Professional Documents
Culture Documents
Catching On To The Pandemic Jolt On Rural Healthcare System in India
Uploaded by
Gautam GhoshOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Catching On To The Pandemic Jolt On Rural Healthcare System in India
Uploaded by
Gautam GhoshCopyright:
Available Formats
Open Access Global Journal of Infectious Diseases and Immune Therapies
Volume 4 Issue 1 ISSN: 2694-3824
Commentary Article
Catching on to the Pandemic Jolt on Rural Healthcare System in India
Gautam Kr Ghosha* and Arpita Deb
aPh.D. PG in Reproductive and Child Health Management, and is research scientist at ICMR NICED, Kolkata, India
bMPH, Junior Consultant, NHSRC under Ministry of Health &Family Welfare, Government of India
Article Info Abstract
Article History: Three consecutive waves of COVID-19 have evidently expressed an insufficient rural health
Received: 13 April, 2022
Accepted: 18 April, 2022 infrastructure of India, in facing the pandemic onslaught. The rural healthcare system in rural India,
Published: 23 April, 2022 primarily developed on the suggestions of Bhore Committee Report, guided Government of India in
adopting population-based norms for establishing the three-tier public health care facilities in rural India.
*Corresponding author: Gautam Kr One of the ramifications of receiving the population-based standards for setting up public health care
Ghosh Ph.D., sociology with PG diploma facilities in the rural areas is that numerous rural habitations, particularly small ones, have no public health
in Reproductive and Child Health care facility. The Ministry of Health and Family Welfare latest report indicated notable shortage in the
Management, and is research scientist at required number of Sub-Centers, Primary Health Centers, and Community Health Centers, that form the
ICMR NICED, Kolkata, India; Tel: +9l backbone of rural healthcare. Also, shortage in Specialist, Doctors, Nursing staff and Paramedics to man
98310 4847; Email:
these centers can be observed. Taking lessons from the impact from current pandemic conditions on rural
gautamkghosh@hotmail.com DOI:
https://doi.org/10.36266/GJIDIT/121
healthcare, this paper suggests steps at empowering rural health care and building healthy rural
communities for facing future unforeseen health emergencies.
Keywords: Pandemic Waves; Rural Healthcare; Manpower Shortage; Suggestions
Copyright: © 2022 Gautam Kr Ghosh, et al. This is an open-access article distributed under the
terms of the Creative Commons Attribution License, which permits unrestricted use, distribution,
and reproduction in any medium, provided the original author and source are credited.
every 5 thousand population in plain areas and for every 3 thousand
Main Text population in hilly/tribal and difficult areas. Besides there is a
Three consecutive waves of COVID-19 have evidently expressed primary health cent (PHC) is established following the norm of one
an insufficient rural health infrastructure of India, in facing the PHC for every 30 thousand population in plain areas and 20
pandemic onslaught. Fortunately, some private organizations, thousand population in hilly/tribal/difficult areas. Similarly, there is
industrial houses and charities gathered in order to collect the one community health centre (CHC) for every 120 thousand
rural healthcare system. Help in the form of funding, supply of population in plain areas and 80 thousand population in
equipment, rapid test kits, PPE, among others flowed in. While hilly/tribal/difficult areas [1]. There are hierarchical linkages
this gave a huge respite to struggling rural hospitals in their battle between the three types of public health care facilities in the rural
with COVID-19, but nonetheless pointed towards immediate areas so that the entire rural population of the country is covered by
need for health policy and funding rejig to confront unforeseen the network of CHCs, PHCs and SCs. One of the ramifications of
future crisis situations. receiving the population-based standards for setting up public health
The first pandemic wave affected directly the health and welfare care facilities in the rural areas is that numerous rural habitations,
of women and children in the poorer section of society, as media particularly small ones, have no public health care facility.
reports stated. Considerable numbers of pregnant women The National Health Profile 2021 projects that India’s rural health
succumbed during child birth, being unable to access to proper care system is comprised of total 158417 Sub-Centre, 25743 Primary
medical help, and others gave birth to underweight and severely Health Centres, and 5624 Community Health Centres but marked
undernourished children subjected to life-long health issues. The with the shortfall in health facilities as- 18% in SC, 22% in PHC and
ordinary times struggles of Indian healthcare system as came out 30% in CHC levels [2]. Going by the country’s Rural Health
in the public domain, multiplied manifold during the pandemic; Statistics 2020-2021, it can be observed that 14.1% of the sanctioned
and has had a devastating impact on social and economic lives. posts of Health Workers (Female)/ ANM and 37% of the sanctioned
The rural healthcare system in rural India, primarily developed posts of Health Workers (Male) are currently vacant in the Sub-
on the suggestions of Bhore Committee Report, guided Centres. Further, there is a shortage of doctors (1,704 positions) in
Government of India in adopting population based norms for PHCs across the rural areas, as well as nursing staff (5,772), female
establishing the three-tier public health care facilities in rural health workers (5,066), pharmacists (6,240), and laboratory
India. The lowest public health care facility is the Sub-Centre technicians (12,098). The healthcare workforce availability is
(SC) which is established on the basis of the norm of one SC for substantially below the World Health Organization recommended
Pubtexto Publishers | www.pubtexto.com 1 Global J Infect Dis Immune Ther
Citation: Gautam Kr Ghosh and Arpita De (2022). Catching On To the Pandemic Jolt on Rural Healthcare System in India. Global J Infect Dis Immune
Ther 4(1): 119 DOI: https://doi.org/10.36266/GJIDIT/121
levels, as can be observed. As published reports indicate, India diseases arising from infection or lack of nutrition continue to
has 1154686 registered doctors in the speciality of modern account for almost two thirds of morality and morbidity India [7].
medicine. At present single Government Allopathic Doctor cater With rural areas lacking access to basic healthcare facilities, there
to the need of 10926 individuals in the country. remain considerable challenges to setting up robust emergency
Utilizing the available information from National Health Profile- medical services, as well.
2021, it is noticeable that there are 7,13,986 government hospital Both increases in government spending and private sector initiatives
beds available in India. This adds up to 0.55 beds per 1000 have improved the health infrastructure, but given rising
populace. Once again, there are between-the-states variations in demographic pressure in India, this increase does not seem to make
the number of beds accessible per patients. On record 12 states the desired difference [8]. It is the extension of life expectancy that
as, Bihar, Jharkhand, Chhattisgarh, Madhya Pradesh Gujarat, has a direct impact on many households. This is because rising
Uttar Pradesh, Andhra Pradesh, Haryana, Maharashtra, Odisha, healthcare cost exacerbate the problem for lower- and middle-class
Assam and Manipur, where dwell nearly 70% of the country’s households [9]. The suggestive way forward, at this juncture, at
total population, they lie below the national level figure (0.55 empowering rural healthcare systems and building healthy rural
beds per 1000 populace). However, some states have improved communities, can be as follows-
upon the national level, as Sikkim with 2.34 bed per 1000
Maximise the implementation of establishing Health and
population in North-East, in East West Bengal with 2.25
government beds per 1000 population, and the southern states as Wellness Centres
Tamil Nadu with 1.1 bed per 1000 population and Kerala with The HWCs under Ayushman Bharat was a good beginning, for it
1.05 beds per 1000 population. Again, going by the information proposed a more comprehensive, better-equipped, and better-staffed
available from the Rural Health Statistics 2019-20, as against model of primary healthcare services in the government health sub-
155404 Sub-Centers across the country, only 5383 SCs was centres and primary health centres. Most of these are located in rural
functioning as per IPHS norms [3]. The total 24918 Primary India, and upgrading them would surely help in achieving the level
Health Centers (PHC) were functioning, of which just 8514 of preparedness needed to face pandemic situation and other
PHCs function on 24x7 basis. As against the requirement of unforeseen emergencies in rural India.
20732 Community Health Centers (CHC), just 4957 CHCs
currently functioning in rural areas. The rural healthcare set-up Long-term public-private partnerships (PPP) to support
does not provide assuring state of affairs, currently. Besides, healthcare inclusion
there is among the states, dissimilarity as far as access to medical PPP partnerships have the potential to revolutionize Indian rural
care, appropriation of public health expenditure as well as health healthcare system in number of ways, while also providing a long-
outcomes. term sustainable approach. With our country’s growing population,
With the implementation of the National Rural Health Mission government efforts will not be enough to strengthen the healthcare
in 2005 and the launch of Ayushman Bharat Programme in 2021, system. PPP can assist in overcoming financial, technological,
India’s rural health infrastructure is observably improving [3,4]. educational, and human resources constraints. While the government
However, it still remains ill-equipped to tackle the challenges of can develop policies to support rural healthcare infrastructure,
unforeseen emergencies and that posed by the recent pandemic. private players can ensure that these policies are implemented
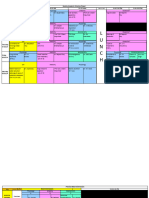
The basic health infrastructure in rural India can be observed appropriately. Long-term partnerships like these improve access to
from the diagram below- healthcare, especially hard-to-reach rural areas, because private
actors’ extensive expertise, experience and financial resources may
aid in the development of novel solutions.
Establish an on-ground supervisory committee
An on-ground supervision committee should be formed to develop a
set of core and additional strategies for improving access to better
healthcare and overseeing the implementation of rural healthcare
projects. While most rural healthcare programs get off to a terrific
start, the results are not always as anticipated. To revive rural health
Source: Ministry of Health and Family Welfare.
systems through efficient monitoring of rural health enhancement
The pressing public health challenges for rural India include
operations, and on-the-ground supervisory committee is required.
preventing, controlling or eliminating major communicable
diseases, as Tuberculosis, Malaria, and in bringing down the risk Continuous competency development and mentoring
of deaths in maternal and peri-natal conditions [5,6]. Endemic
Another key concern in rural regions is skill development and
Pubtexto Publishers | www.pubtexto.com 2 Global J Infect Dis Immune Ther
Citation: Gautam Kr Ghosh and Arpita De (2022). Catching On To the Pandemic Jolt on Rural Healthcare System in India. Global J Infect Dis Immune
Ther 4(1): 119 DOI: https://doi.org/10.36266/GJIDIT/121
mentoring. According to a report published by the Union
Ministry of Health and Family welfare, there is 76.1 % shortage
of specialists in 5,183 Community Health Centers operating in
rural areas. Doctors can benefit from skill development courses
and ongoing learning programs to assist address the dearth of
trained doctors in rural areas. Doctors in rural areas encounter
several problems when it comes to accessing training
opportunities due to their location. This is where a focused
mentoring program, with online or offline sessions, skill
upgradation and exchange programs may be immensely
beneficial.
Coherent machine upgrade and paramedic training
Essential amenities, such as most up-to-date medical equipment
and skilled medical personnel to operate them, are lacking in rural
areas. While medical equipment can still be upgraded on a regular
basis, training courses for nurses and paramedical workers on
how to handle, operate and manage these machines are also
necessary. As new technologies become available, the
requirement for training becomes more pronounced and require
to be recognized.
Conclusion
In summing up, it needs to be point out that it is impossible to
transform the primary health care system of the country in a day
or a week or a month, and that a sporadic approach to uplifting
rural healthcare infrastructure will be an exercise in futility. But,
with the ongoing dedication and regular efforts can a robust
healthcare system be developed in rural areas. Implementing the
procedures outlined above will have positive benefits in the long
run and will aid in the development of a robust health care system.
The primary goal should be to improve preparation beyond
COVID, rather than focusing simply on short-term fixes that will
return the system to its previous state once external help is
withdrawn.
References
1. Rural Health Care System in India.
2. National Health Profile (NHP) of India- 2021.
3. National Rural Health Mission.
4. Ayushman Bharat Programme in 2021.
5. WHO Background Paper: Burden of Disease in India.
6. Prakash A, Swain S, Seth A. Maternal mortality in India:
current status and strategies for reduction. Indian Pediatr.
1991; 28: 1395-400.
7. Health care in India-vision 2020.
8. Relationship between Infrastructure and Population; ADBI
Working Paper Series.
9. Balarajan Y, Selvaraj S, Subramanian SV. Health care and
equity in India. Lancet (London, England). 2011; 377: 505-
515.
Pubtexto Publishers | www.pubtexto.com 3 Global J Infect Dis Immune Ther
You might also like
- Application Letter To NDP 2016Document2 pagesApplication Letter To NDP 2016tinea nigra50% (2)
- Rural Health in Andhra PradeshDocument5 pagesRural Health in Andhra PradeshInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Health Infrastucture in IndiaDocument8 pagesHealth Infrastucture in IndiaBinit kumarNo ratings yet
- Health System in India: Opportunities and ChallengesDocument3 pagesHealth System in India: Opportunities and ChallengesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- "It Is Health That Is Real Wealth and Not Pieces of Gold and Silver" Mahatma GandhiDocument8 pages"It Is Health That Is Real Wealth and Not Pieces of Gold and Silver" Mahatma GandhishivamNo ratings yet
- Health Care in India in The Prevailing COVID-19 Pandemic ScenarioDocument6 pagesHealth Care in India in The Prevailing COVID-19 Pandemic ScenarioHimanshu ShahNo ratings yet
- ResearchPaper SwarajAgarwalDocument5 pagesResearchPaper SwarajAgarwalAshish KumarNo ratings yet
- Health Care Delivery Concerns in IndiaDocument43 pagesHealth Care Delivery Concerns in IndiaSaji Sadanandan50% (4)
- Essay On PHCDocument4 pagesEssay On PHCShivanshu PandeyNo ratings yet
- India: Current State of HealthcareDocument15 pagesIndia: Current State of HealthcareYadav MannuNo ratings yet
- Review-Health Systems in India PDFDocument4 pagesReview-Health Systems in India PDFTehMarianNo ratings yet
- M2022LSP007 Q2Document3 pagesM2022LSP007 Q2krishna vamsyNo ratings yet
- Literature Review of Quality of Healthcare Services in IndiaDocument27 pagesLiterature Review of Quality of Healthcare Services in IndiaMunnangi NagendrareddyNo ratings yet
- Evidence Based Field Work ReportDocument16 pagesEvidence Based Field Work ReportSuraj MauryaNo ratings yet
- Ayushman Bharat Yojana A Memorable Health InitiatiDocument2 pagesAyushman Bharat Yojana A Memorable Health InitiatiPiyush ChaturvediNo ratings yet
- Health Status of IndiaDocument10 pagesHealth Status of IndiaSutapa PawarNo ratings yet
- 23-02-2021-1614065941-6-Impact - Ijrbm-2. Ijrbm - An Economic Study Utilisation of Healthcare Services Among Rural Households in Vellore DistrictDocument6 pages23-02-2021-1614065941-6-Impact - Ijrbm-2. Ijrbm - An Economic Study Utilisation of Healthcare Services Among Rural Households in Vellore DistrictImpact JournalsNo ratings yet
- Anup Kumar MishraDocument11 pagesAnup Kumar MishraMahila Pratishtha JournalNo ratings yet
- Brief On Public Health IsssuesDocument7 pagesBrief On Public Health IsssuesAAKASH BATRANo ratings yet
- Health Care Challenges in IndiaDocument8 pagesHealth Care Challenges in IndiaKailash NagarNo ratings yet
- Rural India Final PaperDocument8 pagesRural India Final Paperapi-664194717No ratings yet
- India's Healthcare SectorDocument24 pagesIndia's Healthcare SectoraNo ratings yet
- India's Healthcare SectorDocument24 pagesIndia's Healthcare SectoraNo ratings yet
- Public Health Sector by AbhishekDocument12 pagesPublic Health Sector by AbhishekfdxgfdgbfbhNo ratings yet
- Human Resources For Public Health in India - Issues and ChallengesDocument13 pagesHuman Resources For Public Health in India - Issues and ChallengesHarikeshYadavNo ratings yet
- Indias Rural Health SystemDocument2 pagesIndias Rural Health SystemhajjdndNo ratings yet
- Rajagopalan India Healthcare Mercatus v2Document38 pagesRajagopalan India Healthcare Mercatus v2Rapper EzyNo ratings yet
- Major Challenges in The Health Sector in BangladeshDocument13 pagesMajor Challenges in The Health Sector in BangladeshRaima Ibnat ChoudhuryNo ratings yet
- Reasons For Development of Health Care in IndiaDocument5 pagesReasons For Development of Health Care in IndiasnehapriyaNo ratings yet
- Rajiv Mishra 3Document32 pagesRajiv Mishra 3Mayank GandhiNo ratings yet
- Ehr Based Data Grid Architecture For Indian Rural HealthcareDocument5 pagesEhr Based Data Grid Architecture For Indian Rural HealthcareInternational Journal of Application or Innovation in Engineering & ManagementNo ratings yet
- Rural Healthcare Financing Management PaperDocument21 pagesRural Healthcare Financing Management Papersri_cbmNo ratings yet
- HealthcareDocument2 pagesHealthcareAvanish SinghNo ratings yet
- Introduction of Health Care Services Under Ayushman Bharat Pradhan Mantri Jan Arogya Yojana AB (PM-JAY) - A Literature ReviewDocument6 pagesIntroduction of Health Care Services Under Ayushman Bharat Pradhan Mantri Jan Arogya Yojana AB (PM-JAY) - A Literature ReviewInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Assignment 307Document4 pagesAssignment 307Saqib KhanNo ratings yet
- State of Indian Healthcare Indian Cities Through The Lens of Healthcare 2 EToaEJdDocument35 pagesState of Indian Healthcare Indian Cities Through The Lens of Healthcare 2 EToaEJdvivek singhNo ratings yet
- Case Study of COVID-19: How The Sudden Disruption Will Set The Way For The Future of India's Health Infrastructure at The Micro and Macro LevelDocument3 pagesCase Study of COVID-19: How The Sudden Disruption Will Set The Way For The Future of India's Health Infrastructure at The Micro and Macro Levelanwesh pradhanNo ratings yet
- Assignment 3 Recent Advances in HealthcareDocument18 pagesAssignment 3 Recent Advances in HealthcaresiazamirNo ratings yet
- Essay-3 HealthcareDocument21 pagesEssay-3 HealthcareShretima AgrawalNo ratings yet
- The Focus of Healthcare Is Increasingly Getting Skewed Towards TheDocument4 pagesThe Focus of Healthcare Is Increasingly Getting Skewed Towards TheNitish KumarNo ratings yet
- Major Challenges in The Health Sector in BangladeshDocument13 pagesMajor Challenges in The Health Sector in Bangladesh12-057 MOHAMMAD MUSHFIQUR RAHMANNo ratings yet
- Health, EducationDocument47 pagesHealth, EducationdiljitgippyNo ratings yet
- Health Care Systems in Transition III. Pakistan, Part I. An Overview of The Health Care System in PakistanDocument5 pagesHealth Care Systems in Transition III. Pakistan, Part I. An Overview of The Health Care System in PakistanAslam KyonNo ratings yet
- CC-5 ACCESS TO RURAL HEALTHCARE-minDocument12 pagesCC-5 ACCESS TO RURAL HEALTHCARE-minsmsunil12345No ratings yet
- Why Health Awareness Is Required: Healthy Mind in Healthy BodyDocument18 pagesWhy Health Awareness Is Required: Healthy Mind in Healthy BodyAileenaMerajNo ratings yet
- Introduction To Healthcare System of IndiaDocument22 pagesIntroduction To Healthcare System of Indiakratika GaurNo ratings yet
- Financing Healthcare For All in India Towards A Common GoalDocument40 pagesFinancing Healthcare For All in India Towards A Common GoalJames MitchellNo ratings yet
- Healthcare Delivery System of PakistanDocument4 pagesHealthcare Delivery System of PakistanRaheen AurangzebNo ratings yet
- Covid-19: The Indian Healthcare Perspective: Meghna Mishra, Dr. Mamta Bansal & Mandeep NarangDocument8 pagesCovid-19: The Indian Healthcare Perspective: Meghna Mishra, Dr. Mamta Bansal & Mandeep NarangTJPRC PublicationsNo ratings yet
- Group2 D IE HealthcareDocument33 pagesGroup2 D IE HealthcareSpandana AchantaNo ratings yet
- The National Health Policy and MalnutritionDocument11 pagesThe National Health Policy and Malnutritiondishydashy88No ratings yet
- Creating Quality and Affordable Healthcare For Every Indian: Challenges That The Healthcare Sector Is FacingDocument4 pagesCreating Quality and Affordable Healthcare For Every Indian: Challenges That The Healthcare Sector Is Facingaditya vermaNo ratings yet
- Public Health Care System in IndiaDocument5 pagesPublic Health Care System in IndiaPela KqbcgrlaNo ratings yet
- Eng102 Term Paper Argumentative EssayDocument14 pagesEng102 Term Paper Argumentative EssayMustafa Abid RahmanNo ratings yet
- Health Sector of BangladeshDocument5 pagesHealth Sector of BangladeshAlo StudentNo ratings yet
- Need of Public Health For Sustainable DevelopmentDocument2 pagesNeed of Public Health For Sustainable DevelopmentAdvanced Research PublicationsNo ratings yet
- HealthcareDocument10 pagesHealthcareTanish DhandNo ratings yet
- "Sehat Sahulat Program" - A Leap Into The Universal Health CoveraDocument9 pages"Sehat Sahulat Program" - A Leap Into The Universal Health Coverasameershah9sNo ratings yet
- An Empirical Study On Various Healthcare Strategies Followed by Selected Hospitals in PuducherryDocument8 pagesAn Empirical Study On Various Healthcare Strategies Followed by Selected Hospitals in PuducherryManagement Journal for Advanced ResearchNo ratings yet
- Viewpoint: Healthcare Agenda For The Indian GovernmentDocument3 pagesViewpoint: Healthcare Agenda For The Indian GovernmentKahmishKhanNo ratings yet
- Khyber Pakhtunkhwa Health Sector Review: Hospital CareFrom EverandKhyber Pakhtunkhwa Health Sector Review: Hospital CareNo ratings yet
- Manifestation of Gender Inequality Its Influence On Health Service Use Among Female Injecting Drug Users - A Study in Champai, Mizoram, IndiaDocument7 pagesManifestation of Gender Inequality Its Influence On Health Service Use Among Female Injecting Drug Users - A Study in Champai, Mizoram, IndiaGautam GhoshNo ratings yet
- Drug Abuse Prognostic Role of Sibbling Position in Bengali Culture - A Study in Kolkata, IndiaDocument5 pagesDrug Abuse Prognostic Role of Sibbling Position in Bengali Culture - A Study in Kolkata, IndiaGautam GhoshNo ratings yet
- Significance of Culture in Shaping The Societal Response of Pandemic AssaultDocument4 pagesSignificance of Culture in Shaping The Societal Response of Pandemic AssaultGautam GhoshNo ratings yet
- Appearances of Stigma and Discrimination Among Immunocompromised Female IDUs - A Study in Champ, Mizoram, IndiaDocument13 pagesAppearances of Stigma and Discrimination Among Immunocompromised Female IDUs - A Study in Champ, Mizoram, IndiaGautam GhoshNo ratings yet
- Motivation For Adherence To Antiretroviral Therapy by Transgender People Living With HIV - A Study in West Bengal, IndiaDocument4 pagesMotivation For Adherence To Antiretroviral Therapy by Transgender People Living With HIV - A Study in West Bengal, IndiaGautam GhoshNo ratings yet
- Covid 19 Health Risk of People With TBDocument4 pagesCovid 19 Health Risk of People With TBGautam GhoshNo ratings yet
- Ethical Issues Concerning Mass Vaccination in IndiaDocument2 pagesEthical Issues Concerning Mass Vaccination in IndiaGautam GhoshNo ratings yet
- 19 in India: Health Implications and Treatment Needs of People Who Use Drugs.Document8 pages19 in India: Health Implications and Treatment Needs of People Who Use Drugs.Gautam GhoshNo ratings yet
- Dimension of Teenagers' Experience of Loneliness During COVID 19 Induced Social Lockdown: A Study in IndiaDocument11 pagesDimension of Teenagers' Experience of Loneliness During COVID 19 Induced Social Lockdown: A Study in IndiaGautam GhoshNo ratings yet
- Distend Concept of HealthDocument5 pagesDistend Concept of HealthGautam GhoshNo ratings yet
- List of Day Care SurgeriesDocument2 pagesList of Day Care SurgeriesVivek SahgalNo ratings yet
- (BowTiedOx) Morning WorkoutDocument2 pages(BowTiedOx) Morning WorkoutJoão PereiraNo ratings yet
- Planned Parenthood Mar Monte and StemExpress InvoiceDocument4 pagesPlanned Parenthood Mar Monte and StemExpress InvoiceMary Margaret Olohan100% (1)
- Raising Canes Allergen and Nutrition InfoDocument1 pageRaising Canes Allergen and Nutrition InfofrankeleeNo ratings yet
- Introduction To Regulatory AffairsDocument15 pagesIntroduction To Regulatory AffairsCyclone Pharmaceuticals Pvt Ltd PuneNo ratings yet
- EIS HPD FinalDocument11 pagesEIS HPD FinalJhilmil GroverNo ratings yet
- 1955-Article Text-4468-1-10-20210827Document4 pages1955-Article Text-4468-1-10-20210827DEVIKA RIZKY MAHARANINo ratings yet
- Cover Letter DDocument1 pageCover Letter DDebela NanessoNo ratings yet
- Anterior Cruciate LigamentDocument26 pagesAnterior Cruciate LigamentAmandeep Singh100% (2)
- ACR In-Service 2007 Exam, Answers, RationalDocument98 pagesACR In-Service 2007 Exam, Answers, RationalDave FullerNo ratings yet
- Manual, Owner'S 1/1: Suffix Language Page RemarkDocument49 pagesManual, Owner'S 1/1: Suffix Language Page RemarkesuardoNo ratings yet
- Final ReportDocument27 pagesFinal ReportHanan KemalNo ratings yet
- Diakogeorgiou123's List of Garden Therapy Articles, Books, Manuals and Professional AssociationsDocument35 pagesDiakogeorgiou123's List of Garden Therapy Articles, Books, Manuals and Professional AssociationsDiakogeorgiou123No ratings yet
- (Zybio) Product Catalogue B 20210803Document30 pages(Zybio) Product Catalogue B 20210803Tinmb FernandoNo ratings yet
- Nursing TheoriesDocument1 pageNursing TheoriesAj GoNo ratings yet
- Math Experiential LearningDocument37 pagesMath Experiential LearningAnjeanette Baltazar CayoteNo ratings yet
- Sample Intervention Planning MatrixDocument2 pagesSample Intervention Planning MatrixOyeesugarNo ratings yet
- Subject:: Applying For The Post of StorekeeperDocument5 pagesSubject:: Applying For The Post of StorekeeperAbdullah HamzaNo ratings yet
- SI - Ferrogard - (VCI C-Type & VCI Stripe)Document5 pagesSI - Ferrogard - (VCI C-Type & VCI Stripe)hamidiNo ratings yet
- Eating Disorders Diagnostic ScaleDocument2 pagesEating Disorders Diagnostic ScaleAbegail (Abby) MirandaNo ratings yet
- GENG 3130 Sec 01 02 Syllabus Full 2022Document14 pagesGENG 3130 Sec 01 02 Syllabus Full 2022pass wordNo ratings yet
- Girela-Lopez, Et Al (2022) Epidemiology and Autopsy Findings of 500 Drowning DeathsDocument6 pagesGirela-Lopez, Et Al (2022) Epidemiology and Autopsy Findings of 500 Drowning DeathsFilbert TandeanNo ratings yet
- Aex 102 - Artificial Intelligence in AgricultureDocument14 pagesAex 102 - Artificial Intelligence in AgricultureBhuvanesh NagamaniNo ratings yet
- LS 2 Herbal Medicine Lesson 1-3Document7 pagesLS 2 Herbal Medicine Lesson 1-3Ken KanikeNo ratings yet
- 4th - 9th March Academic ScheduleDocument3 pages4th - 9th March Academic Schedulehexit73528No ratings yet
- TH Participant-Guide WebDocument5 pagesTH Participant-Guide WebYarden ShneyourNo ratings yet
- Daftar Pegawai PKM Ibun Februari 2023Document3 pagesDaftar Pegawai PKM Ibun Februari 2023syauqiNo ratings yet
- Tau AngleDocument5 pagesTau AngleMSHNo ratings yet
- Manual Inspire 3 en USDocument72 pagesManual Inspire 3 en USTheNo ratings yet