Professional Documents
Culture Documents
Table 25-2
Uploaded by
Dragutin PetrićOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Table 25-2
Uploaded by
Dragutin PetrićCopyright:
Available Formats
Behavioral Medicine: A Guide for Clinical Practice, 5e >Opioids
Mitchell D. Feldman, John F. Christensen, Jason M. Satterfield, Ryan Laponis+
Table 25-2.CDC recommendations for prescribing opioids for chronic pain.
1. Nonpharmacologic therapy and nonopioid pharmacologic therapy are preferred for chronic pain. Clinicians should consider opioid therapy only if expected benefits for both pain and function are anticipated
to outweigh risks to the patient. If opioids are used, they should be combined with nonpharmacologic therapy and nonopioid pharmacologic therapy, as appropriate.
2. Before starting opioid therapy for chronic pain, clinicians should establish treatment goals with all patients, including realistic goals for pain and function, and should consider how therapy will be discontinued
if benefits do not outweigh risks. Clinicians should continue opioid therapy only if there is clinically meaningful improvement in pain and function that outweighs risks to patient safety.
3. Before starting and periodically during opioid therapy, clinicians should discuss with patients known risks and realistic benefits of opioid therapy and patient and clinician responsibilities for managing therapy.
4. When starting opioid therapy for chronic pain, clinicians should prescribe immediate-release opioids instead of extended-release/long-acting (ER/LA) opioids.
5. When opioids are started, clinicians should prescribe the lowest effective dosage. Clinicians should use caution when prescribing opioids at any dosage, should carefully reassess evidence of individual
benefits and risks when increasing dosage to 50 morphine milligram equivalents (MME) or more per day, and should avoid increasing dosage to 90 MME or more per day or carefully justify a decision to
titrate dosage to 90 MME or more per day.
6. Long-term opioid use often begins with treatment of acute pain. When opioids are used for acute pain, clinicians should prescribe the lowest effective dose of immediate-release opioids and should prescribe
no greater quantity than needed for the expected duration of pain severe enough to require opioids. Three days or less will often be sufficient; >7 days will rarely be needed.
7. Clinicians should evaluate benefits and harms with patients within 1–4 weeks of starting opioid therapy for chronic pain or of dose escalation. Clinicians should evaluate benefits and harms of continued
therapy with patients every 3 months or more frequently. If benefits do not outweigh harms of continued opioid therapy, clinicians should optimize therapies and work with patients to taper opioids to lower
dosages or to taper and discontinue opioids.
8. Before starting and periodically during continuation of opioid therapy, clinicians should evaluate risk factors for opioid-related harms. Clinicians should incorporate into the management plan strategies to
mitigate risk, including considering offering naloxone when factors that increase risk for opioid overdose, such as history of overdose, history of substance use disorder, higher opioid dosages (≥50 MME/d),
or concurrent benzodiazepine use are present.
9. Clinicians should review the patient’s history of controlled substance prescriptions using state prescription drug monitoring program (PDMP) data to determine whether the patient is receiving opioid dosages
or dangerous combinations that put him or her at high risk for overdose. Clinicians should review PDMP data when starting opioid therapy for chronic pain and periodically during opioid therapy for chronic
pain, ranging from every prescription to every 3 months.
10. When prescribing opioids for chronic pain, clinicians should use urine drug testing before starting opioid therapy and consider urine drug testing at least annually to assess for prescribed medications as well
as other controlled prescription drugs and illicit drugs.
11. Clinicians should avoid prescribing opioid pain medication and benzodiazepines concurrently whenever possible.
12. Clinicians should offer or arrange evidence-based treatment (usually medication-assisted treatment with buprenorphine or methadone in combination with behavioral therapies) for patients with opioid use
disorder.
Adapted from Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain—United States, 2016. JAMA. 2016;315(15):1624-1645.
Date of download: 12/27/22 from AccessMedicine: accessmedicine.mhmedical.com, Copyright © McGraw Hill. All rights reserved.
You might also like
- Medspan's Pharmacy Guide For OSCEDocument8 pagesMedspan's Pharmacy Guide For OSCEDeviselvamNo ratings yet
- Focus On Nursing SEVENTH EDITION PharmacologyDocument2 pagesFocus On Nursing SEVENTH EDITION PharmacologynananaNo ratings yet
- Steinway Case - CH 03Document5 pagesSteinway Case - CH 03Twēéty TuiñkleNo ratings yet
- ASTM G165-99 (R2005) Standard Practice For Determining Rail-To-Earth ResistanceDocument5 pagesASTM G165-99 (R2005) Standard Practice For Determining Rail-To-Earth Resistance曾乙申100% (1)
- Adapted From CDC Guideline: Assess Pain & FunctionDocument2 pagesAdapted From CDC Guideline: Assess Pain & FunctionSolomon Seth SallforsNo ratings yet
- PocketGuide FINAL6 PDFDocument2 pagesPocketGuide FINAL6 PDFSolomon Seth SallforsNo ratings yet
- Practice Standard: Safe Prescribing of Opioids and SedativesDocument4 pagesPractice Standard: Safe Prescribing of Opioids and SedativesSteve GreenNo ratings yet
- College of Physicians and Surgeons of British Columbia: Safe Prescribing of OpioidsDocument4 pagesCollege of Physicians and Surgeons of British Columbia: Safe Prescribing of OpioidsAshley WadhwaniNo ratings yet
- 2reconsidering Opioid Therapy Mar 2013Document6 pages2reconsidering Opioid Therapy Mar 2013Anonymous 4txA8N8etNo ratings yet
- Guía de OpioidesDocument13 pagesGuía de OpioidesJAIME MUÑOZNo ratings yet
- Introduction To PharmacotherapeuticsDocument49 pagesIntroduction To PharmacotherapeuticsChandraprakash JadhavNo ratings yet
- Chapter 1Document23 pagesChapter 1Kuia AllardeNo ratings yet
- 10 TH Conf Poly PharmacyDocument5 pages10 TH Conf Poly Pharmacytr14niNo ratings yet
- Clinical Paractis Paperghazanfar AYazDocument7 pagesClinical Paractis Paperghazanfar AYazassassain creedNo ratings yet
- Anesthesia Books 2019 Bonica's-2001-3000Document845 pagesAnesthesia Books 2019 Bonica's-2001-3000rosangelaNo ratings yet
- Clinical Pharmacy Complete Notes-CompressedDocument355 pagesClinical Pharmacy Complete Notes-CompressedM. Huzaifa Nasir100% (1)
- Clinical Pocket Guide Tapering-ADocument4 pagesClinical Pocket Guide Tapering-AEdmealemNo ratings yet
- Rational Use of Drugs-IDocument38 pagesRational Use of Drugs-IUmair Mazhar100% (1)
- Pain Management GuidelinesDocument3 pagesPain Management GuidelinesMr. BamsNo ratings yet
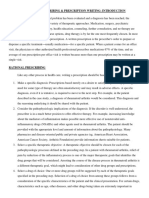
- Rational Prescribing & Prescription Writing: IntroductionDocument3 pagesRational Prescribing & Prescription Writing: IntroductionAnmol KudalNo ratings yet
- Drugs Materials - Prescription of Opioids 2017 AAOMS White PaperDocument2 pagesDrugs Materials - Prescription of Opioids 2017 AAOMS White PaperCathleen LiNo ratings yet
- Anesthesia Books 2019 Bonica's-2001-3000Document1,000 pagesAnesthesia Books 2019 Bonica's-2001-3000rosangelaNo ratings yet
- Prescribing Guidelines-1Document6 pagesPrescribing Guidelines-1nusaiba0313No ratings yet
- Pharmacotherapy PlanDocument25 pagesPharmacotherapy PlanMahum SohailNo ratings yet
- Lect Rational Drug UseDocument23 pagesLect Rational Drug UseNabila putri DelfiantiNo ratings yet
- Ward Round Participation & Drug Therapy MonitoringDocument20 pagesWard Round Participation & Drug Therapy MonitoringAman UpadhyayNo ratings yet
- Nej MP 1512932Document3 pagesNej MP 1512932anggiNo ratings yet
- Acute Post-Op Pain ManagementDocument4 pagesAcute Post-Op Pain Management1234chocoNo ratings yet
- Jurnalnantipsychotic PDFDocument9 pagesJurnalnantipsychotic PDFamiaslimNo ratings yet
- 12 Benar in EnglishDocument3 pages12 Benar in EnglishAjiNo ratings yet
- IntroductionDocument2 pagesIntroductionnusaiba0313No ratings yet
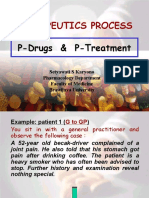
- Pdrugs and P TreatmentDocument66 pagesPdrugs and P TreatmentPoppy Pradina0% (1)
- Drug Utilization ReviewDocument5 pagesDrug Utilization ReviewWàrìs Ràfìqùé ßàlòçhNo ratings yet
- Rational Drug Use and PharmacistDocument4 pagesRational Drug Use and PharmacistJozef CherianNo ratings yet
- Rational Drug Use: Zikria, PH.DDocument47 pagesRational Drug Use: Zikria, PH.DKiran ZahraNo ratings yet
- Draft Revisions To FDA ERLA Opioid Analgesic Education BlueprintDocument10 pagesDraft Revisions To FDA ERLA Opioid Analgesic Education BlueprintIvan BlandeNo ratings yet
- Medication Administration: BY Thomas PetriciniDocument204 pagesMedication Administration: BY Thomas PetricinisaheedvkNo ratings yet
- Patient CounselingDocument12 pagesPatient CounselingPearlNo ratings yet
- Good PrescribingDocument20 pagesGood Prescribingbil sitNo ratings yet
- Pharmacotherapeutics UNIT1Document44 pagesPharmacotherapeutics UNIT1Bharti ChauhanNo ratings yet
- Clinical MidDocument13 pagesClinical MidUmair MazharNo ratings yet
- New Topics in phaRMcology (97-2003)Document18 pagesNew Topics in phaRMcology (97-2003)api-3761895No ratings yet
- Use of Methadone For Opioid Weaning in Children: Prescribing Practices and TrendsDocument8 pagesUse of Methadone For Opioid Weaning in Children: Prescribing Practices and TrendsJessica VillanuevaNo ratings yet
- Rushall Medical Centre Pain Management GPD May 2021Document39 pagesRushall Medical Centre Pain Management GPD May 2021novi irwan fauziNo ratings yet
- Management of ChronincsDocument15 pagesManagement of ChronincsJAIME MUÑOZNo ratings yet
- UNIT4 Clinical PharmacyDocument21 pagesUNIT4 Clinical PharmacyIsha AgarwalNo ratings yet
- 8-Page Version - HHS Guidance For Dosage Reduction or Discontinuation of OpioidsDocument8 pages8-Page Version - HHS Guidance For Dosage Reduction or Discontinuation of OpioidsAnonymous YsPsAHLNo ratings yet
- Pharma Slide 75-100Document27 pagesPharma Slide 75-100Bee LeriosNo ratings yet
- Pdrugs and P TreatmentDocument64 pagesPdrugs and P TreatmentWendz BouvierNo ratings yet
- Colorado Medical Board Policy Guidelines For The Use of Controlled Substances For The Treatment of Pain 12-36-117, C.R.S.Document5 pagesColorado Medical Board Policy Guidelines For The Use of Controlled Substances For The Treatment of Pain 12-36-117, C.R.S.Brian HarrisNo ratings yet
- Lecture 8-Principles of Drug Use in Palliativ EcareDocument6 pagesLecture 8-Principles of Drug Use in Palliativ EcareMachukiNo ratings yet
- Essential Drug UseDocument25 pagesEssential Drug Usegaurang3003No ratings yet
- Vivitrol TreatmentDocument8 pagesVivitrol TreatmentHarish RathodNo ratings yet
- Range Order Proceedure 1Document3 pagesRange Order Proceedure 1mauchkNo ratings yet
- SchizoDocument4 pagesSchizoArlene Bonife MontallanaNo ratings yet
- Drug Use EvaluationDocument27 pagesDrug Use Evaluationshanthi dasariNo ratings yet
- BPJ64 PolypharmacyDocument11 pagesBPJ64 PolypharmacyLimYouhokNo ratings yet
- Acute Pain Management in Patients With Opioid ToleranceDocument6 pagesAcute Pain Management in Patients With Opioid ToleranceHendrikus Surya Adhi PutraNo ratings yet
- Module For Students: Urinary SystemDocument10 pagesModule For Students: Urinary Systemasus kuningNo ratings yet
- Pain ManagementDocument67 pagesPain ManagementMohammad KhoderNo ratings yet
- Therapeutics Process: P-Drugs & P-TreatmentDocument35 pagesTherapeutics Process: P-Drugs & P-TreatmentdesyisrooNo ratings yet
- Pharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceFrom EverandPharmacoepidemiology, Pharmacoeconomics,PharmacovigilanceRating: 3 out of 5 stars3/5 (1)
- ŠizofrenijaDocument216 pagesŠizofrenijaDragutin PetrićNo ratings yet
- Emocionalna Ucjena Susan Forward Donna FraizerDocument153 pagesEmocionalna Ucjena Susan Forward Donna FraizerDragutin PetrićNo ratings yet
- Psychopharmacology (Fourth Edition) (Jerry Meyer) (Z-Library)Document841 pagesPsychopharmacology (Fourth Edition) (Jerry Meyer) (Z-Library)Dragutin PetrićNo ratings yet
- Etika (Benedikt de Spinoza) (Z-Library)Document238 pagesEtika (Benedikt de Spinoza) (Z-Library)Dragutin PetrićNo ratings yet
- Psychopharmacology (Fourth Edition) (Jerry Meyer) (Z-Library)Document841 pagesPsychopharmacology (Fourth Edition) (Jerry Meyer) (Z-Library)Dragutin PetrićNo ratings yet
- World Health Organization - 2007 - Mental Health Policy and Service Guidance PackageDocument168 pagesWorld Health Organization - 2007 - Mental Health Policy and Service Guidance PackageSugra Elena100% (1)
- Clinical Handbook of Psychotropic Drugs, 25e (May 8, 2023) - (0889376328) - (Hogrefe Publishing) (Etc.) (Z-Library)Document555 pagesClinical Handbook of Psychotropic Drugs, 25e (May 8, 2023) - (0889376328) - (Hogrefe Publishing) (Etc.) (Z-Library)Dragutin PetrićNo ratings yet
- Tony Thrasher (Editor) - Emergency Psychiatry (PRIMER ON SERIES) - Oxford University Press (2023)Document537 pagesTony Thrasher (Editor) - Emergency Psychiatry (PRIMER ON SERIES) - Oxford University Press (2023)StefanNo ratings yet
- PsihijatrijaDocument223 pagesPsihijatrijaDragutin PetrićNo ratings yet
- Sepehr Hafizi, Peter B. Jones, Veronika Dobler, Liliana Galindo, Stephen M. Stahl, George Griffiths, Neil Hunt, Mohammad Malkera, Asha Praseedom, Pranathi Ramachandra, Judy Rubinsztein, Shamim RuhiDocument739 pagesSepehr Hafizi, Peter B. Jones, Veronika Dobler, Liliana Galindo, Stephen M. Stahl, George Griffiths, Neil Hunt, Mohammad Malkera, Asha Praseedom, Pranathi Ramachandra, Judy Rubinsztein, Shamim Ruhirakeshbhagtwani5362100% (1)
- Clinical Handbook of Psychotropic Drugs, 25e (May 8, 2023) - (0889376328) - (Hogrefe Publishing) (Etc.) (Z-Library)Document555 pagesClinical Handbook of Psychotropic Drugs, 25e (May 8, 2023) - (0889376328) - (Hogrefe Publishing) (Etc.) (Z-Library)Dragutin PetrićNo ratings yet
- Ipap SchizDocument1 pageIpap SchizDragutin PetrićNo ratings yet
- Emocionalna Ucjena Susan Forward Donna FraizerDocument153 pagesEmocionalna Ucjena Susan Forward Donna FraizerDragutin PetrićNo ratings yet
- Tony Thrasher (Editor) - Emergency Psychiatry (PRIMER ON SERIES) - Oxford University Press (2023)Document537 pagesTony Thrasher (Editor) - Emergency Psychiatry (PRIMER ON SERIES) - Oxford University Press (2023)StefanNo ratings yet
- DSM 5 ScanDocument492 pagesDSM 5 ScanDragutin PetrićNo ratings yet
- Etika (Benedikt de Spinoza) (Z-Library)Document238 pagesEtika (Benedikt de Spinoza) (Z-Library)Dragutin PetrićNo ratings yet
- EtikaDocument218 pagesEtikaDragutin PetrićNo ratings yet
- Dva Ja Nedan Protokol Za Vodenje PsihijatrijskihDocument21 pagesDva Ja Nedan Protokol Za Vodenje PsihijatrijskihDragutin PetrićNo ratings yet
- Agitacija Verbalna DeeskalacijaDocument2 pagesAgitacija Verbalna DeeskalacijaDragutin PetrićNo ratings yet
- Medications Chart Updated 1209Document2 pagesMedications Chart Updated 1209Hannah ClaireNo ratings yet
- DSM 5 ScanDocument492 pagesDSM 5 ScanDragutin PetrićNo ratings yet
- Selected Root Causes of Moral DistressDocument1 pageSelected Root Causes of Moral DistressDragutin PetrićNo ratings yet
- Drug Therapy For Patients With Bipolar DisordersDocument1 pageDrug Therapy For Patients With Bipolar DisordersDragutin PetrićNo ratings yet
- Sepehr Hafizi, Peter B. Jones, Veronika Dobler, Liliana Galindo, Stephen M. Stahl, George Griffiths, Neil Hunt, Mohammad Malkera, Asha Praseedom, Pranathi Ramachandra, Judy Rubinsztein, Shamim RuhiDocument739 pagesSepehr Hafizi, Peter B. Jones, Veronika Dobler, Liliana Galindo, Stephen M. Stahl, George Griffiths, Neil Hunt, Mohammad Malkera, Asha Praseedom, Pranathi Ramachandra, Judy Rubinsztein, Shamim Ruhirakeshbhagtwani5362100% (1)
- Gender PsychiatryDocument12 pagesGender PsychiatryDragutin PetrićNo ratings yet
- AgrsivnostDocument2 pagesAgrsivnostDragutin PetrićNo ratings yet
- Medications Chart Updated 1209Document2 pagesMedications Chart Updated 1209Hannah ClaireNo ratings yet
- Treatment of Patients With SchizophreniaDocument30 pagesTreatment of Patients With SchizophreniaDragutin PetrićNo ratings yet
- Psihijatrija StresDocument250 pagesPsihijatrija StresDragutin Petrić100% (2)
- Albert Ellis & Robert A. Harper - Vodić Kroz Razuman Život (1996, RET Centar)Document241 pagesAlbert Ellis & Robert A. Harper - Vodić Kroz Razuman Život (1996, RET Centar)Brigita Nemet100% (1)
- RFBT - Law On Sales Cont. Week 11Document1 pageRFBT - Law On Sales Cont. Week 11Jennela VeraNo ratings yet
- General Mathematics 2nd Quarter ExamDocument3 pagesGeneral Mathematics 2nd Quarter ExamDeped TambayanNo ratings yet
- Non-Hazardous Areas Adjustable Pressure Switch: 6900P - Piston SensorDocument2 pagesNon-Hazardous Areas Adjustable Pressure Switch: 6900P - Piston SensorDiana ArredondoNo ratings yet
- Multiage Education in Small School SettingsDocument19 pagesMultiage Education in Small School SettingsMichelle Ronksley-PaviaNo ratings yet
- Digest of Ganila Vs CADocument1 pageDigest of Ganila Vs CAJohn Lester LantinNo ratings yet
- Hi 3 Yt 318201Document3 pagesHi 3 Yt 318201partha khatuaNo ratings yet
- SHPXXX 20 IS XX 13Document240 pagesSHPXXX 20 IS XX 13Geyciane PinheiroNo ratings yet
- Pfmar SampleDocument15 pagesPfmar SampleJustin Briggs86% (7)
- One Way Slab DesignDocument10 pagesOne Way Slab DesignBijendra PradhanNo ratings yet
- A88438-23 Critical Procedure 11-01 - Pipeline Cut Outs - A5X9W9Document7 pagesA88438-23 Critical Procedure 11-01 - Pipeline Cut Outs - A5X9W9mahmoudNo ratings yet
- Surface News - 20130704 - Low Res PDFDocument9 pagesSurface News - 20130704 - Low Res PDFYoko GoldingNo ratings yet
- Cyclical Iterative Design Process, Learning From ExperienceDocument7 pagesCyclical Iterative Design Process, Learning From ExperiencemartinsmitNo ratings yet
- Template For Homework6Document2 pagesTemplate For Homework6Никола СтефановићNo ratings yet
- CIE Physics IGCSE: General Practical SkillsDocument3 pagesCIE Physics IGCSE: General Practical SkillsSajid Mahmud ChoudhuryNo ratings yet
- Innova M3 New: 3. InstallationDocument8 pagesInnova M3 New: 3. InstallationAndreea DanielaNo ratings yet
- Danais 150 ActuadoresDocument28 pagesDanais 150 Actuadoresedark2009No ratings yet
- 50 Hotelierstalk MinDocument16 pages50 Hotelierstalk MinPadma SanthoshNo ratings yet
- Analysis and Design of Foundation of ROB at LC-9 Between Naroda and Dabhoda Station On Ahmedabad-Himmatnagar RoadDocument10 pagesAnalysis and Design of Foundation of ROB at LC-9 Between Naroda and Dabhoda Station On Ahmedabad-Himmatnagar RoadmahakNo ratings yet
- Course Syllabus: Ecommerce & Internet MarketingDocument23 pagesCourse Syllabus: Ecommerce & Internet MarketingMady RamosNo ratings yet
- HyderabadDocument3 pagesHyderabadChristoNo ratings yet
- Telstra InterviewsDocument3 pagesTelstra InterviewsDaxShenNo ratings yet
- TM9-238 Deepwater Fording of Ordnance Materiel PDFDocument35 pagesTM9-238 Deepwater Fording of Ordnance Materiel PDFdieudecafeNo ratings yet
- ShinojDocument4 pagesShinojArish BallanaNo ratings yet
- LG LCD TV 32lp1dc - Al-04ca Service ManualDocument47 pagesLG LCD TV 32lp1dc - Al-04ca Service ManualJavin GallardoNo ratings yet
- MODULE 5 - WeirDocument11 pagesMODULE 5 - WeirGrace MagbooNo ratings yet
- French Revolution EssayDocument2 pagesFrench Revolution Essayapi-346293409No ratings yet
- Ex 6 Duo - 2021 Open-Macroeconomics Basic Concepts: Part 1: Multple ChoicesDocument6 pagesEx 6 Duo - 2021 Open-Macroeconomics Basic Concepts: Part 1: Multple ChoicesTuyền Lý Thị LamNo ratings yet
- Instructions: This Affidavit Should Be Executed by The PersonDocument1 pageInstructions: This Affidavit Should Be Executed by The PersonspcbankingNo ratings yet