Professional Documents
Culture Documents
Noncardiogenic Pulmonary Edema
Uploaded by
Irina DuceacOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Noncardiogenic Pulmonary Edema
Uploaded by
Irina DuceacCopyright:
Available Formats
11/8/2022 Noncardiogenic pulmonary edema - UpToDate
Official reprint from UpToDate®
www.uptodate.com © 2022 UpToDate, Inc. and/or its affiliates. All Rights Reserved.
Noncardiogenic pulmonary edema
Author: Michael M Givertz, MD
Section Editor: Stephen S Gottlieb, MD
Deputy Editor: Geraldine Finlay, MD
All topics are updated as new evidence becomes available and our peer review process is complete.
Literature review current through: Oct 2022. | This topic last updated: Jun 14, 2022.
INTRODUCTION
Pulmonary edema is due to the movement of excess fluid into the alveoli as a result of an
alteration in one or more of Starling's forces. In cardiogenic pulmonary edema, a high
pulmonary capillary pressure (as estimated clinically from the pulmonary artery wedge
pressure) is responsible for the abnormal fluid movement [1,2]. (See "Pathophysiology of
cardiogenic pulmonary edema" and "Approach to diagnosis and evaluation of acute
decompensated heart failure in adults".)
In contrast, noncardiogenic pulmonary edema is caused by various disorders in which factors
other than elevated pulmonary capillary pressure are responsible for protein and fluid
accumulation in the alveoli [3]. The distinction between cardiogenic and noncardiogenic causes
is not always possible, since the clinical syndrome may represent a combination of several
different disorders. The diagnosis is important, however, because treatment varies
considerably depending upon the underlying pathophysiologic mechanisms.
THE STARLING RELATIONSHIP
Fluid balance between the interstitium and vascular bed in the lung, as in other
microcirculations, is determined by the Starling relationship, which predicts the net flow of
liquid across a membrane. This can be expressed in the following equation:
Net filtration = (Lp x S) x (delta hydraulic pressure - delta oncotic pressure)
https://www.uptodate.com/contents/noncardiogenic-pulmonary-edema/print?search=pulmonary edema physiology&source=search_result&selectedTitle=1~150… 1/12
11/8/2022 Noncardiogenic pulmonary edema - UpToDate
= (Lp x S) x [(Pcap - Pif) - s(πcap - πif)]
where:
● Lp is the unit permeability (or porosity) of the capillary wall.
● S is the surface area available for fluid movement.
● Pcap and Pif are the capillary and interstitial fluid hydraulic pressures.
● πcap and πif are the capillary and interstitial fluid oncotic pressures; the interstitial
oncotic pressure is derived primarily from filtered plasma proteins and to a lesser degree
from proteoglycans in the interstitium.
● s represents the reflection coefficient of proteins across the capillary wall (with values
ranging from 0 if completely permeable to 1 if completely impermeable).
In normal microvessels, there is ongoing filtration of a small amount of low protein liquid. In
noncardiogenic pulmonary edema, the most common mechanism for a rise in transcapillary
filtration is an increase in capillary permeability. At a given increase in capillary permeability,
the rate of accumulation of lung liquid is related in part to the functional capacity of the
lymphatic vessels to remove the excess fluid.
DEFINITION OF NONCARDIOGENIC PULMONARY EDEMA
Noncardiogenic pulmonary edema is identified clinically by the presence of radiographic
evidence of alveolar fluid accumulation without hemodynamic evidence to suggest a
cardiogenic etiology (ie, pulmonary artery wedge pressure ≤18 mmHg). The accumulation of
fluid and protein in the alveolar space leads to decreased diffusing capacity, hypoxemia, and
shortness of breath.
The major causes of noncardiogenic pulmonary edema are the acute respiratory distress
syndrome (ARDS) [2] and, less often, high altitude and neurogenic pulmonary edema. Other
less common causes include pulmonary edema due to opioid overdose, pulmonary embolism,
eclampsia, transfusion-related acute lung injury and acute kidney injury (sometimes referred
to as “uremic lung”) [4]. Hypoalbuminemia alone is not a cause of pulmonary edema. (See
'Absence of pulmonary edema with hypoalbuminemia' below.)
PERMEABILITY PULMONARY EDEMA DUE TO ARDS
https://www.uptodate.com/contents/noncardiogenic-pulmonary-edema/print?search=pulmonary edema physiology&source=search_result&selectedTitle=1~150… 2/12
11/8/2022 Noncardiogenic pulmonary edema - UpToDate
The alveolar-capillary membrane becomes damaged and leaky in cases of permeability
pulmonary edema, allowing increased movement of water and proteins from the intravascular
space to the interstitial space. In most patients, the concentration of protein in the interstitium
exceeds 60 percent of the plasma value, compared to less than 45 percent in cardiogenic
pulmonary edema [5].
Permeability pulmonary edema is the most prominent feature of acute respiratory distress
syndrome (ARDS) [6]. In the past, many authors equated the clinical disorder ARDS with the
pathological entity of permeability pulmonary edema. However, these two terms should not
be used interchangeably. Although some degree of permeability edema is invariably present at
the onset of ARDS, other important structural abnormalities of the lung typically emerge as
ARDS evolves. Furthermore, many episodes of permeability pulmonary edema never result in
the severe physiological impairment that is required for the designation ARDS. (See "Acute
respiratory distress syndrome: Clinical features, diagnosis, and complications in adults".)
ARDS can be seen in a number of disorders, including sepsis, acute pulmonary infection, non-
thoracic trauma, inhaled toxins, disseminated intravascular coagulation, shock lung, freebase
cocaine smoking, postcoronary artery bypass grafting (especially in patients on amiodarone),
inhalation of high oxygen concentrations, and acute radiation pneumonitis. Regardless of
etiology, the clinical scenario is similar in most patients once membrane damage has occurred.
Sepsis- or ischemia-induced release of cytokines, such as interleukin-1, interleukin-8, and
tumor necrosis factor, may play an important role in the increase in pulmonary capillary
permeability, at least in part via the recruitment of neutrophils [7]. (See "Acute respiratory
distress syndrome: Epidemiology, pathophysiology, pathology, and etiology in adults".)
Presentation and diagnosis — Patients with ARDS present with severe respiratory distress
(dyspnea) in association with the acute appearance of diffuse chest radiographic infiltrates
and hypoxemia. The onset of ARDS is often within the first two hours after an inciting event,
although this can be delayed as long as one to three days. Chest radiographs usually progress
to a bilateral alveolar filling pattern. The diagnosis of permeability pulmonary edema requires
distinction from cardiogenic pulmonary edema and from other causes of lung disease or
injury.
Patients with noncardiogenic (or cardiogenic) pulmonary edema rarely have unilateral edema
[8-10]. Unilateral noncardiogenic pulmonary edema may be caused by conditions ipsilateral to
the edema such as aspiration, contusion, re-expansion, and pulmonary vein occlusion (eg,
veno-occlusive disease or extrinsic compression) and by conditions contralateral to the edema
such as pulmonary embolism and lobectomy [8]. These lesions should be distinguished from
https://www.uptodate.com/contents/noncardiogenic-pulmonary-edema/print?search=pulmonary edema physiology&source=search_result&selectedTitle=1~150… 3/12
11/8/2022 Noncardiogenic pulmonary edema - UpToDate
unilateral cardiogenic pulmonary edema, which is chiefly caused by eccentric mitral
regurgitation [11] or following minimally invasive cardiac surgery [12].
Distinction from heart failure — Clinically and radiographically, ARDS closely resembles
severe cardiogenic pulmonary edema. The distinction between these disorders is often
apparent from the clinical circumstances at the onset of respiratory distress. As examples,
pulmonary edema occurring in the setting of an acute coronary syndrome is almost always
cardiogenic, while that occurring in the setting of sepsis strongly suggests a noncardiac
etiology. Pulmonary edema occurring in the setting of multiple transfusions could be due to a
combination of cardiogenic pulmonary edema (eg, due to volume) and acute lung injury. (See
"Clinical manifestations and diagnosis of cardiogenic shock in acute myocardial infarction" and
"Approach to diagnosis and evaluation of acute decompensated heart failure in adults".)
● Pulmonary artery catheter – A pulmonary artery (or Swan-Ganz) catheter should be
placed if the mechanism of edema formation cannot be discerned with confidence. A
pulmonary artery wedge pressure less than 18 mmHg favors acute lung injury over
cardiogenic pulmonary edema. (See "Pulmonary artery catheterization: Indications,
contraindications, and complications in adults".)
It is important to appreciate that pulmonary artery catheterization can be misleading in certain
settings. Most important, myocardial ischemia can cause severe but transient left ventricular
dysfunction, leading to "flash" pulmonary edema. If the wedge pressure is first measured after
the ischemia has resolved (and left ventricular function has improved), a relatively normal
value may be obtained, leading to the erroneous conclusion that the respiratory distress was
caused by acute lung injury. (See "Approach to diagnosis and evaluation of acute
decompensated heart failure in adults".)
On the other hand, an elevated pulmonary artery wedge pressure does not exclude the
possibility of acute lung injury. It is estimated that as many as 20 percent of patients with ARDS
have concomitant left ventricular dysfunction [7], and the percentages are much higher in
patients with ARDS secondary to sepsis [13]. Right ventricular dilation is also commonly
present in ARDS, while right ventricular dysfunction may be present in the most severe cases
and predict worse outcomes [14]. The diagnosis of acute lung injury cannot be made easily
when the wedge pressure is elevated; thus, the clinical course must be observed as the wedge
pressure responds to treatment. If pulmonary infiltrates and hypoxemia do not improve
appreciably within 24 to 48 hours after fluid restriction (with or without diuresis) and
normalization of the wedge pressure, then acute lung injury probably coexists with
cardiogenic edema.
https://www.uptodate.com/contents/noncardiogenic-pulmonary-edema/print?search=pulmonary edema physiology&source=search_result&selectedTitle=1~150… 4/12
11/8/2022 Noncardiogenic pulmonary edema - UpToDate
● Plasma BNP – Measurement of plasma B-type natriuretic peptide (BNP), or N-terminal
pro-BNP, has been used to distinguish heart failure (high BNP) from lung disease (normal
or mildly elevated BNP) as a cause of dyspnea with a high degree of accuracy even in
patients with both lung and heart disease [15]. However, intermediate values are often
not helpful. The role of these biomarkers in the diagnosis of pulmonary edema has been
less well studied. Data in the ICU setting suggested limited ability to discriminate ARDS
from cardiogenic pulmonary edema [16], as levels may increase with the development
[17]and severity [18] of ARDS. (See "Approach to diagnosis and evaluation of acute
decompensated heart failure in adults".)
Clinical prediction tools have been developed to distinguish acute lung injury from cardiogenic
pulmonary edema [19]. These may provide a guide to expediting initial therapy, but require
further prospective evaluation. A number of novel biomarkers have also been proposed to aid
in this distinction [20].
Other lung diseases — Two pulmonary disorders are sometimes confused with ARDS:
diffuse alveolar hemorrhage and cancer.
● Diffuse alveolar hemorrhage, often due to a pulmonary capillaritis or diffuse alveolar
damage, should be considered whenever respiratory distress develops in association
with a large, otherwise unexplained drop in the blood hemoglobin concentration.
Hemoptysis may be minimal or absent prior to intubation; however, bronchoscopy after
intubation invariably reveals bloody secretions throughout the airways during active
hemorrhage.
Bland alveolar hemorrhage, which is characterized by hemorrhage into the alveolar spaces
without inflammation or destruction of the alveolar structures, may be caused by elevated LV
end diastolic pressure, coagulopathy, and, rarely, anticoagulant or antiplatelet therapy. (See
"The diffuse alveolar hemorrhage syndromes".)
● Cancer sometimes disseminates throughout the lungs so rapidly that the ensuing
respiratory failure may be mistaken for ARDS. This is most often due to lymphoma or
acute leukemia [21], but lymphangitic spread of solid tumors, acute toxicity from
chemotherapy (eg, mitomycin [also known as Mitomycin-C], methotrexate), and cancer-
associated DIC occasionally behave in a similar fashion [22]. Newer cancer treatments,
including immune checkpoint inhibitors, have also been associated with pneumonitis
[23]. (See "Toxicities associated with checkpoint inhibitor immunotherapy".)
Treatment — There are currently no known measures to correct the permeability abnormality
in ARDS. Clinical management involves treatment of the underlying disease (eg, antibiotics for
https://www.uptodate.com/contents/noncardiogenic-pulmonary-edema/print?search=pulmonary edema physiology&source=search_result&selectedTitle=1~150… 5/12
11/8/2022 Noncardiogenic pulmonary edema - UpToDate
infection) and supportive measures to maintain cellular and metabolic function, while waiting
for the acute lung injury to resolve. These supportive measures include mechanical ventilation,
maintenance of adequate nutrition, and hemodynamic monitoring when necessary to guide
fluid management and cardiovascular support [24]. Patients with severe ARDS may require
extracorporeal membrane oxygenation in addition to supportive medical therapies [25]. (See
"Ventilator management strategies for adults with acute respiratory distress syndrome" and
"Acute respiratory distress syndrome: Supportive care and oxygenation in adults" and
"Evaluation and management of suspected sepsis and septic shock in adults".)
Lowering the pulmonary artery wedge pressure with diuretics and fluid restriction can
improve pulmonary function and perhaps outcome [26,27]. One study, for example, analyzed
survival and length of stay in the intensive care unit for 40 patients with ARDS [26]. The patients
were divided into two groups: those with a reduction in pulmonary capillary wedge pressure
(PCWP) of at least 25 percent; and those with less or no reduction in PCWP. Survival was
greater in the patients with a large fall in PCWP (75 versus 29 percent). This difference
remained statistically significant after stratifying patients by age and by the APACHE II severity
of illness index. In a later study in which 1000 patients with acute lung injury were randomized
to a conservative versus liberal fluid management strategy, the conservative strategy
improved oxygenation and shortened duration of mechanical ventilation and ICU stay, but did
not reduce the incidence of shock, use of dialysis or mortality during the first 60 days [28]. (See
"Predictive scoring systems in the intensive care unit".)
A number of pharmacologic therapies for ARDS have been evaluated [29]. These include
inhaled vasodilators (nitric oxide, prostacyclin), anti-inflammatory therapies (glucocorticoids,
statins [30], prostaglandin E1), antioxidants (dietary oil supplementation), and exogenous
surfactant. Novel mechanical ventilation strategies, including high-frequency ventilation, liquid
ventilation, and prone positioning [31], as well as preventive strategies (eg, aspirin) [32] have
also been investigated. At present, NONE has shown consistent and unequivocal clinical
benefit [33]. Preclinical and early clinical data suggest that human mesenchymal stem cells may
attenuate lung injury and promote tissue repair in ARDS. (See "Acute respiratory distress
syndrome: Investigational or ineffective therapies in adults".)
Prognosis — The outcome of patients with ARDS has improved over time; hospital mortality
was approximately 60 percent in the years 1967 to 1981 and declined to 30 to 40 percent in the
1990s. As an example of this trend, one study evaluated 918 patients with ARDS at a single
institution between 1983 and 1993 [34]. The mortality from sepsis-related ARDS declined from
67 percent in 1990 to 40 percent in 1993; the improvement was largely confined to patients
under age 60. In a systematic analysis of ARDS studies published between 1994 and 2006, a
https://www.uptodate.com/contents/noncardiogenic-pulmonary-edema/print?search=pulmonary edema physiology&source=search_result&selectedTitle=1~150… 6/12
11/8/2022 Noncardiogenic pulmonary edema - UpToDate
decline in overall mortality rates of 1.1 percent per year was demonstrated [35]. The enhanced
survival is probably related to a variety of improvements in supportive care. Despite these
encouraging data, ARDS remains a world-wide problem with high mortality that is both under
recognized and undertreated [36].
Most deaths are due to the severity of the underlying disease, particularly multiorgan failure,
rather than the respiratory disease. While early deaths are typically due to the underlying
cause of the ARDS, later deaths often result from nosocomial pneumonia and sepsis. Long-
term survivors of ARDS typically show only mild abnormalities in pulmonary function and are
usually asymptomatic, although long-term physical, cognitive, and psychological sequelae have
been described [37,38]. (See "Acute respiratory distress syndrome: Prognosis and outcomes in
adults".)
OTHER NONCARDIOGENIC FORMS OF PULMONARY EDEMA
Other more unusual types of noncardiogenic pulmonary edema, often with unclear
pathophysiology, have been described.
High altitude pulmonary edema — High-altitude pulmonary edema (HAPE), which generally
occurs among individuals who rapidly ascend to altitudes above 12,000 to 13,000 feet (3600 to
3900 m), accounts for a majority of deaths due to high altitude disease [39,40]. An abnormally
pronounced degree of hypoxic pulmonary vasoconstriction at a given altitude appears to
underlie the pathogenesis of this disorder [14]. (See "High-altitude illness: Physiology, risk
factors, and general prevention" and "High-altitude pulmonary edema".)
Neurogenic pulmonary edema — Neurogenic pulmonary edema occurs after a variety of
neurologic disorders and procedures, including head injury, intracranial surgery, grand mal
seizures, subarachnoid or intracerebral hemorrhage, and electroconvulsive therapy [41].
Sympathetic overreactivity, with massive catecholamine surges, shifts blood from the systemic
to the pulmonary circulation with secondary elevations of left atrial and pulmonary capillary
pressures [42]. Pulmonary capillary leak caused by pressure-induced mechanical injury and/or
direct nervous system control over capillary permeability may play a contributory role. The
clinical presentation is characterized by acute hypoxemia, tachypnea, tachycardia, diffuse
rales, and frothy sputum or hemoptysis. Symptom onset tends to be rapid and most cases
resolve within 48 to 72 hours. The outcome is determined by the course of the primary
neurologic insult. It is important to distinguish neurogenic pulmonary edema from
cardiogenic pulmonary edema in the setting of stress cardiomyopathy. (See "Neurogenic
https://www.uptodate.com/contents/noncardiogenic-pulmonary-edema/print?search=pulmonary edema physiology&source=search_result&selectedTitle=1~150… 7/12
11/8/2022 Noncardiogenic pulmonary edema - UpToDate
pulmonary edema" and "Clinical manifestations and diagnosis of stress (takotsubo)
cardiomyopathy".)
Reperfusion pulmonary edema — Reperfusion pulmonary edema appears to represent a
form of high-permeability lung injury that is limited to those areas of lung from which
proximal thromboembolic obstructions have been removed. It may appear up to 72 hours
after surgery and is highly variable in severity, ranging from a mild form of edema resulting in
postoperative hypoxemia to an acute, hemorrhagic and fatal complication [43-45]. At
experienced centers, venovenous extracorporeal life support has been used as a bridge to
recovery or transplant when all other conventional strategies have failed [46,47] (see "Chronic
thromboembolic pulmonary hypertension: Pulmonary thromboendarterectomy"). A similar
condition may occur following lung transplantation due to ischemia-reperfusion injury. (See
"Primary lung graft dysfunction".)
Re-expansion pulmonary edema — Re-expansion pulmonary edema (RPE) usually occurs
unilaterally after rapid re-expansion of a collapsed lung (typically for greater than three days)
in patients with a pneumothorax [48], with rates ranging from 16 to 33 percent. Risk factors
include diabetes, size of pneumothorax, and presence of pleural effusion [49,50]. It may rarely
follow evacuation of large volumes of pleural fluid (>1 to 1.5 liters) (<1 percent) [51-54] or
removal of an obstructing endobronchial tumor.
The pathophysiologic mechanism is unknown. Proposed mechanisms include direct injury
from surfactant dysfunction in chronic atelectatic lung, increased transpleural pressures when
excessively negative pleural pressures are created during fluid or air removal in the setting of
an unexpandable lung, or indirect injury from reperfusion.
RPE appears to be related to the rapidity of lung re-expansion and to the severity and duration
of lung collapse. However, a study examining development of re-expansion pulmonary edema
following thoracentesis found that it was independent of the volume of fluid removed and
pleural pressures, and recommended that even large pleural effusions be drained completely
as long as chest pain or end-expiratory pleural pressure less than -20 cm H2O does not
develop [53].
Patients typically present soon (minutes to hours) after the inciting event, although
presentation can be delayed for up to 24 to 48 hours in some cases. The clinical course varies
from isolated radiographic changes to complete cardiopulmonary collapse but most patients
present with acute onset dyspnea, cough and hypoxemia. Typical CT findings include ipsilateral
ground-glass opacities, septal thickening, focal consolidation, and areas of atelectasis [55].
https://www.uptodate.com/contents/noncardiogenic-pulmonary-edema/print?search=pulmonary edema physiology&source=search_result&selectedTitle=1~150… 8/12
11/8/2022 Noncardiogenic pulmonary edema - UpToDate
A mortality rate as high as 20 percent has been described in one small review [56]; however
consistent with our experience, the mortality is much lower with later and larger series
reporting a mortality rate less than 5 percent [52,53,57].
Treatment is supportive, mainly consisting of supplemental oxygen and, if necessary,
mechanical ventilation. The disease is usually self-limited.
Opioid overdose — First described by Osler in 1880 [58], pulmonary edema can sometimes
complicate an overdose of heroin or methadone [59]; other related agents, including fentanyl
and naloxone, have also been implicated [60]. Risk factors include male sex and shorter
duration of heroin use. Most cases occur immediately or within hours of drug injection. The
chest radiograph usually demonstrates a nonuniform distribution of pulmonary edema.
The pathophysiology of this form of pulmonary edema is unknown; a combination of direct
toxicity of the drug, hypoxia, and acidosis secondary to hypoventilation and/or cerebral edema
has been proposed [61,62]. The observation that edema fluid contains protein concentrations
nearly identical to plasma and that pulmonary artery wedge pressures, when measured, are
normal suggests an alveolar-capillary membrane leak as the initiating cause. Resolution of this
form of pulmonary edema is rapid once hypoventilation and hypoxia are reversed by the
institution of assisted ventilation. In one case series, 9 of 27 patients (33 percent) required
mechanical ventilation; all but one were extubated within 24 hours [63]. Supportive care also
includes use of naloxone to reverse the opioid effects. The alarming increase in opioid use and
dependency suggests that clinicians will see more cases of pulmonary edema related to opioid
overdose in the emergency room and intensive care unit [64,65].
Salicylate toxicity — Aspirin is one of many drugs occasionally associated with the
development of noncardiogenic pulmonary edema. Salicylate-induced noncardiogenic
pulmonary edema and acute lung injury (ALI) generally occur in older patients with chronic
salicylate intoxication [66,67], but should be considered in all patients following aspirin
overdose. The medical history is critical to making the diagnosis, as misdiagnosis or delayed
diagnosis can lead to a significant increase in morbidity and mortality [67]. Salicylate-induced
ALI and pulmonary edema can complicate volume resuscitation and administration of sodium
bicarbonate, two mainstays of treatment in this setting. Thus, the presence of salicylate-
induced pulmonary edema is considered an absolute indication for hemodialysis [68]. (See
"Salicylate (aspirin) poisoning in adults".)
Other exogenous agents — Several commonly-prescribed medications have been associated
with noncardiogenic pulmonary edema, including amiodarone, bortezomib, and
immunosuppressive agents (eg, sirolimus, everolimus) [69,70]. It may be difficult to distinguish
https://www.uptodate.com/contents/noncardiogenic-pulmonary-edema/print?search=pulmonary edema physiology&source=search_result&selectedTitle=1~150… 9/12
11/8/2022 Noncardiogenic pulmonary edema - UpToDate
noncardiogenic pulmonary edema from heart failure in cardiac patients or infection in
immunosuppressed patients. Additional objective data, including invasive hemodynamics and
tissue biopsy, may be helpful in these cases. Acute lung injury and death have also been
reported with use of electronic cigarettes (vaping), and direct injury to lung epithelial cells with
capillary leak has been proposed as a mechanism. (See "E-cigarette or vaping product use-
associated lung injury (EVALI)" and "Vaping and e-cigarettes".)
Pulmonary embolism — Acute pulmonary edema in association with a massive pulmonary
embolus (PE) or multiple smaller emboli is uncommon but well described [71,72]. PE can cause
pulmonary edema by injuring the pulmonary and adjacent pleural systemic circulations,
elevating hydrostatic pressures in pulmonary and/or systemic veins, and perhaps by lowering
pleural pressure due to atelectasis. PE may also decrease the exit rates of pleural fluid by
increasing the systemic venous pressure (thereby hindering lymphatic drainage) or possibly by
decreasing pleural pressure (thereby hindering lymphatic filling). The effusions are typically
small and unilateral, and may become loculated if the diagnosis is delayed [73]. Older studies
showed that 20 percent of PE-related effusions are transudates, suggesting that hydrostatic
changes can also be important [74]. However, in a later case series, 26 of 93 patients with
effusions following PE underwent thoracentesis and all of the fluids met Light's criteria for
exudate (see "Diagnostic evaluation of a pleural effusion in adults: Initial testing"), suggesting
a primary role for vascular injury [75].
Viral infections — Rapidly progressive noncardiogenic pulmonary edema associated with
profound hypotension and a high case fatality rate has been described with hantavirus
infection (see "Hantavirus cardiopulmonary syndrome") [76], dengue hemorrhagic
fever/dengue shock syndrome (see "Dengue virus infection: Clinical manifestations and
diagnosis"), and most recently with COVID-19 infection (see "COVID-19: Clinical features").
Enteroviral 71 infection in young children [77] and SARS coronavirus infection in adults [78] are
other causes of viral-induced noncardiogenic pulmonary edema and hemorrhage (see "Severe
acute respiratory syndrome (SARS)"). The strain of H1N1 influenza A that caused the 2009 to
2010 pandemic caused severe ARDS in some patients (see "Seasonal influenza in adults: Clinical
manifestations and diagnosis"). There have also been reports of vascular leakage and
respiratory failure in the setting of severe Ebola virus disease [79].
Pulmonary veno-occlusive disease — Pulmonary veno-occlusive disease is a cause of
pulmonary hypertension and noncardiogenic pulmonary edema. This condition is discussed in
detail separately. (See "Epidemiology, pathogenesis, clinical evaluation, and diagnosis of
pulmonary veno-occlusive disease/pulmonary capillary hemangiomatosis in adults".)
https://www.uptodate.com/contents/noncardiogenic-pulmonary-edema/print?search=pulmonary edema physiology&source=search_result&selectedTitle=1~15… 10/12
11/8/2022 Noncardiogenic pulmonary edema - UpToDate
Transfusion-related acute lung injury — Transfusion-related acute lung injury (TRALI) is a
rare but potentially fatal complication of blood product transfusion that involves neutrophil
activation and pulmonary edema. Further details are provided separately. (See "Transfusion-
related acute lung injury (TRALI)".)
ABSENCE OF PULMONARY EDEMA WITH HYPOALBUMINEMIA
In older patients with heart failure with preserved ejection fraction, hypoalbuminemia due to
age, malnutrition, or sepsis may lower colloid osmotic pressure and facilitate the onset of
pulmonary edema [80]. In patients with acute heart failure, hypoalbuminemia has also been
associated with pleural effusions [81], and is an independent predictor of in-hospital and post-
discharge mortality [82]. In a study of more than 7000 patients with acute coronary syndrome,
serum albumin level ≤3.50 g/dL was an independent predictor of new-onset heart failure and
in-hospital mortality [83].
Although hypoalbuminemia can lead to peripheral edema by lowering the transcapillary
oncotic pressure gradient, it does not generally produce pulmonary edema. The pulmonary
capillaries appear to have a greater baseline permeability to albumin and therefore have a
higher interstitial oncotic pressure (about 18 mmHg) than do peripheral capillaries [84]. A fall
in the plasma albumin concentration is associated with a parallel decline in the pulmonary
interstitial oncotic pressure. The net effect is little or no change in the transcapillary oncotic
pressure gradient and therefore no pulmonary edema, unless there is a concurrent rise in left
atrial and pulmonary capillary pressures. (See "Pathophysiology and etiology of edema in
adults", section on 'Compensatory factors'.)
SUMMARY
● Overview – Noncardiogenic pulmonary edema is caused by various disorders in which
factors other than elevated pulmonary capillary pressure are responsible for protein and
fluid accumulation in the alveoli. In contrast, a high pulmonary capillary pressure is
responsible for the abnormal fluid movement in cardiogenic pulmonary edema.
Noncardiogenic pulmonary edema may be difficult to distinguish from cardiogenic
pulmonary edema and a mixed picture can occur. (See 'Introduction' above.)
● Pathogenesis – Fluid balance between the interstitium and vascular bed in the lung, as in
other microcirculations, is determined by the Starling relationship, which predicts the net
flow of liquid across a membrane. In noncardiogenic pulmonary edema, the most
https://www.uptodate.com/contents/noncardiogenic-pulmonary-edema/print?search=pulmonary edema physiology&source=search_result&selectedTitle=1~150… 11/12
11/8/2022 Noncardiogenic pulmonary edema - UpToDate
common mechanism for a rise in transcapillary filtration is an increase in capillary
permeability. Hypoalbuminemia alone is not a cause of pulmonary edema but can
contribute to pleural effusions and increased mortality in patients with acute heart
failure as well as in those with acute coronary syndrome. (See 'The Starling relationship'
above and 'Absence of pulmonary edema with hypoalbuminemia' above.)
● Definition – Noncardiogenic pulmonary edema is identified clinically by the presence of
radiographic evidence of alveolar fluid accumulation without hemodynamic evidence to
suggest a cardiogenic etiology (ie, pulmonary artery wedge pressure ≤18 mmHg). (See
'Definition of noncardiogenic pulmonary edema' above.)
● Etiologies
• The most common cause of noncardiogenic pulmonary edema is acute respiratory
distress syndrome. (See 'Permeability pulmonary edema due to ARDS' above.)
• Less common causes are high altitude and neurogenic pulmonary edema. (See 'High
altitude pulmonary edema' above and 'Neurogenic pulmonary edema' above.)
• Others include reperfusion and re-expansion pulmonary edema, heroin overdose or
use of vaping products, and salicylate or other drug toxicity. (See 'Reperfusion
pulmonary edema' above and 'Re-expansion pulmonary edema' above and 'Opioid
overdose' above and 'Salicylate toxicity' above and 'Other exogenous agents' above.)
• Other less common causes include pulmonary edema due to pulmonary embolism
and eclampsia, viral infections, pulmonary veno-occlusive disease, and transfusion-
related acute lung injury. (See 'Pulmonary embolism' above and 'Viral infections' above
and 'Pulmonary veno-occlusive disease' above and 'Transfusion-related acute lung
injury' above.)
Use of UpToDate is subject to the Terms of Use.
Topic 3456 Version 23.0
https://www.uptodate.com/contents/noncardiogenic-pulmonary-edema/print?search=pulmonary edema physiology&source=search_result&selectedTitle=1~15… 12/12
You might also like
- Guyton and Hall Textbook of Medical PhysiologyDocument13 pagesGuyton and Hall Textbook of Medical PhysiologyRobert StevenNo ratings yet
- Valvular Heart DiseaseDocument27 pagesValvular Heart DiseaseOwen J. WieseNo ratings yet
- Cardiac AsthmaDocument12 pagesCardiac AsthmaNeupane KsabNo ratings yet
- The Spectrum of TBDocument174 pagesThe Spectrum of TBcmolina84No ratings yet
- InflammationDocument59 pagesInflammationKarthik KumarNo ratings yet
- Vascular Complication of Injectable FillerDocument17 pagesVascular Complication of Injectable Fillerahmed100% (1)
- Valvular Heart DiseaseDocument2 pagesValvular Heart DiseaseAnonymous TVk12eX4No ratings yet
- Fontan Operation: DR Hussain BuxDocument62 pagesFontan Operation: DR Hussain BuxMujeeb Ur RehmanNo ratings yet
- Cardiogenic Pulmonary EdemaDocument1 pageCardiogenic Pulmonary EdemaAirish LimNo ratings yet
- Sepsis: PathophysiologyDocument8 pagesSepsis: PathophysiologyDonald NashNo ratings yet
- Asthma and Rhinitis During PregnancyDocument175 pagesAsthma and Rhinitis During PregnancyAndika Wima PratamaNo ratings yet
- Cardiac AssessmentDocument48 pagesCardiac AssessmentRatheesh NathNo ratings yet
- Anat FisioDocument653 pagesAnat Fisiodenydeniche388No ratings yet
- Sepsis WhoDocument36 pagesSepsis WholcycrlnNo ratings yet
- Diagnostic Thoracoscopy (VATS) in Lung CancerDocument18 pagesDiagnostic Thoracoscopy (VATS) in Lung CancerlmdarlongNo ratings yet
- Idiopathic Pulmonary Fibrosis: Optimizing The Diagnosis and Multi-Disciplinary Decision MakingDocument4 pagesIdiopathic Pulmonary Fibrosis: Optimizing The Diagnosis and Multi-Disciplinary Decision MakingAnna LiachenkoNo ratings yet
- Drenaj LimfaticDocument71 pagesDrenaj LimfaticGugiu Bogdan Ștefan90% (20)
- BronchoPulmonary Hygiene TechniquesDocument88 pagesBronchoPulmonary Hygiene Techniques私 シャーロットNo ratings yet
- Interstitial Lung DiseaseDocument26 pagesInterstitial Lung DiseaseEnimia ShyNo ratings yet
- Lung Mechanics and Ventilation-Lecture NotesDocument16 pagesLung Mechanics and Ventilation-Lecture NotesCarlos Eduardo LinaresNo ratings yet
- Cardiac Risk AssessmentDocument4 pagesCardiac Risk Assessmentmonir61No ratings yet
- Restrictive Lung DiseaseDocument32 pagesRestrictive Lung DiseaseSalman Khan100% (1)
- The PERT Concept Q1 A Step-By-Step Approach To Managing Pulmonary EmbolismDocument9 pagesThe PERT Concept Q1 A Step-By-Step Approach To Managing Pulmonary EmbolismntnquynhproNo ratings yet
- Textbook of Surgery For Dental Students-smile4DrDocument400 pagesTextbook of Surgery For Dental Students-smile4DrRotariu Ana Maria100% (8)
- Arterial Line Arterial LineDocument13 pagesArterial Line Arterial LineLinamaria Lozano100% (1)
- Sepsis and Septic ShockDocument70 pagesSepsis and Septic ShockLily SolNo ratings yet
- Chronic Obstructive Pulmonary DiseaseFrom EverandChronic Obstructive Pulmonary DiseaseRobert A. StockleyNo ratings yet
- Ultrasonography of the Lung: Understanding the BLUE, FALLS and SESAME ProtocolsDocument12 pagesUltrasonography of the Lung: Understanding the BLUE, FALLS and SESAME ProtocolsMauricio Tapia100% (1)
- Unstable Angina, STEMI, NSTEMI Diagnosis and ManagementDocument21 pagesUnstable Angina, STEMI, NSTEMI Diagnosis and ManagementNabil Mosharraf Hossain100% (2)
- Recent TB Treatment GuidelinesDocument28 pagesRecent TB Treatment GuidelinesDr venkatesh jalluNo ratings yet
- 9D NLBA Illustrated Glossary 2015Document141 pages9D NLBA Illustrated Glossary 2015galante81No ratings yet
- Refractory Septic ShockDocument5 pagesRefractory Septic ShockBrian Antonio Veramatos LopezNo ratings yet
- BLUE-Protocol and FALLS-Protocol: Two Applications of Lung Ultrasound in The Critically IllDocument12 pagesBLUE-Protocol and FALLS-Protocol: Two Applications of Lung Ultrasound in The Critically IllChristiaan CordovaNo ratings yet
- An Assignment ON: Bronchial HygieneDocument12 pagesAn Assignment ON: Bronchial Hygienesoniya joseph100% (1)
- Pulmonary SequestrationDocument15 pagesPulmonary SequestrationEmily EresumaNo ratings yet
- IntroductionDocument13 pagesIntroductionSiyara AntonyNo ratings yet
- DO /VO Relationships: J. L. VincentDocument8 pagesDO /VO Relationships: J. L. VincentLucas Cárcamo SaavedraNo ratings yet
- Clinical Case Study Guide - Cardiopulmonary Physical Therapy 3ed PDFDocument245 pagesClinical Case Study Guide - Cardiopulmonary Physical Therapy 3ed PDFraquelbibi0% (1)
- Pneumonia Management ProtocolDocument2 pagesPneumonia Management Protocolsky nuts100% (1)
- Suctioning Artificial Airways - AdultsDocument27 pagesSuctioning Artificial Airways - AdultssdaNo ratings yet
- CABG Case Study ReportDocument83 pagesCABG Case Study ReportSherena NicolasNo ratings yet
- Heart FailureDocument6 pagesHeart FailureNatasha MarksNo ratings yet
- Atrial Fibrillation: Discussed by - DR Kunwar Sidharth SaurabhDocument45 pagesAtrial Fibrillation: Discussed by - DR Kunwar Sidharth SaurabhKunwar Sidharth SaurabhNo ratings yet
- Epid COPDDocument9 pagesEpid COPDAgung WistaraNo ratings yet
- Anesthesia for Congenital Heart DiseaseFrom EverandAnesthesia for Congenital Heart DiseaseStephen A. StayerNo ratings yet
- Abdominal TuberculosisDocument28 pagesAbdominal TuberculosisNajezita Sachenka CH CNo ratings yet
- A Prospective Study of Prescribing Pattern in The Management of Stroke at A Tertiary Care HospitalDocument6 pagesA Prospective Study of Prescribing Pattern in The Management of Stroke at A Tertiary Care HospitalInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Clinical ECG RoundsDocument2 pagesClinical ECG RoundsKai Siang ChanNo ratings yet
- Abdominal TuberculosisDocument35 pagesAbdominal TuberculosisAWw LieyaNo ratings yet
- CNS Tuberculosis Pathogenesis, Diagnosis and TreatmentDocument19 pagesCNS Tuberculosis Pathogenesis, Diagnosis and TreatmentFabricio NuñezNo ratings yet
- Ventricular Septal DefectsDocument7 pagesVentricular Septal DefectsMuhammadAldoGiansyahNo ratings yet
- End-Stage Heart Disease Management and Palliative Care GuidelinesDocument44 pagesEnd-Stage Heart Disease Management and Palliative Care GuidelinesCyrille AgnesNo ratings yet
- Left-Sided Congestive Heart Failure Case PresentationDocument64 pagesLeft-Sided Congestive Heart Failure Case PresentationNicole Villanueva, BSN - Level 3ANo ratings yet
- Pulmonary HypertensionDocument9 pagesPulmonary HypertensionDesriani Anisa YakubNo ratings yet
- Lung Protective Mechanical Ventilation StrategiesDocument4 pagesLung Protective Mechanical Ventilation StrategiesAnne Julia AgustinNo ratings yet
- Ventilator-Associated Pneumonia Prevention: We Still Have A Long Way To Go!Document2 pagesVentilator-Associated Pneumonia Prevention: We Still Have A Long Way To Go!AzmachamberAzmacareNo ratings yet
- DR Sandeep - EISENMENGER SYNDROMEDocument81 pagesDR Sandeep - EISENMENGER SYNDROMEAlexandrescuNo ratings yet
- Drug Compliance Among Hypertensive PatientsDocument5 pagesDrug Compliance Among Hypertensive PatientsSyifa MunawarahNo ratings yet
- Anti T.B DrugsDocument120 pagesAnti T.B DrugsromalaramNo ratings yet
- Disorders of AortaDocument25 pagesDisorders of Aortavani reddyNo ratings yet
- Scape Vs FospeDocument5 pagesScape Vs FospeDr. FarhanNo ratings yet
- Cardiogenic ShockDocument6 pagesCardiogenic ShockhamadaelgenNo ratings yet
- Causes, Symptoms and Nursing Care of AtherosclerosisDocument16 pagesCauses, Symptoms and Nursing Care of AtherosclerosisSAZZY ASHLEY GADDANGNo ratings yet
- Primer On Clinical Acid-Base Problem Solving - DisAMon 2004Document41 pagesPrimer On Clinical Acid-Base Problem Solving - DisAMon 2004Ashley100% (1)
- Primary and Secondary CV Prevention - Iman EvanDocument104 pagesPrimary and Secondary CV Prevention - Iman EvanFikriYTNo ratings yet
- Acute Respiratory Distress SyndromeDocument30 pagesAcute Respiratory Distress SyndromeNikhil GhubadeNo ratings yet
- Tetralogy of FallotDocument24 pagesTetralogy of FallotjustinahorroNo ratings yet
- 2015 Chest - Blue & Falls ProtocolsDocument12 pages2015 Chest - Blue & Falls ProtocolsWilmer Yanquen VillarrealNo ratings yet
- Definition, Classification, Etiology, and Pathophysiology of Shock in Adults - UpToDateDocument16 pagesDefinition, Classification, Etiology, and Pathophysiology of Shock in Adults - UpToDatevara prasadNo ratings yet
- Pathophysiology of Cardiogenic Pulmonary EdemaDocument13 pagesPathophysiology of Cardiogenic Pulmonary EdemaIrina DuceacNo ratings yet
- Initial Assessment and Management of Acute StrokeDocument49 pagesInitial Assessment and Management of Acute StrokeIrina DuceacNo ratings yet
- Clostridioides Difficile Infection in AdultsDocument28 pagesClostridioides Difficile Infection in AdultsIrina DuceacNo ratings yet
- AdrenalineDocument6 pagesAdrenalineIrina DuceacNo ratings yet
- Acute Pulmonary OdemaDocument9 pagesAcute Pulmonary OdemaAnonymous ysrxggk21cNo ratings yet
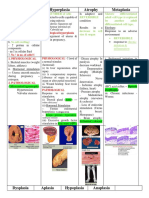
- Hypertrophy Hyperplasia Atrophy MetaplasiaDocument20 pagesHypertrophy Hyperplasia Atrophy MetaplasiaYunQingTanNo ratings yet
- Arterial HyperemyDocument10 pagesArterial HyperemyRohit NaiduNo ratings yet
- Int Endodontic J - 2020 - Zhan - Dental Nerves A Neglected Mediator of PulpitisDocument15 pagesInt Endodontic J - 2020 - Zhan - Dental Nerves A Neglected Mediator of PulpitisDevin KwanNo ratings yet
- Cerebral Perfusion Simulation Using Realistically Generated Synthetic TreesDocument9 pagesCerebral Perfusion Simulation Using Realistically Generated Synthetic Treessunhao13287710014No ratings yet
- Circulatory System REVIEWERDocument6 pagesCirculatory System REVIEWERClyde BaltazarNo ratings yet
- Sindrom Multiple Disfungsi OrganDocument8 pagesSindrom Multiple Disfungsi OrganAdi Nugroho MelyanaNo ratings yet
- Lecture 6 Cardiovascular: Vascular System - The HemodynamicsDocument61 pagesLecture 6 Cardiovascular: Vascular System - The HemodynamicsAndreea ŞtefănescuNo ratings yet
- PubMed Links 20171119Document2 pagesPubMed Links 20171119Scott BermanNo ratings yet
- Cvs BdsDocument142 pagesCvs BdsDr Dhiren Kumar PandaNo ratings yet
- Relationship Between Endogenous Hydrogen Sulfide and Blood Stasis Syndrome Based On The Qi-Blood Theory of Chinese MedicineDocument6 pagesRelationship Between Endogenous Hydrogen Sulfide and Blood Stasis Syndrome Based On The Qi-Blood Theory of Chinese MedicineleonieNo ratings yet
- Human Anat 2 Year Volume 4Document122 pagesHuman Anat 2 Year Volume 4HARSHINI PANDIANNo ratings yet
- Gelofusine®: Stop Infusion andDocument2 pagesGelofusine®: Stop Infusion andRudy Arindra WijayaNo ratings yet
- Dry Cupping Therapy Reduces Cellulite in WomenDocument7 pagesDry Cupping Therapy Reduces Cellulite in WomenDorothee RosarioNo ratings yet
- Charny - Mathematical Models of Bioheat TransferDocument137 pagesCharny - Mathematical Models of Bioheat TransferMadalena PanNo ratings yet
- 2019 Raynaud's PhenomenonDocument21 pages2019 Raynaud's PhenomenonGerman Gustavo Salgado TapiaNo ratings yet
- 1b-Physio-1m-Cvs 4Document12 pages1b-Physio-1m-Cvs 4urvashi rao rajputNo ratings yet
- Acute Inflammation (Vascular Changes) - 1Document33 pagesAcute Inflammation (Vascular Changes) - 1Ramesh KumarNo ratings yet
- High performance BodyWave tanning and beauty machineDocument11 pagesHigh performance BodyWave tanning and beauty machinetranspotNo ratings yet
- Dermatitits StasisDocument11 pagesDermatitits StasisRiyan TjahyaNo ratings yet