Professional Documents
Culture Documents
Cardiovascular Disorders
Uploaded by
Christine Evan HoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cardiovascular Disorders
Uploaded by
Christine Evan HoCopyright:
Available Formats
OBSTETRICS 2
Cardiovascular
3S-2 | CEU-SOM A & B
ELEYNETH I. VALENCIA, MD, FPOGS, FPSUOG
Disorders
OUTLINE Ø At 30-32 weeks: repeat CBC to check if maternal iron supplement
is sufficient
I. CARDIOVASCULAR PHYSIOLOGY Ø If with heart disease: the heart cannot always accommodate these
II. DIAGNOSIS OF HEART DISEASE changes
III. PERIPARTUM MANAGEMENT CONSIDERATIONS Ø Ventricular dysfunction leads to cardiogenic heart failure
IV. SURGICALLY CORRECTED HEART DISEASE Ø In most, HEART FAILURE develops PERIPARTUM
V. VALVULAR HEART DISEASE o In labor
VI. CONGENITAL HEART DISEASE o During delivery
VII. PULMONARY HYPERTENSION o (+) several obstetric conditions that may add burden e.g.,
VIII. CARDIOMYOPATHIES preeclampsia, hemorrhage, anemia, and sepsis
IX. HEART FAILURE
X. INFECTIVE ENDOCARDITIS U One of the recommendations of the Society of Maternal and Fetal
XI. ISCHEMIC HEART DISEASE Medicine, patients with cardiovascular disease should stay in the
XII. REFERENCE hospital for at least 10 days postpartum.
XIII. APPENDIX
EFFECT OF PREGNANCY ON HEART DISEASE
MATERNAL MORTALITY
Worsening Cardiac Status: decomposition (heart failure)
Ø Between 2011 to 2013: previously responsible for maternal deaths
– declining Ø During pregnancy: increase CO at 28-32 weeks
Ø Hemorrhage Ø During labor: due to stress of labor
Ø Hypertensive Disorders Ø After delivery: the most dangerous period due to sudden return of
Ø Embolism the blood to the general circulation
Ø Cardiovascular disorders: 26% of pregnancy related deaths
VENTRICULAR FUNCTION IN PREGNANCY
Prevalence
Ø ↑ end systolic and systolic dimensions
Ø Rising prevalence is due to: Ø Septal thickness/Ejection Fraction are unchanged
Ø Obesity Ø Ventricular remodeling – plasticity (eccentric expansion of the L.
Ø Hypertension ventricular mass – 30-35% near term)
Ø Diabetes
Ø National Center for Health Statistics & Remodeling will return to its pre-pregnancy values usually on the
Ø Almost ½ of adults aged ≥20 – at least 1 risk factor 6th to 12th weeks postpartum
Ø Delayed childbearing
II. DIAGNOSIS OF HEART DISEASE
I. CARDIOVASCULAR PHYSIOLOGY
Physiological adaptations of normal pregnancy
Marked Pregnancy-Induced Anatomical and Functional Changes in o Induce symptoms
Cardiac Physiology → profound effect on underlying heart disease o Alter clinical findings
o Confound the diagnosis of heart disease
1. Cardiac Output: increased 40% (at term; ½ of total by 8 weeks
and max by midpregnancy) Normal pregnancy
2. ↑ Stroke Volume o Functional systolic heart murmur common
3. ↓ Vascular resistance o Accentuated respiratory effort
4. ↑ Resting pulse and SV due to ↑ EDV from pregnancy o Lower extremity edema after midpregnancy
hypervolemia o Fatigue and exercise intolerance
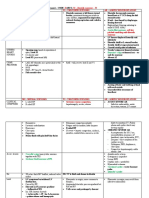
VARIABLE CHANGE NORMAL PREGNANCY INDICATORS OF
Cardiac Output Increased by 30-50% ISCHEMIC HEART DISEASE
Strove Volume Increases to a maximum of 85 mL at 20 weeks of Mild dyspnea Severe or progressive dyspnea
gestation Fatiguability Syncope with exertion
Heart rate Increased (approaches 90-100 bpm at rest during the Decreased exercise tolerance Chest pain with effort of emotion
3rd trimester Chest pain at rest
Systemic Decrease 21% (nadir at 14-24 weeks; around 1200 Table 2. Indicators of Ischemic Heart Disease
Vascular dyne/s/cm5)
Resistance Clinical indicators of heart disease during pregnancy
Pulmonary Decrease by 34% to a nadir of 78 dyne/s/cm5
Vascular
Ø Symptoms
Resistance o Progressive dyspnea or orthopnea
Pulmonary No significant change o Nocturnal cough, hemoptysis, syncope, chest pain
Capillary
Wedge Ø Clinical findings
Pressure Ø Cyanosis, clubbing of fingers
Colloid Decreased by 14% (associated with a decrease in Ø Persistent neck vein distension
Osmotic serum osmolarity noticed as early as first trimester of Ø Systolic murmur grade 3/6 or greater
Pressure pregnancy)
Ø Diastolic murmur, cardiomegaly
Hemoglobin Decreased (maximum hemodilution is achieved at 30-
Concentration 32 weeks) Ø Persistent arrythmia
Table 1. Physiologic changes during pregnancy Ø Persistent split – second sound
Ø Criteria for pulmonary hypertension
3S-2 CARDIOVASCULAR DISORDERS ESTUYE • HO • JAVIER • PASAJOL • RAMOS • ROCHA
PAGE 1 of 9
DIAGNOSTIC STUDIES
Noninvasive cardiovascular studies such as electrocardiography, chest
radiography, and echocardiography will provide data necessary for
evaluation
Normal Diagnostic Studies
Ø ECG
o Average of 15º left axis deviation – diaphragm is elevated in
advancing pregnancy
o Reduced PR interval
o Inverted or flattened T waves
o Voltage findings not altered
o Atrial and ventricular premature contractions – relatively
frequent
Ø Chest X-ray
o AP and lateral views
o Must use lead apron shield – fetal radiation exposure –
minimal
o Slight heart enlargement – not detected accurately due to
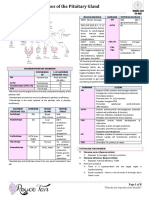
heart silhouette larger in pregnancy Table 4. WHO risk classifIcation of CVD & pregnancy
Ø Echocardiography (2D-echo) PRECONCEPTIONAL COUNSELLING
o Widely used; permits accurate diagnosis of most heart
diseases Ø Most especially beneficial for patients with SEVERE heart disease
o Some normal pregnancy-induced changes: Ø Referred for Maternal-Fetal Medicine or Cardio Consult
§ Small increase in dimensions of the cardiac chambers Ø Must identify life threatening cardiac abnormalities
§ Slight growth in the left ventricular mass Ø Fetal teratogenic concerns
§ Tricuspid and mitral valve regurgitation Ø Issues on congenital heart lesions
Ø Cardiovascular MRI III. PERIPARTUM MANAGEMENT CONSIDERATIONS
o With higher reproducibility
o Less hindered by ventricular geometry and body habitus Ø Team approach: OB, Cardiologist, Anesthesiologist and other
o classification of functional heart disease specialties as needed
Ø Prognosis and Management: Influenced by the TYPE and
SEVERITY of lesions and MATERNAL FUNCTIONAL
CLASSIFICATION
Ø NYHA Class I and most in NYHA Class II – may negotiate
pregnancy without morbidity
§ If III and IV: pregnancy is contraindicated
Ø To prevent or to early recognize HF
Ø Identify infection or sepsis syndrome that can precipitate HF
Ø To avoid contact with respiratory infections
Ø Pneumococcal and influenza vaccines recommended
Ø Cigarette smoking prohibited
Ø Illicit drug use is prohibited
Ø peripartum management
CLASSIFICATION OF FUNCTIONAL HEART DISEASE Ø NYHA Class III and IV are UNCOMMON
Ø If a woman chooses pregnancy: MUST understand the risk and
must be encouraged to be compliant with PLANNED CARE
§ (+) prolonged hospitalization or bed rest is often
necessary with continued plan of care
Table 3. Clinical classification of the New York Heart Association based on the
past and present disability uninfluenced by physical signs
Space Filler
3S-2 CARDIOVASCULAR DISORDERS ESTUYE • HO • JAVIER • PASAJOL • RAMOS • ROCHA
PAGE 2 of 9
LABOR AND DELIVERY Ø Over-all estimated maternal mortality rate: 1.2
Ø Pregnancy FREE of SERIOUS complications:
Ø In general o Mechanical: 58%; increased risk of thrombosis
o Vaginal Delivery is preferred o Tissue Heart Valve: 79%
o Labor induction is usually safe o Porcine Tissue Valves: safer; anticoagulation not required;
Ø Planned CS conferred NO ADVANTAGE for maternal or neonatal less durable; longevity average 10-15 years
outcome
o Limited to obstetrical indications Anticoagulation
o For specific cardiac lesions
o Over all maternal condition Ø Critical for women with mechanical prosthetic valves
o Availability of experience, Anesthesia personnel and hospital Ø Warfarin – risk HIGH: mean daily dose >5 mg; embryopathy >8%
capabilities o Most effective anticoagulant for preventing maternal
Ø Mother in labor – kept in semi-recumbent position (left lateral) thromboembolism
with lateral tilt o Teratogenic, causes miscarriage, still births
Ø VS taken frequently between contractions Ø Heparin – is less hazardous for fetus – ↑ thromboembolism
Ø Watch out for impending ventricular failure: PR: >100 bpm or
RR >24 cpm Pregnancy after Heart Transplantation
Ø Cesarean Section is recommended:
o Dilated aortic root >4 cm or aortic aneurysm Ø May have successful pregnancies following cardiac
o Acute severe congestive heart failure transplantation
o Recent myocardial infarction Ø International Society of Heart and Lung Transplantation: Don’t
o Severe aortic stenosis discourage pregnancy in stable heart transplant recipients > 1 year
o Warfarin administration within 2 weeks of delivery posttransplant
o Need for emergency valve replacement immediately after
delivery V. VALVULAR HEART DISEASE
RHEUMATIC FEVER
Analgesia and Anesthesia
Ø Uncommon in the US because of:
Ø Relief from pain and apprehension o less crowded living conditions
Ø IV anesthesia: satisfactory relief for pain o penicillin availability
Ø Continuous epidural anesthesia is recommended o evolution of non-rheumatogenic streptococcal strains
Ø Still remains the chief cause of serious mitral valvular disease in
Intrapartum Heart Failure women of childbearing age
Ø Cardiovascular decompensation during labor: MITRAL STENOSIS
o Pulmonary edema (tx with diuresis)
o Hypoxia Ø Rheumatic endocarditis causes most mitral stenosis
o Hypotension Ø For severe stenosis: L atrium dilates, elevated L atrial pressure,
significant passive pulmonary hypertension develops.
PUERPERIUM Ø These women have a relatively fixed CO, thus, the increased
preload of normal pregnancy and other factors that raise CO may
Ø May still decompensate postpartum cause ventricular failure and pulmonary edema
Ø Fluid is mobilized into intravascular compartment Ø (+) dyspnea, fatigue, palpitations, cough, hemoptysis
Ø Reduced peripheral vascular resistance place higher demands
on myocardial performance PREGNANCY OUTCOMES
Ø Worsen heart failure:
o PPH Ø 43% develops heart failure
o Anemia Ø 20% develops arrhythmias
o Infection Ø IUGR common for mitral valve area < 1 cm2
o Thromboembolism Ø Prognosis depends on functional capacity: 8 out of 10 deaths for
Ø Severe preeclampsia may cause or worsen pulmonary edema NYHA Classes III or IV
Ø Puerperal tubal sterilization – after VD – delayed after SEVERAL
DAYS MANAGEMENT
Ø Mother is hemodynamically stable, afebrile, not anemic,
ambulatory Ø Limited physical activities
Ø If with pulmonary congestion: dietary Na restriction + diuretics
IV. SURGICALLY CORRECTED HEART DISEASE Ø Beta-blocker if tachycardic
Ø Surgical intervention: mitral valve area is 1.5-2 cm2
Ø Significant congenital heart lesions – repaired during childhood Ø Ideal for delivery: vaginal delivery under epidural anesthesia
Ø Not diagnosed until adulthood:
o ASD
o Pulmonic stenosis
o Bicuspid Aortic Valve
o Aortic Coarctation
Ø Some are mild and surgery NOT required
Ø If for surgery, IDEALLY performed BEFORE pregnancy
Valve Replacement Before Pregnancy
Ø Prosthetic mitral or aortic valve → may cause MI, anticoagulation
is needed
Ø Type of valve:
o Mechanical
o Biological
3S-2 CARDIOVASCULAR DISORDERS ESTUYE • HO • JAVIER • PASAJOL • RAMOS • ROCHA
PAGE 3 of 9
o Symptomatic: strict limitation of activity, treatment of
infection; surgery
MITRAL INSUFFICIENCY
Ø Trivial degree of mitral insufficiency is found in normal patients
Ø If mitral valve leaflets align improperly during systole – abnormal
degrees of mitral regurgitation can develop
Ø Followed by left ventricular dilatation, eccentric hypertrophy
Ø Acute mitral insufficiency is caused by:
o Chordae tendinae rupture
o Papillary muscle infarction
o Leaflet perforation
Ø Chronic mitral regurgitation is caused by:
o Rheumatic fever
o Connective tissue disease
Ø Mitral valve vegetations: Libman-Sacks endocarditis relatively
common in women with antiphospholipid antibodies, sometimes
coexist with SLE
Ø Mitral Regurgitation is tolerated in pregnancy because the lowered
systemic vascular resistance yields less regurgitation AORTIC INSUFFICIENCY
MITRAL VALVE PROLAPSE (MVP) Ø Allows diastolic flow of blood from the aorta back into the LV
Ø Frequent causes:
Ø This diagnosis implies the presence of pathological connective o Rheumatic fever
tissue disorder – myxomatous degeneration – which may involve o Connective tissue abnormalities
the valve leaflets, annulus, chordae tendinae o Congenital lesions
Ø Usually asymptomatic and are diagnosed during routine Ø Acute insufficiency may develop from bacterial endocarditis
examination or echocardiography Ø Symptoms: slow onset fatigue, dyspnea, pulmonary edema
Ø Pregnant women with MVP rarely have cardiac complications Ø Generally well-tolerated during pregnancy due to diminished
Ø For symptomatic women, give beta-blocking agents – decrease vascular resistance (improve hemodynamic function)
sympathetic tone, relieve chest pain and palpitations, and reduce Ø Treatment: diuretics and bed rest (if symptoms of heart failure
risk of life-threatening arrhythmias develops)
Ø Women with symptoms have anxiety, palpitations, atypical chest
pain, dyspnea with exertion and syncope
PULMONARY STENOSIS
Ø Usually congenital and may be associated with Tetralogy of Fallot
or Noonan syndrome.
Ø The greater hemodynamic burden of pregnancy can precipitate
right sided HF or atrial arrhythmias in women with severe stenosis
Ø Surgical correction: ideal before pregnancy
AORTIC STENOSIS VI. CONGENITAL HEART DISEASE
Ø A disease of aging; if in young: congenital lesion Ø Most common type of heart disease encountered in pregnancy
Ø Concentric L ventricle hypertrophy → increase end diastolic Ø Greater maternal mortality rates
pressure → decrease ejection fraction → CO
Ø Manifestations: chest pain, syncope, heart failure, sudden death ATRIAL SEPTAL DEFECT
from arrhythmias
Ø Life expectancy after exertional chest pain develops: 5 years Ø ¼ of all adults has a patent foramen ovale
Ø In pregnancy: mild – mod – well tolerated Ø Most ASDs are asymptomatic until 3rd to 4th decade
Ø Maternal mortality rate: 8% Ø Secundum type defect accounts for 70%, and associated with
Ø Management: mitral valve myxomatous abnormalities with prolapse
o Asymptomatic: no treatment, observe Ø If discovered in childhood → repair
Ø Pregnancy is well tolerated unless pulmonary hypertension has
developed (uncommon)
Ø Treatment of ASD during pregnancy is indicated for congestive
heart failure or an arrhthmia
Ø Right → Left shunt: paradoxical embolism – entry of venous
thrombus through the defect and into the systemic arterial
circulation may cause embolic stroke
3S-2 CARDIOVASCULAR DISORDERS ESTUYE • HO • JAVIER • PASAJOL • RAMOS • ROCHA
PAGE 4 of 9
PATENT DUCTUS ARTERIOSUS
Ø The ductus connects the proximal left pulmonary artery to the
ascending aorta just distal to the L subclavian artery
Ø Functional closure from vasoconstriction occurs shortly after birth
Ø If persistent and unrepaired: high mortality after the 5th decade
Ø Pregnancy: develops pulmonary hypertension, heart failure,
cyanosis if systemic blood pressure falls and leads to shunt
reversal of blood from the pulmonary artery into the aorta; sudden
hypotension at delivery after regional anesthesia or hemorrhage
may lead to fatal collapse
VENTRICULAR SEPTAL DEFECT
Ø Close spontaneously during childhood in 90% of cases
Ø Most defects are paramembranous, and the degree of left-to-right
shunt and associated physiological derangements are related to
lesion size
Ø Pulmonary hypertension and heart failure may develop
Ø Ideal: children to undergo surgical repair before pulmonary
hypertension develops
Ø Pregnancy: well-tolerated for small-to-moderate sized shunts
Ø Bacterial endocarditis is more common with unrepaired defects, CYANOTIC HEART DISEASE
and antimicrobial prophylaxis is often required
Ø 10-16% of offspring has VSDs Ø Cyanosis: R to L shunting of blood past pulmonary capillary bed
Ø Most commonly encountered lesion in adults: Tetralogy of Fallot
o Characterized by a large ventricular septal defect,
pulmonary stenosis, RV hypertrophy, and an overriding
aorta that receives blood from both the right and left
ventricles
Ø Do poorly during pregnancy
Ø Maternal mortality rate: 10%
Ø Chronic hypoxemia, polycythemia, miscarriage and perinatal
morbidity
Ø Not all cyanotic lesions are repairable
PREGNANCY AFTER SURGICAL REPAIR
TRANSPOSITION OF THE GREAT VESSELS
Ø Pregnancy following surgical correction of transposition of the great
ATRIOVENTRICULAR SEPTAL DEFECT vessels has prominent risks
Ø 3% of all congenital cardiac anomalies are AVSD SINGLE FUNCTIONAL VENTRICLE
Ø AV septal defect is characterized by a common, ovoid AV junction.
Ø This defect is associated with aneuploidy, Eisenmenger syndrome,
other malformations Ø Hypoplastic left heart syndrome – 70% survived ADULTHOOD
Ø Compared with simple septal defects, complications are more Ø Cardiac arrhythmias, thromboembolism
frequent during pregnancy.
Ø Identified in 15% of offspring EISENMENGER SYNDROME
Ø Secondary pulmonary hypertension that arises from any cardiac
lesion
Ø Develops when pulmonary vascular resistance exceeds systemic
resistance and leads to concomitant right-to-left shunting
Ø Pregnant women with this syndrome tolerate hypotension poorly,
and death usually is caused by right ventricular failure with
cardiogenic shock
Ø Given such poor outcomes for both the mother and the fetus,
Eisenmenger syndrome is considered to be an ABSOLUTE
CONTRAINDICATION to pregnancy
3S-2 CARDIOVASCULAR DISORDERS ESTUYE • HO • JAVIER • PASAJOL • RAMOS • ROCHA
PAGE 5 of 9
DIAGNOSIS
Ø Hypertrophied heart, non-dilated left ventricle in the absence of
other CV conditions
Ø Asymptomatic: may have with dyspnea, angina, or atypical chest
pain, syncope, arrhythmias
Ø Symptoms worsen with exercise; ventricular tachycardia ® death
MANAGEMENT
Ø Avoid strenuous exercise, abrupt positional changes
Ø Delivery route: OB indications
Ø Choice of anes: controversial
SEE APPENDIX
DILATED CARDIOMYOPATHY
Ø Left or right ventricular enlargement
VII. PULMONARY HYPERTENSION
Ø Reduced systolic function in the absence of coronary, valvular,
congenital or systemic diseases causing myocardial dysfunction
Ø Normal resting mean pulmonary artery pressure is 12 to 16 mmHg.
Ø Both inherited and acquired (viral infection: myocarditis or HIV)
Ø Pulmonary hypertension is defined in nonpregnant individuals as a
Ø Potentially reversible if causes: alcoholism, cocaine abuse, thyroid
resting mean pulmonary pressure > 25 mmHg
disease
Ø Pregnant: Group 2 disorders are the most common – secondary to
pulmonary venous hypertension caused by L-sided atrial,
PERIPARTUM CARDIOMYOPATHY
ventricular or valvular disorders
Ø Non-ischemic dilated CM
(See appendix for comprehensive clinical classification of pulmo HTN)
Ø Unique relationship with pregnancy
Ø Shares genetic predisposition
DIAGNOSIS
Ø Etiology: remains unknown
Ø Oxidative stress during late pregnancy: proteolytic cleavage of
Ø Vague symptoms, dyspnea with exertion is the most frequent prolactin ® 16-kDa prolactin fragment: cardiotoxic and impair
Ø For group 2 disorders: orthopnea, nocturnal dyspnea cardiomyocyte metabolism and contractility
Ø Angina and syncope occur when right ventricular output is fixed and
they suggest advanced disease DIAGNOSIS OF EXCLUSION
Ø Chest radiography: enlarged pulmonary hilar arteries and
attenuated peripheral markings
Ø With the following Diagnostic Criteria:
PROGNOSIS • Development of heart failure in the last month of pregnancy or
within 5 months postpartum
• Absence of an identifiable cause of heart failure
Ø Regardless of etiology, the final common pathway of pulmonary
• Absence of recognizable heart disease before the last month
hypertension is right heart failure and death (<4 years)
of pregnancy
Ø Pregnancy contraindicated: with severe disease
• Left ventricular systolic dysfunction demonstrated by left
ventricular ejection fraction of less than45%, fractional
MANAGEMENT
shortening of less than 30%, or both, with or without a left
ventricle end-diastolic dimension less than 2.7 cm/m2 of body
Ø Activity limitation surface area
Ø Avoidance of supine position later in gestation
Ø Standard treatment: Diuretics; supplemental 02; pulmonary PROGNOSIS
vasodilator drugs
Ø During labor and Delivery:
Ø >1/2 recover baseline recovery within 6 months of delivery
o These women are at greatest risk when venous return
Ø If with persistent cardiac failure: 85% mortality rate (5 years)
and right ventricular filling are diminished
o To avoid hypotension, assiduous attention is given to
SUBSEQUENT PREGNANCY
epidural analgesia induction and to blood loss prevention
and treatment at delivery.
Ø may suffer relapse with worsening of symptoms
Ø 20% of women at risk for deterioration in left ventricular function
VIII. CARDIOMYOPATHIES
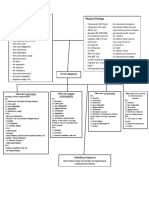
IX. HEART FAILURE
Ø Heterogenous group of myocardial disease with mechanical and/or
electrical dysfunction (American Heart Association) Ø Pre-existing heart ds + PES = 30% risk of heart failure
Ø Primary Cardiomyopathy – solely or predominantly confined to Ø with infection and sepsis - carbon dioxide and oxygen utilization
heart muscle, e.g., hypertrophic CM, dilated CM, peripartum CM and depress myocardial function
Ø Secondary Cardiomyopathy – result from generalized systemic
disorders that produce pathological myocardial involvement, e.g., SYMPTOMS
DM, SLE, CHVD, thyroid disorder
Ø Gradual onset or acute pulmonary edema on 3rd trimester
HYPERTROPHIC CARDIOMYOPATHY Ø Dyspnea
Ø Orthopnea
Ø Cardiac hypertrophy, myocyte disarray, interstitial fibrosis Ø Palpitations
Ø Inheritance is autosomal dominant Ø Substernal chest pain
Ø Left ventricular myocardial hypertrophy with pulmonary gradient vs Ø Decline in the performance of duty
left ventricular outflow Ø Nocturnal cough
3S-2 CARDIOVASCULAR DISORDERS ESTUYE • HO • JAVIER • PASAJOL • RAMOS • ROCHA
PAGE 6 of 9
CLINICAL FINDINGS TREATMENT
Ø Persistent bibasilar rales Ø Primarily medical
Ø Hemoptysis Ø Ascertain infecting organism
Ø Progressive enema
Ø Tachypnea PREGNANCY
Ø Tachycardia
Ø Uncommon even in puerperium
HALLMARK RADIOLOGIC FINDINGS Ø (+) heart valve problems: given Endocarditis prophylaxis
Ø Cardiomegaly
Ø Pulmonary edema PROPHYLAXIS
ECHOCARDIOGRAPHY Ø American Heart Association (AHA)
• According to AHA, patients for whom dental prophylaxis is
Ø EF < 0.45 recommended:
Ø Fractional shortening <30% o Only those at highest risk, i.e., those with:
Ø End diastolic dimension >2.7 cm/m2 § a prosthetic cardiac valve
§ a history of infective endocarditis
MANAGEMENT § certain forms of congenital heart disease
§ unrepaired cyanotic congenital heart disease,
Ø Pulmonary edema – responds to diuretics to reduce preload including palliative shunts and conduits
Ø Hypertension – hydralazine and other vasodilator to reduce § completely repaired congenital heart disease
afterload with prosthetic material or device during the
Ø Left ventricular assist device first 6 months after the procedure
Ø ECMO – extracorporeal membrane oxygenation – life-saving if with § repaired congenital heart disease with residual
fulminating CM and pulmonary HPN defects at the site or adjacent to the site of
prosthetic patch or prosthetic device
X. INFECTIVE ENDOCARDITIS § valvulopathy after cardiac transplantation
Ø Greatest risk: (+) CHD • AHA recommends prophylaxis:
Ø Sub-Acute Endocarditis o does not recommend endocarditis prophylaxis for
o Low virulence bacterial infection + underlying structural either vaginal or CS delivery in the absence of
lesion pelvic infection except with the lesion cited by AHA
Ø Viridans-group streptococcus o given for women at risk for endocarditis (cyanotic
Ø Staphylococcus heart disease, prosthetic valves, or both)
Ø Enterococcus
Ø IV drug abusers/ catheter related infection: Staphylococcus aureus Ø American College of Obstetrics and Gynecologists (ACOG,
Ø Prosthetic valves: Staphylococcus epidermidis 2016)
Ø Fulminating disease: Streptococcus pneumoniae and Neisseria • Administer 30-60 minutes prior to the anticipate delivery
gonorrhea • Standard (IV): Ampicillin 2g or Cefazolin or Ceftriaxone 1g
• Penicillin-allergic (IV): Cefazolin or Ceftriaxone 1g or
DIAGNOSIS Clindamycin 600mg
• Oral: Amoxicillin 2g
Ø Fever with chills – 80-90%
Ø Murmur – 85% XIII. ISCHEMIC HEART DISEASE
Ø Anorexia, fatigue and constitutional symptoms
CLINICAL CLUES Ø Mortality rate is higher compared to non-pregnant woman
Ø If sustained <2 weeks before delivery: high risk for death due
to greater demand of labor and delivery
Ø Anemia
Ø Proteinuria
Ø Diagnosis
Ø Manifestations of embolic lesions: petechiae, focal neurological
o It does not differ in non-pregnant woman which
changes, chest and abdominal pain, ischemia in extremity
include:
Ø Symptoms of heart failure
§ Characteristic ECG changes
§ Evidence of myocardial necrosis –
elevated Troponin levels
§ High index of suspicion: (+) chest pain
o Coronary Angiography – diagnostic standard
Ø Treatment
o Similar to non-pregnant woman
CS reserved for obstetrical indications or epidural anesthesia id
XIV.REFERENCES
Ø Williams Obstetrics, 25th Edition (Cunningham et al)
Ø Dr. Valencia’s PPT
Ø Notes and Recordings of OB2 Trans Team
“Vitanda est improba siren desidia. (One must avoid that
wicked temptress, Laziness.)”― Horace
3S-2 CARDIOVASCULAR DISORDERS ESTUYE • HO • JAVIER • PASAJOL • RAMOS • ROCHA
PAGE 7 of 9
XV.APPENDIX
Table 3. Clinical classification of the New York Heart Association based on the past and present disability uninfluenced by physical signs
HELLO, HAPPY PILL!
Table 4.WHO risk classifIcation of CVD & pregnancy
3S-2 CARDIOVASCULAR DISORDERS ESTUYE • HO • JAVIER • PASAJOL • RAMOS • ROCHA
PAGE 8 of 9
Table 5. Summary of Valvular Heart Diseases
Table 6. Comprehensive Clinical Classification of Pulmonary HTN
3S-2 CARDIOVASCULAR DISORDERS ESTUYE • HO • JAVIER • PASAJOL • RAMOS • ROCHA
PAGE 9 of 9
You might also like
- Derain Carla Elize-Group9 DXRDocument6 pagesDerain Carla Elize-Group9 DXRCarla Elize Derain100% (1)
- Luminare PGI Primer PDFDocument62 pagesLuminare PGI Primer PDFChristine Evan HoNo ratings yet
- Luminare PGI Primer PDFDocument62 pagesLuminare PGI Primer PDFChristine Evan HoNo ratings yet
- Case Presentation: NeurologyDocument19 pagesCase Presentation: NeurologySydrex SarmientoNo ratings yet
- Medical Triads, Tetrads, and PentadsDocument10 pagesMedical Triads, Tetrads, and PentadsAyessa BandalNo ratings yet
- Rouge No DengonDocument2 pagesRouge No DengonNaylimar D Alvarez CNo ratings yet
- Manure HandlingDocument14 pagesManure HandlingIvan Sampson100% (1)
- UST Medicine I Schedule 2016-2017Document6 pagesUST Medicine I Schedule 2016-2017ina17_eaglerNo ratings yet
- Freebie The Great Composerslapbookseries ChopinDocument24 pagesFreebie The Great Composerslapbookseries ChopinAnonymous EzNMLt0K4C100% (1)
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Case Mannequin Body InteractDocument5 pagesCase Mannequin Body InteractAVITA TRISTA NINGRUM100% (1)
- CARDIO - Valvular Heart Diseases Table DR BARTOLOMEDocument8 pagesCARDIO - Valvular Heart Diseases Table DR BARTOLOMEShams JailaniNo ratings yet
- 2016 CPG Ent PDFDocument21 pages2016 CPG Ent PDFCamelle CelisNo ratings yet
- Approach to Hypertension ManagementDocument11 pagesApproach to Hypertension ManagementNoreenNo ratings yet
- Protocol - IM DyspneaDocument7 pagesProtocol - IM DyspneaTrisNo ratings yet
- Diseases of the Pituitary GlandDocument8 pagesDiseases of the Pituitary GlandSheryl Layne Lao-SebrioNo ratings yet
- Cardiology Dr. Payawal UltimateDocument9 pagesCardiology Dr. Payawal UltimateSven OrdanzaNo ratings yet
- MTB Cardiology NotesDocument11 pagesMTB Cardiology Noteskabal321No ratings yet
- Acute Coronary SyndromesDocument82 pagesAcute Coronary Syndromesmidras taranNo ratings yet
- Umnl & LMNLDocument13 pagesUmnl & LMNLTammy BoudNo ratings yet
- Cardiac MurmursDocument3 pagesCardiac MurmursDanielleNo ratings yet
- Table of Content: Post-Streptococcal Glomerulonephritis 3Document5 pagesTable of Content: Post-Streptococcal Glomerulonephritis 3rup100% (1)
- Krok 2014 Base All 2Document237 pagesKrok 2014 Base All 2Gaurav S Batra0% (1)
- Valvular Heart DiseaseDocument71 pagesValvular Heart DiseaseChadi Alraies100% (9)
- Recognize Valvular Heart Diseases and Their Clinical FeaturesDocument8 pagesRecognize Valvular Heart Diseases and Their Clinical FeaturesRobert So JrNo ratings yet
- Internal MedicineDocument83 pagesInternal MedicineSumbul PNo ratings yet
- Lung Cancer with Pleural EffusionsDocument8 pagesLung Cancer with Pleural EffusionsL4 CLERK - UY, Rhea Andrea F.No ratings yet
- Acute Hypertension-Hypertensive Urgency and Hypertensive EmergencyDocument13 pagesAcute Hypertension-Hypertensive Urgency and Hypertensive EmergencyAmitKumarNo ratings yet
- CVS II Tutorials Apr 12-17Document7 pagesCVS II Tutorials Apr 12-17rishitNo ratings yet
- Physical Inactivity: Aging Men Hypertension Smoker ObesityDocument1 pagePhysical Inactivity: Aging Men Hypertension Smoker ObesityKEn PilapilNo ratings yet
- Medicine1 Grand PE ScriptDocument10 pagesMedicine1 Grand PE ScriptCarmeline Santi BeronillaNo ratings yet
- IM - Heart Failure Concept Map - PathophysDocument5 pagesIM - Heart Failure Concept Map - PathophysTrisNo ratings yet
- Pediatric Pharmacology: Dr. Putrya Hawa, M.Biomed Faculty of Medicine, UIIDocument27 pagesPediatric Pharmacology: Dr. Putrya Hawa, M.Biomed Faculty of Medicine, UIIAfied Fitrah100% (1)
- Approach To AnemiaDocument33 pagesApproach To AnemiaVaibhav KrishnaNo ratings yet
- Tumor Markers: Blood Group AntigenDocument5 pagesTumor Markers: Blood Group AntigenAngela ReyesNo ratings yet
- B4 DyspneaDocument100 pagesB4 DyspneaAnonymous HH3c17osNo ratings yet
- Source NotesDocument30 pagesSource NotesChris Jardine Li100% (1)
- أدوية الطوارىءDocument162 pagesأدوية الطوارىءManar22No ratings yet
- Medical Case 1: Language Centre of Malahayati University at 2010Document16 pagesMedical Case 1: Language Centre of Malahayati University at 2010putri1114No ratings yet
- Health HistoryDocument19 pagesHealth HistoryAngelene Caliva100% (1)
- Picu Case StudyDocument3 pagesPicu Case Studyapi-455545776No ratings yet
- MCQ 1. Heart Sound Heart Sound S1 S2Document7 pagesMCQ 1. Heart Sound Heart Sound S1 S2Atirah AaNo ratings yet
- Portal Hypertension - A Case ReportDocument65 pagesPortal Hypertension - A Case ReportTEAM K 1920No ratings yet
- PD 17 To 21Document148 pagesPD 17 To 21Loai Mohammed IssaNo ratings yet
- Blood and Drugs Medicine NotesDocument39 pagesBlood and Drugs Medicine Notesrahuul prasadNo ratings yet
- Management of Severe Hypertension, Hypertension in Special ConditionDocument43 pagesManagement of Severe Hypertension, Hypertension in Special Conditionabhandlung100% (3)
- Endocrine Disorders and Exam QuestionsDocument6 pagesEndocrine Disorders and Exam QuestionsMartina GarciaNo ratings yet
- Cardiovascular History: Chest PainDocument5 pagesCardiovascular History: Chest PainTom MallinsonNo ratings yet
- Medical History Outline-2020Document9 pagesMedical History Outline-2020sumiti_kumarNo ratings yet
- Shivaani (Internal Medicine CWU)Document12 pagesShivaani (Internal Medicine CWU)S.M. Manogaran Shivaani AP S.M. ManogaranNo ratings yet
- Acid-Base Disorder 27 July 2017 PDFDocument48 pagesAcid-Base Disorder 27 July 2017 PDFPauline ChanNo ratings yet
- Medical Israeli Syllabus For Internal Medicine For Exam LicenseDocument4 pagesMedical Israeli Syllabus For Internal Medicine For Exam Licensemohammadeid0% (2)
- CVA Case PresentationDocument16 pagesCVA Case PresentationgolokipokNo ratings yet
- 24 HR History 2Document2 pages24 HR History 2Arjun KatariaNo ratings yet
- CHF, HPN and CAPDocument17 pagesCHF, HPN and CAPJhune VillegasNo ratings yet
- Cardiomyopathy My LectureDocument33 pagesCardiomyopathy My LectureAbraha HailuNo ratings yet
- ASCITESDocument25 pagesASCITESGanesh BabuNo ratings yet
- History Physical FormatDocument3 pagesHistory Physical FormatfilchibuffNo ratings yet
- Common Ecg Abnormalities PDFDocument2 pagesCommon Ecg Abnormalities PDFRonNo ratings yet
- #9 Ie 8 PDFDocument8 pages#9 Ie 8 PDFOmar BasimNo ratings yet
- Problem-based Approach to Gastroenterology and HepatologyFrom EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisNo ratings yet
- A Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Circulatory Shock, Diagnosis, Treatment and Related ConditionsNo ratings yet
- A Case-Based Approach to Interventional Pulmonology: A Focus on Asian PerspectivesFrom EverandA Case-Based Approach to Interventional Pulmonology: A Focus on Asian PerspectivesJamalul Azizi Abdul RahamanNo ratings yet
- Breech Delivery: Types, Diagnosis and ManagementDocument5 pagesBreech Delivery: Types, Diagnosis and ManagementChristine Evan HoNo ratings yet
- Molecular Oncology in Gynecologic CancerDocument7 pagesMolecular Oncology in Gynecologic CancerChristine Evan HoNo ratings yet
- Ectopic PregnancyDocument6 pagesEctopic PregnancyChristine Evan HoNo ratings yet
- Antepartum Surveillance and Intrapartum MonitoringDocument11 pagesAntepartum Surveillance and Intrapartum MonitoringChristine Evan HoNo ratings yet
- Gynecology History and Exam GuideDocument9 pagesGynecology History and Exam GuideChristine Evan HoNo ratings yet
- Essential Intrapartum and Newborn CareDocument23 pagesEssential Intrapartum and Newborn CareEarl ReyesNo ratings yet
- Gestational Trophoblastic DiseaseDocument7 pagesGestational Trophoblastic DiseaseChristine Evan HoNo ratings yet
- Prenatal CareDocument8 pagesPrenatal CareChristine Evan HoNo ratings yet
- MNEMONICSDocument80 pagesMNEMONICSChristine Evan HoNo ratings yet
- NSD ChecklistDocument3 pagesNSD ChecklistChristine Evan HoNo ratings yet
- MED 1 GASTRO - Jaundice and GI Bleeding v2.0Document6 pagesMED 1 GASTRO - Jaundice and GI Bleeding v2.0Christine Evan HoNo ratings yet
- Ple TipsDocument14 pagesPle TipsChristine Evan HoNo ratings yet
- ABORTIONDocument7 pagesABORTIONChristine Evan Ho100% (1)
- Conduct of LaborDocument8 pagesConduct of LaborChristine Evan HoNo ratings yet
- HPV and cervical cancer screeningDocument7 pagesHPV and cervical cancer screeningChristine Evan HoNo ratings yet
- Principles of Chemotherapy and Radiation in Gyne-OncoDocument5 pagesPrinciples of Chemotherapy and Radiation in Gyne-OncoChristine Evan HoNo ratings yet
- (Ob2) 5S-3 EndometriosisDocument7 pages(Ob2) 5S-3 EndometriosisChristine Evan HoNo ratings yet
- Review of Related LiteratureDocument4 pagesReview of Related LiteratureChristine Evan HoNo ratings yet
- Gynecology Family Planning MethodsDocument7 pagesGynecology Family Planning MethodsIan Christopher RochaNo ratings yet
- PD Hx+PE Template 2Document11 pagesPD Hx+PE Template 2Raffy BantangNo ratings yet
- Patient History Amang 2Document7 pagesPatient History Amang 2Christine Evan HoNo ratings yet
- Expansion With Excision: George Clooney Nasal Dorsum Length of Eye Angle of Mandible/jawDocument4 pagesExpansion With Excision: George Clooney Nasal Dorsum Length of Eye Angle of Mandible/jawChristine Evan HoNo ratings yet
- Clinical Case 01-2019 by SlidesgoDocument40 pagesClinical Case 01-2019 by SlidesgoChristine Evan HoNo ratings yet
- CASE STUDY Acute PancreatitisDocument12 pagesCASE STUDY Acute PancreatitisChristine Evan HoNo ratings yet
- 5th Shift ReadingsDocument7 pages5th Shift ReadingsChristine Evan HoNo ratings yet
- Major Case 3Document3 pagesMajor Case 3Christine Evan HoNo ratings yet
- Open Access Atlas of Otolaryngology, Head & Neck Operative SurgeryDocument12 pagesOpen Access Atlas of Otolaryngology, Head & Neck Operative SurgeryChristine Evan HoNo ratings yet
- LEARNING OBJECTIVESpart2Document4 pagesLEARNING OBJECTIVESpart2sere marcNo ratings yet
- Identify statements that match birthday party picturesDocument1 pageIdentify statements that match birthday party picturesprotogina100% (1)
- Muscovite Mica Flakes and Mica Powder For Industrial ApplicationsDocument5 pagesMuscovite Mica Flakes and Mica Powder For Industrial ApplicationsAnuradhaPatraNo ratings yet
- Reigeluth 1983Document14 pagesReigeluth 1983agssuga100% (1)
- English Reviewer Subject-Verb Agreement Exercise 1Document3 pagesEnglish Reviewer Subject-Verb Agreement Exercise 1Honeybel EmbeeNo ratings yet
- CRIMINAL LAW 101Document7 pagesCRIMINAL LAW 101Rimwel GarafilNo ratings yet
- Madbarz Routines Plan: Strength - AdvancedDocument18 pagesMadbarz Routines Plan: Strength - AdvancedJuan Sebastian AnguloNo ratings yet
- Rigging & Slinging For Engineers - Purchasers PDFDocument2 pagesRigging & Slinging For Engineers - Purchasers PDFΈνκινουαν Κόγκ ΑδάμουNo ratings yet
- WBCSC Information Sheet For Interview Advt - 1 - 2015 - UpdatedDocument1 pageWBCSC Information Sheet For Interview Advt - 1 - 2015 - UpdatedArindam GhoshNo ratings yet
- How Plant and Animal Adapt To Aquatic HabitatDocument16 pagesHow Plant and Animal Adapt To Aquatic HabitatCharles Amaechi100% (2)
- Controller Spec SheetDocument4 pagesController Spec SheetLuis JesusNo ratings yet
- Mikro Prism Manual English PDFDocument18 pagesMikro Prism Manual English PDFrakeshr2007No ratings yet
- Fuellas Vs CadanoDocument4 pagesFuellas Vs CadanoMutyaAlmodienteCocjinNo ratings yet
- Zombie Apocolypse: The Five Themes of GeographyDocument6 pagesZombie Apocolypse: The Five Themes of Geographyapi-663760583No ratings yet
- Taketo SUZUKIDocument3 pagesTaketo SUZUKIJane DeckerNo ratings yet
- User Manual: SM-R800 SM-R805F SM-R810 SM-R815FDocument154 pagesUser Manual: SM-R800 SM-R805F SM-R810 SM-R815Fbatto1No ratings yet
- AP Microeconomics 2016 Free-Response QuestionsDocument4 pagesAP Microeconomics 2016 Free-Response QuestionsSHIN SeoYoungNo ratings yet
- Soymilk MenDocument7 pagesSoymilk Mentonious95No ratings yet
- Airframe QuestionsDocument41 pagesAirframe QuestionsJDany Rincon Rojas100% (1)
- Department of Labor: Logsafe Fall 01Document8 pagesDepartment of Labor: Logsafe Fall 01USA_DepartmentOfLaborNo ratings yet
- Stratigrapghy Mineral Potential of BalochistanDocument45 pagesStratigrapghy Mineral Potential of BalochistanMohsin Ali KhuhawarNo ratings yet
- Children Nutrition Action PlanDocument64 pagesChildren Nutrition Action PlanpapayNo ratings yet
- Credits Is Hereby Given To Mrs. Jaylynne Escalona, Mscrim For Her Substantial Contribution As Regards To This NotesDocument15 pagesCredits Is Hereby Given To Mrs. Jaylynne Escalona, Mscrim For Her Substantial Contribution As Regards To This NoteseuniceNo ratings yet
- Occlusal Considerations in Implant Therapy Clinical Guidelines With Biomechanical Rationale PDFDocument10 pagesOcclusal Considerations in Implant Therapy Clinical Guidelines With Biomechanical Rationale PDFSoares MirandaNo ratings yet
- Client Hunting HandbookDocument105 pagesClient Hunting Handbookc__brown_3No ratings yet
- CPE655 Solid Waste ManagementDocument108 pagesCPE655 Solid Waste ManagementAmirah SufianNo ratings yet