Professional Documents
Culture Documents
123418P 123120 Kim Crain
Uploaded by
Ankit BhatiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
123418P 123120 Kim Crain
Uploaded by
Ankit BhatiCopyright:
Available Formats
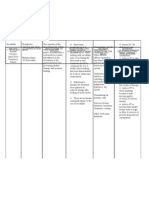
PROGRESS NOTE
PROVIDER NAME: SYDNEY DOWELL, A.P.R.N.
PATIENT: KIM CRAIN
DATE OF BIRTH: 03/12/1961
DATE OF EVALUATION: 12/31/2020
PLACE OF EVALUATION: Office
HISTORY OF PRESENT ILLNESS: Green nasal drainage for one month, bilateral
earaches. No fever. She does have tinnitus for a long time, but it does get worse when she
has a respiratory infection. She has not been taking vitamin D or amlodipine for a couple
of months. She does have a blood pressure monitor, but she has not checked it. She
occasionally does have edema and at that time she will take furosemide and potassium
p.r.n. She does have joint pain at multiple sites. The Celebrex does help. She has fainted
when she gets her blood drawn so she does not like to have test done.
MEDICAL (GENERAL) HISTORY
ALLERGIES: Reviewed.
PAST MEDICAL HISTORY: Reviewed.
IMMUNIZATIONS: Reviewed.
SOCIAL HISTORY: Reviewed.
FAMILY HISTORY: Reviewed.
REVIEW OF SYSTEMS:
GENERAL: No fever, chills.
CARDIOVASCULAR: No chest pain.
RESPIRATORY: No difficulty breathing.
GI: No abdominal pain, nausea, vomiting.
GU: No difficulty urinating.
INTEGUMENTARY: No rash.
PSYCHIATRIC: No depression.
PHYSICAL EXAMINATION:
VITAL SIGNS: ______
GENERAL APPEARANCE: Well developed, well nourished, and cooperative.
No acute distress.
PROVIDER NAME: SYDNEY DOWELL, A.P.R.N. Page 2
PATIENT: KIM CRAIN
DATE OF BIRTH: 03/12/1961
DATE OF EVALUATION: 12/31/2020
PLACE OF EVALUATION: Office
HEENT: Head normocephalic. Conjunctiva, sclera, and lids
unremarkable.
CARDIOVASCULAR: Heart regular, rate and rhythm. Normal S1 and S2,
No edema.
RESPIRATORY: Respiratory effort unremarkable. Respiratory rate
and pattern normal. Lungs clear to auscultation.
MUSCULOSKELETAL: Normal gait.
INTEGUMENTARY: Skin warm and dry.
PSYCHIATRIC: Alert and oriented to person, place, time, mood, and
affect appropriate for situation. Judgment and
insight normal. Normal attention and concentration.
ASSESSMENT:
1. Sinusitis
2. Pain, joint, multiple sites
3. Vitamin D deficiency
4. HLD (hyperlipidemia)
5. Hypertension
6. Tinnitus
7. Edema
8. Medication refill
9. History of Barrett's esophagus
10. Encounter for long-term current use of medication
11. NPDx Abn react-blood sampling
12. Influenza vaccination declined
13. Pedal edema
PLAN: She will come in for labs on 01/06/2021. Notation written that she is to lie down
when she has her labs drawn. She brings someone with her to stay with her while it is
done. We will obtain CBC, CMP, TSH, lipids, vitamin D, PTH, rheumatoid panel, and
ANA. Amoxil given. Discussed medication administration, side effects, and risks.
Discontinue for any rash or itching. Recommended yogurt to prevent yeast. She declines
flu vaccine. Call if any problems. Phone visit total lasting 33 minutes.
PROVIDER NAME: SYDNEY DOWELL, A.P.R.N.
DICTATED AND CONFIRMED.
SD/is/kk
99214-95
J32.9, m25.50, e55.9, e78.5, i10, h93.19, r60.9, z76.0, z87.19, z79.899, y87.7, z28.21,
r60.0
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (589)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5806)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- ServeSafe Practice Exam (English Version)Document98 pagesServeSafe Practice Exam (English Version)Jessica Morales100% (9)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- 249-Oxford American Handbook of Clinical Examination and Practical Skills (Oxford American HandboDocument526 pages249-Oxford American Handbook of Clinical Examination and Practical Skills (Oxford American HandboSamuel Gomes100% (1)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Iaso Tea IngredientDocument7 pagesIaso Tea Ingredientsizzla7No ratings yet
- Stan Checketts DocumentationDocument2 pagesStan Checketts Documentationnikdolly50% (4)
- CABALIDA - Herbal PlantsDocument29 pagesCABALIDA - Herbal PlantsJeralyn CABALIDANo ratings yet
- OET Reading Sample Test 2 Answer KeyPart ADocument2 pagesOET Reading Sample Test 2 Answer KeyPart AReina Anne Jayme33% (3)
- Care Plan For Bowel ResectionDocument4 pagesCare Plan For Bowel Resectionviki840488% (8)
- Medical Surgical NursingDocument24 pagesMedical Surgical NursingWilmaBongotanPadawilNo ratings yet
- Pathological Obstetrics, Basic Family Planning and Care of InfantsDocument96 pagesPathological Obstetrics, Basic Family Planning and Care of InfantsScarlet AmodiaNo ratings yet
- GastritisDocument16 pagesGastritisAngie Mandeoya50% (2)
- NCP PneumoniaDocument28 pagesNCP PneumoniaW'ton Borbe83% (6)
- Risk For Fluid and Electrolyte Imbalances Nursing Care PlanDocument1 pageRisk For Fluid and Electrolyte Imbalances Nursing Care PlanTrixia Dacles100% (1)
- Summer Internship Report MBA 3rd SemDocument79 pagesSummer Internship Report MBA 3rd SemAnkit BhatiNo ratings yet
- Report 3 1Document5 pagesReport 3 1Ankit BhatiNo ratings yet
- Research Project Report STUDENTSDocument15 pagesResearch Project Report STUDENTSAnkit BhatiNo ratings yet
- Report 1 2Document5 pagesReport 1 2Ankit BhatiNo ratings yet
- I NT Er Nat I Onal Conf Er Ence On "Cont Empor Ar y Chal L Enges I N Management, Educat I On, Technol Ogy & Appl I Ed Sci Ences"Document10 pagesI NT Er Nat I Onal Conf Er Ence On "Cont Empor Ar y Chal L Enges I N Management, Educat I On, Technol Ogy & Appl I Ed Sci Ences"Ankit BhatiNo ratings yet
- A Study On Employee Motivation at Work Place With Reference To BSNL, KadapaDocument8 pagesA Study On Employee Motivation at Work Place With Reference To BSNL, KadapaAnkit BhatiNo ratings yet
- Worksheet - Siddhartha and The Swan 17th JanDocument1 pageWorksheet - Siddhartha and The Swan 17th JanAnkit BhatiNo ratings yet
- 4th Sem MBA ProjectDocument7 pages4th Sem MBA ProjectAnkit BhatiNo ratings yet
- Chapter 58 - Drugs Affecting Gastrointestinal MotilityDocument12 pagesChapter 58 - Drugs Affecting Gastrointestinal MotilityJonathonNo ratings yet
- AntiemeticsDocument30 pagesAntiemeticsDustyNo ratings yet
- The-Gastrointestinal-Symptoms-Present-In-Patients-With POTSDocument8 pagesThe-Gastrointestinal-Symptoms-Present-In-Patients-With POTSEmilie ChateletNo ratings yet
- OndansetronDocument11 pagesOndansetronIlyes FerenczNo ratings yet
- Improving Diet To Avoid Gastritis Disease: Teaching Unit ActivitiesDocument26 pagesImproving Diet To Avoid Gastritis Disease: Teaching Unit ActivitiesVeren VeronicaNo ratings yet
- JM DrugDocument3 pagesJM DrugVerdie B. NgayanNo ratings yet
- Recording The Medical HistoryDocument8 pagesRecording The Medical HistorypasambalyrradjohndarNo ratings yet
- Drug Study On METHERGINEDocument4 pagesDrug Study On METHERGINEshadow gonzalezNo ratings yet
- MEDSURG TEST 5 RationalizationDocument4 pagesMEDSURG TEST 5 RationalizationJohn Derama SagapsapanNo ratings yet
- Common Complaints in Pregnancy 508Document4 pagesCommon Complaints in Pregnancy 508Happybaby incNo ratings yet
- AGE PPT Case Study 2020Document31 pagesAGE PPT Case Study 2020Marco VelaNo ratings yet
- NCP For ConcussionDocument3 pagesNCP For Concussiontamtam_antonio100% (1)
- Heart Failure Care Plan LippincottDocument62 pagesHeart Failure Care Plan LippincottDyllano100% (1)
- Health Teaching Plan Mars and LainDocument7 pagesHealth Teaching Plan Mars and LainMarissa AsimNo ratings yet
- HomeopathyDocument32 pagesHomeopathyavidmasterNo ratings yet
- Magnesium Sulfate 250 500 MG Metoclopramide Drug StudyDocument4 pagesMagnesium Sulfate 250 500 MG Metoclopramide Drug Studyprog.ecleo.swuNo ratings yet
- Drug Study CHDCDocument1 pageDrug Study CHDCIannBlancoNo ratings yet
- Drug StudyDocument5 pagesDrug StudyOlivia Solomon100% (1)