Professional Documents
Culture Documents
SA Performance
Uploaded by
fernin96Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SA Performance
Uploaded by
fernin96Copyright:
Available Formats
Journal of Perinatology (2018) 38:505–511
https://doi.org/10.1038/s41372-018-0049-3
ARTICLE
Performance of the Silverman Andersen Respiratory Severity Score
in predicting PCO2 and respiratory support in newborns: a
prospective cohort study
Anna Bruett Hedstrom1 Nancy E. Gove2 Dennis E. Mayock1 Maneesh Batra1
● ● ●
Received: 30 July 2017 / Revised: 6 December 2017 / Accepted: 2 January 2018 / Published online: 9 February 2018
© The Author(s) 2018. This article is published with open access
Abstract
Objective: To determine if the Silverman Andersen respiratory severity score, which is assessed by physical exam, within 1
h of birth is associated with elevated carbon dioxide level and/or the need for increased respiratory support.
Study design: Prospective cohort study including 140 neonates scored within 1 h of birth. We report respiratory scores and
their association with carbon dioxide and respiratory support within 24 h.
1234567890();,:
Results: Carbon dioxide level correlated with respiratory score (n = 33, r = 0.35, p = 0.045). However, mean carbon
dioxide for patients with score <5 vs. ≥5 did not differ significantly (56 vs. 67, p = 0.095). Patients with respiratory scores
≥5 had respiratory support increased within 24 h more often than those with scores <5 (79% vs. 28%, p < 0.001).
Conclusion: The Silverman Andersen respiratory severity score may be valuable for predicting need for escalation of
respiratory support and facilitate decision making for transfer in low-resource settings.
Introduction develop respiratory distress syndrome (RDS) due to sur-
factant deficiency, while full-term newborns can suffer from
In 2013, over two million neonates died from the leading infection, meconium aspiration, birth asphyxia or retained
causes of death in children under 5 years of age: pre- lung fluid. There is a critical need for tools to correctly
maturity, sepsis, birth asphyxia and pneumonia [1]. The diagnose and therefore appropriately triage and treat
Millennium Development Goals of 2000 successfully tar- respiratory distress in this population.
geted and reduced childhood mortality, but neonatal deaths Providers in settings where advanced support for
have declined slower than under 5 deaths overall, and hence respiratory failure such as CPAP (continuous positive air-
now almost half of all deaths under 5 years of age occur in way pressure) or mechanical ventilation are not available
the neonatal period [1–3]. The 2014 Every Newborn Action are often faced with the difficult decision regarding when to
Plan highlighted key interventions required to further transfer ill newborns to a facility with higher levels of
reduce global neonatal mortality, and among them both respiratory support. Especially in low-income countries,
immediate newborn care (within the first minutes extending these transfers can be dangerous and draining of family
to one week of age) and care for small or sick babies are resources. Meanwhile, at some facilities, there may be
expected to have the greatest impact on mortality [4]. limited number of respiratory support devices, and deci-
Respiratory complications are common in the newborn sions must be made about who is most appropriate to treat
period. Small babies (a marker for prematurity) often with such therapy. The judicious use of respiratory support
and neonatal transfer, therefore, require an objective mea-
sure for predicting which patients are most likely to require
or benefit from advanced respiratory therapies [5].
* Anna Bruett Hedstrom Recently, facilities in low-resource settings have used the
hedstrom@uw.edu
respiratory severity score (RSS) designed by Silverman and
1
University of Washington/Seattle Children’s Hospital, Andersen in 1956 to quantify respiratory distress among
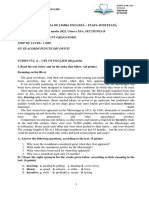
Seattle, WA, United States neonates (Fig. 1) [6–10]. The RSS is objective, easy to
2
Core for Biomedical Statistics, Seattle Children’s Research learn, quick to perform and requires no expensive equip-
Institute, Seattle, WA, United States ment. It can be taught to personnel with limited medical
Content courtesy of Springer Nature, terms of use apply. Rights reserved
506 A. B. Hedstrom et al.
Fig. 1 The Silverman Andersen Respiratory Severity Score (RSS) respiratory distress a “10”. Reprinted with permission from ref. [10] as
evaluates five parameters of work of breathing and assigns an overall modified from ref. [6]
score with a patient breathing comfortably a “0” and a patient in severe
training and can be assessed without physically disturbing for 12 sequential months (November 2015 to October
the patient. Studies of its validity, however, are lacking [8, 2016).
11, 12]. An ideal clinical scoring system would be corre- All neonates admitted to the NICU within 1 h of birth
lated to other laboratory parameters by which respiratory were eligible. Exclusion criteria included intubation prior to
distress is evaluated in high-resource settings to prog- 1 h of life, death within 24 h of birth or diagnosis of hypoxic
nosticate a patient’s respiratory trajectory [13]. ischemic encephalopathy or a primary neuromuscular
This goal of this study was to evaluate the ability of the condition.
Silverman Andersen RSS to identify newborns in current or Hospital assistants (HAs), who were not involved in
impending respiratory distress. Our study objectives were to clinical decision making for the patients, were trained to
determine if the RSS measured within 1 h of birth is asso- assign a respiratory severity score, measure respiratory rate
ciated with: and record respiratory settings. Via convenience sampling,
(1) elevated PCO2 level and/or patients were enrolled only when an HA was able to assign
(2) the impending need for increased respiratory support. a RSS at the time of admission. An RSS was not assigned if
We hypothesized that newborns with high RSS (≥5) an HA was not on duty, too busy or if a patient was
have higher PCO2 (partial pressure of carbon dioxide) swaddled or under sterile drapes. Decisions to obtain blood
values and are more likely to require increased respiratory gases and change respiratory support were at the discretion
support within 24 h compared to those with low RSS (<5). of the medical team with guidance from unit guidelines.
If so, this simple visual assessment tool would show great The medical team was blinded to the RSS. In and out sur-
promise to guide respiratory treatment decisions. factant (for patients failing CPAP) was not the standard of
care in the unit during the study. Demographic information
and respiratory support at 4, 12 and 24 h were abstracted
Materials and methods from the medical record. Patients had incomplete data when
they were transferred to another hospital in the first 24 h.
This was a prospective cohort study in a single-center level Patients who were transferred to mother’s room were
IV neonatal intensive care unit (NICU; University of determined to have had “no increase in respiratory support”
Washington, Seattle, WA, USA). Data collection occurred after transfer.
Content courtesy of Springer Nature, terms of use apply. Rights reserved
Performance of the Silverman Andersen Respiratory Severity Score... 507
Fig. 2 Flowchart of patient
enrollment via convenience
sampling. HA hospital assistant,
RSS Silverman Anderson
Respiratory Severity Score
IRB approval with waiver of consent was obtained from settings of the same mode). Respiratory mode was con-
the University of Washington Human Subjects Division sidered “higher” in the following order: no support<nasal
(Application number 49762). Study data were collected and cannula<high-flow nasal cannula<CPAP<mechanical ven-
managed using REDCap electronic data capture tools hos- tilation. Another post-hoc analysis examined clinical char-
ted at the University of Washington [14]. acteristics of patients below 32 weeks of gestation who did or
did not undergo endotracheal intubation between enrollment
Statistics and 24 h of age.
Descriptive statistics were used to summarize demo-
We used RSS ≥5 for exposure of interest given our graphics. Fisher's exact test was used for the analysis of
experience with CPAP initiation at this threshold in rural associations between the dichotomous variables (RSS group
Uganda [10]. Other settings use cutoffs ranging from 3 to 6 (high/low), any increase in support (Y/N), blood gas taken
for escalation of neonatal respiratory support [7, 8, 15]. For (Y/N) and increase in support mode (Y/N)). The associa-
comparison of RSS with PCO2 and with need for increased tions of the dichotomous variables with the numerical
support, patients were assigned to cohorts of high RSS (≥5) variables (gestation, birth weight, RSS score and PCO2)
and low RSS (<5). Respiratory support was “increased from were analyzed with a two-sided t-test. For the t-test, the
admission” if there was any increase in settings (i.e., flow, normality was assessed graphically and using the
pressure) or change in modality (i.e., room air to high-flow Anderson–Darling test. The normal distribution assumption
nasal cannula or CPAP to mechanical ventilation). For the was violated for the blood gas obtained vs. RSS score, the
comparisons with RSS and whether or not the patient had a respiratory rate vs. the intubation in the first 24 h and the
blood gas taken, the actual value of RSS was used as that RSS score vs. the intubation in the first 24 h; thus, the exact
would increase the power for detecting a difference in the Wilcoxon’s test was used for these comparisons. The
case where one existed to determine if there were differ- Levene test was used to determine if the variance was
ences in the patients who had blood gases taken. The dif- constant across both of the categories in the t-test. The
ferences in gestation, birth weight and actual RSS scores variances was not constant for the gestation age of the
were compared between patients who received blood gas to patients with a blood gas compared to the patients without a
those who did not, as the standard care was used in deter- blood gas; thus, Welch’s two-sample t-test for unequal
mining which patients to draw blood from to evaluate the variance was used. A receiver operating characteristic
blood gas. (ROC) curve was used to evaluate the impact of using
A post-hoc analysis assessed the association between RSS different RSS cutoffs on the detection of increased
and proportion of patients who were increased to a higher respiratory support. For correlation, we will use the guide-
mode of respiratory support (as opposed to just an increase in lines suggested by Evans for the absolute value of r
Content courtesy of Springer Nature, terms of use apply. Rights reserved
508 A. B. Hedstrom et al.
Table 1 Characteristics of enrolled patients with and without blood gas within 1 h of birth
Blood gas obtained (n = 33) No blood gas (n = 107)
Mean (Range) Mean (Range) P-value
Gestation (weeks) 32.5 (24–41) 35.7 (26–42) <0.001**
Birth weight (g) 1924 (574–4286) 2525 (742–4966) <0.001*
RSS 3.9 (0–8) 1.6 (0–10) <0.001†
Proportion (n) Proportion (n) P-value^
Any antenatal steroids 73% (24/33) 36% (37/102) <0.001^
Respiratory support increased in first 24 h 77% (23/30) 26% (21/82) <0.001^
Each analysis is based on available data for that measure, as such denominators differ
RSS Silverman Andersen respiratory severity score
*Two-sided t-test
**Two-sided t-test with unequal variance
^Fisher's exact test
†
Exact Wilcoxon’s rank sum test
Table 2 Mean PCO2 by high vs. low RSS category 0–4
RSS 0–4 (n = 19) RSS 5–10 (n = 14)
Mean (SD) Mean (SD) P-value
Arterial PCO2 56.4 (16.7) 66.7 (17.3) 0.095
Two-sided t-test
difference between those enrolled and not enrolled with
respect to mean gestational age (35.0 vs. 34.1 weeks, p =
0.07), birth weight (2383 vs. 2257 g, p = 0.27) and gender
(49 vs. 48% female, p = 0.87).
Among the 140 patients enrolled, 49% were female,
Fig. 3 Correlation between arterial PCO2 and respiratory sevety score mean gestational age was 35 weeks (SD 3.7), mean birth
weight was 2383 g (SD 896) and 44% had been exposed to
(correlation) as follows, where 0.00–0.19 is very weak, antenatal steroids. At the time of RSS assessment, 59% (n
0.20–0.39 is weak, 0.40–0.59 is moderate, 0.60–0.79 is = 83) were on no respiratory support, 3.6% (n = 5) on nasal
strong and 0.80–1.0 is very strong [16]. cannula, 3.6% (n = 5) on high-flow nasal cannula and
A priori power calculations indicated that we would need 33.6% (n = 47) were on CPAP.
9 patients with blood gases in each study group (high and The 33 enrolled patients had a blood gas within 1 h of
low RSS) to detect a 10 mm Hg PCO2 difference between birth and all were from an arterial source. Patients with a
groups and to demonstrate a 0.36 proportion difference in blood gas were smaller, more premature, had higher RSS,
increased respiratory support, with 80% power at the were more likely to be exposed to antenatal corticosteroids
0.05 significance level. The estimates for the means and and were more likely to have their respiratory support
standard deviations of PCO2 were based on data previously increased in the first 24 h than those who did not have a
reported by Nguyen et al. [17]. blood gas (Table 1). Mean PCO2 correlated to RSS (Fig. 3).
There was a trend towards difference in PCO2 between
patients with low and high RSS but this did not reach sta-
Results tistical significance (Table 2).
Median RSS among those who had their support
Of the 495 patients admitted to the NICU during the period increased in the first 24 h was 4 (range 0–10) vs. 0 (range
of study, 140 were enrolled and had an RSS within 1 h of 0–8) among those whose support was not increased. Among
birth (Fig. 2). No patients were excluded due to a primary all patients, those with high RSS had their respiratory
neuromuscular problem, diagnosis of hypoxic ischemic support increased at each time point assessed more often
encephalopathy or death within 24 h. Of the 298 evaluated than those with low RSS (Table 3). In the post-hoc analysis,
for enrollment, there was no statistically significant the patients with high RSS were also significantly more
Content courtesy of Springer Nature, terms of use apply. Rights reserved
Performance of the Silverman Andersen Respiratory Severity Score... 509
likely to have been increased to a higher mode of respira- significantly in regards to gestational age, birth weight,
tory support (instead of just increased settings of the same arterial PCO2 or respiratory rate during their admission
mode) than those with low RSS (56% (14/25) vs. 16% (16/ exam. The FiO2 and RSS, however, were significantly
98), p < 0.001). higher in those subsequently intubated.
In an a priori analysis restricted to the patients of
28–36 weeks of gestation (n = 72), patients with high RSS
were also more likely to have their respiratory support Discussion
increased in the first 24 h when compared with those with
low RSS (71% vs. 29%, p < 0.01). Elevated RSS within 1 h of birth was strongly associated
The ROC curve (Fig. 4) shows RSS thresholds of ≥3–5 with an increase in respiratory support in the subsequent 24
had similar specificities (83–94%) for predicting an increase h in our study. This relationship was significant at all time
in respiratory support. Sensitivity, however, was greater points assessed (4, 12 and 24 h since birth), suggesting that
with thresholds of ≥3 (78%) and ≥4 (62%) compared with a
threshold of ≥5 (44%). Table 4 Subgroup analysis of patients of <32 weeks of gestation:
A post-hoc analysis examined clinical characteristics of characteristics of those who were and were not intubated in first 24 h
patients below 32 weeks of gestation who did or did not Intubated in Not intubated
undergo endotracheal intubation between enrollment and first 24 h (n = 18)
24 h of age (Table 4). These groups did not differ (n = 9)
Mean (SD) Mean (SD) P-value
Table 3 Frequency of need for increased respiratory support from Gestational age (weeks) 28.4 (1.8) 29.7 (1.8) 0.09†
baseline among newborns with high vs. low RSS category Birth weight (g) 1063 (407) 1225 (291) 0.25†
RSS 0–4 RSS 5–10 Arterial PCO2 (n = 15) 61.9 (17.7) 52.3 (11.5) 0.24†
Time since birth % (n) % (n) P-value FiO2 during RSS (n = 19) 0.35 (0.19) 0.26 (0.9) 0.048*
Respiratory rate during 38.4 (8.8) 42.1 (7.7) 0.12*
4h 17% (16/96) 64% (16/25) <0.001 RSS (bpm)
12 h 24% (21/88) 56% (14/25) 0.003 Respiratory severity score 6.1 (2.1) 2.8 (2.3) 0.003*
24 h 22% (19/88) 54% (13/24) 0.004 Each analysis is based on available data for that measure, as such
Anytime in first 24 h 28% (25/88) 79% (19/24) <0.001 sample size differs
Fisher’s exact test RSS Silverman Andersen respiratory severity score
†
Each analysis is based on available data for that measure, as such Two-sided t-test
sample size differs *Wilcoxon’s rank sum
Fig. 4 Respiratory severity score cutoff to predict increased respiratory Silverman Andersen respiratory severity score, N/A not applicable
support in the first 24 h. a Receiver operating characteristic curve. b given divisor is 0, dns data not sufficient
Sensitivity, specificity and likelihood ratios (LR) of each cutoff. RSS
Content courtesy of Springer Nature, terms of use apply. Rights reserved
510 A. B. Hedstrom et al.
a newborn with an elevated RSS (≥5) could require traditional “predictive” factors for impending intubation,
increased respiratory support anytime in the first 24 h. These such as gestational age, birth weight, arterial PCO2 or
results corroborate the few studies of the clinical correla- respiratory rate, did not. The RSS, therefore, may be helpful
tions of elevated RSS. Very early studies of newborns in determining which patients are at high risk of need for
below 2 kg demonstrated that a RSS of ≥2 was highly subsequent intubation and could be considered for “in and
associated with mortality and subsequent autopsy findings out” surfactant.
consistent with RDS [11, 12]. More recent case series of This study had several strengths. The assets of a high-
preterm patients with respiratory distress showed improve- resource neonatal unit (such as capacity for blood gases and
ment in RSS after treatment with CPAP [7, 10]. In a case retaining patients who needed increased respiratory support)
series from India, a RSS score of 6 at 6 h of age was allowed close following of each patient’s clinical course.
associated with patients who failed CPAP therapy [8]. Although work of breathing is one of the many factors that
Although many facilities in low-resource areas use the medical team uses to decide the amount of respiratory
threshold scores of 3–6 to guide decisions to initiate and support a patient receives, in this study the blinding of the
increase respiratory support, these thresholds have not been team to the RSS was helpful to assess its performance.
validated for their predictive abilities [7–10]. The ROC Meanwhile, the use of carefully trained but medically
curve (Fig. 4) shows that cutoffs of RSS ≥3 or ≥4 would inexperienced hospital assistants suggests this score is fea-
best differentiate patients who subsequently did and did not sible for staff that may be present in lower-resource settings.
need increased respiratory support. However, the pros and A principal limitation of this study was sampling done
cons of false positive vs. a failed detection must be deter- via convenience—most admitted patients (355/495) were
mined for different clinical scenarios. For example, a low- not enrolled. Although we did not find demographic dif-
resource setting may wish to keep only patients unlikely to ferences between those enrolled and not enrolled, this
have impending need for increased support, and might potential for selection bias limits generalizability. Also,
therefore transfer patients with scores of ≥2. Of equal while the choice to obtain the RSS in the first hour is a
importance for this setting, patients with RSS below the reasonable assessment point clinically, the respiratory exam
cutoff are likely to remain stable from a respiratory per- after birth is dynamic and examination at one time point
spective and can avoid the risk, stress and financial burden may not be representative of the patient’s clinical trajectory.
associated with a transfer. Future study, therefore, will require considering all patients
Among the small subset of patients with a blood gas near for enrollment and performing the RSS at additional times
birth, we found that RSS and PCO2 had a statistically sig- to better define its predictive abilities.
nificant linear correlation. However, when patients were In this study, we were unable to verify accuracy of the
segregated into clinically relevant groups (low and high scores assigned and this can be an area of difficulty even
RSS), the relationship was not significant. Our study design among experienced providers. A recent study showed very
was susceptible to selection bias given that not all patients poor inter-rater reliability (IRR) in aspects of the respiratory
had a blood gas assessment; rather only those deemed “ill- exam of term-corrected infants between attending neona-
enough” by the care team. As is the standard of care in the tologists and pulmonologists [18]. As the author points out,
neonatal unit, the clinical team obtained gases on patients these clinicians, however experienced, had no standardized
who were smaller, more premature and appeared to have training for the assessment they were performing. In the
more work of breathing on admission (as indicated by their only study to date of reliability of the RSS, the IRR of the
elevated RSS) compared with those without blood gases. RSS between the doctor and nurses in a low-resource
Few patients with minimal work of breathing (RSS of 0 or neonatal unit who had undergone standardized instruction
1) had blood gases collected. This selection bias is con- (ρ = 0.73) was similar to their agreement on the patient’s
firmed by the mean arterial PCO2 of 60 mm Hg in our respiratory rate (r = 0.86) [10]. Therefore, the imple-
sample, which is markedly elevated from published means mentation of the RSS in any setting should be accompanied
of 41 mm Hg among all newborns on CPAP [17]. We by reliable, standardized instruction.
believe the effect of this bias on our findings was con- The Silverman Andersen Respiratory Severity Score is
servative, and that we may have failed to demonstrate a an easy, quick, non-invasive method to assess newborn
possible association given the paucity of patients with low respiratory distress with a long history of use in many low-
RSS scores and normal-range PCO2. resource settings to guide therapy. It is particularly well
Of interest to settings able to perform endotracheal suited for settings where laboratory, monitoring or diag-
intubation, the post-hoc analysis of very preterm infants nostic abilities and capacity to provide increased respiratory
shows those intubated in first 24 h had significantly higher support are limited. Based on our results, we conclude the
RSS than those not subsequently intubated (Table 4). The RSS may be a valuable tool to predict impending need for
RSS differentiates these groups while some of the other escalation of respiratory support among newborns. This
Content courtesy of Springer Nature, terms of use apply. Rights reserved
Performance of the Silverman Andersen Respiratory Severity Score... 511
should be of particular relevance to clinical decision making 5. Hundalani SG, Richards-Kortum R, Oden M, Kawaza K, Gest A,
regarding judicious timing of transfer for patients who need Molyneux E. Development and validation of a simple algorithm
for initiation of CPAP in neonates with respiratory distress in
increased respiratory support.
Malawi. Arch Dis Child Fetal Neonatal Ed. 2015;100:F332–6.
6. Silverman WA, Andersen DH. A controlled clinical trial of effects
Acknowledgements Samantha J. Nikirk was the Research Coordi- of water mist on obstructive respiratory signs, death rate and
nator. This study was funded by the Seattle Children’s Hospital Center necropsy findings among premature infants. Pediatrics.
for Clinical and Translational Research Academic Enrichment Fund. 1956;17:1–10.
REDCap was provided through the University of Washington Institute 7. Rego MA, Martinez FE. Comparison of two nasal prongs for
of Translational Health Science (ITHS) grant support (UL1TR000423 application of continuous positive airway pressure in neonates.
from NCRR/NIH). Pediatr Crit Care Med. 2002;3:239–43.
8. Tagare A, Kadam S, Vaidya U, Pandit A, Patole S. Bubble CPAP
Compliance with ethical standards versus ventilator CPAP in preterm neonates with early onset
respiratory distress--a randomized controlled trial. J Trop Pediatr.
Conflict of interest The authors declare that they have no conflict of 2013;59:113–9.
interest. 9. Kribs A, Roll C, Gopel W, Wieg C, Groneck P, Laux R, et al.
Nonintubated surfactant application vs. conventional therapy in
extremely preterm infants: a randomized clinical trial. JAMA
Open Access This article is licensed under a Creative Commons
Pediatr. 2015;169:723–30.
Attribution-NonCommercial-NoDerivatives 4.0 International License,
10. McAdams RM, Hedstrom AB, DiBlasi RM, Mant JE, Nyo-
which permits any non-commercial use, sharing, distribution and
nyintono J, Otai CD, et al. Implementation of bubble CPAP in a
reproduction in any medium or format, as long as you give appropriate
rural Ugandan neonatal ICU. Respir Care. 2015;60:437–45.
credit to the original author(s) and the source, and provide a link to the
11. Bauman WA, Nadelhaft J. Chest radiography of prematures; a
Creative Commons license. You do not have permission under this
planned study of 104 patients including clinico-pathologic corre-
license to share adapted material derived from this article or parts of it.
lation of the respiratory distress syndrome. Pediatrics.
The images or other third party material in this article are included in
1958;21:813–24.
the article’s Creative Commons license, unless indicated otherwise in a
12. Bauman WA. The respiratory distress syndrome and its sig-
credit line to the material. If material is not included in the article’s
nificance in premature infants. Pediatrics. 1959;24:194–205.
Creative Commons license and your intended use is not permitted by
13. Downes JJ, Vidyasagar D, Boggs TR Jr, Morrow GM 3rd.
statutory regulation or exceeds the permitted use, you will need to
Respiratory distress syndrome of newborn infants. New clinical
obtain permission directly from the copyright holder. To view a copy
scoring system (RDS score) with acid-base and blood-gas corre-
of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
lations. Clin Pediatr. 1970;9:325–31.
14. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG.
Research electronic data capture (REDCap)--a metadata-driven
References methodology and workflow process for providing translational
research informatics support. J Biomed Inform. 2009;42:377–81.
15. Mathai SS, Raju U, Kanitkar M. Management of respiratory
1. Liu L, Oza S, Hogan D, Perin J, Rudan I, Lawn JE, et al. Global,
distress in the newborn. Med J Armed Forces India.
regional, and national causes of child mortality in 2000-13, with
2007;63:269–72.
projections to inform post-2015 priorities: an updated systematic
16. Evans JD. Straightforward statistics for the behavioral sciences.
analysis. Lancet. 2015;385:430–40.
Pacific Grove: Brooks/Cole Publishing; 1996.
2. United Nations General Assembly. Resolution 55/2, United
17. Nguyen AT, Aly H, Milner J, Patel KM, El-Mohandes A. Partial
Nations Millennium Declaration. 2000 (Available from: http://
pressure of carbon dioxide in extremely low birth weight infants
www.un.org/millennium/declaration/ares552e.htm).
supported by nasal prongs continuous positive airway pressure.
3. Oza S, Lawn JE, Hogan DR, Mathers C, Cousens SN. Neonatal
Pediatrics. 2003;112:e208–11.
cause-of-death estimates for the early and late neonatal periods for
18. Jensen EA, Panitch H, Feng R, Moore PE, Schmidt B. Inter-
194 countries: 2000-2013. Bull World Health Organ.
observer reliability of the respiratory physical examination in
2015;93:19–28.
premature infants: a multicenter study. J Pediatr. 2016;178:87–92.
4. Bhutta ZA, Das JK, Bahl R, Lawn JE, Salam RA, Paul VK, et al.
Can available interventions end preventable deaths in mothers,
newborn babies, and stillbirths, and at what cost? Lancet.
2014;384:347–70.
Content courtesy of Springer Nature, terms of use apply. Rights reserved
Terms and Conditions
Springer Nature journal content, brought to you courtesy of Springer Nature Customer Service Center GmbH (“Springer Nature”).
Springer Nature supports a reasonable amount of sharing of research papers by authors, subscribers and authorised users (“Users”), for small-
scale personal, non-commercial use provided that all copyright, trade and service marks and other proprietary notices are maintained. By
accessing, sharing, receiving or otherwise using the Springer Nature journal content you agree to these terms of use (“Terms”). For these
purposes, Springer Nature considers academic use (by researchers and students) to be non-commercial.
These Terms are supplementary and will apply in addition to any applicable website terms and conditions, a relevant site licence or a personal
subscription. These Terms will prevail over any conflict or ambiguity with regards to the relevant terms, a site licence or a personal subscription
(to the extent of the conflict or ambiguity only). For Creative Commons-licensed articles, the terms of the Creative Commons license used will
apply.
We collect and use personal data to provide access to the Springer Nature journal content. We may also use these personal data internally within
ResearchGate and Springer Nature and as agreed share it, in an anonymised way, for purposes of tracking, analysis and reporting. We will not
otherwise disclose your personal data outside the ResearchGate or the Springer Nature group of companies unless we have your permission as
detailed in the Privacy Policy.
While Users may use the Springer Nature journal content for small scale, personal non-commercial use, it is important to note that Users may
not:
1. use such content for the purpose of providing other users with access on a regular or large scale basis or as a means to circumvent access
control;
2. use such content where to do so would be considered a criminal or statutory offence in any jurisdiction, or gives rise to civil liability, or is
otherwise unlawful;
3. falsely or misleadingly imply or suggest endorsement, approval , sponsorship, or association unless explicitly agreed to by Springer Nature in
writing;
4. use bots or other automated methods to access the content or redirect messages
5. override any security feature or exclusionary protocol; or
6. share the content in order to create substitute for Springer Nature products or services or a systematic database of Springer Nature journal
content.
In line with the restriction against commercial use, Springer Nature does not permit the creation of a product or service that creates revenue,
royalties, rent or income from our content or its inclusion as part of a paid for service or for other commercial gain. Springer Nature journal
content cannot be used for inter-library loans and librarians may not upload Springer Nature journal content on a large scale into their, or any
other, institutional repository.
These terms of use are reviewed regularly and may be amended at any time. Springer Nature is not obligated to publish any information or
content on this website and may remove it or features or functionality at our sole discretion, at any time with or without notice. Springer Nature
may revoke this licence to you at any time and remove access to any copies of the Springer Nature journal content which have been saved.
To the fullest extent permitted by law, Springer Nature makes no warranties, representations or guarantees to Users, either express or implied
with respect to the Springer nature journal content and all parties disclaim and waive any implied warranties or warranties imposed by law,
including merchantability or fitness for any particular purpose.
Please note that these rights do not automatically extend to content, data or other material published by Springer Nature that may be licensed
from third parties.
If you would like to use or distribute our Springer Nature journal content to a wider audience or on a regular basis or in any other manner not
expressly permitted by these Terms, please contact Springer Nature at
onlineservice@springernature.com
You might also like
- 2174 8646 1 PBDocument5 pages2174 8646 1 PBKiran PantheeNo ratings yet
- Prone Positioning in Severe Acute Respiratory Distress SyndromeDocument4 pagesProne Positioning in Severe Acute Respiratory Distress SyndromeJholo AlvaradoNo ratings yet
- Cpap Vs SurfactanteDocument10 pagesCpap Vs SurfactanteAngelicia Varela MuñozNo ratings yet
- Home-Made Continuous Positive Airways Pressure Device May Reduce Mortality in Neonates With Respiratory Distress in Low-Resource SettingDocument5 pagesHome-Made Continuous Positive Airways Pressure Device May Reduce Mortality in Neonates With Respiratory Distress in Low-Resource SettingNovi AryandaNo ratings yet
- 1466 FullDocument15 pages1466 FullMelvy RozaNo ratings yet
- Tto Crup NatureDocument7 pagesTto Crup NatureCarolina Mora RuedaNo ratings yet
- Effectiveness of Prone vs. Supine Position on Respiratory Patterns in NeonatesDocument4 pagesEffectiveness of Prone vs. Supine Position on Respiratory Patterns in NeonatesLaelannie MagpayoNo ratings yet
- Shortacting-sedativeanalgesic-drugs-protect-against-development-of-ventilatorassociated-events-in-children-Secondary-analysis-of-the-EUVAE-study_2021_American-Association-for-Respiratory-CareDocument8 pagesShortacting-sedativeanalgesic-drugs-protect-against-development-of-ventilatorassociated-events-in-children-Secondary-analysis-of-the-EUVAE-study_2021_American-Association-for-Respiratory-CareevyNo ratings yet
- IJN - Volume 11 - Issue 4 - Pages 50-56nbnDocument7 pagesIJN - Volume 11 - Issue 4 - Pages 50-56nbnfitriNo ratings yet
- Bronchiolitis High Risk ApneaDocument7 pagesBronchiolitis High Risk ApneaclikgoNo ratings yet
- Lung Ultrasound Score As A Predictor of Ventilator Use in Preterm Infants With Dyspnea Within 24 H After Dhospitalization PDFDocument8 pagesLung Ultrasound Score As A Predictor of Ventilator Use in Preterm Infants With Dyspnea Within 24 H After Dhospitalization PDFcesar juarezNo ratings yet
- Assessment Nursing Care in Neonatal Respiratory Distress: Qusay H.Mansi, Afifa R. AzizDocument4 pagesAssessment Nursing Care in Neonatal Respiratory Distress: Qusay H.Mansi, Afifa R. AzizGioni ArthurNo ratings yet
- A Framework For The Management of The Pediatric AirwayDocument23 pagesA Framework For The Management of The Pediatric AirwayDaniel GallegoNo ratings yet
- Dyke 2023 Ped Radiol PREFUL Lung MRI Ventilation NICUDocument9 pagesDyke 2023 Ped Radiol PREFUL Lung MRI Ventilation NICUJonathan DykeNo ratings yet
- Aynalem 2020@journal - Pone.0235544Document14 pagesAynalem 2020@journal - Pone.0235544Huệ MinhNo ratings yet
- SurE vs InSurE Surfactant TherapyDocument44 pagesSurE vs InSurE Surfactant TherapySubash PaudealNo ratings yet
- Wright Et Al 2022 PDFDocument9 pagesWright Et Al 2022 PDFRadu CiprianNo ratings yet
- Severity Scoring Systems: Are They Internally Valid, Reliable and Predictive of Oxygen Use in Children With Acute Bronchiolitis?Document7 pagesSeverity Scoring Systems: Are They Internally Valid, Reliable and Predictive of Oxygen Use in Children With Acute Bronchiolitis?Ivan VeriswanNo ratings yet
- Jurnal Pubme 1 RdsDocument13 pagesJurnal Pubme 1 Rdsriri risna aNo ratings yet
- 2010 Early CPAP Vs Surfactant in EPTI NEJMDocument10 pages2010 Early CPAP Vs Surfactant in EPTI NEJMFiorella VilcaNo ratings yet
- NakatoIJP Volume6 Issue9 Pages8215-8223Document9 pagesNakatoIJP Volume6 Issue9 Pages8215-8223Siti HumairahNo ratings yet
- Jurnal Anak RirinDocument10 pagesJurnal Anak RirinDexter BluesNo ratings yet
- Uts KMB - Yovid Nur Azz - 20191660044Document20 pagesUts KMB - Yovid Nur Azz - 20191660044Amjad NabilNo ratings yet
- Factors Influencing Decisions on Weaning Preterm Infants from Noninvasive VentilationDocument18 pagesFactors Influencing Decisions on Weaning Preterm Infants from Noninvasive Ventilationfernin96No ratings yet
- Pulmonary Assessment and Management of Patients with Pediatric Neuromuscular DiseaseFrom EverandPulmonary Assessment and Management of Patients with Pediatric Neuromuscular DiseaseOscar Henry MayerNo ratings yet
- Risks and Outcomes of Infants with Transient Tachypnea of the NewbornDocument5 pagesRisks and Outcomes of Infants with Transient Tachypnea of the NewbornVerushka CrespoNo ratings yet
- 28 - MatthewDocument6 pages28 - MatthewRosa PerezNo ratings yet
- Buonsenso Et Al-2018-Pediatric PulmonologyDocument9 pagesBuonsenso Et Al-2018-Pediatric Pulmonologywawa chenNo ratings yet
- 114 How Parents To Technology Dependent Children Experience The Transition From A Hospital Stay To Professional Home Care NursingDocument1 page114 How Parents To Technology Dependent Children Experience The Transition From A Hospital Stay To Professional Home Care NursingDaniella AwurumibeNo ratings yet
- A Study On Role of Chest X-Rays in Children AboveDocument3 pagesA Study On Role of Chest X-Rays in Children AboveDavid Al HavizNo ratings yet
- Causes and Outcomes of Respiratory Distress in NeonatesDocument8 pagesCauses and Outcomes of Respiratory Distress in NeonatesMohammad AlmuhaiminNo ratings yet
- Diagnosis of Pneumonia in Children With Dehydrating DiarrhoeaDocument6 pagesDiagnosis of Pneumonia in Children With Dehydrating DiarrhoeaEmaa AmooraNo ratings yet
- Resp Emer in ChildrenDocument35 pagesResp Emer in ChildrenvgmanjunathNo ratings yet
- Evidence Based Nursing: Batch 2011Document7 pagesEvidence Based Nursing: Batch 2011Eimhie Lee CasiNo ratings yet
- Quality of Nursing Care Provided For PreDocument16 pagesQuality of Nursing Care Provided For PreAmmar Mustafa Mahadi AlzeinNo ratings yet
- Clinical Predictors of Radiographic Abnormalities Among Infants With Bronchiolitis in A Paediatric Emergency DepartmentDocument5 pagesClinical Predictors of Radiographic Abnormalities Among Infants With Bronchiolitis in A Paediatric Emergency Departmentnavali rahmaNo ratings yet
- Joi 140178Document11 pagesJoi 140178holisNo ratings yet
- Clinical Scores For Dyspnoea Severity in Children: A Prospective Validation StudyDocument11 pagesClinical Scores For Dyspnoea Severity in Children: A Prospective Validation StudyMeylindha Ekawati Biono PutriNo ratings yet
- Bubble CPAP Vs Ventilatory CPAPDocument9 pagesBubble CPAP Vs Ventilatory CPAPRyan Rahman OesmanNo ratings yet
- IDSA Guidelines for Managing Community-Acquired Pneumonia in ChildrenDocument14 pagesIDSA Guidelines for Managing Community-Acquired Pneumonia in ChildrenAaron Nureña JaraNo ratings yet
- Children: Antenatal Corticosteroids: Extending The Practice For Late-Preterm and Scheduled Early-Term Deliveries?Document10 pagesChildren: Antenatal Corticosteroids: Extending The Practice For Late-Preterm and Scheduled Early-Term Deliveries?ADRIANA FERNANDA MENESES AYALANo ratings yet
- Journal Pone 0000192Document5 pagesJournal Pone 0000192TriponiaNo ratings yet
- Basic EcgDocument19 pagesBasic EcgIrma SihotangNo ratings yet
- Clinical Controversies in Aerosol Therapy For Infants and ChildrenDocument23 pagesClinical Controversies in Aerosol Therapy For Infants and Childrencelma44No ratings yet
- PneumoniaDocument18 pagesPneumoniareshma mbbsNo ratings yet
- Newborn Respiratory Distress CausesDocument5 pagesNewborn Respiratory Distress CausesNovia KurniantiNo ratings yet
- Clinical StudyDocument7 pagesClinical StudyAlif ZainalNo ratings yet
- Pneumonia GuidelinesDocument14 pagesPneumonia GuidelinesWilber Martin BaltodanoNo ratings yet
- BBLR 2Document8 pagesBBLR 2Radhiatul AdillahNo ratings yet
- A Randomized Trial of High-Flow Oxygen Therapy in Infants With BronchiolitisDocument11 pagesA Randomized Trial of High-Flow Oxygen Therapy in Infants With BronchiolitisErwin YanthoNo ratings yet
- Clinical Study of Bronchial Asthma in Children Aged 5 To 12 Years With Special Reference To Peak Expiratory Flow RateDocument6 pagesClinical Study of Bronchial Asthma in Children Aged 5 To 12 Years With Special Reference To Peak Expiratory Flow Rateturky hadiNo ratings yet
- NAC en NiñosDocument14 pagesNAC en NiñosAnonymous DxJyWJwtNo ratings yet
- Guler Et Coll (2020) - DONEDocument8 pagesGuler Et Coll (2020) - DONEMaya HammoudNo ratings yet
- The Pediatric Sedation Unit: A Mechanism For Pediatric SedationDocument9 pagesThe Pediatric Sedation Unit: A Mechanism For Pediatric SedationSantosa TandiNo ratings yet
- Lung Recruitment Using Oxygenation during HFVDocument7 pagesLung Recruitment Using Oxygenation during HFVGustavo Carhuamaca RoblesNo ratings yet
- PneumoniaDocument7 pagesPneumoniaAldora OktavianaNo ratings yet
- Surfactant For Respiratory Distress SyndromeDocument12 pagesSurfactant For Respiratory Distress Syndromesanjuy_garzaNo ratings yet
- Mechanical Ventilation of The Premature NeonateDocument16 pagesMechanical Ventilation of The Premature NeonateHaitham HafezNo ratings yet
- JPCC 2380 0534 01 0002 PDFDocument4 pagesJPCC 2380 0534 01 0002 PDFLuiggi D. Chambi MaidaNo ratings yet
- Fluid and Electrolyte Therapy for Pets with Vomiting and DiarrheaDocument22 pagesFluid and Electrolyte Therapy for Pets with Vomiting and Diarrheafernin96No ratings yet
- Lethal Diquat Poisoning Manifesting As Central Pontine Myelinolysis and Acute Kidney Injury - A Case Report and Literature ReviewDocument3 pagesLethal Diquat Poisoning Manifesting As Central Pontine Myelinolysis and Acute Kidney Injury - A Case Report and Literature Reviewfernin96No ratings yet
- Central Pontine Myelinolysis in A Patient With Methamphetamine AbuseDocument10 pagesCentral Pontine Myelinolysis in A Patient With Methamphetamine Abusefernin96No ratings yet
- Central Pontine Myelinolysis - StatPearlsDocument9 pagesCentral Pontine Myelinolysis - StatPearlsfernin96No ratings yet
- Central Pontine Myelinolysis in Pregnancy - A Case of Rare OccurrenceDocument5 pagesCentral Pontine Myelinolysis in Pregnancy - A Case of Rare Occurrencefernin96No ratings yet
- ScoreDocument7 pagesScorefernin96No ratings yet
- Factors Influencing Decisions on Weaning Preterm Infants from Noninvasive VentilationDocument18 pagesFactors Influencing Decisions on Weaning Preterm Infants from Noninvasive Ventilationfernin96No ratings yet
- Clinical pathway for IV fluid therapyDocument13 pagesClinical pathway for IV fluid therapyfernin96No ratings yet
- Lead Research TeamDocument236 pagesLead Research TeamBabas IDNo ratings yet
- ICT Skills MOOC Covers Education BenefitsDocument24 pagesICT Skills MOOC Covers Education Benefitssudheer babu arumbakaNo ratings yet
- Subiect Clasa A XI Sectiunea BDocument4 pagesSubiect Clasa A XI Sectiunea Belenamarin1987No ratings yet
- Problems of Psychology in The 21st Century, Vol. 16, No. 1, 2022Document53 pagesProblems of Psychology in The 21st Century, Vol. 16, No. 1, 2022Scientia Socialis, Ltd.No ratings yet
- Scientific Research Journals (Call For Papers)Document8 pagesScientific Research Journals (Call For Papers)Sr journalsNo ratings yet
- Studies On The Use of Academic Social Networking Sites by Academics and Researchers: A ReviewDocument11 pagesStudies On The Use of Academic Social Networking Sites by Academics and Researchers: A ReviewlibrarianNo ratings yet
- Researchgate vs. Google Scholar: Which Finds More Early Citations?Document7 pagesResearchgate vs. Google Scholar: Which Finds More Early Citations?jramongvNo ratings yet
- IAEME Publication Call For Paper March 2022Document12 pagesIAEME Publication Call For Paper March 2022IAEME PublicationNo ratings yet
- An Analysis of Functional Modelling Approaches Across Disicplines-AnnotatedDocument11 pagesAn Analysis of Functional Modelling Approaches Across Disicplines-AnnotatedKarthik KarunanidhiNo ratings yet
- Art of Writing Research ArticlesDocument40 pagesArt of Writing Research ArticlesjalajaeNo ratings yet
- Linkedin: Recruit Researchers Join For Free LoginDocument3 pagesLinkedin: Recruit Researchers Join For Free LoginlluettaNo ratings yet
- ResearchGate - Find and Share ResearchDocument3 pagesResearchGate - Find and Share Researchakdo.zumNo ratings yet
- Testing "Saintly" Authenticity: Investigations On Two Catacomb SaintsDocument8 pagesTesting "Saintly" Authenticity: Investigations On Two Catacomb SaintsRed OdisseyNo ratings yet
- Aw w5m2Document14 pagesAw w5m2Saujanya SahuNo ratings yet
- Fpe Convocation LectureDocument21 pagesFpe Convocation LectureAdeniji OlusegunNo ratings yet
- Seun Ajayi Paragraphic Letter of MotivationDocument2 pagesSeun Ajayi Paragraphic Letter of MotivationadeNo ratings yet
- SWOT Analysis - Strengths, Weaknesses, Opportunities and ThreatsDocument8 pagesSWOT Analysis - Strengths, Weaknesses, Opportunities and ThreatsMomo NamasteNo ratings yet
- What's The Annual Consumption of Concrete in The WorldDocument2 pagesWhat's The Annual Consumption of Concrete in The WorldSqueak DollphinNo ratings yet
- ResearchGate - An Effective Altmetric Indicator For Active Researchers?Document6 pagesResearchGate - An Effective Altmetric Indicator For Active Researchers?Aura LombanaNo ratings yet
- Ugc Care Journal FormDocument3 pagesUgc Care Journal FormbhasutkarmaheshNo ratings yet
- Scientific Recruitment With ResearchGateDocument16 pagesScientific Recruitment With ResearchGateMuhammad OktaviansyahNo ratings yet
- Ecology Indonesian SeasDocument2 pagesEcology Indonesian SeasÖjiNo ratings yet
- European Management Journal: Pawel Korzynski, Grzegorz Mazurek, Michael HaenleinDocument9 pagesEuropean Management Journal: Pawel Korzynski, Grzegorz Mazurek, Michael HaenleinkharismaNo ratings yet
- Purushottam Sah NP000327 Section B'Document6 pagesPurushottam Sah NP000327 Section B'shaedowNo ratings yet
- The Depression Anxiety Stress Scale DASSDocument2 pagesThe Depression Anxiety Stress Scale DASSMiruna MoanțăNo ratings yet
- This Content Downloaded From 94.67.106.235 On Fri, 05 Nov 2021 15:40:08 UTCDocument17 pagesThis Content Downloaded From 94.67.106.235 On Fri, 05 Nov 2021 15:40:08 UTCGeorgiaSopiadouNo ratings yet
- ResearchGate PDFDocument21 pagesResearchGate PDFChristian Hdez0% (1)
- IAEME Publication Call For Paper February 2024Document23 pagesIAEME Publication Call For Paper February 2024Santosh Kumar Sharma RCBSNo ratings yet
- IAEME Publication Call For Paper June 2021 IssueDocument15 pagesIAEME Publication Call For Paper June 2021 IssueIAEME PublicationNo ratings yet
- AAAAAAADocument4 pagesAAAAAAACaryl Martin100% (2)