Professional Documents
Culture Documents
Family Nursing Process
Uploaded by
RANDY ERNEST GESTOSANI0 ratings0% found this document useful (0 votes)
21 views9 pagesOriginal Title
FAMILY NURSING PROCESS
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
21 views9 pagesFamily Nursing Process
Uploaded by
RANDY ERNEST GESTOSANICopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 9
FAMILY NURSING PROCESS
Community Health Nursing | Glenda Fronteras | BSN 2P
Objectives: C. conditions in the home and
1. Define the family nursing process environment
2. Determine the steps for Assessment Physical Examination
3. Distinguish First Level Assessment from Second o Significant data about the health
Level Assessment status of the individual members can
4. Identify Health Problems of a Family be obtained through direct
5. Interpret data related to the identified health examination through IPPA
condition o Measurement of specific body parts
6. Formulate a plan of care to address the health and reviewing the body systems
o Data gathering from PE form
conditions, needs, problems, and issues based
substantial first level assessment
on priorities
which may indicate the presence of
7. Determine Barriers to Joint Setting of Goals
health deficits (illness status)
Interview
Definition o Productivity of interview process
Family Nursing Process depends upon the use of effective
o The blueprint in the care that the nurse communication techniques to elicit
design to systematically minimize or needed response of PROBLEMS
eliminate the identified health and family ENCOUNTERED
nursing problems through explicitly Records Review
formulated outcomes of care (goals and o E.g. laboratory or diagnostic tests?
objectives) and deliberately chosen set o Gather information through reviewing
of interventions, resources, and existing records and reports
evaluation criteria, standards and tools. pertinent to the client
o A systematic approach of solving an o Individual clinical records of the family
existing problem/meeting the needs of member, laboratory and diagnostic
family records, immunization records
report about house and
environmental condition
FAMILY NURSING PROCESS
Mnemonic: RAPIE
TYPOLOGY OF NURSING PROBLEM
1. RAPPORT
FIRST LEVEL ASSESSMENT
o Trust building
o To determine problems of family
o Knowing your client o Sources or Problems using IDB
o Adjusting to the situation and o Family: use of Initial Data Base (IDB)
environment o Nature: Health Deficit (HD), Health
o RESPECT Threat (HT), Foreseeable Crisis (FC)
2. ASSESSMENT SECOND LEVEL ASSESSMENT
o First major phase of nursing process o Defines the nature or type of
o Involves a set of action by which the nursing problem that family
nurse measures the status of the encounters in performing health
family as a client. Its ability to maintain task with respect to given health
wellness, prevent, control or resolve condition or problem and etiology or
problems in order to achieve health and barriers to the family’s assumption of
task
wellness among its members
o Data about present condition or status
FAMILY HEALTH ASSESSMENT: Tools for
of the family are compared against the
Assessment
norms and standards of personal,
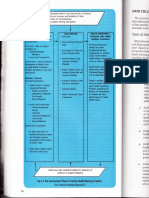
Initial Data Base (IDB)
social, and environmental health,
o Family structure characteristics and
system integrity and ability to resolve
social problems dynamics
o The norms and standards are derived Members of the household and
relationship to the head of the
from values, beliefs, principles, rules
family
or expectation
Demographic data-age, sex,
DATA COLLECTION METHODS
civil status, position in the family
Observation
Place of residence of each
o The family’s health status can be
member – whether living with
inferred from the s/sx of problem
areas the family or elsewhere
A. communication and Type of family structure – e.g.
interaction patterns patriarchal, matriarchal, nuclear
expected, used, and tolerated or extended
by family members Dominant family members in
B. role perception/task terms of decision making
assumption by each especially on matters of health
member including decision care
making patterns
General family Formula:
relationship/dynamics – TFA (in sqm) = Length of the house x
presence of any obvious/readily width of the house
observable conflict between TSR = number of household members x
members; characteristics, corresponding space required for that
communication / interaction member
patterns among members
Consider:
o Socio-economic and cultural factors Adults (13 y/o and above ) = 15 sqm
Income and expenses Children (1 y/o to 12 y/o) = 8 sqm
Infants (below 12 months) = 0 sqm
Occupation, place of
work and income of
Compare the TFA (total floor area) with the TSR
each working member
(total space requirement)
Adequacy to meet basic
necessities (food, Crowded if: TFA < TSR
clothing, shelter) Not Crowded if: TFA > TSR
Who makes decision
about money and how it Example:
is spent TFA = 21 sqm
Educational Attainment of each TSR = 2(15) + 3(8)
member =30+24
Ethnic background and =54
Religious Affiliation
Significant others – role(s) they 21 < 54
play in family’s life TFA < TSR
Relationship of the family to
larger community – nature and Interpretation: TFA <TSR (crowded)
extent of participation of the
family in community activities TYPES OF MATERIAL USED FOR HOUSE
Light
o Home and environment factors Refers to such materials as bamboo, nipa,
Information on housing and sawali, coconut leaves, or card board
sanitation facilities, kind of
neighborhood and availability of Strong
social, health, communication Refers to predominantly concrete house
and transportation facilities
Housing Mixed
Adequacy of living Refers to a combination of light materials
space wood and/or concrete
Typically concrete floor and foundation and
Sleeping in
light walls or a concrete 1st floor and a light 2nd
arrangement
floor
Presence of breathing
or resting sites of vector LIGHT FACILITIES
of diseases (e.g. Artificial means of providing light/illumination
mosquitoes, roaches,
Facilities used already reflect adequacy and
flies, rodents etc.)
safety for the family
Presence of accident
Example: electricity, kerosene, candles or none
hazard
Food storage and
APPROVED TYPE OF WATER FACILITIES
cooking facilities
o Level I (Point Source)
Water supply – source,
A protected well or a developed
ownership, pot ability
spring with an outlet but without
Toilet facilities – type, a distribution system
ownership, sanitary Indicated for rural areas where
condition houses are scattered
Garbage/refuse Serves 15-25 household; its
disposal – type, sanitary outreach is not more than 250m
condition from the farthest user
Drainage system – type, Yields 40-140 L/m
sanitary condition o Level II (Communal Faucets or Stand
Kind of neighborhood, e.g., Posts)
congested, slum etc. With a source, reservoir, piped
Social and Health facilities distribution network and
available communal faucets
Communication and Located at not more than 25m
transportation facilities available from the farthest house
ADEQUACY OF LIVING SPACE
Delivers 40-80L of water per feet) but relatively
capital per day to an average of narrow (less than 2
100 households meters in diameter) hole
Serves 4-6 household per made with boring
faucet equipment
Fit for rural areas where houses Overhung Latrine
are densely clustered Toilet house is
o Level III (Individual House constructed over a body
Connections or Waterworks System) of water (stream, lake,
With a source, reservoir, piped and river) into which
distribution network and excreta is allowed to fall
household taps freely
One or more faucets per Level II
household o On site toilet facilities of the water
Fit for densely populated urban carriage type with water-sealed and
communities flush type with septic vault/tank disposal
o Flush Type
TYPE OF EXCRETA DISPOSAL A toilet system where waste is
Level I disposed by flushing water
o Non water carriage toilet facility through the pipes (sewers) into
No water necessary to flush the the public sewerage system or
waste into the receiving space into an individual disposal
Example: pit latrines, bored-hole system like an individual septic
latrines tank
o Toilet facilities requiring small amount of o Water Sealed Latrine
water to wash the waste into the An Antipolo type of toilet, bored-
receiving space holed latrine, or any pit privy
Example: pour flush toilet and wherein water sealed toilet bowl
aqua privies is placed instead of the simple
o Pail System platform hole (+) septic tank
A pail or box is used to receive Level III
excreta and dispose later when o Water carriage types of toilet facilities
filled connected to septic tanks and/or
Include ballot system where in sewerage system to treatment plant
excreta is wrapped in a piece of
paper/plastic and thrown later SEWERAGE SYSTEM
o Open Pit Privy/Latrine Blind Drainage
Consist of a pit covered with a o Waste water flows through a system of
platform with a hole and is closed pipes to an underground pit or
usually not covered covered canal
The platform may, in its simplest Open drainage
form, consist only of 2 pieces of o Waste water flows through a system of
wood or bamboo pipes (could be improvised from
o Closed Pit Privy/Latrine bamboo) to an open pit canal
A pit privy in which the hole over None
the platform is provided with a o When no drainage system or container
cover used for garbage. Waste water from the
o Type of pit include: kitchen flows directly to the ground,
Ventilated improved pit (VIP) oftentimes forming a nearly permanent
Pit with a vent pipe pool. Garbage is not put in a container
Reed Odorless Earth Closet when disposed.
(ROEC)
A pit completely TYPES OF WASTE DISPOSAL
displaced from the Hog feeding
superstructure and o Garbage is used as hog feed and also
connect to the squatting to chicken and other livestock
plate by a curved chute Open Dumping
Antipolo Type o Refuse and/or garbage piled in a
Toilet house is elevated dumping place (with or without pit) with
and the shallow pit is no soil covering
extended upwards to
Open burning
the platform (toilet floor)
o Regularly piles refused/garbage and
by means of a chute or
later burned in open air. This is
pipe made of metal,
uncontrolled burning which is usually
clay, aluminum or board
done for yard and street sweeping. It
Bored-Hole Latrine
may be allowed in rural areas where it
Toilet consist of a deep
will not worsen already existing air
(usually more than 10
pollution
Burial pit and contributing modifiable risk
o Refuse/garbage places in a pit and factors for specific lifestyle
covered when filled up. There is no diseases
intention to dig it up later for use as Hypertension, physical
fertilizer. This should be located 25 inactivity, sedentary
METERS AWAY from any well used for lifestyle,
water supply. cigarette/tobacco
Composting smoking, elevated blood
o Involved buying or stacking of lipids/cholesterol,
alternating layers of organic based obesity, diabetes
refuse/garbage and treated soil mellitus, inadequate
arranged as to hasted rapid decay and fiber intake, stress,
decomposition into compost. alcohol drinking, and
o This organic mixture can be later be other substance abuse
used as fertilizer Physical assessment indicating
Garbage collection presence of illness state/s
o Refuse/garbage collected by truck and (diagnosed or undiagnosed by
medical practitioners)
any type of garbage collected in the
Results of laboratory/diagnostic
community
and other screening procedure
supportive of assessment
findings
o Health assessment of each member
Medical nursing history
o Value placed on prevention of
indicating current or past
significant illnesses or beliefs disease (Values health practices on
and practices conducive to health promotion, maintenance and
health and illness disease prevention)
Nutritional assessment Immunization status of family
(especially for vulnerable or at members
risk members) Healthy lifestyle practices
Specify adequacy of:
Anthropometric data:
measures of nutritional Rest and sleep
status of children Exercise/activities
Weight, height, mid- Use of protective
upper arm measure
circumference; E.g. adequate footwear
Risk assessment in parasite-infested
measures for obesity areas; use of bed nets
o BMI and protective clothing
o Waist in malaria and filariasis
endemic areas
circumference
(WC: >90 cm in Relaxation and other
men and >80 stress management
cm in women) activities
o Waist hip ratio Use of promotive-preventive
health services
(WHR = waist
circumference
in cm / hip
TOOLS USE IN FAMILY HEALTH ASSESSMENT
circum. in cm)
Family health assessment form
o Central obesity:
o Is a guide in data collection as a means
WHR >= 1.0 cm
in men and 0.85 to record pertinent information about the
in women family that will assist the nurse in
working with family.
Dietary history
Genogram
specifying quality and
quantity of food or o Helps the nurse outline the family’s
nutrient intake per day structure. It is a way to diagram the
Eating/feeding family. Three generations of family
habits/practice members are included with symbols
Developmental assessment of denoting genealogy
infant, toddlers and Ecomap
preschoolers o A classic tool that is used to depict a
E.g. Metro Manila family’s linkages to its suprasystem
Developmental o Portrays an overview of the family in
Screening Test their situation; it depicts the important
(MMDST) nurturant of a conflict laden connection
Risk factor assessment between the family and the world. It
indicating presence of major
demonstrates the flow of resources or function in a
the lacks and deprivation specific area on
o A mapping procedure that highlights the health
nature of the interfaces and points to promotion and
conflicts to be mediated, bridges to built, maintenance
and resources to be sought and I. PRESENCE OF WELLNESS CONDITION
mobilized A. Potential for enhanced capability for:
Healthy lifestyle – eg nutrition/diet,
exercise/activity
Health maintenance/health management
FAMILY HEALTH ASSESSMENT: Typology of Parenting
Nursing Problems in Family Nursing Practice Breastfeeding
Spiritual well-being – process of client’s
First Level Assessment developing/unfolding of mystery through
harmonious interconnectedness that comes
o Categorize if:
from inner strength/sacred source/God
Presence of wellness condition (NANDA, 2001)
Stated as potential or Others. Specify _____
readiness
A clinical or nursing B. Readiness for enhanced capability for:
judgment about a client Healthy lifestyle
in transition from a Health maintenance/health management
specific level of Parenting
wellness or capability to Breastfeeding
a higher level Spiritual well-being
Wellness potential Others. Specify ____
o Is a nursing _
judgment on
wellness state Presence of health threat
or condition Conditions that are
based on conducive to disease
client’s and accident or may
performance, result to failure to
current maintain wellness or
competencies, realize health potential
or clinical data Family is health but
BUT NO there are risks
EXPLICIT o HICE
EXPRESSION o Hazards
OF DESIRE to o Inadequate/
achieve a lack of
higher level of immunization
state or function o Cross infection
in a specific o Environmental
area on health sanitation is
promotion and poor
maintenance.
Examples are ff:
Readiness for o Presence of risk
Enhanced Wellness
factors of
state
specific
o Is a nursing
diseases (e.g.
judgment on lifestyle
wellness state diseases,
or condition metabolic
based on syndrome)
client’s o Threat of cross
performance, or
infection from
condition based
communicable
on client’s
disease case
current
o Family size
competencies
beyond what
or performance
family
clinical data or
resources can
EXPLICIT
adequately
EXPRESSION
provide
OF DESIRE TO
o Accident
ACHIEVE A
hazards specify
HIGHER
Broken
LEVEL OF
chairs
STATE or
Pointed/ Polluted
sharp water
objects, supply
poisons Presence of
and breeding or
medicines resting
improperly sights of
kept vectors of
Fire diseases
hazards Improper
Fall garbage/ref
hazards use
Others disposal
specify Unsanitary
o Faulty/ waste
unhealthful disposal
nutritional/eatin Improper
g habits or drainage
feeding system
techniques/prac Poor
tices. Specify lighting and
Inadequate ventilation
food intake Noise
both in pollution
quality and Air pollution
quantity o Unsanitary food
Excessive handling and
intake of preparation
certain o Unhealthy
nutrients lifestyle and
Faulty Personal
eating Habits/Practice
habits s. Specify
Ineffective Alcohol
breastfeedi drinking
ng Cigarette/
Faulty tobacco
feeding smoking
techniques Walking
o Stress barefooted
provoking or
factors. Specify inadequate
Strained footwear
marital Eating raw
relationship meat or fish
Strained Poor
parent- personal
sibling hygiene
relationship Self
Interperson medication/
al conflicts substance
between abuse
family o Inherent
members personal
Care-giving characteristics
burden Poor
o Poor impulse
Home/Environm control
ental o Health history,
Condition/Sanit which may
ation. Specify. participate/indu
Inadequate ce the
living space occurrence of
Lack of health deficit
food Previou
storage s
facilities history
of
difficult Disability – whether congenital or arising from
labor illness; transient/temporary
o Inappropriate
role assumption
Child
Presence of stress
assumi points/foreseeable crisis
ng Anticipated periods of
mother’ unusual demand on the
s role, individual or family in
father terms of
not adjustment/family
assumi resources
ng his Anything which is
role anticipated/expected to
o Lack of become a problem
immunization/in SACCIPDA
adequate S-chool entrance
immunization A-dolescents
status specially C-ourtships and
of children marriage
o Family disunity C-ircumcision
Self-oriented I-llegitimacy
behavior of P-regnancy
member(s)
D-eath
Unresolved
A-ddiction
conflicts of
EXAMPLES OF PRESENCE OF STRESS
member(s)
POINTS/FORESEEABLE CRISIS SITUATIONS
Intolerable
Marriage
disagreemen
Pregnancy, labor, puerperium
t
Parenthood
o Others. Specify
Additional member e.g. newborn, lodger
____ Abortion
Entrance at school
Presence of health deficits Menopause
Instances of failure in Loss of job
health maintenance Hospitalization of a family member
If identified problem is Death of a member
an abnormality, illness Resettlement
or disease, there’s a Adolescence
gap/difference between Divorce or separation
normal status (ideal, Resettlement in a new community
desirable, expected) & Illegitimacy
actual status (the Others, specify _____
outcome/result/problem
encountered on the
actual day)
Illness states,
regardless of whether it
is diagnosed or not by
medical practitioner
Failure to
thrive/developmental
according to normal rate
Disability – whether
congenital or arising
from illness; temporary
4Ds
o Disease
o Disorder
o Disability
o Developmental Second Level Assessment
problems I. INABILITY TO RECOGNIZE THE
EXAMPLES OF PRESENCE OF HEALTH DEFICITS PRESENCE OF THE CONDITION OR
Illness states, regardless of whether it is PROBLEM DUE TO:
diagnosed or undiagnosed by medical Lack of or inadequate knowledge
practitioner Denial about its existence or severity as a
Failure to thrive/develop according to normal result of fear of consequences of diagnosis of
rate problem, specifically:
-social-stigma, loss of respect of peer/significant 3. Limitation of luck/lack of physical resources
others Significant persons unexpressed feelings (e.g.
-economic/cost implications hostility/anger, guilt, fear/anxiety, despair,
-physical consequences rejection) which his/her capacities to provide
-emotional/psychological issues/concerns care
Attitude/philosophy in life, which hinders Philosophy in life which negates/hinder caring
recognition/acceptance of a problem for the sick, disabled, dependent,
Others. Specify ____ vulnerable/at risk member
Member’s preoccupation with on
concerns/interests
II. INABILITY TOMAKE DECISIONS WITH Prolonged disease or disabilities, which
RESPECT TO TAKING APPROPRIATE exhaust supportive capacity of family
HEALTH ACTION DUE TO: members
Failure to comprehend the nature/magnitude Altered role performance, specify.
of the problem/condition 1. Role denials or ambivalence
Low salience of the problem/condition 2. Role strain
Feeling of confusion, helplessness and/or 3. Role dissatisfaction
resignation brought about by perceive 4. Role conflict
magnitude/severity of the situation or problem 5. Role confusion
-i.e. failure to breakdown problems into manageable 6. Role overload
units of attack Others. Specify ____
Lack of/inadequate knowledge/insight as to
alternative courses of action open to them
Inability to decide which action to take from IV. INABILITY TOPROVIDE A HOME
among a list of alternatives ENVIRONMENT CONDUCIVE TO HEALTH
Conflicting opinions among family MAINTENANCE AND PERSONAL
members/significant others regarding action DEVELOPMENT DUE TO:
to take. Inadequate family resources specifically:
Lack of/inadequate knowledge of community 1. Financial constraints/limited financial
resources for care resources
Fear of consequences of action, specifically: 2. Limited physical resources – i.e. lack of space
1. Social consequences to construct facility
2. Economic consequences Failure to see benefits (specifically long term
3. Physical consequences ones) of investments in home environment
4. Emotional/psychological consequences improvement
Negative attitude towards the health condition Lack of/inadequate knowledge of importance
or problem – by negative attitude is meant of hygiene and sanitation
one that interferes with rational decision- Lack of/inadequate knowledge of preventive
making measures
Inaccessibility of appropriate resources for Lack of skill in carrying out measures to
care, specifically: improve home environment
1. Physical inaccessibility Ineffective communication pattern within the
2. Costs constraints or economic/financial family
inaccessibility Lack of supportive relationship among family
Lack of trust/confidence in the health members
personnel/agency Negative attitudes/philosophy in life which is
Misconceptions or erroneous information not conducive to health maintenance and
about proposed course(s) of action personal development
Others specify ____ Lack of/inadequate competencies in relating
to each other for mutual growth and
maturation
III. INABILITY TOPROVIDE ADEQUATE e.g. reduced ability to meet the physical and
NURSING CARE TO THE SICK, DISABLED, psychological needs of other members as a result of
DEPENDENT OR VULNERABLE/AT RISK family’s preoccupation with current problem or
MEMBER OF THE FAMILY DUE TO: condition.
Lack of/inadequate knowledge about the Others specify ____
disease/health condition (nature, severity,
complications, prognosis and management)
Lack of/inadequate knowledge about child V. FAILURE TO UTILIZE COMMUNITY
development and care RESOURCES FOR HEALTH CARE DUE TO:
Lack of/inadequate knowledge of the nature Lack of/inadequate knowledge of community
or extent of nursing care needed resources for health care
Lack of the necessary facilities, equipment Failure to perceive the benefits of health
and supplies of care care/services
Lack of/inadequate knowledge or skill in Lack of trust/confidence in the
carrying out the necessary intervention or agency/personnel
treatment/procedure of care (i.e. complex Previous unpleasant experience with health
therapeutic regimen or healthy lifestyle worker
program) Fear of consequences of action (preventive,
Inadequate family resources of care diagnostic, therapeutic, rehabilitative)
specifically: specifically:
1. Absence of responsible member 1. Physical/psychological consequences
2. Financial constraints 2. Financial consequences
3. Social consequences
Unavailability of required care/services
Inaccessibility of required services due to:
1. Cost constraints
2. Physical inaccessibility
Lack of or inadequate family resources,
specifically
1. Manpower resources, eg baby sitter
2. Financial resources, cost of medicines
prescribe
Feeling of alienation to/lack of support from
the community
e.g. stigma due to mental illness, AIDS, etc.
Negative attitude/philosophy in life which
hinders effective/maximum utilization of
community resources for health care
Others, specify ____
3. PLANNING
4. INTERVENTION
5. EVALUATION
You might also like
- Family health assessment nursing problemsDocument8 pagesFamily health assessment nursing problemsMari MazNo ratings yet
- CHN MergedDocument16 pagesCHN MergedJilliary AlexandraNo ratings yet
- Community AssessmentDocument3 pagesCommunity AssessmentMariah Jane TaladuaNo ratings yet
- Community Health Nursing Skills Lec MIDTERMSDocument43 pagesCommunity Health Nursing Skills Lec MIDTERMSKrisha CafongtanNo ratings yet
- Nursing Assessment in Family Nursing Practice2Document64 pagesNursing Assessment in Family Nursing Practice2Gian DimayugaNo ratings yet
- 03 Family Nursing Assessment CHN-1Document4 pages03 Family Nursing Assessment CHN-1Ivan MaximusNo ratings yet
- CHN Rle - Midterm Transes MergedDocument12 pagesCHN Rle - Midterm Transes MergedJayla MarieNo ratings yet
- 02 Family Nursing Assessment CHN-1Document4 pages02 Family Nursing Assessment CHN-1Ivan MaximusNo ratings yet
- Family Nursing Assessment: A Guide to Collecting DataDocument6 pagesFamily Nursing Assessment: A Guide to Collecting DataAbigail BascoNo ratings yet
- OUR LADY OF FATIMA UNIVERSITY COLLEGE OF NURSING STEPS IN NURSING ASSESSMENTDocument6 pagesOUR LADY OF FATIMA UNIVERSITY COLLEGE OF NURSING STEPS IN NURSING ASSESSMENTJM RomiasNo ratings yet
- CHN Lec - Midterm TransesDocument25 pagesCHN Lec - Midterm TransesKaela ChoiNo ratings yet
- NCM 104 Family Health AssessmentDocument2 pagesNCM 104 Family Health AssessmentnikkibooNo ratings yet
- 3lec wk3Document6 pages3lec wk3claire yowsNo ratings yet
- Family Nursing Care Plan: 2 Major Types of Nursing AssessmentDocument3 pagesFamily Nursing Care Plan: 2 Major Types of Nursing AssessmentMariah Jane TaladuaNo ratings yet
- Ha Chapter 1Document3 pagesHa Chapter 1Angel MeñozaNo ratings yet
- Family Health AssessmentDocument12 pagesFamily Health Assessmentlorelie asisNo ratings yet
- Assessing Family Health NeedsDocument5 pagesAssessing Family Health NeedsRodolf Gerone G. MacahilosNo ratings yet
- Family Nursing ProcessDocument11 pagesFamily Nursing ProcessSofia Marie GalendezNo ratings yet
- Prelim Health Assessment Lec TransesDocument17 pagesPrelim Health Assessment Lec TransesVhan Antonette EscoridoNo ratings yet
- CHN - Skills and RLE - Steps in Family Nursing AssessmentDocument20 pagesCHN - Skills and RLE - Steps in Family Nursing AssessmentMary Joyce Victoriano UngsodNo ratings yet
- Mod 2 CHN Lec 2Document11 pagesMod 2 CHN Lec 2Emily BernatNo ratings yet
- Family Health Nursing PracticeDocument54 pagesFamily Health Nursing PracticeTrixNo ratings yet
- CHN Skills Lab Module 2020Document138 pagesCHN Skills Lab Module 2020mysterioushumane100% (4)
- Family Nursing Case Study AnalysisDocument3 pagesFamily Nursing Case Study AnalysisJoshua MendozaNo ratings yet
- Coll (: To ForDocument1 pageColl (: To ForggggangNo ratings yet
- Family Case Study FormatDocument3 pagesFamily Case Study FormatkasjdkasNo ratings yet
- MODULE 4 Family Nursing ProcessDocument5 pagesMODULE 4 Family Nursing ProcessAmethystNo ratings yet
- Family Nursing ProcessDocument12 pagesFamily Nursing ProcessChristine CornagoNo ratings yet
- RLE 104 JOIE22Community Assessment Diagnosis ADocument59 pagesRLE 104 JOIE22Community Assessment Diagnosis AESTE CRECIA EDULLANTES BULLECERNo ratings yet
- Nursing Family AssessmentDocument5 pagesNursing Family AssessmentElizabeth IdananNo ratings yet
- Saint Louis University: School of NursingDocument1 pageSaint Louis University: School of NursingheatherNo ratings yet
- Family Clientele Levels and Assessment ToolsDocument5 pagesFamily Clientele Levels and Assessment ToolsKris Elaine GayadNo ratings yet
- Saint Louis University: School of NursingDocument2 pagesSaint Louis University: School of NursingAzizah VillaminNo ratings yet
- Week 1: Community Health Nursing (RLE) Midterm PeriodDocument13 pagesWeek 1: Community Health Nursing (RLE) Midterm PeriodAndrea AputenNo ratings yet
- Family Health Data OrganizationDocument4 pagesFamily Health Data OrganizationEric Matig-a EbradaNo ratings yet
- CHAPTER 11-14 NURSING PROCESS (ADPIE)Document7 pagesCHAPTER 11-14 NURSING PROCESS (ADPIE)Alyssa SegubreNo ratings yet
- 3 AssessmentDocument9 pages3 AssessmentChelette MazurNo ratings yet
- "Energized Families": Data Collection - Data Analysis - DiagnosisDocument3 pages"Energized Families": Data Collection - Data Analysis - DiagnosisEric Matig-a EbradaNo ratings yet
- Module 3 - Nursing Assessment in Family Nursing PracticeDocument7 pagesModule 3 - Nursing Assessment in Family Nursing PracticeRogedith DelaRosaNo ratings yet
- ST JUDE CA2 Day 1 Note Taking GuideDocument4 pagesST JUDE CA2 Day 1 Note Taking Guidefaker than fakeNo ratings yet
- CHN SLDocument21 pagesCHN SLKristine CernaNo ratings yet
- Patient-Centered, Family Focused, Community Oriented Care MatrixDocument13 pagesPatient-Centered, Family Focused, Community Oriented Care MatrixJesse MonsalveNo ratings yet
- Nursing AssessmentDocument28 pagesNursing AssessmentDobby AsahiNo ratings yet
- Text Book of Pediatric Dentistry-81-86Document6 pagesText Book of Pediatric Dentistry-81-86Karma YogaNo ratings yet
- Unit 4Document6 pagesUnit 4Reniella HidalgoNo ratings yet
- CHN 211 Week 5 PPT Family Nursing and Nursing ProcessDocument63 pagesCHN 211 Week 5 PPT Family Nursing and Nursing ProcessAlyssa Marie SantosNo ratings yet
- Week 1: Community Health Nursing (RLE) Midterm PeriodDocument13 pagesWeek 1: Community Health Nursing (RLE) Midterm PeriodAndrea AputenNo ratings yet
- CHN 5-7 RleDocument45 pagesCHN 5-7 RleFranz keannu Libunao GonzalesNo ratings yet
- Pafp Foundation Courses: Instructional DesignDocument12 pagesPafp Foundation Courses: Instructional DesignZaqueo Gutierrez FajardoNo ratings yet
- Jurnal KeluargaDocument6 pagesJurnal KeluargavharsyaNo ratings yet
- Children With ChronicDocument9 pagesChildren With ChronicMado Rachman DzakiNo ratings yet
- Interview and History Taking (Reviewer)Document10 pagesInterview and History Taking (Reviewer)James Lord GalangNo ratings yet
- GENOGRAM AND FAMILY COPINGDocument15 pagesGENOGRAM AND FAMILY COPINGJmarie Brillantes PopiocoNo ratings yet
- 3.1 NCM 211 Rle - Family Health Nursing - AssessmentDocument16 pages3.1 NCM 211 Rle - Family Health Nursing - AssessmentLYRIZZA LEA BHEA DESIATANo ratings yet
- Family Nursing Care Plan: Nursing Interventions Rationale Methods of Nurse-Family Contact Resources RequiredDocument2 pagesFamily Nursing Care Plan: Nursing Interventions Rationale Methods of Nurse-Family Contact Resources RequiredAlma Cayap100% (1)
- Family Health Assessment - 121832Document21 pagesFamily Health Assessment - 121832RumochiiNo ratings yet
- Module 5 104Document17 pagesModule 5 104camille nina jane navarroNo ratings yet
- Concept of Family and Nursing AssessmentDocument9 pagesConcept of Family and Nursing AssessmentJunry PilapilNo ratings yet
- Improving the Quality of Child Custody Evaluations: A Systematic ModelFrom EverandImproving the Quality of Child Custody Evaluations: A Systematic ModelNo ratings yet
- PGB 2 - Parte IiDocument32 pagesPGB 2 - Parte Iikira1234No ratings yet
- The Importance of Social Interaction and Social RelationshipsDocument12 pagesThe Importance of Social Interaction and Social Relationshipsp007No ratings yet
- 2020 Pathology Compilation Questions by TopicsDocument7 pages2020 Pathology Compilation Questions by Topicsrupertgrint2000No ratings yet
- OM. K 970 III, K 970 III Rescue, K 970 SmartGuard. 2021-11Document152 pagesOM. K 970 III, K 970 III Rescue, K 970 SmartGuard. 2021-11SamossyzNo ratings yet
- Learning Packet in Level 1-NCM 106 NURSING PHARMACOLOGY: College of Nursing School Year 2020-2021Document15 pagesLearning Packet in Level 1-NCM 106 NURSING PHARMACOLOGY: College of Nursing School Year 2020-2021Nur Sanaani100% (1)
- DrugDocument8 pagesDrugAlyzza DagoyNo ratings yet
- Maas 2007Document11 pagesMaas 2007Caroline FelicianoNo ratings yet
- MPH Internship PresentationDocument20 pagesMPH Internship PresentationIfedayo AdegbeyeniNo ratings yet
- Hyperthermia NCPDocument1 pageHyperthermia NCPmaeca101No ratings yet
- Cardio Exercise Testing in Children and AdolecentsDocument288 pagesCardio Exercise Testing in Children and AdolecentsTeoNo ratings yet
- Lymphatic Drainage of HNFDocument80 pagesLymphatic Drainage of HNFMehek BatraNo ratings yet
- Hay Job Evaluation Manual Best Practice PDFDocument376 pagesHay Job Evaluation Manual Best Practice PDFKukuh Hidayat92% (12)
- Australia Modified Karnofsky Performance ScaleDocument1 pageAustralia Modified Karnofsky Performance ScaleSirish ExpertNo ratings yet
- Handbook of Pulmonary RehabilitationDocument4 pagesHandbook of Pulmonary RehabilitationAndreea MoalesNo ratings yet
- Urinary: Rachel Neto, DVM, MS, DACVP May 28 2020Document15 pagesUrinary: Rachel Neto, DVM, MS, DACVP May 28 2020Rachel AutranNo ratings yet
- MatrizDocument91 pagesMatrizndsjNo ratings yet
- Kartu Soal Bahasa Inggris XIIDocument7 pagesKartu Soal Bahasa Inggris XIICut FitriasariNo ratings yet
- EATIING DISORDERS Fall 2023-2024Document64 pagesEATIING DISORDERS Fall 2023-2024bill haddNo ratings yet
- Camping Recreational ActivityDocument5 pagesCamping Recreational ActivityGylle Marie PlazaNo ratings yet
- Dalal & MishraDocument491 pagesDalal & MishraKarthika M TharakanNo ratings yet
- Quiz Critical CareDocument15 pagesQuiz Critical CareSuma AhmadNo ratings yet
- 21th July - The Indian ExpressDocument16 pages21th July - The Indian ExpressAbc DownNo ratings yet
- Oxygen Therapy ChildrenDocument2 pagesOxygen Therapy ChildrenAnisha SalujaNo ratings yet
- Registering As A Dentist With The General Dental Council (Overseas Qualified)Document18 pagesRegistering As A Dentist With The General Dental Council (Overseas Qualified)zahra seraj0% (1)
- Head To Toe AssessmentDocument2 pagesHead To Toe AssessmentAyucahyaNo ratings yet
- Effectiveness of BNT162b2 Vaccine Against Omicron Variant in South AfricaDocument3 pagesEffectiveness of BNT162b2 Vaccine Against Omicron Variant in South AfricaDaniel A. SaldanaNo ratings yet
- Blood ReportsDocument16 pagesBlood ReportsHafsa NawaazNo ratings yet
- Antihypertensive Drugs GuideDocument11 pagesAntihypertensive Drugs GuideRanes AndyNo ratings yet
- AMENORRHOEADocument16 pagesAMENORRHOEAĶHwola ƏľsHokryNo ratings yet
- 【医脉通】2021 EAST实践指南:横纹肌溶解症的管理Document9 pages【医脉通】2021 EAST实践指南:横纹肌溶解症的管理rd ytNo ratings yet