Professional Documents
Culture Documents
SAFEMOB Final18673
Uploaded by
Muhammad FarisOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
SAFEMOB Final18673
Uploaded by
Muhammad FarisCopyright:
Available Formats
SAFE PRESCRIPTION OF MOBILIZING PATIENTS IN ACUTE CARE SETTINGS
WHAT TO ASSESS, WHAT TO MONITOR, WHEN NOT TO MOBILIZE AND HOW TO MOBILIZE AND PROGRESS
PURPOSE, SCOPE & DISCLAIMER: The purpose of this document is to provide physical therapists with guidance on safe mobilization of the patient in acute care settings. This decision-making guide is evidence informed and where there is insufficient evidence, expert
informed. It is not intended to replace the clinician’s clinical reasoning skills and interprofessional collaboration. Mobilization, for the purposes of this document, has been defined as “To work towards the functional task of locomotion”
WHAT TO ASSESS
The chart The patient , family and team member
Medical history. Multisystem review (e.g., cognition, respiratory, cardiac, musculoskeletal & neuro systems)
Premorbid level of function (e.g., mobility aids), activity and exercise response. Level of cooperation.
Primary diagnosis. Ask patient what he/she currently feels about mobilization concerns and readiness.
Medications. Consider the impact of the illness or medical procedures & medications on the patient’s mobility
Investigations, lab work (e.g., Hgb, RBC, Blood sugar, ECG, fluid/electrolytes). (e.g., weakness from disuse, incision, trauma, pain, equipment needs, e.g., walker).
Risk factors and lifestyle conditions. Coordinate with team members the timing of treatment with medication, availability of equipment
Physician orders re specific restrictions on mobilization. and of personnel to optimize effectiveness.
WHEN TO CONSIDER NOT MOBILIZING1-6
*Please note: the cited values are not absolute criteria for withholding mobilization but are within the range of concern that could benefit from team discussion
FiO2: >60% .
5
Cardiovascular status
Mean arterial pressure: <65 or >110 .
1,3 3
Ventilator issues: Decreased ventilatory support that could precipitate fatigue or increased
BP: A drop in systolic pressure (>20 mm Hg) or below pre-exercise level OR a disproportionate ventilatory support.
4
Ventilator asynchrony ; unsecure airway ; pressure control ventilation ; uncontrolled airway
3 3 5
rise i.e., >200 mm Hg for systolic or >110 mm Hg for diastolic .
HR: <40 or >130 ; requiring temporary pacer.
3 3,5
irritability.
Hemodynamic: Administration of a new pressor e.g., inotropes agent ; two or more pressor or Uncontrolled asthma.
1
5 3,5
frequent increase ; uncontrolled systemic hypertension; active bleeding.
Acute or unstable cardiac status: New MI ; dysrhythmia requiring new medications ; active
1 1 Neurological status
Patient status: Severe agitation, distress, or combative ; not able to understand instructions
3 5 5 2,3
cardiac ischemia ; unstable rhythm ; intra aortic balloon.
Pulmonary embolus: Discussion with physician required to determine suitability. thus risking patient or therapist safety.
ICP: Increased i.e., >20 mm Hg, however, ICP needs to be considered in conjunction with
3
Deep venous thrombosis: May mobilize as tolerated immediately after low molecular weight
heparin (e.g., enoxaparin (lovenox®), dalteparin (fragmin®), tinzaparin (innohep®), nadroparin cerebral compliance.
Uncleared, unstable/non fixated spinal cord injury or head injury.
5
(fraxiparine®)) is given. If patient is on any other form of anticoagulation (e.g., IV heparin) please
check mobility orders with the physician. Monitor patient for changes in pain, swelling, colour and
sudden shortness of breath.
6 Other
Intermittent hemodialysis .
3
Respiratory Status Unstable fracture.
SpO2: <88% or undetermined cyanosis.
1,3
Excessive muscle soreness or fatigue that is residual from last exercise or activity session.
RR: <5 or >40 .
3
Other contraindications specific to a given setting/unit.
WHAT TO MONITOR DURING MOBILIZATION
Subjective: Dizziness, vertigo, shortness of breath, fatigue, nausea, pain *consider use of scales e.g., Borg scale of perceived exertion.
Objective: Cognition, balance, perspiration, cyanosis, heart rate, oxygen saturation, respiratory rate and blood pressure and all other factors relevant to patient and mobility task, for example, cardiac
rhythm in those patients when ECG is essential during mobilization.
HOW TO MOBILIZE AND PROGRESS7
Step 1 Prepare If postural hypotension is suspected, monitor BP and ask patient about lightheadedness at each
Note obstacles or challenges related to the patient and environment and plan appropriately phase of the mobilization i.e., sitting on edge of bed, standing, walking a few paces.
(e.g., set up equipment – chairs, transfer belt, mobility aids, length of leads/lines).
Determine whether the benefits outweigh the risk. Step 3 When to quit while you are still ahead
Ensure pre-medication as indicated (analgesia, bronchodilators, oxygen). Monitor closely. Watch for signs of fatigue, pain, diaphoresis and intolerance during activity.
Obtain baseline vital signs (heart rate, blood pressure, oxygen saturation). Frequently ask patient how he/she feels.
Have objective end-points such as limits of blood pressure, heart rate, oxygen saturation and Evaluate patient’s status at each progression to determine whether to continue or stop.
level of exertion pre-determined before mobilization. Step 4 Monitor and progress
Determine the limiting factor of the mobilization and any undesirable response(s).
Step 2 Safety first
Use objective outcome measures to monitor progress e.g., ease of transfer, sitting duration,
Use proper body mechanics during transfer and allow gradual change from lying to upright
walking distance, HR, RR, oxygen saturation, Borg scales, and pain scales.
position. Encourage circulation exercises i.e., foot and ankle, knee flexion/extension before
After mobilization, monitor patient until vital signs have returned to pre-activity level.
commencing more demanding mobilization procedures.
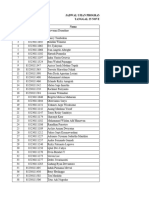
HOW TO PROGRESS1,3,8-13 *
Continue to monitor vitals to guide progression*
LEVEL (Morris )
1
LEVEL I LEVEL II LEVEL III LEVEL IV
TARGET LEVEL OF
14 RASS -5 to -2 RASS -2 to -1 RASS -1 to +1 RASS -1 to +1
CONSCIOUS (RASS)
STRENGTH CRITERIA FOR
Able to move arm vs. gravity. Able to move arm and leg vs. gravity.
ENTERING THIS LEVEL
Q2H Q2H Q2H Q2H
TURNING Patient to assist as able. Same as Level I, plus: Gradual withdrawal of assistance. Focus on training to promote patient’s
AND BED MOBILITY Scooting/bridging Initiation of training to promote patient’s independence.
Supine sitting. independence.
Keep HOB >30o. Same as Level I. Same as Level I. Assess for seating Same as Level III.
Apply splints, other positioning devices needs.
POSITIONING
as per OT/PT instructions.
AND DEVICES
Focusing on preventing pressure
ulcers, especially on heels and sacrum.
PROM ex to incorporate into patient Encourage pt assist with ROM during Same as Level II with more active Same as Level III.
care e.g., during washing, turns. patient care e.g., during washing, involvement.
turns.
Consider inclusion of: Same as Level II with more active Same as Level III with more active
Breathing exercises. involvement. involvement.
EXERCISE PROGRAM
Stretching exercises. Consider inclusion of: Consider inclusion of:
Balance/coordination exercises for Arm ergometry. Weight bearing/ weight shifting
head, neck, and trunk. exercises.
Additional exercise/mobilization as per Same as Level I. Same as Level I. Same as Level I.
physio assessment.
HOB >45° x 30-60 minutes BID, support High fowlers or cardiac chair position Assist physio with dangle on side of If dangle and stand at bedside
to achieve midline head and trunk x 30-60 minutes TID. bed. May need ceiling lift if patient successful, physio assesses ability to
position. heavy. weight shift, ability to transfer to chair.
Sitting balance exercises with physio as Initial time in chair 30 minutes, progress
appropriate, 5 to 10 minutes to start. per OT/PT assessment.
Initially OD, progress to BID as patient Initially OD, progress to BID as patient
MOBILIZATION tolerates. tolerates.
Mobilization may include* tilt table, As per physio assessment of patient If patient able to transfer to chair,
dangle or to chair with mechanical lift strength, assist physio with sit to stand, tolerates well, physio assesses
prn. walking in place; +/- walker. ambulation, begins walking practice
Patients with neuro/ortho status with appropriate aids, increasing
*Use caution for patients at risk of precluding WB require individualized distance and frequency as patient
hypotension. mobilization prescription. tolerates.
14
References
Richmond Agitation Sedation Scale (RASS) :
1. Morris PE, Goad A, Thompson C, Taylor K, Harry B, Passmore L et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Critical Care Medicine,
+4 Combative; violent, immediate danger to staff 2008; 36:2238-43.
+3 Very agitated; pulls or removes tubes/lines; aggressive 2. Stiller, K. Safety issues that should be considered when mobilizing critically ill patients. Crit Care Clin 2007; 23, 35-53.
3. Schweickert WD, Pohlman MC, Pohlman NS Nigos C, Pawlik AJ, Esbrook CL et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: an RCT.
+2 Agitated; frequent non-purposeful movement, fights ventilator
Lancet. 2009; 373:1874-82.
+1 Restless; anxious but movement not aggressive or vigorous 4. ACSM Guidelines for Exercise Testing and Prescription. 8th edition. Lippincott Williams & Wilkins. Philadelphia 2010 pp.209-10.
0 Alert and Calm 5. Timmerman, RA. A mobility protocol for critically ill adults. [DIMENS CRIT CARE NURS. 2007; 26(5):175-9.
-1 Drowsy; not fully alert, sustained wakening (eye-opening/contact) to voice 6. Singh C, Fletcher R, Cunningham K, and Szlivka M. Mobilization with a Deep Vein Thrombosis. Clinical Practice Guideline (DRAFT in process). Fraser Health Authority. 2009.
>10 sec 7. Reid WD, Chung F. Clinical management notes and case histories in cardiopulmonary physical therapy. New Jersey: Slack; 2004.
-2 Light sedation; briefly awakens with eye contact to voice < 10 sec 8. Chung F, Fletcher R, Lavoie K, Parrent L, Perret D, Roy L, Urbina,M. Members of the physiotherapy professional practice council critical care practice stream for the Fraser Health
Authority. Canada. Forthcoming. 2009.
-3 Moderate sedation; Movement or eye opening to voice but no eye contact
9. Bailey P, Thomsen GE, Spuhler VJ, Blair R, Jewkes J, Bezdjian L, et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med. 2007; 35:139-45.
-4 Deep sedation; No response to voice but movement or eye opening to 10. Collard HR, Saint S, Matthay MA. Prevention of ventilator-associated pneumonia: an evidence-based systematic review. Ann Intern Med. 2003;138:494-501.
physical stimulation 11. Dodek P, Keenan S, Cook D, MD, Heyland D, Jacka M, Hand L et al. Evidence-based clinical practice guideline for the prevention of ventilator associated pneumonia. Ann Intern
-5 Unarousable; No response to voice or physical stimulation Med. 2004; 141:305-13.
12. Needham D. Mobilizing patients in the intensive care unit: improving neuromuscular weakness and physical function. JAMA. 2008; 300:1685-90.
13. Perme C, Chandrashekar R. Early mobility and walking program for patients in intensive care units: creating a standard of care. Am J Crit Care. 2009; 18:212-21.
Developed by the SAFEMOB Task Force: Dr. Elizabeth Dean, Dr. Darlene Reid, Frank Chung,
14. Sessler CN, Gosnell M, Grap MJ, Brophy GT, O'Neal PV, Keane KA et al. The Richmond Agitation-Sedation Scale: validity and reliability. Am J Respir Crit Care Med 2002;
Simone Gruenig, Rosalyn Jones, Jocelyn Ross, Maylinda Urbina, Alison Hoens.
166:1338-44.
You might also like
- Lab Act 2 SensoryDocument5 pagesLab Act 2 SensoryZgama AbdulrahmanNo ratings yet
- Modified Jobe Versus Docking Technique For Elbow Ulnar Collateral Ligament ReconstructionDocument13 pagesModified Jobe Versus Docking Technique For Elbow Ulnar Collateral Ligament ReconstructionLuisFernandoDelRíoEspinozaNo ratings yet
- The Fim Instrument: Its Background, Structure, and UsefulnessDocument31 pagesThe Fim Instrument: Its Background, Structure, and UsefulnesssamiratumananNo ratings yet
- Effect of Dry-Needling and Exercise Treatment On Myofascial Trigger PointDocument7 pagesEffect of Dry-Needling and Exercise Treatment On Myofascial Trigger PointDavid ElirazNo ratings yet
- Abstracts From The Global Embolization Sympo 2021 Journal of Vascular and inDocument21 pagesAbstracts From The Global Embolization Sympo 2021 Journal of Vascular and infreedy freedyNo ratings yet
- Brochure The MS Disease Modifying MedicationsDocument16 pagesBrochure The MS Disease Modifying MedicationsBarath R BaskaranNo ratings yet
- Stunting DR AmanDocument63 pagesStunting DR AmantotoksaptantoNo ratings yet
- Key Changes Gold 2023Document15 pagesKey Changes Gold 2023joao cNo ratings yet
- Tennis Elbow - StatPearls - NCBI BookshelfDocument9 pagesTennis Elbow - StatPearls - NCBI BookshelfADITYA ARI HERLAMBANGNo ratings yet
- Jadwal-Ujian-Tpa-Program-Spesialis-Pascasarjana-Sesi-IDocument32 pagesJadwal-Ujian-Tpa-Program-Spesialis-Pascasarjana-Sesi-IAndrio PalayukanNo ratings yet
- ENLS Meningitis and Encephalitis ProtocolDocument20 pagesENLS Meningitis and Encephalitis ProtocolFransiskus MikaelNo ratings yet
- Lidocain and BuvipacainDocument6 pagesLidocain and BuvipacaintinahermantoNo ratings yet
- Dokumen Pengujian Tera HertzDocument57 pagesDokumen Pengujian Tera HertzAhmad HariyantoNo ratings yet
- Fluid ResponsivenessDocument70 pagesFluid Responsivenessrina febriatiNo ratings yet
- 2013 Urology CatalogDocument233 pages2013 Urology CatalogAna LauraNo ratings yet
- Checklist Blood Culture NZZ - EditDocument10 pagesChecklist Blood Culture NZZ - EditJaaydevNo ratings yet
- Sun Pharma AR 2021 22Document324 pagesSun Pharma AR 2021 22Dushyant PratapNo ratings yet
- Case Report - Fungus BallDocument13 pagesCase Report - Fungus BallAdrian ErindraNo ratings yet
- Neurology 4 PDF-mergedDocument358 pagesNeurology 4 PDF-mergedAnuraag YadavNo ratings yet
- Nippv Revisi Final Picu Nicu MaretDocument51 pagesNippv Revisi Final Picu Nicu MaretJulian Ammar Zaidan GunawanNo ratings yet
- Tele Rehabilitation Service Delivery Journey From Prototype To Robust in Home Use D and R OnlineDocument10 pagesTele Rehabilitation Service Delivery Journey From Prototype To Robust in Home Use D and R OnlineFelipe Palma UrrutiaNo ratings yet
- List of Empanelled Hospitals/Diagnostic Centres, and Cghs RatesDocument2 pagesList of Empanelled Hospitals/Diagnostic Centres, and Cghs RatesBabita KumariNo ratings yet
- PIVDDocument18 pagesPIVDAayushi SrivastavaNo ratings yet
- Chest Trauma: Annet Mary Mathew Anu Krishna Arathi.KDocument60 pagesChest Trauma: Annet Mary Mathew Anu Krishna Arathi.KAsif AbbasNo ratings yet
- AbbreviationDocument90 pagesAbbreviationIrwanshah MohammadNo ratings yet
- Determination of Brain Death: Clinical PracticeDocument8 pagesDetermination of Brain Death: Clinical PracticeAlexander Pabon Moreno100% (1)
- ITU Handbook For Non-Anaesthetists 214Document23 pagesITU Handbook For Non-Anaesthetists 214AtikaNo ratings yet
- Health Assessment Proforma of School StudentsDocument4 pagesHealth Assessment Proforma of School StudentsMantu Roy100% (1)
- Early Recognition Critical Illness by Scoring System & Case ExampleDocument17 pagesEarly Recognition Critical Illness by Scoring System & Case ExampleRyan GusnaintinNo ratings yet
- Cardio Pulmonary Master Document Google DocsDocument186 pagesCardio Pulmonary Master Document Google DocsGokulakrishnan KrishnanNo ratings yet
- AttachmentDocument2 pagesAttachmentRoni Sartika TampubolonNo ratings yet
- Meningitis - 2018Document55 pagesMeningitis - 2018Abraham Anaely100% (1)
- Multimodal Analgesia A CL 2022Document14 pagesMultimodal Analgesia A CL 2022Alejandra SanchezNo ratings yet
- Master ObatDocument319 pagesMaster ObatsoniaZDNo ratings yet
- Medel SonataDocument54 pagesMedel Sonatamaclab macNo ratings yet
- Physiotherapist ScopesDocument79 pagesPhysiotherapist ScopesSujin StephenNo ratings yet
- Galeazzi-Fracture 6Document14 pagesGaleazzi-Fracture 6MIGUEL ANGEL MEJIA FERNANDEZNo ratings yet
- ENLS Sub-Arachnoid Hemorrhage ProtocolDocument22 pagesENLS Sub-Arachnoid Hemorrhage ProtocolFransiskus MikaelNo ratings yet
- Important QuestionsDocument11 pagesImportant QuestionsRajan JattNo ratings yet
- Lumbarspinalstenosisin Olderadults: Anna M. Lafian,, Karina D. TorralbaDocument12 pagesLumbarspinalstenosisin Olderadults: Anna M. Lafian,, Karina D. TorralbaIhsan KNo ratings yet
- Report ViewerDocument1 pageReport ViewerZeeshan JunejoNo ratings yet
- Transverse Myelitis: A Guide For Patients and CarersDocument36 pagesTransverse Myelitis: A Guide For Patients and CarersMartina Acosta RamaNo ratings yet
- Coronary Chronic Total Occlusion CTO A ReviewDocument8 pagesCoronary Chronic Total Occlusion CTO A ReviewcNo ratings yet
- Mindray iMEC12 SpecsDocument6 pagesMindray iMEC12 SpecsJose Ivan Carvajal CortizosNo ratings yet
- Abstract Dexmed Vs Lignocaine Final Abstract and ArticleDocument25 pagesAbstract Dexmed Vs Lignocaine Final Abstract and ArticleDr.S.Easwaramoorthy IAGES Secretary 2020No ratings yet
- Presentation On GangreneDocument24 pagesPresentation On GangreneAmrutha KappatrallaNo ratings yet
- CP100MEDICALtermPSAbbr. 2Document78 pagesCP100MEDICALtermPSAbbr. 2RAISA N. RASIDNo ratings yet
- CORONARY ARTERY BYPASS GRAFT Nurse CareDocument32 pagesCORONARY ARTERY BYPASS GRAFT Nurse CareCharisma Bailey Doody100% (1)
- 3 - Right Heart AssessmentDocument47 pages3 - Right Heart Assessmentpatricia wageyNo ratings yet
- Slide - PrecedexDocument47 pagesSlide - PrecedexHendi PrihatnaNo ratings yet
- PennDot ADA Pocket GuideDocument57 pagesPennDot ADA Pocket GuideChad DavenportNo ratings yet
- Diagnosis Dan Tatalaksana Dislokasi Lensa Intraokular Ke Posterior Dengan Prosedur IOL Exchange To Iris Claw Retropupillary - Siti AisyahDocument13 pagesDiagnosis Dan Tatalaksana Dislokasi Lensa Intraokular Ke Posterior Dengan Prosedur IOL Exchange To Iris Claw Retropupillary - Siti Aisyahmemmuse95No ratings yet
- Curriculum Vitae Curriculum VitaeDocument46 pagesCurriculum Vitae Curriculum VitaeJuwita PratiwiNo ratings yet
- Cardio Respiratory Asessment For PhysiotDocument10 pagesCardio Respiratory Asessment For PhysiotJayden HiiNo ratings yet
- Healthy Start, Grow Smart Series - 02 - Two MonthDocument15 pagesHealthy Start, Grow Smart Series - 02 - Two MonthMihaelaPantaNo ratings yet
- Neurologic Disorder FinalDocument9 pagesNeurologic Disorder FinalMary Reigns BuhatNo ratings yet
- Choice of Surgical Methods in Patients With Urinary Stone DiseaseDocument6 pagesChoice of Surgical Methods in Patients With Urinary Stone DiseaseCentral Asian StudiesNo ratings yet
- Case Study: Congestive Heart Failure By: Daniel Angelo E. ArangoDocument7 pagesCase Study: Congestive Heart Failure By: Daniel Angelo E. ArangoDaniel Angelo ArangoNo ratings yet
- History Taking and PF CVD Iman Evan Final Fix - Dr. M Yusak SPJPDocument84 pagesHistory Taking and PF CVD Iman Evan Final Fix - Dr. M Yusak SPJPFikriYTNo ratings yet
- Nanda NCP BasedDocument14 pagesNanda NCP Baseddeliejoyce100% (1)
- Biology of Domestic Animals PDFDocument371 pagesBiology of Domestic Animals PDFfeketerigo67% (3)
- Normal Vital Signs Guidelines For EmsDocument2 pagesNormal Vital Signs Guidelines For Emsisabelo_laguraNo ratings yet
- Assessment - Blood PressureDocument3 pagesAssessment - Blood PressuremArLoNNo ratings yet
- Advanced Pm2000b Monitor SERVICE MANUALDocument55 pagesAdvanced Pm2000b Monitor SERVICE MANUALNur Adam Abd RahmanNo ratings yet
- Toefl Test: (Section 3. Reading Comprehension)Document4 pagesToefl Test: (Section 3. Reading Comprehension)Weka patrianaNo ratings yet
- Pulmonary Vascular Resistance (PVR)Document11 pagesPulmonary Vascular Resistance (PVR)Dermatologi FkunsNo ratings yet
- Jurnal 1 HipertensiDocument7 pagesJurnal 1 Hipertensidinarikasari baskaraNo ratings yet
- Measurements To Guide Your Patient Care: EfficiaDocument16 pagesMeasurements To Guide Your Patient Care: EfficiaXinwen ChenNo ratings yet
- Acute Heart Failure WORKBOOKDocument28 pagesAcute Heart Failure WORKBOOKFadhlan ABNo ratings yet
- Question BankDocument6 pagesQuestion Bankkoang lual gachNo ratings yet
- n360 Concept Map Care Plan Week 3 Sheryl SatoDocument15 pagesn360 Concept Map Care Plan Week 3 Sheryl Satoapi-283363983No ratings yet
- Lipids in Health and Disease: Amaranth Oil Application For Coronary Heart Disease and HypertensionDocument12 pagesLipids in Health and Disease: Amaranth Oil Application For Coronary Heart Disease and HypertensionvitorNo ratings yet
- Risk For Decreased Cardiac Output: Nursing DiagnosisDocument4 pagesRisk For Decreased Cardiac Output: Nursing DiagnosisRiska RamadaniNo ratings yet
- SAMPLE FDAR CHARTING PainDocument1 pageSAMPLE FDAR CHARTING PainjpmNo ratings yet
- Transfusion-Associated Circulatory Overload (TACO) Draft Revised Reporting CriteriaDocument4 pagesTransfusion-Associated Circulatory Overload (TACO) Draft Revised Reporting CriteriaAarón LinaresNo ratings yet
- StudyDocument23 pagesStudyJose Paul RaderNo ratings yet
- What Are The Benefits of GarlicDocument7 pagesWhat Are The Benefits of GarlicBellia AyudiaNo ratings yet
- Does Obesity Influence Early Target Organ Damage in Hypertensive PatientsDocument8 pagesDoes Obesity Influence Early Target Organ Damage in Hypertensive PatientsHenri TantyokoNo ratings yet
- EUROSCOREIIDocument3 pagesEUROSCOREIIFabiánBejaranoLeónNo ratings yet
- Haad Mle FundaDocument20 pagesHaad Mle FundaGreggy Francisco LaraNo ratings yet
- Metarminol and Its Role in EDDocument2 pagesMetarminol and Its Role in EDbharatNo ratings yet
- Anaphy - Lesson 4 - Topic 4 and 5Document21 pagesAnaphy - Lesson 4 - Topic 4 and 5Rica Abigail DagosNo ratings yet
- Nursing Management of Patient With CCFDocument34 pagesNursing Management of Patient With CCFJayarani Ashok100% (1)
- ASCIA HP Guidelines Acute Management Anaphylaxis 2020Document8 pagesASCIA HP Guidelines Acute Management Anaphylaxis 2020Munshi KamrulNo ratings yet
- Biology 11 - Cardiovascular System True/False Intro Activity (With Answers)Document2 pagesBiology 11 - Cardiovascular System True/False Intro Activity (With Answers)ascd_msvuNo ratings yet
- Garam LososaDocument8 pagesGaram LososaHamiidah InNo ratings yet
- WelchAllyn Vital Signs - User ManualDocument106 pagesWelchAllyn Vital Signs - User Manualhassan niazyNo ratings yet
- Liquid Restriction For Patients With Chronic Kidney Disease To Prevent The Risk of Fluid OverloadDocument9 pagesLiquid Restriction For Patients With Chronic Kidney Disease To Prevent The Risk of Fluid OverloadaisyahNo ratings yet
- Police Personnel ManagementDocument22 pagesPolice Personnel ManagementApple Del RosarioNo ratings yet
- Chucks Drug BoxDocument2 pagesChucks Drug BoxKara Dawn MasonNo ratings yet