Professional Documents
Culture Documents
ACR Appropriateness Criteria For Hematuria
Uploaded by
Andrew TaliaferroOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ACR Appropriateness Criteria For Hematuria
Uploaded by
Andrew TaliaferroCopyright:
Available Formats
Date of origin: 1995
Last review date: 2014
American College of Radiology
ACR Appropriateness Criteria®
Clinical Condition: Hematuria
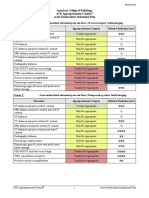
Variant 1: Patients with vigorous exercise, presence of infection or viral illness, or present or recent
menstruation.
Radiologic Procedure Rating Comments RRL*
US kidneys and bladder retroperitoneal 3 O
CT abdomen and pelvis without and with
2 ☢☢☢☢
IV contrast
CT abdomen and pelvis with IV contrast 2 ☢☢☢☢
CT abdomen and pelvis without IV ☢☢☢☢
2
contrast
X-ray intravenous urography 2 ☢☢☢
MRI abdomen and pelvis without and with
2 O
IV contrast
MRI abdomen and pelvis without IV
2 O
contrast
X-ray retrograde pyelography 1 ☢☢☢
Arteriography kidney 1 ☢☢☢
X-ray abdomen and pelvis (KUB) 1 ☢☢
*Relative
Rating Scale: 1,2,3 Usually not appropriate; 4,5,6 May be appropriate; 7,8,9 Usually appropriate
Radiation Level
Variant2: Patients with disease of renal parenchyma as the cause of hematuria.
Radiologic Procedure Rating Comments RRL*
US kidneys and bladder retroperitoneal 8 O
X-ray retrograde pyelography 2 ☢☢☢
CT abdomen and pelvis without and with
2 ☢☢☢☢
IV contrast
CT abdomen and pelvis with IV contrast 2 ☢☢☢☢
CT abdomen and pelvis without IV ☢☢☢☢
2
contrast
MRI abdomen and pelvis without and with
2 O
IV contrast
MRI abdomen and pelvis without IV
2 O
contrast
Arteriography kidney 1 ☢☢☢
X-ray abdomen and pelvis (KUB) 1 ☢☢
X-ray intravenous urography 1 ☢☢☢
*Relative
Rating Scale: 1,2,3 Usually not appropriate; 4,5,6 May be appropriate; 7,8,9 Usually appropriate
Radiation Level
ACR Appropriateness Criteria® 1 Hematuria
Clinical Condition: Hematuria
Variant3: All patients except those described in variant 1 or 2.
Radiologic Procedure Rating Comments RRL*
CT abdomen and pelvis without and with CT urography. Must include high-
9 ☢☢☢☢
IV contrast resolution imaging during excretory phase.
CT abdomen and pelvis without IV
6 ☢☢☢☢
contrast
For patient with contraindication to
iodinated contrast or strong suspicion of
X-ray retrograde pyelography 6 ☢☢☢
urothelial lesion, to clarify abnormality
suspected on CT or IVU.
This procedure may be appropriate but
there was disagreement among panel
CT abdomen and pelvis with IV contrast 5 ☢☢☢☢
members on the appropriateness rating as
defined by the panel’s median rating.
US kidneys and bladder retroperitoneal 5 O
MRI abdomen and pelvis without and with MR urography. For patients with
5 O
IV contrast contraindication to iodinated contrast.
MRI abdomen and pelvis without IV
4 O
contrast
Arteriography kidney 2 ☢☢☢
X-ray abdomen and pelvis (KUB) 2 ☢☢
X-ray intravenous urography 1 ☢☢☢
*Relative
Rating Scale: 1,2,3 Usually not appropriate; 4,5,6 May be appropriate; 7,8,9 Usually appropriate
Radiation Level
ACR Appropriateness Criteria® 2 Hematuria
HEMATURIA
Expert Panel on Urologic Imaging: Luyao Shen, MD 1 ; Steven S. Raman, MD2; Michael D. Beland, MD3;
Courtney Coursey Moreno, MD4; Stanley Goldfarb, MD5; Howard J. Harvin, MD6; Marta E. Heilbrun, MD7;
Matthew T. Heller, MD8; Paul Nikolaidis, MD9; Glenn M. Preminger, MD10; Andrei S. Purysko, MD11;
Myles T. Taffel, MD12; Raghunandan Vikram, MD13; Zhen J. Wang, MD14; Robert M. Weinfeld, MD15;
Don Chan Yoo, MD16; Erick M. Remer, MD17; Mark E. Lockhart, MD, MPH.18
Summary of Literature Review
Introduction/Background
Hematuria is one of the most common presentations of patients with urinary tract diseases and of patients referred
for urinary imaging. This review summarizes practice for the radiologic approach to such patients. It is limited to
adults and does not refer to patients whose hematuria coexists with other clinical situations reviewed in other
ACR Appropriateness Criteria® topics, including acute trauma, infection, renal failure, symptoms of acute stone
disease, known renal masses, and prostatism. It is also limited to initial tests; follow-up of normal or abnormal
first tests is beyond its scope.
The initial decision to be made is whether all patients with any degree of hematuria need imaging evaluation.
Hematuria can originate from any site in the urinary tract and be due to a wide range of causes, which can be
roughly divided into renal, urothelial, or prostatic causes. Thorough evaluation of gross hematuria is
recommended, and this is usually done with a combination of clinical examination, cystoscopic evaluation, and
urinary tract imaging [1-3]. Patients on anticoagulants who present with gross or microscopic hematuria have a
sufficiently high prevalence of important disease including tumors that workup cannot be forgone [2-4].
Microscopic Hematuria
In comparison to gross hematuria, the situation is somewhat different in patients with microscopic hematuria. The
recommended definition of microscopic hematuria is three or more red blood cells per high-power field on
microscopic evaluation of urinary sediment from two of three properly collected urinalysis specimens [3]. Patients
with no detectable abnormalities in their urinary tracts may release small amounts of blood into the urine, so that
several red cells per high-power field may be seen upon microscopic examination of the spun sediment.
The low prevalence of clinically detectable disease in some groups of patients with asymptomatic microscopic
hematuria has led some investigators to suggest that minimal microhematuria in an asymptomatic young adult
needs no evaluation. Unfortunately, no threshold number of red blood cells per high-power field has been found
that separates patients with clinically important disease from those with no detectable urinary tract abnormalities
[3].
As alluded to above, hematuria can be due to a wide variety of causes such as calculi, neoplasms, infection,
trauma, coagulopathy etc. [1-3,5]. In patients with risk factors such as cigarette smoking, occupational exposure
to chemicals, irritative voiding symptoms, a full urologic evaluation for urothelial carcinoma is recommended if
even one urinalysis documents the presence of at least three red blood cells per high-power field [4].
There may be specific circumstances in which complete radiologic workup of microscopic hematuria is
unnecessary [6]. Young women with a clinical picture of simple cystitis, and other patients whose hematuria
completely and permanently resolves after successful therapy, are unlikely to benefit from any imaging [7].
Patients who have a disease of the renal parenchyma (which include glomerulonephritis, glomerulonephropathy,
acute tubular necrosis, and acute kidney injury) also constitute a special group. A thorough urinary analysis
1
Research Author, University of California Los Angeles Medical Center, Los Angeles, California. 2Principal Author, University of California Los Angeles
Medical Center, Los Angeles, California. 3Rhode Island Hospital, Providence, Rhode Island. 4Emory University Hospital, Atlanta, Georgia. 5University of
Pennsylvania School of Medicine, Philadelphia, Pennsylvania, American Society of Nephrology. 6Scottsdale Medical Imaging, Scottsdale, Arizona.
7
University of Utah, Salt Lake City, Utah. 8University of Pennsylvania Medical Center, Pittsburgh, Pennsylvania. 9Northwestern University, Chicago,
Illinois. 10Duke University Medical Center, Durham, North Carolina, American Urological Association. 11Cleveland Clinic Imaging Institute, Cleveland,
Ohio. 12George Washington University Hospital, Washington, District of Columbia. 13University of Texas MD Anderson Cancer Center, Houston, Texas.
14
University of California San Francisco School of Medicine, San Francisco, California. 15Oakland University William Beaumont School of Medicine, Troy,
Michigan.16Rhode Island Medical Imaging Inc, East Providence, Rhode Island. 17Specialty Chair, Cleveland Clinic, Cleveland, Ohio. 18Panel Chair,
University of Alabama at Birmingham, Birmingham, Alabama.
The American College of Radiology seeks and encourages collaboration with other organizations on the development of the ACR Appropriateness
Criteria through society representation on expert panels. Participation by representatives from collaborating societies on the expert panel does not necessarily
imply individual or society endorsement of the final document.
Reprint requests to: publications@acr.org
ACR Appropriateness Criteria® 3 Hematuria
should be the initial workup in this population. Although such patients should have renal ultrasound (US) to
evaluate the kidneys for coexistent morphologic abnormalities, an extensive workup to exclude a mass that may
be the cause of the hematuria is thought to be unnecessary [1,4]. In patients with recent history of infection or
viral illness, vigorous exercise, or urological procedures such as catheterization, initial imaging workup is also not
beneficial [3,4]. Chronic hematuria in the above populations of patients warrants further workup that probably
should include imaging.
In situations of recent trauma, patients with minor blunt trauma may not need imaging initially, but penetrating or
major trauma will definitely warrant some imaging early. In the setting of trauma, please see the ACR
Appropriateness Criteria® “Suspected Lower Urinary Tract Trauma” [8].
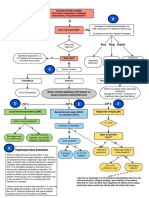
Imaging Evaluation
Imaging evaluation is recommended for all other adult patients with hematuria [4] to detect urologic malignancies
as well as the other possible causes of hematuria mentioned above. A complete history, physical examination,
urine analysis, and appropriate serologic tests such as antinuclear antibody (ANA) and double-stranded DNA
(dsDNA) should precede or accompany the imaging examinations. The imaging evaluation will almost always be
accompanied by cystoscopy to evaluate the urinary bladder, since many bleeding urinary tract lesions arise in the
urinary bladder [5], and imaging procedures are not yet conclusively proven to be as sensitive as cystoscopy in
diagnosing most of them. Multi-detector-row computed tomography (CT) has been evaluated in detecting bladder
cancers [9,10], and reports suggest a sensitivity and specificity of 95% and 92%, respectively [11]. One
retrospective study reports that computed tomography urography (CTU) and cystoscopy had similar diagnostic
accuracy for detection of bladder cancer in patients with hematuria alone; however, cystoscopy remains superior
in patients with prior urothelial malignancy [12].
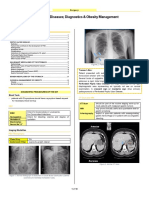
Computed Tomography
Until the mid-1990’s, excretory urography (IVU) was the imaging study used in evaluating hematuria [2,5,9,13],
but development of multidetector CT and the excretory phase CT urogram, also known as CTU, have supplanted
IVU over the past 15 years [14,15]. Compared to CT and US, IVU has low sensitivity for detecting renal masses
<2–3 cm in size, and even if a mass is visualized, further cross sectional studies such as US, CT, or magnetic
resonance imaging (MRI) are then necessary to characterize the mass. In one prospective study that compared CT
and IVU in the same patients with microhematuria [16], radiographic abnormalities were noted in 38 patients;
sensitivity and accuracy of CT were 100% and 98.3% compared to 60.5% and 80.9% for IVU. Fewer additional
radiographic studies were recommended after CT than after IVU in the experience of these authors. Another
prospective study that compared CT and IVU in different patients with hematuria found that CTU had higher
sensitivity than IVU for detecting upper tract pathology (94.1% versus 50%), but both imaging modalities had
low sensitivities (40% or less) for detecting lower tract lesions [17].
Dual energy, split bolus CT protocol that provides virtual noncontrast, parenchymal and urographic phases in a
single scan is being researched, but its benefits are unclear at this time [18,19].
Ultrasound
US still has a role in the initial workup of hematuria to search for bleeding urinary tract lesions [6,13,20-22]. It is
especially useful in radiation-sensitive populations, such as children and pregnant or child-bearing age women, to
detect renal calculi and renal masses. In patients in whom glomerular disease is the cause of hematuria, US can
examine the renal parenchyma and follow disease progression. US can evaluate length, quantitative echogenicity,
cortical thickness, and parenchymal thickness. One study showed that echogenicity correlated the strongest with
histological parameters that include glomerular sclerosis, tubular atrophy, interstitial fibrosis, and interstitial
inflammation [23]. In a prospective study, US had higher sensitivity (96% versus 25%) and negative predictive
value (98% versus 91%) than IVU in detecting abnormalities of the upper urinary tract in patients present with
hematuria [22]. Therefore, US should replace IVU for first-line screening of the upper tracts in radiation-sensitive
populations and patients with glomerular disease as the cause of hematuria. However, in comparison to cross-
sectional imaging modalities such as multidetector CTU or magnetic resonance urography (MRU), US has lower
sensitivity in detecting urinary tract abnormalities [22]. Another prospective study of 841 hematuria patients who
had CTU or MRU showed no significant upper urinary tract lesions in 86.1%. US was a significant predictor of
the final CTU/MRU result [20]; that is, US can be used as an initial screening tool and can triage patients who
need further cross-sectional urography. For the majority of patients with hematuria, multidetector CTU remains
the best overall imaging modality due to its widespread availability, ability to detect a range of possible causes
ACR Appropriateness Criteria® 4 Hematuria
including small renal masses, calcifications and stones and ability to image the upper tract collecting system.
MRU is a reasonable alternative for detection of small renal masses but is poor for detection of calcifications and
small stones. In patients who have contraindications to CTU or are sensitive to radiation, or who have a very low-
risk of having a malignant cause of hematuria, US is the first-line imaging modality [20,22]. One study has shown
that 3D US improved accuracy of detecting bladder cancer compared to 2D US, especially for small lesions [24].
In patients with medullary sponge kidney disease and papillary necrosis, US can be used as an initial imaging
study and subsequent follow-up study for progression.
Intravenous Urography and Retrograde Pyelography
The detection of urothelial lesions in the upper tracts was traditionally performed with IVU and/or ureteroscopy
along with cystoscopy [3]. CTU has largely supplanted IVU for imaging the upper urinary tract [15,25,26];
images are acquired prior to contrast administration and then during nephrographic and excretory urographic
phases of enhancement for a complete evaluation for urinary tract stones, neoplasms in the upper and lower
urinary tracts, and other pathologies. Reconstructed 3D images can be used to produce IVU-like images in
different projections.
Numerous studies have established that CTU is superior to IVU for detecting upper tract urothelial lesions in
patients with hematuria [27-29]. In a meta-analysis, CTU proved to be a very sensitive and specific method for
the detection of urothelial malignancy with pooled sensitivity of 96% and pooled specificity of 99%, and was
superior in direct comparison to IVU in terms of sensitivity and specificity [27].
Retrograde pyelography does not rely on renal excretion of intravascular contrast. In patients with impaired renal
function, or contraindications to CTU or MRU, or suboptimal CTU or MRU, a retrograde pyelography may be a
reasonable adjunct to cystoscopy in patients with suspected upper tract lesions [4].
Magnetic Resonance Urography
MRU can be performed with or without contrast. MRU without contrast is an excellent technique to demonstrate
the cause and level of urinary obstruction, particularly if it is not due to calculous disease [30,31]. The sensitivity
of MRU in detecting urothelial lesions remains under investigation, and at present it is not believed to be the
equivalent of either IVU or CTU [25,32]. However, in patients who cannot receive iodinated contrast material or
are radiation sensitive, MRU can be useful [30]. Now there is research to study other sequences such as diffusion-
weighted MR imaging in detecting bladder cancer [33].
MRI and CT have shown comparable accuracy in detection and characterization of most renal lesions. However,
with indeterminate renal lesions on CT or complicated cysts, MRI can be useful for better characterization
[34,35].
Cystoscopy
Although bladder neoplasms can be visualized on IVU, CT, and MRI, cystoscopy is still considered to be the
optimal technique to detect the plaque-like lesions of early bladder cancers, although newer studies suggest that a
properly performed CTU in an adequately distended bladder is quite sensitive in detecting bladder cancer [11].
CTU as the first study in patients with hematuria may help in the triage of such patients [9,10]. Patients with no
bladder abnormality on CTU can proceed to office cystoscopy, while those with a suspected bladder neoplasm
can undergo cystoscopy in the operating room with intent to biopsy.
Other Imaging Studies
Plain radiography of the abdomen and pelvis (KUB) and catheter arteriography of kidneys are not used as first
line image modalities for initial evaluation of hematuria. KUB may be useful in patients with history of kidney
stones for evaluation of stone size and position and for assessment of stone passage. Rarely, vascular disorders
such as aneurysms, arterio-venous malformations or obstruction of a calyx from overlying artery (Fraley’s
syndrome) may result in hematuria. In these suspected situations, catheter angiography may be useful for
diagnosis and for therapeutic interventions [36].
Summary of Recommendations
Most adults with gross or persistent microhematuria require urinary tract imaging, with CTU replacing the
traditional IVU for this indication.
Although MRI is an excellent technique to evaluate the renal parenchyma for masses and other abnormalities,
it is inferior to CTU and IVU in detection of small stones and urothelial lesions.
ACR Appropriateness Criteria® 5 Hematuria
In patients with microscopic hematuria with suspected renal parenchymal disease, renal US may be useful to
exclude coexistent morphologic abnormalities. In a few carefully chosen patients with selected indications, no
imaging may be necessary.
Summary of Evidence
Of the 36 references cited in the ACR Appropriateness Criteria® Hematuria document, 1 is categorized as a
quality therapeutic study that may have design limitations. Additionally, 35 references are categorized as
diagnostic references including 1 well-designed study, 6 good quality studies, and 10 quality studies that may
have design limitations. There are 18 references that may not be useful as primary evidence.
The 36 references cited in the ACR Appropriateness Criteria® Hematuria document were published between
2002–2014.
While there are references that report on studies with design limitations, seven well-designed or good quality
studies provide good evidence.
Relative Radiation Level Information
Potential adverse health effects associated with radiation exposure are an important factor to consider when
selecting the appropriate imaging procedure. Because there is a wide range of radiation exposures associated with
different diagnostic procedures, a relative radiation level (RRL) indication has been included for each imaging
examination. The RRLs are based on effective dose, which is a radiation dose quantity that is used to estimate
population total radiation risk associated with an imaging procedure. Patients in the pediatric age group are at
inherently higher risk from exposure, both because of organ sensitivity and longer life expectancy (relevant to the
long latency that appears to accompany radiation exposure). For these reasons, the RRL dose estimate ranges for
pediatric examinations are lower as compared to those specified for adults (see Table below). Additional
information regarding radiation dose assessment for imaging examinations can be found in the ACR
Appropriateness Criteria® Radiation Dose Assessment Introduction document.
Relative Radiation Level Designations
Adult Effective Dose Estimate Pediatric Effective Dose Estimate
Relative Radiation Level*
Range Range
O 0 mSv 0 mSv
☢ <0.1 mSv <0.03 mSv
☢☢ 0.1-1 mSv 0.03-0.3 mSv
☢☢☢ 1-10 mSv 0.3-3 mSv
☢☢☢☢ 10-30 mSv 3-10 mSv
☢☢☢☢☢ 30-100 mSv 10-30 mSv
*RRL assignments for some of the examinations cannot be made, because the actual patient doses in these procedures vary
as a function of a number of factors (eg, region of the body exposed to ionizing radiation, the imaging guidance that is
used). The RRLs for these examinations are designated as “Varies”.
Supporting Documents
For additional information on the Appropriateness Criteria methodology and other supporting documents go to
www.acr.org/ac.
References
1. McDonald MM, Swagerty D, Wetzel L. Assessment of microscopic hematuria in adults. Am Fam Physician.
2006;73(10):1748-1754.
2. Sing RI, Singal RK. What is significant hematuria for the primary care physician? Can J Urol. 2012;19 Suppl
1:36-41.
3. Yun EJ, Meng MV, Carroll PR. Evaluation of the patient with hematuria. Med Clin North Am.
2004;88(2):329-343.
4. Davis R, Jones JS, Barocas DA, et al. Diagnosis, evaluation and follow-up of asymptomatic microhematuria
(AMH) in adults: AUA guideline. J Urol. 2012;188(6 Suppl):2473-2481.
ACR Appropriateness Criteria® 6 Hematuria
5. Dooley RE, Pietrow PK. Ureteroscopy for benign hematuria. Urol Clin North Am. 2004;31(1):137-143.
6. Edwards TJ, Dickinson AJ, Natale S, Gosling J, McGrath JS. A prospective analysis of the diagnostic yield
resulting from the attendance of 4020 patients at a protocol-driven haematuria clinic. BJU Int.
2006;97(2):301-305; discussion 305.
7. Stanford EJ, Mattox TF, Parsons JK, McMurphy C. Prevalence of benign microscopic hematuria among
women with interstitial cystitis: implications for evaluation of genitourinary malignancy. Urology.
2006;67(5):946-949.
8. American College of Radiology. ACR Appropriateness Criteria®: Suspected Lower Urinary Tract Trauma.
Available at: https://acsearch.acr.org/docs/69376/Narrative/. Accessed November 26, 2014.
9. Blick CG, Nazir SA, Mallett S, et al. Evaluation of diagnostic strategies for bladder cancer using computed
tomography (CT) urography, flexible cystoscopy and voided urine cytology: results for 778 patients from a
hospital haematuria clinic. BJU Int. 2012;110(1):84-94.
10. Turney BW, Willatt JM, Nixon D, Crew JP, Cowan NC. Computed tomography urography for diagnosing
bladder cancer. BJU Int. 2006;98(2):345-348.
11. Park SB, Kim JK, Lee HJ, Choi HJ, Cho KS. Hematuria: portal venous phase multi detector row CT of the
bladder--a prospective study. Radiology. 2007;245(3):798-805.
12. Sadow CA, Silverman SG, O'Leary MP, Signorovitch JE. Bladder cancer detection with CT urography in an
Academic Medical Center. Radiology. 2008;249(1):195-202.
13. Rodgers M, Nixon J, Hempel S, et al. Diagnostic tests and algorithms used in the investigation of haematuria:
systematic reviews and economic evaluation. Health Technol Assess. 2006;10(18):iii-iv, xi-259.
14. Coakley FV, Yeh BM. Invited Commentary. Radiographics. 2003;23(6):1455-1456.
15. Joffe SA, Servaes S, Okon S, Horowitz M. Multi-detector row CT urography in the evaluation of hematuria.
Radiographics. 2003;23(6):1441-1455; discussion 1455-1446.
16. Gray Sears CL, Ward JF, Sears ST, Puckett MF, Kane CJ, Amling CL. Prospective comparison of
computerized tomography and excretory urography in the initial evaluation of asymptomatic microhematuria.
J Urol. 2002;168(6):2457-2460.
17. Albani JM, Ciaschini MW, Streem SB, Herts BR, Angermeier KW. The role of computerized tomographic
urography in the initial evaluation of hematuria. J Urol. 2007;177(2):644-648.
18. Kulkarni NM, Eisner BH, Pinho DF, Joshi MC, Kambadakone AR, Sahani DV. Determination of renal stone
composition in phantom and patients using single-source dual-energy computed tomography. J Comput Assist
Tomogr. 2013;37(1):37-45.
19. Toepker M, Kuehas F, Kienzl D, et al. Dual energy computerized tomography with a split bolus-a 1-stop shop
for patients with suspected urinary stones? J Urol. 2014;191(3):792-797.
20. Cauberg EC, Nio CY, de la Rosette JM, Laguna MP, de Reijke TM. Computed tomography-urography for
upper urinary tract imaging: is it required for all patients who present with hematuria? J Endourol.
2011;25(11):1733-1740.
21. Sandhu KS, LaCombe JA, Fleischmann N, Greston WM, Lazarou G, Mikhail MS. Gross and microscopic
hematuria: guidelines for obstetricians and gynecologists. Obstet Gynecol Surv. 2009;64(1):39-49.
22. Unsal A, Caliskan EK, Erol H, Karaman CZ. The diagnostic efficiency of ultrasound guided imaging
algorithm in evaluation of patients with hematuria. Eur J Radiol. 2011;79(1):7-11.
23. Moghazi S, Jones E, Schroepple J, et al. Correlation of renal histopathology with sonographic findings.
Kidney Int. 2005;67(4):1515-1520.
24. Mitterberger M, Pinggera GM, Neuwirt H, et al. Three-dimensional ultrasonography of the urinary bladder:
preliminary experience of assessment in patients with haematuria. BJU Int. 2007;99(1):111-116.
25. Kawashima A, Glockner JF, King BF, Jr. CT urography and MR urography. Radiol Clin North Am.
2003;41(5):945-961.
26. Nambirajan T, Sohaib SA, Muller-Pollard C, Reznek R, Chinegwundoh FI. Virtual cystoscopy from
computed tomography: a pilot study. BJU Int. 2004;94(6):828-831.
27. Chlapoutakis K, Theocharopoulos N, Yarmenitis S, Damilakis J. Performance of computed tomographic
urography in diagnosis of upper urinary tract urothelial carcinoma, in patients presenting with hematuria:
Systematic review and meta-analysis. Eur J Radiol. 2010;73(2):334-338.
28. Maheshwari E, O'Malley ME, Ghai S, Staunton M, Massey C. Split-bolus MDCT urography: Upper tract
opacification and performance for upper tract tumors in patients with hematuria. AJR Am J Roentgenol.
2010;194(2):453-458.
ACR Appropriateness Criteria® 7 Hematuria
29. Wang LJ, Wong YC, Huang CC, Wu CH, Hung SC, Chen HW. Multidetector computerized tomography
urography is more accurate than excretory urography for diagnosing transitional cell carcinoma of the upper
urinary tract in adults with hematuria. J Urol. 2010;183(1):48-55.
30. Silverman SG, Leyendecker JR, Amis ES, Jr. What is the current role of CT urography and MR urography in
the evaluation of the urinary tract? Radiology. 2009;250(2):309-323.
31. Shokeir AA, El-Diasty T, Eassa W, et al. Diagnosis of noncalcareous hydronephrosis: role of magnetic
resonance urography and noncontrast computed tomography. Urology. 2004;63(2):225-229.
32. Leyendecker JR, Barnes CE, Zagoria RJ. MR urography: techniques and clinical applications. Radiographics.
2008;28(1):23-46; discussion 46-27.
33. Abou-El-Ghar ME, El-Assmy A, Refaie HF, El-Diasty T. Bladder cancer: diagnosis with diffusion-weighted
MR imaging in patients with gross hematuria. Radiology. 2009;251(2):415-421.
34. Israel GM, Hindman N, Bosniak MA. Evaluation of cystic renal masses: comparison of CT and MR imaging
by using the Bosniak classification system. Radiology. 2004;231(2):365-371.
35. Nikken JJ, Krestin GP. MRI of the kidney-state of the art. Eur Radiol. 2007;17(11):2780-2793.
36. Zhang Z, Yang M, Song L, Tong X, Zou Y. Endovascular treatment of renal artery aneurysms and renal
arteriovenous fistulas. J Vasc Surg. 2013;57(3):765-770.
The ACR Committee on Appropriateness Criteria and its expert panels have developed criteria for determining appropriate imaging examinations for
diagnosis and treatment of specified medical condition(s). These criteria are intended to guide radiologists, radiation oncologists and referring physicians
in making decisions regarding radiologic imaging and treatment. Generally, the complexity and severity of a patient’s clinical condition should dictate the
selection of appropriate imaging procedures or treatments. Only those examinations generally used for evaluation of the patient’s condition are ranked.
Other imaging studies necessary to evaluate other co-existent diseases or other medical consequences of this condition are not considered in this
document. The availability of equipment or personnel may influence the selection of appropriate imaging procedures or treatments. Imaging techniques
classified as investigational by the FDA have not been considered in developing these criteria; however, study of new equipment and applications should
be encouraged. The ultimate decision regarding the appropriateness of any specific radiologic examination or treatment must be made by the referring
physician and radiologist in light of all the circumstances presented in an individual examination.
ACR Appropriateness Criteria® 8 Hematuria
You might also like
- Embryology QNSDocument33 pagesEmbryology QNSElizabeth Gabriel HoyaNo ratings yet
- AphakiaDocument26 pagesAphakiaapi-3742497100% (3)
- Indeterminate Renal Mass ACR Appropriateness CriteriaDocument10 pagesIndeterminate Renal Mass ACR Appropriateness CriteriaAndrew TaliaferroNo ratings yet
- Acute Onset Flank Pain-Suspicion of Stone DiseaseDocument9 pagesAcute Onset Flank Pain-Suspicion of Stone DiseasecubirojasNo ratings yet
- Renal Cell Carcinoma Staging (ACR Appropriateness Criteria)Document10 pagesRenal Cell Carcinoma Staging (ACR Appropriateness Criteria)Andrew TaliaferroNo ratings yet
- Onset Flank PainDocument11 pagesOnset Flank PainPipitNo ratings yet
- Hematuria PDFDocument11 pagesHematuria PDFPipitNo ratings yet
- Acute PancreatitisDocument16 pagesAcute PancreatitisLoredana BoghezNo ratings yet
- Acute Nonlocalized Abdominal PainDocument17 pagesAcute Nonlocalized Abdominal PainghassanNo ratings yet
- Major Blunt TraumaDocument18 pagesMajor Blunt TraumaghassanNo ratings yet
- Radiologic Management of Upper Gastrointestinal BleedingDocument13 pagesRadiologic Management of Upper Gastrointestinal BleedingshadowlightfoxNo ratings yet
- Postmenopausal Subacute or Chronic Pelvic PainDocument9 pagesPostmenopausal Subacute or Chronic Pelvic PainM SNo ratings yet
- Low Back PainDocument10 pagesLow Back Paindigimon666No ratings yet
- Low Back PainDocument22 pagesLow Back PainSF TifarinNo ratings yet
- Abdominal Aortic Aneurysm-Interventional Planning and Follow-UpDocument13 pagesAbdominal Aortic Aneurysm-Interventional Planning and Follow-Upvictor contrerasNo ratings yet
- Adrenal Mass EvaluationDocument19 pagesAdrenal Mass Evaluationpj rakNo ratings yet
- American College of Radiology ACR Appropriateness CriteriaDocument7 pagesAmerican College of Radiology ACR Appropriateness CriteriaMeutia PutriNo ratings yet
- Acute Nonspecific Chest Pain-Low Probability of Coronary Artery DiseaseDocument10 pagesAcute Nonspecific Chest Pain-Low Probability of Coronary Artery Diseasevictor contrerasNo ratings yet
- Acute Hip Pain-Suspected FractureDocument9 pagesAcute Hip Pain-Suspected FractureMario UmañaNo ratings yet
- Abnormal Uterine BleedingDocument12 pagesAbnormal Uterine Bleedingvictor contrerasNo ratings yet
- Infective EndocarditisDocument13 pagesInfective Endocarditispaquidermo85No ratings yet
- Abdominal Truama (Handout)Document6 pagesAbdominal Truama (Handout)Ayuub AbdirizakNo ratings yet
- Suspected Spine TraumaDocument25 pagesSuspected Spine TraumaFelix Valerian HalimNo ratings yet
- Acute Respiratory Illness in Immunocompetent PatientsDocument14 pagesAcute Respiratory Illness in Immunocompetent PatientsVianney OlveraNo ratings yet
- Dyspnea-Suspected Cardiac Origin (Ischemia Already Excluded)Document20 pagesDyspnea-Suspected Cardiac Origin (Ischemia Already Excluded)Parth PatilNo ratings yet
- Abdominal Aortic Aneurysm Follow-Up (Without Repair)Document7 pagesAbdominal Aortic Aneurysm Follow-Up (Without Repair)victor contrerasNo ratings yet
- Chylothorax Treatment PlanningDocument10 pagesChylothorax Treatment PlanningVianney OlveraNo ratings yet
- Occupational Lung DiseasesDocument13 pagesOccupational Lung DiseasesVianney OlveraNo ratings yet
- DR David Scott Gastroenterologist Tamworth Base HospitalDocument49 pagesDR David Scott Gastroenterologist Tamworth Base HospitalyuddNo ratings yet
- Renovascular HypertensionDocument11 pagesRenovascular HypertensionJoseph GlaserNo ratings yet
- ACR Appropriateness Criteria Pancreatic CystDocument9 pagesACR Appropriateness Criteria Pancreatic CystSole GonzalezNo ratings yet
- WTAAbd Stab WoundsDocument1 pageWTAAbd Stab WoundsMariyam AlblooshiNo ratings yet
- 1stprize CR Auditpostercomp C Reid 2015Document1 page1stprize CR Auditpostercomp C Reid 2015webber_denzNo ratings yet
- Tut10 (Group GH) Preinvasive DS - ScreeningDocument7 pagesTut10 (Group GH) Preinvasive DS - ScreeningRishwini SelvanNo ratings yet
- CA Treatment Osteosarcoma Pedi Web AlgorithmDocument6 pagesCA Treatment Osteosarcoma Pedi Web AlgorithmyaseenNo ratings yet
- ACR Appropriateness Criteria® Acute Chest Pain - Suspected Pulmonary Embolism.Document16 pagesACR Appropriateness Criteria® Acute Chest Pain - Suspected Pulmonary Embolism.Madalina TalpauNo ratings yet
- Oncology Table SummaryDocument4 pagesOncology Table SummaryAiah AbenesNo ratings yet
- Laparoscopic in TraumaDocument37 pagesLaparoscopic in TraumaronaldNo ratings yet
- TMCC Ecu Package 6.24.21Document3 pagesTMCC Ecu Package 6.24.21Cinja ShidoujiNo ratings yet
- American College of Radiology End User License AgreementDocument9 pagesAmerican College of Radiology End User License AgreementYori PrimandaNo ratings yet
- 1 - Radiology Git l1 - 2Document7 pages1 - Radiology Git l1 - 2deemagNo ratings yet
- Pancreatic MassesDocument47 pagesPancreatic MassesOlga DianaNo ratings yet
- Blunt Trauma Abdomen: (Operative V/S Conservative Management)Document41 pagesBlunt Trauma Abdomen: (Operative V/S Conservative Management)Bhi-An BatobalonosNo ratings yet
- Blunt Abdominal TraumaDocument11 pagesBlunt Abdominal TraumaRahmat SyahiliNo ratings yet
- Emergenze Addome RXDocument9 pagesEmergenze Addome RXBrovazzo PieroNo ratings yet
- Cancer of The Endometrium PDFDocument6 pagesCancer of The Endometrium PDFYanita BetraNo ratings yet
- 1.40 (Surgery) GIT Surgical Diseases - Diagnostics - Obesity ManagementDocument10 pages1.40 (Surgery) GIT Surgical Diseases - Diagnostics - Obesity ManagementLeo Mari Go LimNo ratings yet
- Trauma Tumpul Abdomen: Stase Bedah Digestif Januari 2019Document49 pagesTrauma Tumpul Abdomen: Stase Bedah Digestif Januari 2019ArifHidayatNo ratings yet
- Breast PainDocument9 pagesBreast PainmarysrbNo ratings yet
- Breast Implant Evaluation - NarrativeDocument25 pagesBreast Implant Evaluation - Narrativeopenlab.doisNo ratings yet
- Mcu Siloam & ProdiaDocument2 pagesMcu Siloam & ProdiaWidyaM putriNo ratings yet
- College of Medicine and Health Sciences: For Public Health C-I StudentsDocument29 pagesCollege of Medicine and Health Sciences: For Public Health C-I StudentsWĩž BŕëãžÿNo ratings yet
- Kuliah Trauma Urologi - DR WibisonoDocument34 pagesKuliah Trauma Urologi - DR WibisonoAgung Budi SuristioNo ratings yet
- Penetrating Abdominal TraumaDocument36 pagesPenetrating Abdominal TraumaSyane KristinaNo ratings yet
- PDFsam ObGynDocument4 pagesPDFsam ObGynAlessandro ZadraNo ratings yet
- Cap-2 27 2015Document73 pagesCap-2 27 2015martyn odekeNo ratings yet
- Gastroenterology - Pancreatitis PDFDocument2 pagesGastroenterology - Pancreatitis PDFMonica J Ortiz PereiraNo ratings yet
- Abdomen Blunt Trauma 2 - 3 - 2020Document6 pagesAbdomen Blunt Trauma 2 - 3 - 2020Iqra NazNo ratings yet
- ch039 PDFDocument7 pagesch039 PDFGhazian AdliNo ratings yet
- ( Û ) Questionnaire Hospital InformationDocument5 pages( Û ) Questionnaire Hospital InformationsjeloNo ratings yet
- Salvage Therapy for Prostate CancerFrom EverandSalvage Therapy for Prostate CancerSanchia S. GoonewardeneNo ratings yet
- Zimmer Trabecular Metal Total Ankle Surgical TechniqueDocument76 pagesZimmer Trabecular Metal Total Ankle Surgical TechniqueAnkira FindoroNo ratings yet
- Report On Visit TO The Sadguru Netra Chikitsalaya Hospital, Chitrakoot, India December 2004Document17 pagesReport On Visit TO The Sadguru Netra Chikitsalaya Hospital, Chitrakoot, India December 2004prabhjotbhangalNo ratings yet
- Definisi Transverse LieDocument5 pagesDefinisi Transverse LieErmi MarlinaNo ratings yet
- Pedia Set B PRNDocument9 pagesPedia Set B PRNEdgar RebuyasNo ratings yet
- ASA Physical Status Classification: GuidelineDocument3 pagesASA Physical Status Classification: GuidelineLUISNo ratings yet
- Sudden Death SyndromeDocument72 pagesSudden Death SyndromeStella CooKeyNo ratings yet
- Thyroid ReportDocument105 pagesThyroid ReportAARVNo ratings yet
- Cardiac TransplantDocument135 pagesCardiac TransplantNakka SrikanthNo ratings yet
- WFNS Program BookDocument350 pagesWFNS Program Bookabidik123100% (1)
- Named Signs, Syndromes, Tests and ProceduresDocument64 pagesNamed Signs, Syndromes, Tests and ProceduresHAMSTRINGNo ratings yet
- The Urinary SystemDocument46 pagesThe Urinary SystemWeb AredomNo ratings yet
- Prosta LacDocument16 pagesProsta LacantoniofacmedNo ratings yet
- Update ACLSDocument64 pagesUpdate ACLSVenansius Ratno KurniawanNo ratings yet
- Class III MalocclusionDocument45 pagesClass III Malocclusionمينا عمار شكري محمودNo ratings yet
- Hypo & HyperthyroidismDocument33 pagesHypo & HyperthyroidismSuchit Kumar50% (2)
- NOTES 1st Sem P FDocument6 pagesNOTES 1st Sem P FReaNo ratings yet
- Musculoskeletal NursingDocument10 pagesMusculoskeletal Nursinglemmeloveyou01No ratings yet
- 3 - Risk Factors For Surgical Site InfectionsDocument6 pages3 - Risk Factors For Surgical Site InfectionsAmor KourdouliNo ratings yet
- Iodinated Contrast Media GuidelineDocument41 pagesIodinated Contrast Media GuidelineN Aa100% (1)
- Assesment Bedah Digestif 21 Oktober 2021Document5 pagesAssesment Bedah Digestif 21 Oktober 2021Yolanda RahayuNo ratings yet
- Module 2 AnaphysioDocument32 pagesModule 2 AnaphysioJomarie RamirezNo ratings yet
- Human Anatomy 4th Edition Mckinley Test BankDocument43 pagesHuman Anatomy 4th Edition Mckinley Test Bankjillhenrysetcjnzrfp100% (35)
- AntiagreganteDocument19 pagesAntiagregantecNo ratings yet
- Angioplasty and Vascular StentingDocument8 pagesAngioplasty and Vascular Stentingrajnishpathak648No ratings yet
- ACLS Healthcare Provider Post-Cardiac Arrest Care Algorithm: o Co Io o CoDocument1 pageACLS Healthcare Provider Post-Cardiac Arrest Care Algorithm: o Co Io o CoAlexis HospitalNo ratings yet
- 30 Items For Funda RLE p2Document6 pages30 Items For Funda RLE p2phoebjaetanNo ratings yet
- Open Fractures and Damage ControlDocument35 pagesOpen Fractures and Damage ControlHamizi MD HanapiahNo ratings yet
- Folio 2022Document10 pagesFolio 2022fila markNo ratings yet