Professional Documents
Culture Documents
Audio Bailey
Uploaded by
Monisa HiraOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Audio Bailey
Uploaded by
Monisa HiraCopyright:
Available Formats
Pure-Tone Audiometry
Pure-tone audiometry is the most common measurement
of hearing sensitivity. Stimuli are pure tones (sinusoids)
at octave frequencies typically from 250 Hz up to 8,000
2274
Hz and, often, two interoctave frequencies (3,000 Hz and
6,000 Hz). Interoctave hearing loss is a characteristic of
commonly encountered problems, such as noise-induced
cochlear dysfunction. High-frequency audiometry for stimulus frequencies greater than 8,000 Hz (up to
20,000 Hz)
is technically feasible and clinically useful to certain populations, such as patients at risk for ototoxicity.
Test results
in many clinics are graphed on an audiogram. Two versions of audiograms are illustrated in Figure 142.1.
All
audiograms include at the minimum a graph for plotting
hearing threshold levels as a function of the frequency of
pure-tone signals, although the exact format and symbols
vary.
The unit of stimulus intensity is the decibel (dB), a
logarithmic unit. The intensity of any sound is defined
by the ratio of its sound pressure or sound intensity to a
reference sound pressure or sound intensity. The reference
sound pressure is the amount of pressure against the eardrum, caused by air molecules when a sound is
present,
that vibrates the eardrum and can just be detected by a
normal human ear. Briefly, the relation for sound intensity is described as dB= 10 log10 (sound
intensity/reference
intensity) or for sound pressure as dB = 20 log10 (sound
pressure/reference pressure). The reference sound pressure
is defined as decibels sound pressure level ( dBSPL) and is
derived from one of two physical quantities: (a) 0.0002
dynefcm2 or (b) 20 micropascals root mean square (J.lPa)
= 2 x lQ-5 Pa.
Clinically, the intensity of sound is described in decibels
hearing level (dB HL), a biologic reference level, rather than
in sound pressure level. On an audiogram (Fig. 142.1), the
decibel scale has as its reference 0 dB, which is described as
audiometric 0. This is the standard for the intensity level
that corresponds to the mean normal hearing threshold
level, the minimal detectable intensity for each test frequency for young adults with normal hearing.
Another
common unit for expressing sound intensity is decibels sensation level (dB SL), which is intensity of the
stimulus
in decibels above an individual's hearing threshold. For
example. a word recognition test can be administered at an
intensity level of 40 dB SL ( 40 dB above the person's puretone average [PTA]).
In audiologic assessment of cooperative children
and adults, hearing thresholds for tonal or speech signals are measured separately for each ear with
earphones
(air-conduction stimulation). Insert earphones (ER-3A)
are now the transducer of choice for routine audiologic
assessment. They offer distinct advantages over traditional supraaural earphones, including increased
comfort,.
reduced likelihood of ear canal collapse, greater interaural
attenuation. and greater acceptance by young children. In
addition. insert earphones contribute importantly to the
control of infection in a clinical setting, as the insert portion is disposable. Pure-tone audiometry can be
performed
with stimuli presented with a bone-conduction oscillator
or vibrator placed on the mastoid bone. During pure-tone
audiometry, all equipment must meet the specifications of
theAmericanNational Standards Institute (ANSI). Periodic
equipment calibration and validation are necessary. Testing
is conducted according to clinical adaptations of psychoacoustic methods (1). Patients are instructed to
listen carefully for the tones and to respond, usually by pushing a
button that activates a response light on the audiometer or
by raising a hand, every time they believe they hear a tone.
To minimize interference by ambient background acoustic
noise. pure-tone audiometry always is performed with the
patient in a double-walled, sound-treated room that meets
ANSI specifications.
The clinically normal region on an audiogram is 0 to
20 dB HL, although for children hearing threshold levels exceeding 15 dB should be considered
abnormal.
Thresholds in the 20 to 40 dB HL region constitute mild
hearing loss, 40 to 60 dB HL thresholds define moderate
loss, and threshold levels greater than 60 dB HL are considered severe hearing loss (2). As a reference.
the intensity
level of whispered speech close to the ear is less than 25 dB
HL. Conversational speech is in the 40 to 50 dB HL region,
and a shouted voice within 1 foot (30 em) of the ear is at
a level of about 80 dB HL. The most important frequencies for understanding speech are 500 through
4,000 Hz,
although higher frequencies can contribute to discrimination between certain speech sounds. Hearing
sensitivity
within the speech frequency region often is summarized by
means of calculation of the PfA (PTA; hearing thresholds
for 500, 1,000, and 2,000 Hz divided by three and reported
in decibels). A four-frequency PfA including 3,000 Hz is
required by the American Academy of OtolaryngologyHead and Neck Surgery.
Audiometric results are valid only when the patient's
responses are caused by stimulation of the test ear. If a
sound greater than 40 dB HL is presented to one ear through
air conduction with supraaural earphones and cushions
(resting on the outer ear), the acoustic energy can cross
over from one side of the head to the other and stimulate
the ear not being tested. The main mechanism of crossover
is presumed to be bone-conduction stimulation caused by
vibration of the earphone cushion against the skull at high
stimulus intensity levels. The amount of sound intensity
needed before crossover occurs is a reflection of interaural
attenuation, that is, the sound insulation between the two
ears provided by the head. Interaural attenuation is usually
about 50 dB for lower test frequencies and 60 dB for higher
test frequencies, such as those contributing to the ABR.
Interaural attenuation is considerably higher for insert earphones (2). With bone-conduction
stimulation, interaural
attenuation is less than 10 dB. In clinical circumstances, the
examiner needs to assume conservatively that interaural
attenuation for bone-conducted signals is 0 dB. In other
words, even a very faint sound presented to the mastoid
bone of one ear by a bone-conduction vibrator can be
transmitted through the skull to either or both inner ears.
Perception of this bone-conducted signal depends on the
patient's sensorineural hearing sensitivity in each ear.
Masking is the audiometric technique used to eliminate participation of the ear not being tested
whenever
air- and bone-conduction stimulation exceeds interaural
attenuation. An appropriate noise (narrow-band noise for
pure-tone signals and speech noise for speech signals) is
presented to the ear not being tested when the stimulus
is presented to the test ear. With adequate masking, any
signal crossing over to the ear not being tested is masked
by the noise. The level of masking noise presented to the
ear not being tested must exceed the threshold of hearing for that ear. Excess levels of masking noise
must be
avoided because the noise can cross back over to the ear
being tested. Selection of appropriate masking can be difficult, especially when there is bilateral hearing
loss (2).
Indeed, patients with severe bilateral conductive hearing
loss may present the "masking dilemma," that is, when
enough masking to the nontest ear actually crosses over to
the test ear and interferes with accurate estimation of hearing threshold. An otolaryngologist
interpreting audiologic
results must verify that appropriate masking was used if
testing was not performed by an audiologist.
Knowledge of the type of hearing loss, determined by
means of comparison of the hearing thresholds for air- and
bone-conduction signals, is useful in classifying a hearing loss as sensorineural (no air-bone gap),
conductive
(normal bone conduction and a loss by air conduction),
or mixed (loss by bone conduction with a superimposed
air-bone conduction gap).
Configuration refers to hearing loss as a function of
the test frequency. With a sloping configuration, hearing
is better for low frequencies and then becomes poorer for
higher frequencies. The most common pattern associated
with sensorineural hearing loss is a deficit in thresholds
for higher test frequencies. The configuration can be gently sloping from low to high frequencies, be
precipitously
decreasing above a high frequency cutoff, such as 2,000 Hz, or be characterized by a notching deficit
within a certain
frequency region,. such as 4,000 Hz. A rising configuration is typified by relatively poor hearing for low-
frequency
stimuli and better hearing for the high frequencies. A rising configuration can be caused by varied types
of middle
ear abnormalities. An exception to the typical association of
conductive hearing loss with rising configuration is Meniere
disease (see Chapter 156). Meniere disease is one cochlear
abnormality that may produce a rising configuration. A flat
audiometric configuration often is recorded from patients
with mixed hearing loss, that is, both sensorineural and
conductive components are present Other configurations,
such as the midfrequency "cookie bite" pattern,. are encountered in clinical practice. Test-retest
variability in clinical
pure-tone threshold estimation is typically ±5 dB.
Guidelines for Evaluation of Hearing
Handicap
The results of pure-tone audiometry are adequately summarized in an audiogram and with the terms
just defined, such
as PIA and the degree.. configuration, and type of hearing
loss. It also is possible to quantify hearing loss in percentage units according to published and accepted
guidelines
(3). This approach sometimes is necessary in medicolegal
cases or when a patient seeks compensation for hearing
loss. According to the guidelines of the American Academy
of Otolaryngology Committee on Hearing and Equilibrium
and the American Council of Otolaryngology Committee
on the Medical Aspects of Noise (3), permanent hearing
impairment is defined as follows: "A change for the worse
in either structure or function, outside the range of normal,
is permanent impairment.... Permanent impairment is
due to any anatomic or functional abnormality that produces hearing loss." This is differentiated from
permanent
hearing handicap, which is defined as follows: "The disadvantage imposed by an impairment sufficient to
affect
a person's efficiency in the activities of daily living is a permanent handicap" (3). The guidelines also
detail the
approach for converting hearing handicap for one or both
ears into a percentage. The first step is to determine the
degree of sensorineural hearing loss for four test frequencies (500, 1,000,2,000, and 3,000 Hz) from the
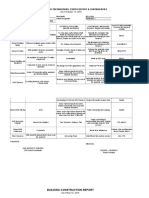
audiogram
(Table 142.1). The next step is to follow the guidelines for
computation of percentage hearing loss (3):
If the monaural percent figure is the same for both ears,
that figure expresses the percent hearing handicap. If
the percent monaural hearing impairments are not
the same, apply the formula:
( 5 x % [better ear]) + ( 1 x % [poorer ear]) /6 = %
hearing handicap
The interoctave test frequency-3,000 Hz-in the calwlation of percentage of hearing handicap is very
important. It is good clinical practice to routinely obtain hearing thresholds
from each ear for the 3,000 Hz frequency. This frequency is
included in the formula for hearing loss (3) because much
of the spectral information vital for speech understanding is
within the 2,000 to 3,000 Hz region. Percentage of binaural
hearing handicap is easily calculated with a detailed tabular
matrix that relates the four-frequency degree of sensorineural
hearing loss for the better versus poorer ear ( 4 ).
You might also like
- Pure Tone AudiometryDocument8 pagesPure Tone AudiometrySuhaimi RostiNo ratings yet
- Assessing Peripheral and Central Hearing FunctionDocument10 pagesAssessing Peripheral and Central Hearing Functionagung anugrahNo ratings yet
- Audiology Pure-Tone TestingDocument9 pagesAudiology Pure-Tone TestingTomás LuisNo ratings yet
- AudiometryDocument5 pagesAudiometrykazchandranNo ratings yet
- 004 Noise Induced Hearing Loss and AudiometryDocument51 pages004 Noise Induced Hearing Loss and AudiometryISCRRNo ratings yet
- FlashcardsDocument140 pagesFlashcardsDoodNo ratings yet
- Rehab - Hi (New)Document3 pagesRehab - Hi (New)devNo ratings yet
- Tes Garpu TalaDocument13 pagesTes Garpu TalaSamuel ChristianNo ratings yet
- Lecture 2 - Audiometry PracticalDocument42 pagesLecture 2 - Audiometry PracticalSaera Hafiz Nikita100% (1)
- Current Diagnosis & Treatment in Otolaryngology—Head & Neck SurgeryDocument3 pagesCurrent Diagnosis & Treatment in Otolaryngology—Head & Neck SurgeryStephanie Vania EmbangNo ratings yet
- How To Read Audiogram ResultsDocument22 pagesHow To Read Audiogram ResultsHey hey100% (2)
- AudiometryDocument2 pagesAudiometryRajesh ChundiNo ratings yet
- Theory and Practice of Pure Tone Audiometry - PTADocument12 pagesTheory and Practice of Pure Tone Audiometry - PTAsolhazNo ratings yet
- Lecture 1Document27 pagesLecture 1stt5xyxq75No ratings yet
- Hearing Loss - A Clinical ApproachDocument70 pagesHearing Loss - A Clinical ApproachJohnson Jayaraj100% (2)
- Hearing TestingDocument6 pagesHearing TestingMelody RodriguezNo ratings yet
- Test of Hearing and Pure Tone AudiometryDocument35 pagesTest of Hearing and Pure Tone AudiometryarjumandNo ratings yet
- Audiometers OK PDFDocument81 pagesAudiometers OK PDFErnesto AcostaNo ratings yet
- Auditory Tests With Disease Specific SignificanceDocument60 pagesAuditory Tests With Disease Specific SignificanceSonal SharmaNo ratings yet
- Element 5Document38 pagesElement 5Farooq MohammadNo ratings yet
- Media 4520 SMXXDocument24 pagesMedia 4520 SMXXAnjela ChakhoyanNo ratings yet
- Hearing AssessmentDocument30 pagesHearing AssessmentRitesh SuranaNo ratings yet
- Aud4001 Lecture NotesDocument13 pagesAud4001 Lecture NotesjazmashNo ratings yet
- Audiometer Testing ExplainedDocument25 pagesAudiometer Testing ExplainedLari EvergardenNo ratings yet
- Ocupational Hearing LossDocument38 pagesOcupational Hearing LossNIKOLAOS CHATZAKISNo ratings yet
- Otoacoustic Emissions From MedscapeDocument5 pagesOtoacoustic Emissions From MedscapeMin-Joo Esther ParkNo ratings yet
- Manual Lab Audiology - For StudentDocument12 pagesManual Lab Audiology - For StudentAnnisa Alifia AksaniNo ratings yet
- What Is A Good Hearing Aid Sound Quality, and Does It Really Matter - Anders HDocument8 pagesWhat Is A Good Hearing Aid Sound Quality, and Does It Really Matter - Anders HIzz AppetonNo ratings yet
- Hearing Tests ExplainedDocument56 pagesHearing Tests ExplainedAbdur RaqibNo ratings yet
- Weber TestDocument5 pagesWeber TestSuranewNo ratings yet
- Conceitos de Ruído - NIOSHDocument4 pagesConceitos de Ruído - NIOSHJanilldo CostaNo ratings yet
- Assessment of HearingDocument51 pagesAssessment of HearingSwetha PasupuletiNo ratings yet
- Dr. Ashman's ENT Notes PDFDocument56 pagesDr. Ashman's ENT Notes PDFJulian GordonNo ratings yet
- Tes PendengaranDocument33 pagesTes PendengaranmylogyiNo ratings yet
- 12 Audiometic TestingDocument99 pages12 Audiometic TestingAashish SinghNo ratings yet
- Overview of TinnitusDocument11 pagesOverview of TinnitusJohn JoseNo ratings yet
- Neonatal Incubators A Toxic Sound EnviroDocument6 pagesNeonatal Incubators A Toxic Sound EnviroJosé Antonio Ayala AguilarNo ratings yet
- Hearing Test Types and ResultsDocument114 pagesHearing Test Types and Resultshonda matiz100% (2)
- Diskusi Klompok2Document1 pageDiskusi Klompok2whooooNo ratings yet
- Presbycusis 181116131215 PDFDocument66 pagesPresbycusis 181116131215 PDFWael ShamyNo ratings yet
- Acoustic - Stapedius - Reflexes PDFDocument6 pagesAcoustic - Stapedius - Reflexes PDFSOFTMERCURYNo ratings yet
- PsychoPhisics, ExperimentsDocument9 pagesPsychoPhisics, ExperimentsMaria Isabel BinimelisNo ratings yet
- AudiometryDocument3 pagesAudiometrySathish KumarNo ratings yet
- HearingDocument3 pagesHearingAnnabelle ArtiagaNo ratings yet
- The Mechanics of Hearing: Ear Is Buried Within The Temporal Bone On Either Side of The Skull. The Temporal BoneDocument14 pagesThe Mechanics of Hearing: Ear Is Buried Within The Temporal Bone On Either Side of The Skull. The Temporal Bonereal_yooriNo ratings yet
- T10 MaskingDocument2 pagesT10 Maskingshel29No ratings yet
- Super Power devices help the hearing impaired understand speechDocument13 pagesSuper Power devices help the hearing impaired understand speechkeriyant0No ratings yet
- The Mechanics of HearingDocument13 pagesThe Mechanics of HearingDustin NguyenNo ratings yet
- Interpretation of Audiometric TestDocument13 pagesInterpretation of Audiometric Testfatimaawan8989No ratings yet
- Intro To SoundDocument16 pagesIntro To SoundsnailbookNo ratings yet
- Measuring Sound BKSVDocument44 pagesMeasuring Sound BKSVRittik ChakrabortyNo ratings yet
- Danesh 2018Document16 pagesDanesh 2018gemapesfNo ratings yet
- Fundamentals of Sound Quality: Dr. Arunkumar M. SampathDocument32 pagesFundamentals of Sound Quality: Dr. Arunkumar M. SampathsikmmmppsNo ratings yet
- AssessmentofhearingDocument85 pagesAssessmentofhearingNitin SharmaNo ratings yet
- Community Noise 4Document11 pagesCommunity Noise 4interlude347No ratings yet
- 9 Audiometer 03 07 2023Document30 pages9 Audiometer 03 07 2023Kushagra Narang 21BML0031No ratings yet
- Slow Auditory Evoked Potentials (1 InterligneDocument8 pagesSlow Auditory Evoked Potentials (1 Interligner.boniver524No ratings yet
- Audiometric Masking TechniquesDocument52 pagesAudiometric Masking TechniquesAlfred L ToruanNo ratings yet
- Astm D 664 - 07Document8 pagesAstm D 664 - 07Alfonso MartínezNo ratings yet
- Lesson 4Document13 pagesLesson 4Annie Mury SantiagoNo ratings yet
- Chanel SWOT AnalysisDocument5 pagesChanel SWOT AnalysisJeish KimNo ratings yet
- Analysis and Design of Multi Storey Building by Using STAAD ProDocument5 pagesAnalysis and Design of Multi Storey Building by Using STAAD Prolikith rockNo ratings yet
- I Button Proper TDocument4 pagesI Button Proper TmariammariaNo ratings yet
- FM 5130Document66 pagesFM 5130Aswini Kr KarmakarNo ratings yet
- EPISIOTOMYDocument17 pagesEPISIOTOMYKaye Arriane TenorioNo ratings yet
- Marulaberry Kicad EbookDocument23 pagesMarulaberry Kicad EbookPhan HaNo ratings yet
- Copy Resit APLC MiniAssignmentDocument5 pagesCopy Resit APLC MiniAssignmentChong yaoNo ratings yet
- The Interview: P F T IDocument14 pagesThe Interview: P F T IkkkkccccNo ratings yet
- CURRICULUM AUDIT: GRADE 7 MATHEMATICSDocument5 pagesCURRICULUM AUDIT: GRADE 7 MATHEMATICSjohnalcuinNo ratings yet
- Siga-Cc1 12-22-2010Document6 pagesSiga-Cc1 12-22-2010Felipe LozanoNo ratings yet
- Bal - 2011 - The New HRM in The 21st Century - A Strategic ViewDocument15 pagesBal - 2011 - The New HRM in The 21st Century - A Strategic ViewJoaquínMartínezMiñoNo ratings yet
- Olympic Ayres Magic LyricsDocument1 pageOlympic Ayres Magic Lyricsjackliddy96No ratings yet
- Project Wise CSR Expenditure FY202223Document15 pagesProject Wise CSR Expenditure FY202223gowowor677No ratings yet
- 16 Week Mountain Marathon Training Plan: WWW - Brutalevents.co - UkDocument2 pages16 Week Mountain Marathon Training Plan: WWW - Brutalevents.co - UkCristina CrsNo ratings yet
- SMEs, Trade Finance and New TechnologyDocument34 pagesSMEs, Trade Finance and New TechnologyADBI EventsNo ratings yet
- BarclaysDocument5 pagesBarclaysMehul KelkarNo ratings yet
- GVB 1Document8 pagesGVB 1Aaron SylvestreNo ratings yet
- 13Document47 pages13Rohan TirmakheNo ratings yet
- One - Pager - SOGEVAC SV 320 BDocument2 pagesOne - Pager - SOGEVAC SV 320 BEOLOS COMPRESSORS LTDNo ratings yet
- Banu Maaruf of The LevantDocument6 pagesBanu Maaruf of The LevantMotiwala AbbasNo ratings yet
- Angelomorphic Christology and The Book of Revelation - Matthias Reinhard HoffmannDocument374 pagesAngelomorphic Christology and The Book of Revelation - Matthias Reinhard HoffmannEusebius325100% (2)
- Class Opening Preparations Status ReportDocument3 pagesClass Opening Preparations Status ReportMaria Theresa Buscato86% (7)
- Eagle Test ReportDocument25 pagesEagle Test ReportMuhammad FahadNo ratings yet
- Common Pesticides in AgricultureDocument6 pagesCommon Pesticides in AgricultureBMohdIshaqNo ratings yet
- Android TabletsDocument2 pagesAndroid TabletsMarcus McElhaneyNo ratings yet
- Aerospace Opportunities in SwitzerlandDocument5 pagesAerospace Opportunities in SwitzerlandBojana DekicNo ratings yet
- Catalogo Head FixDocument8 pagesCatalogo Head FixANDREA RAMOSNo ratings yet
- Corporate Governance in SMEsDocument18 pagesCorporate Governance in SMEsSana DjaanineNo ratings yet