pagesOrtho LecKemmy GarciaNo ratings yet
- General Care of Patients With TractionDocument2 pagesGeneral Care of Patients With TractionRebizz Bizz100% (1)
- Achilles Mid Substance Speedbridge Rehab Guidelines CompressedDocument11 pagesAchilles Mid Substance Speedbridge Rehab Guidelines CompressedRAUL8609No ratings yet
- Casts N TractionDocument3 pagesCasts N Tractionkatmarie14344100% (1)
- Traction: Presented By: Kristine Irish C. Almonte Tricia Nicole AlimatoDocument26 pagesTraction: Presented By: Kristine Irish C. Almonte Tricia Nicole AlimatoAlex Delos SantosNo ratings yet
- Balance Skeletal Traction. BST ProcedureDocument4 pagesBalance Skeletal Traction. BST Procedurehannjazz80% (10)
- Proper Patient PositioningDocument40 pagesProper Patient Positioningdagsimarifel26No ratings yet
- SplintsDocument16 pagesSplintsShini SimonNo ratings yet
- Adm Traction PDFDocument10 pagesAdm Traction PDFbitha p bNo ratings yet
- CASTINGDocument44 pagesCASTINGMaria Sofia Stephanie SatoriNo ratings yet
- Tractions in OrthopaedicsDocument132 pagesTractions in Orthopaedicssiddhartha100% (1)
- 3 Modalities (Traction, Fixator and Surgery)Document57 pages3 Modalities (Traction, Fixator and Surgery)Maria Lynne ParambitaNo ratings yet
- PT Guidelines For Ankle SprainDocument5 pagesPT Guidelines For Ankle SprainKirti GunjikarNo ratings yet
- Traction in Orthopaedics - Mus'Document72 pagesTraction in Orthopaedics - Mus'Muslihah Zainon100% (1)
- Musculoskeletal DisordersDocument8 pagesMusculoskeletal DisordersMode Devi Publising IncorporatedNo ratings yet
- Balance Skeletal Traction ApplicationDocument6 pagesBalance Skeletal Traction ApplicationAia JavierNo ratings yet
- Activation:: Lateral Crab WalkDocument13 pagesActivation:: Lateral Crab WalkClaudia DoroteoNo ratings yet
- Use of Different Types of Comfort/Support DevicesDocument20 pagesUse of Different Types of Comfort/Support DevicesConvalescent Nursing HomeNo ratings yet
- Chapter 17 VocabularyDocument3 pagesChapter 17 Vocabularymph440No ratings yet
- Traction in ORTHOPAEDICSDocument16 pagesTraction in ORTHOPAEDICSJuswa ViasonNo ratings yet
- Regaining Bladder Control: For Incontinence on Exertion or Following Pelvic SurgeryFrom EverandRegaining Bladder Control: For Incontinence on Exertion or Following Pelvic SurgeryNo ratings yet
- Reviewer - 1st LEDocument68 pagesReviewer - 1st LEMARIA ANGELIKA DEL ROSARIONo ratings yet
- Care of Mother, Child at Risk or With Problems (Acute and Chronic) NURS-10Document30 pagesCare of Mother, Child at Risk or With Problems (Acute and Chronic) NURS-10MARIA ANGELIKA DEL ROSARIONo ratings yet
- Case ScenarioDocument2 pagesCase ScenarioMARIA ANGELIKA DEL ROSARIONo ratings yet
- Competitive AnalysisDocument1 pageCompetitive AnalysisMARIA ANGELIKA DEL ROSARIONo ratings yet
- 3107en Contempt of Court in Family Law Cases The BasicsDocument8 pages3107en Contempt of Court in Family Law Cases The BasicsJason Howard100% (1)
- Math Assignment 1Document5 pagesMath Assignment 1Jeric SalasNo ratings yet
- Holstein B Cell Lecture 11-13-14Document47 pagesHolstein B Cell Lecture 11-13-14Alex DennisNo ratings yet
- USH 1.05 HonorsDocument7 pagesUSH 1.05 HonorsAubrey HovanNo ratings yet
- Mill Power SAG MillsDocument5 pagesMill Power SAG MillsRolando QuispeNo ratings yet
- ATP Bugayong AgencyDocument6 pagesATP Bugayong AgencyIrvy LongnoNo ratings yet
- EnglishDocument76 pagesEnglishTak ProNo ratings yet
- Short Corporations OutlineDocument39 pagesShort Corporations OutlineRosie BrownNo ratings yet
- Section A: CLASS IX (2019-20) Social Science (Code 087) Sample Paper-5Document8 pagesSection A: CLASS IX (2019-20) Social Science (Code 087) Sample Paper-5Harish LungeNo ratings yet
- Distance Learning BrochureDocument8 pagesDistance Learning BrochurecaphilNo ratings yet
- Be Lab WriteupDocument8 pagesBe Lab WriteupRachel BeningtonNo ratings yet
- Act 518 National Land Code (Penang & Malacca Titles) 1963Document145 pagesAct 518 National Land Code (Penang & Malacca Titles) 1963Raymond ChanNo ratings yet
- Application - For - Adjunct Faculty - COEPDocument7 pagesApplication - For - Adjunct Faculty - COEPSwapnilMahajanNo ratings yet
- Liste Provizorii PompieriDocument11 pagesListe Provizorii Pompieridica1041No ratings yet
- FCE Unit 2Document9 pagesFCE Unit 2Ana H S0% (1)
- MedievalPeriod PowerPointDocument25 pagesMedievalPeriod PowerPointmarina guevaraNo ratings yet
- Lauren Gantz On - The Palm Wine Drinkard - E3W Review of BooksDocument2 pagesLauren Gantz On - The Palm Wine Drinkard - E3W Review of BooksjayasriniNo ratings yet
- 5 Bivariate Statistics - P1 - QPDocument7 pages5 Bivariate Statistics - P1 - QPSarah HilyNo ratings yet
- RA 8371 Key PointsDocument6 pagesRA 8371 Key PointsKristine DiamanteNo ratings yet
- 09 Revelation PPTDocument16 pages09 Revelation PPTr_mukuyuNo ratings yet
- Endodontic-Periodontal Lesion: A Two-Way Traffic: Dr. Anindya Priya Saha, Dr. Anindya Chakraborty and Dr. Sananda SahaDocument6 pagesEndodontic-Periodontal Lesion: A Two-Way Traffic: Dr. Anindya Priya Saha, Dr. Anindya Chakraborty and Dr. Sananda Sahanovia chantikaNo ratings yet
- Julius Klaproth: His Life and Works With Special Emphasis On Japan Hartmut Walravens, BerlinDocument15 pagesJulius Klaproth: His Life and Works With Special Emphasis On Japan Hartmut Walravens, BerlinSarbu Ana100% (1)
- 2016 03 31 Basa Pilipinas Quarter 3 Grade 1 English Teacher's Guide (Second Edition) PDFDocument186 pages2016 03 31 Basa Pilipinas Quarter 3 Grade 1 English Teacher's Guide (Second Edition) PDFIris SamonteNo ratings yet
- Cost Based AnalysisDocument14 pagesCost Based AnalysisAyesha KashaNo ratings yet
- Chapter Two Relations and Functions 2.1. Relations A Relation Is Used To Describe Certain Properties of Things. That Way, Certain ThingsDocument27 pagesChapter Two Relations and Functions 2.1. Relations A Relation Is Used To Describe Certain Properties of Things. That Way, Certain ThingsHaria BitalangisNo ratings yet
- SSL VPN For Remote Users - Fortinet CookbookDocument12 pagesSSL VPN For Remote Users - Fortinet CookbookJhonnySinatraNo ratings yet
- Nutrition Presentation 2021-1Document14 pagesNutrition Presentation 2021-1Paljesza may PamateNo ratings yet
- Discipline and Ideas in Applied Social Science Quarter 1 - Module 5: The Clientele and Audiences in Counseling and The Counseling ProcessesDocument17 pagesDiscipline and Ideas in Applied Social Science Quarter 1 - Module 5: The Clientele and Audiences in Counseling and The Counseling ProcessesBenilda Pensica SevillaNo ratings yet
- Chararacteristics of LanguageDocument2 pagesChararacteristics of LanguageMariz EntodNo ratings yet
- Morality and Abstract ThinkingDocument16 pagesMorality and Abstract ThinkingNzugu HoffmanNo ratings yet