Professional Documents
Culture Documents
Nihms 1029267
Uploaded by
ryaalwiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nihms 1029267
Uploaded by
ryaalwiCopyright:
Available Formats
HHS Public Access
Author manuscript
Retina. Author manuscript; available in PMC 2019 October 01.
Author Manuscript
Published in final edited form as:
Retina. 2018 October ; 38(10): 1896–1904. doi:10.1097/IAE.0000000000002302.
Changes in Diabetic Retinopathy Severity when Treating
Diabetic Macular Edema with Ranibizumab: DRCR.net Protocol I
5-year Report
Susan B. Bressler, MD1, Isoken Odia, OD, MPH2, Adam R. Glassman, MS2, Ronald P. Danis,
MD4, Sandeep Grover, MD5, Bob Hampton, MD6, Lee M. Jampol, MD7, Maureen G. Maguire,
PhD3, and Michele Melia, ScM2
Author Manuscript
1Wilmer Institute, Johns Hopkins Univeristy School of Medicine
2Jaeb Center for Health Research
3Department of Ophthalmology, University of Pennsylvania
4Ophthalmology and Visual Sciences, University of Wisconsin, Madison
5University
of Florida College of Med., Department of Ophthalmology, Jacksonville Health
Science Center
6Retina-Vitreous Surgeons of Central New York, PC
7Feinberg School of Medicine, Northwestern University, Chicago, Illinois
Author Manuscript
Summary Statement:
In the DRCR.net Protocol I individuals managed with ranibizumab therapy for DME had favorable
changes in retinopathy severity at 5-years. Rates of improvement and worsening do not appear
altered by a reduction in the number of intravitreous ranibizumab injections for DME during the
later years
Purpose: Explore 5-year changes from baseline in diabetic retinopathy severity among eyes
treated with ranibizumab for diabetic macular edema.
Corresponding Author: Isoken Odia, Jaeb Center for Health Research, 1530 Amberly Drive, Suite 350, Tampa, FL 33647; Phone:
Author Manuscript
(813) 975-8690, Fax: (800) 816-7601, drcrstat9@jaeb.org.
Additional Contributions: Genentech provided the ranibizumab for this study. As per the DRCR.net Industry Collaboration
Guidelines (available at www.drcr.net), the DRCR.net had complete control over the design of the protocol, ownership of the data, and
all editorial content of presentations and publications related to the protocol. Genentech has provided funds restricted to DRCR.net
clinical sites.
Financial Disclosures: Some authors have financial disclosures to declare, and will submit them with their financial disclosure forms
via e-mail when it is requested by the journal.
A complete list of all DRCR.net investigator financial disclosures can be found at www.drcr.net.
Role of the Sponsor: The funding organization (National Institutes of Health) participated in oversight of the conduct of the study and
review of the manuscript but not directly in the design or conduct of the study, nor in the collection, management, analysis, or
interpretation of the data, or in the preparation of the manuscript.
The Study was completed at 52 sites within the United States a published list of the Diabetic Retinopathy Clinical Research
Network investigators and staff participating in this protocol can be found in Ophthalmology 2010;117:1064–1077.e35 with a current
list available at www.drcr.net.
Bressler et al. Page 2
Methods: Diabetic Retinopathy Severity was assessed from study visits and annual fundus
Author Manuscript
photographs among participants in Protocol I (DRCR.net). The proportion of eyes that improved at
annual examinations and the cumulative probability of worsening through 5 years were estimated.
Results: Among 235 participants with non-proliferative diabetic retinopathy (NPDR) at baseline,
there were 29%, 28%, and 32% eyes with retinopathy improvement at 1, 3 and 5 years,
respectively. Among 111 participants with proliferative diabetic retinopathy (PDR), corresponding
improvement percentages were 38%, 35% and 23%. The 5-year cumulative probability of
worsening was 18% (95% CI: 14%−25%) among NPDR eyes and 31% (95% CI: 23%−42%)
among PDR eyes (P = .01). In years 1, 3, and 5, the mean (SD) number of ranibizumab injections
was 8.1 (2.5), 2.2 (2.6), and 1.8 (2.6) for NPDR eyes , and 9.0 (2.8), 2.3 (2.9) and 1.7 (2.6) for
PDR eyes. Proportions with improvement or rates of worsening did not change with time.
Conclusion: Individuals receiving ranibizumab therapy for DME may have favorable changes in
DR severity throughout a 5-year period concomitant with sequential reduction in anti-VEGF
Author Manuscript
therapy.
Keywords
Retinopathy; Diabetic Macular Edema; Ranibizumab
INTRODUCTION
Clinical trial results support intravitreous anti-vascular endothelial growth factor (anti-
VEGF) agents as first-line therapy to manage vision impairment in eyes with central-
involved diabetic macular edema (DME).1–9 Anti-permeability properties of these agents
promote anatomic resolution of edema, which favorably affects vision outcomes.10 These
Author Manuscript
agents also retard angiogenesis and may reverse or slow the progression of diabetic
retinopathy.11 Pivotal trials evaluating anti-VEGF therapy for DME have reported
improvement in diabetic retinopathy severity (DRS) and slower progression of retinopathy
through 2 to 3 years among eyes treated with ranibizumab (monthly or using a structured
retreatment protocol) or aflibercept (monthly or 5-monthly doses followed by every other
month).1,4,12–13
In the first year of anti-VEGF therapy, most eyes with DME experience improved visual
acuity (VA) and central retinal thickness. 1,4,12–13 The annual mean number of injections
using the DRCR.net re-treatment algorithm is greatest in year 1 and progressively falls
through year 5.5 Despite a decline in injection frequency, early beneficial effects on vision
and macular thickening are maintained.5 This report evaluates, relative to baseline, the
annual cross-sectional proportion of eyes with DRS improvement and the cumulative
Author Manuscript
probability with retinopathy worsening through 5 years of follow up, in the context of
sequential reduction in ranibizumab frequency. An exploratory analysis of baseline factors
associated with change in DRS also is provided.
METHODS
Study procedures were previously reported.4 The study was conducted between March 2007
and December 2013, and the protocol is available at www.drcr.net (accessed 20 February
Retina. Author manuscript; available in PMC 2019 October 01.
Bressler et al. Page 3
2018). The study adhered to the tenets of the Declaration of Helsinki and was approved by
Author Manuscript
multiple institutional review boards. Study participants provided written informed consent.
Participants had central-involved DME (central subfield thickness [CST] ≧250 µm on
optical coherence tomography [OCT, Stratus; Carl Zeiss Meditec]) and had best-corrected
electronic visual acuity (VA) letter scores of 78 through 24 (approximate Snellen equivalent,
20/32 to 20/320). Ranibizumab-assigned eyes received prompt laser at baseline or deferred
laser beginning at 24 weeks if DME persisted and was no longer improving.
After completion of the 3-year visit, participants were offered extended follow up through 5
years. Protocol visits occurred every 4 to 16 weeks between the 1-year and 5-year visits,
depending on CST and VA response. Assessment of DRS was performed by masked graders
(Fundus Photograph Reading Center, Madison, Wisconsin) using standard 7-field color
fundus photographs obtained at baseline, 1 year, and annually between years 3 and 5.
Author Manuscript
Included in this report are 346 of 375 (92%) ranibizumab-assigned eyes. Twenty-nine eyes
are excluded from this analysis due to missing (12) or ungradable (3) baseline photographs,
or failure to meet Protocol I OCT eligibility criteria (14). Evolution of DR severity was
evaluated in two pre-specified subgroups based on DR severity from baseline photographs:
non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR).
Additional post hoc analyses are reported subdividing the NPDR group into moderate NPDR
or better (Early Treatment Diabetic Retinopathy Study [ETDRS] retinopathy levels 10
through 43) versus moderate-severe and severe NPDR (ETDRS levels 47 and 53).
Table 1 provides definitions for improvement, sustained improvement, and worsening in
DRS. Events indicating worsening of PDR were collected prospectively and any occurence
made an eye ineligible for later improvement. Data from participants who completed a visit
Author Manuscript
but did not have gradable photographs available at the 1-, 3-, 4- or 5-year visit were
excluded from the cross-sectional improvement analyses (35, 25, 23, and 19 eyes,
respectively), but were included in the analyses for cumulative probability of worsening, as
some worsening events were determined based on ophthalmoscopy or treatment for PDR
(Table 1).
Statistical methods
No definitive differences between the deferred and prompt laser treatment groups (P > .05)
were identified, therefore this report combines both ranibizumab groups. The cross-sectional
results for retinopathy improvement at each annual visit are reported as percentages with
exact 95% Clopper-Pearson confidence intervals (CI). Generalized linear regression models
were used to test for a difference in percentages improving between the NPDR and PDR
Author Manuscript
subgroups and to test for a trend in the percentage with retinopathy improvement through 5
years.12 Cumulative probabilities of retinopathy worsening throughout 5 years were
calculated using the life-table method.13 Proportional hazards regression was used to test for
a difference in the rates of worsening between baseline DR subgroups. The Z-test was used
to compare hazard rates between time intervals with P-values adjusted using the Hochberg
method to account for multiple comparisons.14, 15 Sensitivity analyses for DR improvement
and DR worsening were conducted by (1) excluding eyes that underwent cataract surgery
during follow up but prior to the visit (improvement analysis) or censoring at the date of
Retina. Author manuscript; available in PMC 2019 October 01.
Bressler et al. Page 4
surgery (worsening analysis), (2) limiting the definition of improvement or worsening to be
Author Manuscript
based only on photographs (NPDR group only).
Exploratory analyses of 9 variables (Table S1) were performed to identify factors associated
with sustained DR improvement through the 3-year visit or of worsening through 5 years. A
Poisson regression model with robust variance estimator was used for estimating the relative
risk for sustained improvement and excluded all eyes that underwent cataract surgery
between baseline and the 3-year visit.16 A Cox proportional hazards model was used for
worsening and censored eyes that underwent cataract surgery during follow up at the date of
surgery. For both models, initial analyses with including a single factor and baseline DRS
level as a covariate were first performed for each factor. Multivariable stepwise selection
analysis including factors with P<.10 from the univariable analyses was performed next.
Only factors with P-values <.05 were retained in the multivariable model. No adjustments
for multiplicity were made. The proportional hazards assumption was verified by testing
Author Manuscript
time-by-baseline characteristic interactions. All P-values are 2-sided. Statistical analyses
were conducted using SAS version 9.4 (SAS Institute Inc, Cary, NC).
RESULTS
Among the 346 participants eligible for analysis, NPDR was present in 235 (68%)
participants (42% female; average age [SD] 63.9 years [9.2]; 72% white) among whom 89
(38%) had moderate NPDR or better (level 47 or better) and 146 (62%) had moderate-severe
to severe NPDR (level 47 or 53). The remaining 111 participants (32%) had PDR at baseline
(43% female; average age [SD] 61.0 years [10.2]; 76% white). Seven NPDR (level 20 or
less) eyes (3%) and 61 PDR (level 60, PRP without active PDR) eyes (55%) were excluded
from the improvement analysis because they could not meet the improvement definition. All
Author Manuscript
eyes in the study were eligible for DR worsening.
Table S2 shows the follow-up status for visits that required fundus photographs. Among
participants alive at each time point, completion rates were 96%, 89% and 75% at the 1-, 3-
and 5-year visits, respectively. The availability of gradable fundus photographs from patients
who remained alive declined from 86% at 1 year to 81% at 3 years and 69% at 5 years.
Comparison of participants by 5-year visit completion status showed that non-completers
with NPDR were more likely at baseline to have had diabetes longer, use insulin, have a
prior cardiovascular event, and be pseudophakic; non-completers with PDR were older, had
higher HbA1c, were more likely to have hypertension, prior cataract surgery, and less severe
DME (Table S3). The baseline distribution of DRS appeared similar between completers and
non-completers within the DR subgroups with one exception: fewer PDR eyes had inactive
PDR among the non-completers.
Author Manuscript
Diabetic Retinopathy Improvement
The proportions of eyes with improvement were similar over time and between the NPDR
and PDR subgroups (Figure 1a). At the 5-year visit, 32% (95% CI: 24%- 41%) of the NPDR
(N = 137) and 23% (95% CI: 9%- 44%) of the PDR (N = 26) eyes improved. In addition,
15% (95% CI: 7%−28%) of the moderate NPDR or better group (N = 52) improved vs. 42%
(95% CI: 32%−54%) of the moderate-severe/severe NPDR eyes (N = 85; P = .002). Similar
Retina. Author manuscript; available in PMC 2019 October 01.
Bressler et al. Page 5
results were found in sensitivity analyses that excluded eyes with cataract surgery prior to
Author Manuscript
the visit (Figure S1) or limited improvement to a 2-step change on photographs (Figure S2).
Among 70 eyes with improvement at the 1-year visit, 53 (76%) had gradable photographs to
assess sustained improvement at the 3-year visit. Improvement was sustained at the 3-year
visit in 25 eyes (47%). The proportion with sustained improvement was similar among the
baseline NPDR (20 of 43 eyes [47%]) and baseline PDR (5 of 10 eyes [50%])) eyes. Of the
70 eyes improved at 1 year, 11 eyes (16%) had DR worsening relative to their baseline status
by the 5th year. Among eyes that did not improve at the 1-year visit, subsequent
improvement was seen in 26 of 133 (20%), 22 of 115 (19%) and 26 of 105 (25%) at the 3-,
4-, and 5-year visits. Percentages of eyes improved appeared similar among the DRS
subgroups (Table 2).
Number of Intravitreous Injections and Improvement in Diabetic Retinopathy Severity
Author Manuscript
Within the improvement cohort, the number of injections administered through each annual
visit during the 5-year period was similar between eyes with baseline NPDR (irrespective of
severity) and baseline PDR, and also was similar when the comparison was limited to eyes
completing the 5-year visit (Table S4). As such, the DRS subgroups were combined in a post
hoc analysis exploring relationships between total injection number and improvement or
sustained improvement.
With a theoretical maximum number of 63 injections during the 5-year follow up, the
cumulative mean (SD) number of injections was 21.2 (13.1) among eyes that had
improvement at the 5-year visit vs.16.3 (8.6) among those that had not improved at this visit
(P =.005). At each annual visit, eyes that improved received more injections since baseline
than eyes that did not improve (P <.05 for each annual visit, Table 3). Overall, the number of
Author Manuscript
annual injections decreased after the 1-year visit.
The mean (SD) cumulative number of injections through the 3-year visit was 15.7 (7.0) for
eyes with improvement at both the 1- and 3-year visits and 12.5 (6.3) injections for eyes that
were not improved at both visits (P = .07). There was no association between number of
injections and sustained DRS improvement through the 3-year visit (P >.05; Table S5).
Worsening of Diabetic Retinopathy
Eyes with NPDR were less likely to worsen than eyes with PDR. The 5-year cumulative
probability of worsening was 18% (95% CI:14%−25%) for the NPDR eyes vs. 31% (95%
CI 23%- 42%, P = .01 vs. NPDR) for the PDR eyes (Figure 2a). This was largely driven by
the low cumulative probability of worsening among eyes with moderate NPDR or better
Author Manuscript
(11% [95% CI: 5%- 20%], P = .002 vs. PDR) while the rate among the eyes with more
severe NPDR (level 47 or 53) approached that of the PDR eyes (24% [95% CI:17%−32%], P
= .20 vs. PDR; Figure 2b). There were no detectable differences in the annual rates of
worsening between the 1st, 2nd, 3rd, 4th, and 5th years within each DRS group (P > .05). As
noted in Table S6, on average, the number of annual injections fell sharply after year 1. The
number of ranibizumab injections was not associated with the risk of worsening (Table S7).
Results were similar in sensitivity analyses that censored eyes at the date of cataract surgery
Retina. Author manuscript; available in PMC 2019 October 01.
Bressler et al. Page 6
performed during follow up (Figure S3) or limited worsening to progression documented on
Author Manuscript
photographs (NPDR subgroup only, Figure S4).
Table 4 shows the distribution of the specific event that initially triggered categorization as
worsening of retinopathy. Among eyes with baseline NPDR, approximately two-thirds of the
events were divided equally between worsening captured on annual photographs (36%) and
clinician-reported vitreous hemorrhage (33%). However, 21 of the 36 NPDR eyes that
worsened by the 5-year visit eventually met more than one DR worsening criterion. Of note,
16 (44%) of the baseline NPDR eyes that worsened developed neovascularization that was
confirmed on photographs. Among eyes with baseline PDR, vitreous hemorrhage accounted
for the majority (55%) of the initial worsening events. However, 12 of the 29 PDR eyes that
worsened eventually met more than one worsening criterion.
Factors Associated With Sustained Retinopathy Improvement or Worsening
Author Manuscript
In the multi-variable model, after adjusting for baseline DR level, VA and lens status
remained associated with sustained improvement (P < .05, Table S8). For every 5 letters, i.e.
1 line, better baseline VA, the likelihood of sustained improvement decreased by 13% (RR:
0.87; 95% CI: 0.77–0.99; P = .03). There was no difference in sustained improvement
between the NPDR and PDR eyes in the multi-variable model (P = .49)
After adjusting only for baseline DR level, cataract surgery prior to entry was associated
with lower rates of worsening. In the multivariable model two factors reduced the likelihood
of DR worsening: cataract surgery prior to study entry (RR: 0.29; 95% CI: 0.14–0.62; P = .
001) and less severe NPDR at entry (RR: 0.16; 95% CI: 0.06–0.47; P < .001) (Table S7).
DISCUSSION
Author Manuscript
The natural evolution of diabetic retinopathy has been well described. Retinopathy scales
based on assessment of disease features present on fundus photographs show an orderly
progression of the disease. Moreover, progressive steps on the scale impart escalating risk of
advancing to vision threatening retinopathy.17, 18 Management of glycemia, blood pressure,
and lipid levels may be instrumental in altering DRS progression rates.19–22 For over 40
years panretinal photocoagulation has been the most effective treatment to stabilize DR until
intraocular anti-VEGF agents administered for DME were observed to promote DR
regression/improvement and slow progression/worsening. Anti-VEGF agents facilitate
reversal of the orderly progression of DR1,2,13
In this exploratory analysis of DRS over a 5-year period in the setting of repeated yet
intermittent administration of ranibizumab to manage DME, long-term improvements were
Author Manuscript
seen. Approximately one-quarter of eyes were observed to have less severe DR than at
baseline at each annual visit through 5 years, irrespective of baseline DR severity. Although
DR improvement was seen in a minority, these observations appear more favorable than the
4-year DR improvement proportions reported in the Wisconsin Epidemiologic Survey.23, 24
In that study, among individuals with diabetes diagnosis before age 30, 7% improved
whereas 17% of subjects diagnosed at age 30 or later had improvement at the 4-year exam.
23,24
Retina. Author manuscript; available in PMC 2019 October 01.
Bressler et al. Page 7
In the present analysis, the most impressive proportions of improvement were found in the
Author Manuscript
moderate/severe to severe NPDR eyes, a subgroup for whom the natural risk of progression
to PDR approaches 50% within 1 year. Importantly, no decline was seen in the proportion of
eyes with DRS improvement, across the DR spectrum, as the frequency of anti-VEGF
administration to manage DME generally declined over the 5-year period. However, about
50% of individuals with DR improvement at 1 year did not sustain this at 3 years, while
others first demonstrated DR improvement only relatively late in their treatment course (e.g.,
at 4 years). When applying a re-treatment protocol aimed at addressing DME rather than
DRS outcomes, DRS improvement at 1 year neither guaranteed that improvement was
sustained nor protected from future worsening. Twenty percent with improvement at 1 year
eventually worsened relative to their baseline exam. Although there may be a relationship
between DRS improvement and larger injection number, the Protocol I study design does not
provide a means to identify the optimal number of anti-VEGF injections to achieve DR
Author Manuscript
improvement. As such, diligent monitoring of DRS level is recommended for all eyes, even
those for whom DRS regression is noted during the course of anti-VEGF therapy for DME.
Despite receiving anti-VEGF therapy, the cumulative proportion of eyes manifesting DR
worsening for the first time increased throughout the 5-year follow up highlighting the need
to remain vigilant for disease worsening. No relationship was identified between number of
injections or HbA1c, and disease worsening while a relationship between baseline DRS and
worsening was confirmed. The cumulative probability of DR worsening was highest among
eyes with PDR and lowest for eyes with moderate NPDR or better, as seen in a similar
analysis from Protocol T.15. Rates of worsening among eyes in Protocol I did not appear to
accelerate in the later years of follow up, in any DRS subgroup, despite a progressive decline
in the average annual ranibizumab exposure. Among control eyes in the ETDRS, 54% of
NPDR eyes developed PDR and about two-thirds of a combined group consisting of levels
Author Manuscript
47/53/61 (mild PDR) progressed 2 or more steps at the 5-year visit.18 The 5-year cumulative
worsening rates reported herein appear more favorable.
Cataract surgery may confound assessment and evolution of DRS. Surgery may accelerate
progression, while a more accurate photographic assessment of DRS level may be facilitated
after cataract removal, introducing ascertainment bias.25 Twenty percent of our participants
underwent cataract surgery during follow up. Sensitivity analysis censoring eyes at the time
of cataract surgery suggested that surgery performed during Protocol I did not substantially
affect the proportionof DRS improvement or rates of worsening. Cataract surgery prior to
study participation lowered the risk of DR worsening during anti-VEGF therapy. Protocol I
excluded those with recent cataract surgery (≤4 months prior to entry). It is possible the
window during which cataract surgery may contribute to DR worsening may have expired in
Author Manuscript
these eyes. In addition, the media clarity achieved in pseudophakic eyes may reduce the
observed rate of worsening over time by minimizing misclassification of DRS level.
Limitations of this analysis include a decline in participation rates and the percentage of
participants with gradable fundus photographs. The reading center assessment of images
was an integral component of definitions for improvement and worsening and their absence
may have biased our estimates. Rates are reported by DRS subgroup with wide confidence
intervals, particularly among the more limited number of eyes with baseline PDR.
Retina. Author manuscript; available in PMC 2019 October 01.
Bressler et al. Page 8
Additional limitations include the limited subset of participants for whom the issue of
Author Manuscript
sustained improvement could be probed and the differences observed between participants
who did not complete the 5-year follow up with those who did.
In summary, individuals managed with ranibizumab therapy for DME simultaneously may
have favorable changes in retinopathy severity. Percentage of eyes improved and worsening
rates did not appear to be altered by the reduction in ranibizumab administration for DME
during the later years of follow up. Confirmation of these longer-term observations of DRS
in other datasets is needed.
Supplementary Material
Refer to Web version on PubMed Central for supplementary material.
Author Manuscript
Acknowledgments
Funding/Support: Supported through a cooperative agreement from the National Eye Institute and the National
Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, U.S. Department of Health
and Human Services EY14231, EY23207, EY18817.
REFERENCES
1. Brown DM, Nguyen QD, Marcus DM, et al. Long-term outcomes of ranibizumab therapy for
diabetic macular edema: the 36-month results from two phase III trials: RISE and RIDE.
Ophthalmology 2013;120(10):2013–22. [PubMed: 23706949]
2. Brown DM, Schmidt-Erfurth U, Do DV, et al. Intravitreal aflibercept for diabetic macular edema:
100-week results from the VISTA and VIVID studies. Ophthalmology 2015;122(10):2044–52.
[PubMed: 26198808]
3. Diabetic Retinopathy Clinical Research N, Elman MJ, Qin H, et al. Intravitreal ranibizumab for
Author Manuscript
diabetic macular edema with prompt versus deferred laser treatment: three-year randomized trial
results. Ophthalmology 2012;119(11):2312–8. [PubMed: 22999634]
4. Diabetic Retinopathy Clinical Research Network. Randomized trial evaluating ranibizumab plus
prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema.
Ophthalmology 2010;117(6):1064–77 e35. [PubMed: 20427088]
5. Elman MJ, Ayala A, Bressler NM, et al. Intravitreal Ranibizumab for diabetic macular edema with
prompt versus deferred laser treatment: 5-year randomized trial results. Ophthalmology
2015;122(2):375–81. [PubMed: 25439614]
6. Elman MJ, Bressler NM, Qin H, et al. Expanded 2-year follow-up of ranibizumab plus prompt or
deferred laser or triamcinolone plus prompt laser for diabetic macular edema. Ophthalmology
2011;118(4):609–14. [PubMed: 21459214]
7. Mitchell P, Bandello F, Schmidt-Erfurth U, et al. The RESTORE study ranibizumab monotherapy or
combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology
2011;118(4):615–25. [PubMed: 21459215]
8. Rajendram R, Fraser-Bell S, Kaines A, et al. A 2-year prospective randomized controlled trial of
Author Manuscript
intravitreal bevacizumab or laser therapy (BOLT) in the management of diabetic macular edema:
24-month data: report 3. Arch Ophthalmol 2012;130(8):972–9. [PubMed: 22491395]
9. Schmidt-Erfurth U, Lang GE, Holz FG, et al. Three-year outcomes of individualized ranibizumab
treatment in patients with diabetic macular edema: the RESTORE extension study. Ophthalmology
2014;121(5):1045–53. [PubMed: 24491642]
10. Chun DW, Heier JS, Topping TM, Duker JS, Bankert JM. A pilot study of multiple intravitreal
injections of ranibizumab in patients with center-involving clinically significant diabetic macular
edema. Ophthalmology 2006;113(10):1706–12. [PubMed: 17011952]
Retina. Author manuscript; available in PMC 2019 October 01.
Bressler et al. Page 9
11. Adamis AP, Shima DT. The role of vascular endothelial growth factor in ocular health and disease.
Retina 2005;25(2):111–8. [PubMed: 15689799]
Author Manuscript
12. Piegorsch WW, Bailer AJ. Statistics for environmental biology and toxicology; 1997.
13. Armitage P, Berry G, Mathew J. Statistical Methods in Medical Research Vol 4: Blackwell
Science; 2002.
14. Glueck DH. Sample Size Calculations in Clinical Research. 2nd edition by CHOW S-C, SHAO J,
and WANG H. Biometrics, 64: 1307–1308. doi:10.1111/j.1541-0420.2008.01138_10.x; 2008.
15. Hochberg Y A sharper Bonferroni procedure for multiple tests of significance. Biometrika
1988;75(4):800–2.
16. Spiegelman D, Hertzmark E. Easy SAS calculations for risk or prevalence ratios and differences.
Am J Epidemiol 2005;162(3):199–200. [PubMed: 15987728]
17. The Diabetic Retinopathy Study Research Group. Four risk factors for severe visual loss in diabetic
retinopathy. The third report from the Diabetic Retinopathy Study. Arch Ophthalmol 1979;97:654–
5. [PubMed: 426679]
18. Early Treatment Diabetic Retinopathy Study Research Group. Fundus photographic risk factors for
progression of diabetic retinopathy. ETDRS report number 12. Ophthalmology 1991;98:823–33.
Author Manuscript
[PubMed: 2062515]
19. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and
microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317(7160):703–13.
[PubMed: 9732337]
20. Keech AC, Mitchell P, Summanen PA, et al. Effect of fenofibrate on the need for laser treatment for
diabetic retinopathy (FIELD study): a randomised controlled trial. Lancet 2007;370(9600):1687–
97. [PubMed: 17988728]
21. Diabetes Control Complications Trial /Epidemiology of Diabetes Interventions Complications
Research Group, Lachin JM, White NH, et al. Effect of intensive diabetes therapy on the
progression of diabetic retinopathy in patients with type 1 diabetes: 18 years of follow-up in the
DCCT/EDIC. Diabetes 2015;64(2):631–42. [PubMed: 25204977]
22. Group AS, Group AES, Chew EY, et al. Effects of medical therapies on retinopathy progression in
type 2 diabetes. N Engl J Med 2010;363(3):233–44. [PubMed: 20587587]
23. Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin Epidemiologic Study of
Author Manuscript
Diabetic Retinopathy. IX. Four-year incidence and progression of diabetic retinopathy when age at
diagnosis is less than 30 years. Arch Ophthalmol 1989;107(2):237–43. [PubMed: 2916977]
24. Klein R, Klein BE, Moss SE, Davis MD, DeMets DL. The Wisconsin Epidemiologic Study of
Diabetic Retinopathy. X. Four-year incidence and progression of diabetic retinopathy when age at
diagnosis is 30 years or more. Arch Ophthalmol 1989;107(2):244–9. [PubMed: 2644929]
25. Jaffe GJ, Burton TC, Kuhn E, Prescott A, Hartz A. Progression of nonproliferative diabetic
retinopathy and visual outcome after extracapsular cataract extraction and intraocular lens
implantation. Am J Ophthalmol 1992;114(4):448–56. [PubMed: 1415456]
Author Manuscript
Retina. Author manuscript; available in PMC 2019 October 01.
Bressler et al. Page 10
Author Manuscript
Author Manuscript
Author Manuscript
Author Manuscript
Retina. Author manuscript; available in PMC 2019 October 01.
Bressler et al. Page 11
Author Manuscript
Author Manuscript
Author Manuscript
Figure 1. Percentage of Ranibizumab-Treated Eyes with Improvement in Diabetic Retinopathy
Severity from Baseline
Percentage of eyes demonstrating improvement in diabetic retinopathy at each annual visit at
which study photographs were required, by baseline DR subgroup. The number of evaluable
study eyes at each visit is listed and error bars represent the Clopper-Pearson exact
confidence limits. Percentage of eyes improved were stable over time using the generalized
score trend test (test for trend). NPDR = non-proliferative diabetic retinopathy, PDR =
proliferative diabetic retinopathy.
Author Manuscript
Retina. Author manuscript; available in PMC 2019 October 01.
Bressler et al. Page 12
Author Manuscript
Author Manuscript
Author Manuscript
Author Manuscript
Retina. Author manuscript; available in PMC 2019 October 01.
Bressler et al. Page 13
Author Manuscript
Author Manuscript
Author Manuscript
Figure 2. Cumulative Probability of Diabetic Retinopathy Worsening Among Eyes Treated with
Ranibizumab for Diabetic Macular Edema
Cumulative probability of worsening of diabetic retinopathy by baseline retinopathy
subgroup. There was a difference in the rate of worsening between the NPDR and PDR
group [P = .01]. There was no difference in the rate of worsening between the 1st, 2nd, 3rd,
4th, and 5th years within each DR group (P > .05). NPDR=non-proliferative diabetic
retinopathy, PDR=proliferative diabetic retinopathy.
Author Manuscript
Retina. Author manuscript; available in PMC 2019 October 01.
Bressler et al. Page 14
Table 1
Definitions for Diabetic Retinopathy Improvement or Worsening During Follow up
Author Manuscript
Non-Proliferative Diabetic Retinopathy (NPDR) at Proliferative Diabetic Retinopathy (PDR)
baseline at baseline
Improvement in retinopathy was achieved if both of the following criteria were met during follow up
Documentation on case report (1) no PRP, vitrectomy, or anti-VEGF injection (to manage PDR or its complications) was performed,
† and no vitreous hemorrhage, retinal detachment (traction, rhegmatogenous, combined, or unspecified),
form anterior segment neovascularization, or neovascular glaucoma was identified
Assessment of annual fundus (2a) improvement by 2 or more levels on the ETDRS diabetic retinopathy scale vs. baseline
photographs by reading center
(2b) regression of active PDR (level 61 or higher) to
no PDR (level 53 or lower if no prior PRP, or to level
60 if PRP was present at entry)
Baseline DR severity ineligible for Microaneurysms only or less Inactive PDR
improvement (level 10, 12, 14, 15, or 20) (level 60)
Author Manuscript
Sustained Improvement in retinopathy was achieved if improvement was demonstrated at the 1-year visit and there were gradable
photographs at the 3-year visit that confirmed improvement relative to baseline.
Worsening of diabetic retinopathy included any of the following events during follow up
Documentation on case report (1) PRP, vitrectomy, or anti-VEGF injection (to manage PDR or its complications), vitreous hemorrhage,
† retinal detachment, or neovascularization of the iris or angle or neovascular glaucoma
form
(2) worsening by 2 or more levels on the ETDRS severity scale vs. baseline
Assessment of annual fundus
‡ (3b) progression from less than high risk PDR
photographs by reading center (3a) worsening from no PDR to PDR (≤ level 53
to advanced PDR (level 60 to 75 progressing
progressing to level 60 or higher)
to level 81 or 85)
Baseline DR severity ineligible for Advanced PDR
N/A
worsening (level 81 or 85)
ETDRS= Early Treatment Diabetic Retinopathy Study; Anti-VEGF=anti-vascular endothelial growth factor.
Author Manuscript
†
Eyes that manifested worsening of retinopathy with any PDR related event were considered as non-improvers from that point foward in the
improvement analysis.
‡
Cases with missing photograph data or nongradable photographs at a completed follow-up visit were considered as no event for the photograph
component in the composite worsening outcome at that annual time point.
Author Manuscript
Retina. Author manuscript; available in PMC 2019 October 01.
Bressler et al. Page 15
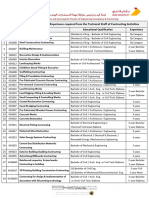
Table 2
Late Improvement in Diabetic Retinopathy: Improvement Status at Annual Visits Among Eyes that Did Not
Author Manuscript
Show Improvement in Retinopathy at the 1-Year Visit
Diabetic Retinopathy Status Between Baseline and 3-Year Visit [Number 4-Year Visit [Number 5-Year Visit [Number
Specified Visit Evaluable] Evaluable] Evaluable]
NPDR at Baseline
No Improvement at 1 Year [N=111] [N=98] [N=89]
N=136
Late Improvement 20 (18%) 18 (18%) 22 (25%)
No Improvement 91 (82%) 80 (82%) 67 (75%)
PDR at Baseline
No Improvement at 1 Year [N=22] [N=17] [N=16]
N=25
Late Improvement 6 (27%) 4 (24%) 4 (25%)
No Improvment 16 (73%) 13 (76%) 12 (75%)
Author Manuscript
NPDR or PDR at Baseline
No Improvement at 1 Year [N=133] [N=115] [N=105]
N=161
Late Improvement 26 (20%) 22 (19%) 26 (25%)
No Improvment 107 (80%) 93 (81%) 79 (75%)
Late Improvement: Status of DR severity was improved relative to baseline at the specified annual visit.
No Improvment: Status of DR severity was “not improved” relative to baseline at the specified annual visit.
Note: 2-Year visit is not shown due to limited fundus photographs
Author Manuscript
Author Manuscript
Retina. Author manuscript; available in PMC 2019 October 01.
Bressler et al. Page 16
Table 3
Cumulative Number of Ranibizumab Injections at Improvement Assessment Visits by Diabetic Retinopathy
Author Manuscript
Improvement Status
Number of injections between baseline and the specified Visit * P-value
**Total no. of injections for each year Improved Not Improved
1-Year Visit N=231 N=70 N=161
Mean ± SD 8.1 ± 2.6 9.1 ± 2.6 7.6 ± 2.5 < .001
Median (IQR) 8 (6, 10) 10 (7, 11) 7 (6, 9)
3-Year Visit N=204 N=60 N=144
Mean ± SD 2.2 ± 2.8 14.9 ± 7.9 12.8 ± 6.3 .05
Median (IQR) 1 (0, 4) 14 (9, 20) 11 (8, 17)
4-Year Visit N=176 N=49 N=127
Author Manuscript
Mean ± SD 1.7 ± 2.6 17.7 ± 9.5 14.4 ± 7.9 .02
Median (IQR) 0 (0, 3) 15 (10, 23) 13 (8, 19)
5-Year Visit N=163 N=50 N=113
Mean ± SD 1.9 ± 2.7 21.2 ± 13.1 16.3 ± 8.6 .005
Median (IQR) 0 (0, 4) 17 (11, 30) 15 (10, 22)
SD= standard deviation; IQR= Interquartile range
*
General linear model used to determine the difference in cumulative number of injections received between eyes with DRS improvement and eyes
without DRS improvement
**
Includes all eyes eligible for improvement at each visit; value represents the number of injections in the 12 month period concluding the day
before the specified visit.
Author Manuscript
Author Manuscript
Retina. Author manuscript; available in PMC 2019 October 01.
Bressler et al. Page 17
Table 4
First Event Triggering Worsening by Baseline Diabetic Retinopathy Subgroup among Ranibizumab Assigned
Author Manuscript
Eyes
NPDR N=36 PDR N=29
First Event Triggering Worsening
N (%) N (%)
Change on Annual Photographs 13 (36) 2 (7)
Vitreous Hemorrhage 12 (33) 16 (55)
PRP 6 (17) 6 (21)
NVI or NVA or NVG 2 (6) 0 (0)
Retinal Detachment 0 (0) 2 (7)
Vitrectomy 0 (0) 2 (7)
PRP and Change on Photographs 2 (6) 0 (0)
PRP and Vitreous Hemorrhage 1 (3) 1 (3)
Author Manuscript
Anti-VEGF to Treat PDR 0 (0) 0 (0)
Anti-VEGF=anti-vascular endothelial growth factor; PDR=proliferative diabetic retinopathy; PRP=panretinal photocoagulation; NPDR=
nonproliferative diabetic retinopathy NVI=neovascularization of the iris; NVA=Neovascularization of the angle; NVG=Neovascular glaucoma.
Author Manuscript
Author Manuscript
Retina. Author manuscript; available in PMC 2019 October 01.
You might also like
- Iodide and Bromide Ions in Brackish Water, Seawater, and Brines D 3869 - 04Document12 pagesIodide and Bromide Ions in Brackish Water, Seawater, and Brines D 3869 - 04stevgonNo ratings yet
- Retina Clinica Trials Update - 0813 - Supp2Document16 pagesRetina Clinica Trials Update - 0813 - Supp2cmirceaNo ratings yet
- Underground Equipment SelectionDocument44 pagesUnderground Equipment SelectionCherotich Silas cheboseiNo ratings yet
- Case AnalysisDocument2 pagesCase AnalysisJessa San PedroNo ratings yet
- Yoga SadhguruDocument6 pagesYoga Sadhgurucosti.sorescuNo ratings yet
- Ranibizumab in Diabetic Retinopathy With or Without Diabetic Macular EdemaDocument3 pagesRanibizumab in Diabetic Retinopathy With or Without Diabetic Macular EdemaVivi DeviyanaNo ratings yet
- Ranibizumab in Diabetic Retinopathy With or Without Diabetic Macular EdemaDocument3 pagesRanibizumab in Diabetic Retinopathy With or Without Diabetic Macular EdemaVivi DeviyanaNo ratings yet
- 5 Yr Outcomes DRCR Prot TDocument18 pages5 Yr Outcomes DRCR Prot TmumbairetinadocNo ratings yet
- Jurnal Retinopaty DiabetikumDocument11 pagesJurnal Retinopaty DiabetikumrestikaNo ratings yet
- Pio y AntivegfDocument14 pagesPio y AntivegfBernardo RomeroNo ratings yet
- Clinical Efficacy of Intravitreal Aflibercept VersDocument11 pagesClinical Efficacy of Intravitreal Aflibercept Versbxno84No ratings yet
- Laser Untuk Diabetik RetinopatiDocument10 pagesLaser Untuk Diabetik RetinopatiIndah KurniawatiNo ratings yet
- Comparing The Ef Ficacy of Bevacizumab and Ranibizumab in Patients With Diabetic Macular Edema (BRDME) The BRDME Study, A Randomized TrialDocument12 pagesComparing The Ef Ficacy of Bevacizumab and Ranibizumab in Patients With Diabetic Macular Edema (BRDME) The BRDME Study, A Randomized Trialkoas mataNo ratings yet
- Comparison of Subfoveal Choroidal Thickness ValuesDocument7 pagesComparison of Subfoveal Choroidal Thickness ValuesNurul Ramadhani MustafaNo ratings yet
- The Effect of Intravitreal Anti-Vascular Endothelial Growth Factor Injections On Corneal Endothelium in Patients With Diabetic Macular Oedema PDFDocument5 pagesThe Effect of Intravitreal Anti-Vascular Endothelial Growth Factor Injections On Corneal Endothelium in Patients With Diabetic Macular Oedema PDFpramukh prasadNo ratings yet
- Clinical Study: Systemic Factors Associated With Treatment Response in Diabetic Macular EdemaDocument6 pagesClinical Study: Systemic Factors Associated With Treatment Response in Diabetic Macular EdemaMuhammad Imam NoorNo ratings yet
- Jurnal Vitamin CDocument15 pagesJurnal Vitamin CbethjohNo ratings yet
- Comparison of Intravitreal Bevacizumab (Avastin) With Triamcinolone For Treatment of Diffused Diabetic Macular Edema: A Prospective Randomized StudyDocument9 pagesComparison of Intravitreal Bevacizumab (Avastin) With Triamcinolone For Treatment of Diffused Diabetic Macular Edema: A Prospective Randomized StudyBaru Chandrasekhar RaoNo ratings yet
- A Ibercept, Bevacizumab, or Ranibizumab For Diabetic Macular Edema Two-Year Results From A Comparative Effectiveness Randomized Clinical TrialDocument9 pagesA Ibercept, Bevacizumab, or Ranibizumab For Diabetic Macular Edema Two-Year Results From A Comparative Effectiveness Randomized Clinical TrialcmirceaNo ratings yet
- Dom 13550Document12 pagesDom 13550mandaNo ratings yet
- Brolucizumab EstudioDocument13 pagesBrolucizumab EstudioJuan Carlos Mejía SernaNo ratings yet
- Panretinal Photocoagulation Versus Ranibizumab For Proliferative Diabetic Retinopathy (Document52 pagesPanretinal Photocoagulation Versus Ranibizumab For Proliferative Diabetic Retinopathy (Bima RizkiNo ratings yet
- Jama 1993 03500100088034Document2 pagesJama 1993 03500100088034Odilia Rondang Mauli SimarmataNo ratings yet
- Asymmetric Diabetic Retinopathy.18Document9 pagesAsymmetric Diabetic Retinopathy.18Syeda F AmbreenNo ratings yet
- Risk factors of diabetic retinopathy and vision threatening diabetic retinopathy and vision threatening diabetic retinopaty based on diabetic retinopathy screening program in greater bandung, west java.astriDocument14 pagesRisk factors of diabetic retinopathy and vision threatening diabetic retinopathy and vision threatening diabetic retinopaty based on diabetic retinopathy screening program in greater bandung, west java.astriSi PuputNo ratings yet
- Estudio Mead and BevordexDocument26 pagesEstudio Mead and BevordexAdrian RuizNo ratings yet
- Aflibercept Monotherapy or Bevacizumab First For Diabetic Macular EdemaDocument12 pagesAflibercept Monotherapy or Bevacizumab First For Diabetic Macular EdemaLee Foo WengNo ratings yet
- Assessing The Severity of Diabetic Retinopathy: Early Treatment Diabetic Retinopathy Study Report Number 10Document2 pagesAssessing The Severity of Diabetic Retinopathy: Early Treatment Diabetic Retinopathy Study Report Number 10Vivi DeviyanaNo ratings yet
- Sum - Clinical DR and DMEDocument2 pagesSum - Clinical DR and DMEsolihaNo ratings yet
- Treatment Outcomes in The DRy Eye Amniotic MembraneDocument5 pagesTreatment Outcomes in The DRy Eye Amniotic MembraneDiny SuprianaNo ratings yet
- Pone 0279765Document10 pagesPone 0279765Fray BotodNo ratings yet
- Current Concepts in Diabetic Retinopathy: Diabetes & Metabolism Journal December 2014Document11 pagesCurrent Concepts in Diabetic Retinopathy: Diabetes & Metabolism Journal December 2014Elison J PanggaloNo ratings yet
- Dry Eye.Document9 pagesDry Eye.Kiky RatnaNo ratings yet
- Esc 150003Document5 pagesEsc 150003marlon GarcíaNo ratings yet
- 2484 FullDocument2 pages2484 FullRuby KumarNo ratings yet
- A Collaborative Retrospective Study On The Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients With Diabetic Macular EdemaDocument17 pagesA Collaborative Retrospective Study On The Efficacy and Safety of Intravitreal Dexamethasone Implant (Ozurdex) in Patients With Diabetic Macular EdemaJosé Díaz OficialNo ratings yet
- Journal ReadingDocument21 pagesJournal ReadingRettyNo ratings yet
- Advances in The Management of Diabetic Macular Oedema Based On Evidence From The Diabetic Retinopathy Clinical Research NetworkDocument11 pagesAdvances in The Management of Diabetic Macular Oedema Based On Evidence From The Diabetic Retinopathy Clinical Research NetworkNatalia LeeNo ratings yet
- Biomedicines 11 03146Document10 pagesBiomedicines 11 03146Andrés HpNo ratings yet
- Review On The Influence of Diabetes Mellitus in TheDocument8 pagesReview On The Influence of Diabetes Mellitus in TheRagni MishraNo ratings yet
- Jurnal Anti VEFGDocument9 pagesJurnal Anti VEFGFitria Sirr Mu'thiarohmahNo ratings yet
- Risk Factors For High-Risk Proliferative Diabetic RetinopathyDocument20 pagesRisk Factors For High-Risk Proliferative Diabetic RetinopathyOdilia Rondang Mauli SimarmataNo ratings yet
- Clinical Pharmacy Therapeu - 2022 - Seiberth - Benefit of Medication Reviews by Renal Pharmacists in The Setting of ADocument8 pagesClinical Pharmacy Therapeu - 2022 - Seiberth - Benefit of Medication Reviews by Renal Pharmacists in The Setting of AMADE ARY SARASMITANo ratings yet
- ABC Nihms625185 PDFDocument24 pagesABC Nihms625185 PDFAhmed NahrawyNo ratings yet
- Toxins 13 00527Document15 pagesToxins 13 00527Otaku RPGNo ratings yet
- 3Document10 pages3Omnia ZapharusNo ratings yet
- Vukicevic Et Al 2021 Wfksizpmfaet PDFDocument5 pagesVukicevic Et Al 2021 Wfksizpmfaet PDFMeri VukicevicNo ratings yet
- Evaluation of Ocular Manifestations in Type 2 Diabetes MellitusDocument5 pagesEvaluation of Ocular Manifestations in Type 2 Diabetes MellitusDona Parenta NantaliaNo ratings yet
- 22222Document9 pages22222Aufi FillaNo ratings yet
- 2022 Article 1931Document9 pages2022 Article 1931LoganNo ratings yet
- Rise and Ride - 2012Document13 pagesRise and Ride - 2012Alv JDNo ratings yet
- IBEPE StudyDocument8 pagesIBEPE StudyKaran KumarswamyNo ratings yet
- 1.CKD and Its Health Related Factor A Case Control StudyDocument7 pages1.CKD and Its Health Related Factor A Case Control StudyBobby PrayogoNo ratings yet
- Jackson2016 PDFDocument10 pagesJackson2016 PDFResearch Assistant of Dr. Rizal HamidNo ratings yet
- The Impact of Dry Eye Disease Treatment On Patient Satisfaction and QualityDocument11 pagesThe Impact of Dry Eye Disease Treatment On Patient Satisfaction and QualityribkaNo ratings yet
- A Review On Drug-Drug Interactions in Renal Impairment PatientsDocument12 pagesA Review On Drug-Drug Interactions in Renal Impairment Patientsnoviantyramadhani12No ratings yet
- Inter-Grader Agreement in The Diabetic Retinopathy Screening Program in Palestine-IJMBS-2018.Document6 pagesInter-Grader Agreement in The Diabetic Retinopathy Screening Program in Palestine-IJMBS-2018.Riyad BanayotNo ratings yet
- Anti VEGF 2020Document18 pagesAnti VEGF 2020Denisse LizarragaNo ratings yet
- Review Article JhaveriDocument2 pagesReview Article JhaveriNikhilNo ratings yet
- Retina 39 426Document9 pagesRetina 39 426ryaalwiNo ratings yet
- BR Med Bull-2013-Sivaprasad-201-11 PDFDocument11 pagesBR Med Bull-2013-Sivaprasad-201-11 PDFKarina Mega WNo ratings yet
- Efficacy of Rituximab Therapy in Children With Nephrotic Syndrome: A 10-Year Experience From An Iranian Pediatric HospitalDocument9 pagesEfficacy of Rituximab Therapy in Children With Nephrotic Syndrome: A 10-Year Experience From An Iranian Pediatric HospitalAris BayuNo ratings yet
- Paciente Sist. Comprometido - Enfermedad RenalDocument10 pagesPaciente Sist. Comprometido - Enfermedad RenalErika Natalia Rubio QuinteroNo ratings yet
- Diabetic Retinopathy: Introduction to Novel Treatment StrategiesFrom EverandDiabetic Retinopathy: Introduction to Novel Treatment StrategiesNo ratings yet
- Retina 39 426Document9 pagesRetina 39 426ryaalwiNo ratings yet
- DC 180148Document6 pagesDC 180148ryaalwiNo ratings yet
- Diagnosis and Analysis of Diabetic Retinopathy Based On Electronic Health RecordsDocument6 pagesDiagnosis and Analysis of Diabetic Retinopathy Based On Electronic Health RecordsryaalwiNo ratings yet
- DC 172224Document10 pagesDC 172224ryaalwiNo ratings yet
- Contemporary Review of The Causes and Differential Diagnosis of Sudden Sensorineural Hearing LossDocument12 pagesContemporary Review of The Causes and Differential Diagnosis of Sudden Sensorineural Hearing LossryaalwiNo ratings yet
- Use of Smartphones To Detect Diabetic Retinopathy: Scoping Review and Meta-Analysis of Diagnostic Test Accuracy StudiesDocument16 pagesUse of Smartphones To Detect Diabetic Retinopathy: Scoping Review and Meta-Analysis of Diagnostic Test Accuracy StudiesryaalwiNo ratings yet
- Pengaruh Kinerja Keuangan Dan Risiko Investasi Terhadap Berita Saham Return SahamDocument12 pagesPengaruh Kinerja Keuangan Dan Risiko Investasi Terhadap Berita Saham Return SahamryaalwiNo ratings yet
- Pengaruh Corporate Governance Terhadap Manajemen Laba Di Industri Perbankan IndonesiaDocument26 pagesPengaruh Corporate Governance Terhadap Manajemen Laba Di Industri Perbankan IndonesiaryaalwiNo ratings yet
- Growth Curve For An Annual PlantDocument2 pagesGrowth Curve For An Annual PlantryaalwiNo ratings yet
- LBM 3 Cahyati WordDocument51 pagesLBM 3 Cahyati WordryaalwiNo ratings yet
- Carinthia Katalog DownloadDocument16 pagesCarinthia Katalog DownloadOperator_010100% (2)
- Flow Zone Indicator Guided Workflows For PetrelDocument11 pagesFlow Zone Indicator Guided Workflows For PetrelAiwarikiaar100% (1)
- Atomic St. Package PDFDocument28 pagesAtomic St. Package PDFSatvik RaoNo ratings yet
- BITS Pilani: Determination of Extreme Pressure, Wear Preventive Characteristics of Lubricants Using Four Ball TesterDocument10 pagesBITS Pilani: Determination of Extreme Pressure, Wear Preventive Characteristics of Lubricants Using Four Ball Testerakash chNo ratings yet
- Recruitment and Selection in Canada 7Th by Catano Wiesner Full ChapterDocument22 pagesRecruitment and Selection in Canada 7Th by Catano Wiesner Full Chaptermary.jauregui841100% (51)
- Asme b16-25Document22 pagesAsme b16-25JamesNo ratings yet
- Patel 2013Document116 pagesPatel 2013hnphuocNo ratings yet
- 3 Curvilinear MotionDocument50 pages3 Curvilinear Motiongarhgelh100% (1)
- Bravo MRI II Operation ManualDocument45 pagesBravo MRI II Operation ManualLuis100% (1)
- Phrasal Verbs Related To HealthDocument2 pagesPhrasal Verbs Related To HealthKnuckles El Naco Narco LechugueroNo ratings yet
- The Process: by Andy ZoppeltDocument4 pagesThe Process: by Andy ZoppeltMark Stephen HuBertNo ratings yet
- Keyword 4: Keyword: Strength of The Mixture of AsphaltDocument2 pagesKeyword 4: Keyword: Strength of The Mixture of AsphaltJohn Michael GeneralNo ratings yet
- Pitot/Static Systems: Flight InstrumentsDocument11 pagesPitot/Static Systems: Flight InstrumentsRoel MendozaNo ratings yet
- Times Square C2C Cardigan: Finished Measurements NotionsDocument8 pagesTimes Square C2C Cardigan: Finished Measurements Notionsdiana.alyNo ratings yet
- The Indian & The SnakeDocument3 pagesThe Indian & The SnakeashvinNo ratings yet
- Blue Modern Company Profile PresentationDocument15 pagesBlue Modern Company Profile PresentationjaneNo ratings yet
- Reynold A. Nicholson - The Mystics of IslamDocument65 pagesReynold A. Nicholson - The Mystics of IslamLuminon SamanNo ratings yet
- YoungMan EN131 GUIDEDocument16 pagesYoungMan EN131 GUIDErcpawar100% (1)
- ELS 06 Maret 223Document16 pagesELS 06 Maret 223Tri WinarsoNo ratings yet
- Coding DecodingDocument21 pagesCoding DecodingAditya VermaNo ratings yet
- Danika Cristoal 18aDocument4 pagesDanika Cristoal 18aapi-462148990No ratings yet
- Harmonic Analysis of Separately Excited DC Motor Drives Fed by Single Phase Controlled Rectifier and PWM RectifierDocument112 pagesHarmonic Analysis of Separately Excited DC Motor Drives Fed by Single Phase Controlled Rectifier and PWM RectifierGautam Umapathy0% (1)
- Tokyo Guidelines 2018Document115 pagesTokyo Guidelines 2018Alik Razi100% (1)
- 5 Contracting Activity and Technical Staff RequirementsDocument2 pages5 Contracting Activity and Technical Staff RequirementsDaniyar KussainovNo ratings yet
- Chap 4 - Basic Principles of ElectricityDocument31 pagesChap 4 - Basic Principles of ElectricityAdiseshuMiddeNo ratings yet
- Petersen Coils Basic 20principle and ApplicationDocument3 pagesPetersen Coils Basic 20principle and ApplicationasotozuazuaNo ratings yet