Professional Documents
Culture Documents
The Rheumatoid Forefoot: Joint-Sparing vs. Joint-Ablation: John T. Campbell, MD
Uploaded by
Yuki SATAKEOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Rheumatoid Forefoot: Joint-Sparing vs. Joint-Ablation: John T. Campbell, MD
Uploaded by
Yuki SATAKECopyright:
Available Formats
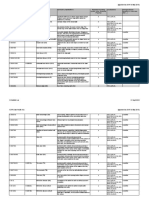
AOFAS Symposium 3 – Lesser Toe Surgeons Are Not Lesser People
Monday, September 22, 2014
11:00 am - 12:00 pm
Moderator:
Thomas H. Lee, MD, Westerville, Ohio
The Rheumatoid Forefoot: Joint-Sparing Vs. Joint-Ablation
John T. Campbell, MD
Baltimore, Maryland
I) Background
A) Pathophysiology
1) Synovitis, pannus
2) Ligament attenuation, failure
3) Joint erosions, cartilage loss, arthritis
B) Pathomechanics
1) Hallux
(a) Progressive valgus
(b) Unloads hallux, transfers stress to lesser MTPs
(c) Loss of windlass mechanism, arch flattening, 1st TMT instability
2) Lesser MTPs
(a) Progressive subluxation → dislocation
(b) Intrinsic minus, claw toe deformity
(c) Fat pad migrates distally – diminished padding
(d) Depresses metatarsal head → metatarsalgia, callus, ulceration
II) Historical Perspective
A) Pan-metatarsal head resection
1) Keller (base proximal phalanx) or Mayo (1st metatarsal head)
2) Lesser met head +/- phalangeal base resections
3) Pain relief, improved shoewear
4) Not as durable – valgus deformity tends to recur (esp. with Keller)
B) Implant arthroplasty 1st MTP
1) Silastic implant
2) Inconsistent pain relief, inadequate restoration hallux WB
3) Durability concerns – particulate wear debris, inflammation and erosive synovitis, bone lysis
C) Arthrodesis 1st MTP with lesser MTP resection arthroplasties
© American Orthopaedic Foot & Ankle Society
1) Biomechanical advantage
(a) Restores WB to medial column
(b) Increased contact area & peak pressure under hallux
(c) Offloads/ protects lesser MTPs
(d) May decrease peak P-time integral – earlier toe-off in stance phase
2) Outcomes
(a) Level II/III studies – most support fusion
(i) Resection patients do have pain relief, satisfaction
Some studies show no difference vs. fusion
(ii) Various pedobarographic data support fusion > resection
(iii) Fusion: better push off hallux, better cadence, more cosmetic, better correction
splayfoot, more durable
(b) Multiple Level IV series support 1st MTP arthrodesis
(i) Fusion rate 90-100%
(ii) Maintenance of deformity correction
(iii) Excellent pain relief, shoewear tolerance, cosmetic improvement
(iv) Durable – follow-up as long as 6 years
(c) Grade B Recommendation
III) Joint-Sparing Alternatives
A) Background
1) DMARDs & biologics
(a) Less severe forefoot disease on presentation
(b) Preferential effects on smaller joint disease? (Nikiphorou et al)
2) Limitations with lesser MTP resection arthroplasties long term
(a) Spur formation, bony proliferation
(b) Plantar callus
(c) Recurrent deformity
3) Thordarson et al series (2002) – high rate of failure, recurrent deformity if hallux MTP not
fused, revised to fusion 45%
4) Barouk described using Scarf & lesser Weils for joint-sparing in textbook (2005), later series
in 2007
(a) 95% satisfactory correction, 55° 1st MTP ROM
(b) 15% floating toes, 10% metatarsalgia
(c) Only 1/55 revised to fusion on 75 months follow-up
B) Indications
1) Mild to moderate deformity
2) Severe claw toe, dislocation?
3) Adequate bone stock
4) Maintained joint space
5) One or two lesser MTP joints affected
C) Contraindications
© American Orthopaedic Foot & Ankle Society
1) Joint destruction, severe arthritis
2) Severe osteopenia – compromised fixation
3) Bone loss
4) More severe systemic disease?
5) Recurrence, revision situation
D) 1st MTP
1) Options
(a) Scarf osteotomy
(b) Proximal osteotomy
(c) Distal osteotomy (chevron, Mitchell)
(d) Lapidus procedure
2) Level IV series for each technique, no clear preference
3) Improvement in various outcomes scores (AOFAS, VAS, FFI, SF-36, etc.)
4) Angular correction which seems to hold up (max = 75 months)
5) Failure (conversion to fusion) 2%-5%
6) IP arthritis 20-30%
E) Lesser MTPs
1) Weil osteotomy / distal oblique osteotomy
(a) Most evidence
(b) 85% correction, 15% floating toes, 14% redislocation
(c) Metatarsalgia 10% - 13%
2) Stainsby procedure
(a) Retain met head, resect phalangeal base, reduce plantar plate and fat pad, extensor
tendon secured to flexor or through met head to stabilize toe
(b) Multiple Level IV series, small numbers, short- to medium-term follow-up (59 months)
(i) Pain relief 83-93%
(ii) Satisfaction 80-90%
(iii) Continued metatarsalgia 8-33%, recurrent deformity 17%
3) Grade B Recommendation –
(a) Appears promising pending further study
(b) Virtually all Level IV case series
(c) No pedobarographic analyses
IV) Unanswered Questions
A) Refine indications
B) Optimal technique
C) Durability – longer term follow-up
D) Pedobarographic data – how well do joint-sparing techniques restore normal function?
E) Outcomes – higher level studies, compare to standard approach
V) Bibliography
© American Orthopaedic Foot & Ankle Society
Amin A, Cullen N, Singh D. Rheumatoid Forefoot Reconstruction. Acta Orthop Belg, 76: 289-297, 2010.
Barouk LS, Barouk P. Joint-Preserving Surgery in Rheumatoid Forefoot: Preliminary Study with More
Than Two Year Follow-Up. Foot Ankle Clin, 12: 435-454, 2007.
Bass EJ, Shariff R, Sirikonda SP. Rheumatoid Forefoot Reconstruction: Outcome of 1st
Metatarsophalangeal Joint Fusion and the Stainsby Procedure in the Lesser Toes. Foot, 24: 56-61, 2014.
Bhavikatti M, Sewell MD, Al-Hadithy N, Awan S, Bawarish MA. Joint Preserving Surgery for Rheumatoid
Forefoot Deformities Improves Pain and Corrects Deformity at Mid-Term Follow-Up. Foot, 22: 81-84,
2012.
Bolland BJRF, Sauve PS, Taylor GR. Rheumatoid Forefoot Reconstruction: First Metatarsophalangeal
Joint Fusion Combined with Weil’s Metatarsal Osteotomies of the Lesser Rays. J Foot Ankle Surg, 47 (2):
80-88, 2008.
Briggs PJ, Stainsby GD. Metatarsal Head Preservation in Forefoot Arthroplasty and the Correction of
Severe Claw Toe Deformity. Foot Ankle Surg, 7: 93-101, 2001.
Chao JC, Charlick D, Tocci S, Brodsky JW. Radiographic and Clinical Outcomes of Joint-Preserving
Procedures for Hallux Valgus in Rheumatoid Arthritis. Foot Ankle Int, 34 (12): 1638-1644, 2013.
Coughlin MJ. Rheumatoid Forefoot Reconstruction: A Long-Term Follow-Up Study. J Bone Joint Surg
[Am], 82-A: 322-341, 2000.
Dodd L, Atinga M, Foote J, Palmer S. Outcomes after the Stainsby Procedure in the Lesser Toes: An
Alternative Procedure for the Correction of Rigid Claw Toes Deformity. J Foot Ankle Surg 50: 522-524,
2011.
Grondal L, Brostrom E, Wretenberg P, Stark A. Arthrodesis versus Mayo Resection: The Management of
the First Metatarsophalangeal Joint in Reconstruction of the Rheumatoid Forefoot. J Bone Joint Surg
[Br], 88-B: 914-919, 2006.
Hanyu T, Yamazaki H, Murasawa A, Tohyama C. Arthroplasty for Rheumatoid Forefoot Deformities by a
Shortening Oblique Osteotomy. Clin Orthop Rel Res, 338: 131-138, 1997.
Hassan K, Rashid MA, Panikkar V, Walters SJ, Henry APJ. Forefoot Reconstruction: Effectiveness of
Stainsby Operation in Treating Dislocated Lesser Toes. Foot, 17: 136-142, 2007.
Jeng C, Campbell J. Current Concepts Review: The Rheumatoid Forefoot. Foot Ankle Int, 29: 959-968,
2008.
Kadambande S, Debnath U, Khurana A, Hemmady M, Hariharan K. Rheumatoid Forefoot Reconstruction:
1st Metatarsophalangeal Fusion and Excision Arthroplasty of Lesser Metatarsal Heads. Acta Orthop Belg,
© American Orthopaedic Foot & Ankle Society
73: 88-95, 2007.
Louwerens JWK, Schrier JCM. Rheumatoid Forefoot Deformity: Pathophysiology, Evaluation, and
Operative Treatment Options. Int Orthop, 37: 1719-1729, 2013.
Mann RA, Schakel ME. Surgical Correction of Rheumatoid Forefoot Deformities. Foot Ankle Int, 16: 1-6,
1995.
Mann RA, Thompson FM. Arthrodesis of the First Metatarsophalangeal Joint for Hallux Valgus in
Rheumatoid Arthritis. J Bone Joint Surg [Am], 66-A: 687-692, 1984.
McGarvey SR, Johnson KA. Keller Arthroplasty in Combination with Resection Arthroplasty of the Lesser
Metatarsophalangeal Joints in Rheumatoid Arthritis. Foot Ankle, 9(2): 75-80, 1988.
Mulcahy D, Daniels TR, Lau JT-C, Boyle E, Bogoch E. Rheumatoid Forefoot Deformity: A Comparison
Study of 2 Functional Methods of Reconstruction. J Rheumatol, 30(7): 1440-1450, 2003.
Niki H, Hirano T, Okada H, Beppu M. Combination Joint-Preserving Surgery for Forefoot Deformity in
Patients with Rheumatoid Arthritis. J Bone Joint Surg [Br], 92-B: 380-386, 2010.
Nikiphorou E, Carpenter L, Morris S, MacGregor AJ, Dixey J, Kiely P, James DW, Walsh DA, Norton S,
Young A. Hand and Foot Surgery Rates in Rheumatoid Arthritis Have Declined from 1986 to 2011, but
Large Joint Replacement Rates Remain Unchanged. Arthritis Rheum, 66 (5): 1081-1089, 2014.
Queally JM, Zgraj OS, Walsh JC, Butt AJ, D’Souza LG. Use of the Modified Stainsby Procedure in
Correcting Severe Claw Toe Deformity in the Rheumatoid Foot: A Retrospective Review. Foot, 19: 110-
113, 2009.
Rosenbaum D, Timte B, Schmiegel A, Miehlke RK, Hilker A. First Ray Resection Arthroplasty versus
Arthrodesis in the Treatment of the Rheumatoid Foot. Foot Ankle Int, 32: 589-594, 2011.
Shi K, Hayashida K, Tomita T, Tanabe M, Ochi T. Surgical Treatment of Hallux Valgus Deformity in
Rheumatoid Arthritis: Clinical and Radiographic Evaluation of Modified Lapidus Technique. J Foot Ankle
Surg, 39 (6): 376-382, 2000.
Takakubo Y, Takagi M, Tamaki Y, Sasaki A, Nakano H, Orui H, Ogino T. Mid-Term Results of Joint-
Preserving Procedures by a Modified Mann Method for Big Toe Deformities in Rheumatoid Patients
Undergoing Forefoot Surgeries. Mod Rheumatol, 20; 147-153, 2010.
Thomas S, Kinninmonth AWG, Kumar CS. Long-Term Results of the Modified Hoffman Procedure in the
Rheumatoid Forefoot. J Bone Joint Surg [Am], 87-A: 748-752, 2005.
Thordarson DB, Aval S, Krieger L. Failure of Hallux MP Preservation Surgery for Rheumatoid Arthritis.
Foot Ankle Int, 23: 486-490, 2002.
© American Orthopaedic Foot & Ankle Society
Torikai E, Kageyama Y, Suzuki M, Ichikawa T, Nagano A. Comparison between Resection Arthroplasty
Alone and Resection Arthroplasty with Arthrodesis of the First MTP Joint for Rheumatoid Forefoot
Deformities. Med Rheumatol, 18: 486-491, 2008.
Trieb K, Hofstaetter SG, Panotopoulos J, Wanivenhaus A. The Weil Osteotomy for Correction of the
Severe Rheumatoid Forefoot. Int Orthop, 37: 1795-1798, 2013.
Vandeputte G, Steenwerckx, Mulier T, Peeraer L, Dereymaeker. Forefoot Reconstruction in Rheumatoid
Arthritis Patients: Keller-Lelievre-Hoffmann versus Arthrodesis MTP1-Hoffmann. Foot Ankle Int., 20(7):
438-443, 1999.
Yano K, Ikari K, Iwamoto T, Saito A, Naito Y, Kawakami K, Suzuki T, Imamura H, Sakuma Y, Hiroshima R,
Momohara S. Proximal Rotational Closing-Wedge Osteotomy of the First Metatarsal in Rheumatoid
Arthritis: Clinical and Radiographic Evaluation of a Continuous Series of 35 Cases. Mod Rheumatol 23:
953-958, 2013.
© American Orthopaedic Foot & Ankle Society
You might also like
- Tka ValgusDocument11 pagesTka ValgusOvidiu RusuNo ratings yet
- Falez New Casella2018Document8 pagesFalez New Casella2018branislavNo ratings yet
- Deltoid Ligament Injuries Associated With Ankle Fractures - Argument For Repair of The Deltoid LigamentDocument3 pagesDeltoid Ligament Injuries Associated With Ankle Fractures - Argument For Repair of The Deltoid LigamentSaifuddin HaswareNo ratings yet
- Exam Corner - September 2012: The Bone & Joint Journal September 2012Document3 pagesExam Corner - September 2012: The Bone & Joint Journal September 2012Mohamad RamadanNo ratings yet
- Basti As 2020Document17 pagesBasti As 2020Martin MoranNo ratings yet
- MainDocument8 pagesMainRamy ElmasryNo ratings yet
- New Principles in Pilon Fractres ManagementDocument17 pagesNew Principles in Pilon Fractres ManagementCamila FontechaNo ratings yet
- Impact of Bone DecompensationDocument11 pagesImpact of Bone DecompensationDe La Cruz RodrigoNo ratings yet
- Orthodontically Driven Corticotomy: Tissue Engineering to Enhance Orthodontic and Multidisciplinary TreatmentFrom EverandOrthodontically Driven Corticotomy: Tissue Engineering to Enhance Orthodontic and Multidisciplinary TreatmentFederico BrugnamiNo ratings yet
- Estudio ComparativoDocument5 pagesEstudio ComparativoDaniel VideaNo ratings yet
- McGlamery Triple ArthrodesisDocument26 pagesMcGlamery Triple ArthrodesisTrudy SalmonNo ratings yet
- Chapter 25: Trauma: (Also See Chapter 19, Pediatrics)Document70 pagesChapter 25: Trauma: (Also See Chapter 19, Pediatrics)poddataNo ratings yet
- Ankle Fracture Fixation - Medial or Lateral First?Document5 pagesAnkle Fracture Fixation - Medial or Lateral First?Diana Marcela Benítez HernándezNo ratings yet
- Pes Cavus ....Document34 pagesPes Cavus ....Rupika Sodhi100% (2)
- Bleazey-2012-Recon of Complex Oc Lesions of The Talus With Cylindrical Sponge Allograft and Particulate Juvenile Cartilage GraftDocument7 pagesBleazey-2012-Recon of Complex Oc Lesions of The Talus With Cylindrical Sponge Allograft and Particulate Juvenile Cartilage Graftapi-212907483No ratings yet
- Anatomia e Biomecanica Pé e TornozeloDocument7 pagesAnatomia e Biomecanica Pé e TornozeloÉrica SilvaNo ratings yet
- Varus Knee Classification and CorrectionDocument8 pagesVarus Knee Classification and CorrectionPraharshaNo ratings yet
- Combined Massive Allograft and Intramedullary Vascularized Fibula Transfer The Capanna Technique For Treatment of Congenital Pseudarthrosis of TheDocument7 pagesCombined Massive Allograft and Intramedullary Vascularized Fibula Transfer The Capanna Technique For Treatment of Congenital Pseudarthrosis of TheHenrique NetoNo ratings yet
- Fai 2007 0529Document7 pagesFai 2007 0529milenabogojevskaNo ratings yet
- Article The Biomechanical Behavior of Distal Foot JointsDocument12 pagesArticle The Biomechanical Behavior of Distal Foot JointsAlessandro MedinaNo ratings yet
- Ankle Arthrodesis Using TSFDocument10 pagesAnkle Arthrodesis Using TSFSeagate PramonoNo ratings yet
- TFAS - 2017 - Davies - New Lateral Fixed Angle Locking AJ Arthrodesis Plate - Technique and Rate of UnionDocument8 pagesTFAS - 2017 - Davies - New Lateral Fixed Angle Locking AJ Arthrodesis Plate - Technique and Rate of UnionJacob DoughertyNo ratings yet
- A Flexion Osteotomy For Correction of A Distal Tibial Recurvatum Deformity - A Retrospective Case SeriesDocument9 pagesA Flexion Osteotomy For Correction of A Distal Tibial Recurvatum Deformity - A Retrospective Case SeriesHamelinYangNo ratings yet
- Giannini SERIDocument9 pagesGiannini SERISeagate PramonoNo ratings yet
- Research ArticleDocument5 pagesResearch ArticleZirco HereNo ratings yet
- Distraction Osteogenesis EbookDocument27 pagesDistraction Osteogenesis EbookSundeep SharmaNo ratings yet
- An Acetabular Fracture With A Series of Complications and Their Solutions A Notable Case ReportDocument6 pagesAn Acetabular Fracture With A Series of Complications and Their Solutions A Notable Case ReportAthenaeum Scientific PublishersNo ratings yet
- Article Touch 2021Document7 pagesArticle Touch 2021LedouxNo ratings yet
- Dynamic Arch Deformation and Its Consequence On Shoe DesignDocument2 pagesDynamic Arch Deformation and Its Consequence On Shoe DesignAbed SolimanNo ratings yet
- Nicholas B (2015) - Retrograde Intramedullary TibiotalocalcanealDocument11 pagesNicholas B (2015) - Retrograde Intramedullary TibiotalocalcanealHariom ShuklaNo ratings yet
- Realignment Surgery For Malunited Ankle Fracture: Clinical ArticleDocument5 pagesRealignment Surgery For Malunited Ankle Fracture: Clinical ArticleGio VandaNo ratings yet
- Evaluation PodiatricDocument4 pagesEvaluation Podiatricjona_kineNo ratings yet
- Chapter 21: Surgery of The Congenital FootDocument30 pagesChapter 21: Surgery of The Congenital FootpoddataNo ratings yet
- A Computer-Assisted Navigation Technique For Complex Primary Knee Arthroplasty With Intra-Articular Bone Defect and Instability: A Case Report and Literature ReviewDocument7 pagesA Computer-Assisted Navigation Technique For Complex Primary Knee Arthroplasty With Intra-Articular Bone Defect and Instability: A Case Report and Literature ReviewNorawee WainipitapongNo ratings yet
- Surgery First Using Skeletal Anchorage With Tandem Mechanics For Mandibular Molar DistalizationDocument13 pagesSurgery First Using Skeletal Anchorage With Tandem Mechanics For Mandibular Molar DistalizationMonojit DuttaNo ratings yet
- AAOS2001 ReconstructionDocument58 pagesAAOS2001 ReconstructionHéctor Pando SánchezNo ratings yet
- Effects of A Knee-Ankle-Foot Orthosis On Gait Biomechanical Characteristics of Paretic 2013Document6 pagesEffects of A Knee-Ankle-Foot Orthosis On Gait Biomechanical Characteristics of Paretic 2013josep ignasiNo ratings yet
- Minimalist Shoes Running Intervention Can Alter The Plantar Loadingdistribution and Deformation of Hallux Valgus A Pilot StudyDocument7 pagesMinimalist Shoes Running Intervention Can Alter The Plantar Loadingdistribution and Deformation of Hallux Valgus A Pilot StudyGourgen GevorgyanNo ratings yet
- Recurrent Giant Cell Tumour of Distal Tibia: Case Report and Review of The LiteratureDocument4 pagesRecurrent Giant Cell Tumour of Distal Tibia: Case Report and Review of The LiteratureAMBS ABMS JMAANo ratings yet
- Chapter LLDocument23 pagesChapter LLWalid AboNo ratings yet
- Cartilage Repair of The Talus: Dirk B. Scha Fer, MDDocument11 pagesCartilage Repair of The Talus: Dirk B. Scha Fer, MDAnonymous kdBDppigENo ratings yet
- Chapter 101. Primary Hip Arthroplasty - I. Total Hip ArthroplastyDocument65 pagesChapter 101. Primary Hip Arthroplasty - I. Total Hip ArthroplastyVanessa Yvonne GurtizaNo ratings yet
- Distal Amputations For The Diabetic Foot PDFDocument4 pagesDistal Amputations For The Diabetic Foot PDFGiuliana ReyesNo ratings yet
- Distal Humeral Fractures-Current Concepts PDFDocument11 pagesDistal Humeral Fractures-Current Concepts PDFRina AlvionitaNo ratings yet
- InTech-Management of Bone Loss in Primary and Revision Knee Replacement SurgeryDocument25 pagesInTech-Management of Bone Loss in Primary and Revision Knee Replacement SurgerySagaram ShashidarNo ratings yet
- Marcheggianimuccioli 2019Document12 pagesMarcheggianimuccioli 2019Ghusun MadaniNo ratings yet
- Management of Bone Defects in Primary Knee Arthroplasty: A Case ReportDocument4 pagesManagement of Bone Defects in Primary Knee Arthroplasty: A Case ReportInternational Journal of Recent Innovations in Academic ResearchNo ratings yet
- Pediatric Orthopaedics: Dr. Zairin Noor Helmi, Spot. (K) .MM - FicsDocument53 pagesPediatric Orthopaedics: Dr. Zairin Noor Helmi, Spot. (K) .MM - FicsmegaFitrianNo ratings yet
- Foot and Ankle Surgery: A.E.E.P.M. Leeuwesteijn M.D., E. de Visser M.D., PH.D., J.W.K. Louwerens M.D., PH.DDocument6 pagesFoot and Ankle Surgery: A.E.E.P.M. Leeuwesteijn M.D., E. de Visser M.D., PH.D., J.W.K. Louwerens M.D., PH.D杨明No ratings yet
- Arthrodesis Techniques in The Management of Stage II and III Acquired Adult Flatfoot Deformity.Document12 pagesArthrodesis Techniques in The Management of Stage II and III Acquired Adult Flatfoot Deformity.C Martin TraumatoNo ratings yet
- Ankle ArthrodesisDocument10 pagesAnkle ArthrodesisariearifinNo ratings yet
- Surgical Technique For Combined D Wyer Calcaneal Osteotomy and PeronealDocument6 pagesSurgical Technique For Combined D Wyer Calcaneal Osteotomy and PeronealleahbayNo ratings yet
- Multidirectional Instability of The Ankle: Surgical ReconstructionDocument7 pagesMultidirectional Instability of The Ankle: Surgical ReconstructionAnonymous kdBDppigENo ratings yet
- Ankle SprainsDocument18 pagesAnkle Sprainsnelson1313No ratings yet
- Changes in Femoral Stem Geometry Reduce Intraoperative Femoral Fracture Rates in Total Hip ReplacementDocument5 pagesChanges in Femoral Stem Geometry Reduce Intraoperative Femoral Fracture Rates in Total Hip Replacementeka henny suryaniNo ratings yet
- Forefoot Injuries in SportsDocument15 pagesForefoot Injuries in SportsJaume SanahujaNo ratings yet
- Use of External Fixation in The Reconstruction of The Charcot Foot and AnkleDocument21 pagesUse of External Fixation in The Reconstruction of The Charcot Foot and AnkleAnonymous kdBDppigENo ratings yet
- Ortho ArticleDocument2 pagesOrtho ArticleSamantha Dela Paz100% (1)
- THR DDH NeglectedDocument7 pagesTHR DDH NeglectedMohan DesaiNo ratings yet
- Cartilage Injury of the Knee: State-of-the-Art Treatment and ControversiesFrom EverandCartilage Injury of the Knee: State-of-the-Art Treatment and ControversiesAaron J. KrychNo ratings yet
- Dudda Et Al. - 2011 - Authors' ReplyDocument2 pagesDudda Et Al. - 2011 - Authors' ReplyYuki SATAKENo ratings yet
- Coste Et Al. - 1968 - Rheumatoid ForefootDocument2 pagesCoste Et Al. - 1968 - Rheumatoid ForefootYuki SATAKENo ratings yet
- DeGroot Et Al. - 2004 - Accumulation of Advanced Glycation End Products As A Molecular Mechanism For Aging As A Risk Factor in OsteoarthDocument9 pagesDeGroot Et Al. - 2004 - Accumulation of Advanced Glycation End Products As A Molecular Mechanism For Aging As A Risk Factor in OsteoarthYuki SATAKENo ratings yet
- DeGroot Et Al. - 2001 - Accumulation of Advanced Glycation Endproducts Reduces Chondrocyte-Mediated Extracellular Matrix Turnover in HumDocument7 pagesDeGroot Et Al. - 2001 - Accumulation of Advanced Glycation Endproducts Reduces Chondrocyte-Mediated Extracellular Matrix Turnover in HumYuki SATAKENo ratings yet
- EL 108 Midterm Module 1Document22 pagesEL 108 Midterm Module 1Ella Marie Gamayon PoloNo ratings yet
- Practical File (Class - Xii)Document179 pagesPractical File (Class - Xii)sachinclash24.4No ratings yet
- 7-Non Locomotor and Locomotor MovementDocument3 pages7-Non Locomotor and Locomotor MovementRylleMatthanCorderoNo ratings yet
- HDC Lesson 1 Body Mechanics NPCI Jan. 2021Document2 pagesHDC Lesson 1 Body Mechanics NPCI Jan. 2021cherryNo ratings yet
- Scaffold 2005-CDocument28 pagesScaffold 2005-CDennis SeparaNo ratings yet
- PDF Marathon Legs 07.13.20Document2 pagesPDF Marathon Legs 07.13.20Alberto Sáez CastilloNo ratings yet
- Self Assisted Techniques ROM Lec 5Document19 pagesSelf Assisted Techniques ROM Lec 5Hareem FatimaNo ratings yet
- 01 EHS Training PPE - EnglishDocument22 pages01 EHS Training PPE - EnglishMarthaNo ratings yet
- Keeping Horses Barefoot A Shared AccomplishmentDocument320 pagesKeeping Horses Barefoot A Shared AccomplishmentRenata C CalfatNo ratings yet
- Full Body MobilityDocument8 pagesFull Body MobilityMARIA PAULA GOMEZ CEBALLOSNo ratings yet
- PE 2 - Module 3Document5 pagesPE 2 - Module 3Agbon TangogNo ratings yet
- Assistive DevicesDocument11 pagesAssistive Devicesshifali guptaNo ratings yet
- ICAR Claw Health Key Coding 20180921Document8 pagesICAR Claw Health Key Coding 20180921junjunNo ratings yet
- 1rki Physical AssesmentDocument18 pages1rki Physical AssesmentIrfan NasrullahNo ratings yet
- Yoga For The Core - Finding Stability in An Unstable Environment PDFDocument11 pagesYoga For The Core - Finding Stability in An Unstable Environment PDFlilguy00100No ratings yet
- Bandaging in Emergencies - 2022Document152 pagesBandaging in Emergencies - 2022Derick Sem100% (1)
- BANDAGING ProcedureDocument6 pagesBANDAGING ProcedureAngelie PantajoNo ratings yet
- Seated Elastic Band Exercise For Foot DropDocument2 pagesSeated Elastic Band Exercise For Foot DropDennis Diaz AgapitoNo ratings yet
- Falling, Impact, Acceleration, Lifting, and Vision HazardsDocument60 pagesFalling, Impact, Acceleration, Lifting, and Vision HazardsAlex CastroNo ratings yet
- Module 3-Anatomy and Physiology (Abegail Relunia - Bsed3-C Science) )Document3 pagesModule 3-Anatomy and Physiology (Abegail Relunia - Bsed3-C Science) )Abegail ReluniaNo ratings yet
- Ejercicios para El Suelo Pelvico Nivel Facil Moderado Dificil yDocument46 pagesEjercicios para El Suelo Pelvico Nivel Facil Moderado Dificil yDilan LinaresNo ratings yet
- Sports Medicine 10-Lesson 4 - Lower Leg Muscles Turf ToeDocument5 pagesSports Medicine 10-Lesson 4 - Lower Leg Muscles Turf Toeapi-383568582No ratings yet
- Head To Toe StretchDocument3 pagesHead To Toe StretchZAIRA N. CNo ratings yet
- Safety Measures in Doing Household TasksDocument30 pagesSafety Measures in Doing Household TasksEdchel Espeña100% (1)
- Ankle Foot OrthosisDocument4 pagesAnkle Foot Orthosis楊畯凱No ratings yet
- Super Band: #BettereverydayDocument2 pagesSuper Band: #BettereverydayDkyNo ratings yet
- Nadine George Breath Work: VOICE - Breath and RelaxationDocument2 pagesNadine George Breath Work: VOICE - Breath and RelaxationlolaestradaNo ratings yet
- Sprinting ShoesDocument48 pagesSprinting ShoesSoumya BhattNo ratings yet
- 2019051029Document20 pages2019051029BagusNo ratings yet
- Exercises For Chronic Neck Pain: StrengtheningDocument3 pagesExercises For Chronic Neck Pain: Strengtheningmelvin ekboteNo ratings yet