Professional Documents
Culture Documents
Nefrotico Mi Favorito
Nefrotico Mi Favorito
Uploaded by
Cristobal Gomez HernandezOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nefrotico Mi Favorito
Nefrotico Mi Favorito
Uploaded by
Cristobal Gomez HernandezCopyright:
Available Formats
Seminar
Idiopathic nephrotic syndrome in children
Damien G Noone, Kazumoto Iijima, Rulan Parekh
The incidence of idiopathic nephrotic syndrome (NS) is 1∙15–16∙9 per 100 000 children, varying by ethnicity and Lancet 2018; 392: 61–74
region. The cause remains unknown but the pathogenesis of idiopathic NS is thought to involve immune Published Online
dysregulation, systemic circulating factors, or inherited structural abnormalities of the podocyte. Genetic risk is more June 14, 2018
http://dx.doi.org/10.1016/
commonly described among children with steroid-resistant disease. The mainstay of therapy is prednisone for the S0140-6736(18)30536-1
vast majority of patients who are steroid responsive; however, the disease can run a frequently relapsing course,
This online publication has been
necessitating the need for alternative immunosuppressive agents. Infection and venous thromboembolism are the corrected. The corrected version
main complications of NS with also increased risk of acute kidney injury. Prognosis in terms of long-term kidney first appeared at thelancet.com
outcome overall is excellent for steroid-responsive disease, and steroid resistance is an important determinant of on July 26, 2018
future risk of chronic or end-stage kidney disease. Department of Paediatrics,
University of Toronto, Toronto,
ON, Canada
Introduction might have minimal change or focal segmental (D G Noone MB BCh BAO,
Nephrotic syndrome (NS) is characterised by the triad of glomerulosclerosis (FSGS). Owing to the heterogeneity of Prof R Parekh MD); Division of
proteinuria, hypoalbuminaemia, and oedema (panel 1). SRNS, only 50% are at risk of progressing to ESRD in Nephrology, The Hospital for
Sick Children, Toronto, ON,
Many glomerular disorders in childhood present with 5 years; typically those children who do not achieve
Canada (D G Noone,
nephrotic syndrome, however, the vast majority are complete or partial remission.14 Long-term prognosis in Prof R Parekh); Department of
idiopathic NS, and the focus of this Seminar (panel 2). adults with paediatric onset NS is not well studied and Pediatrics, Kobe University
The precise cause of this common childhood disease would provide important information on risk for families. Graduate School of Medicine,
Kobe, Japan (K Iijima MD); Child
remains elusive despite substantial advances in our Standard definitions are established and highlighted in
Health Evaluative Sciences,
understanding of podocyte biology. Idiopathic NS can the 2012 Kidney Disease Initiatives: Global Outcomes Research Institute, Hospital for
be classified on the basis of response to steroid therapy, (KDIGO; panel 1).1 Sick Children, Toronto, ON,
pattern of relapse, histopathology, or by genetic Canada (Prof R Parekh);
mutations. Most simply, NS is categorised on the basis Clinical presentation University Health Network,
Toronto, ON, Canada
of clinical response to steroid therapy, as steroid Classically, a child presents with a history of progressive (Prof R Parekh); and Dalla Lana
sensitive (SS) or steroid resistant (SR). Although helpful oedema, initially periorbital and noticeable in the School of Public Health, and
for guiding therapy, this classification lends very little morning. There can be an antecedent infection, typically Health Policy, Management
and Evaluation, University of
understanding to disease mechanism. Idiopathic NS of the upper respiratory tract. Urine output is described Toronto, Toronto, ON, Canada
is best defined as a podocytopathy due to loss or as frothy or foamy. Abdominal pain is relatively common (R Parekh)
altered function of the podocytes, resulting in massive and, if accompanied by fever, could signify spontaneous Correspondence to:
proteinuria. bacterial peritonitis. Headache with accompanying Dr Rulan Parekh, The Hospital for
The mainstay of treatment for NS is corticosteroids neurological signs or irritability should raise the Sick Children, Toronto,
ON M5G 1X8, Canada
(steroids) with protocols largely based on seminal studies suspicion for cerebral venous sinus thrombosis. Clinical
rulan.parekh@sickkids.ca
from the International Study of Kidney Disease in investigations are summarised in panel 3.
Children and the Arbeitsgemeinschaft für Pädiatrische
Nephrologie.2,3 Steroid responsiveness and frequency Pathology
of relapses provide the best guide to therapy in Most children do not get a kidney biopsy at presentation.
idiopathic NS. The majority of children respond well to Historical studies have demonstrated that the most
steroids within 4 weeks (steroid-sensitive NS [SSNS]);
however, most will relapse, with approximately half
becoming frequent relapsers or steroid dependent.4,5 Search strategy and selection criteria
Although historically fewer than 10% of children We conducted a systematic literature search of published
with SSNS continue to have relapses in adulthood,3,6 literature using Cochrane, PubMed, Embase, and MEDLINE.
contemporary cohorts suggest higher proportions of Key search terms included “children”, “nephrotic
16∙4–42%. Frequency of relapses during childhood and syndrome”, “steroid sensitive nephrotic syndrome”, “steroid
the need for non-steroid immunosuppressants such as resistant nephrotic syndrome” and “focal segmental
cyclophosphamide or ciclosporin are predictive of active glomerulosclerosis”. The reference lists of all included
disease as young adults.7–-10 Among 287 children followed papers and review articles were also cross-referenced to
up for over 15 years, 85% achieved long-term remission.11 identify additional relevant studies. The search was not
Despite ongoing relapses, kidney outcomes remain limited by study design, year of publication, or language
excellent, with risk of progression to chronic kidney but precedence was given where possible to randomised
disease estimated to be less than 5% in those with SSNS controlled trials and studies from the last 5 years. The initial
at 10 years after diagnosis.12 In contrast, SRNS is search was done on Nov 29, 2015 and repeated on Dec 1,
associated with increased risk of progression to end-stage 2017 to update with the recent published clinical trials.
renal disease (ESRD).13 Children with SRNS on biopsy
www.thelancet.com Vol 392 July 7, 2018 61
Seminar
Panel 1: Relevant definitions in nephrotic syndrome1 Panel 2: Causes of non-idiopathic childhood nephrotic
syndrome (NS)
Nephrotic syndrome (NS)
Oedema with protein excretion >40 mg/m² per h or urine • Nephritic/nephrotic glomerular disorders
protein:creatinine ratio ≥2000 mg/g (≥200 mg/mmol) or • IgA nephropathy and Henoch–Schonlein purpura
>3+ proteinuria on dipstick with serum albumin <2∙5 g/dL • Membranoproliferative glomerulonephritis
(25 g/L) • Lupus nephritis
• Postinfectious glomerulonephritis
Remission
• Immune complex mediated glomerulopathy
Urine albumin trace or negative on dipstick or proteinuria
• C1q nephropathy
<4 mg/m² per h or urinary protein:creatinine ratio <200 mg/g
(20 mg/mmol) for 3 consecutive days • Thin basement membrane disease
Relapse • Membranous nephropathy
Urine albumin 3+ or 4+ or proteinuria >40 mg/m² per h or
• Sickle-cell nephropathy
urinary protein:creatinine ratio >200 mg/g (20 mg/mmol) for
3 consecutive days • Thrombotic microangiopathy
Frequently relapsing NS • Interstitial nephritis
≥2 relapses within 6 months of initial response or ≥4 in any
• Infections associated with NS
12 month period
• Hepatitis B and C
Steroid-dependent NS • HIV-1
2 consecutive relapses occurring while weaning to alternate • Malaria
day steroids or within 2 weeks of steroid discontinuation • Syphilis
• Toxoplasmosis
Steroid-resistant NS
• Varicella zoster
Persistent proteinuria despite 60 mg/m² or 2 mg/kg for
8 weeks, after ensuring no infection or non-adherence to • Drugs associated with NS
medication • Non-steroidal anti-inflammatory drugs
• Bisphosphonates
common pathological findings in childhood NS are • d-penicillamine
either classified as minimal change and termed • Heavy metals (mercury and gold)
minimal change disease (MCD) or FSGS.1 In minimal • Lithium
change, the glomeruli appear normal under light • Rifampicin
microscopy, with evidence of podocyte effacement by • Sulfasalazine
electron microscopy.17 Characteristic histology in FSGS • T-cell-related malignancy
is segmental sclerosis of affected glomeruli, with the • Hodgkin’s lymphoma
segment often adherent to Bowman’s capsule by • Thymoma
synechiae.18 • Leukaemia
Incidence
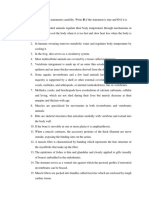
There is considerable variation in incidence of NS in south Asian children, FSGS is reported less
depending on country of origin, or ethnicity, with commonly and ranges from 15 to 39%.19
proportions ranging from 1∙15 to 16∙9 per
100 000 children (figure 1).11,19 Incidence is highest in Pathophysiology
those of south Asian ancestry compared to European Abnormalities in the podocyte and glomerular filtration
ancestry as reported in studies from the UK, barrier
South Africa, and Canada. Incidence of steroid- The podocyte is a polarised epithelial cell with inter
resistance ranges from 2∙1 to 27∙3% and also varies by digitating foot processes with a unique cell–cell junction
country of origin (figure 1).19 Most studies are known as the slit diaphragm. Along with the glomerular
retrospective or cross-sectional with only a few basement membrane and the fenestrated glomerular
longitudinal studies. Reported differences can thus be endothelium, the podocyte forms a trilayered structure—
partially attributable to management variations across the glomerular filtration barrier. The podocyte and
practices or regions, as well as use of differing filtration barrier allow an ultrafiltrate almost completely
definitions of outcomes. African–American children devoid of protein to pass into the Bowman’s space and
are more likely to have biopsy-proven FSGS (42–72%)19 proceed onto the proximal tubule. Podocyte architecture
and have the highest proportion of progression to is maintained by an extensive actin cyto skeleton that
ESRD as compared to European Americans,20 whereas enables the glomerular filtration barrier to withstand the
62 www.thelancet.com Vol 392 July 7, 2018
Seminar
Panel 3: Investigations in a child with nephrotic syndrome A
(NS) City, country Ethnicity (n)
New Zealand Multi-ethnic (n= 49)*
Baseline investigations Australia Not specified (n=135)
1 Urinalysis and urine microscopy The Netherlands Not specified (n=231)
2 Urine albumin or protein:creatinine ratio
Kentucky, USA Not specified (n=34)
3 24-h timed collection of urine for protein quantification
Benghazi, Libya Arabs (n=134)
4 Serum electrolytes, albumin, total protein, renal function,
Farwaniya/Jahra, Kuwait Arabs (n=55)
and cholesterol
Ohio, USA African-Americans (n=15)
Additional testing if there is a suspicion of a Whites (n=157)
glomerulonephritis Kansas City, USA African-Americans (n=25)
Europeans (n=54)
1 Serum complement C3 and C4 concentrations
Erie county, USA Whites (n=9)
2 Serum immunoglobulins
Non-whites (n=73)
3 Antistreptolysin titres
Birmingham, UK Afro-Caribbeans (n=2)
4 Anti-DNAse B antibodies Europeans (n=15)
5 Antinuclear antigen antibodies Asians (n=27)
6 Anti-double-stranded DNA antibodies Former Yorkshire, UK Non-Asians (n=49)†
7 Anti-neutrophil cytoplasmic antibodies Asians (n=121)†
Leicestershire, UK Non-Asians (n=22)
Infectious work-up depending on clinical context Asians (n=21)
1 Hepatitis B and C, HIV, syphilis, or tuberculosis can also be Toronto, Canada East/Southeast Asians (n=69)
considered depending on the clinical context South Asians (n=237)
Europeans (n=173)
Consideration of genetic testing Others (n= 232)
1 A positive family history of NS 0 2 4 6 8 10 12 14 16 18
2 Congenital NS Incidence‡ (per 100 000 people)
3 Infantile onset (<1 year)
4 Failure to respond to steroid therapy B
Steroid resistant Steroid sensitive
5 Persistent kidney dysfunction
City, country Ethnicity (total n, SR%)§
6 Features suggestive of a known syndrome (appendix)15
New Zealand Multi-ethnic (n=49, 19·6%)
Renal biopsy considered in the following situations Durban, South Africa Black and Indian (n=816, 27·3%)
1 Age <1 or >12 years
Diyarbakir, Turkey Turkish (n=138, 13·2%)
2 Persistent or sustained elevation in creatinine
Sindh, Pakistan Pakistani (n=538, 31·1%)
3 Significant haematuria or gross haematuria16
Siem Reap, Cambodia Cambodian (n=112, 6·2%)
4 Hypocomplementaemia
Poland Polish (n=178, 24·7%)
5 Findings indicative of another autoimmune disease
Boston and New York, European (n=65, 6·2%)
6 Infection with hepatitis B or C, HIV, or tuberculosis
USA Black and Hispanic
7 Hypertension (n=177, 15·3%)
8 Glucocorticoid resistance New Orleans, USA African-American (n=96, 11·0%)
Caucasian (n=103, 3·6%)
Toronto, Canada Others (n=232, 2·6%)
substantial capillary hydrostatic pressure. Loss of normal East/Southeast Asians
podocyte structure, the foot processes or the slit (n=66, 4·5%)
diaphragm that spans these interdigitations can lead to South Asians (n=237, 2·1%)
loss of albumin in the ultrafiltrate. Podocytes are Europeans (n=173, 6·8%)
terminally differentiated cells with minimal regeneration 0 10 20 30 40 50 60 70 80 90 100
and thus, vulnerable to injury. %
Complete effacement of the podocyte with the loss of
Figure 1: Incidence of childhood nephrotic syndrome per 100 000 persons by ethnicity, reported from
normal architecture results in massive proteinuria, a 1946 to 2014 (A) and variability of steroid responsiveness by ethnicity among children with nephrotic
hallmark of nephrotic syndrome (figure 2). The syndrome in reported studies from 1986 to 2014 (B)
pathogenesis leading to podocyte effacement is not clear Published with permission from Ethnic differences in childhood nephrotic syndrome, published in Frontiers in
Pediatrics, 2016.19 n=total number of patients; SR%=proportion of steroid resistance. *New Zealand European,
in idiopathic NS, nor the specific mechanism in
Maori, Pacific Island, Asian, Other. †Only those with steroid-sensitive nephrotic syndrome. ‡Estimated on the basis
which treatment with steroids leads to the recovery of of data in published studies.
podocyte structure and function. Systemic factors,
immune mediated or circulating, can contribute to familial forms of nephrotic syndrome underscores
podocyte effacement, but there is no single uni the importance of genetic variants leading to specific
fying hypo thesis. Supporting evidence from rare or podocyte abnormalities.
www.thelancet.com Vol 392 July 7, 2018 63
Seminar
Congenital and steroid-resistant forms of NS are podocyte structure and function is dependent on
associated with mutations in genes encoding com the molecular interplay between the network of
ponents of the slit diaphragm, podocyte actin cyto proteins that anchor the podocyte to the glom
skeleton, podocyte mitochondrial proteins, lysosomal erular basement membrane and maintain its unique
proteins, nuclear transcription factors, and glomerular structure, and also the crosstalk with the fenestrated
basement membrane (figure 2).21 Maintenance of glomerular endothelium. Thus, any injury to the
Figure 2: The glomerular
filtration barrier and
pathogenesis of idiopathic Glomerular filtration barrier in nephrotic syndrome
nephrotic syndrome Kidney Nephron Glomerulus
Within the kidney is the
glomerulus, a capillary tuft that
filters the blood. The podocyte,
glomerular basement
Glomerular
membrane and the fenestrated filtrate
glomerular endothelium
comprise the glomerular
filtration barrier allowing the
ultrafiltrate to enter the urinary Afferent
space. The podocyte has capillary
extensive cellular extensions
that interdigitate and these Efferent
capillary
foot processes are connected by
the slit diaphragm. In nephrotic
syndrome, there is extensive Normal Nephrotic syndrome
effacement of the podocytes Pathogenesis
and loss of this barrier to (a) Immune-mediated
protein, allowing excessive (b) Systemic circulating factors (eg, suPAR)
serum albumin to leak into the (c) Podocyte related factors (eg, ANGPTL4)
urine. The pathogenesis of (d) Genetic variants
idiopathic nephrotic syndrome
Mutant proteins play roles in:
is hypothesised to be either
immune-mediated, owing to a 1 Nucleus 4 Actin
systemic podocyte-derived Urinary space 2 Mitochondria 5 Slit diaphragm
circulating factor, or, in rarer or
familial forms, a genetic variant. 3 Lysosomes 6 Basement membrane
Numerous mutations are Podocyte
associated with steroid- cell body
resistant nephrotic syndrome
that affect various parts of the
podocyte itself, or the other 1
constituents of the glomerular 3
basement membrane. These
include mutations affecting
the podocyte nucleus, 4
mitochondria or lysosomes, the 2
slit diaphragm or actin
cytoskeleton, and the
Slit diaphragm 5
glomerular basement
membrane. Nephrin, podocin,
and CD2AP, for example, are
essential components of a
zipper-like structure spanning
the interdigitating foot Podocyte
processes of the podocyte, the effacement
slit diaphragm and link directly
with the podocyte actin
cytoskeleton. The actin
cytoskeleton is further Red White
supported by microfilaments Basement blood cell blood cell
6
membrane
that maintain structural
stability and facilitate the
dynamic nature of the podocyte
structure and function. The
importance of these Fenestrated
microfilaments is evident as endothelial
mutations in both α-actinin 4 cells
and INF2, which are involved in
actin regulation and
polymerisation lead to FSGS.
64 www.thelancet.com Vol 392 July 7, 2018
Seminar
podocyte has implications for the entire glomerular proteinuria, through an effect on either the glomerular
filtration barrier.22 basement membrane or the endothelial cells, and by
affecting the charge of the glomerular filtration barrier,
Immune mediated which prevents albumin from traversing the barrier. In
It is suspected that dysfunction or dysregulation of contrast, a sialylated form is released into circulation
T lymphocytes are involved in the pathogenesis of NS from other tissues and can mitigate proteinuria by
(figure 2).23–25 Supportive evidence includes the efficacy of binding αvβ5 integrins on the glomerular endothelium.
immunosuppressive agents in NS, spontaneous NS Exploration of how sialylated ANGPTL4 could be used to
remission following infection with measles,24 and the treat NS is ongoing, however, off-target effects, such
resolution of NS following chemotherapy for Hodgkin’s as inhibition of lipoprotein lipase leading to hyper
and other T-cell lymphomas, which can trigger or precede triglyceridaemia in NS, could be exacerbated.32
NS.25 Lastly, development of NS after allergic reactions
to various stings and poisons suggests an immune- Genetics
mediated role in disease pathogenesis. Genetic risk and SSNS
A recent molecular candidate for the cause of A genetic locus on chromosome 6p and single
podocytopathies and proteinuric states is CD80 (B7-1). nucleotide polymorphisms in HLA-DQA1 and HLA-
CD80, is a protein expressed on antigen-presenting cells DQB1 were substantially associated with SSNS using an
that provides the primary co-stimulatory signal for T-cell exome array.36 This locus, however, only explains
activation via receptors on the T-cell surface. The T-cell 4∙6% of the genetic risk for SSNS.36 A common finding
surface expresses protein receptor CTLA-4, which binds from genome-wide association studies of glom
CD80. An increase in podocyte B7-1 expression is erular diseases is the significant association with
evident in a variety of animal models of proteinuria and polymorphisms from the major histocompatibility
in human studies.26 This hypothesis was further tested complex. It is not clear whether the HLA loci are
through the CTLA-4 mimicking therapeutic agents, causal, given the commonality among glomerular
abatacept and belatacept in FSGS, but remains studies, or it reflects the allele frequency by specific
controversial and clinical trials are under way.27,28 ethnicity studied.36
Systemic circulating factors Genetics and SRNS
A circulating glomerular permeability factor has been Identifying genetic causes for children with SRNS early in
hypothesised to cause NS, however, defining a single their course could allow discontinuation of immuno
putative factor remains elusive. The majority of studies suppressive agents, aid in transplant management, and
favour a circulating factor in SRNS or FSGS (figure 2). provide information for prenatal counselling. Con
A few studies demonstrate proof of a blood-derived firmation of a genetic defect generally implies a reduced
glomerular permeability factor. For example, serum risk of recurrence afer transplantation, as it is likely
from patients with FSGS in pre-clinical and ex-vivo a kidney-specific disease. De novo auto-immune-mediated
studies induced proteinuria or increased permeability of NS can develop in the transplanted kidney owing to
glomeruli to albumin.29 There was also successful neoantigens,37 especially among children with NPHS1
treatment of recurrent FSGS after kidney transplantation (nephrin) mutations.38 Depending on the age of onset of
with immunoadsorption. Finally, maternal transmission SRNS, the likelihood of defining a monogenic cause
of FSGS confirmed a circulating factor.30 There are num decreases as children age. Mutations in key podocyte
erous factors proposed including heparanase, haemo genes such as NPHS1, NPHS2, LAMB2, or WT1 explain
pexin, angiopoietin-like 4 (ANGPTL4), cardiotrophin-like 69–85% of cases of NS presenting in the first 3 months of
cytokine-1 and, more recently, soluble urokinase plasmino life and 50–66% of NS cases presenting between 4 and
gen activator receptor (suPAR).31–33 These factors might 12 months.39,40 After 1 year of age, the chance of identifying
impact glomerular permeability, possibly through effects a genetic cause for SRNS decreases substantially to
on the endothelial cell or podocyte. 25% between the ages of 1 and 6 years, 18% between 7 and
suPAR affects the podocyte actin cytoskeleton via an 12 years, and as low as 11% in those aged 13–18 years.39 In
interaction with αvβ3-integrin receptor on the surface of an international registry of over 1340 children with SRNS
podocytes. Increased suPAR con centrations were over 1 year of age, approximately 14% had a genetic
originally described in FSGS;34 however, suPAR as a mutation.41 Over 30 genes are reported to be associated
circulating factor has been refuted since concentrations with SRNS or FSGS, and the list is expected to expand
vary by kidney function, there is an absence of specificity (appendix). Mutations in the mitochondrial genes involved See Online for appendix
for FSGS, and findings are not easily reproducible.35 in biosynthesis of coenzyme Q10 leading to deficiency,
Two distinct forms of ANGPTL4, a glycoprotein and occur in 1% of cases of familial SRNS.39 Coenzyme Q10 is
acute phase reactant expressed in adipose tissue, the an antioxidant and an essential component of the electron
heart, and skeletal muscle, are elevated in NS.32 A hypo chain and, most importantly, supplementation can be
sialylated form secreted from podocytes can lead to effective for mitochondrial podocytopathies—a potentially
www.thelancet.com Vol 392 July 7, 2018 65
Seminar
curative therapy. High-throughput next generation DNA is with low-molecular-weight heparin. There is in
sequencing from patients with sporadic FSGS, targeting sufficient evidence to warrant universal thrombosis
all known podocyte genes, might identify other FSGS prophylaxis in childhood NS.50
susceptibility genes.42
Acute kidney injury (AKI)
Complications of nephrotic syndrome AKI, an underappreciated complication, is now recognised
Infection as the third most important complication in children
Infection is the leading cause of morbidity and, treated in hospital with NS.53 Recently, a multicentre study
historically, mortality in children with NS.43 NS is from the USA reported that 58∙6% of 336 children
associated with low concentrations of immunoglobulin admitted to hospital for NS had evidence of AKI with
G (IgG) from urinary loss and altered production, which identified risk factors such as concomitant infections, use
contributes to infection risk. Loss of complement can of nephrotoxic medications and SRNS.53 The use of
also predispose to infection risk. Spontaneous bacterial diuretics in a child with haemoconcentration and intra
peritonitis, especially by Streptococcus pneumoniae, vascular volume depletion might predispose to AKI. Renal
remains a serious complication of NS, and a low serum vein thrombosis, acute tubular necrosis in the setting of
albumin (<15 g/L or 1∙5 g/dL) is associated with hypovolaemia and sepsis, and interstitial nephritis in
increased risk of peritonitis.44 Routine antibiotic duced by non-steroidal anti-inflammatory drugs or
prophylaxis for prevention of spontaneous bacterial antibiotics are also recognised contributors to AKI.
peritonitis in children with active NS is generally not
recommended owing to scarcity of evidence, although Dyslipidaemia
some centres could opt for prophylaxis in children with NS is associated with substantial abnormalities in lipid
a history of peritonitis.45 Pneumococcal vaccination can metabolism, leading to hypercholesterolaemia, hyper
successfully be given to children with NS, even when triglyceridaemia, and various other lipoprotein abnor
on steroid therapy, and is recommended by the malities. Lipid abnormalities are primarily related to
Children’s Nephrotic Syndrome Consensus Con urinary losses of key transport proteins including
ference.46,47 Children with NS are also at risk of albumin, which carries free cholesterol, and also a com
developing pneumonia from Streptococcus pneumoniae, pensatory increase in proteins involved in triglyceride
Haemophilus influenzae, Staphylococcus aureus, and metabolism.54 It is unknown whether altered lipid
cellulitis, caused by Staphylococci, group A Streptococci, metabolism confers long-term cardiovascular risk from
and H influenzae species.45 atherosclerosis in children with NS. The use of lipid-
Varicella-zoster infection poses a substantial risk to lowering agents for the dyslipidaemia in NS is not advised,
children with NS. The vaccine is a weakened form of unless there is substantial persistent proteinuria with
the virus, which is typically best avoided in immuno extremely high levels of hypertriglyceridaemia. The
compromised children. It appears to be safe, however, evidence of benefit is not clear and side-effects such as
for children who are in remission or who are on liver dysfunction, risk of rhabdomyolysis, and delayed
low-dose alternate-day steroids, an optimised, two-dose growth and development although rare are not in
vaccination schedule has been developed.48 Prophylactic substantial.55 If statins are initiated, it is only recommended
varicella-zoster immune globulin (VZIG) is rec for children over the age of 10 years with monitoring of
ommended for exposure to chickenpox. VZIG should liver function and creatinine kinase prior to initiating
be given as soon as possible but can be given up to therapy and after 4 weeks.56
10 days after exposure. Therapeutic intravenous
aciclovir could also be effective in NS, however, data are Management
scarce and extrapolated from solid organ transplant Oedema in nephrotic syndrome
ation reports.49 Based on the pathogenesis of oedema in NS, one of the
primary strategies in the management of oedema is salt
Venous thromboembolism and fluid restriction with addition of a loop diuretic for
NS is a well recognised hypercoagulable state in severe or symptomatic oedema.57 The addition of an
which children are at risk of venous thrombo albumin infusion, typically in combination with a loop
embolism (VTE) including cerebral sinus venous throm diuretic, is sometimes employed to induce diuresis and
bosis, pulmonary embolism, and renal vein thrombosis.50 natriuresis, especially if signs of intravascular underfilling
VTE complicates an estimated 3% of cases of NS during or severe oedema are present. Response to diuretics alone
childhood.50,51 The pathophysiology of VTE in NS is multi might be blunted, especially in an underfilled state, where
factorial resulting from abnormalities in platelet aggre there is activation of neurohormonal systems in an attempt
gation, increased synthesis of prothrombotic factors to maintain intravascular volume. Furthermore, furo
(factors V and VIII), urinary loss of anticoagulant semide is highly protein bound and, in a hypoalbuminaemic
proteins (antithrombin III, protein C and S), altered state, the volume of distribution substantially increases
fibrinolysis, and intravascular fluid depletion.52 Treatment with less drug available to reach the proximal tubule for
66 www.thelancet.com Vol 392 July 7, 2018
Seminar
secretion into the urinary space. The combined use of
FRNS
albumin and furosemide remains controversial. Many or SDNS Low dose
studies involved small numbers of patients, were largely alternate day
steroids
uncontrolled, and, in most, only a small benefit of diuresis, SSNS
Ongoing relapses
Infrequent
natriuresis, and weight loss were observed with the relapses or steroid toxicity
combination of furosemide and albumin over furosemide Cyclophosphamide
alone. Approximately 25% of children with NS might or levamisole
actually be hypovolaemic at presentation, as assessed by Long-term
Ongoing relapses
Steroids or steroid toxicity
clinical, laboratory, and echocardiographic parameters.58 remission
Biopsy every
Diuretics alone might aggravate hypovolaemia and 2–3 years Tacrolimus or
mycophenolate mofetil
intravascular depletion, thus, the use of albumin could be
warranted. Care should be taken with the administration No response after Ongoing relapses
8 weeks of steroids Biopsy every or steroid toxicity
of albumin in children who are not exhibiting signs of 2–3 years
SRNS Rituximab ± other
hypovolaemia, as the resultant expansion in intravascular
immunosuppressants
fluid could precipitate pulmonary oedema.57
Tacrolimus
Management of nephrotic syndrome Genetic cause
No response
Standardising management of NS has been hampered confirmed ACE inhibitor
ARB
by the paucity of high-quality trial evidence supporting
international guidelines. This lack of evidence has
Progression over time to ESRD
resulted in substantial variation in care based on
physicians’ preference, drug availability by country, and Figure 3: Principal treatments for nephrotic syndrome at diagnosis and follow-up
interpretation of the sparse trial data. Substantial After initial therapy with steroids, children are classified as having SSNS or SRNS after at least 8 weeks of therapy.
physician variability in choice of steroid-sparing agents Frequently relapsing SSNS can first be treated with low-dose alternate-day steroids prior to consideration of
steroid-sparing agents. Typically, the steroid-sparing agents include cyclophosphamide, or levamisole, and if this fails
for children with NS is described in Europe, Canada, and the child continues to relapse or is steroid dependent, then a calcineurin inhibitor is often the next agent, or
and the USA.59,60 In the following section, we outline the mycophenolate mofetil. The scarcity of trial evidence has resulted in substantial variation in choice of steroid-sparing
principal treatments for NS (figure 3). Certain agents, agents based on physicians’ preference, drug availability by country, and cost. SSNS=steroid sensitive nephrotic
such as mizoribine, or chlorambucil with restricted syndrome. SRNS=steroid resistant nephrotic syndrome. FRNS=frequently relapsing nephrotic syndrome.
SDNS=steroid dependent nephrotic syndrome. ACE=angiotensin converting enzyme inhibitor. ARB=angiotensin
availability are not discussed in detail.1 Baseline and receptor blocker.
additional investigations, as well as considerations
for genetic testing and renal biopsy are presented and require steroids into adulthood, osteo porosis and
in panel 3. being overweight cause substantial morbidity.9
Initial therapy Treatment of frequently relapsing nephrotic syndrome
Standard therapy is at least 4–6 weeks of steroids each (FRNS) or steroid-dependent nephrotic syndrome
day (prednisone or prednisolone), followed by a mini (SDNS)
mum of 6 weeks of alternate day therapy based on For relapses of SSNS, the efficacy of steroids is not in
evidence from clinical trials.1 Many published protocols doubt; however, tapering schedules remains controversial,
by guideline, centre, or country highlight the variability as data are scarce.1,64 KDIGO recommends a tailored
in the prednisone taper (table). approach to steroid therapy depending on whether
Until recently, a Cochrane review strongly suggested that children relapse either infrequently or frequently (table).1
6 months of therapy was superior to 2–3 months, owing to
a substantial reduction in relapses after initial presentation Triggers of relapse
of NS. The meta-analysis of randomised controlled trials Additional factors triggering relapses include allergies and
(RCTs) involved over 700 children.64 Since 2013, three RCTs infection. Treatment for allergies with dietary restrictions,
demonstrated that extending treatment to 6 months skin desensitisation, mast cell stabilisers such as disodium
compared with 2–3 months did not reduce the risk cromoglycate demonstrate little benefit in preventing
of relapse, the development of frequent relapses, or relapsing disease.69 On the contrary, several trials suggest
steroid dependence and the eventual need for an add- that relapses might be reduced if prednisolone is
itional immunosuppressive agent.65–67 Thus, treatment administered daily for 5–7 days at the onset of upper
with steroids for 6 months is no longer recommended.68 respiratory tract infection in FRNS or SDNS. Although
Chronic steroid use is associated with many side-effects studies have a high risk of bias owing to small sample
including obesity, cushingoid features, striae, ocular sizes and variability in study design, treatment is still
complications, such as cataracts and glaucoma, metabolic recommended by the KDIGO guide lines.1,70–72 A large,
features, musculoskeletal features, such as osteoporosis placebo-controlled, multicentre trial of 300 children in the
and avascular necrosis of the head of the femur, and UK (PREDNOS 2) will clarify the effectiveness and safety
behavioural features. In those that continue to relapse of this approach when completed.73
www.thelancet.com Vol 392 July 7, 2018 67
Seminar
International Arbeitsgemeinschaft Haute Autorité de Santé Italian Society for KDIGO Glomerulonephritis Hospital for Sick Children
Study of Kidney für Pädiatrische (France)62 Pediatric Nephrology Guidelines1 (Toronto, Canada)11
Disease in Children Nephrologie (APN)2 (SINePe)63
(ISKDC)61
Year of 1970 1988 2008 2017 2012 2016
publication
Initial presentation
Initial dose 60 mg/m² per 60 mg/m² per 60 mg/m² per day × 4 weeks 60 mg/m² per 60 mg/m² per day or 2 mg/kg 60 mg/m² per day × 6 weeks
and day × 4 weeks day × 6 weeks (maximUm (maximum dose 60 mg) day × 6 weeks per day × 4–6 weeks (maximum (maximum 60 mg in single
duration dose 80 mg) (maximum 60 mg in 60 mg) morning dose)
single or 2 divided
doses)
Subsequent 4 weeks of 40 mg/m² per 60 mg/m² per alternate 40 mg/m² per 40 mg/m² per alternate day or 40 mg/m² per alternate
dose and 40 mg/m² alternate day × 6 weeks day × 8 weeks (maximum 60 mg) alternate day × 6 weeks 1∙5 mg/kg/alternate day day × 6 weeks
tapering per alternate day but (maximum dose 60 mg) followed by a 15 mg/m² per (single dose; maximum (maximum 40 mg ) × 6–8 weeks (maximum 60 mg), 30 mg/m²
given on alternate day × 15 days and 40 mg) without (at least 12 weeks) and per alternate day × 8 days
3 consecutive days continue to wean. In addition, tapering continued for 2–5 months with (maximum 30 mg), 20 mg/m²
out of a week 3 methylprednisolone pulses if tapering per alternate day × 8 days
proteinuria persists after 1 month (maximum 20 mg), 10 mg/m²
of daily prednisone therapy per alternate day × 12 days
(maximum 10 mg)
Relapses
Starting ·· ·· 60 mg/m² per day until urine 60 mg/m² (max 60 mg 60 mg/m² per day or 2∙0 mg/kg 60 mg/m² per day until urinary
dose and protein is negative for 6 days in a single or 2 divided per day (maximum of protein is trace or negative for
duration doses) until urine 60 mg/day) until urine is 5 consecutive days
protein is negative for negative for 3 days
5 days
Follow-up ·· ·· 60 mg/m² per alternate 40 mg/m² per 40 mg/m² or 1∙5 mg/kg/ 60 mg/m² per alternate
dose and day × 4 weeks, 45 mg/m² per alternate day (max alternate day (maximum day × 8 days (maximum
duration alternate day × 4 weeks, 40 mg) × 4 weeks 40 mg) × 4 weeks (minimum) 60 mg/day), 50 mg/m² per
30 mg/m² per alternate alternate day × 8 days
day × 4 weeks, 15 mg/m² per (maximum 50 mg/day),
alternate day × 4 weeks 40 mg/m² per alternate
day × 8 days (maximum
40 mg/day), 30 mg/m² per
alternate day × 8 days
(maximum 30 mg/day),
20 mg/m2/alternate
day × 8 days (maximum
20 mg/day), 10 mg/m2 per
alternate day × 8 days
(maximum 10 mg/day)
Frequent ·· ·· ·· ·· 60 mg/m2 per day or ··
relapses 2∙0 mg/kg per day (maximum of
60 mg/day) until urine is
negative for 3 days followed by
alternate-day prednisone for at
least 3 months; use the lowest
dose to maintain remission
without major adverse effects
and daily if alternate day is
ineffective
Table: Published protocols for steroid treatment (prednisone or prednisolone) for initial presentation of idiopathic nephrotic syndrome
Low-dose, alternate-day steroid medications and physician preferences greatly influence
In general, the first step in managing a child with choice of steroid-sparing medication (panel 4).59,60 We
frequent relapses is to maintain them on low-dose, provide the list of agents below based on the strength of
alternate-day steroid, typically at the lowest dose possible, evidence (figure 3).
or just above the steroid dose associated with the latest
relapse. Children could be treated with steroid-sparing Steroid-sparing agents
agents when low-dose alternative-day steroid therapy Levamisole, an antihelminthic agent, has immuno
fails or when severe adverse effects of steroids develop modulatory properties and a favourable side-effect profile.
(figure 3). The decision to choose steroid-sparing treat Levamisole reduced the risk of relapse compared with
ments should be based on drug efficacy, side-effects and placebo or no treatment.74,75 There was, however, con
the patient’s condition. Also, regional availability of siderable heterogeneity in study design described in a
68 www.thelancet.com Vol 392 July 7, 2018
Seminar
meta-analysis.76 An international, multicentre, double-
blind, placebo-controlled, RCT of levamisole in SSNS Panel 4: Steroid-sparing agents for frequently relapsing
found that 6% of patients on placebo versus 26% on nephrotic syndrome (FRNS) or steroid-dependent
levamisole were in remission at 1 year.103 nephrotic syndrome (SDNS)
Cyclophosphamide, the most commonly used steroid- Levamisole
sparing agent, is effective in multiple RCTs for the • Reduces risk of relapse compared with placebo or no
treatment of FRNS and SDNS.78–81 A Cochrane review treatment;74,75 there was, however, considerable
reported that cyclophosphamide substantially reduced heterogeneity in the meta-analysis76
the relapse risk at 6–12 months by 56% when compared
to prednisolone alone (relative risk [RR] 0∙44, 95% CI Cyclophosphamide
0∙26–0∙73).76 A meta-analysis reported that studies for • Effective for FRNS,76,77,79 but less so for steroid-dependent
non-steroid-dependent FRNS resulted in remission in nephrotic99 syndrome;43,79–81,82 however, there is overlap in
72% of patients after 2 years and 36% after 5 years, the classification
whereas the proportions for SDNS were 40% and 24%, Ciclosporin
respectively.43 Studies to date used various definitions • Effective for FRNS or SDNS,83–90 but many patients suffer
of response, which leads to hetereogeneity in re relapses after discontinuation of ciclosporin therapy
ported outcomes. (ciclosporin dependence)85,86,89–91
Important side-effects of cyclophosphamide include
gonadal dysfunction (azoospermia in boys), myelo Tacrolimus
suppression (leucopenia), infection, alopecia, haemor • Several case series suggest that tacrolimus is effective for
rhagic cystitis, and hepatic dysfunction. Meta-analyses FRNS or SDNS,92–96 but there are no randomised controlled
report that risk of azoospermia is higher in boys of trials
pubertal age (Tanner stage 2 or greater) or post-pubertal Mycophenolate mofetil
age, especially when the cumulative dose of cyclo • Less effective than ciclosporin,97,98 but has a favourable
phosphamide ranges from 100 to 300 mg/kg, but higher side-effect profile
doses could be safe in pre-pubertal boys.43,104 In NS,
substantially lower doses of cyclophosphamide are Rituximab
prescribed typically, 2–2∙5 mg/kg on average for • Rituximab and lower doses of prednisone and calcineurin
8–12 weeks, with a maximum daily dose of 100 mg and inhibitors are non-inferior to standard doses of these
only as a single course.1 The risk of female infertility is agents in maintaining short-term remission in children
documented to be lower than in boys, and a cumulative who show dependence on both drugs, and allow their
dose up to 200 mg/kg is reported safe105 as infertility temporary withdrawal99
occurred at a dose of 300 mg/kg or higher.104 Approxi • Effective for complicated FRNS or SDNS, but all children
mately 32% of NS patients developed leucopenia, during had relapses by 19 months after rituximab infusion100
cyclophosphamide therapy.43 Therefore, if the leucocyte • Non-inferior to steroids in maintaining remission in SDNS101
count drops below 4500 cells per μL, a lower dose could be Mizoribine
used or suspended if the leucocyte count falls below • Not effective for SDNS, but a subgroup analysis of
3000 cells per μL.43 Long-term studies with decades of children aged 10 years and younger demonstrated that
follow-up are needed to understand long-term risk of the proportion of patients who relapsed was substantially
cyclophosphamide. lower in the mizoribine group than the placebo group102
Calcineurin inhibitors
Ciclosporin is effective for both FRNS and SDNS.83–87 increasing risk after prolonged use of the drug for 2 years
Blood concentration of ciclosporin should be monitored, or more.106,107
usually by trough levels or C2 (at 2 h post-dose) levels, Tacrolimus could be considered when ciclosporin
and the dose should be adjusted within target cannot be used owing to cosmetic side-effects, including
levels (trough levels: 60–100 ng/mL; C2 levels: hypertrichosis and gingival hypertrophy. Both medi
300–700 ng/mL).83,84,88 There is, however, no international cations are now generic, thus cost should not be an issue.
consensus on target con centrations owing to incon Potential onset of diabetes and nephrotoxicity are
clusive evidence.1 In Japan, dose is adjusted to maintain important side-effects. No definitive dosing for tacro
trough concentrations within 80–100 ng/mL for the first limus is established, but it typically starts at 0∙1 mg/kg
6 months, and within 60–80 ng/mL for the next per day (range 0∙05–0∙2).97,98,108 Optimal trough con
18 months, and in North America, reported levels range centrations are not defined but ranges from 5 to 8 ng/mL
from 50 to 100 ng/ml.85,86,91 Additionally, the length of have been reported, and persistent levels greater
therapy is not well defined as children frequently than 8 ng/mL were associated with increased risk of
relapse after discontinuation of the drug (ciclosporin nephrotoxicity in a single study.93,94 Hypertension could
dependence).85,86,91 Nephrotoxicity is also problematic with also be worsened with calcineurin inhibitors and
www.thelancet.com Vol 392 July 7, 2018 69
Seminar
could potentiate the development of posterior reversible Rituximab is generally safe and well tolerated in most
encephalopathy syndrome.108 children; however, potentially serious adverse events
include persistent low B cell and failure to repopulate,
Mycophenolate mofetil (MMF) depletion of memory B cells , and a risk of hypo
Mycophenolate mofetil (MMF) is used as a steroid- gammaglobulinaemia, occasionally requiring infusions
sparing agent for FRNS or SDNS owing to the favourable of immunoglobulin. Rarer adverse events are also report
side-effect profile and absence of nephrotoxicity. ed, including fatal hepatitis induced by reactivation
Physician preference for MMF stems from the concerns of hepatitis B virus, progressive multifocal leuko
about the toxicity of cyclophosphamide and calcineurin encephalopathy, pulmonary fibrosis, fulminant myo
inhibitors; however, trial evidence is scarce. A randomised, carditis,111 pneumocystis pneumonia,112 immune-mediated
multicentre, open-label, crossover study comparing the ulcerative colitis, and agranulocytosis. Recently, hyper
efficacy and safety of a 1-year treatment with MMF or sensitivity reactions were reported with autoantibodies to
ciclosporin in 60 pediatric patients with FRNS, reported rituximab during the second course of rituximab.113
more relapses per patient per year with MMF than with Despite the benefit of rituximab, residual issues require
ciclosporin.96 Similar results were reported in another further study such as the total number of infusions,
multicentre RCT comparing the efficacy of MMF to that whether to redose every 6 months or base dose on
of ciclosporin in 24 children with FRNS and biopsy- repopulation of CD20 B cells. Importantly, we need to
proven MCD.98 A French study that employed Bayesian understand the long-term consequences of rituximab
techniques and probability in 23 children, found that therapy in children as treatment is considered earlier in
MMF could reduce the number of relapses and steroid disease course.
doses, suggesting use of MMF prior to cyclophosphamide
or ciclosporin.109 Recent studies demonstrate efficacy at Treatment for steroid-resistant nephrotic syndrome
higher doses, which are not routinely monitored and Identification of a podocyte gene defect is fundamental to
typically used in kidney transplantation. Maintaining an determining treatment response to steroids and calci
area under the curve for mycophenolic acid, assessed by neurin inhibitors as demonstrated in recent studies.114,115
pharmacokinetic studies higher than 45 mg × h per L, SRNS with no proven genetic mutation is expected to
might be associated with less frequent relapses.110 respond with complete remission in up to 60% of cases
and with partial remission in up to 19%.114,115 Furthermore,
Rituximab those with no genetic mutation have a substantial
Rituximab, a chimeric anti-CD20 monoclonal antibody, advantage in terms of kidney survival over 10 years, with
is effective and allows for discontinuation or reduction ESRD occurring in 71% of those with a genetic disease
of steroids and other steroid-sparing agents in NS. An versus 29% in those without.114
initial open-label RCT concluded that rituximab and Calcineurin inhibitors such as ciclosporin and tacro
lower doses of prednisone and calcineurin inhibitors are limus are recommended as initial therapy for children
non-inferior to standard therapy in maintaining short- with SRNS,1,116 with cumulative complete and partial
term remission.99 Findings were confirmed by a multi remission in ciclosporin treatment substantially better
centre, double-blind, randomised, placebo-controlled than placebo.117–119 Also, tacrolimus is similar to ciclosporin
trial that assessed efficacy and safety of rituximab versus in combination with low-dose steroids in inducing
placebo in 48 children with complicated FRNS or remission in patients with SRNS.120 Optimal duration of
SDNS.100 Those on rituximab received 375 mg/m² body calcineurin inhibitor therapy is still unknown, although
surface area (maximum 500 mg) once weekly for KDIGO guidelines recommended a minimum of
4 weeks, and the placebo group received placebo at 12 months,1 and in clinical practice, can be con
similar frequency. Prednisolone was gradually tapered tinued up to 24 months. Combination therapy in
after remission was achieved. Tapering of ciclosporin volving steroid pulse therapy and ciclosporin could be
was started on day 85, and discontinued by day 169. The considered effective in inducing remission of SRNS in
50% relapse-free period (267 vs 101 days; hazard ratio extreme cases.121,122
[HR] 0∙267, 95% CI 0∙135–0∙528, p<0∙0001), and the Two RCTs demonstrated a substantial reduction in
daily steroid dose was substantially lower in those on proteinuria with enalapril123 and fosinopril.105 KDIGO
rituximab than placebo (9∙12 [SD 5∙88] vs 20∙85 therefore recommended angiotensin-converting enzyme
[SD 9∙28] mg/m² per day, p<0∙0001) up to 1 year. In inhibitors or angiotensin II receptor blockers for children
follow-up, all children relapsed by 19 months, suggesting with SRNS.1
that the benefit of rituximab was not permanent. Re Cyclophosphamide has no benefit for SRNS.78,124 MMF
cently, rituximab was also shown to be non-inferior to use in the treatment of SRNS has been described and the
steroids in maintaining remission in patients with proportion of patients in remission is low.125–127 A recent
SDNS never exposed to a calcineurin inhibitor and who randomised trial of 138 children evaluated dexamethasone
had not received either MMF or cyclophosphamide in plus MMF as a therapy for patients with steroid-resistant
the preceding 6 months.101 FSGS versus ciclosporin, and found no significant
70 www.thelancet.com Vol 392 July 7, 2018
Seminar
difference in achieving partial or complete remission writing of the manuscript, and construction of the figures, panels, and
at 1 year; however, the trial was substantially under tables. All authors reviewed and approved the final version.
powered.128 Several case series suggested that rituximab is Declaration of interests
effective with refractory (failing to respond to calcineurin DGN declares no competing interests. KI has received grants from
Novartis Pharma, Japan Blood Product Organization, AbbVie,
inhibitors) SRNS; however, an open-label, randomised
JCR Pharmaceuticals, Daiichi Sankyo, Teijin Pharma, CSL Behring, Novo
trial of rituximab failed to demonstrate an improvement Nordisk Pharma, Air Water Medical, Astellas Pharma, Takeda
in 31 children with SRNS, compared to either 16 children Pharmaceutical, Taisho Toyama Pharmaceutical, Eisai, and Biofermin
who received calcineurin inhibitors, prednisolone, and Pharmaceutical, and lecture fees or consulting fees, or both from Zenyaku
Kogyo, Novartis Pharma, Chugai Pharmaceutical, Astellas Pharma,
two infusions of rituximab, or 15 children who received
Springer Japan, Meiji Seika Pharma, Asahi kasei Pharma Corporation,
calcineurin inhibitors and prednisolone alone.129 Medical Review, Nippon Boehringer Ingelheim, Baxter Limited, Ono
Pharmaceutical, Sanwa Kagaku Kenkyusho, Sanofi, Alexion Pharma, and
Controversies, uncertainties, and outstanding Kyowa Hakko Kirin. RP has received grants from Astellas Pharma.
research questions References
There are many remaining questions about NS and these 1 KDIGO clinical practice guideline for glomerulonephritis.
Kidney Int Suppl 2012; 2: 139–274.
can be grouped into understanding: (1) who develops NS 2 Nephrotic syndrome in children: prediction of histopathology from
and what is the cause?; (2) factors contributing to clinical and laboratory characteristics at time of diagnosis. A report of
interindividual variability in response to medications; the International Study of Kidney Disease in Children.
Kidney Int 1978; 13: 159–65.
and (3) specific triggers leading to relapsing disease. 3 Arbeitsgemeinschaft fur Padiatrische Nephrologie. Short versus
There are several controversies and uncertainties. What standard prednisone therapy for initial treatment of idiopathic
is the expected dose of calcineurin inhibitors that will nephrotic syndrome in children. Lancet 1988; 331: 380–83.
4 Koskimies O, Vilska J, Rapola J, Hallman N. Long-term outcome of
induce and maintain remission? When should we primary nephrotic syndrome. Arch Dis Child 1982; 57: 544–48.
discontinue calcineurin inhibitors in children who 5 Tarshish P, Tobin JN, Bernstein J, Edelmann CM Jr. Prognostic
maintain remission? What is the role of MMF and significance of the early course of minimal change nephrotic
rituximab? Well designed RCTs need to be conducted to syndrome: report of the International Study of Kidney Disease in
Children. J Am Soc Nephrol 1997; 8: 769–76.
clarify these uncertainties. Additionally, there is a need for 6 Trompeter RS, Lloyd BW, Hicks J, White RH, Cameron JS. Long-term
optimal trials to address novel treatments and tapering outcome for children with minimal-change nephrotic syndrome.
regimens, and follow-up studies to address potential long- Lancet 1985; 325: 368–70.
7 Ruth EM, Kemper MJ, Leumann EP, Laube GF, Neuhaus TJ.
term risk of medications, especially among those who Children with steroid-sensitive nephrotic syndrome come of age:
receive biological agents. For complicated FRNS or SDNS, long-term outcome. J Pediatr 2005; 147: 202–07.
further modification of rituximab treat ment, including 8 Lewis MA, Baildom EM, Davis N, Houston IB, Postlethwaite RJ.
Nephrotic syndrome: from toddlers to twenties. Lancet 1989;
adjunct immunosuppressive therapies and repeated 33: 255–59.
courses of rituximab, might be necessary to extend the 9 Fakhouri F, Bocquet N, Taupin P, et al. Steroid-sensitive nephrotic
relapse-free period. Finally, a comparison of the efficacy, syndrome: from childhood to adulthood. Am J Kidney Dis 2003;
41: 550–57.
safety, and cost-effectiveness of various rituximab dosing
10 Skrzypczyk P, Panczyk-Tomaszewska M, Roszkowska-Blaim M, et al.
regimens and B-cell-driven regimens are needed. Long-term outcomes in idiopathic nephrotic syndrome: from
There is also a need to develop novel therapies to childhood to adulthood. Clin Nephrol 2014; 81: 166–73.
address refractory disease and FSGS. Several therapies 11 Banh TH, Hussain-Shamsy N, Patel V, et al. Ethnic differences in
incidence and outcomes of childhood nephrotic syndrome.
are in the research phase, including sirolimus, apheresis, Clin J Am Soc Nephrol 2016; 11: 1760–68.
adalimumab, fresolimumab, rosiglitazone, galactose at 12 Mendonca AC, Oliveira EA, Froes BP, et al. A predictive model of
high dose, and ofatumumab (appendix). Finally, a progressive chronic kidney disease in idiopathic nephrotic syndrome.
Pediatr Nephrol 2015; 30: 2011–20.
determination of the social and patient-centred factors
13 Trautmann A, Schnaidt S, Lipska-Zietkiewicz BS, et al. Long-term
that affect outcomes will aid in counselling children and outcome of steroid-resistant nephrotic syndrome in children.
families about long-term prognosis. J Am Soc Nephrol 2017; 28: 3055–65.
14 Gipson DS, Chin H, Presler TP, et al. Differential risk of remission
and ESRD in childhood FSGS. Pediatr Nephrol 2006; 21: 344–49.
Conclusion 15 Joshi S, Andersen R, Jespersen B, Rittig S. Genetics of
Although, there is substantial morbidity due to chronic steroid-resistant nephrotic syndrome: a review of mutation spectrum
use of steroids and other steroid-sparing agents, less than and suggested approach for genetic testing. Acta Paediatr 2013;
102: 844–56.
5% of children with SSNS progress to ESRD. Steroid 16 Hama T, Nakanishi K, Shima Y, et al. Renal biopsy criterion in
resistance, however, is an important determinant of future idiopathic nephrotic syndrome with microscopic hematuria at onset.
risk for ESRD.8 Historically, more than 90% of children Pediatr Nephrol 2015; 30: 445–50.
with NS enter long-term remission after puberty,6,7 17 Vivarelli M, Massella L, Ruggiero B, Emma F. Minimal Change
Disease. Clin J Am Soc Nephrol 2017; 12: 332–45.
however, the precise number is not known, especially in 18 D’Agati VD, Kaskel FJ, Falk RJ. Focal segmental glomerulosclerosis.
frequent relapsers or those on steroid-sparing agents with N Engl J Med 2011; 365: 2398–411.
the potential of active disease in adulthood.8–10 19 Chanchlani R, Parekh RS. Ethnic differences in childhood nephrotic
syndrome. Front Pediatr 2016; 4: 39.
Contributors 20 Boyer O, Moulder JK, Somers MJ. Focal and segmental
DGN and RP conducted the literature search with initial manuscript glomerulosclerosis in children: a longitudinal assessment.
preparation. All authors contributed equally to data interpretation, Pediatr Nephrol 2007; 22: 1159–66.
www.thelancet.com Vol 392 July 7, 2018 71
Seminar
21 Akchurin O, Reidy KJ. Genetic causes of proteinuria and nephrotic 46 Ulinski T, Leroy S, Dubrel M, Danon S, Bensman A.
syndrome: impact on podocyte pathobiology. Pediatr Nephrol 2015; High serological response to pneumococcal vaccine in nephrotic
30: 221–33. children at disease onset on high-dose prednisone.
22 Buscher AK, Weber S. Educational paper: the podocytopathies. Pediatr Nephrol 2008; 23: 1107–13.
Eur J Pediatr 2012; 171: 1151–60. 47 Gipson DS, Massengill SF, Yao L, et al. Management of childhood
23 Shalhoub RJ. Pathogenesis of lipoid nephrosis: a disorder of T-cell onset nephrotic syndrome. Pediatrics 2009; 124: 747–57.
function. Lancet 1974; 304: 556–60. 48 Furth SL, Arbus GS, Hogg R, et al. Varicella vaccination in children
24 Lin CY, Hsu HC. Histopathological and immunological studies in with nephrotic syndrome: a report of the Southwest Pediatric
spontaneous remission of nephrotic syndrome after intercurrent Nephrology Study Group. J Pediatr 2003; 142: 145–48.
measles infection. Nephron 1986; 42: 110–15. 49 Prelog M, Schonlaub J, Zimmerhackl LB. Aciclovir and
25 Audard V, Larousserie F, Grimbert P, et al. Minimal change varicella-zoster-immunoglobulin in solid-organ transplant
nephrotic syndrome and classical Hodgkin’s lymphoma: report of recipients. Pediatr Nephrol 2011; 26: 663–73.
21 cases and review of the literature. Kidney Int 2006; 69: 2251–60. 50 Kerlin BA, Ayoob R, Smoyer WE. Epidemiology and
26 Reiser J, von Gersdorff G, Loos M, et al. Induction of B7-1 in pathophysiology of nephrotic syndrome-associated thromboembolic
podocytes is associated with nephrotic syndrome. disease. Clin J Am Soc Nephrol 2012; 7: 513–20.
J Clinical Invest 2004; 113: 1390–97. 51 Kerlin BA, Haworth K, Smoyer WE. Venous thromboembolism in
27 Yu CC, Fornoni A, Weins A, et al. Abatacept in B7-1-positive pediatric nephrotic syndrome. Pediatr Nephrol 2014; 29: 989–97.
proteinuric kidney disease. N Engl J Med 2013; 369: 2416–23. 52 Kerlin BA, Blatt NB, Fuh B, et al. Epidemiology and risk factors for
28 Benigni A, Gagliardini E, Remuzzi G. Abatacept in B7-1-positive thromboembolic complications of childhood nephrotic syndrome:
proteinuric kidney disease. N Engl J Med 2014; 370: 1261–63. a Midwest Pediatric Nephrology Consortium (MWPNC) study.
29 Savin VJ, Sharma R, Sharma M, et al. Circulating factor J Pediatr 2009; 155: 105–10.
associated with increased glomerular permeability to albumin in 53 Rheault MN, Zhang L, Selewski DT, et al. AKI in children
recurrent focal segmental glomerulosclerosis. N Engl J Med 1996; hospitalized with nephrotic syndrome. Clin J Am Soc Nephrol 2015;
334: 878–83. 10: 2110–18.
30 Kemper MJ, Wolf G, Muller-Wiefel DE. Transmission of glomerular 54 Vaziri ND. HDL abnormalities in nephrotic syndrome and chronic
permeability factor from a mother to her child. N Engl J Med 2001; kidney disease. Nat Rev Nephrol 2016; 12: 37–47.
344: 386–67. 55 Kong X, Yuan H, Fan J, Li Z, Wu T, Jiang L. Lipid-lowering agents
31 Brenchley PE. Vascular permeability factors in steroid-sensitive for nephrotic syndrome. Cochrane Database Syst Rev 2013;
nephrotic syndrome and focal segmental glomerulosclerosis. 12: CD005425.
Nephrol Dial Transplant 2003; 18 (suppl 6): vi21–25. 56 National Heart, Lung and, Blood Institute. Expert panel on
32 Clement LC, Mace C, Avila-Casado C, Joles JA, Kersten S, integrated guidelines for cardiovascular health and risk reduction in
Chugh SS. Circulating angiopoietin-like 4 links proteinuria with children and adolescents: summary report. Pediatrics 2011;
hypertriglyceridemia in nephrotic syndrome. Nat Med 2014; 128 (suppl 5): S213–56.
20: 37–46. 57 Teoh CW, Robinson LA, Noone D. Perspectives on edema in
33 McCarthy ET, Sharma M, Savin VJ. Circulating permeability factors childhood nephrotic syndrome. Am J Physiol Renal Physiol 2015;
in idiopathic nephrotic syndrome and focal segmental 309: F575–82.
glomerulosclerosis. Clin J Am Soc Nephrol 2010; 5: 2115–21. 58 Buyukavci MA, Civilibal M, Elevli M, Selcuk Duru HN. Hypo- and
34 Wei C, El Hindi S, Li J, et al. Circulating urokinase receptor as a hypervolemic edema in children with steroid sensitive nephrotic
cause of focal segmental glomerulosclerosis. Nat Med 2011; syndrome. Turk J Med Sci 2015; 45: 178–83.
17: 952–60. 59 Samuel S, Morgan CJ, Bitzan M, et al. Substantial practice variation
35 Hayek SS, Quyyumi AA, Reiser J. Soluble urokinase receptor and exists in the management of childhood nephrotic syndrome.
chronic kidney disease. N Engl J Med 2016; 374: 891. Pediatr Nephrol 2013; 28: 2289–98.
36 Gbadegesin RA, Adeyemo A, Webb NJ, et al. HLA-DQA1 and 60 Pasini A, Aceto G, Ammenti A, et al. Best practice guidelines for
PLCG2 are candidate risk loci for childhood-onset steroid-sensitive idiopathic nephrotic syndrome: recommendations versus reality.
nephrotic syndrome. J Am Soc Nephrol 2015; 26: 1701–10. Pediatr Nephrol 2015; 30: 91–101.
37 Patrakka J, Ruotsalainen V, Reponen P, et al. Recurrence of 61 Abramowicz M, Barnett HL, Edelmann CM Jr, et al. Controlled trial
nephrotic syndrome in kidney grafts of patients with congenital of azathioprine in children with nephrotic syndrome. A report for the
nephrotic syndrome of the Finnish type: role of nephrin. international study of kidney disease in children. Lancet 1970;
Transplantation 2002; 73: 394–403. 295: 959–61.
38 Kuusniemi AM, Qvist E, Sun Y, et al. Plasma exchange and 62 Haute Autorité de Santé. Syndrome néphrotique idiopathique de
retransplantation in recurrent nephrosis of patients with congenital l’enfant. Protocole national de diagnostic et de soins pour une
nephrotic syndrome of the Finnish type (NPHS1). maladie rare. http://www.afpssu.com/wp-content/
Transplantation 2007; 83: 1316–23. uploads/2013/07/NephrotiqueIdiopthiquePNDS.pdf 2008
39 Sadowski CE, Lovric S, Ashraf S, et al. A single-gene cause in (accessed March 5, 2018).
29.5% of cases of steroid-resistant nephrotic syndrome. 63 Pasini A, Benetti E, Conti G, et al. The Italian Society for Pediatric
J Am Soc Nephrol 2015; 26: 1279–89. Nephrology (SINePe) consensus document on the management of
40 Hinkes BG, Mucha B, Vlangos CN, et al. Nephrotic syndrome in the nephrotic syndrome in children: Part I - Diagnosis and treatment of
first year of life: two thirds of cases are caused by mutations in the first episode and the first relapse. Ital J Pediatr 2017; 43: 41.
4 genes (NPHS1, NPHS2, WT1, and LAMB2). Pediatrics 2007; 64 Hodson EM, Willis NS, Craig JC. Corticosteroid therapy for
119: e907–19. nephrotic syndrome in children. Cochrane Database Syst Rev 2007;
41 Trautmann A, Bodria M, Ozaltin F, et al. Spectrum of 4: CD001533.
steroid-resistant and congenital nephrotic syndrome in children: the 65 Teeninga N, Kist-van Holthe JE, van Rijswijk N, et al. Extending
PodoNet registry cohort. Clin J Am Soc Nephrol 2015; 10: 592–600. prednisolone treatment does not reduce relapses in childhood
42 Yu H, Artomov M, Brahler S, et al. A role for genetic susceptibility nephrotic syndrome. J Am Soc Nephrol 2013; 24: 149–59.
in sporadic focal segmental glomerulosclerosis. J Clin Invest 2016; 66 Yoshikawa N, Nakanishi K, Sako M, et al. A multicenter randomized
126: 1067–78. trial indicates initial prednisolone treatment for childhood nephrotic
43 Latta K, von Schnakenburg C, Ehrich JH. A meta-analysis of syndrome for two months is not inferior to six-month treatment.
cytotoxic treatment for frequently relapsing nephrotic syndrome in Kidney Int 2015; 87: 225–32.
children. Pediatr Nephrol 2001; 16: 271–82. 67 Sinha A, Saha A, Kumar M, et al. Extending initial prednisolone
44 Hingorani SR, Weiss NS, Watkins SL. Predictors of peritonitis in treatment in a randomized control trial from 3 to 6 months did not
children with nephrotic syndrome. Pediatr Nephrol 2002; 17: 678–82. significantly influence the course of illness in children with
steroid-sensitive nephrotic syndrome. Kidney Int 2015; 87: 217–24.
45 McCaffrey J, Lennon R, Webb NJ. The non-immunosuppressive
management of childhood nephrotic syndrome. 68 Hodson E. The management of idiopathic nephrotic syndrome in
Pediatr Nephrol 2016; 31: 1383–402. children. Paediatr Drugs 2003; 5: 335–49.
72 www.thelancet.com Vol 392 July 7, 2018
Seminar
69 Abdel-Hafez M, Shimada M, Lee PY, Johnson RJ, Garin EH. 91 Ishikura K, Yoshikawa N, Nakazato H, et al. Two-year follow-up of a
Idiopathic nephrotic syndrome and atopy: is there a common link? prospective clinical trial of cyclosporine for frequently relapsing
Am J Kidney Dis 2009; 54: 945–53. nephrotic syndrome in children. Clin J Am Soc Nephrol 2012;
70 Mattoo TK, Mahmoud MA. Increased maintenance corticosteroids 7: 1576–83.
during upper respiratory infection decrease the risk of relapse in 92 Sinha MD, MacLeod R, Rigby E, Clark AG. Treatment of severe
nephrotic syndrome. Nephron 2000; 85: 343–45. steroid-dependent nephrotic syndrome (SDNS) in children with
71 Abeyagunawardena AS, Trompeter RS. Increasing the dose of tacrolimus. Nephrol Dial Transplant 2006; 21: 1848–54.
prednisolone during viral infections reduces the risk of relapse in 93 Roberti I, Vyas S. Long-term outcome of children with
nephrotic syndrome: a randomised controlled trial. steroid-resistant nephrotic syndrome treated with tacrolimus.
Arch Dis Child 2008; 93: 226–28. Pediatr Nephrol 2010; 25: 1117–24.
72 Gulati A, Sinha A, Sreenivas V, Math A, Hari P, Bagga A. Daily 94 Butani L, Ramsamooj R. Experience with tacrolimus in children with
corticosteroids reduce infection-associated relapses in frequently steroid-resistant nephrotic syndrome. Pediatr Nephrol 2009; 24: 1517–23.
relapsing nephrotic syndrome: a randomized controlled trial. 95 Morgan C, Sis B, Pinsk M, Yiu V. Renal interstitial fibrosis in
Clin J Am Soc Nephrol 2011; 6: 63–69. children treated with FK506 for nephrotic syndrome.
73 Webb NJ, Frew E, Brettell EA, et al. Short course daily prednisolone Nephrol Dial Transplant 2011; 26: 2860–65.
therapy during an upper respiratory tract infection in children with 96 Sinha A, Bagga A, Gulati A, Hari P. Short-term efficacy of rituximab
relapsing steroid-sensitive nephrotic syndrome (PREDNOS 2): versus tacrolimus in steroid-dependent nephrotic syndrome.
protocol for a randomised controlled trial. Trials 2014; 15: 147. Pediatr Nephrol 2012; 27: 235–41.
74 Levamisole for corticosteroid-dependent nephrotic syndrome in 97 Gellermann J, Weber L, Pape L, et al. Mycophenolate mofetil versus
childhood. British Association for Paediatric Nephrology. Lancet 1991; cyclosporin A in children with frequently relapsing nephrotic
337: 1555–57. syndrome. J Am Soc Nephrol 2013; 24: 1689–97.
75 Dayal U, Dayal AK, Shastry JC, Raghupathy P. Use of levamisole in 98 Dorresteijn EM, Kist-van Holthe JE, Levtchenko EN, Nauta J,
maintaining remission in steroid-sensitive nephrotic syndrome in Hop WC, van der Heijden AJ. Mycophenolate mofetil versus
children. Nephron 1994; 66: 408–12. cyclosporine for remission maintenance in nephrotic syndrome.
76 Pravitsitthikul N, Willis NS, Hodson EM, Craig JC. Non-corticosteroid Pediatr Nephrol 2008; 23: 2013–20.
immunosuppressive medications for steroid-sensitive nephrotic 99 Ravani P, Magnasco A, Edefonti A, et al. Short-term effects of
syndrome in children. Cochrane Database Syst Rev 2013; rituximab in children with steroid- and calcineurin-dependent
10: CD002290. nephrotic syndrome: a randomized controlled trial.
77 Barratt TM, Soothill JF. Controlled trial of cyclophosphamide in Clin J Am Soc Nephrol 2011; 6: 1308–15.
steroid-sensitive relapsing nephrotic syndrome of childhood. 100 Iijima K, Sako M, Nozu K, et al. Rituximab for childhood-onset,
Lancet 1970; 296: 479–82. complicated, frequently relapsing nephrotic syndrome or
78 Prospective, controlled trial of cyclophosphamide therapy in children steroid-dependent nephrotic syndrome: a multicentre, double-blind,
with nephrotic syndrome. Report of the International study of Kidney randomised, placebo-controlled trial. Lancet 2014; 384: 1273–81.
Disease in Children. Lancet 1974; 304: 423–27. 101 Ravani P, Rossi R, Bonanni A, et al. Rituximab in children with
79 Vester U, Kranz B, Zimmermann S, Hoyer PF. Cyclophosphamide in steroid-dependent nephrotic syndrome: a multicenter, open-label,
steroid-sensitive nephrotic syndrome: outcome and outlook. noninferiority, randomized controlled trial. J Am Soc Nephrol 2015;
Pediatr Nephrol 2003; 18: 661–64. 26: 2259–66.
80 Zagury A, de Oliveira AL, de Moraes CA, et al. Long-term follow-up 102 Yoshioka K, Ohashi Y, Sakai T, et al. A multicenter trial of
after cyclophosphamide therapy in steroid-dependent nephrotic mizoribine compared with placebo in children with frequently
syndrome. Pediatr Nephrol 2011; 26: 915–20. relapsing nephrotic syndrome. Kidney Int 2000; 58: 317–24.
81 Kemper MJ, Altrogge H, Ludwig K, Timmermann K, 103 Gruppen MP, Bouts AH, Jansen-van der Weide MC, et al.
Muller-Wiefel DE. Unfavorable response to cyclophosphamide in A randomized clinical trial indicates that levamisole increases the
steroid-dependent nephrotic syndrome. Pediatr Nephrol 2000; time to relapse in children with steroid-sensitive idiopathic
14: 772–75. nephrotic syndrome. Kidney Int 2017; 93: 510–18.
82 Garin EH, Pryor ND, Fennell RS III, Richard GA. Pattern of 104 Rivkees SA, Crawford JD. The relationship of gonadal activity and
response to prednisone in idiopathic, minimal lesion nephrotic chemotherapy-induced gonadal damage. JAMA 1988; 259: 2123–25.
syndrome as a criterion in selecting patients for cyclophosphamide 105 Yi Z, Li Z, Wu XC, He QN, Dang XQ, He XJ. Effect of fosinopril in
therapy. J Pediatr 1978; 92: 304–48. children with steroid-resistant idiopathic nephrotic syndrome.
83 Ishikura K, Ikeda M, Hattori S, et al. Effective and safe treatment Pediatr Nephrol 2006; 21: 967–72.
with cyclosporine in nephrotic children: a prospective, randomized 106 Iijima K, Hamahira K, Tanaka R, et al. Risk factors for
multicenter trial. Kidney Int 2008; 73: 1167–73. cyclosporine-induced tubulointerstitial lesions in children with
84 Ishikura K, Yoshikawa N, Hattori S, et al. Treatment with minimal change nephrotic syndrome. Kidney Int 2002;
microemulsified cyclosporine in children with frequently relapsing 61: 1801–05.
nephrotic syndrome. Nephrol Dial Transplant 2010; 25: 3956–62. 107 Fujinaga S, Kaneko K, Muto T, Ohtomo Y, Murakami H,
85 El-Husseini A, El-Basuony F, Mahmoud I, et al. Long-term effects Yamashiro Y. Independent risk factors for chronic cyclosporine
of cyclosporine in children with idiopathic nephrotic syndrome: induced nephropathy in children with nephrotic syndrome.
a single-centre experience. Nephrol Dial Transplant 2005; Arch Dis Child 2006; 91: 666–70.
20: 2433–38. 108 Ishikura K, Ikeda M, Hamasaki Y, et al. Nephrotic state as a risk
86 Tanaka R, Yoshikawa N, Kitano Y, Ito H, Nakamura H. Long-term factor for developing posterior reversible encephalopathy syndrome
ciclosporin treatment in children with steroid-dependent nephrotic in paediatric patients with nephrotic syndrome.
syndrome. Pediatr Nephrol 1993; 7: 249–52. Nephrol Dial Transplant 2008; 23: 2531–36.
87 Inoue Y, Iijima K, Nakamura H, Yoshikawa N. Two-year cyclosporin 109 Baudouin V, Alberti C, Lapeyraque AL, et al. Mycophenolate mofetil
treatment in children with steroid-dependent nephrotic syndrome. for steroid-dependent nephrotic syndrome: a phase II Bayesian
Pediatr Nephrol 1999; 13: 33–38. trial. Pediatr Nephrol 2012; 27: 389–96.
88 Iijima K, Sako M, Oba MS, et al. Cyclosporine C2 monitoring for the 110 Hackl A, Cseprekal O, Gessner M, et al. Mycophenolate mofetil
treatment of frequently relapsing nephrotic syndrome in children: therapy in children with idiopathic nephrotic syndrome: does
a multicenter randomized phase II trial. Clin J Am Soc Nephrol 2014; therapeutic drug monitoring make a difference?
9: 271–78. Ther Drug Monit 2016; 38: 274–79.
89 Niaudet P, Broyer M, Habib R. Treatment of idiopathic nephrotic 111 Sellier-Leclerc AL, Belli E, Guerin V, Dorfmuller P, Deschenes G.
syndrome with cyclosporin A in children. Clin Nephrol 1991; Fulminant viral myocarditis after rituximab therapy in pediatric
35 (suppl 1): S31–36. nephrotic syndrome. Pediatr Nephrol 2013; 28: 1875–79.
90 Kitano Y, Yoshikawa N, Tanaka R, Nakamura H, Ninomiya M, Ito H. 112 Sato M, Ito S, Ogura M, et al. Atypical Pneumocystis jiroveci
Ciclosporin treatment in children with steroid-dependent nephrotic pneumonia with multiple nodular granulomas after rituximab for
syndrome. Pediatr Nephrol 1990; 4: 474–77. refractory nephrotic syndrome. Pediatr Nephrol 2013; 28: 145–49.
www.thelancet.com Vol 392 July 7, 2018 73
Seminar
113 Ahn YH, Kang HG, Lee JM, Choi HJ, Ha IS, Cheong HI. 122 Waldo FB, Benfield MR, Kohaut EC. Therapy of focal and segmental
Development of antirituximab antibodies in children with nephrotic glomerulosclerosis with methylprednisolone, cyclosporine A,
syndrome. Pediatr Nephrol 2014; 29: 1461–64. and prednisone. Pediatr Nephrol 1998; 12: 397–400.
114 Buscher AK, Kranz B, Buscher R, et al. Immunosuppression and 123 Bagga A, Mudigoudar BD, Hari P, Vasudev V. Enalapril dosage in
renal outcome in congenital and pediatric steroid-resistant nephrotic steroid-resistant nephrotic syndrome. Pediatr Nephrol 2004; 19: 45–50.
syndrome. Clin J Am Soc Nephrol 2010; 5: 2075–84. 124 Tarshish P, Tobin JN, Bernstein J, Edelmann CM, Jr.
115 Buscher AK, Beck BB, Melk A, et al. Rapid response to cyclosporin A Cyclophosphamide does not benefit patients with focal segmental
and favorable renal outcome in nongenetic versus genetic steroid- glomerulosclerosis. A report of the International Study of Kidney
resistant nephrotic syndrome. Clin J Am Soc Nephrol 2016; Disease in Children. Pediatr Nephrol 1996; 10: 590–93.
11: 245–53. 125 de Mello VR, Rodrigues MT, Mastrocinque TH, et al. Mycophenolate
116 Hodson EM, Willis NS, Craig JC. Interventions for idiopathic mofetil in children with steroid/cyclophosphamide-resistant
steroid-resistant nephrotic syndrome in children. nephrotic syndrome. Pediatr Nephrol 2010; 25: 453–60.
Cochrane Database Syst Rev 2010; 11: CD003594. 126 Li Z, Duan C, He J, et al. Mycophenolate mofetil therapy for
117 Garin EH, Orak JK, Hiott KL, Sutherland SE. Cyclosporine therapy children with steroid-resistant nephrotic syndrome.
for steroid-resistant nephrotic syndrome. A controlled study. Pediatr Nephrol 2010; 25: 883–88.
Am J Dis Child 1988; 142: 985–88. 127 Gargah TT, Lakhoua MR. Mycophenolate mofetil in treatment of
118 Lieberman KV, Tejani A. A randomized double-blind childhood steroid-resistant nephrotic syndrome. J Nephrol 2011;
placebo-controlled trial of cyclosporine in steroid-resistant idiopathic 24: 203–07.
focal segmental glomerulosclerosis in children. 128 Gipson DS, Trachtman H, Kaskel FJ, et al. Clinical trial of focal
J Am Soc Nephrol 1996; 7: 56–63. segmental glomerulosclerosis in children and young adults.
119 Ponticelli C, Rizzoni G, Edefonti A, et al. A randomized trial of Kidney Int 2011; 80: 868–78.
cyclosporine in steroid-resistant idiopathic nephrotic syndrome. 129 Magnasco A, Ravani P, Edefonti A, et al. Rituximab in children with
Kidney Int 1993; 43: 1377–84. resistant idiopathic nephrotic syndrome. J Am Soc Nephrol 2012;
120 Choudhry S, Bagga A, Hari P, Sharma S, Kalaivani M, Dinda A. 23: 1117–24.
Efficacy and safety of tacrolimus versus cyclosporine in children
with steroid-resistant nephrotic syndrome: a randomized controlled © 2018 Elsevier Ltd. All rights reserved.
trial. Am J Kidney Dis 2009; 53: 760–69.
121 Hamasaki Y, Yoshikawa N, Hattori S, et al. Cyclosporine and steroid
therapy in children with steroid-resistant nephrotic syndrome.
Pediatr Nephrol 2009; 24: 2177–85.
74 www.thelancet.com Vol 392 July 7, 2018
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5813)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1092)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (844)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (540)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (348)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (822)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- NephrologyDocument32 pagesNephrologyPharmacotherapyNo ratings yet
- Gynecomastia Surgery: Know Everything About The ProcedureDocument2 pagesGynecomastia Surgery: Know Everything About The ProcedureTandon ClinicNo ratings yet
- Online Geriatrics CurriculumDocument203 pagesOnline Geriatrics CurriculumAn-Nisa Khoirun UmmiNo ratings yet
- Zoology ExamDocument4 pagesZoology Examgabriel omliNo ratings yet
- CardiovascularDocument16 pagesCardiovascularMilena VargasNo ratings yet
- Gastroenteritis': Dr. Yanga'S Colleges, IncDocument9 pagesGastroenteritis': Dr. Yanga'S Colleges, IncZyren FuentabellaNo ratings yet
- Acute Kidney Injury Managing Acute Kidney InjuryDocument11 pagesAcute Kidney Injury Managing Acute Kidney InjuryDilaPrasetyaBelindaNo ratings yet
- Breast Cancer Awareness (2023)Document2 pagesBreast Cancer Awareness (2023)The Livingston County NewsNo ratings yet
- Right Side EcgDocument4 pagesRight Side EcgDragos CirsteaNo ratings yet
- SIADH, DI and Cerebral Salt Wasting: Karim Rafaat, MDDocument54 pagesSIADH, DI and Cerebral Salt Wasting: Karim Rafaat, MDMahendra PrasetyoNo ratings yet
- Case StudyDocument4 pagesCase Studyllyryc100% (1)
- Pathology of The Lungs 3rd Ed (PDF) (Tahir99) VRGDocument746 pagesPathology of The Lungs 3rd Ed (PDF) (Tahir99) VRGCosmin SilviuNo ratings yet
- Endocrine System Reviewer - BAYLONDocument6 pagesEndocrine System Reviewer - BAYLONElijah Joaquin Payumo BaylonNo ratings yet
- Anatomy and Physiology - GallbladderDocument2 pagesAnatomy and Physiology - GallbladderCHi NAiNo ratings yet
- GRADES 1 To 12 Daily Lesson LogDocument6 pagesGRADES 1 To 12 Daily Lesson LogJeanelle Marie RamosNo ratings yet
- Excretion in Humans: Question Paper 1Document10 pagesExcretion in Humans: Question Paper 1Annmary AbrahamNo ratings yet
- Nursing Process of A Client With CholelithiasisDocument21 pagesNursing Process of A Client With Cholelithiasisapi-3822508100% (6)
- Pituitary GlandDocument22 pagesPituitary GlandSara Musavi100% (2)
- Male Reproductive SystemDocument44 pagesMale Reproductive SystemTuaha MasoodNo ratings yet
- Soojeedes Human Anatomy and Physiology PDFDocument119 pagesSoojeedes Human Anatomy and Physiology PDFmaxamed Buule IsaaqNo ratings yet
- Anaphy Midterm ExaminationDocument6 pagesAnaphy Midterm ExaminationCarmela Jane SonzaNo ratings yet
- The Renin-Angiotensin Aldosterone System: Pathophysiological Role and Pharmacologic InhibitionDocument12 pagesThe Renin-Angiotensin Aldosterone System: Pathophysiological Role and Pharmacologic Inhibitionfatimah hasibuanNo ratings yet
- Human Body Systems: Study GuideDocument11 pagesHuman Body Systems: Study Guideapi-242114183No ratings yet
- Cardiovascular DoDocument2 pagesCardiovascular Dogladz25No ratings yet
- HLTAAP002 CardiovascularDocument56 pagesHLTAAP002 CardiovascularJesse SimonNo ratings yet
- Case Study TbiDocument13 pagesCase Study Tbiaica_184No ratings yet
- Fluid Deprivation TestDocument3 pagesFluid Deprivation TestsakuraleeshaoranNo ratings yet
- Essentials of Medical PhysiologyDocument6 pagesEssentials of Medical Physiologykumarraushan1000No ratings yet
- Full FileDocument105 pagesFull Filekrishan kumarNo ratings yet
- Important Topics For Medical PG by Subject Experts and Toppers Prepladder April 2 PDFDocument69 pagesImportant Topics For Medical PG by Subject Experts and Toppers Prepladder April 2 PDFSudheer Chowdary100% (1)