Professional Documents
Culture Documents
IPE-COM A Pilot Study On Interprofessional Learning Design For Medical and Midwifery Students
Uploaded by
JASMIEN AISYA SASTIARINI AISYA SASTIARINIOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
IPE-COM A Pilot Study On Interprofessional Learning Design For Medical and Midwifery Students
Uploaded by
JASMIEN AISYA SASTIARINI AISYA SASTIARINICopyright:
Available Formats
Journal of Multidisciplinary Healthcare Dovepress
open access to scientific and medical research
Open Access Full Text Article
ORIGINAL RESEARCH
IPE-COM: a pilot study on interprofessional learning
design for medical and midwifery students
Journal of Multidisciplinary Healthcare downloaded from https://www.dovepress.com/ by 109.94.173.62 on 13-Oct-2019
This article was published in the following Dove Press journal:
Journal of Multidisciplinary Healthcare
ABT Randita 1 Background: The skills of interprofessional teamwork, such as collaboration, team manage-
W Widyandana 2 ment, and interprofessional communication skills, should be embedded in the early stages of
M Claramita 2 health profession education. In Indonesia, medical doctors and midwives have important roles
1
and often work closely to partnership within the primary health care settings. Therefore, both
Medical Education Unit, Faculty of
Medicine, Universitas Sebelas Maret, medical students and midwifery students should have an interprofessional education training
Surakarta, Indonesia; 2Department of together during their professional education, using a community-based learning approach.
Medical, Health Professions Education,
For personal use only.
Purpose: This study aimed to investigate the effect of a community-based interprofessional
and Bioethics, Faculty of Medicine, Public
Health and Nursing, Universitas Gadjah educational learning on collaborative competencies (communication, collaboration, roles and
Mada, Yogyakarta, Indonesia responsibilities, collaborative patient-centered approach, the team functioning, and conflict
management).
Method: Pre-experimental study with one group pre- and post-test design in 15 medical
students and 19 midwifery students were involved in the community-based IPE (IPE-COM)
course, later divided into nine groups. Data were collected by direct observations of super-
visors using Interprofessional Collaborator Assessment Rubric (ICAR) instrument.
Results: The finding showed significant increase in IPE competencies before and after the 4-week
course. IPE community-based learning had the strongest effect on the team’s functioning compe-
tence, while collaborative patient-centered approach competence had a moderate effect.
Conclusion: IPE community-based learning had positive impact with increasing collabora-
tive competencies for both medical and midwifery students.
Keywords: interprofessional education, community-based learning, medical and midwifery
students, interprofessional competencies
Introduction
The quality of health service is often determined by the concern and responsiveness
of care providers to the preferences, needs, and values of patients and consumers,
when applying the concept of patient-centered care. To achieve the holistic patient-
centered care, health professionals need to be equipped with collaborative compe-
tences since the early stage of their health professional education. Collaborative
competencies are widely known as Interprofessional Education (IPE), which has the
main purposes of patient safety and improved quality of health service.3 IPE refers
to a common goal among health care providers that can be learned in a shared
Correspondence: ABT Randita learning process with the core curriculum coordination. In such learning process,
Medical Education Unit, Faculty of joint decision making and professional accountability will also be nurtured.
Medicine, Universitas Sebelas Maret, Jl. Ir
Sutami No. 36 A Kentingan, Surakarta, Moreover, in IPE, each professional discipline maintains shared values, contributes
Central Java 57126, Indonesia to knowledge sharing, and commits in a joint decision making process with all the
Tel +62 8 222 667 4919
Email boy.timor@staff.uns.ac.id disciplines working together.18
submit your manuscript | www.dovepress.com Journal of Multidisciplinary Healthcare 2019:12 767–775 767
DovePress © 2019 Randita et al. This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.
php and incorporate the Creative Commons Attribution – Non Commercial (unported, v3.0) License (http://creativecommons.org/licenses/by-nc/3.0/). By accessing the
http://doi.org/10.2147/JMDH.S202522
work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For
permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms (https://www.dovepress.com/terms.php).
Powered by TCPDF (www.tcpdf.org)
Randita et al Dovepress
IPE can occur when two or more health professions learn both professions must also collaborate in primary health
together, learn from each other, and work together in study- care settings. National health problems, concerning mater-
ing the roles of each health profession to improve the colla- nal and neonatal health issues, are the highest priorities in
boration and quality of health service.27 However, the the two professions.
implementation of IPE still varies and depends on the policy The report of the Millennium Development Goals
of institutions, hospitals, and attitudes of students and the (MDGs) by the World Health Organization (WHO)
community.22 One of the variations can be seen in the diverse
Journal of Multidisciplinary Healthcare downloaded from https://www.dovepress.com/ by 109.94.173.62 on 13-Oct-2019
revealed that there were 36 neonatal deaths per 1000 births
IPE curriculum and teaching forms. IPE may be taught as in the region of South East Asia. In Indonesia, the inci-
short duration courses, or served as student field project dence is among the worst, where 40 neonatal deaths were
tasks, or applied as a “spiral” concept where every year IPE reported in 1000 births. Meanwhile, WHO set the goal in
learning is scaffolded as a long-term terraced approach to 2015’s MDGs as low as 25 neonatal deaths per 1000
continued higher education.2,5 births.28 Accordingly, the neonatal death per 1000 birth
With the wide range of forms of IPE, the implementa- in Indonesia are still high. Data from the Indonesian
tion can fundamentally refer to the theory of “Situated Ministry of Health in 2013 showed the rates of newborn
learning” and “Community practice”.24 The second impor- and maternal mortality as high. The factors that raised a
tant aspect of the theory involving collaborative learning is tremendous concern include inadequate health care facil-
interactive learning experiences with direct observation ities, lack of informed health workers, and referral systems
and professional cooperation.3 Previous research also that did not run well. Collaboration between midwives and
For personal use only.
emphasized the emergent need for early exposure for doctors continued to be a serious challenge for the govern-
collaborative learning, understanding obligations and ment and community agendas that would determine the
demands of each professions’ roles and responsibilities, national health priority issues.16
and developing of intensive interprofessional communica- In Universitas Sebelas Maret, one preliminary study sup-
tion to achieve the common goals.17 ported by national funding resources revealed a set of guide-
In Indonesia, interprofessional collaboration should lines of IPE for community-based learning (IPE-COM) from
occur between doctors and midwives in primary care set- a series of focus group discussions (FGDs) with lecturers,
tings. Collaborations could be formed as partnership general practitioners in primary health care centers, and
between midwives (bidan desa), who work closely with managers from the district health care.19 In this study, the
a community in a village, and doctors, who serve as a qualitative results were combined with an extensive literature
functional health center physician. Recent indicators show review to produce the set of guidelines called, IPE-COM
that the majority of collaborations occur in health-based (Interprofessional Education in Community-based
community work.15 This form of collaboration is men- Learning), which details three phases of learning design
tioned in the rules of the new Indonesian National (Table 1).5,7,23,25 This IPE-COM paradigm was different
Universal Health Coverage System, which stipulates that from the previous literature in the ways students started to
Table 1 IPE-COM learning design adapted for Indonesia
Phase Instruction Activities
First IPE socialization and training Students and supervisors trained about IPE and community
development in health services.
Second Implementation IPE-CBL with 7 steps: Students engaged in community in order to do health projects
1. Identify the stakeholders in the community
2. Approach the community
3. Assess the needs of local communities
4. Planning project in each perspective.
5. Focus project
6. Implementation of the project
7. Reflection
Third Evaluation by IPE students’ report Students reported their learning experiences to supervisors
submit your manuscript | www.dovepress.com Journal of Multidisciplinary Healthcare 2019:12
768
DovePress
Powered by TCPDF (www.tcpdf.org)
Dovepress Randita et al
engage with the community in a local cultural approach.19 IPE skill training, involving assessments of students and
The IPE-COM paradigm has not yet been tested and pub- facilitating in IPE, was delivered to the supervisors.
lished. Therefore, we aimed to conduct a pilot study of IPE-
COM for medical and midwifery students and evaluated it (b) Second phase: Implementation of IPE-COM
with the previously validated Intercollaborator Assessment
Rubric.8 All students, who were engaged in the implementation
Journal of Multidisciplinary Healthcare downloaded from https://www.dovepress.com/ by 109.94.173.62 on 13-Oct-2019
of IPE-COM, were assigned to a community health center
for three weeks. There were seven steps that were per-
Methods
formed by the supervised students to implement IPE:
Research design
The design of this study is a one-group pre-experimental 1. Identify the stakeholders in the community
study with a pre- and post-test. The treatment group ● The first act of IPE team was to identify persons
included medical and midwifery students who engaged in who have a significant role in the community, such
IPE-COM course. Data were collected twice: before and us head of community health center, leader of health
after the intervention. Before intervention (pre-test), all care provider, district leader, religious leader, etc.
participants were assessed for IPE competencies. At the 2. Approach in the community
end of the intervention, all participants were assessed ● To be in contact with the community, the IPE team
again in the same competencies to provide post-test data. need to consider how to approach the community.
For personal use only.
The team should be considerate about the culture
Participants and local wisdom in order to communicate and
Participants were selected purposively with a total sampling invite the community into health care projects.
of 15 medical students and 19 midwifery students. The 3. Assess the needs of local communities
participants in this study followed the public health clinical ● A comprehensive need assessment was conducted
rotation in the obstetric community at two primary health to catch the gap of health condition and percep-
care centers (Puskesmas) in Surakarta, Central Java, from tion within the community. The IPE team would
December 2015 to January 2016. All participants were ran- perform assessment in the holistic aspects of
domly divided into nine groups that consisted of at least one community, which are biological, psychological,
medical student and two midwifery students. Each group was social, cultural, religion, environmental, family
assigned to provide health prevention and promotion for one safety, and community regulation (local rules).
family who had maternal and child health risks. Each group 4. Plan project in each perspective.
● After the IPE team assessed the community’s
defined their own strategies in delivering their task for the
family. We had previously trained the students with colla- needs, the team would arrange a list of problems
borative interprofessional learning during the first phase of derived from the identified gap of health status.
this study (introduction of IPE). The identification of problems should be based on
all perspectives and by both professions (medical
and midwifery). Then, the IPE team made some
IPE community-based learning (IPE-COM) project plans in order to solve the problems.
design Project plans should gather necessary knowledge
There were three phases in this learning design, namely: and skills of all team members.
5. Focus project
(a) First phase: Introduction of IPE-COM ● To prioritize was crucial to focus the project
plans, given the limited time and resources avail-
During the first week of the course, students and super- able. The team should be able to concentrate on
visors were given detailed explanations about IPE and the specific goals for the planned family or commu-
structure of the IPE-COM course in Sebelas Maret nity project.
University. Skill training, such as leadership building, 6. Implementation of the project
interprofessional communication, team management, and ● The IPE team did their project that lasted for two
reflection skills, was conducted for students. Additionally, to three weeks.
submit your manuscript | www.dovepress.com
Journal of Multidisciplinary Healthcare 2019:12 769
DovePress
Powered by TCPDF (www.tcpdf.org)
Randita et al Dovepress
7. Reflection patient-centered approach, and (6) conflict management.
● Reflection means evaluation of all the processes. Interrater reliability was measured to be inter-rater agree-
During this step, the IPE team did not only dis- ment between supervisors.
cuss about the project, but they also reflected on
the interprofessional collaboration and communi-
cation. For example, the students might describe
Data collection
The supervisors were two medical doctors and two mid-
Journal of Multidisciplinary Healthcare downloaded from https://www.dovepress.com/ by 109.94.173.62 on 13-Oct-2019
what they have accomplished, the plans that have
wives who were recruited by the researchers in this study.
not been completed, their limitations, and their
They assessed the IPE competencies by direct observation
thoughts for future recommendation.
in student activities before and after the IPE learning. Each
Additionally, the project for this IPE-COM involved group was observed by one medical doctor and one mid-
comprehensive family medicine. In this pilot project, each wife who were randomly assigned. The first family visit
group was engaged in assessing one family for maternal was done by students and supervisors as a pre-test for the
and child health risks. The students assessed antenatal student. After several family visits and when the student
patients with specific diseases, such as anemia, gestational finished the project intervention, the last family visit was
hypertension, low intake protein, and poor hygiene. Then, repeated by the students and supervisors as the post-test
the students planned promotive and preventive initiatives for the student. Collecting measurements of the student’s
to provide intervention and remedy for those diseases. The IPE competencies was conducted by the supervisors.
For personal use only.
students did not only help the patients but also treated and
educated the family. Analysis of results
We analyzed the results of the IPE assessment rubric using
(c) Third phase: Reporting IPE paired t-test non paramatric (Wilcoxon test) analysis with
the non-parametric Wilcoxon test with a value of 95%
By the end of the course, students created reports by
confidence interval (CI) (P<0.05). The Wilcoxon test was
documenting and reflecting about their activities during
used because the result of ICAR was ordinal (nonpara-
IPE community-based learning.
metric variables). The analysis was continued with tests of
significant correlations with an Effect Size test.9
Instrument
In order to assess student’s IPE competencies, we used the
Interprofessional Collaborator Assessment Rubric or ICAR Research ethics
that was adapted from Curran et al.8 We validated the instru- This study has been approved by the Bioethics Committee,
ment by checking the translation (English–Indonesian), and Faculty of Medicine, Universitas Sebelas Maret (No: 54/I/
back translation (Indonesian–English) with the formal HREC/2016). Before the data collection began, all of the
English translator unit of University of Sebelas Maret, and medical and midwifery students had read and signed an
then tested it with 30 health professional teachers. We used informed consent form. The patients and their family who
the Pearson correlation and alpha cronbach tests for reliabil- were also involved in the health project intervention
ity measurements. There were 2 items dropped because the (focused on promotive and prevention) were also asked
results were less than 0.6 in the domains of collaboration and for informed consent before they got the intervention. The
communication competences. The alpha Cronbach test for IPE team provided informed consent to them as ethical
this validated instrument was 0.87, which means high clearance.
reliability.9 Then, we trained the teachers on how to use the
instrument in the first phase (introduction of IPE) in this
study. In the process, we discussed with the teachers how to Results
observe and interpret each of the items of the ICAR, which Characteristics of participants
had already been translated into Bahasa Indonesia. Thirty-four students of medical and midwifery courses
There were six IPE competence measures in the assess- were divided into nine groups. Each group consisted of
ment: (1) communication, (2) collaboration, (3) roles and medical students and midwives. Participants’ characteris-
responsibilities, (4) team functioning, (5) collaborative tics are presented in Table 2.
submit your manuscript | www.dovepress.com Journal of Multidisciplinary Healthcare 2019:12
770
DovePress
Powered by TCPDF (www.tcpdf.org)
Dovepress Randita et al
Table 2 Characteristics of participants Pre- and post-test results
Characteristics Frequency Based on the interpretation of effect size by Cohen,9 the
Gender
competence of communication, collaboration, roles and
a. Male 6 people (18%) responsibilities, functioning team, and conflict manage-
b. Female 28 people (82%) ment had a strong effect (d>1.00); thus, it is assumed
that the IPE interventions had a strong effect on the five
Profession
Journal of Multidisciplinary Healthcare downloaded from https://www.dovepress.com/ by 109.94.173.62 on 13-Oct-2019
a. Midwife 19 people (56%) competencies, while the competency of a collaborative
b. Doctor 15 people (44%) approach centered on the patient and family had a moder-
ate effect (d=0.51 to 1.00); thus, it is assumed that the
Supervisor
a. Doctor 2 people (50%) effect of the IPE intervention had only a “moderate”
b. Midwife 2 people (50%) impact to improve the competency.
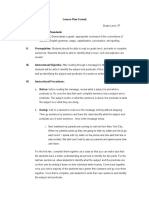
Based on Figure 1, it appears that the mean value of
Supervisor educational background
a. Master 2 people (50%)
the medical students’ competency perception achieve-
b. Bachelor degree/profession 1 person (25%) ment was higher than that of the midwifery students at
c. 3-Year diploma 1 person (25%) the time of measurement. However, both professions
showed an increase in their scores between the pre-test
and post-test.
Interrater reliability test of ICAR
For personal use only.
instruments Discussion
Based on the inter-rater reliability test data in Table 2, it Community-based learning or community-based education is
can be concluded that the four raters had a close inter-rater a comprehensive method to apply and practice the IPE knowl-
agreement (>0.80). There was only one value of 0.738 in edge, skills, and attitudes of health profession students. In
the pre-test involving the competency of roles and respon- addition to clinical learning, the community-based learning is
also an experiential vehicle for the real world of work (real
sibilities. Based on these results, the ICAR instrument
settings). Therefore, it becomes an important learning experi-
could be used by all raters to assess the attainment of
ence that should be obtained by students, including how to
IPE competencies in the pre- and post-test.
better understand the influence of the socio-cultural, econom-
Based on Table 4, the six domains of IPE compe-
ical, and epidemiological challenges of a community, popula-
tence perceptions measured in all participants had a
tion demographics, and government policies regarding the
significant difference between the measurements before
health of individuals, families, and communities.21 Learning
and after the IPE intervention (P<0.05). This result
communities also train students to be more able to effectively
shows there was an increase in the competences in all
collaborate, both in better collaboration with the community
six IPE competencies after the intervention was con-
and also greater competency with other health care
ducted with all participants. professionals.4 Therefore, we recommend the application of
appropriate community learning as well as community-based
interprofessional teaching methods for IPE curriculum.
Table 3 Data on inter-rater reliability test
In general, the purpose of the IPE intervention is to
Competency Result of intraclass
enable the students to gain learning experiences in the
correlation*
community by doing collaborative projects with health
Data pre- Data post- care professionals. This study depicted that the participa-
test test
tion of two different health professions students enabled
Communication 0.848 0.853 more comprehensive approach to solve personal and com-
Collaboration 0.867 0.870 munity health problems. It is argued here that a good
Role and responsibility 0.738** 0.827
collaboration of a health profession team will support the
Collaborative patient-centered approach 0.823 0.887
realization of improving the quality of health services.
Team functioning 0.911 0.815
Conflict management/resolution 0.847 0.898 With this purpose, community-based IPE should not only
aim to handle a public health problem but also to help with
Notes: *Intraclass correlation >0.80=high stability. **Intraclass correlation
0.50–0.80=moderate stability. the implementation of government programs.5,29
submit your manuscript | www.dovepress.com
Journal of Multidisciplinary Healthcare 2019:12 771
DovePress
Powered by TCPDF (www.tcpdf.org)
Randita et al Dovepress
Table 4 Wilcoxon test result
Competency Pre-test Post-test Value P* Effect size
Min Max Median SD Min Max Median SD
1. Communication 2.29 3.16 2.87 0.22 2.79 3.33 3.04 0.20 0.00 1.33**
2. Collaboration 2.43 3.25 2.68 0.29 2.68 3.50 3.06 0.26 0.00 1.37**
3. Role and responsibility 2.03 3.46 2.62 0.28 2.75 3.46 3.05 0.16 0.00 1.88**
Journal of Multidisciplinary Healthcare downloaded from https://www.dovepress.com/ by 109.94.173.62 on 13-Oct-2019
4. Collaborative patient-centered approach 2.06 3.00 2.50 0.25 2.25 3.25 2.87 0.30 0.00 0.86***
5. Team Functioning 1.75 3.20 2.50 0.31 2.90 3.65 3.20 0.20 0.00 2.76**
6. Conflict management/resolution 2.06 3.00 2.59 0.25 2.62 3.68 3.25 0.31 0.00 2.45**
Notes: *Value P<0.05 meaning there is a statistically significant difference. **Effect size d>1.00 meaning the intervention effect is statistically strong. ***Effect size
0.51≤d≤1.00 meaning the intervention effect is statistically moderate.
In addition, the community-learning program that was the students to see health perspectives in an interprofes-
piloted in this study is one example of experimental learn- sional way. Next, they learned how to provide treatment
ing, where the field experiences become constructive for a disease by facing non-medical aspects that can affect
building blocks of students’ knowledge, skills, and atti- the quality of health. In the process, social hierarchy and
tude. Development of new methods of teaching IPE should barriers with other professionals were expected not to pose
be collaboratively developed and should consider to focus any problem for communication and team performance.1
For personal use only.
on work-based learning in the community where students Students were also trained about team management,
will gain learning experiences by engaging with the real project planning, and communication between professions
population setting.11 at the introduction stage. According to Barr et al3 and
The results of the increased value of IPE collaborative Kahaleh et al,14 team building and establishing good com-
competency perceptions in this study showed that the munication must be performed from the beginning of
intervention process during the IPE community-based health care collaboration. Building a collaborative team
learning was effective and had a significant impact on of health professionals needs to focus on individual
increasing students’ IPE competency achievement based aspects of each profession, including behaviors, personal
on the supervisors’ perceptions. There were three major feelings, internalized norms, beliefs, and self-concepts.26
processes designed in the IPE learning intervention in this At the second phase, the students were guided using the
study: the introduction, implementation and reflection, and aforementioned seven-step implementation of the IPE-
evaluation. COM curriculum. The seven steps helped students to intro-
In this study, the learning process and success of IPE duce themselves to the community, interact with the com-
intervention were measured at the level of supervisors’ munity, conduct a community assessment, create health
perceptions. This measurement needs to be taken to deter- project planning, implementation, make a conclusion after
mine the IPE competency achievement in students by reflecting on the activities, and have a final evaluation.
developing an appropriate assessment blueprint so that it According to recent research, Foroushani et al10 suggested
can properly assess changes in attitudes, skills and IPE that the initial approach process and the early involvement
knowledge of students. However, in this study, the level of acts in the community would determine how people in the
perception obtained from the raters who performed direct community receive the health care team. The process of
observation provided clear indication that the students had self-introduction, the provision of health care purposes, and
engaged in IPE learning experience capable of changing treatment methods are important aspects to consider before
collaborative perspectives with other health professions, IPE team can be delivered. These essential components are
from before applying new knowledge, through making also important aspects of the safety of patients.6,12
joint projects and finally after implementation, performing In the phase of project planning, focusing and project
reflection and evaluation. implementation are steps that assist students in good pro-
This study showed that health care teams and compre- ject management. Interprofessional group discussion was
hensive care are important in improving the quality of important in providing perceptions, suggestions, and key
care. In the first phase, this study emphasized and exposed understanding from other professions about how their
submit your manuscript | www.dovepress.com Journal of Multidisciplinary Healthcare 2019:12
772
DovePress
Powered by TCPDF (www.tcpdf.org)
Dovepress Randita et al
Communication Collaboration
Journal of Multidisciplinary Healthcare downloaded from https://www.dovepress.com/ by 109.94.173.62 on 13-Oct-2019
Midwife Medical Midwife Medical
student student student student
Collaborative approach centered
Roles and responsibilities on the patient
For personal use only.
Midwife Medical Midwife Medical
student student student student
Team functioning conflict management
Midwife Medical Midwife Medical
student student student student
Information:
: Pre-test results : median
: Post-test results o : outlier
Figure 1 Difference on collaborative competency perception value in each profession.
roles, opinions, and methods for conflict management can communication, collaboration, roles and responsibilities,
create a core resolution group for any challenges asso- functioning team, and conflict management. Thus, this
ciated with health care services.13 study demonstrated that IPE learning interventions can
There were five among six IPE competencies in the help to increase the levels of core competency of IPE
results of this study which had a mean value above three in students.
the post-test. These results indicated that students reached The impact of interventions, that had a moderate effect,
the stage of “competent”, compared to pre-test results, was related to the competence of ethics, which involves a
which showed the level of the five competencies as collaborative approach that concentrates on the patient or
“developing”.8 The competencies mentioned were family (patient-centeredness). Some studies similarly have
submit your manuscript | www.dovepress.com
Journal of Multidisciplinary Healthcare 2019:12 773
DovePress
Powered by TCPDF (www.tcpdf.org)
Randita et al Dovepress
also mentioned that ethical issues are a challenge to the well, demonstrating core competencies supported by com-
implementation of IPE, such as aspects of patient safety, munication training at the stage of introduction.
considerations about patient comfort with a variety of This study had some limitations during the process in
health workers who treat them, and how patients are the field. First, this study did not have a control group to
treated as human beings.1,20 In this study, the ethical serve as the comparison group. This approach was because
aspects became challenges for students to be competent of the short period of the study, the limited number of
Journal of Multidisciplinary Healthcare downloaded from https://www.dovepress.com/ by 109.94.173.62 on 13-Oct-2019
as a provider of patient-centered health care. Our recom- medical students in public health clinical rotation, as well
mendations for future study involve how IPE curriculum as midwifery students in the obstetric community phase.
should emphasize about collaborative patient-centered Second, IPE competency assessment by observation is
care for both undergraduate and postgraduate health pro- actually an effective way to see the changes and the
fession educations. In this study, the students only had achievement of student competency. However, in this
short-term experiences in working collaboratively in the study, the change could not be observed in the mid-time
health prevention and promotion sectors. Therefore, colla- of the study. This approach was because the researchers
borative patient-centered care might be more challenging had difficulty to adjust the times of the assessment.
and not appear to be as significant, because the students Finally, the time of this study was adjusted with the
had little to no experience in real patient care. students’ community placement at the health centers, to
The highest achievement of competency occurred in the only three weeks; thus, the time was perceived lacking for
competency of a “functioning team”. This achievement was giving extended IPE learning intervention and seeing long-
For personal use only.
made possible due to the collaborative process, involving term changes in students’ competency.
the very high intensity and frequency of inter-professionals
engagement, to meet and discuss the health projects. This Conclusion
result was evident at every stage of the IPE learning The IPE-COM learning design in this study was demon-
between the medical students and midwifery students that strated to have positive impacts to increase the objectives
always met regularly (for 3 weeks) while they intensively of IPE’s core competencies, which were tested by the
conducted the projects together. Similar results were also ICAR instrument: communication, collaboration, roles
revealed in the research by Sevin et al,25 Saxell et al,23 and and responsibilities, team functioning, and conflict man-
Zanoti et al29 that found the intensity of interprofessional agement for the medical and midwifery undergraduate
discussion and communication in a course or learning activ- students. The IPE-COM approach has a strong impact on
ity specifically designed with the concepts of IPE would the achievement of the “functioning team” and a moderate
raise awareness and create a more conducive environment impact on the competency of “patient-centered collabora-
for good teamwork in patient health care. tive approach”. Therefore, we recommend medical educa-
The second highest achievement of IPE competencies of tors to use IPE-COM learning designs for future research
conflict management and resolution becomes important to and skill training in an IPE learning context.
address the challenges and barriers to the implementation of
the curriculum related to the IPE in the differing paradigms
of each profession. Conflicts seen in this study involved Acknowledgment
challenges to honor the perspectives of other professions, The authors would like to acknowledge the IPE team of
difficulties in listening to others’ involvement in the discus- Faculty of Medicine Universitas Sebelas Maret, Dr. Eti
sions, and a lack of resolution strategies in the event of Poncorini Pamungkasari, Dr., MPd; Ari Probandari, Dr.,
disagreements. In this study, each profession had to under- MPH, PhD; Sri Anggarini, SSIT, MKes; Bulan Kakanita
stand and appreciate the role and responsibilities of the Hermasari, Dr; and Zulaika Nur Afifah, Dr., MKes and the
other profession, so it would be easier to collaborate in students of Faculty of Medicine Universitas Sebelas Maret
conflict management. Another aspect that was also suppor- who have participated actively and enthusiastically in
tive was that the students were able to manage conflict, for helping the research process.
example, in their improvement of the communication com-
petency where students were rated “respectful” toward Disclosure
interprofessional communication and how to communicate The authors report no conflicts of interest in this work.
submit your manuscript | www.dovepress.com Journal of Multidisciplinary Healthcare 2019:12
774
DovePress
Powered by TCPDF (www.tcpdf.org)
Dovepress Randita et al
15. Ministry of Health of Indonesia. Kinerja Dua Tahun Kementerian
References Kesehatan Republik Indonesia. Jakarta: Kementerian Kesehatan
Republik Indonesia; 2011.
1. Altin SV, Tebest R, Freimuth SK, Redaelli M, Stock S. Barriers in the 16. Ministry of Health of Indonesia. Riset Dasar Kesehatan 2013. Jakarta:
implementation of interprofessional continuing education programs – Badan Penelitian dan Pengembangan KesehatanKementerian Kesehatan
a qualitative study from Germany. BMC Med Educ. 2014;14:227. RI; 2014.
doi:10.1186/1472-6920-14-227 17. Morrison S. Working together: why bother with collaboration? Work
2. Barr H. An anatomy of continuing interprofessional education. J Contin Bas Learn Prim Care. 2007;5:65–70.
Educ Health Prof. 2009;29(3):147–150. doi:10.1002/chp.20027 18. Olenick M, Allen LR, Smego RA. Interprofessional education: a
Journal of Multidisciplinary Healthcare downloaded from https://www.dovepress.com/ by 109.94.173.62 on 13-Oct-2019
3. Barr H, Koppel I, Reeves S, et al. Effective Interprofessional concept analysis. Adv Med Educ Pract. 2010;1:75–84.
Education: Argument, Assumption and Evidence. Oxford: Blackwell 19. Pamunkasari EP, Probandari AN, Anggarini S, Randita ABT.
Publishing Ltd; 2005. Pengembangan Model Pembelajaran Interprofessional Education
4. Brennan CW, Olds DM, Dolansky M, Estrada CA, Patrician PA. (IPE) Mahsiswa Kedokteran dan Kebidanan. Universitas Sebelas
Learning by doing: observing an interprofessional process as an Maret research Grant Report; 2015.
interprofessional team. J Interprof Care. 2014;28(3):249–251. 20. Rathbone AP, Mansoor SM, Krass I, Hamrosi K, Aslani P.
doi:10.3109/13561820.2013.838750 Qualitative study to conceptualise a model of interprofessional colla-
5. Bridge D, Davidson R, Odegard PS, Maki I, Tomkowiak J. boration between pharmacists and general practitioners to support
Interprofessional collaboration: three best practice models of interpro- patients’ adherence to medication. BMJ Open. 2016;6:e010488.
fessional education. Med Educ Online. 2011;16:6035. doi:10.3402/meo.
doi:10.1136/bmjopen-2015-010488
v16i0.6035
21. Robert KB. Educational principles of community-based education.
6. Buring SM, Bhusan A, Broseker A, et al. Interprofessional education:
Pediatrics. 1996;98(6 Pt 2):1259–1292.
definitions, student competencies, and guidelines for implementation.
22. Rosenfield D, Oandasan I, Reeves S. Perceptions versus reality: a
Am J Pharm Educ. 2009;73(4):59. Article 59.
qualitative study of students’ expectations and experiences of inter-
7. Cullen L, Fraser D, Symonds I. Strategies for interprofessional educa-
professional education. Med Educ. 2011;45:471–477. doi:10.1111/
tion: the Interprofessional Team Objective Structured Clinical
med.2011.45.issue-5
For personal use only.
Examination for midwifery and medical students. Nurse Education
23. Saxell L, Harris S, Elarar L. The collaboration for maternal and
Today. 2003;23(6):427–433.
newborn health: interprofessional maternity care education for med-
8. Curran V, Hollet A, Casimiro L, et al. Development and validation of the
ical, midwifery, and nursing students. J Midwifery Womens Health.
interprofessional collaborator assessment rubric (ICAR). J Interprof
2009;54:314–320. doi:10.1016/j.jmwh.2009.03.017
Care. 2011;25:339–344. doi:10.3109/13561820.2011.589542
24. Sargeant J. Theories to aid understanding and implementation of
9. Cohen L, Manion L, Morrison K. Research Methods in EducationSixth
interprofessional education. J Contin Educ Health Prof. 2009;29
Edition. New York: Routledge; 2007.
10. Foroushani PS, Travagliat J, Debono D, Braithwaite J. Implementing (3):178–184. doi:10.1002/chp.20033
strategies in consumer and community engagement in health care: 25. Sevin AM, Hale KM, Brown NV, McAuley JW. Assessing interpro-
results of a large-scale, scoping meta-review. BMC Health Serv Res. fessional education collaborative competencies in service-learning
2014;14:402. doi:10.1186/1472-6963-14-402 course. Am J Pharm Educ. 2016;80(2):32. Article 32. doi:10.5688/
11. Hall LW, Zierler BK. Interprofessional Education and Practice Guide No. ajpe80232
1: developing faculty to effectively facilitate interprofessional education. J 26. Weiss D, Tilin F, Morgan M. The Interprofessional Health Care
Interprof Care. 2015;29(1):3–7. doi:10.3109/13561820.2014.937483 Team: Leadership and Development. Massachusetts: Jones &
12. Hallin K, Henriksson P, Dalen N, Kiessling A. Effects of interprofes- Bartlett Learning; 2014.
sional education on patient perceived quality of care. Med Teach. 27. WHO. Interprofessional colaborative practice in primary health care.
2011;33(1):e22–e26. doi:10.3109/0142159X.2011.530314 Nursing and midwifery perspective. Six case studies. Hum Resour
13. Interprofessional Education Collaborative Expert Panel. Core Health Obs. 2013;13:4.
Competencies for Interprofessional Collaborative Practice: Report 28. WHO. (2014). The Millenium Development Goals Report 2014. New
of an Expert Panel. Washington (DC): Interprofessional Education York: WHO.
Collaborative; 2011. 29. Zanotti R, Sartor G, Canova C. Effectiveness of interprofessional
14. Kahaleh AA, Danielson J, Franson KL, et al. An interprofessional educationby on-field training for medical students, with a pre-post
education panel on development, implementation, and assessment stra- design. BMC Med Educ. 2015;15:121. doi:10.1186/s12909-015-
tegies. Am J Pharm Educ. 2015;79(6):78. Article 78. doi:10.5688/ 0409-z
ajpe79799
Journal of Multidisciplinary Healthcare Dovepress
Publish your work in this journal
The Journal of Multidisciplinary Healthcare is an international, peer- covers a very wide range of areas and welcomes submissions from
reviewed open-access journal that aims to represent and publish practitioners at all levels, from all over the world. The manuscript
research in healthcare areas delivered by practitioners of different management system is completely online and includes a very quick and
disciplines. This includes studies and reviews conducted by multi- fair peer-review system. Visit http://www.dovepress.com/testimonials.
disciplinary teams as well as research which evaluates the results or php to read real quotes from published authors.
conduct of such teams or healthcare processes in general. The journal
Submit your manuscript here: https://www.dovepress.com/journal-of-inflammation-research-journal
submit your manuscript | www.dovepress.com
Journal of Multidisciplinary Healthcare 2019:12 775
DovePress
Powered by TCPDF (www.tcpdf.org)
You might also like
- Textbook of Pharmacovigilance: Concept and Practice, Second EditionFrom EverandTextbook of Pharmacovigilance: Concept and Practice, Second EditionNo ratings yet
- Lestari 2018Document15 pagesLestari 2018Nadila Hermawan PutriNo ratings yet
- Martinell ArtikelDocument9 pagesMartinell ArtikelRama SaloukhaNo ratings yet
- Mardani Et Al. - 2020 - The Role of The Nurse in The Management of MedicinDocument15 pagesMardani Et Al. - 2020 - The Role of The Nurse in The Management of Medicincolinebriot2003No ratings yet
- State of Interprofessional Education in Nursing: Nurse EducatorDocument5 pagesState of Interprofessional Education in Nursing: Nurse EducatorAndi Fajrin PermanaNo ratings yet
- JMDH 118419 Role of The Multidisciplinary Team in The Care of The Trache - 101117Document8 pagesJMDH 118419 Role of The Multidisciplinary Team in The Care of The Trache - 101117MilenOjedaNo ratings yet
- Interprofessional Education DR DianthaDocument24 pagesInterprofessional Education DR DianthaInges PSNo ratings yet
- TraditionalDocument9 pagesTraditionalErni SalehNo ratings yet
- An Interdisciplinary Community Diagnosis Experience in An Undergraduate Medical Curriculum: Development at Ghent UniversityDocument9 pagesAn Interdisciplinary Community Diagnosis Experience in An Undergraduate Medical Curriculum: Development at Ghent UniversityEgi NabilaNo ratings yet
- Sicometrik ICP IndonesiaDocument10 pagesSicometrik ICP IndonesiaUchi SuhermanNo ratings yet
- Depression in Medical Students: Current InsightsDocument11 pagesDepression in Medical Students: Current InsightswatiNo ratings yet
- IPEM NotesDocument28 pagesIPEM NotesJelcy MangulabnanNo ratings yet
- 1.current Trends in Interprofessional Education of Health Sciences StudentsDocument8 pages1.current Trends in Interprofessional Education of Health Sciences StudentsNguyên NguyễnNo ratings yet
- The Effect of Study Preparation On Test Anxiety AnDocument7 pagesThe Effect of Study Preparation On Test Anxiety AnjuneldelmundoNo ratings yet
- 484-Article Text-2064-1-10-20210507Document8 pages484-Article Text-2064-1-10-20210507QOMARIYATUL ULYAHNo ratings yet
- 02 - Soemantri Et AlDocument8 pages02 - Soemantri Et Alany fitriyaniNo ratings yet
- Confidence-In-Dental-Care-And-Public-Health-Competency-During-Rural PracticeDocument9 pagesConfidence-In-Dental-Care-And-Public-Health-Competency-During-Rural PracticerezautamaNo ratings yet
- Community Pharmacy Job SatisfactionDocument5 pagesCommunity Pharmacy Job SatisfactionAnburaj JNo ratings yet
- Knowledge and Perception About Epidemiology Among Pharmacy StudentsDocument7 pagesKnowledge and Perception About Epidemiology Among Pharmacy StudentsArwinda NugraheniNo ratings yet
- Pharmacy Student Professional Identity Formation: A Scoping ReviewDocument20 pagesPharmacy Student Professional Identity Formation: A Scoping ReviewLitera HusadaNo ratings yet
- Jurnal THTDocument6 pagesJurnal THTkhansaalmiraNo ratings yet
- Effect of Structured Yoga Program On StresDocument10 pagesEffect of Structured Yoga Program On StresrajeshskNo ratings yet
- Role of Pharmacists in Providing Parenteral Nutrition Support: Current Insights and Future DirectionsDocument16 pagesRole of Pharmacists in Providing Parenteral Nutrition Support: Current Insights and Future DirectionsLUIZ BATISTA FILHONo ratings yet
- Interprofessional Education - The Way Forward in Health ProfessionDocument2 pagesInterprofessional Education - The Way Forward in Health ProfessionJLatriece Elizabeth CedeñoNo ratings yet
- GRR - Academic Integrity and Professionalism of MHPE TeachersDocument24 pagesGRR - Academic Integrity and Professionalism of MHPE TeachersBayu Fajar PratamaNo ratings yet
- Interprofessional Education: A Concept Analysis: Advances in Medical Education and Practice DoveDocument10 pagesInterprofessional Education: A Concept Analysis: Advances in Medical Education and Practice DovekevlarazNo ratings yet
- Jurnal IPE - JIC Editorial - Cox Et Al 2016Document4 pagesJurnal IPE - JIC Editorial - Cox Et Al 2016Benk GazeNo ratings yet
- Determining The Expected Competencies For OncologyDocument5 pagesDetermining The Expected Competencies For OncologyNaghib BogereNo ratings yet
- PubSub2202 Pontes PosterDocument57 pagesPubSub2202 Pontes PosterJay Mark PornelaNo ratings yet
- 3 Impact of Pharmacist Led Interventions Adherence HTADocument11 pages3 Impact of Pharmacist Led Interventions Adherence HTARosalinda Marquez VegaNo ratings yet
- 1288 1 1257 1 10 20170525 PDFDocument9 pages1288 1 1257 1 10 20170525 PDFNabila Noor IswariNo ratings yet
- Amep 259557 Perceived Stress Among Iranian Nursing Students in A ClinicaDocument7 pagesAmep 259557 Perceived Stress Among Iranian Nursing Students in A ClinicaMarianne CoracheaNo ratings yet
- Kelompok 4Document11 pagesKelompok 4fransiskus mekuNo ratings yet
- Therapeutic Communication Through Simulation PDFDocument5 pagesTherapeutic Communication Through Simulation PDFNicole GadrinabNo ratings yet
- Titulo 5Document9 pagesTitulo 5StéphanieLyanieNo ratings yet
- The Development of A Scale To Measure Personal Reflection in Medical Practice and EducationDocument6 pagesThe Development of A Scale To Measure Personal Reflection in Medical Practice and EducationBaoz PingNo ratings yet
- NRR 328749 The Magnitude of Perceived Professionalism and Its AssociateDocument10 pagesNRR 328749 The Magnitude of Perceived Professionalism and Its AssociateAklile TsegaNo ratings yet
- Felter Et Al. (2022) PDFDocument14 pagesFelter Et Al. (2022) PDFAyesha HanifNo ratings yet
- Dhps 187829 Pattern of Medication Use in Geriatric Patients at Primary H 020719Document5 pagesDhps 187829 Pattern of Medication Use in Geriatric Patients at Primary H 020719DHIVYANo ratings yet
- Health Literacy Assessment-2363Document10 pagesHealth Literacy Assessment-2363hanady shehataNo ratings yet
- Factors Influencing Medical Students in Choosing Medicine As A CareerDocument4 pagesFactors Influencing Medical Students in Choosing Medicine As A CareerRYAN JOSHUA MANALONo ratings yet
- Interprofessional Collaboration in Primary Health CareDocument12 pagesInterprofessional Collaboration in Primary Health Caremira maryanilaifaNo ratings yet
- AR10Document6 pagesAR10nadiah thahirah arNo ratings yet
- Aurizki Et Al - 2022Document15 pagesAurizki Et Al - 2022Jonas MartinsNo ratings yet
- Journal of Tissue Viability: SciencedirectDocument11 pagesJournal of Tissue Viability: SciencedirectYuridiaNo ratings yet
- The Effect of Patient Safety Education On Undergraduate Nursing Students Patient Safety CompetenciesDocument6 pagesThe Effect of Patient Safety Education On Undergraduate Nursing Students Patient Safety CompetenciesRandom HNo ratings yet
- JMDH 400734 Application Benefits and Limitations of Telepharmacy For PDocument9 pagesJMDH 400734 Application Benefits and Limitations of Telepharmacy For PIrma RahmawatiNo ratings yet
- Measurement of The Quality of Life of Prolanis Hypertension Patients in Sixteen Primary Healthcare Centers in Pandeglang District, Banten Province, Indonesia, Using EQ-5D-5L InstrumentDocument7 pagesMeasurement of The Quality of Life of Prolanis Hypertension Patients in Sixteen Primary Healthcare Centers in Pandeglang District, Banten Province, Indonesia, Using EQ-5D-5L InstrumentShree WhynieNo ratings yet
- Perceived Threat and Benefit Toward Community Compliance of Filariasis' Mass Drug Administration in Pekalongan District, IndonesiaDocument9 pagesPerceived Threat and Benefit Toward Community Compliance of Filariasis' Mass Drug Administration in Pekalongan District, IndonesiaAnnisa FitriyaniNo ratings yet
- Idr 290992 Knowledge Attitude and Practice On Hospital AcquiredDocument8 pagesIdr 290992 Knowledge Attitude and Practice On Hospital AcquiredZeenat ArifNo ratings yet
- JHL 80011 Assment of The Management Factors Which Influence The Develo - 030215Document11 pagesJHL 80011 Assment of The Management Factors Which Influence The Develo - 030215Bayu PrabuNo ratings yet
- Adverse Reactions in Leprosy Patients Who Underwent Dapsone Multidrug Therapy: A Retrospective StudyDocument6 pagesAdverse Reactions in Leprosy Patients Who Underwent Dapsone Multidrug Therapy: A Retrospective StudyTheva CharaanNo ratings yet
- Medical Abortions Among University Students in GhanaDocument8 pagesMedical Abortions Among University Students in GhanaZulfa FinkaNo ratings yet
- Interface 2018 - Interprofissionalidade ENDocument12 pagesInterface 2018 - Interprofissionalidade ENCésar FonoNo ratings yet
- Atractive Training To PSADocument8 pagesAtractive Training To PSANenden Lesmana WatiNo ratings yet
- What A Doctor Does RolesDocument48 pagesWhat A Doctor Does RolesI Al WNo ratings yet
- PPA 333111 Between Curing and Torturing Burden of Adverse Reaction inDocument11 pagesPPA 333111 Between Curing and Torturing Burden of Adverse Reaction indiana.alyNo ratings yet
- Interprofessional Education Esmarliza K. Tacud-Luzon, MDDocument3 pagesInterprofessional Education Esmarliza K. Tacud-Luzon, MDRaphael MiguelNo ratings yet
- What Are Private Sector Physiotherapists' Perceptions Regarding Interprofessional and Intraprofessional Work For Managing Low Back Pain?Document5 pagesWhat Are Private Sector Physiotherapists' Perceptions Regarding Interprofessional and Intraprofessional Work For Managing Low Back Pain?Lorena CostaNo ratings yet
- Early Marriage and Its Relationship With Child DevelopmentDocument401 pagesEarly Marriage and Its Relationship With Child DevelopmentFerry EfendiNo ratings yet
- Healthcare Students Experiences of An InterprofesDocument5 pagesHealthcare Students Experiences of An InterprofesJASMIEN AISYA SASTIARINI AISYA SASTIARININo ratings yet
- Impact of Peer Pressure On Accuracy of Reporting Vital Signs An Interprofessional Comparison Between Nursing and Medical StudentsDocument8 pagesImpact of Peer Pressure On Accuracy of Reporting Vital Signs An Interprofessional Comparison Between Nursing and Medical StudentsJASMIEN AISYA SASTIARINI AISYA SASTIARININo ratings yet
- Impact of Simulation On Student Attitudes AboutDocument8 pagesImpact of Simulation On Student Attitudes AboutJASMIEN AISYA SASTIARINI AISYA SASTIARININo ratings yet
- 15CowperthwaitEtAl HealthcareTheatreInterprof ClinSimNursDocument11 pages15CowperthwaitEtAl HealthcareTheatreInterprof ClinSimNursJASMIEN AISYA SASTIARINI AISYA SASTIARININo ratings yet
- Assignment - Quantities and Chemical ReactionsDocument3 pagesAssignment - Quantities and Chemical Reactionsharisiqbal111No ratings yet
- Subject and Predicate Lesson PlanDocument2 pagesSubject and Predicate Lesson Planapi-437536657100% (1)
- Aparri School of Arts and Trades-Senior High School ProgramDocument12 pagesAparri School of Arts and Trades-Senior High School ProgramMyra Jane Pe BenitoNo ratings yet
- Language Dysfunction - Continnum - 2015Document19 pagesLanguage Dysfunction - Continnum - 2015Carolina Posada OrtizNo ratings yet
- Ex 4Document3 pagesEx 4ethel hyugaNo ratings yet
- Wim Coca L1Document8 pagesWim Coca L1Abdul Shahfi DahalanNo ratings yet
- Stat501.101 SU14Document2 pagesStat501.101 SU14Hafizah HalimNo ratings yet
- Performace Task in Heat, Sound, and Light Grade 6Document1 pagePerformace Task in Heat, Sound, and Light Grade 6Fernando AbuanNo ratings yet
- 5813 Reported Speech Step by Step Step 6 Reported Statements in The Past With KeyDocument5 pages5813 Reported Speech Step by Step Step 6 Reported Statements in The Past With KeyGabriela GarciaNo ratings yet
- English Test Unit 1 3rd GradeDocument3 pagesEnglish Test Unit 1 3rd GradeJasmín GálvezNo ratings yet
- Peds OspeDocument85 pagesPeds OspeMin Maw60% (5)
- Idea Generation Techniques Among Creative Professionals: 2.1. Creativity ModelsDocument11 pagesIdea Generation Techniques Among Creative Professionals: 2.1. Creativity ModelsAse SharewNo ratings yet
- 16 TensesDocument6 pages16 TensesMat PochoNo ratings yet
- Resume To School PMKDocument4 pagesResume To School PMKPravisk Pravi KNo ratings yet
- 4-ProjectCharterTemplatePDF 0Document5 pages4-ProjectCharterTemplatePDF 0maria shintaNo ratings yet
- Unit 2 - Assignment Brief-đã chuyển đổiDocument5 pagesUnit 2 - Assignment Brief-đã chuyển đổiNhật HuyNo ratings yet
- Hiring Recent University Graduates Into Internal Audit Positions: Insights From Practicing Internal AuditorsDocument14 pagesHiring Recent University Graduates Into Internal Audit Positions: Insights From Practicing Internal AuditorsBrigitta Dyah KarismaNo ratings yet
- Masouda New CVDocument4 pagesMasouda New CVmasoudalatifi65No ratings yet
- Person PerceptionDocument2 pagesPerson Perceptionuzii09No ratings yet
- Philosophical Thoughts in EducationDocument22 pagesPhilosophical Thoughts in Educationapi-619738021No ratings yet
- Oxford Rooftops 4th - Reinforcement and Extension-19Document1 pageOxford Rooftops 4th - Reinforcement and Extension-19MontseNo ratings yet
- Mathematical Excursions 4th Edition Aufmann Test Bank 1Document12 pagesMathematical Excursions 4th Edition Aufmann Test Bank 1malissa100% (50)
- Top Management Colleges in Greater NoidaDocument5 pagesTop Management Colleges in Greater Noidaaanaya mehraNo ratings yet
- HR Questions InterviewDocument54 pagesHR Questions InterviewAlice AliceNo ratings yet
- Grammar D - Types of Processes in Experiential Meaning (Part 1)Document13 pagesGrammar D - Types of Processes in Experiential Meaning (Part 1)Dena BenNo ratings yet
- Describe The Effects of The Sun: Detailed Learning PlanDocument8 pagesDescribe The Effects of The Sun: Detailed Learning PlanRL Cua Jao100% (5)
- TA in PsychotherapyDocument37 pagesTA in PsychotherapyJesús RiveraNo ratings yet
- SPH Sabbath and HealthDocument14 pagesSPH Sabbath and HealthFerdy LainsamputtyNo ratings yet
- Module 1 Teaching PE Health in Elem. Updated 1Document10 pagesModule 1 Teaching PE Health in Elem. Updated 1ja ninNo ratings yet