Professional Documents
Culture Documents
Control of Acute Respiratory Infections 2
Uploaded by
إحسان ماجد محمد0 ratings0% found this document useful (0 votes)
38 views6 pages1. Acute respiratory infections (ARI) are a major public health problem worldwide, especially in developing countries, where they are the leading cause of death in children under five.
2. ARIs are usually caused by viruses, which account for 90% of upper respiratory infections, though bacterial infections sometimes cause severe disease.
3. The document provides guidelines for classifying and treating ARI cases based on age, symptoms, vital signs, and physical exam findings. Treatments range from home care to antibiotic treatment to emergency hospital referral depending on the severity and risk level.
Original Description:
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document1. Acute respiratory infections (ARI) are a major public health problem worldwide, especially in developing countries, where they are the leading cause of death in children under five.
2. ARIs are usually caused by viruses, which account for 90% of upper respiratory infections, though bacterial infections sometimes cause severe disease.
3. The document provides guidelines for classifying and treating ARI cases based on age, symptoms, vital signs, and physical exam findings. Treatments range from home care to antibiotic treatment to emergency hospital referral depending on the severity and risk level.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
38 views6 pagesControl of Acute Respiratory Infections 2
Uploaded by
إحسان ماجد محمد1. Acute respiratory infections (ARI) are a major public health problem worldwide, especially in developing countries, where they are the leading cause of death in children under five.
2. ARIs are usually caused by viruses, which account for 90% of upper respiratory infections, though bacterial infections sometimes cause severe disease.
3. The document provides guidelines for classifying and treating ARI cases based on age, symptoms, vital signs, and physical exam findings. Treatments range from home care to antibiotic treatment to emergency hospital referral depending on the severity and risk level.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 6
Control of Acute Respiratory Infections (ARI) Program
Acute respiratory tract infection (ARI) is considered as one of the major
public health problems and it is recognized as the leading cause of
mortality and morbidity in many developing countries. The greatest
problem for developing countries is the mortality from ARI in children
less than five year of age. In most countries, ARI occurs more frequently
than any other acute illness, including diarrhea and other tropical
diseases.In developing countries 30% of all patients' consultation and
25% of all pediatric admission are of ARI. Most infections are limited to
the upper respiratory tract and 5% involve the lower respiratory tract.
Incidence of ARI is almost the same all over the world: 5-7 episodes per
child per years in urban areas and 3-5 episodes in rural area.
ARI is mostly caused by both viruses and bacteria. Viral agents account
for 90% of upper respiratory tract infection (URIs), however most of
these infections do not result in fatal sever disease; they are mild and self-
limited illnesses. While bacterial pulmonary infections are common in
developing countries associated with a greater risk of death.
Standard Case Management of ARI
History taken ask about:
a. Age of the patient.
b. Duration of cough.
c. If the child able to drink (2 month to 5 years), or if infant stop feeding
well (< 2 months).
d. If child had fever and was difficult to be awake (for how long).
e. If child had convulsion , difficult breathing and history of cyanosis.
f. History of associated disease like measles and history of treatment.
Physical examination:
a. Count breaths per one minute : Fast breathing is present when
respiratory rate is:
1. 60 or more per one minute for (age <2 months).
2. 50 or more per one minute for (age 2 months up to one year).
3. 40 or more per one minute for (age 1 up to 5 year).
b. Look for chest indrawing :
The child has chest indrawing when lower chest wall goes in when child
breath in. This occur when effort need for breathing more than normal.
c. Look and listen for strider:
Strider is harsh sound when child breathing in. This occurs as a result of
narrowing of upper respiratory passages including (trachea, larynx and
epiglottis).
d. Look and listen for wheeze:
Wheeze is soft musical sound when child breathing out. This occurs as a
result of narrowing of lower respiratory passages.
e. See: if child abnormally sleep or difficult to be a wake.
f. Feel for fever or low body temperature.
g. Check for malnutrition.
H. Check for cyanosis.
Case Classification:
1. Child age less than 2 months: classify into
a. Very severe disease: when any of the following danger signs is
detected:
1. Stop feeding well.
2. Convulsions.
3. Abnormally sleep or difficult to be awake.
4. Strider in previously calm child.
5. Wheezing.
6. Fever or low body temperature.
Treatment: Refer urgently to hospital, keep the infant warm and give
first dose of antibiotic.
b. Severe pneumonia: When the child presented with severe chest
indrawing or fast breathing (≥ 60 / minute).
Treatment: Refer urgently to hospital, keep the infant warm and
give first dose of antibiotic.
c. No pneumonia (cough and cold): when there was no chest
indrawing and no fast breathing.
Treatment: advise the mother about home care including (keep
warm, continue breast feeding, clear nose).Return back to health
center if breathing become difficult or faster or occurrence of any
danger signs.
2. Child age 2 months to 5 years : classify into
a. Very severe disease: when any of the following danger signs is
detected:
1. Not able to drink.
2. Convulsions.
3. Abnormally sleep or difficult to be awake.
4. Strider in previously calm child.
5. Severe malnutrition.
Treatment: Refer urgently to hospital, keep the child warm and
give first dose of antibiotic. Treat fever or wheeze if present.
b. Severe pneumonia: When the child presented with chest indrawing.
Treatment: Refer urgently to hospital, keep the child warm and
give first dose of antibiotic. Treat fever or wheeze if present.
c. Pneumonia: When the child presented with only fast breathing (≥
50 / minute for child age from 2months up to 1 year , ≥ 40 / minute
for child age 1year up to 5 year ) , no chest indrawing.
Treatment: advise the mother about home care including (keep warm,
continue breast feeding, clear nose).Give antibiotic, treat fever and
wheeze if present. Reassess in 2 days (if child improve continue with
treatment for 5 days, if child present with same condition change
antibiotic, if worse refer to hospital).
d. No pneumonia (cough and cold): when there was no chest
indrawing and no fast breathing.
Treatment: advise the mother about home care including (keep warm,
continue breast feeding, clear nose). Treat fever or wheeze if present.
Assess and treat ear or throat problems when present.
Questions:
1. 2 years old female child was brought to PHC with history of
cough and fever for 4 days and not able to drink. On
examination the baby had fever and RR=45/minute. From
above data how you diagnose and treat that patient?
2. 3 years old male child was brought to PHC with history of
cough and fever for 2 days. On examination the baby had fever
and RR=38 /minute and baby had chest indrawing. From above
data how you diagnose and treat that patient?
3. 30 months old male child was brought to PHC with history of
cough and difficulty of breathing for 3 days. On examination
RR=55 /minute and no chest indrawing. From above data how
you diagnose and treat that patient?
4. 10 days old neonate complains from sneezing. On examination
the RR=40/minute, no chest indrawing. Enumerate lines of
treatment.
You might also like
- Acute Respiratory InfectionsDocument26 pagesAcute Respiratory InfectionsSuneel SagareNo ratings yet
- Roll. 66 J 133 Batch PSM AssignmentDocument3 pagesRoll. 66 J 133 Batch PSM AssignmentMishaNo ratings yet
- Control of Diarrheal Diseases (CCD) Definition of DiarrhoeaDocument27 pagesControl of Diarrheal Diseases (CCD) Definition of Diarrhoeaإحسان ماجد محمدNo ratings yet
- Imci Test Quest SamplerDocument6 pagesImci Test Quest Samplerjenalyn_ingaran_sanluisNo ratings yet
- Viral Bronchiolitis GuidelineDocument21 pagesViral Bronchiolitis GuidelineYenni AndrianaNo ratings yet
- Bronchiolitis Clinical Practice GuidelineDocument21 pagesBronchiolitis Clinical Practice GuidelineJuwita PratiwiNo ratings yet
- Cough and Dyspnea Case StudyDocument4 pagesCough and Dyspnea Case StudyAbigail Balbuena100% (1)
- Acute Respiratory Infection (ARI) Programs in Children U5YDocument16 pagesAcute Respiratory Infection (ARI) Programs in Children U5YsamiNo ratings yet
- Case Management of Ari at PHC LevelDocument29 pagesCase Management of Ari at PHC Levelapi-3823785No ratings yet
- IMCIDocument35 pagesIMCIharutoshippuden0No ratings yet
- Pediatric Pneumonia: Signs, Diagnosis and TreatmentDocument29 pagesPediatric Pneumonia: Signs, Diagnosis and TreatmentNur NurhasyanahNo ratings yet
- ARI, Influenza and SarsDocument72 pagesARI, Influenza and SarsKaruna PrasanthNo ratings yet
- IMCI - ContentDocument13 pagesIMCI - ContentMarianne Daphne GuevarraNo ratings yet
- Classification: A. No Pneumonia: Cough or Cold B. PneumoniaDocument2 pagesClassification: A. No Pneumonia: Cough or Cold B. PneumoniaSheryl Nishmae Bernardo SantosNo ratings yet
- EtatDocument121 pagesEtatBhoja Raj GAUTAMNo ratings yet
- Cough, Pediatric: What Are The Causes?Document2 pagesCough, Pediatric: What Are The Causes?astarimediantoNo ratings yet
- MCN 109 A Well High Risk Compilation of ExamsDocument204 pagesMCN 109 A Well High Risk Compilation of ExamsChristine Airah Tanaliga100% (1)
- AEMT - Obstetrics and Pediatrics Exam PracticeDocument26 pagesAEMT - Obstetrics and Pediatrics Exam PracticeEMS DirectorNo ratings yet
- TB Dots: Public Health Nursing Responsibilities (Adult TB)Document7 pagesTB Dots: Public Health Nursing Responsibilities (Adult TB)Roevanie Corpuz CagoNo ratings yet
- Integrated Management On Childhood Illnesses 0101Document132 pagesIntegrated Management On Childhood Illnesses 0101James Felix Gallano Gales100% (1)
- ARI CONTROL PROGRAMMEDocument13 pagesARI CONTROL PROGRAMMEArun George50% (8)
- Breathing Problems in A NewbornDocument2 pagesBreathing Problems in A NewbornMuhammad Danantyo HimawanNo ratings yet
- Approach to Fever in Children: Indications for AntibioticsDocument13 pagesApproach to Fever in Children: Indications for Antibioticsasraf amirullahNo ratings yet
- ALRI Control ProgrammeDocument20 pagesALRI Control ProgrammeDr.G.Bhanu PrakashNo ratings yet
- Presentation of Alina CommunityDocument29 pagesPresentation of Alina CommunitySmita PandeyNo ratings yet
- Casestudy 5Document14 pagesCasestudy 5krystelle jade labineNo ratings yet
- Name: Muhib Abdullah Karim S T U D e N T I D: 2 1 1 1 6 2 9 6 3 0 Course: Introduction To Public Health Faculty: AFC Section: 6Document11 pagesName: Muhib Abdullah Karim S T U D e N T I D: 2 1 1 1 6 2 9 6 3 0 Course: Introduction To Public Health Faculty: AFC Section: 6Nazifa IbnatNo ratings yet
- Work SheetDocument5 pagesWork Sheettefesih tube ተፈስሕ ቲዮብNo ratings yet
- Case Write Up 2Document16 pagesCase Write Up 2Shidev100% (1)
- Sas 26Document2 pagesSas 26Gwenn SalazarNo ratings yet
- Pneumonia Case StudyDocument14 pagesPneumonia Case StudyMaryann LayugNo ratings yet
- Micro para Laboratory Activity 4 - Case Study 2Document5 pagesMicro para Laboratory Activity 4 - Case Study 2Vannesa TarifaNo ratings yet
- Contoh MCQ PediDocument9 pagesContoh MCQ PediPrillye DeasyNo ratings yet
- CASE SIMUlation 112Document6 pagesCASE SIMUlation 112Princess Levie CenizaNo ratings yet
- SEO-Optimized Title for Febrile Seizures and Ear Infection DocumentDocument6 pagesSEO-Optimized Title for Febrile Seizures and Ear Infection DocumentKirstin del CarmenNo ratings yet
- IMCIDocument2 pagesIMCIxtinemarie_d4977No ratings yet
- Acute Respiratory InfectionDocument68 pagesAcute Respiratory InfectionArun GeorgeNo ratings yet
- Ari Workshop.2Document40 pagesAri Workshop.2drusmanjamilhcmdNo ratings yet
- Ped Paper CaseDocument9 pagesPed Paper CaseImmah PinedaNo ratings yet
- Kristia Carpio Pulmonary TuberculosisDocument31 pagesKristia Carpio Pulmonary TuberculosiskisNo ratings yet
- Ca1 Diagnostic ExamDocument17 pagesCa1 Diagnostic ExamMJ O. JulianoNo ratings yet
- IMCIDocument42 pagesIMCIMichael Anthony ErmitaNo ratings yet
- Chronic Cough In Children, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandChronic Cough In Children, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Doc-20240131-Wa0 240131 224959Document3 pagesDoc-20240131-Wa0 240131 22495922alhumidi2020No ratings yet
- IMCI Nov 2009Document141 pagesIMCI Nov 2009togononkaye100% (1)
- Final Case Study PCAPDocument73 pagesFinal Case Study PCAPMaria Norilyn75% (4)
- Integrated Management of Childhood Illness Flip ChartDocument78 pagesIntegrated Management of Childhood Illness Flip ChartkjtomananNo ratings yet
- Primary ComplexDocument12 pagesPrimary ComplexLevi PosadasNo ratings yet
- Fever in 18-Month-OldDocument2 pagesFever in 18-Month-Oldkenmcmillin100% (1)
- Pubdoc 4 14280 150Document6 pagesPubdoc 4 14280 150jadarcNo ratings yet
- BronchiolitisDocument4 pagesBronchiolitistingtingcrazyNo ratings yet
- Acute Respiratory Infections: Streptococcus PneumoniaeDocument9 pagesAcute Respiratory Infections: Streptococcus Pneumoniaesunma09082001No ratings yet
- Clinical Signs in PaediatricsDocument24 pagesClinical Signs in PaediatricsNURUL AFZA MOHD SHAMSUL KAMALNo ratings yet
- Bronchiolitis ScriptDocument6 pagesBronchiolitis ScriptAhmed RmelahNo ratings yet
- Pneumonia PDFDocument3 pagesPneumonia PDFSari RamadhanNo ratings yet
- Boy's Severe Asthma & Cystic Fibrosis CaseDocument3 pagesBoy's Severe Asthma & Cystic Fibrosis CaseElsayed MohamedNo ratings yet
- Pneumonia: - It Is An Inflammation and Consolidation ofDocument44 pagesPneumonia: - It Is An Inflammation and Consolidation ofBinita ShakyaNo ratings yet
- Febrile convulsions: assessment, treatment and educationDocument12 pagesFebrile convulsions: assessment, treatment and educationPalash NagdeoteNo ratings yet
- CasesDocument25 pagesCasesfatemaNo ratings yet
- Case Write Up on 1-Year-Old Boy with Cough and Rapid BreathingDocument7 pagesCase Write Up on 1-Year-Old Boy with Cough and Rapid Breathinganon_67984147No ratings yet
- Manual diskAshur-PRO - HDDSSD enDocument38 pagesManual diskAshur-PRO - HDDSSD enإحسان ماجد محمدNo ratings yet
- Family Transfer DetailsDocument1 pageFamily Transfer Detailsإحسان ماجد محمدNo ratings yet
- Maternal Health During Pregnancy عمليDocument4 pagesMaternal Health During Pregnancy عمليإحسان ماجد محمدNo ratings yet
- TuberculosisDocument5 pagesTuberculosisإحسان ماجد محمدNo ratings yet
- Candidiasis Opportunistic Mycosis Within Nigeria: A ReviewDocument6 pagesCandidiasis Opportunistic Mycosis Within Nigeria: A ReviewUMYU Journal of Microbiology Research (UJMR)No ratings yet
- Bahan Paparan Prof. Ratu Ayu - Guest Lecture OH 27 Agustus 2021 Rev3 VfinalDocument23 pagesBahan Paparan Prof. Ratu Ayu - Guest Lecture OH 27 Agustus 2021 Rev3 VfinalZulkarnaenUchihaNo ratings yet
- Acute Otitis Media in Young Children - Diagnosis and MGT PDFDocument9 pagesAcute Otitis Media in Young Children - Diagnosis and MGT PDFdanny17phNo ratings yet
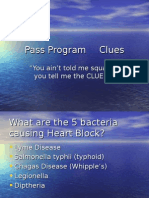
- Pass Program CluesDocument851 pagesPass Program CluesAlfyGototron100% (1)
- Nutrition and Exercise ImmunologyDocument204 pagesNutrition and Exercise ImmunologytodayisnovemberNo ratings yet
- Gastritis CronicaDocument12 pagesGastritis CronicaKati RondonNo ratings yet
- Questions ExplanationDocument20 pagesQuestions ExplanationnomintmNo ratings yet
- The Great Imitator A Rare Case of Lues Maligna in An Hiv Positive Patient 4Document4 pagesThe Great Imitator A Rare Case of Lues Maligna in An Hiv Positive Patient 4Talaat OmranNo ratings yet
- Draf LaporanDocument18 pagesDraf LaporanNers officialNo ratings yet
- Microbiology QuestionsDocument5 pagesMicrobiology QuestionsNaeem AminNo ratings yet
- Jurnal DBDDocument10 pagesJurnal DBDFirman FajriNo ratings yet
- Reference 1. Satyanarayanajois, S., Stephanie, V., Liu, J., Go, M.L., 2009, Design, Synthesis, and Docking Studies ofDocument1 pageReference 1. Satyanarayanajois, S., Stephanie, V., Liu, J., Go, M.L., 2009, Design, Synthesis, and Docking Studies ofScholastika Palayukan100% (1)
- AbscessDocument3 pagesAbscessSandeep SinghNo ratings yet
- Molecular Diagnostics of Infectious Diseases, 2010, PGDocument207 pagesMolecular Diagnostics of Infectious Diseases, 2010, PGrieza_husein100% (2)
- Chain of Infection: Mr. Migron Rubin M.Sc. Nursing StudentDocument43 pagesChain of Infection: Mr. Migron Rubin M.Sc. Nursing StudentJarnel CabalsaNo ratings yet
- Green BookDocument287 pagesGreen Bookrahanian100% (1)
- Program Hivr4p2018Document90 pagesProgram Hivr4p2018jadwongscribdNo ratings yet
- 5.2 PhysDocument39 pages5.2 PhysshivaniNo ratings yet
- Prion Diseases and MeningitisDocument39 pagesPrion Diseases and Meningitisraanja2No ratings yet
- DR Dina - TB & CovidDocument10 pagesDR Dina - TB & CovidDina FaizahNo ratings yet
- Sharma - 2023 - Emerging Evidence On Monkeypox - Resurgence, Global Burden, Molecular Insights, Genomics and Possible ManagementDocument21 pagesSharma - 2023 - Emerging Evidence On Monkeypox - Resurgence, Global Burden, Molecular Insights, Genomics and Possible ManagementIsabella FernandesNo ratings yet
- Journal of Internal Medicine - 2023 - Okushin - Ursodeoxycholic Acid For Coronavirus Disease 2019 PreventionDocument4 pagesJournal of Internal Medicine - 2023 - Okushin - Ursodeoxycholic Acid For Coronavirus Disease 2019 PreventionCT DAMNo ratings yet
- Complement SystemDocument4 pagesComplement SystemFait HeeNo ratings yet
- Immunization Requirements For Students in K12 in Texas 2018Document4 pagesImmunization Requirements For Students in K12 in Texas 2018KCEN Channel 6No ratings yet
- Herpes Opportunity Disclosure Handout 2Document1 pageHerpes Opportunity Disclosure Handout 2Thong Huynh100% (1)
- The Blood PoisonersDocument45 pagesThe Blood Poisonersgreatha marmalNo ratings yet
- Tyhpoid FeverDocument6 pagesTyhpoid FeverMade Oka Heryana100% (1)
- Epidemiology of Escherichia Coli Bacteremia: A Systematic Literature ReviewDocument9 pagesEpidemiology of Escherichia Coli Bacteremia: A Systematic Literature ReviewMaria Chacón CarbajalNo ratings yet
- Concept Map - MumpsDocument4 pagesConcept Map - MumpsElleNo ratings yet
- Celiac DiseaseDocument42 pagesCeliac DiseaseTri P BukerNo ratings yet