Professional Documents
Culture Documents
v13n3 CPG Update
Uploaded by
edfZSEADFsfsafafOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
v13n3 CPG Update
Uploaded by
edfZSEADFsfsafafCopyright:
Available Formats
CPG UPDATE
Management of asthma in adults in primary care
Ban AYL, Omar A, Chong LY, Lockman H, Ida Zaliza ZA, Ali IAH, Jaya M, Leong SW,
Mazapuspavina MY, Yusof MAM, Zim MAM, Nor Azila MI, Jamal SM, Yoon CK, Malek
Abdol Hamid ZI
Ban AYL, Omar A, Chong LY, Lockman H, et al. Clinical Practice Guidelines Management of asthma in adults. Management of asthma in adults
in primary care. Malays Fam Physician. 2018;13(3); 20–26.
Abstract
Keywords:
asthma, acute asthma, stable Asthma is a chronic inflammatory disease of the airway which is often misdiagnosed and
asthma, written asthma action undertreated. Early diagnosis and vigilant asthma control are crucial to preventing permanent
plan, asthma control airway damage, improving quality of life and reducing healthcare burdens. The key approaches
to asthma management should include patient empowerment through health education and self-
management and, an effective patient-healthcare provider partnership.
Authors:
Introduction Diagnosis
Andrea Ban Yu-lin
(Corresponding author) Asthma is a common medical condition in The diagnosis of asthma is based on a combination
Mb.Bch BAO (Ireland) adults, with a prevalence of 4.5% in Malaysia, of clinical features suggestive of reversible airway
MMed internal Medicine (UKM) based on the National Health and Morbidity obstruction supported by investigations, as
Jabatan Perubatan, Pusat Survey 2006. It is an inflammatory disease of shown in Tables 2 and 3. A response to treatment
PerubatanUKM, Malaysia the airway which is triggered by external stimuli may support the diagnosis; however, a lack of
Email: andreaban@gmail.com in genetically-predisposed individuals, leading response does not exclude asthma.
to mucus secretion, bronchoconstriction and
airway narrowing. Table 2. Clinical features of asthma
Azza Omar
Common • Cough
MD (USM) The most common symptom is a chronic cough. symptoms • Wheeze
MMed Internal Medicine (USM) Misdiagnoses or underdiagnoses cause persistent • Chest tightness
Jabatan Perubatan, Hospital Raja airway inflammation, airway remodeling, and • Shortness of breath
Perempuan Zainab II subsequently, fixed airway obstruction. Therefore,
Malaysia it is important for healthcare professionals to Symptom • Episodic symptoms
variability • Diurnal symptoms
diagnose and manage asthma confidently. • Symptoms after/during
exercise
Chong Li Yin Risk Factors
B. Pharm (UKM) Triggers • Common cold (viral infection)
16, Jalan Jelok Ria 7, Taman SriJelok Asthma is a multifactorial disease brought about • Allergens, e.g. dust mites, pets
• Cold weather
43000 Kajang, Selangor by various familial and environmental influences, • Irritants
Malaysia as seen in Table 1 below: • smoke
• haze
Table 1. Risk factors for asthma • strong smells, i.e.
Hilmi Lockman Genetic factors perfumes, cleaning
MB, BCh, BAO (Ireland) solutions
CCT(UK) (Respiratory & Internal Environmental factors • exhaust fumes
Medicine), Respiratory Clinic Prince • Smoking
Court Medical Centre
• Air pollution History • Eczema
• Paint of atopy • Allergic rhinitis
Malaysia
• Pesticides
Family • Asthma
Other risk factors/co-morbidities history • Allergic rhinitis
• Eczema
• Overweight or obese
• Gastroesophageal reflux disease
• Nasal blockage, rhinorrhea, and allergic Physical • Eczema
examination • Use of accessory muscles
rhinitis • Hyperinflation
• Elevated fractional exhaled nitric oxide and • Audible wheeze
positive skin prick test • Ronchi on auscultation
20 Malaysian Family Physician 2018; Volume 13, Number 3
CPG UPDATE
Ida Zaliza Zainol Abidin Table 3. Investigations for asthma
MD UKM Investigation Description
MMed (Emergency) USM
Demonstration of airway obstruction
Jabatan Kecemasan & Trauma
Hospital Tuanku Fauziah
Spirometry • A FEV1 (forced expiratory volume in 1 second)/FVC (forced vital
capacity) ratio of <70% is a positive test for obstructive airway disease.
Malaysia
Demonstration of airway obstruction variability
Bronchodilator reversibility • An improvement in FEV1 of ≥12% AND ≥200 ml is a positive
bronchodilator reversibility test.
Irfhan Ali Hyder Ali
MBBS (Malaya) MMed (Int Med) Other method • An increase in FEV1 >12% and >200 ml [or peak expiratory flow
(PEF) >20%] from baseline after four weeks on inhaled corticosteroids
33-11-3 Sri York Condominium (ICS) is a positive test. Patient must not have respiratory infections.
Halaman York 10450 George Town
Peak flow charting • Peak flow monitoring over 2 - 4 weeks.
Penang, Malaysia • Calculate mean variability. Daily diurnal PEF variability is calculated
from twice daily PEFs as [(day’s highest - day’s lowest)/mean of day’s
highest and lowest] and averaged over one week.
• Variability ≥20% or diurnal variation >15% on >3 days/week indicates
Jaya Muneswarao a positive test.
Ramadoo@Devudu
B.Biomed.Sc.(UKM), B.Pharm(USM- General Principles of Management • a regular medical review by healthcare
UCSI),M.Pharm(Clin Pharm) (USM) providers
School of Pharmaceutical Sciences The aims of management are to achieve good
Universiti Sains Malaysia asthma symptom control and minimise future A home nebuliser should be avoided, as it
Malaysia. risk of exacerbations. The partnership between leads to underestimation of the severity of an
the patients/caregivers and healthcare providers acute exacerbation of asthma.
is important in ensuring the success of the
Leong Swee Wei management. The patient’s preferences for Stable Asthma
MD(UKM), MRCP(UK) treatment, ability to use an inhaler correctly,
157, Taman Selatan, Leboh Tamarind, side effects and cost of medications should be Stable asthma is defined as the absence of
41200, Klang, Selangor. taken into consideration during the treatment symptoms, no limitations on activities and
Malaysia process. not requiring any relievers in the last four
weeks.
Asthma Self-Management
Mazapuspavina Md. Yasin a. Assessment of asthma control
MBBS (U.Malaya) MMed Fam Med The patient’s active participation is important
Malaya (U.Malaya) in asthma management. All patients should Asthma control can be assessed by using
Faculty of Medicine UiTM Selayang be made aware of the components of asthma Asthma Control Test (ACT) scores or asking
Campus, Malaysia self-management, which include: recommended questions, as shown in Table
4 below.
• self-monitoring of symptoms and/or PEF
Mohd Aminuddin Mohd Yusof • a written asthma action plan (WAAP) for
MD (UKM), MPH (Epid)(UM) optimisation of asthma control through
Cawangan Penilaian Teknologi self- adjustment of medications
Kesihatan, Bahagian Perkembangan
Perubatan, KKM Putrajaya Table 4. Assessment of asthma symptom control
Malaysia
Asthma symptom control Level of asthma symptom control
Well- Partly
In the past four weeks, has the patient had: Uncontrolled
controlled controlled
• Daytime asthma
symptoms more Yes No
than twice/week?
• Any night waking Yes No
due to asthma?
• Reliever needed for None of these 1 - 2 of these 3 - 4 of these
symptoms more Yes No
than twice/week?
• Any activity
limitation due to Yes No
asthma?
Malaysian Family Physician 2018; Volume 13, Number 3 21
CPG UPDATE
Mohd. Arif Mohd. Zim b. Assessment of the severity of future risks
MBBch BAO (Ire), MMed (Mal)
Fellowship Respiratory (Mal) Assessment of the risk factors for a poor asthma outcome is important in treatment adjustments
Fakulti Perubatan, Universiti Teknologi and prediction of exacerbation. Refer to Table 5 for more details.
MARA, Kampus Selayang
Malaysia Table 5. Investigations for asthma
Email: firadhom@yahoo.com
Risk factors for poor asthma outcome
Nor Azila Mohd. Isa
MBBS UM, MMed Fam Medicine • Assess risk factors at diagnosis and periodically (1 - 2 years)
(UKM) • Measure FEV1 at the start of treatment and periodically
PT 22097, JalanKolej 5, Desa Kolej,
71800 Putra Nilai. N.Sembilan
Malaysia Independent risk factors Having one or more of these risk factors increases the risk of
Email: iradit@yahoo.com exacerbations, even if symptoms are well-controlled:
• Uncontrolled asthma symptoms
• ICS not prescribed, poor ICS adherence, incorrect inhaler
Shamsuriani Md. Jamal technique
MBBS (Adelaide), Masters of • High short-acting β2-agonists (SABA) use
Emergency Medicine (UKM)
• Low FEV1, especially if <60% predicted
77, Jalan C10, Taman Melawati,
53100, Kuala Lumpur, Malaysia • Major psychological or socioeconomic problems
Email: suriazwa@gmail.com • Exposures: smoking; allergen exposure, if sensitised
• Co-morbidities: obesity, rhinosinusitis, confirmed food allergy
Yoon Chee Kin • Sputum or blood eosinophilia, elevated fractional exhaled nitric
oxide in allergic adults
MB BCH BAO (Ire), MRCP(UK)
1-2-21, Cascadia Apartment, • Pregnancy
Halaman Cantonment, 10350 • Ever being intubated or in intensive care for asthma
Pulau Pinang, Malaysia
• Having ≥1 severe exacerbations in the last 12 months
Email: yooncheekin@gmail.com
Risk factors for fixed airflow • Lack of ICS treatment
Zul Imran Malek Abdol Hamid limitation
B.MedSci.MB, BCh BaO (Ireland)
• Exposure to tobacco smoke
Masters of Emergency Medicine • Noxious chemical or occupational exposures
(UKM)
• Low FEV1
55, Jalan Mega, Taman Mega, Jalan
Abd Rahman 84150 Parit Jawa
• Chronic mucus hypersecretion
Muar, Johor, Malaysia • Sputum or blood eosinophilia
Email: drzulimran@gmail.com
Risk factors for medication • Systemic: frequent oral corticosteroids (OCS); long-term, high-dose
side effect ICS; taking P450 inhibitors, e.g. itraconazole, ketoconazole, etc.
• Local: high-dose or potent ICS, poor inhaler technique
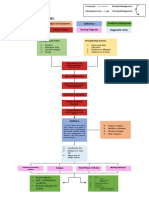
c. Treatment
The goal of asthma treatment is to achieve and maintain symptom control. This is done using a
stepwise approach, as shown in Figure 1. Any of the following issues should be addressed before
considering treatment adjustment:
• inhaler technique
• adherence to medications
• modifiable risk factors
• presence of co-morbidities
22 Malaysian Family Physician 2018; Volume 13, Number 3
CPG UPDATE
Figure 1. Stepwise treatment ladder in stable asthma
• Reliever o Leukotriene receptor antagonists as
add-on can be beneficial in patients
Inhaled SABA are the reliever of choice with concomitant seasonal allergic
in stable asthma. Oral SABA should be rhinitis and asthma.
avoided in asthma due to their side effects. o The soft-mist inhaler tiotropium may
be used as add-on therapy in patients
A low dose of budesonide/formoterol or with asthma that is not well-controlled
beclometasone/formoterol may be used as a with medium- or high-dose ICS.
single inhalant for maintenance and reliever o Patients with difficult-to-control
therapy in moderate to severe asthma. asthma should be referred to a
respiratory physician.
Inhaled long-acting β2-agonists without
ICS should not be used in reliever Non-Pharmacological Treatment
monotherapy in stable asthma.
Non-pharmacological treatments may improve
• Controller (in addition to as-needed symptom control and/or reduce future risk of
reliever inhaler) asthma exacerbation. This includes smoking
cessation, vaccination and weight loss
o ICS are the preferred controller therapy management.
in asthma.
o Initiation of ICS should not be delayed Acute Exacerbation of Asthma
in symptomatic asthma.
o Low-dose ICS should be considered in Acute exacerbation of asthma is defined as
steroid-naïve, symptomatic asthma. a progressive or sudden onset of worsening
o Long-acting β2-agonists should not symptoms. Status asthmaticus is a life-
be used as controller monotherapy threatening and medical emergency situation.
without ICS in asthma.
Malaysian Family Physician 2018; Volume 13, Number 3 23
CPG UPDATE
a. Assessment of severity and management
Rapid clinical assessment of severity (refer to Table 6) should be performed in all acute
exacerbation of asthma. Treatment should be initiated immediately based on the severity of the
asthma (refer to Algorithm 1).
Table 6. Level of severity of acute exacerbation of asthma
Severity Clinical features Clinical parameters
Mild to moderate • Speaks in phrases • Respiratory Rate (RR): 20 - 30/min
• Sits up • Pulse rate (PR): 100 - 120/min
• Not agitated • O2 saturation: 90 - 95%
• PEF: >50% predicted or best
Severe • Speaks in words • RR: >30/min
• Sits forward • PR: >120/min
• Agitated • O2: Saturation <90%
• Accessory muscles used • PEF: <50% predicted or best
Life-threatening Severe asthma with ANY OF THE FOLLOWING:
• Drowsy • PEF: <33%
• Confused • PaO2: <60 mmHg
• Exhaustion • Normal (30 - 45 mmHg) or raised
• Cyanosis PaCO2
• Hypotension
• Silent chest
• Poor respiratory effort
In acute exacerbation of asthma, inhaled β2-agonists are the first-line treatment.
• In mild to moderate exacerbations, a pressurised metered dose inhaler with a spacer is the
preferred method of delivery.
• In severe and life-threatening exacerbations, continuous delivery of nebulised oxygen-driven
β2-agonists should be used.
Systemic corticosteroids should be given to all patients with acute exacerbation of asthma. They
should be continued for 5 to 7 days. Asthma patients prescribed OCS should continue their
regular ICS.
b. Criteria for admission/discharge
All patients with severe, life-threatening asthma and those with PEF<75% personal best or
predicted one hour after initial treatment should be admitted. The following factors may be
considered for admission:
• persistent symptoms
• pregnancy
• previous near-fatal asthma attack
• deteriorating PEF
• living alone/socially isolated
• persisting or worsening hypoxia
• psychological problems
• exhaustion
• physical disability or learning difficulties
• drowsiness, confusion or altered conscious state
• asthma attack despite recent adequate steroid treatment
• respiratory arrest
Patients with resolution of symptoms and PEF >75% personal best or predicted one hour after
initial treatment may be discharged home with a WAAP.
24 Malaysian Family Physician 2018; Volume 13, Number 3
CPG UPDATE
Algorithm 1. Management of acute asthma in primary care
INITIAL ASSESSMENT
• Speaks in phrases • Speaks in words • Drowsy
• Sits up • Sits forward • Confused
• Not agitated • Agitated • Exhausted
• Accessory muscles used • Cyanosis
• Poor respiratory effort
MILD TO MODERATE SEVERE LIFE-THREATENING
FURTHER ASSESSMENT
• RR: 20 - 30/min • RR: >30/min • Features of severe asthma
• PR: 100 - 120/min • PR: >120/min and any of the following:
o PaO2: <60 mmHg
• SpO2: 90 - 95% • SpO2: Saturation <90% o Normal or ↑ PaCO2
PEF: >50% predicted or PEF: ≤50% predicted or o Hypotension
best best o Silent chest
o PEF: <33%
INITIAL MANAGEMENT
• Maintain SpO2 >94% • Maintain SpO2 >94% TRANSFER TO NEAREST
• Administer β2-agonist HOSPITAL IMMEDIATELY
• β2-agonist pMDI While waiting for transfer, do
preferable with spacer (4 (salbutamol 2.5 - 5 mg)
via oxygen-driven the following:
puffs up to a maximum of
10 puffs) or nebuliser nebuliser, repeat every • Maintain SpO2 >94%
(salbutamol 5 mg); repeat 20 minutes for 1 hour • Administer β2-agonist
every 20 minutes for 1 • Administer ipratropium (salbutamol 5 mg) and
hour bromide nebuliser 0.5 ipratropium bromide 0.5
• Prednisolone 1 mg/kg with mg every 4 - 6 hours mg via oxygen-driven
maximum of 50 mg • Administer IV nebuliser
• Continue or increase hydrocortisone 200 mg • Repeat β2-agonist
usual treatment or prednisolone 1 mg/kg nebuliser every 20
with maximum of 50 mg minutes and ipratropium
• If no improvement, bromide every 4 - 6
MONITOR progress: refer to hospital hours
• RR OR SpO2 (if available) • Administer IV
• PR No hydrocortisone 200 mg
• Assess symptoms & PEF improvement or prednisolone 1 mg/kg
o Symptoms improve with maximum of 50 mg
o PEF >50%
Improvement
DISCHARGE HOSPITAL ADMISSION CONTINUE TREATMENT
• WAAP • Continue treatment AND MONITOR
PROGRESS throughout
• Continue oral during transfer
transport (SpO2, RR, PR and
prednisolone (5 - 7 days)
BP)
• Increase usual treatment
(refer to Algorithm 1 on
Stepwise Treatment
Ladder)
• Ensure follow-up within 1-
2 weeks 7
Malaysian Family Physician 2018; Volume 13, Number 3 25
CPG UPDATE
Referral Acknowledgement
A referral to a specialist with experience in Details of the evidence supporting the above
asthma should be made for asthma patients statements can be found in the Clinical
with the following conditions: Practice Guidelines on the Management
of Asthma in Adults 2017, available on
• diagnosis of asthma is not clear the following websites: Ministry of Health
• suspected occupational asthma Malaysia: http://www.moh.gov.my and
• poor response to asthma treatment Academy of Medicine: http://www.acadmed.
• persistent use of high-dose ICS without org.my. Corresponding organisation: CPG
being able to taper off Secretariat, Health Technology Assessment
• symptoms remain uncontrolled with Section, Medical Development Division,
persistent use of high-dose ICS Ministry of Health Malaysia, contactable at
• persistent symptoms despite continuous htamalaysia@moh.gov.my
use of moderate- to high-dose ICS
combined with LABA
• severe/life-threatening asthma exacerbations
• asthma in pregnancy
• asthma with multiple co-morbidities
26 Malaysian Family Physician 2018; Volume 13, Number 3
You might also like
- Bronchial AsthmaDocument29 pagesBronchial AsthmaDrShaheen100% (5)
- COPD-and-Asthma - Lachica, RN, MDDocument57 pagesCOPD-and-Asthma - Lachica, RN, MDbekbekk cabahugNo ratings yet
- Asthma Diagnosis and TreatmentDocument16 pagesAsthma Diagnosis and TreatmentRabina PantaNo ratings yet
- Diagnosing and Managing Childhood AsthmaDocument12 pagesDiagnosing and Managing Childhood Asthmaturky hadiNo ratings yet
- Pneumonia in COVID -19 ContextDocument70 pagesPneumonia in COVID -19 ContextdrshekarforyouNo ratings yet
- Bronchial AsthmaDocument22 pagesBronchial AsthmaAdhithiayan ANo ratings yet
- MED - Finals 1.5 - Asthma PDFDocument12 pagesMED - Finals 1.5 - Asthma PDFYestin Reece Corpus ArcegaNo ratings yet
- Infectious Disorder: Prepared By: Dellero, Sarah Joy P. BSN3-DDocument19 pagesInfectious Disorder: Prepared By: Dellero, Sarah Joy P. BSN3-Dngoto88No ratings yet
- Brochial Asthma EditedDocument40 pagesBrochial Asthma EditedMituran IshwarNo ratings yet
- Asma Okupasi (DR - Retno)Document40 pagesAsma Okupasi (DR - Retno)rft akbr0% (1)
- Anaphylaxis TalkDocument60 pagesAnaphylaxis TalkAqib NabiNo ratings yet
- Asthma: DR Mayank Kumar MishraDocument51 pagesAsthma: DR Mayank Kumar MishraMukesh ThakurNo ratings yet
- Asthma & Copd Cme 2 FinalDocument51 pagesAsthma & Copd Cme 2 Finaldrewstark496No ratings yet
- AsthmaDocument41 pagesAsthmaMuhammad AdnanNo ratings yet
- Allergic Rhinitis: Diagnosis and TreatmentDocument59 pagesAllergic Rhinitis: Diagnosis and TreatmentYibeltalNo ratings yet
- Aspirin-Exacerbated Respiratory DiseaseDocument64 pagesAspirin-Exacerbated Respiratory DiseaseVenkatesh PaiNo ratings yet
- Drugs Used in The Treatment of Bronchial Asthma: Ayesha IdrissDocument76 pagesDrugs Used in The Treatment of Bronchial Asthma: Ayesha Idrissmatchees-gone rogueNo ratings yet
- Immunology TA v.01 Paramita Mycomments v.01Document80 pagesImmunology TA v.01 Paramita Mycomments v.01Miral Sandipbhai MehtaNo ratings yet
- DraggedDocument39 pagesDraggednadiahNo ratings yet
- CopdDocument17 pagesCopdNAMREENNo ratings yet
- Bronchial Asthma 3rd YearDocument50 pagesBronchial Asthma 3rd YearArmoured SpartanNo ratings yet
- Managing Asthma PatientsDocument2 pagesManaging Asthma PatientsBelle MakinanoNo ratings yet
- AsthmaDocument61 pagesAsthmaYohannes hailuNo ratings yet
- Allergic Rhinitis & Vasomotor Rhinitis: Dr. Ritesh Mahajan ENT Consultant GMC, KathuaDocument70 pagesAllergic Rhinitis & Vasomotor Rhinitis: Dr. Ritesh Mahajan ENT Consultant GMC, Kathuamanoj kumarNo ratings yet
- How Should One Investigate A Chronic CoughDocument3 pagesHow Should One Investigate A Chronic Coughtsiko111No ratings yet
- Bronchial Asthma - HandoutDocument3 pagesBronchial Asthma - HandoutkimerellaNo ratings yet
- Resp PCPADocument47 pagesResp PCPAPatrick MathewNo ratings yet
- Family Medicine: Asthma (GINA Guidelines 2012) : V. ManagementDocument3 pagesFamily Medicine: Asthma (GINA Guidelines 2012) : V. ManagementamdylananNo ratings yet
- Dr. Retno Ariza, Sp. P. FCCPDocument40 pagesDr. Retno Ariza, Sp. P. FCCPKaren KuniyaNo ratings yet
- LP31 Health HazardsDocument7 pagesLP31 Health HazardsGlenn Fortades SalandananNo ratings yet
- NCM 112: Oxygen Exchange and Utilization: Bambam2017Document25 pagesNCM 112: Oxygen Exchange and Utilization: Bambam2017Alyssa Claire TumulakNo ratings yet
- COPD Guide: Causes, Symptoms, TreatmentDocument2 pagesCOPD Guide: Causes, Symptoms, TreatmentKdamnzNo ratings yet
- Anaphylaxis: Allergy, Asthma & Clinical ImmunologyDocument8 pagesAnaphylaxis: Allergy, Asthma & Clinical ImmunologyBabad BagusNo ratings yet
- Asthma: Presented Bygroup 1: A Robani Martina Fepep Suherman Alam Resi Wulansari Rizky Fauzi Triska OktarianiDocument11 pagesAsthma: Presented Bygroup 1: A Robani Martina Fepep Suherman Alam Resi Wulansari Rizky Fauzi Triska OktarianiTriska OktarianiNo ratings yet
- RhinitisDocument22 pagesRhinitisJo CanensNo ratings yet
- Who Aria 2008 YrDocument94 pagesWho Aria 2008 YrFairuz NazilahNo ratings yet
- 8 DF 25 H6 KD PTBR DJV 7 Od D1610768568Document42 pages8 DF 25 H6 KD PTBR DJV 7 Od D1610768568rhegi isdiara FairuzNo ratings yet
- AthmaDocument47 pagesAthmadrthanallaNo ratings yet
- Tata Laksana Rinitis Alergi Pada Dewasa FINALDocument27 pagesTata Laksana Rinitis Alergi Pada Dewasa FINALNikko Khairul DafaNo ratings yet
- COPD Pathophysiology, Assessment and Diagnosis GuideDocument20 pagesCOPD Pathophysiology, Assessment and Diagnosis GuideTony LeeNo ratings yet
- Allergic Rhinitis PathoDocument3 pagesAllergic Rhinitis PathoAce FabrigasNo ratings yet
- Ambulatory CareDocument6 pagesAmbulatory CareEvelyn LimNo ratings yet
- WR - Senior Paeds Notes 2nd Ed UPDATED JAN 2019 - Anggelos EditDocument223 pagesWR - Senior Paeds Notes 2nd Ed UPDATED JAN 2019 - Anggelos Editdale 99No ratings yet
- MED II 22.1 AsthmaDocument6 pagesMED II 22.1 AsthmayayayanizaNo ratings yet
- Asthma in Children: Dr. Vinia Rusli SpaDocument30 pagesAsthma in Children: Dr. Vinia Rusli SpaOlivia FatrinNo ratings yet
- AsthmaDocument4 pagesAsthmaIsabel CastilloNo ratings yet
- Bronchial AsthmaDocument20 pagesBronchial AsthmaJuliet De GuzmanNo ratings yet
- ACFrOgCoxAEPf B5bFXXj0n0ogZgNdJimPp0HP25fR0kWmUQfj5aodpDMX Y2yxgw FKGZR QuqtH7SZyDlG8F4JVDjQOuJN8At7iKpg7xji x2zqAMu YaQmBFHVDJ12jag4khHkNk5gAYOo25zDocument6 pagesACFrOgCoxAEPf B5bFXXj0n0ogZgNdJimPp0HP25fR0kWmUQfj5aodpDMX Y2yxgw FKGZR QuqtH7SZyDlG8F4JVDjQOuJN8At7iKpg7xji x2zqAMu YaQmBFHVDJ12jag4khHkNk5gAYOo25zRheeanne AmilasanNo ratings yet
- Pemicu 6 KGD AditDocument76 pagesPemicu 6 KGD AditAditya SuksmawanNo ratings yet
- Lecture 7-Non Infection Rhino Disorder-Dr. Kartono Sudarman, SP - THT-KL (K) (2021)Document31 pagesLecture 7-Non Infection Rhino Disorder-Dr. Kartono Sudarman, SP - THT-KL (K) (2021)PutriNo ratings yet
- (PULMO) - Asthma PDFDocument5 pages(PULMO) - Asthma PDFKeith LajotNo ratings yet
- Respiratory EmergenciesDocument58 pagesRespiratory EmergenciesDennis MiritiNo ratings yet
- Bronchial Asthma: West Visayas State University Medical Center - Department of PediatricsDocument9 pagesBronchial Asthma: West Visayas State University Medical Center - Department of PediatricsPGI Miayo, StephenNo ratings yet
- Concept Map March 11Document1 pageConcept Map March 11Dinah Rose VitorilloNo ratings yet
- Atopic Dermatitis, Allergic Rhinits, and Asthma: Tracie Kirkland, DNP, RN, ANP-BC, CPNPDocument19 pagesAtopic Dermatitis, Allergic Rhinits, and Asthma: Tracie Kirkland, DNP, RN, ANP-BC, CPNPNick flemmingNo ratings yet
- Asthma and COPDDocument79 pagesAsthma and COPDDawit g/kidanNo ratings yet
- WCS 015 - Shortness of Breath in A Construction Site Worker - Occupational Lung Diseases - Pulmonary Fibrosis - Workman's Compensation by DR DCL LamDocument60 pagesWCS 015 - Shortness of Breath in A Construction Site Worker - Occupational Lung Diseases - Pulmonary Fibrosis - Workman's Compensation by DR DCL LamJenniferFooNo ratings yet
- Anaphylaxis: Diagnosis and Management: Mja Practice Essentials - AllergyDocument7 pagesAnaphylaxis: Diagnosis and Management: Mja Practice Essentials - AllergyFran ramos ortegaNo ratings yet
- Asma Pada AnakDocument24 pagesAsma Pada AnaksevyarvintaNo ratings yet
- Fast Facts: Respiratory Allergies: Understand aeroallergens, improve treatment responseFrom EverandFast Facts: Respiratory Allergies: Understand aeroallergens, improve treatment responseNo ratings yet
- Pedia CardsDocument40 pagesPedia CardsKristine Marie Santos100% (1)
- Barley Grass Benefits for Diabetes Control and Detox SupportDocument4 pagesBarley Grass Benefits for Diabetes Control and Detox SupportGyelamagne EstradaNo ratings yet
- Allergic PDFDocument17 pagesAllergic PDFSiska HarapanNo ratings yet
- Open Airways Annual Report 2020Document2 pagesOpen Airways Annual Report 2020BernewsAdminNo ratings yet
- Respiratory Drugs Midterm ExamDocument10 pagesRespiratory Drugs Midterm ExamKevin VillaranteNo ratings yet
- Oms BookDocument292 pagesOms BookLUisNo ratings yet
- Understanding Pneumothorax PathophysiologyDocument8 pagesUnderstanding Pneumothorax PathophysiologyKyle FernandezNo ratings yet
- Jurnal - Rhinitis AlergiDocument8 pagesJurnal - Rhinitis AlergiRezky PutriNo ratings yet
- HSE From WeldingDocument7 pagesHSE From WeldingMichael RujuwaNo ratings yet
- 253 Complexes For Biomedis Trinity - DescriptionDocument74 pages253 Complexes For Biomedis Trinity - Descriptionjanhendrik4444100% (1)
- Rath in A MalaDocument187 pagesRath in A MalapgsbeNo ratings yet
- Asthma in Adults and AdolescentsDocument29 pagesAsthma in Adults and AdolescentsAbdullah Al ArifNo ratings yet
- Medical Surgical Nursing - RespiratoryDocument15 pagesMedical Surgical Nursing - RespiratoryChristian Esteves75% (4)
- DR Lila - Patient Preparation For Emergencies Surgeries - New 11012017Document37 pagesDR Lila - Patient Preparation For Emergencies Surgeries - New 11012017bloadyroar100% (1)
- Paediatric AsthmaDocument246 pagesPaediatric AsthmaOxana TurcuNo ratings yet
- HEENT Focused Exam Soap NoteDocument5 pagesHEENT Focused Exam Soap Noteariel sparkmanNo ratings yet
- Nursing Interventions for Effective Airway ManagementDocument2 pagesNursing Interventions for Effective Airway ManagementwaadNo ratings yet
- Homelessness: and Its Effects On ChildrenDocument16 pagesHomelessness: and Its Effects On ChildrenRagnar LothbrokNo ratings yet
- AsthmaDocument2 pagesAsthmaTuna AhsanNo ratings yet
- Evaluasi Kualitas Hidup Penderita Asma Di Kabupaten BelitungDocument8 pagesEvaluasi Kualitas Hidup Penderita Asma Di Kabupaten BelitungInanda DamantiaNo ratings yet
- 2022ABFM ITEMultChoiceDocument71 pages2022ABFM ITEMultChoiceMaryam FadahNo ratings yet
- Clean Air Outlook Economic Impact ReportDocument59 pagesClean Air Outlook Economic Impact ReportpablomartinezdiezNo ratings yet
- OB CH20 NotesDocument16 pagesOB CH20 NotesVeronica EscalanteNo ratings yet
- Effect of Particulate Matter On Human Health, Prevention, and Imaging Using Pet or SpectDocument13 pagesEffect of Particulate Matter On Human Health, Prevention, and Imaging Using Pet or SpectViet Bui DucNo ratings yet
- Buteyko Breathing Technique: A Golden Cure For AsthmaDocument9 pagesButeyko Breathing Technique: A Golden Cure For AsthmaGerry KrikhoffNo ratings yet
- AsthmaDocument12 pagesAsthmaKallu AnNo ratings yet
- Pediatric Nursing - Respiratory DisordersDocument9 pagesPediatric Nursing - Respiratory Disordershasan ahmdNo ratings yet
- MCN 2-Pedia-Clinical Scenario 6-RLE-PlanDocument3 pagesMCN 2-Pedia-Clinical Scenario 6-RLE-PlanMark oliver GonzalesNo ratings yet
- IspaDocument30 pagesIspahary anggoroNo ratings yet
- Onchial AsthmaDocument13 pagesOnchial Asthmaram krishna100% (1)