Professional Documents
Culture Documents
Diabetes Summary
Uploaded by
christine gisembaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diabetes Summary
Uploaded by
christine gisembaCopyright:
Available Formats
Symptoms of Diabetes Mellitus
❚❚ Frequent urination (polyuria)
❚❚ Dehydration, dry mouth
❚❚ Excessive thirst (polydipsia)
❚❚Weight loss
❚❚ Excessive hunger (polyphagia)
❚❚ Blurred vision
❚❚ Increased infections
❚❚ Fatigue
KEY WORDS
Diabetes -a group of metabolic disorders characterized by hyperglycemia and disordered insulin metabolism.
❚ diabetes 5 siphon (in Greek), referring to the excessive passage of urine that is characteristic of untreated diabetes
❚ mellitus 5 sweet, honeylike insulin: a pancreatic hormone that regulates glucose metabolism; its actions are countered mainly by the hormone
glucagon.
renal threshold: the blood concentration of a substance that exceeds the kidneys’ capacity for reabsorption, causing the substance
to be passed into the urine.
hyperosmolar: having an abnormally high osmolarity; osmolarity refers to the concentration of osmotically
active particles in solution. Hyperglycemia may cause some body fluids to become hyperosmolar.
oral glucose tolerance test: a test that evaluates a person’s ability to tolerate an oral glucose load.
glycated hemoglobin (HbA1c): hemoglobin that has nonenzymatically attached to glucose; the level of HbA1c in the blood helps to
diagnose diabetes and evaluate long-term glycemic control. Also called glycosylated hemoglobin.
acetone breath: a distinctive fruity odor on the breath of a person with ketosis.
Albuminuria: the presence of albumin (a blood protein) in the urine, a sign of diabetic nephropathy.
Claudication (CLAW -dih-KAY -shun): pain in the legs while walking; usually due to an inadequate supply
of blood to muscles.
Diabetic coma: a coma that occurs in uncontrolled diabetes; may be due to diabetic ketoacidosis, the
hyperosmolar hyperglycemic syndrome, or severe hypoglycemia. Diabetic coma was a frequent cause of
death before insulin was routinely used to manage diabetes.
Diabetic nephropathy (neh-FRAH-pah-thee): damage to the kidneys that results from long-term
diabetes.
Diabetic neuropathy (nur-RAH-pah-thee): nerve damage that results from long-term diabetes.
Diabetic retinopathy (REH-tih-NAH-pah-thee): retinal damage that results from long-term diabetes.
Gangrene: death of tissue due to a deficient blood supply and/or infection.
Gastroparesis (GAS-tro-pah-REE-sis): delayed stomach emptying caused by nerve damage in stomach
tissue.
Glycosuria (GLY -co-SOOR-ee-ah): the presence of glucose in the urine.
hyperglycemia: elevated blood glucose concentrations.
Normal fasting plasma glucose levels are less than 100 mg/dL.
Fasting plasma glucose levels between 100 and 125 mg/dL suggest prediabetes; values of 126 mg/dL
and above suggest diabetes.
hyperosmolar hyperglycemic syndrome: a condition of extreme hyperglycemia associated with
dehydration, hyperosmolar blood, and altered mental status; sometimes called the hyperosmolar
hyperglycemic nonketotic state.
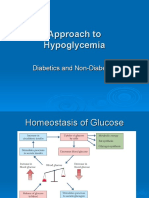
hypoglycemia: abnormally low blood glucose concentrations. In diabetes, hypoglycemia is treated when
plasma glucose falls below 70 mg/dL.
ketoacidosis (KEY-to-ass-ih-DOE-sis): an acidosis (lowering of blood pH) that results from the excessive
production of ketone bodies.
ketonuria (KEY-to-NOOR-ee-ah): the presence of ketone bodies in the urine.
ketosis (key-TOE-sis): elevated levels of ketone bodies in the body.
macrovascular complications: disorders that affect large blood vessels, including the coronary arteries
and arteries of the limbs.
microvascular complications: disorders that affect small bloodvessels, including those in the retina and
kidneys.
peripheral vascular disease: a condition characterized by impaired blood circulation in the limbs.
polydipsia (POL-ee-DIP-see-ah): excessive thirst.
polyphagia (POL-ee-FAY -jee-ah): excessive appetite or hunger.
polyuria (POL-ee-YOOR-ee-ah): excessive urine production.
prediabetes: the state of having plasma glucose levels that are higher than normal but not high enough
to be diagnosed as diabetes (100–125 mg/dL when fasting or 140–199 mg/dL when measured two hours
after ingesting 75 grams of glucose); occurs in individuals who have metabolic defects that often lead to
type 2 diabetes. type 1 diabetes: diabetes that is characterized by absolute insulin deficiency, usually
resulting from the autoimmune destruction of pancreatic beta cells.
autoimmune: refers to an immune response directed against the body’s own tissues.
Strategies for diabetes prevention may include:
❚❚ Loose weight if overweight or obese, or prevent additional weight gain
❚❚ Perform at least 150 minutes of moderate physical activity weekly
❚❚ Increase intake of whole grains and dietary fiber; limit intake of sugar-sweetened
foods and beverages
❚❚ Monitor health status with yearly check-ups
In Summary
❚❚ Diabetes mellitus is a chronic condition characterized by inadequate insulin secretion and/or impaired
insulin action; diagnosis is based on indicators of hyperglycemia.
❚❚ In type 1 diabetes, the pancreas secretes little or no insulin, and insulin therapy is necessary for
survival. Type 2 diabetes is characterized by insulin resistance coupled with relative insulin deficiency.
❚❚ Acute complications of poorly controlled diabetes include diabetic ketoacidosis, in which
hyperglycemia is accompanied by ketosis and acidosis; the hyperosmolar hyperglycemic syndrome,
characterized by severe hyperglycemia, dehydration, and mental impairments; and hypoglycemia, which
most often results from inappropriate disease management.
❚❚ Chronic complications of diabetes include macrovascular disorders such as cardiovascular disease and
peripheral vascular disease, microvascular conditions such as retinopathy and nephropathy, and
neuropathy.
You might also like
- Solutions to Diabetes and Hypoglycemia (Translated): How to prevent and get rid of it in a natural way, without resorting to medicines but adopting a correct way of lifeFrom EverandSolutions to Diabetes and Hypoglycemia (Translated): How to prevent and get rid of it in a natural way, without resorting to medicines but adopting a correct way of lifeNo ratings yet
- 9 - Assessment and Management of Patients With Diabetes MellitusDocument60 pages9 - Assessment and Management of Patients With Diabetes Mellitussohaib salamehNo ratings yet
- Diabetic Cooking for One and TwoFrom EverandDiabetic Cooking for One and TwoRating: 3 out of 5 stars3/5 (1)
- Blood Glucose Practical Handout For 2nd Year MBBSDocument10 pagesBlood Glucose Practical Handout For 2nd Year MBBSIMDCBiochemNo ratings yet
- Chapter 4 Carbohydrate DisorderDocument26 pagesChapter 4 Carbohydrate DisorderNida RidzuanNo ratings yet
- Hand Out DM Medical Surgical Nursing 2Document11 pagesHand Out DM Medical Surgical Nursing 2Zarlou OtamiasNo ratings yet
- Soluzioni al Diabete e all'Ipoglicemia - Come prevenire e disfarsene naturalmente e senza medicineFrom EverandSoluzioni al Diabete e all'Ipoglicemia - Come prevenire e disfarsene naturalmente e senza medicineNo ratings yet
- Type 1 Diabetes Mellitus Nael HernandezDocument15 pagesType 1 Diabetes Mellitus Nael HernandezShermayne Mallapre HernandezNo ratings yet
- Diabetes: Jumarang, Kim Enrico M. BSN401 STI - Global CityDocument5 pagesDiabetes: Jumarang, Kim Enrico M. BSN401 STI - Global CityKim Enrico JumarangNo ratings yet
- Diabetic Recipes for One and TwoFrom EverandDiabetic Recipes for One and TwoRating: 3 out of 5 stars3/5 (1)
- Diabetes Mellitus DMC 6th SemesterDocument23 pagesDiabetes Mellitus DMC 6th SemesterHuzaifa CHNo ratings yet
- Hypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandHypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Insulin Secretion and FunctionDocument8 pagesInsulin Secretion and FunctionWendy EscalanteNo ratings yet
- Metabolic Disorders Diabetes HandoutDocument21 pagesMetabolic Disorders Diabetes HandoutEdelen GaleNo ratings yet
- Diabetes NotesDocument10 pagesDiabetes Notestripj33No ratings yet
- Diabetes OutlineDocument7 pagesDiabetes OutlineJenny VargheseNo ratings yet
- DiabetesDocument99 pagesDiabetes489226fahimNo ratings yet
- Causes of Metabolic AcidosisDocument10 pagesCauses of Metabolic AcidosisKimberly Anne SP PadillaNo ratings yet
- Practical Biochemistry: Number of Experiment: (1) Name of Exp.:-Blood Glucose TestDocument6 pagesPractical Biochemistry: Number of Experiment: (1) Name of Exp.:-Blood Glucose TestHiba EmadNo ratings yet
- REVALIDADocument53 pagesREVALIDAMercy Anne EcatNo ratings yet
- REVALIDADocument53 pagesREVALIDAMercy Anne EcatNo ratings yet
- Diabetes Millitus PDFDocument41 pagesDiabetes Millitus PDFAbdullah BhattiNo ratings yet
- Problem 11 Study Guide 1 1.discuss Type 2 DM and Its PathophysiologyDocument68 pagesProblem 11 Study Guide 1 1.discuss Type 2 DM and Its PathophysiologyAnishilNo ratings yet
- Case Study of DMDocument6 pagesCase Study of DMbuzz Q0% (1)
- Glucose, Part1Document33 pagesGlucose, Part1SarahNo ratings yet
- 01 - CLS 382 - 443 - DMDocument19 pages01 - CLS 382 - 443 - DMamalNo ratings yet
- Lecture 1 Carbohydrate 1Document39 pagesLecture 1 Carbohydrate 1mer12sswNo ratings yet
- Diabetes MellitusDocument31 pagesDiabetes MellitusElenaCondratscribdNo ratings yet
- Diabetes MellitusDocument6 pagesDiabetes MellituscrisrimartNo ratings yet
- Diabetis Mellitus Case StudyDocument16 pagesDiabetis Mellitus Case StudyJim Davis RNNo ratings yet
- Hyperglycemia 131115111956 Phpapp02Document27 pagesHyperglycemia 131115111956 Phpapp02tiaraherianNo ratings yet
- Blood GlucoseDocument8 pagesBlood Glucoseعبدالرحمن عابدNo ratings yet
- Diabetes Mellitus: NZ Diploma in Enrolled NursingDocument38 pagesDiabetes Mellitus: NZ Diploma in Enrolled NursingRegina PunNo ratings yet
- Diabetes Mellitus LectureDocument68 pagesDiabetes Mellitus LectureDikyAksiramNo ratings yet
- Diabetes Mellitus, Disorder Of: Institute For BiotechnologyDocument10 pagesDiabetes Mellitus, Disorder Of: Institute For BiotechnologyAndre Jonathan Siàńsàkà IINo ratings yet
- Metabolic SyndromeDocument55 pagesMetabolic SyndromeAakash BalasubramanianNo ratings yet
- Diabetes Diabetes InformationDocument15 pagesDiabetes Diabetes InformationbalatnplNo ratings yet
- DIABETES MELLITUS FinalDocument83 pagesDIABETES MELLITUS FinalYuvi Yuvaraj100% (1)
- Diabetes MellitusDocument10 pagesDiabetes Mellitusjoeln_9No ratings yet
- DM Case Study - Nursing CribDocument6 pagesDM Case Study - Nursing CribFrancis VillanuevaNo ratings yet
- DiabetesmellitusDocument24 pagesDiabetesmellitusSania SaeedNo ratings yet
- HypoglycemiaDocument68 pagesHypoglycemialiaputranti100% (3)
- Diabetes Mellitus: Risks FactorsDocument5 pagesDiabetes Mellitus: Risks FactorsAmer Abdulla SachitNo ratings yet
- Wepik Understanding Diabetes Mellitus A Comprehensive Analysis of Causes Management and Prevention 20231126074011dxZFDocument15 pagesWepik Understanding Diabetes Mellitus A Comprehensive Analysis of Causes Management and Prevention 20231126074011dxZFtripathyabinash39No ratings yet
- DiabetesDocument81 pagesDiabetesJustin MutuaNo ratings yet
- Diabetes InfoDocument24 pagesDiabetes Infoalle manoharNo ratings yet
- 06.disorder of Carbohydrate MetabolismDocument47 pages06.disorder of Carbohydrate MetabolismRizka NizarNo ratings yet
- Diabete Mellitus HandoutsDocument7 pagesDiabete Mellitus HandoutsSittie Nashieva A. UsmanNo ratings yet
- Diabetes MellitusDocument85 pagesDiabetes MellitusPriyanka Hr GowdaNo ratings yet
- CARBOHYDRATE METABOLISM AND DISORDERS (Herbal Med)Document44 pagesCARBOHYDRATE METABOLISM AND DISORDERS (Herbal Med)AhjNo ratings yet
- Diabetes and MassageDocument23 pagesDiabetes and MassagemassagekevinNo ratings yet
- REVALIDADocument49 pagesREVALIDAMercy Anne EcatNo ratings yet
- Diabetes MellitusDocument11 pagesDiabetes MellitusRoshni JemimahNo ratings yet
- Diabetes PPT FianlDocument31 pagesDiabetes PPT FianlUqba MishalNo ratings yet
- DIABETISDocument52 pagesDIABETISNeeraja M SureshNo ratings yet
- Responses To Metabolic Gi Liver Alterations Compiled HandoutsDocument185 pagesResponses To Metabolic Gi Liver Alterations Compiled HandoutsJoanna Taylan100% (1)
- Diagnosis of Diabetes MellitusDocument23 pagesDiagnosis of Diabetes MellitusNkosinathi ShongweNo ratings yet
- Elements of PHCDocument38 pagesElements of PHCchristine gisembaNo ratings yet
- Diet Therapy 1Document2 pagesDiet Therapy 1christine gisembaNo ratings yet
- Osh Notes Lecturer 1 and 2Document100 pagesOsh Notes Lecturer 1 and 2christine gisembaNo ratings yet
- PHC Short NotesDocument17 pagesPHC Short Noteschristine gisembaNo ratings yet
- PHC 1Document11 pagesPHC 1christine gisembaNo ratings yet
- PHC 2Document10 pagesPHC 2christine gisembaNo ratings yet
- COMMUNICABLE AND NCDsDocument147 pagesCOMMUNICABLE AND NCDschristine gisembaNo ratings yet
- Family Planning MethodsDocument1 pageFamily Planning Methodschristine gisembaNo ratings yet
- Primary Health CareDocument119 pagesPrimary Health Carechristine gisembaNo ratings yet
- KU - Lesson 5 - Drugs For Hyperlipidaemia PDFDocument51 pagesKU - Lesson 5 - Drugs For Hyperlipidaemia PDFchristine gisembaNo ratings yet
- KU - Lesson 4A - DRUGS USED IN ANAEMIADocument60 pagesKU - Lesson 4A - DRUGS USED IN ANAEMIAchristine gisembaNo ratings yet
- COMMUNICABLE AND NCDsDocument147 pagesCOMMUNICABLE AND NCDschristine gisembaNo ratings yet
- Relation of A Variant in Adiponectin Gene (rs266729) With Metabolic Syndrome and Diabetes Mellitus Type 2 in Adult Obese SubjectsDocument7 pagesRelation of A Variant in Adiponectin Gene (rs266729) With Metabolic Syndrome and Diabetes Mellitus Type 2 in Adult Obese SubjectsVivi yenni aryantiNo ratings yet
- SOAP Note DiabetesDocument16 pagesSOAP Note Diabetesmichael thorn92% (25)
- The Human Machine by RL Bijlani, SK ManchandaDocument176 pagesThe Human Machine by RL Bijlani, SK ManchandaMUSKANNo ratings yet
- Resume ClaireDocument2 pagesResume Claireapi-548863648No ratings yet
- DAS Research Version 2.docx: Paper NameDocument43 pagesDAS Research Version 2.docx: Paper Namemiko balisiNo ratings yet
- Diagnosis and Management of Type 2 Diabetes Mellitus ©stephen D. Sisson MD/Ambulatory Curriculum 2021Document48 pagesDiagnosis and Management of Type 2 Diabetes Mellitus ©stephen D. Sisson MD/Ambulatory Curriculum 2021Carolina González RiveraNo ratings yet
- Conceptual Map - Diabetic KetoacidosisDocument2 pagesConceptual Map - Diabetic KetoacidosisLovie Japhet LopezNo ratings yet
- RWAnda NCD Strategic PlanDocument66 pagesRWAnda NCD Strategic PlanMoss MbuguaNo ratings yet
- DiabetesDocument6 pagesDiabetesnayraNo ratings yet
- Standards of Care in Diabetes - 2024Document13 pagesStandards of Care in Diabetes - 2024Areshmi Gómez MendiolaNo ratings yet
- Hba1C Study: 51 Years /femaleDocument4 pagesHba1C Study: 51 Years /femalesangani.gayatriNo ratings yet
- Diabetes Self-Management Questionnaire (DSMQ)Document2 pagesDiabetes Self-Management Questionnaire (DSMQ)Wayan SugitaNo ratings yet
- Diabetes Medication ChartDocument21 pagesDiabetes Medication CharttmleNo ratings yet
- The Integrative Biology of Type 2 DiabetesDocument10 pagesThe Integrative Biology of Type 2 DiabetesAdrian GhiţăNo ratings yet
- Procedure Urine Test For Sugar and AlbuminDocument5 pagesProcedure Urine Test For Sugar and AlbuminVaishali SinghNo ratings yet
- Effect of Variability of Hemoglobin Value On Type and Severity of Diabetic Retinopathy in Adult Type II Diabetes Mellitus PatientsDocument11 pagesEffect of Variability of Hemoglobin Value On Type and Severity of Diabetic Retinopathy in Adult Type II Diabetes Mellitus PatientsInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Riska Amelia, A. Mushawwir Taiyeb, Irma Suryani IdrisDocument11 pagesRiska Amelia, A. Mushawwir Taiyeb, Irma Suryani IdrisÈkä Sêtýä PrätämäNo ratings yet
- Terapi Farmakologi Diabetes Mellitus IIKDocument40 pagesTerapi Farmakologi Diabetes Mellitus IIKDewi PatniNo ratings yet
- Office of The SecretaryDocument15 pagesOffice of The SecretaryPatricia CastellanoNo ratings yet
- Diabetes Mellitus in ChildrenDocument98 pagesDiabetes Mellitus in ChildrenBuyinza mihadNo ratings yet
- Green Tea and Its BenefitsDocument1 pageGreen Tea and Its BenefitsVine CorpzNo ratings yet
- Contoh Kuasi EksperimentalDocument7 pagesContoh Kuasi EksperimentalNovita SariNo ratings yet
- Prevalence of Diabetes Mellitus Among Female 15 Years and Above in KuringafaDocument57 pagesPrevalence of Diabetes Mellitus Among Female 15 Years and Above in KuringafaUsman Ahmad TijjaniNo ratings yet
- Daftar PustakaDocument5 pagesDaftar PustakafiqhiNo ratings yet
- Pengaruh Senam Kaki Terhadap Kadar Glukosa Darah Dan Nilai ABI Penderita DMDocument6 pagesPengaruh Senam Kaki Terhadap Kadar Glukosa Darah Dan Nilai ABI Penderita DMSetyardiNo ratings yet
- BDJ Perio and DiabetesDocument8 pagesBDJ Perio and DiabetesGowriNo ratings yet
- The Care Process of Diabetic Foot Ulcer Patients: A Qualitative Study in IranDocument5 pagesThe Care Process of Diabetic Foot Ulcer Patients: A Qualitative Study in IranSofyan IndrayanaNo ratings yet
- Teaching Experience LogDocument2 pagesTeaching Experience Logapi-668844754No ratings yet
- Definition of DiabetesDocument6 pagesDefinition of DiabetesSuyi PhoebeNo ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!From EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Rating: 5 out of 5 stars5/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)From EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Rating: 4 out of 5 stars4/5 (378)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)