Professional Documents
Culture Documents
Sommers-Flanagan Et Al. (2020) - Clinical Interviewing
Uploaded by
Isaac FullartonOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Sommers-Flanagan Et Al. (2020) - Clinical Interviewing
Uploaded by
Isaac FullartonCopyright:
Available Formats
10 Clinical Interviewing
JOHN SOMMERS-FLANAGAN, VERONICA I. JOHNSON, AND MAEGAN RIDES AT THE DOOR
The clinical interview is a fundamental assessment and Tackling and managing all or some of these goals and
intervention procedure that mental and behavioral health objectives during a limited time frame is no small feat,
professionals learn and apply throughout their careers. even for experienced clinicians. In cases when clinical
Psychotherapists across all theoretical orientations, pro- interviewing is used solely for assessment purposes, there
fessional disciplines, and treatment settings employ differ- is still an art to balancing information gathering with
ent interviewing skills, including, but not limited to, efforts to develop rapport and solicit client cooperation.
nondirective listening, questioning, confrontation, inter- In this chapter, we describe and explore clinical inter-
pretation, immediacy, and psychoeducation. As a process, viewing as foundational to mental health assessment and
the clinical interview functions as an assessment (e.g., intervention. To start, we review the origins and develop-
neuropsychological or forensic examinations) or signals ment of clinical interviewing, including how interviews
the initiation of counseling or psychotherapy. Either way, can vary with respect to theoretical orientation, setting,
clinical interviewing involves formal or informal client problem, and purpose. Subsequently, we present
assessment. a generic, atheoretical interviewing model, along with sev-
Clinical interviewing is dynamic and flexible; every inter- eral variations for clinicians who are required or inspired
view is a unique interpersonal interaction, with interviewers to use the clinical interview as a specific assessment
integrating cultural awareness, knowledge, and skills, as procedure. We close the chapter with a discussion of lim-
needed. It is difficult to imagine how clinicians could begin itations, cultural issues, technological advances, and the
treatment without an initial clinical interview. In fact, clin- future of clinical interviewing.
icians who do not have competence in using clinical inter-
viewing as a means to initiate and inform treatment would THE CLINICAL INTERVIEW: ORIGINS,
likely be considered unethical (Welfel, 2016). DIALECTICS, AND INFLUENTIAL FORCES
Clinical interviewing has been defined as
In the 1920s, Swiss psychologist Jean Piaget first used the
a complex and multidimensional interpersonal process that term “semi-clinical interview” to describe an assessment pro-
occurs between a professional service provider and client [or cess (Elkind, 1964). Piaget’s efforts to understand how chil-
patient]. The primary goals are (1) assessment and (2) help- dren acquire and understand concepts related to religion and
ing. To achieve these goals, individual clinicians may empha- God led him to blend psychiatric interviewing with standar-
size structured diagnostic questioning, spontaneous and
dized mental testing questions. Piaget’s approach was foun-
collaborative talking and listening, or both. Clinicians use
information obtained in an initial clinical interview to develop dational to how contemporary mental health professionals
a [therapeutic relationship], case formulation, and treatment later came to think about and practice clinical interviewing.
plan. (Sommers-Flanagan & Sommers-Flanagan, 2017, p. 6) Although the ideas and applications of clinical interviewing
have moved beyond Piaget’s original strategies, many of the
Given their breadth and multidisciplinary nature, clin-
core attitudes required to conduct successful clinical inter-
ical interviews have one or more of the following goals and
views remain the same (e.g., “a liking for [clients], a respect
objectives:
for their individuality, and patience”; Elkind, 1964, p. 41).
1. initiate and develop a therapeutic relationship Piaget’s purpose was primarily assessment (i.e., informa-
2. provide a role induction or orientation to therapy tion gathering). More recently, postmodern theorists and
3. acquire assessment and diagnostic information psychotherapists have emphasized that initial interviews
4. formulate a case conceptualization and treatment are therapeutic. Specifically, during interviews, clinicians
plan are viewed as not just “taking [a] history” but also “making
5. implement a psychological or educational intervention history” (Hoyt, 2000, p. 3). Hoyt’s description speaks to the
(adapted from Sommers-Flanagan, 2016). therapeutic component of clinical interviewing.
113
https://doi.org/10.1017/9781108235433.010 Published online by Cambridge University Press
114 JOHN SOMMERS-FLANAGAN, VERONICA I. JOHNSON, AND MAEGAN RIDES AT THE DOOR
An Interviewing Dialectic MSE, psychological or psychiatric evaluations, and treat-
ment planning. Social workers typically focus more on
Clinical interviewing’s flexibility includes a dialectic in
psychosocial history, family history, and systemic or cul-
purpose and process. On the one hand, many researchers
tural issues. In contrast, professional counselors orient
view clinical interviews primarily as a means for gathering
toward relationship development, collaborative engage-
objective, quantifiable data. In contrast, practitioners
ment, and client wellness or strengths.
value clinical interviews as a relational process that facil-
Clinician theoretical orientation and skills also influ-
itates client and clinician collaboration. Despite polariza-
ence how professionals conduct interviews. An Adlerian
tion regarding the true purpose and process of clinical
therapist is likely to conduct a family constellation inter-
interviews, interviews can and should integrate both scien-
view during a first session. Family systems therapists
tific and relational components (Sommers-Flanagan &
might engage clients in a similar process but call it
Sommers-Flanagan, 2017). Overall, clinical interviewing
a genogram assessment. Clinicians with a behavioral
exists within a large tent; it encompasses the richness of
orientation conduct in-session or in vivo functional beha-
witnessing and empathically resonating with human
vioral assessments; their focus would be on defining spe-
experiences; it also involves collecting reliable and valid
cific problem behaviors and identifying behavioral
assessment data.
antecedents and consequences. These theory-based inter-
view approaches contribute to case formulation and treat-
ment planning.
Factors That Influence and Drive Clinical Interviews
Clinical interviews look and feel quite different depending Structured, semi-structured, and unstructured interviews.
on many factors. Clinical interviews also vary based on time and structure.
The most prescriptive clinical interview is the structured
Interview setting and purpose. Interview purpose and interview. Structured interviews follow a predetermined
clinical setting are intimately intertwined. For example, question list. Nearly all structured interviews are psycho-
a clinician working at an adoption agency might interview diagnostic interviews; clinicians gather symptom-related
prospective parents with the singular goal of assessing their information with diagnostic formulation or behavioral
suitability as adoptive parents. In other settings, clinicians prediction as their ultimate goal. In contrast, unstructured
focus on mental status examinations (MSEs), violence interviews allow clients to talk freely while clinicians
potential, collecting forensic assessment data, or psy- respond with reflections, summaries, and open questions.
chotherapy preparation. Interviews conducted in private Semi-structured interviews, a middle ground of sorts, pro-
practice settings look very different from interviews in inpa- vide clinicians with structure and focus while retaining
tient settings or those conducted in outpatient mental health flexibility to explore content areas that emerge organically.
agency settings. Some settings (e.g., employee assistance
programs) emphasize interventions from first contact.
A GENERIC CLINICAL INTERVIEWING MODEL
Client factors. Clinicians should be sensitive to unique cli- All clinical interviews follow a common process or outline.
ent characteristics (Sue & Sue, 2016). Clients who present in Shea (1998) offered a generic or atheoretical model, includ-
crisis will likely benefit from brief and structured clinical ing five stages: (1) introduction, (2) opening, (3) body,
interviews, whereas clients struggling with divorce might (4) closing, and (5) termination. Each stage includes speci-
appreciate less structure and more opportunity to talk freely. fic relational and technical tasks.
Common client factors that influence clinical interviewing
process and content include, but are not limited to, (1) pre-
Introduction
senting problems or goals, (2) preferences about therapy, (3)
religious or spiritual identity, (4) coping style, (5) expecta- The introduction stage begins at first contact. An introduc-
tions, (6) culture, and (7) client resources (Norcross & tion can occur via telephone, online, or when prospective
Lambert, 2011). Identifying and addressing these character- clients read information about their therapist (e.g., online
istics can determine whether or not clients return to psy- descriptions, informed consents). Client expectations, role
chotherapy following an initial session (Sue & Sue, 2016). induction, first impressions, and initial rapport-building
are central issues and activities.
Clinician factors. Several clinician factors drive the inter- First impressions, whether developed through informed
view. At minimum, these include professional discipline, consent paperwork or initial greetings, can exert powerful
theoretical orientation, and clinician skills. influences on interview process and clinical outcomes.
Clinicians from psychiatry, psychology, social work, and Mental health professionals who engage clients in ways
professional counseling use interviews for overlapping pur- that are respectful and culturally sensitive are likely to
poses. However, each discipline also has a primary empha- facilitate trust and collaboration, consequently resulting
sis. Specifically, psychiatrists and psychologists tend to use in more reliable and valid assessment data (Ganzini et al.,
interviews for assessment, including psychiatric diagnosis, 2013). Technical strategies include authentic opening
https://doi.org/10.1017/9781108235433.010 Published online by Cambridge University Press
CLINICAL INTERVIEWING 115
statements that invite collaboration. For example, the clin- structured interviews, specific question protocols are fol-
ician might say something like, “I’m looking forward to lowed. These protocols are designed to help clinicians stay
getting to know you better” and “I hope you’ll feel comfor- focused and systematically collect reliable and valid
table asking me whatever questions you like as we talk assessment data.
together today.” Using friendliness and small talk can be
especially important to connecting with diverse clients Closing
(Hays, 2016; Sue & Sue, 2016). The introduction stage
also includes discussions of (1) confidentiality, (2) thera- As the interview progresses, it is the clinician’s responsi-
pist theoretical orientation, and (3) role induction (e.g., bility to organize and close the session in ways that assure
“Today I’ll be doing a diagnostic interview with you. That there is adequate time to accomplish the primary inter-
means I’ll be asking lots of questions. My goal is to better view goals. Tasks and activities linked to the closing
understand what’s been troubling you.”). The introduction include (1) providing support and reassurance for clients,
ends when clinicians shift from paperwork and small talk (2) returning to role induction and client expectations, (3)
to a focused inquiry into the client’s problems or goals. summarizing crucial themes and issues, (4) providing an
early case formulation or mental disorder diagnosis, (5)
instilling hope, and, as needed, (6) focusing on future
Opening homework, future sessions, and scheduling (Sommers-
The opening provides an initial focus. Most mental health Flanagan & Sommers-Flanagan, 2017).
practitioners begin clinical assessments by asking some-
thing like, “What concerns bring you to counseling today?” Termination
This question guides clients toward describing their pre-
senting problem (i.e., psychiatrists refer to this as the Termination involves ending the session and parting ways.
“chief complaint”). Clinicians should be aware that open- The termination stage requires excellent time management
ing with questions that are more social (e.g., “How are you skills; it also requires intentional sensitivity and responsive-
today?” or “How was your week?”) prompt clients in ways ness to how clients might react to endings in general or
that can unintentionally facilitate a less focused and more leaving the therapy office in particular. Dealing with termi-
rambling opening stage. Similarly, beginning with direct nation can be challenging. Often, at the end of an initial
questioning before establishing rapport and trust can eli- session, clinicians will not have enough information to
cit defensiveness and dissembling (Shea, 1998). establish a diagnosis. When diagnostic uncertainty exists,
Many contemporary therapists prefer opening state- clinicians may need to continue gathering information
ments or questions with positive wording. For example, about client symptoms during a second or third session.
rather than asking about problems, therapists might ask, Including collateral informants to triangulate diagnostic
“What are your goals for our meeting today?” For clients information may be useful or necessary. See Chapter 11 of
with a diverse or minority identity, cultural adaptations this volume for more details on collateral reports.
may be needed to increase client comfort and make certain
that opening questions are culturally appropriate and rele- CLINICAL INTERVIEWING AS ASSESSMENT
vant. When focusing on diagnostic assessment and using The clinical interview often involves more assessment and
a structured or semi-structured interview protocol, the for- less intervention. Interviewing assessment protocols or
mal opening statement may be scripted or geared toward procedures may not be limited to initial interviews; they
obtaining an overview of potential psychiatric symptoms can be woven into longer term assessment or therapy
(e.g., “Does anyone in your family have a history of mental encounters. Allen Frances (2013), chair of the DSM-IV
health problems?”; Tolin et al., 2018, p. 3). task force, recommended that clinicians “be patient,”
because accurate psychiatric diagnosis may take “five min-
Body utes,” “five hours,” “five months, or even five years” (p. 10).
Four common assessment interviewing procedures are
The interview purpose governs what happens during the discussed next: (1) the intake interview, (2) the psycho-
body stage. If the purpose is to collect information pertain- diagnostic interview, (4) MSEs, and (4) suicide assessment
ing to psychiatric diagnosis, the body includes diagnostic- interviewing.
focused questions. In contrast, if the purpose is to initiate
psychotherapy, the focus could quickly turn toward the
The Intake Interview
history of the problem and what specific behaviors, peo-
ple, and experiences (including previous therapy) clients The intake interview is perhaps the most ubiquitous clin-
have found more or less helpful. ical interview; it may be referred to as the initial interview,
When the interview purpose is assessment, the body the first interview, or the psychiatric interview. What fol-
stage focuses on information gathering. Clinicians actively lows is an atheoretical intake interview model, along with
question clients about distressing symptoms, including examples of how theoretical models emphasize or ignore
their frequency, duration, intensity, and quality. During specific interview content.
https://doi.org/10.1017/9781108235433.010 Published online by Cambridge University Press
116 JOHN SOMMERS-FLANAGAN, VERONICA I. JOHNSON, AND MAEGAN RIDES AT THE DOOR
Broadly speaking, intake interviews focus on three The Mental Status Examination
assessment areas: (1) presenting problem, (2) psychoso-
The MSE is a semi-structured interview protocol. MSEs
cial history, and (3) current situation and functioning. The
are used to organize, assess, and communicate informa-
manner in which clinicians pursue these goals varies
tion about clients’ current mental state (Sommers-
greatly. Exploring the client’s presenting problem could
Flanagan, 2016; Strub & Black, 1977). To achieve this
involve a structured diagnostic interview, generation and
goal, some clinicians administer a highly structured Mini-
analysis of a problem list, or clients free associating to
Mental State Evaluation (MMSE; Folstein, Folstein, &
their presenting problem. Similarly, the psychosocial his-
McHugh, 1975), while others conduct a relatively unstruc-
tory can be a cursory glimpse at past relationships and
tured assessment interview but then organize their obser-
medical history or a rich and extended examination of
vations into a short mental status report. There are also
the client’s childhood. Gathering information about the
clinicians who, perhaps in the spirit of Piaget’s semi-
client’s current situation and functioning can range from
clinical interviews, combine the best of both worlds by
an informal query about the client’s typical day to a formal
integrating a few structured MSE questions into a less
MSE (Yalom, 2002).
structured interview process (Sommers-Flanagan &
Sommers-Flanagan, 2017).
Psychodiagnostic Interviewing Although the MSE involves collecting data on diagnostic
symptoms, it is not a psychodiagnostic interview. Instead,
The psychodiagnostic interview is a variant of the intake
clinicians collect symptom-related data to communicate
interview. For mental health professionals who embrace
information to colleagues about client mental status.
the medical model, initial interviews are often diagnostic
Sometimes MSEs are conducted daily or hourly. MSEs
interviews. The purpose of a psychodiagnostic interview is
are commonly used within medical settings. Knowledge
to establish a psychiatric diagnosis. In turn, the purpose of
of diagnostic terminology and symptoms is a prerequisite
psychiatric diagnosis is to describe the client’s current
to conducting and reporting on mental status.
condition, prognosis, and guide treatment.
Psychodiagnostic interviewing is controversial. Some
Introducing the MSE. When administering an MSE, an
clinicians view it as essential to treatment planning and
explanation or role induction is needed. A clinician might
positive treatment outcomes (Frances, 2013). Others
state, “In a few minutes, I’ll start a more formal method
view it in ways similar to Carl Rogers (1957), who
of getting . . . to know you. This process involves me asking
famously wrote, “I am forced to the conclusion that . . .
you a variety of interesting questions so that I can understand
diagnostic knowledge is not essential to psychotherapy. It
a little more about how your brain works” (Sommers-
may even be . . . a colossal waste of time” (pp. 102–103). As
Flanagan & Sommers-Flanagan, 2017, pp. 580–581).
with many polarized issues, it can be useful to take
a moderate position, recognizing the potential benefits
Common MSE domains. Depending on setting and clini-
and liabilities of diagnostic interviewing. Benefits include
cian factors, the MSE may focus on neurological responses
standardization, a clear diagnostic focus, and identifica-
or psychiatric symptoms. Nine common domains included
tion of psychiatric conditions to facilitate clinical
in a psychiatric-symptom oriented MSE are
research and treatment (Lilienfeld, Smith, & Watts,
2013). Liabilities include extensive training required,
1. Appearance
substantial time for administration, excess structure
2. Behavior/psychomotor activity
and rigidity that restrain experienced clinicians, and
3. Attitude toward examiner (interviewer)
questionable reliability and validity, especially in real-
4. Affect and mood
world clinical settings (Sommers-Flanagan & Sommers-
5. Speech and thought
Flanagan, 2017).
6. Perceptual disturbances
Clinicians who are pursuing diagnostic information
7. Orientation and consciousness
may integrate structured or semi-structured diagnostic
8. Memory and intelligence
interviews into an intake process. The research literature
9. Reliability, judgment, and insight.
is replete with structured and semi-structured diagnostic
interviews. Clinicians can choose from broad and compre- Given that all assessment processes include error and bias,
hensive protocols (e.g., the Structured Clinical Interview mental status examiners should base their reports on direct
for DSM-5 Disorders – Clinician Version; First et al., 2016) observations and minimize interpretive statements. Special
to questionnaires focusing on a single diagnosis (e.g., care to cross-check conclusive statements is necessary, espe-
Autism Diagnostic Interview – Revised; Zander et al., cially when writing about clients who are members of tradi-
2017). Additionally, some diagnostic interviewing proto- tionally oppressed minority groups (Sommers-Flanagan &
cols are designed for research purposes, while others help Sommers-Flanagan, 2017). Additionally, using multiple
clinicians attain greater diagnostic reliability and validity. assessment data sources (aka triangulation; see “Using mul-
Later in this chapter we focus on psychodiagnostic inter- tiple (collateral) data sources”) is essential in situations
viewing reliability and validity. where patients may have memory problems (e.g.,
https://doi.org/10.1017/9781108235433.010 Published online by Cambridge University Press
CLINICAL INTERVIEWING 117
confabulation) or be motivated to over- or underreport • Hopelessness: Hopelessness is a cognitive variable
symptoms (Suhr, 2015). linked to suicide risk. It can also contribute to problem-
solving impairments.
MSE reports. MSE reports are typically limited to one para- • Suicide intent and plan: Although suicide ideation is
graph or one page. The content of an MSE report focuses a poor predictor of suicide, when ideation is accompa-
specifically on the previously listed nine domains. Each nied by an active suicide plan and suicide intent, the
domain is addressed directly with at least one statement. potential of death by suicide is magnified.
• Desensitization to physical pain and thoughts of death:
Fear of death and aversion to physical pain are natural
Suicide Assessment Interviewing
suicide deterrents; when clients lose their fear of death
The clinical interview is the gold standard for suicide or become desensitized to pain, suicide behaviors can
assessment and intervention (Sommers-Flanagan, 2018). increase.
This statement is true, despite the fact that suicide assess- • Access to firearms: Availability of a lethal means, in gen-
ment interviewing is not a particularly reliable or valid eral, and access to firearms, in particular, substantially
method for predicting death by suicide (Large & Ryan, increase suicide risk.
2014). The problem is that, although standardized written
(For additional information on suicide assessment inter-
assessments exist, they are not a stand-alone means for
viewing and the eight suicide dimensions, see Sommers-
predicting or intervening with clients who present with
Flanagan, 2018; and Chapter 23 in this volume.)
suicide ideation. In every case, when clients endorse sui-
cide ideation on a standardized questionnaire or scale,
a clinical interview follow-up is essential. Although other LIMITATIONS, CULTURAL ISSUES,
assessment approaches exist, they are only supplementary AND INNOVATIONS
to the clinical interview. Key principles for conducting
Although clinical interviews are a flexible assessment and
suicide assessment interviews are summarized below.
therapy tool, they also have limitations. These limitations
vary depending on the particular approach being
Contemporary suicide assessment principles. Historically,
implemented.
suicide assessment interviewing involved a mental health
professional conducting a systematic suicide risk
assessment. Over the past two decades, this process has
Diagnostic Reliability and Validity
changed considerably. Now, rather than taking an author-
itative stance, mental health professionals seek to estab- The publication of the third edition of the Diagnostic and
lish an empathic and collaborative relationship with Statistical Manual of Mental Disorders (DSM-III; American
clients who are suicidal (Jobes, 2016). Also, rather than Psychiatric Association, 1980) was greeted with high praise
assuming that suicide ideation indicates psychopathology from the psychiatric-medical community. Previous ver-
or suicide risk, clinicians frame suicide ideation as sions of the DSM adhered to a psychoanalytic model and
a communication of client distress. Finally, instead of had vague symptom criteria sets. Advocates for psychiatric
focusing on risk factors and suicide prediction, mental diagnosis emphasized that DSM-III’s improved specificity
health professionals gather information pertaining to and atheoretical model approach had solved previous pro-
eight superordinate suicide dimensions or drivers and blems with diagnostic reliability. Later, with the publica-
then work with suicidal clients to address these dimen- tion of the DSM-III-R (American Psychiatric Association,
sions through a collaborative and therapeutic safety plan- 1994), structured diagnostic interviewing protocols like the
ning process (Jobes, 2016). The eight superordinate Structured Clinical Interview for DSM-III-R (then the SCID-
suicide dimensions include: III-R, now the SCID-5; First et al., 2016) were praised as
greatly improving clinician inter-rater reliability. Currently,
• Unbearable emotional or psychological distress: most diagnostic interview protocols or schedules are based
Unbearable distress can involve one or many trauma, on diagnostic criteria from the DSM-5 (American
loss, or emotionally disturbing experiences. Psychiatric Association, 2013).
• Problem-solving impairments: Suicide theory and Despite apparent improvements, inter-rater reliability
empirical evidence both point to ways in which depres- for specific diagnostic conditions remains questionable
sive states can reduce client problem-solving abilities. (Lobbestael, Leurgans, & Arntz, 2011; Salamon et al.,
• Interpersonal disconnection, isolation, or feelings of 2018). In 1997, Kutchins and Kirk wrote, “Twenty years
being a social burden: Joiner (2005) has posited that after the reliability problem became the central scientific
thwarted belongingness and perceiving oneself as focus of DSM, there is still not a single major study showing
a burden contributes to suicidal conditions. that DSM (any version) is routinely used with high reliabil-
• Arousal or agitation: Many different physiological states ity by regular mental health clinicians . . . The DSM revolu-
can increase arousal/agitation and push clients toward tion in reliability has been a revolution in rhetoric, not in
using suicide as a solution to their unbearable distress. reality” (Kutchins & Kirk, 1997, p. 53).
https://doi.org/10.1017/9781108235433.010 Published online by Cambridge University Press
118 JOHN SOMMERS-FLANAGAN, VERONICA I. JOHNSON, AND MAEGAN RIDES AT THE DOOR
Over the past twenty years, researchers and reviewers their symptoms, particularly in some contexts where indivi-
have described structured diagnostic interviews as demon- duals have a substantial incentive (e.g., a forensic
strating “adequate” or “moderate” or “excellent” inter-rater assessment).
reliability (Lilienfeld et al., 2013; Lobbestael et al., 2011; Contemporary researchers and practitioners refer to
Tolin et al., 2018). Although these claims provide surface inaccurate client responses as noncredible responding
support for diagnostic reliability, a deeper examination (Suhr & Berry, 2017). As Suhr (2015) summarized, non-
raises questions and doubts. Specifically, studies focusing credible responding is a substantial problem for clinical
on inter-rater reliability utilize highly trained diagnostic interviewers; under certain circumstances, “the base rate
raters. These raters are not clinicians in everyday practice; for noncredible responding in individuals reporting psy-
consequently, results based on their inter-rater reliability chological, physical, and/or cognitive symptoms and con-
are unlikely to generalize to real-world clinical practice. cerns is higher than the base rate of most actual
Additionally, the language used to describe and label the disorders!” (p. 61).
acceptability of kappa coefficients (a reliability measure) is
derived from DSM field trial recommendations. For exam- Overreporting symptoms. Clients who exaggerate symp-
ple, following the DSM-5 field trial recommendations, one toms to obtain external gain are often referred to as mal-
study described the kappa coefficient for an attention- ingering or feigning (Green & Rosenfeld, 2011; Rogers,
deficit/hyperactivity disorder (ADHD) diagnosis as “very 2008). Several assessment tools have been designed to
good.” The label very good was used despite researchers detect malingering. An interview-based example is the
reporting a confidence interval for the ADHD-related Structured Interview of Reported Symptoms-2 (SIRS-2;
kappa reliability index as in the range “0.33–0.87” (Tolin Rogers, Sewell, & Gillard, 2010). The SIRS-2 includes 172
et al., 2018). In this case, using the DSM convention for interview items (with thirty-two items repeated to evaluate
labeling kappa coefficients made a coefficient with an R2 for consistency) and takes one to two hours to administer.
(coefficient of determination) ranging as low as R2 = 0.10 The original SIRS was often regarded as the gold standard
sound “very good” (which is clearly misleading). Further, for measuring malingering. However, more recently,
even highly trained diagnostic interviewers have only mod- researchers have critiqued the SIRS as being susceptible
est agreement regarding specific diagnoses; they perform to misclassifying patients as feigning (Green & Rosenfeld,
more acceptably when using the simple categorical criter- 2011) and the SIRS-2 has been questioned as possibly hav-
ion of determining the presence or absence of a mental ing less sensitivity and utility than the original SIRS (Green,
disorder (Widiger & Edmundson, 2011). Rosenfeld, & Belfi, 2013).
Beyond reliability issues, many practicing clinicians
avoid using structured diagnostic interviews because Underreporting symptoms. Research on symptom under-
they take too much time and are not helpful for establish- reporting is generally within the substance use arena
ing therapy relationships. Nevertheless (and this makes (Bahorik et al., 2014; Hormes, Gerhardstein, & Griffin,
both sides of the argument more complex), if the purpose 2012). To avoid being viewed as ill, clients with addiction
of a clinical interview is psychiatric diagnosis, using problems are inclined to underestimate or deny substance
a structured diagnostic interviewing protocol based on use. Underreporting is also common in settings where full
the DSM system has significant scientific support, espe- symptom disclosure could have significant negative con-
cially if clinicians are trained to use these protocols. In sequences or in situations where having mental disorder
fact, diagnostic reliabilities for major mental disorders symptoms are in violation of social norms (e.g., athletic or
(e.g., depression, anxiety) typically have alpha or kappa military settings; Kroshus et al., 2015; Vannoy et al., 2017).
coefficients similar to what physicians obtain when diag- There are no published interview protocols designed to
nosing medical disorders (Lilienfeld et al., 2013). identify underreporting. Often, clinicians feel an urge to
Diagnostic validity is a more difficult issue. There are no confront clients who appear to be minimizing their pro-
genetic markers or gold standard for determining whether blems. Alternatives to using confrontation are integrated
a specific diagnosis is true or valid. To support diagnostic into the next section.
validity, researchers often rely on longitudinal studies
focusing on predictive validity. Unfortunately, results
Strategies for Addressing Noncredible
from diagnostic predictive validity studies tend to be
Responding in a Clinical Interview
mixed (Edens et al., 2015).
Clinical interviewing strategies for dealing with noncred-
ible client responses include (1) developing clinician
Noncredible or Invalid Client (Self-) Report
awareness, (2) managing countertransference, (3) using
Diagnostic clinical interviews rely on clients disclosing truth- specific questioning or interpersonal strategies, and (4)
ful or accurate information via self-report. Unfortunately, using additional or supplementary data sources.
client self-report is notoriously suspect (Rogers, 2008;
Sommers-Flanagan & Sommers-Flanagan, 1998; Suhr, Clinician awareness. Clinician awareness of the potential
2015). It is not unusual for clients to over- or underreport for noncredible responding is the foundation for dealing
https://doi.org/10.1017/9781108235433.010 Published online by Cambridge University Press
CLINICAL INTERVIEWING 119
with this common client response style. Specifically, clin- best, and so I’ll need to rely on what you tell me” and
icians should be aware that, due to motivational, contex- “Please ask me any questions at any time and I’ll do my
tual, and other factors, clients may systematically best to answer them.”
overreport, underreport, or misreport their presenting Normalizing statements are recommended for inter-
symptoms, personal history, social-cultural-sexual orienta- viewing potentially suicidal clients. Specifically, it can be
tion, and/or current functioning (i.e., impairment). As Suhr useful to precede direct questions about suicide ideation
(2015) wrote, “It might help for the assessor to remember with a statement like, “It’s not unusual for people who are
that inaccuracy of self-report is normal and often adaptive feeling stressed to have thoughts of suicide.” Similar nor-
behavior, even outside of the clinical context” (p. 100). malizing statements can be used with other symptoms
To avoid decision-making biases, it is recommended (e.g., “Lots of college students have difficulty sleeping,
that clinicians adopt a “scientific mindedness” frame dur- I wonder if that’s the case for you?”).
ing assessment interviews (S. Sue, 1998). Scientific mind- When interviewing clients with high potential for sub-
edness was originally described as a means to help stance use, Shea (1998) recommended using a questioning
clinicians avoid making premature cultural assumptions. strategy called gentle assumption. To use gentle assump-
However, adopting a mentality of intentionally forming tion, interviewers presume that specific embarrassing or
and testing hypotheses about the accuracy of client self- illegal behaviors are a regular occurrence in the client’s
reports can also help mitigate clinician bias (Shea, 1998). life. For example, instead of asking, “Do you drink alco-
hol?,” an interviewer might ask, “When was your most
Managing countertransference. Clinicians can have recent drink?”
countertransference reactions to clients before, during,
or after clients engage in noncredible responding. Using multiple (collateral) data sources. Stand-alone clin-
Countertransference reactions may, in turn, adversely ical interviews are especially vulnerable to over- or under-
affect rapport and relationship development. When this reporting of symptoms. This is particularly true when
happens, clinicians may prompt clients to provide non- situational factors offer external rewards and/or the avoid-
credible responses. For example, countertransference or ance of negative consequences for symptom exaggeration
lack of skills might lead clinicians to stray from an accept- or minimizing. For example, personal injury cases, learn-
ing stance and ask a question that includes a judgmental ing disability or ADHD evaluations, athletic or military
tone: “You aren’t using substances to help you sleep settings, and assessments conducted for forensic purposes
are you?” This sort of question can easily stimulate can motivate clients to present as having more or fewer
a noncredible, underreporting response of denial, “No. symptoms (Sellbom & Hopwood, 2016; Suhr, Cook, &
I wouldn’t do that.” Morgan, 2017; Sullivan, May, & Galbally, 2007; Vannoy
Several strategies can be used to manage countertrans- et al., 2017).
ference. Most commonly, personal therapy or additional Collateral information is data or information
skills-based training is helpful. For example, motivational obtained via a third party. For example, when conduct-
interviewing was designed, in part, to help clinicians move ing child assessments, clinicians commonly conduct
away from judgmental-confrontational approaches with collateral interviews with, or gather information via
substance-using clients. The central philosophy of motiva- questionnaire from, parents or teachers. Collateral
tional interviewing is person-centered, with a strong interviews can provide illuminating alternative perspec-
emphasis on the “profound acceptance of what the client tives. Unfortunately, parents, teachers, and other col-
brings” (Miller & Rollnick, 2013, p. 16). If countertransfer- lateral informants also may have motivational and
ence reactions occur, rather than engaging in confronta- memory issues that cause them to provide inaccurate
tion, clinical interviewers can refocus on adopting an information. Finding significant discrepancies between
attitude of profound acceptance. Otherwise, relational rup- parents, teachers, and child reports is a common occur-
tures and under- or overreporting of symptoms may occur rence (see Chapter 11 in this volume; Sommers-
(Sommers-Flanagan & Sommers-Flanagan, 2017). Flanagan & Sommers-Flanagan, 2017).
Medical, educational, and psychological/psychiatric
Using specific questioning or interpersonal strategies. records constitute additional sources of collateral assess-
Specific clinical skills or strategies can be used to address ment information. Unfortunately, clients’ previous
underreporting. These skills and strategies include (1) records also are not free from bias or inaccuracy.
modeling openness, (2) using normalizing statements, Consequently, although gathering collateral information
and (3) phrasing questions to make it easier for clients to is recommended for clinicians who are using a clinical
disclose symptoms. interview for assessment purposes, collateral information
Clinicians who begin sessions with an open and trans- is also susceptible to error. In the end, the best approach
parent informed consent process and role induction may typically involves gathering information from at least
be able to mitigate underreporting. Transparency can also three sources and then triangulating data in an effort to
include statements that invite collaboration. Examples present a reasonably accurate assessment report (see
include “I’d like to be helpful, but you know yourself Chapter 11, this volume).
https://doi.org/10.1017/9781108235433.010 Published online by Cambridge University Press
120 JOHN SOMMERS-FLANAGAN, VERONICA I. JOHNSON, AND MAEGAN RIDES AT THE DOOR
Cultural Considerations: Cultural Validity past; it will continue to flex along with various new social
and Cultural Humility and cultural dynamics, including the rise of technology in
the delivery of mental health services.
Cultural validity refers to how well assessment procedures
Technological advancements have affected mental and
address and are sensitive to client-specific cultural per-
behavioral health assessment and treatment in many
spectives (Basterra, Trumbull, & Solano-Flores, 2011).
ways. Some mental health professionals believe that tech-
Client cultural perspectives can include, but are not lim-
nology can improve their ability to acquire information,
ited to, “the sets of values, beliefs, experiences, commu-
support treatment plans, and track client outcomes.
nication patterns, teaching and learning styles, and
Others believe technology detracts from therapeutic rela-
epistemologies inherent in the [clients’] cultural back-
tionship development. Controversies around technology
grounds, and the socioeconomic conditions prevailing in
have been incorporated into professional ethical guide-
their cultural groups” (Solano-Flores & Nelson-Barber,
lines; clinicians should consult their respective ethical
2001, p. 55). If cultural validity is not considered, conclu-
codes when using technology (e.g., American Counseling
sions may be inaccurate and cause client harm.
Association, 2014; APA, 2010).
Clinicians are encouraged to make cultural adaptations
Computer-based assessments sometimes outperform
to address cultural validity. These adaptations may involve
clinician-based assessments (Richman et al., 1999). This
administering assessments in the client’s native language,
is particularly true when clients are expected to reveal
consulting with cultural experts, and using multidimen-
sensitive personal information (e.g., sexual behavior, sui-
sional assessment models (Hays, 2016). Using cultural
cide ideation). Regardless of computer-based assessment
validity checks and balances is especially important
efficiency, therapeutic follow-up requires face-to-face or
when implementing diagnostic assessment and mental
virtual human contact. Integrating technology for data
status protocols (Sommers-Flanagan & Sommers-
gathering and note-taking appears to have no adverse
Flanagan, 2017).
effects on assessment process or the development of ther-
Cultural humility is also linked to successful clinical
apeutic relationships (Wiarda et al., 2014).
interviewing. Clinicians who demonstrate cultural humi-
Online assessment and psychotherapy is growing as
lity go beyond the core multicultural competencies of clin-
a method of mental health service delivery. Proponents
ician self-awareness, culture-specific knowledge, and
include research scientists and medical practitioners who
culturally specific skills. Culturally humble clinicians are
deliver services from a distance, as well as entrepreneurial
defined as (1) other-oriented, (2) seeing clients as experts
independent practitioners seeking to expand their practice
of their cultural experience, and (3) approaching relation-
domain. Technological methods for delivering assessment
ships from a position of respect and curiosity (Hook et al.,
and therapy services include (1) text-only synchronous or
2013). Clients’ perceptions of their clinician’s cultural
asynchronous communication, (2) voice-only synchro-
humility are associated with the development of
nous or asynchronous communication, and (3) video-link
a working alliance and positive therapy outcomes.
synchronous communication. Overall, researchers have
Cultural humility applies to all clinician–client relation-
reported that telephonic and online assessments are
ships. Clinical interviews inherently place clinicians in an
equal to face-to-face assessment interviewing (Sommers-
expert position and can leave clients feeling leery of clin-
Flanagan & Sommers-Flanagan, 2017). Similarly, non–
ician judgments. To collect valid and reliable information,
face-to-face therapy outcomes are similar to face-to-face
clinicians must create environments where clients feel
outcomes, at least for clients who choose non–face-to-face
welcomed, accepted, and valued no matter what informa-
therapeutic modalities (Hanley & Reynolds, 2009).
tion is shared. Adopting a culturally humble stance can
help clinicians communicate respect to clients.
Information gathered in the clinical interview can drive FUTURE DEVELOPMENTS
psychotherapy and should therefore be gathered in
The clinical interview is a time-honored and flexible pro-
a collaborative and culturally sensitive manner. The tricky
cedure that encompasses mental health assessment and
business of clinical interviewing is to integrate relevant
intervention. Given its traditional status and flexibility of
questions with the core conditions of congruence, uncon-
application, it is doubtful that the future of clinical inter-
ditional positive regard, and empathic understanding
viewing process or content will drastically change.
(Rogers, 1957; Suhr, 2015). These core conditions, parti-
However, for the past several decades, clinical and psycho-
cularly empathic understanding, transcend theory, set-
diagnostic interviewing has consistently, albeit slowly,
ting, and client presenting problems.
evolved and expanded its reach. Specifically, practitioners
who adhere to postmodern psychotherapy models have
used language to transform the form and function of tradi-
Technological Advances in Psychotherapy
tional clinical interviews. These transformations can be
and Clinical Interviewing
captured, in part, with the relabeling of the initial clinical
Clinical interviewing procedures shift and change with interview as an initial therapeutic conversation.
time. Clinical interviewing has flexed and changed in the Additionally, but in the opposite direction, substantial
https://doi.org/10.1017/9781108235433.010 Published online by Cambridge University Press
CLINICAL INTERVIEWING 121
time and energy has been devoted to structuring clinical Green, D., Rosenfeld, B., & Belfi, B. (2013). New and improved?
interviews as a diagnostic procedure; this has involved A comparison of the original and revised versions of the structured
operationalizing and standardizing clinical interviewing interview of reported symptoms. Assessment, 20(2), 210–218.
data collection and interpretation, as well as research Hanley, T., & Reynolds, D. J. (2009). Counselling psychology and
the internet: A review of the quantitative research into online
focusing on methods for discerning when clients are over-
outcomes and alliances within text-based therapy. Counselling
reporting, underreporting, and/or providing inaccurate
Psychology Review, 24(2), 4–13.
assessment information. Finally, clinical interviews have Hays, P. A. (2016). Addressing cultural complexities in practice:
simultaneously evolved in a third direction – toward Assessment, diagnosis, and therapy (3rd ed.). Washington, DC:
greater cultural sensitivity, relevance, and validity. No American Psychological Association.
doubt, these past developments will continue forward Hook, J. N., Davis, D. E., Owen, J., Worthington, E. L., & Utsey, S. O.
but the course and trajectory of clinical interviewing (2013). Cultural humility: Measuring openness to culturally
appears predictable: learning and applying clinical inter- diverse clients. Journal of Counseling Psychology, 60(3), 353–366.
views for assessment and treatment purposes will remain Hormes, J. M., Gerhardstein, K. R., & Griffin, P. T. (2012). Under-
central to the role and function of all mental health reporting of alcohol and substance use versus other psychiatric
professionals. symptoms in individuals living with HIV. AIDS Care, 24(4),
420–423.
Hoyt, M. F. (2000). Some stories are better than others: Doing what
works in brief therapy and managed care. Philadelphia: Brunner/
REFERENCES
Mazel.
American Counseling Association. (2014). The American Jobes, D. A. (2016). Managing suicidal risk: A collaborative approach
Counseling Association code of ethics. Alexandria, VA: Author. (2nd ed.). New York: Guilford Press.
American Psychiatric Association. (1980). Diagnostic and statistical Joiner, T. (2005). Why people die by suicide. Cambridge, MA:
manual of mental disorders (3rd ed.). Washington, DC: Author. Harvard University Press.
American Psychiatric Association. (1994). Diagnostic and statisti- Kroshus, E., Kubzansky, L. D., Goldman, R. E., & Austin, S. B.
cal manual of mental disorders (3rd ed., rev.). Washington, DC: (2015). Norms, athletic identity, and concussion symptom
Author. under-reporting among male collegiate ice hockey players:
American Psychiatric Association. (2013). Diagnostic and statistical A prospective cohort study. Annals of Behavioral Medicine, 49(1),
manual of mental disorders (5th ed.). Washington, DC: Author. 95–103.
APA (American Psychological Association). (2010). Ethical prin- Kutchins, H., & Kirk, S. A. (1997). Making us crazy. New York:
ciples for psychologists and code of conduct. Washington, DC: Free Press.
Author. Large, M. M., & Ryan, C. J. (2014). Suicide risk categorisation of
Bahorik, A. L., Newhill, C. E., Queen, C. C., & Eack, S. M. (2014). psychiatric inpatients: What it might mean and why it is of no
Under-reporting of drug use among individuals with schizo- use. Australasian Psychiatry, 22(4), 390–392.
phrenia: Prevalence and predictors. Psychological Medicine, 44 Lilienfeld, S. O., Smith, S. F., & Watts, A. L. (2013). Issues in diag-
(1), 61–69. nosis: Conceptual issues and controversies. In W. E. Craighead &
Basterra, M. D., Trumbull, E., & Solano-Flores, G. (2011). D. J. Miklowitz (Eds.), Psychopathology: History, diagnosis, and
Cultural validity in assessment: Addressing linguistic and cul- empirical foundations (2nd ed., pp. 1–35). Hoboken, NJ: Wiley.
tural diversity. New York: Routledge. Lobbestael, J., Leurgans, M., & Arntz, A. (2011). Inter‐rater relia-
Edens, J. F., Kelley, S. E., Lilienfeld, S. O., Skeem, J. L., & bility of the structured clinical interview for DSM‐IV axis
Douglas, K. S. (2015). DSM-5 antisocial personality disorder: I disorders (SCID I) and axis II disorders (SCID II). Clinical
Predictive validity in a prison sample. Law and Human Psychology and Psychotherapy, 18(1), 75–79.
Behavior, 39(2), 123–129. Miller, W. R., & Rollnick, S. (2013). Motivational interviewing:
Elkind, D. (1964). Piaget’s semi-clinical interview and the study of Preparing people for change (3rd ed.). New York: Guilford Press.
spontaneous religion. Journal for the Scientific Study of Norcross, J. C., & Lambert, M. J. (2011). Psychotherapy relation-
Religion, 4, 40–47. ships that work II. Psychotherapy: Theory, Research, and
First, M. B., Williams, J. B. W., Karg, R. S., & Spitzer, R. L. (2016). Practice, 48, 4–8.
Structured Clinical Interview for DSM-5 Disorders, clinician version Richman, W. L., Weisband, S., Kiesler, S., & Drasgow, F. (1999). A
(SCID-5-CV). Arlington, VA: American Psychiatric Association. meta-analytic study of social desirability distortion in
Folstein, M. F., Folstein, S. E., & McHugh, P. R. (1975). Mini- computer-administered questionnaires, traditional question-
mental state: A practical method for grading the cognitive state naires, and interviews. Journal of Applied Psychology, 84(5),
of patients for the clinician. Journal of Psychiatric Research, 12 754–775.
(3), 189–198. Rogers, C. R. (1957). The necessary and sufficient conditions of
Frances, A. (2013). Essentials of psychiatric diagnosis: Responding therapeutic personality change. Journal of Consulting
to the challenge of DSM-5 (rev ed.). New York: Guilford Press. Psychology, 21, 95–103.
Ganzini, L., Denneson, L. M., Press, N., Bair, M. J., Helmer, D. A., Rogers, R. (2008). Clinical assessment of malingering and decep-
Poat, J., & Dobscha, S. K. (2013). Trust is the basis for effective tion (3rd ed.). New York: Guilford Press.
suicide risk screening and assessment in veterans. Journal of Rogers, R., Sewell, K. W., & Gillard, N. D. (2010). SIRS-2:
General Internal Medicine, 28(9), 1215–1221. Structured Interview of Reported Symptoms: Professional man-
Green, D., & Rosenfeld, B. (2011). Evaluating the gold standard: ual. Odessa, FL: Psychological Assessment Resources.
A review and meta-analysis of the structured interview of Salamon, S., Santelmann, H., Franklin, J., & Baethge, C. (2018).
reported symptoms. Psychological Assessment, 23(1), 95–107. Test-retest reliability of the diagnosis of schizoaffective
https://doi.org/10.1017/9781108235433.010 Published online by Cambridge University Press
122 JOHN SOMMERS-FLANAGAN, VERONICA I. JOHNSON, AND MAEGAN RIDES AT THE DOOR
disorder in childhood and adolescence: A systematic review and special section on noncredible presentation in ADHD.
meta-analysis. Journal of Affective Disorders, 230, 28–33. Psychological Assessment, 29(12), 1427–1428.
Sellbom, M., & Hopwood, C. J. (2016). Evidence‐based assess- Suhr, J. A., Cook, C., & Morgan, B. (2017). Assessing functional
ment in the 21st century: Comments on the special series impairment in ADHD: Concerns for validity of self-report.
papers. Clinical Psychology: Science and Practice, 23(4), Psychological Injury and Law, 10(2), 151–160.
403–409. Sullivan, B. K., May, K., & Galbally, L. (2007). Symptom exaggera-
Shea, S. C. (1998). Psychiatric interviewing: The art of understand- tion by college adults in attention-deficit hyperactivity disorder
ing (2nd ed.). Philadelphia: Saunders. and learning disorder assessments. Applied Neuropsychology, 14
Solano-Flores, G., & Nelson-Barber, S. (2001). On the cultural (3), 189–207.
validity of science assessments. Journal of Research in Science Tolin, D. F., Gilli Tolin, D. F., Gilliam, C., Wootton, B. M.,
Teaching, 38, 553–573. https://doi.org/10.1002/tea.1018 Bowe, W., Bragdon, L. B. et al. (2018). Psychometric properties
Sommers-Flanagan, J. (2016). Clinical interview. In of a structured diagnostic interview for DSM-5 anxiety, mood,
J. C. Norcross, G. R. VandenBos, & D. K. Freedheim (Eds.), and obsessive-compulsive and related disorders. Assessment, 25
APA handbook of clinical psychology (pp. 3–16). Washington, (1), 3–13.
DC: American Psychological Association. Vannoy, S. D., Andrews, B. K., Atkins, D. C., Dondanville, K. A.,
Sommers-Flanagan, J. (2018). Conversations about suicide: Young-McCaughan, S., & Peterson, A. L. (2017). Under report-
Strategies for detecting and assessing suicide risk. Journal of ing of suicide ideation in US Army population screening: An
Health Service Psychology, 44, 33–45. ongoing challenge. Suicide and Life-Threatening Behavior, 47
Sommers-Flanagan, J., & Sommers-Flanagan, R. (1998). (6), 723–728.
Assessment and diagnosis of conduct disorder. Journal of Welfel, E. R. (2016). Ethics in counseling and psychotherapy:
Counseling and Development, 76, 189–197. Standards, research, and emerging issues (6th ed.). Boston:
Sommers-Flanagan, J., & Sommers-Flanagan, R. (2017). Clinical Cengage.
interviewing (6th ed.). Hoboken, NJ: Wiley. Wiarda, N. R., McMinn, M. R., Peterson, M. A., & Gregor, J. A.
Strub, R. L., & Black, F. W. (1977). The mental status exam in (2014). Use of technology for note taking and therapeutic
neurology. Philadelphia: Davis. alliance. Psychotherapy, 51(3), 443–446.
Sue, D. W., & Sue, D. (2016). Counseling the culturally diverse (7th Widiger, T. A., & Edmundson, M. (2011). Diagnoses, dimensions,
ed.). Hoboken, NJ: Wiley. and DSM-5. In D. H. Barlow (Ed.), The Oxford handbook of
Sue, S. (1998). In search of cultural competence in psychotherapy clinical psychology (pp. 254–278). New York: Oxford
and counseling. American Psychologist, 53(4), 440–448. University Press.
Suhr, J. A. (2015). Psychological assessment: A problem-solving Yalom, I. D. (2002). The gift of therapy. New York: HarperCollins.
approach. New York: Guilford Press. Zander, E., Willfors, C., Berggren, S., Coco, C., Holm, A., Jifält, I.
Suhr, J. A., & Berry, D. T. R. (2017). The importance of assessing et al. (2017). The interrater reliability of the autism diagnostic
for validity of symptom report and performance in attention interview-revised (ADI-R) in clinical settings. Psychopathology,
deficit/hyperactivity disorder (ADHD): Introduction to the 50(3), 219–227.
https://doi.org/10.1017/9781108235433.010 Published online by Cambridge University Press
You might also like
- Self Measures For Love and Compassion Research General Relationship SatisfactionDocument13 pagesSelf Measures For Love and Compassion Research General Relationship SatisfactionQasim AliNo ratings yet
- Assessment of Family Violence - A Handbook For Researchers and Practitioners (2002)Document563 pagesAssessment of Family Violence - A Handbook For Researchers and Practitioners (2002)Erica Oliveira100% (1)
- An Introduction To Theories of Personality 5th Edition by Robert B EwenDocument6 pagesAn Introduction To Theories of Personality 5th Edition by Robert B EwenBaby Glorypath0% (1)
- DSM-5 and Culture - The Need To Move Towards A Shared Model of Care Within A More Equal Patient-Physician PartnershipDocument3 pagesDSM-5 and Culture - The Need To Move Towards A Shared Model of Care Within A More Equal Patient-Physician PartnershipPearl SkyNo ratings yet
- Conners2011 PDFDocument297 pagesConners2011 PDFCristinaNo ratings yet
- Essentials of Neuropsychological Assessment 2ndDocument4 pagesEssentials of Neuropsychological Assessment 2ndRodrigo Caron0% (2)
- Global Assessment FunctioningDocument8 pagesGlobal Assessment Functioningapi-260339450No ratings yet
- Psychological Basis of School PsychologyDocument27 pagesPsychological Basis of School PsychologyVivek RamachandranNo ratings yet
- QS: Social Exchange Theory: FoundersDocument2 pagesQS: Social Exchange Theory: FounderssoulxpressNo ratings yet
- Zech - Alexithymia and Its Measurement Confirmatory Factor Analyses of The Twenty-Item Toronto Alexithymia ScaleDocument38 pagesZech - Alexithymia and Its Measurement Confirmatory Factor Analyses of The Twenty-Item Toronto Alexithymia ScaleGUSREYES69No ratings yet
- Y Bocs Information SampleDocument2 pagesY Bocs Information SampledevNo ratings yet
- Mechanisms of Change in Prolonged Exposure Therapy For PTSD-Implications For Clinical PracticeDocument9 pagesMechanisms of Change in Prolonged Exposure Therapy For PTSD-Implications For Clinical PracticeKelly GCNo ratings yet
- APA DSM 5 Paraphilic DisordersDocument2 pagesAPA DSM 5 Paraphilic DisordersAli FenNo ratings yet
- Psychosocial Dimensions of Displacement: Prevalence of Mental Health Outcomes and Related Stressors Among Idps in IraqDocument34 pagesPsychosocial Dimensions of Displacement: Prevalence of Mental Health Outcomes and Related Stressors Among Idps in IraqSocial InquiryNo ratings yet
- Men, Suicide and SocietyDocument155 pagesMen, Suicide and Societytimaza100% (2)
- Parent Child Bed SharingDocument24 pagesParent Child Bed SharingquinhoxNo ratings yet
- SAS 7 CRI 188 Therapeutic ModalitiesDocument9 pagesSAS 7 CRI 188 Therapeutic ModalitiesKaren Angel AbaoNo ratings yet
- 2001 - Schizophrenia in Children and Adolescents - RemschmidtDocument322 pages2001 - Schizophrenia in Children and Adolescents - RemschmidtvdenkerNo ratings yet
- Whats in The Name AlexithymiaDocument15 pagesWhats in The Name AlexithymiathebeholderNo ratings yet
- KIDDIE Formal Thought Disorder - Caplan1989Document9 pagesKIDDIE Formal Thought Disorder - Caplan1989Rafael MartinsNo ratings yet
- Clinical Intake SummaryDocument9 pagesClinical Intake Summaryvaz21No ratings yet
- Experimental Manipulations of Self-Affirmation REVIEW PDFDocument67 pagesExperimental Manipulations of Self-Affirmation REVIEW PDFAlex RichieNo ratings yet
- Clinical Interview: January 2015Document10 pagesClinical Interview: January 2015KAROL GUISELL PATIÑO ATEHORTUANo ratings yet
- 1 Clinical InterviewDocument14 pages1 Clinical InterviewClara Del Castillo ParísNo ratings yet
- Mueller Segal 2015Document7 pagesMueller Segal 2015Mónica RibeiroNo ratings yet
- Understanding The Assessment of Clinical Reasoning: Omar S. LaynesaDocument20 pagesUnderstanding The Assessment of Clinical Reasoning: Omar S. Laynesaomar laynesaNo ratings yet
- Lesson 1 Clinical PsychologyDocument7 pagesLesson 1 Clinical PsychologyTin EupenaNo ratings yet
- What Is Clinical Psychology?: DefinitionsDocument15 pagesWhat Is Clinical Psychology?: DefinitionsJay Mark CabreraNo ratings yet
- Self CompassionDocument2 pagesSelf CompassionMUSYOKA KITUKUNo ratings yet
- Clinical Psychology at WorkDocument22 pagesClinical Psychology at WorkMark Kenneth NicartNo ratings yet
- Clinical Pre Finals Chapter 11-15Document49 pagesClinical Pre Finals Chapter 11-15justfunkyou1No ratings yet
- Interview Method in AssessmentDocument13 pagesInterview Method in AssessmentAnanya100% (2)
- Research On Psychotherapy Efficacy and EffectivenessDocument18 pagesResearch On Psychotherapy Efficacy and EffectivenesspsicandreiaNo ratings yet
- Getting The Most Out of The Clinical Encounter: The Four Habits ModelDocument10 pagesGetting The Most Out of The Clinical Encounter: The Four Habits Modelliao01No ratings yet
- Clinical Reasoning: Linking Theory To Practice and Practice To TheoryDocument14 pagesClinical Reasoning: Linking Theory To Practice and Practice To Theorylumac1087831No ratings yet
- Clinical Reasoning in Manual TherapyDocument11 pagesClinical Reasoning in Manual TherapyKhushboo PakhraniNo ratings yet
- Clinical Psychology Notes No. 1Document2 pagesClinical Psychology Notes No. 1Jerine Bonus ApostolNo ratings yet
- Clinical Assessment Psychodiagnostic Decision MakingDocument158 pagesClinical Assessment Psychodiagnostic Decision MakingKilana LichterfeldNo ratings yet
- Introduction To Clinical AssessmentDocument13 pagesIntroduction To Clinical AssessmentnurmeenNo ratings yet
- Unit-1 Unit-3 PsychodiadnosisDocument18 pagesUnit-1 Unit-3 PsychodiadnosisOmi PreetamNo ratings yet
- Training Professionals in Motivational InterviewingDocument38 pagesTraining Professionals in Motivational InterviewingMdEssaNo ratings yet
- Van Scoyoc, S. (2017) - The Use and Misuse of Psychometrics in Clinical Settings. in B. Cripps (Ed.)Document17 pagesVan Scoyoc, S. (2017) - The Use and Misuse of Psychometrics in Clinical Settings. in B. Cripps (Ed.)susanvanscoyoc9870No ratings yet
- Documentary of ExplanationDocument17 pagesDocumentary of ExplanationMuhammad Hamza AshfaqNo ratings yet
- Critical Thinking in NursingDocument37 pagesCritical Thinking in NursingAmmar Zaki NabilaNo ratings yet
- Clinical Reasoning in Psychosocial Occupational Therapy - The Evaluation Process. Barris1987Document16 pagesClinical Reasoning in Psychosocial Occupational Therapy - The Evaluation Process. Barris1987saraNo ratings yet
- Approaches To LearningDocument10 pagesApproaches To LearningBulan KakanitaNo ratings yet
- Clinical Assessment - TahiraDocument72 pagesClinical Assessment - TahiraVaneeza AliNo ratings yet
- Understanding and Evaluating QualitativeDocument16 pagesUnderstanding and Evaluating QualitativeSubashni VeeramuthuNo ratings yet
- Mental HealthDocument11 pagesMental Healthmahmoodosman91No ratings yet
- Clinical Assessment Referral, Components, and PurposeDocument53 pagesClinical Assessment Referral, Components, and PurposeBrinda ChughNo ratings yet
- A Scientific Approach To Your Research: Sample Chapter From Conducting Your Pharmacy Practice Research ProjectDocument18 pagesA Scientific Approach To Your Research: Sample Chapter From Conducting Your Pharmacy Practice Research ProjectKrisel IbanezNo ratings yet
- Qualitative Research-Critical Appraisal A Qualitative Study Experiences of Stigma by People With Mental Health ProblemsDocument16 pagesQualitative Research-Critical Appraisal A Qualitative Study Experiences of Stigma by People With Mental Health Problemscaleb mwanziaNo ratings yet
- Clinical ReasoningDocument23 pagesClinical Reasoningathe_triiaNo ratings yet
- What Is Mental Health? Evidence Towards A New Definition From A Mixed Methods Multidisciplinary International SurveyDocument11 pagesWhat Is Mental Health? Evidence Towards A New Definition From A Mixed Methods Multidisciplinary International SurveyBRENNETH CANIBELNo ratings yet
- Case Formulation in PsychotherapyDocument5 pagesCase Formulation in PsychotherapySimona MoscuNo ratings yet
- Clinical Interview PhasesDocument5 pagesClinical Interview Phasesmomina sarwarNo ratings yet
- Tests SsDocument14 pagesTests SsjvtoselaNo ratings yet
- Conducting 2e SampleDocument18 pagesConducting 2e SampleIbn Hamz El-SalamyNo ratings yet
- Assessment of Clinical Reasoning Three EvolutionsDocument6 pagesAssessment of Clinical Reasoning Three EvolutionsFrederico PóvoaNo ratings yet
- Getting The Most Out of The Clinical Encounter: The Four Habits ModelDocument11 pagesGetting The Most Out of The Clinical Encounter: The Four Habits ModelFacu YaneNo ratings yet
- Case Study - IPT For DepressionDocument13 pagesCase Study - IPT For DepressionIsaac FullartonNo ratings yet
- Prevalence and Correlates of Suicide Planning and Attempt Among Individuals With SIDocument8 pagesPrevalence and Correlates of Suicide Planning and Attempt Among Individuals With SIIsaac FullartonNo ratings yet
- Psychologistsas Expert Witnessesin Australian CourtroomsDocument10 pagesPsychologistsas Expert Witnessesin Australian CourtroomsIsaac FullartonNo ratings yet
- Clinical Considerations for a Strength-Based Intake AssessmentDocument12 pagesClinical Considerations for a Strength-Based Intake AssessmentIsaac FullartonNo ratings yet
- Allan 2006 Prediction of The Risk of Male SexuDocument10 pagesAllan 2006 Prediction of The Risk of Male SexuIsaac FullartonNo ratings yet
- 22 Psychol Pub Poly L427Document13 pages22 Psychol Pub Poly L427Isaac FullartonNo ratings yet
- Using family systems, migration histories and acculturation in CBT assessmentDocument21 pagesUsing family systems, migration histories and acculturation in CBT assessmentIsaac FullartonNo ratings yet
- W1 - Why Therapists Should Walk The TalkDocument13 pagesW1 - Why Therapists Should Walk The TalkIsaac FullartonNo ratings yet
- The Mental Status ExaminationDocument7 pagesThe Mental Status Examinationdra.hadleyNo ratings yet
- Vuoskoski Eerola 2011 Music Pers Mood EmotpercDocument8 pagesVuoskoski Eerola 2011 Music Pers Mood EmotpercIsaac FullartonNo ratings yet
- Understanding School Shootings With Crime Script AnalysisDocument14 pagesUnderstanding School Shootings With Crime Script AnalysisIsaac FullartonNo ratings yet
- Depression and Anxiety in High-Achieving Researcher due to Childhood TraumaDocument2 pagesDepression and Anxiety in High-Achieving Researcher due to Childhood TraumaIsaac FullartonNo ratings yet
- The State of Mentoring - Change Agents ReportDocument31 pagesThe State of Mentoring - Change Agents ReportIsaac FullartonNo ratings yet
- Stimulus Set 2Document3 pagesStimulus Set 2Isaac FullartonNo ratings yet
- The Effect of Exercise on Episodic Memory in Individuals With and Without SCDDocument60 pagesThe Effect of Exercise on Episodic Memory in Individuals With and Without SCDIsaac FullartonNo ratings yet
- HUMSS - DIASS12-Ia-1 Aug.24Document3 pagesHUMSS - DIASS12-Ia-1 Aug.24Sharon DannugNo ratings yet
- Critical Reading StrategiesDocument3 pagesCritical Reading StrategiesJoash Charlotte VillanuevaNo ratings yet
- Research Ethic Review Form TemplateDocument7 pagesResearch Ethic Review Form Templatejohnlloydt045No ratings yet
- Acupressure Points For Brain StimulationDocument9 pagesAcupressure Points For Brain Stimulationلوليتا وردةNo ratings yet
- TOEFL Writing SamplesDocument3 pagesTOEFL Writing SamplesMai Hà ThanhNo ratings yet
- Introduction to Assessment in Education: Qualities of a Good Traditional TestDocument24 pagesIntroduction to Assessment in Education: Qualities of a Good Traditional TestHarvagale BlakeNo ratings yet
- 42 Rules For Your New Leadership Role - The Manual They Didn't Hand You When You Made VP, Director, or ManagerDocument136 pages42 Rules For Your New Leadership Role - The Manual They Didn't Hand You When You Made VP, Director, or Managerpntuanhcm100% (1)
- Activity Ac 1Document4 pagesActivity Ac 1faye cuevasNo ratings yet
- Great-Management-Lessons - HTML 1. The Elephant RopeDocument99 pagesGreat-Management-Lessons - HTML 1. The Elephant RopeSathyanarayanan Srinivasan RajappaNo ratings yet
- Five Kinds of Listening PDFDocument4 pagesFive Kinds of Listening PDFAnand MauryaNo ratings yet
- Child Development Theories and StagesDocument18 pagesChild Development Theories and StagesRaffy EsquilloNo ratings yet
- Paranoid Mage - InadvisablyCompelledDocument254 pagesParanoid Mage - InadvisablyCompelledspeedsspiegelNo ratings yet
- How People Lived in the PastDocument4 pagesHow People Lived in the PastTram NguyenNo ratings yet
- ESL Language Test English 2024 01-06-47231Document4 pagesESL Language Test English 2024 01-06-47231louiehernandez11No ratings yet
- Final Exam English 12Document2 pagesFinal Exam English 12api-550115538No ratings yet
- Cool Air by H.P. LovecraftDocument13 pagesCool Air by H.P. LovecraftpattoninplaidNo ratings yet
- Project End 2013-14 EvaluationDocument98 pagesProject End 2013-14 Evaluationhoneysinghuk14% (7)
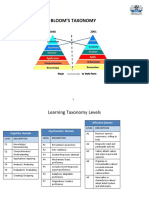
- BloomsTaxonomy SamplesDocument6 pagesBloomsTaxonomy SamplesWan HamizaNo ratings yet
- What Is "Academic" Writing?: by L. Lennie IrvinDocument1 pageWhat Is "Academic" Writing?: by L. Lennie IrvinNeri La LunaNo ratings yet
- Detailed Lesson Plan For English 10Document3 pagesDetailed Lesson Plan For English 10Kristela Tapis ReyesNo ratings yet
- Influencing Factors of Emotional Attachment On Luxury Brands: An Empirical Study in TanzaniaDocument7 pagesInfluencing Factors of Emotional Attachment On Luxury Brands: An Empirical Study in TanzaniaNovelty JournalsNo ratings yet
- What It's Like Being An INTJ Woman Introvert, DearDocument1 pageWhat It's Like Being An INTJ Woman Introvert, DearVaneza PhieterNo ratings yet
- A Practice Theory For Organizational Learning John Shibley PDFDocument6 pagesA Practice Theory For Organizational Learning John Shibley PDFDayana SierraNo ratings yet
- Curriculum EvaluationDocument2 pagesCurriculum Evaluationglenn florNo ratings yet
- JMW PersonaltheoryDocument8 pagesJMW Personaltheoryapi-632123997No ratings yet
- Meskimen Ogl340 Aikidoway ReflectionDocument4 pagesMeskimen Ogl340 Aikidoway Reflectionapi-444454786No ratings yet
- Importance of Travelling Essay: FriendsDocument2 pagesImportance of Travelling Essay: FriendsĐào Trần Nhật AnhNo ratings yet
- A Tale of Three SistersDocument14 pagesA Tale of Three SistersNila AlifahNo ratings yet
- Mariam Mohamed Pema Chunto Making Connections Lab Report TemplateDocument6 pagesMariam Mohamed Pema Chunto Making Connections Lab Report Templateapi-395788256100% (1)
- Senior High School Gretchen S. Osabel: Decoding Watch?V F0Txm-C5Qyy-How H?V Iqsahmtn7N4 - BodyDocument4 pagesSenior High School Gretchen S. Osabel: Decoding Watch?V F0Txm-C5Qyy-How H?V Iqsahmtn7N4 - BodyGretchen SanchezNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (15)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Troubled: A Memoir of Foster Care, Family, and Social ClassFrom EverandTroubled: A Memoir of Foster Care, Family, and Social ClassRating: 4.5 out of 5 stars4.5/5 (25)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeFrom EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeNo ratings yet
- Summary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (11)
- Daniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisFrom EverandDaniel Kahneman's "Thinking Fast and Slow": A Macat AnalysisRating: 3.5 out of 5 stars3.5/5 (130)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (61)