Professional Documents
Culture Documents
Standar Asuhan Keperawatan Diabetes Mellitus
Uploaded by
Sherly Densie0 ratings0% found this document useful (0 votes)
19 views39 pagesOriginal Title
StandarAsuhanKeperawatanDiabetesMellitus
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
19 views39 pagesStandar Asuhan Keperawatan Diabetes Mellitus
Uploaded by
Sherly DensieCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 39
See discussions, stats, and author profiles for this publication at: https://www.researchgate.
net/publication/338209795
Standar Asuhan Keperawatan Diabetes Mellitus
Presentation · May 2019
DOI: 10.13140/RG.2.2.18928.00008
CITATIONS READS
0 897
1 author:
Lukman Lukman
Politeknik Kesehatan Palembang
18 PUBLICATIONS 2 CITATIONS
SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Standar Asuhan Keperawatan Diabetes Mellitus View project
All content following this page was uploaded by Lukman Lukman on 28 December 2019.
The user has requested enhancement of the downloaded file.
ASUHAN KEPERAWATAN
DIABETES MELLITUS
Ns. Lukman, S.Kep., MM., M.Kep
Disampaikan pada Seminar “Kupas Tuntas Askep dan Penatalaksanaan DM Tipe II
pada Individu Dewasa pada Bulan Ramadhan” Palembang, 26 Mei 2019
Statistics
• Morbidity: More than 20.8 million Americans diagnosed
with either type 1 or type 2 diabetes; affects 20% of people
over the age of 65 years; approximately 1.5 million new
cases of diabetes diagnosed in 2005 (National Diabetes
Information Clearinghouse [NDIC], 2007).
• Mortality: In 2002, diabetes was reported to be the sixth
leading cause of death (NDIC, 2007).
• Cost: In 2007, the total cost (direct and indirect) of diabetes
in the United States was estimated to be $174 billion (ADA,
2007).
PATOFISIOLOGI
• Diabetes mellitus (DM) is a chronic metabolic
disorder in which the body cannot metabolize
carbohydrates, fats, and proteins because of a lack of,
or ineffective use of, the hormone insulin.
• Diabetic ketoacidosis (DKA) is a life-threatening
emergency caused by a relative or absolute
deficiency of insulin.
Classification
a. Three primary types that are different disease
entities but share the symptoms and complications
of hyperglycemia
b. Type 1, type 2, and impaired glucose tolerance or
pre-diabetes—formerly known as “borderline
diabetes”
Etiology
• Conditions or situations known to exacerbate glucose
and insulin imbalance
– Previously undiagnosed or newly diagnosed type 1
diabetes
– Food intake in excess of available insulin
iii.Adolescence and puberty
– Exercise in uncontrolled diabetes
– Stress associated with illness, infection, trauma, or
emotional distress
Type 1 diabetes (ADA, 2004)
• An autoimmune disease possibly triggered by genetic and environmental factors,
such as with virus, toxin, stress
– 1. Destroys beta-cells in the pancreas
– 2. When 80% to 90% of the beta cells are destroyed, overt symptoms occur.
• Totally insulin-deficient; clients require exogenous insulin to survive (Peeples &
Seley, 2007).
• Characteristics
– 1. Usually occurs before 30 years of age, but can occur at any age
– 2. Peak incidence occurs during puberty
– 3.Abrupt onset of signs and symptoms of hyperglycemia
– 4. Prone to ketoacidosis
Type 2 diabetes (ADA, 2004)
• Involves a decreased ability to use the insulin produced in the
pancreas (Peeples & Seley, 2007)
– 1. Decreased insulin secretion in response to glucose levels
– 2. Insulin resistance blocking cells from absorbing glucose
– 3. Excess production of glucose because of defective
insulin secretory response
• Accounts for 90% to 95% of all diabetes in the United States
Type 2 diabetes (ADA, 2004)
• Characteristics
– 1. Usually occurs after 30 years of age, but is now occurring in
children and adolescents.
– 2. Increased prevalence in some ethnic groups—African
Americans, Hispanic/Latino, Native Americans, Asian Americans,
and Pacific Islanders
– 3. Strong genetic predisposition
– 4. Frequently obese
– 5. Not prone to ketoacidosis until late in course or with
prolonged hyperglycemia
Type 2 diabetes (ADA, 2004)
• Associated with many complications, including heart
disease and stroke, high blood pressure, blindness,
kidney and nervous system disease, amputations,
and complications of pregnancy
Client Assessment Database
ACTIVITY/REST
• Sleep and rest disturbances • Tachycardia & tachypnea at
• Weakness, fatigue, difficulty rest or with activity
walking and moving • Lethargy, disorientation,
• Muscle cramps, decreased coma
muscle strength • Decreased muscle strenght
and tone
CIRCULATION
• History of hypertension; • Decrased & absent
acute myocardial pulses
infarction (MI),
claudication, numbness, • Dysrhythmias
tingling of extremities • Crackles; jugular vein
(long-term effects) distention (JVD) if
• Leg ulcers, slow healing heart failure present
• Tachycardia • Hot, dry, flushed skin;
• Postural BP chnages: sunken eyeballs if
• ypertension dehydration is severe
EGO INTEGRITY
• Life stressors, including financial concerns
related to condition
• Anxiety, irritability
ELIMINATION
• Change in usual voiding pattern • Pale, yellow, dilute urine
• Excessive urination (polyuria)
• Nocturia • Polyuria may progress to
• Pain and burning, difficulty oliguria and anuria if severe
voiding (infection neurogenic hypovolemia
bladder)
• Recent and recurrent urinary • Cloudy, odorous urine
tract infections (UTIs) (infection)
• Abdominal tenderness, bloating,
diarrhea • Abdomen firm, distended
FOOD/FLUID
• Loss of appetite, nausea and • Use of medications
vomiting exacerbating dehydration,
such as diuretics
• Not following prescribed
• Dry and cracked skin, poor
diet, increased intake of skin tugor
glucose and carbohydrates
• Abdominal rigidity and
• Weight loss over a period of distention
days or weeks • Halitosis and sweet, fruity
• Thirst breath odor
NEUROSENSORY
• Fainting spells, dizziness • • Confusion, disorientation
Headaches • Drowsiness, lethargy, stupor
• Tingling, numbness, & coma (later stages)
weakness in muscles • Deep tendon reflexes (DTR)
• Visual disturbances may be decreased
• Seizure activity (late stages
of DKA or hypoglycemia)
PAIN/DISCOMFORT
• Abdominal bloating and pain
• Facial grimacing with abdominal
palpitation, gurading
RESPIRATION
• Air hunger (late stages • Tachycardia
of DKA) • Kussmaul’s respiration
• Cough, with and (metabolic acidosis
without purulent • Rhonchi, wheezes
sputum (infection) • Yellow or green sputum
(infection)
SAFETY
• Dry, itching skin, skin • Decreased general strenght
ulcerations and range of motion (ROM)
• Paresthesia (diabetic • Weakness and paralysis of
neuropathy) muscles, including
• Fever, diaphoresis respiratory musculate if
potassium levels are
• Skin breakdown, lession and
markedly decreased
ulceration
SEXUALITY
• Vaginal discharge (prone to
infection)
• Problems with impotence (men),
orgasmic difficulty (women)
TEACHING/LEARNING
• Familial risk factors, such as diabetes
mellitus, heart disease, stroke, hypertension
• Slow and delayed healing
• Use of drugs, such as steroids, thiazide
diuretics, phenytoin (Dilantin), and
phenobarbital (can increase glucose levels)
• May or may not be taking diabetic
medications as ordered
Nursing Priorities
1. Restore fluid and electrolyte and acid-
acid-base
balance..
balance
2. Correct or reverse metabolic abnormalities.
3. Identify and assist with management of
underlying cause or disease process.
4. Prevent complications.
5. Provide information about disease process,
prognosis,, self-
prognosis self-care, and treatment needs.
DISCHARGE GOALS
1. Homeostasis achieved.
2. 2. Causative and precipitating factors
corrected or controlled.
3. Complications prevented or minimized.
4. Disease process, prognosis, self-care needs,
and therapeutic regimen understood.
5. Plan in place to meet needs after discharge.
NURSING DIAGNOSIS
• Deficient Fluid Volume • Fatigue
• Unstable blood Glucose • Powerlessness
Level • Deficient Knowledge
• Risk for Infection, [sepsis] [Learning Need] regarding
• risk for disturbed Sensory disease, prognosis,
Perception treatment, self-care, and
discharge needs
NURSING DIAGNOSIS
• Hipovolemia (D.0023) • Keletihan (D.0057)
• Ketidakstabilan kadar gula • Ketidakberdayaan (D.0092)
darah (D.0027) • Defisit Pengetahuan
• Risiko Infeksi (D.0142) (D.0111)
• Gangguan persepsi sensori
(D.0085)
Hipovolemia
Intervensi Utama
Manajemen Hipovolemia
Mengidentifikasi dan mengelola penurunan volume cairan
intravaskuler
Manajemen Syok Hipovolemik
Mengidentifikasi dan mengelola ketidakmampuan tubuh
menyediakan oksigen dan nutrien untuk mencukupi kebutuhan
jaringan akibat kehilangan cairan /darah berlebihan
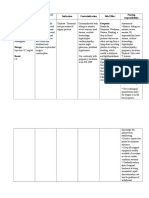
Manajemen Hipovolemia
Observasi (Kaji) Terapeutik Edukasi Kolaborasi
(Mandiri)
Periksa tanda & gejala •Hitung Anjurkan Pemberian cairan
hipovolemia (nadi kebutuhan cairan memperbanyak IV isotonis (msi,
meningkat dan lemah, •Berikan posisi asupan cairan NaCl, RL
TD turun, turgor modified oral …hipotonis (mis
menurun, membran trendelenburg Anjurkan glukosa 2,5 %, NaCl
mukosa kering, vol urin •Berikan asupan menghindari 0,4%)
menurun, HT cairan oral perubahan …koloid
meningkat, haus, lemah posisi (mis.albumin,
- Monitor Intake mendadak Plasmanate)
Output Pemberian
produk darah
Manajemen Syok Hipovolemik
Observasi (Kaji) Terapeutik (Mandiri) Kolaborasi
Monitor status •Pertahankan jalan napas paten Pemberian
kardiopulmonal (nadi, •Berikan O2 u/ mempertahankan Efineprin
napas, TD, MAP) saturasi O2 >94 Dipenhidramin, jika perlu
Monitor status •Persiapan intubasi , jika perlu Bronkodilator, jika perlu
oksigen (oksimetri •Berikan posisi syok (modified Krikotiroidektomi, jika
nadi, AGD) Trendelenburg) perlu
Monitor status cairan •Pasang jalur IV Intubasi endotrakeal, jika
(I, O, turgor kulit, CRT) •Pasang kateter urin untuk perlu
Monitor tk kesadaran menilai produksi urin Resusitasi cairan, jika
dan respon pupil) •Pasang NGT u/ dekomresi perlu
lambung, jika perlu
Ketidakstabilan kadar gula darah
Intervensi Utama
Manajemen Hiperglikemia
Mengidentifikasi dan mengelola kadar gula darah di atas
normal
Manajemen Hipoglikemia
Mengidentifikasi dan mengelola kadar gula darah endah
Manajemen Hiperglikemia
Observasi (Kaji) Terapeutik Edukasi Kolaborasi
(Mandiri)
Identifikasi kemungkinan •Berikan asupan Hindari olahraga bila KGD Pemberian:
penyebab hiperglikemia cairan oral >250 mg/dL Insulin
Identifikasi situasi yg •Konsultasi dg Anjurkan monitor KGD Cairan IV
membutuhkan insulin meningkat medis jika mandiri Kalium
(penyakit kambuhan) memburuk Anjurkan kepatuhan
Minotor KGD •Fasilitasi terhadap diet dan olahraga
Monitor tanda dan gejala ambulasi jika ada Ajarkan pentingnya
hiperglikemia (3poli, kelemahan, hipetensi pemeriksaan keton urin
padangan kabur, sakit kepala) ortostatik Ajarkan pengelolaan DM
Monitor I & O (obat, insulin,
Monitor keton urin, kadar AGD,
elektrolit, TD, frekuensi nadi
Manajemen Hipoglikemia
Observasi (Kaji) Terapeutik (Mandiri) Edukasi Kolaborasi
Identifikasi tanda & •Berikan karbohidrat Anjurkan membawa Pemberian:
gejala hipoglikemia sederhana bila perlu karbohidrat sederhana Dektrose, jika
Identifikasi •Berikan karbohidrat Anjurkan memakai perlu
kemungkinan penyebab kompleks dan protein identitas darurat yg tepat Glukagon jika
sesuai diet Anjurkan monitor KGD perlu
•Pertahankan kepatenan Anjurkan berdiskusi dg tim
jalan napas perawatan ttg penyesuaian
•Pertahankan akses IV, jika program pengobatan
perlu Jelaskan interaksi diet,
•Hub. Layanan medis bila obat/insulin, olahraga
perlu Ajarkan pengelolaan hipog
(tanda & gejala, risiko dan
pengobatan)
Ajarkan perawatan mandiri
untuk mencegah
hipoglikemia
Risiko Infeksi
Intervensi Utama
Manajemen Imunisasi/Vaksinasi
Mengidentifikasi dan mengelola pemberian
kekebalan tubuh secara aktif dan pasif
Pencegahan Infeksi
Mengidentifikasi dan menurunkan risiko
terserang organisme patogenik
Manajemen Imunisasi
Imunisasi//Vaksinasi
Observasi (Kaji) Terapeutik (Mandiri) Edukasi
Identifikasi riw. Kes dan •Dokumentasikan informasi Jelaskan tujuan, manfaat, reaksi
alergi vaksinasi (produsen, tgl terjadi, jadwal dan efek samping
Identifikasi KI pemberian kedaluarsa) Informasikan imunisasi yg
insulin (mis. Reaksi •Jadwalkan imunisasi pd waktu diwajibkan pemerintah (mis.
anafilaksis) yg tepat Hepatitis B, BCG, difteri, tetanus,
Identifikasi status imunisasi pertusis, H. Influenza, polio,
campak, meales, rubela)
Informasikan vaksinasi untuk
kejadian khusus (mis. Rabies,
tetanus)
Informasikan layanan Pekan
Imunisasi Nasional yg
menyediakan vaksin gratis
PENCEGAHAN INFEKSI
Observasi (Kaji) Terapeutik (Mandiri) Edukasi Kolaborasi
Monitor tanda dan •Batasi jumlah Jelaskan tanda dan Kolaborasi pemberian
gejala infeksi lokal pengunjung gejala infeksi imunisasi bila perlu
dan sistemik •Berikan perawatan Ajarkan cara cuci
kulit pada area edema tangan yang benar
•Cuci tangan sblm dan Ajarkan etika batuk
sesudah kontak dg Ajarkan cara
pasien dan ling.pasien memeriksa kondisi
•Pertahankan teknik luka/luka operasi
aseptik pd pasien Anjurkan
beriko tinggi meningkatkan asupan
cairan
Keletihan
Intervensi Utama
Edukasi aktivitas/istirahat
Mengajarkan pengaturan aktivitas dan istirahat
Manajemen Energi
Edukasi aktivitas
aktivitas//istirahat
Observasi (Kaji) Terapeutik (Mandiri) Edukasi
•Identifikasi kesiapan •Sediakan materi dan Jelaskan pentingnya
dan kemampuan media pengaturan aktivitas melakukan aktivitas
menerim informasi dan istirahat fisik/olahraga secara rutin
•Jadwalkan pemberian Anjurkan terlibat dlm
penkes sesuai kesepakatan aktivitas kelompok, bermain,
•Berikan kesemapatan dll
pasien dan klg untuk Anjurkan menyusun jadwal
bertanya aktivitas dan istirahat
Ajarkan cara
mengidentifikasi kebutuhan
istirahat (mis, kelelahan,
sesak napas saat aktivitas)
OBSERVASI
- Identifikasi kesiapan &
kemampuan menerima
informasi
- Identifikasi faktor2 yg
meningkatkan dan m
menurunkan motivasi hidup
bersih dan sehat
TERAPEUTIK
DEFISIT EDUKASI - Sediakan materi dan media
penkes
PENGETAHUAN
(D 0111) KESEHATAN - Jadwalkan penkes sesuai
kesepakatan
- Berikan kesempatan bertanya
EDUKASI
- Jelaskan faktor risiko
mempengaruhi kes
- Ajarkan prilaku hdup bersih
dan sehat
(PPNI, 2018) - Jelaskan strategi
meningkatkan PHBS
37
View publication stats
You might also like
- Nursing Care Plan For "Diabetes Mellitus - Diabetic Ketoacidosis"Document17 pagesNursing Care Plan For "Diabetes Mellitus - Diabetic Ketoacidosis"jhonroks97% (36)
- OB - Normal Labor and DeliveryDocument51 pagesOB - Normal Labor and DeliveryJosh Matthew Rosales33% (3)
- Nursing Care of PT With DiabetesDocument71 pagesNursing Care of PT With DiabetesEricka Lj Robles DimaculanganNo ratings yet
- Standar Asuhan Keperawatan Diabetes Mellitus: PresentationDocument39 pagesStandar Asuhan Keperawatan Diabetes Mellitus: PresentationpuspitaNo ratings yet
- Diabetes Long Term 2016Document20 pagesDiabetes Long Term 2016Regina PunNo ratings yet
- Presentation On Diabetes MellitusDocument47 pagesPresentation On Diabetes Mellitusankita guptaNo ratings yet
- Sristika SharmaDocument26 pagesSristika SharmaSristi ChNo ratings yet
- DiabetesDocument14 pagesDiabetesaravindNo ratings yet
- Type 1 Diabetes Mellitus PP pth617Document10 pagesType 1 Diabetes Mellitus PP pth617api-621438645No ratings yet
- Week 7 Diabetes MellitusDocument34 pagesWeek 7 Diabetes MellitusHERLIN HOBAYANNo ratings yet
- Diabetes MellitusDocument52 pagesDiabetes MellitusMervis masatunyaNo ratings yet
- Bio Project On DiabetesDocument17 pagesBio Project On DiabetesNishant KumarNo ratings yet
- Paeda DMDocument38 pagesPaeda DMAmanuel LemiNo ratings yet
- Eating Disorder by Group 8Document18 pagesEating Disorder by Group 8Lynjenne OcenarNo ratings yet
- Diabetes Mellitus - Diabetic KetoacidosisDocument21 pagesDiabetes Mellitus - Diabetic KetoacidosisJamil Lorca100% (5)
- Diabetes Mellitus: December 2014Document10 pagesDiabetes Mellitus: December 2014Hashim OmarNo ratings yet
- If DIABETESDocument22 pagesIf DIABETESVictor Jesus Victorsg Siguas GarciaNo ratings yet
- A Presentation On: Diabetes MellitusDocument17 pagesA Presentation On: Diabetes MellitusAnil YadavNo ratings yet
- Diabetes Mellitus Lecture - 23!24!1Document83 pagesDiabetes Mellitus Lecture - 23!24!1afeefahalli5No ratings yet
- Diabetes Mellitus - Diabetic KetoacidosisDocument17 pagesDiabetes Mellitus - Diabetic Ketoacidosismardsz100% (1)
- Holistic Approach To Endocrine: Presented By: Sadia YaqoobDocument17 pagesHolistic Approach To Endocrine: Presented By: Sadia YaqoobSadia NadeemNo ratings yet
- Diabetes MellitusDocument24 pagesDiabetes MellitusAdi Prabowo SyamsNo ratings yet
- DiabetesDocument142 pagesDiabetesMushfiqa HasanNo ratings yet
- Diabetes 101 - An Overview of Diabetes and Its Management - Michael SeeDocument88 pagesDiabetes 101 - An Overview of Diabetes and Its Management - Michael SeeSangar MahmoodNo ratings yet
- 5 DM - Introduction, Diagnosis& ComplicationsDocument81 pages5 DM - Introduction, Diagnosis& ComplicationsLexis SanchizieNo ratings yet
- DiabetesDocument38 pagesDiabetesAlfie SorianoNo ratings yet
- Physical Evaluation I (Dent 5121) : Endocrine System: Diabetes MellitusDocument47 pagesPhysical Evaluation I (Dent 5121) : Endocrine System: Diabetes MellitusShosoo ShooshoNo ratings yet
- Diabetes Younes Ferwana Mohamed MehgizDocument43 pagesDiabetes Younes Ferwana Mohamed MehgizHakim oğluNo ratings yet
- Diabetes Melitus Group 4Document10 pagesDiabetes Melitus Group 4ahmad rizalNo ratings yet
- Diabetic NephropathyDocument62 pagesDiabetic Nephropathydevyani meshramNo ratings yet
- Grp.10 DiabetesDocument15 pagesGrp.10 DiabetesVanessa JanneNo ratings yet
- DefinitionDocument4 pagesDefinitionAgieNo ratings yet
- DIABETESDocument12 pagesDIABETESbenjamin morianoNo ratings yet
- Diabetes MellitusDocument19 pagesDiabetes Mellitusroshinirose2005No ratings yet
- Type 1 Diabetes Mellitus Nael HernandezDocument15 pagesType 1 Diabetes Mellitus Nael HernandezShermayne Mallapre HernandezNo ratings yet
- Nursing Care Plan For Diabetes Mellitus Diabetic KetoacidosisDocument17 pagesNursing Care Plan For Diabetes Mellitus Diabetic KetoacidosisJordz Placi100% (2)
- Addisons DiseaseDocument14 pagesAddisons DiseaseJils SureshNo ratings yet
- Diabetic EmergenciesDocument41 pagesDiabetic EmergenciesYuNa YoshinoyaNo ratings yet
- Sindrom Nefrotik Diabetus Melitus Type 2 DyslipidemiaDocument6 pagesSindrom Nefrotik Diabetus Melitus Type 2 DyslipidemiaAndi WidyaNo ratings yet
- DiabatesDocument10 pagesDiabatesMuhammad touseefNo ratings yet
- Diabetes Mellitus: Prepared by Divya Bhusal B.SC - Nursing 3 YearDocument43 pagesDiabetes Mellitus: Prepared by Divya Bhusal B.SC - Nursing 3 YearSristi LamsalNo ratings yet
- Diabetes Students Fall21Document59 pagesDiabetes Students Fall21Ismael SerunjogiNo ratings yet
- Paper ElektifDocument10 pagesPaper Elektifamyliadwi22No ratings yet
- The Disease Called DiabetesDocument71 pagesThe Disease Called Diabetesone_nd_onlyuNo ratings yet
- Addtl DMDocument5 pagesAddtl DMBautista, Lian RobbieNo ratings yet
- DiabetesDocument34 pagesDiabetesqurat-ul-ain.sonNo ratings yet
- Diabetes Mellitus - Nursing CareDocument51 pagesDiabetes Mellitus - Nursing CareJoice DasNo ratings yet
- Diabetes Foot CheckDocument62 pagesDiabetes Foot CheckIosefina DudeanuNo ratings yet
- Case Study 12Document7 pagesCase Study 12Steve MizzoNo ratings yet
- Diabetes Mellitus HospitalDocument29 pagesDiabetes Mellitus HospitalgegeNo ratings yet
- Metabolic DiseasesDocument35 pagesMetabolic DiseasesSOFIA YVONNE ZANONo ratings yet
- DIABETES MELLITUS Presentation (1) .PPTMDocument124 pagesDIABETES MELLITUS Presentation (1) .PPTMfrankNo ratings yet
- A Guide to Diabetes: Symptoms; Causes; Treatment; PreventionFrom EverandA Guide to Diabetes: Symptoms; Causes; Treatment; PreventionNo ratings yet
- Type 2 Diabetes: How to Eat Better, Lower Blood Sugar, and Manage DiabetesFrom EverandType 2 Diabetes: How to Eat Better, Lower Blood Sugar, and Manage DiabetesNo ratings yet
- Smoothies for Diabetics: Reverse Diabetes and Lower Blood Sugar with 36 Quick & Easy Delicious Diabetic Smoothie RecipesFrom EverandSmoothies for Diabetics: Reverse Diabetes and Lower Blood Sugar with 36 Quick & Easy Delicious Diabetic Smoothie RecipesRating: 5 out of 5 stars5/5 (2)
- Benefits of Cardiorespiratory Endurance ExercisesDocument8 pagesBenefits of Cardiorespiratory Endurance ExercisesFarhah RahimanNo ratings yet
- Spinal SurgeryDocument19 pagesSpinal SurgerySalomeSibashviliNo ratings yet
- Case Study UrtiDocument9 pagesCase Study UrtiRonica GonzagaNo ratings yet
- Influence of Infection at The Time of Root Filling On The Outcome of Endodontic Treatment of Teeth With Apical Periodontitis Sjogren 1997Document10 pagesInfluence of Infection at The Time of Root Filling On The Outcome of Endodontic Treatment of Teeth With Apical Periodontitis Sjogren 1997abcder1234No ratings yet
- Akapulko: Herbal Medicines Approved by DOHDocument4 pagesAkapulko: Herbal Medicines Approved by DOHYohan NahoNo ratings yet
- TALLY 79 Respondents FinalDocument7 pagesTALLY 79 Respondents FinalMarissa AsimNo ratings yet
- Effect of Periodontal Therapy On C-Reactive Protein Levels in Gingival Crevicular Fluid of Patients With Gingivitis and Chronic PeriodontitisDocument5 pagesEffect of Periodontal Therapy On C-Reactive Protein Levels in Gingival Crevicular Fluid of Patients With Gingivitis and Chronic PeriodontitisKanagavalli VijayakumarNo ratings yet
- MAPEH 9 PE and Halth 2nd Quarter Examination FinalDocument2 pagesMAPEH 9 PE and Halth 2nd Quarter Examination Finalcecile80% (10)
- RH Factor PGDocument3 pagesRH Factor PGapi-375530349No ratings yet
- Complication of Sinus DiseaseDocument27 pagesComplication of Sinus DiseaseukhuholicNo ratings yet
- Short Case Hydrocephalus: by Febrianto Haba Bunga, S.Ked Consultant DR .Donny Argie, SP - BSDocument29 pagesShort Case Hydrocephalus: by Febrianto Haba Bunga, S.Ked Consultant DR .Donny Argie, SP - BSErkoNo ratings yet
- Shock RosenDocument10 pagesShock RosenJuan GallegoNo ratings yet
- IsoketDocument2 pagesIsoketJaessa FelicianoNo ratings yet
- HSC4555 0001 Fall17 SyllabusDocument6 pagesHSC4555 0001 Fall17 SyllabusDilly RijoNo ratings yet
- ANC ModuleDocument103 pagesANC ModulePreeti ChouhanNo ratings yet
- Hospital Infections PDFDocument794 pagesHospital Infections PDFJOSEPH APPIAHNo ratings yet
- Glass Prescription - SutrishnaDocument15 pagesGlass Prescription - SutrishnaSutrishna PramanikNo ratings yet
- A Leading Surgical Gastroenterologist in Hyderabad Dr. Dinesh ReddyDocument4 pagesA Leading Surgical Gastroenterologist in Hyderabad Dr. Dinesh Reddydrdineshreddy02No ratings yet
- General DeclarationDocument1 pageGeneral DeclarationPos SMB IINo ratings yet
- What Is Jet Lag?: Fatigue InsomniaDocument20 pagesWhat Is Jet Lag?: Fatigue InsomniaAfria Beny SafitriNo ratings yet
- BreechDocument2 pagesBreechBrel KirbyNo ratings yet
- Requires Ongoing Support From Your Service: A Heart AttackDocument2 pagesRequires Ongoing Support From Your Service: A Heart AttackBîrlădeanu VlăduţNo ratings yet
- Cyanosis Definition of Cyanosis in The MedicalDocument4 pagesCyanosis Definition of Cyanosis in The MedicalTavish B PrasadNo ratings yet
- General AnaestheticsDocument71 pagesGeneral AnaestheticsTamilarasanNo ratings yet
- The Chronicle of Neurology + Psychiatry Aug 30 2011Document24 pagesThe Chronicle of Neurology + Psychiatry Aug 30 2011Nino AvantiNo ratings yet
- Medicago Sativa LloydDocument4 pagesMedicago Sativa LloydDr Rushen SinghNo ratings yet
- Khushboo PPT Covid 19Document17 pagesKhushboo PPT Covid 19Birlal SinghNo ratings yet
- Drug Study - LactuloseDocument1 pageDrug Study - LactuloseCarla Tongson MaravillaNo ratings yet
- Intership Questionnaire For Cleaning Tools Used in HospitalsDocument4 pagesIntership Questionnaire For Cleaning Tools Used in HospitalsSomannaNo ratings yet