Professional Documents
Culture Documents
ZRT Neurotransmisores Reporte Muestra 0422
Uploaded by
Job MonobeOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ZRT Neurotransmisores Reporte Muestra 0422
Uploaded by
Job MonobeCopyright:
Available Formats
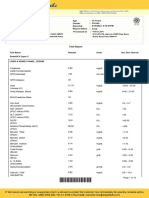
TEST REPORT
8605 SW Creekside Place
Beaverton, OR 97008
Phone: 503-466-2445 Fax: 503-466-1636
# D2021 03 17 876 U Samples Received Samples Collected
Ordering Provider: 03/17/2021 Urine - 03/15/21 05:30
Getuwell Urine - 03/15/21 07:30
Report Date Urine - 03/15/21 18:00
03/18/2021 Urine - 03/15/21 22:00
Patient Name: NeuroAdvanced w-Diurnal
Patient Phone Number: 555 555 5555
Gender Height Waist
Male 5 ft 11 in 30 in
DOB Weight BMI
5/17/1997 (23 yrs) 160 lb 22.3
TEST NAME RESULTS | 03/15/21 RANGE
Urinary Inhibitory Neurotransmitters
Tryptophan 14082 H 2633-12688 µg/g Cr (Optimal 3970-8450)
Serotonin 72.6 47.6-140.3 µg/g Cr (Optimal 61.0-103.2)
5-HIAA 3857 2205-11816 µg/g Cr (Optimal 2988-5850)
GABA 341 167-463 µg/g Cr (Optimal 193-367)
Glycine 56 41-295 mg/g Cr (Optimal 61-159)
Taurine 4.2 L 7.1-293.1 mg/g Cr (24.5-134.1)
Urinary Excitatory Neurotransmitters
Glutamate 1436 1213-4246 µg/g Cr (Optimal 1515-2710)
Glutamine 38 27-106 mg/g Cr (Optimal 37-71)
Histidine 63.8 10.8-98.9 mg/g Cr (Optimal 19.7-58.4)
Histamine 25.4 3.6-44.3 µg/g Cr (Optimal 5.2-15.3)
N-Methylhistamine 285 H 59-195 µg/g Cr (Optimal 79-140)
PEA 4.3 3.6-38.8 µg/g Cr (Optimal 5.3-16.1)
Tyrosine 5240 3128-15548 µg/g Cr (Optimal 4790-10278)
Tyramine 353 187-910 µg/g Cr (Optimal 279-588)
Dopamine 132 103-282 µg/g Cr (Optimal 144-240)
DOPAC 658 495-2456 µg/g Cr (Optimal 658-1449)
HVA 6122 3025-9654 µg/g Cr (Optimal 3737-7048)
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
1 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
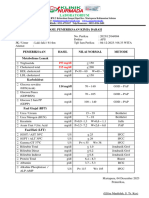
TEST REPORT | Results continued # D2021 03 17 876 U
TEST NAME RESULTS | 03/15/21 RANGE
Urinary Excitatory Neurotransmitters
Norepinephrine
21.8 10.0-35.7 µg/g Cr (Optimal 15.0-28.1)
(pooled)
Normetanephrine 18.1 13.4-44.8 µg/g Cr (Optimal 17.9-31.7)
Epinephrine (pooled) 3.3 0.8-6.2 µg/g Cr (Optimal 1.4-4.2)
Ratio: Norepi/Epi 6.6 2.9-25.2 (Optimal 5.2-13.7)
VMA 2849 1996-5939 µg/g Cr (Optimal 2580-4766)
Urinary Inflammatory Markers
Kynurenine 1462 108-1641 µg/g Cr (Optimal 257-960)
Kynurenic Acid 916 437-1719 µg/g Cr (Optimal 639-1200)
3-Hydroxykynurenine 1227 H 80-822 µg/g Cr (Optimal 147-467)
Xanthurenic Acid 1308 450-2175 µg/g Cr (694-1510)
Urinary Free Diurnal Cortisol
Free Cortisol 57.28 H 7.8-29.5 µg/g Cr (1st Morning)
Free Cortisol 9.54 L 23.4-68.9 µg/g Cr (2nd Morning)
Free Cortisol 10.51 6.0-19.2 µg/g Cr (Evening)
Free Cortisol 4.13 2.6-8.4 µg/g Cr (Night)
Urinary Free Diurnal Cortisone
Free Cortisone 234.25 H 31.6-91.6 µg/g Cr (1st Morning)
Free Cortisone 53.48 L 63.3-175.8 µg/g Cr (2nd Morning)
Free Cortisone 66.8 30.6-88.5 µg/g Cr (Evening)
Free Cortisone 25.99 15.5-44.7 µg/g Cr (Night)
Urinary Diurnal Melatonin MT6s
Melatonin 6.14 L 10.1-26.0 µg/g Cr (1st Morning)
Melatonin 5.79 L 6.0-17.0 µg/g Cr (2nd Morning)
Melatonin 1.69 0.5-3.6 µg/g Cr (Evening)
Melatonin 1.7 1.3-8.4 µg/g Cr (Night)
Urinary Diurnal Norepinephrine
Norepinephrine 40.6 H 9.4-22.0 µg/g Cr (1st Morning)
Norepinephrine 22.74 12.6-38.2 µg/g Cr (2nd Morning)
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
2 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
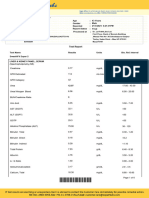
TEST REPORT | Results continued # D2021 03 17 876 U
TEST NAME RESULTS | 03/15/21 RANGE
Urinary Diurnal Norepinephrine
Norepinephrine 51.42 H 21.1-42.9 µg/g Cr (Evening)
Norepinephrine 29.77 16.9-38.8 µg/g Cr (Night)
Urinary Diurnal Epinephrine
Epinephrine 7.33 H 0.5-1.5 µg/g Cr (1st Morning)
Epinephrine 1.24 0.7-6.1 µg/g Cr (2nd Morning)
Epinephrine 6.96 2.3-8.1 µg/g Cr (Evening)
Epinephrine 4.12 1.2-4.2 µg/g Cr (Night)
Urinary Creatinine
Creatinine (pooled) 0.92 0.3-2.0 mg/mL
Creatinine 0.34 0.3-2.0 mg/mL (1st morning)
Creatinine 1.54 0.3-2.0 mg/mL (2nd morning)
Creatinine 0.56 0.3-2.0 mg/mL (Evening)
Creatinine 1.24 0.3-2.0 mg/mL (Night)
<dl = Less than the detectable limit of the lab. N/A = Not applicable; 1 or more values used in this calculation is less than the detectable limit. H = High. L = Low.
Therapies
BID topical Clobex (clobetasol propionate) (Pharmaceutical) (7 Hours Last Used)
Graphs
Disclaimer: Graphs below represent averages for healthy individuals not using hormones. Supplementation ranges may be
higher. Please see supplementation ranges and lab comments if results are higher or lower than expected. Average Off Graph
Urinary Free Cortisol Urinary Free Cortisone
80 200
70 180
160
60
140
50 120
µg/g Cr
µg/g Cr
40 100
30 80
60
20
40
10 20
03:00 06:00 09:00 12:00 15:00 18:00 21:00 00:00 03:00 03:00 06:00 09:00 12:00 15:00 18:00 21:00 00:00 03:00
Time of Day Time of Day
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
3 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
TEST REPORT | Results continued # D2021 03 17 876 U
Urinary Melatonin (MT6s) Urinary Norepinephrine
30 50
45
25
40
35
20
30
µg/g Cr
µg/g Cr
15 25
20
10
15
10
5
5
03:00 06:00 09:00 12:00 15:00 18:00 21:00 00:00 03:00 03:00 06:00 09:00 12:00 15:00 18:00 21:00 00:00 03:00
Time of Day Time of Day
Urinary Epinephrine
10
9
8
7
6
µg/g Cr
5
4
3
2
1
03:00 06:00 09:00 12:00 15:00 18:00 21:00 00:00 03:00
Time of Day
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
4 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
5 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
6 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
TEST REPORT | Patient Reported Symptoms # D2021 03 17 876 U
Disclaimer: Symptom Categories below show percent of symptoms self-reported by the patient compared to total available symptoms for each category. For
detailed information on category breakdowns, go to www.zrtlab.com/patient-symptoms.
SYMPTOM CATEGORIES RESULTS | 03/15/21
Estrogen / Progesterone Deficiency 12%
Estrogen Dominance / Progesterone Deficiency 3%
Low Androgens (DHEA/Testosterone) 17%
High Androgens (DHEA/Testosterone) 44%
Low Cortisol 20%
High Cortisol 28%
Hypometabolism 21%
Metabolic Syndrome 7%
SYMPTOM CHECKLIST MILD MODERATE SEVERE
Acne
ADD/ADHD
Addictive Behaviors
Aggressive Behavior
Allergies
Anxious
Apathy
Autism Spectrum Disorder
Blood Pressure High
Blood Pressure Low
Blood Sugar Low
Body Temperature Cold
Bone Loss
Burned Out Feeling
Chemical Sensitivity
Cholesterol High
Constipation
Depressed
Developmental Delays
Dizzy Spells
Eating Disorders
Erections Decreased
Fatigue - Evening
Fatigue - Mental
Fatigue - Morning
Flexibility Decreased
Forgetfulness
Goiter
Hair - Dry or Brittle
Hair or Skin Oily
Headaches
Hearing Loss
Heart Palpitations
Hoarseness
Hot Flashes
Infertility
Irritable
Joint Pain
Libido Decreased
Mania
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
7 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
TEST REPORT | Patient Reported Symptoms continued # D2021 03 17 876 U
SYMPTOM CHECKLIST MILD MODERATE SEVERE
Mental Sharpness Decreased
Muscle Size Decreased
Muscle Soreness
Nails Breaking or Brittle
Neck or Back Pain
Nervous
Night Sweats
Numbness - Feet or Hands
OCD
Panic Attacks
Prostate Cancer
Prostate Problems
Pulse Rate Slow
Rapid Aging
Rapid Heartbeat
Ringing In Ears
Skin Thinning
Sleeping Difficulty
Stamina Decreased
Stress
Sugar Cravings
Sweating Decreased
Swelling or Puffy Eyes/Face
Triglycerides Elevated BLANK
Urinary Urge Increased
Urine Flow Decreased
Weight Gain - Breast or Hips
Weight Gain - Waist
Lab Comments
INHIBITORY NEUROTRANSMITTERS
TRYPTOPHAN
Tryptophan is high likely due to supplementation. The essential amino acid tryptophan originates in diet and serves as a constituent of proteins
and a precursor to neurotransmitters. Only a fraction of tryptophan is used by the GI tract, the vast majority of this amino acid enters portal
circulation and undergoes liver metabolism. The remaining tryptophan pool, together with its liver degradation products, is distributed to
peripheral circulation and transported to tissues such as the brain, heart, and skeletal muscle. Tryptophan not taken up by the upper GI tract is
metabolized by resident microbiota.
Tryptophan is a substrate for two important biosynthetic pathways relevant to the inflammatory neuropsychiatric interface: the generation of the
neurotransmitter serotonin and therefore hormone melatonin, and the formation of kynurenine derivatives and therefore niacin (vitamin B3).
Tryptophan hydroxylase initiates the two-step conversion to serotonin, a process that requires tetrahydrobiopterin (BH4), iron and vitamin B6.
Approximately 5-10% of tryptophan is converted to serotonin. Tryptophan dioxygenase and indoleamine 2,3-dioxygenase are the enzymes
responsible for tryptophan's conversion to kynurenine in a copper and iron-dependent manner. In fact, upward of 90-95% of tryptophan is
metabolized to the kynurenine pathway, and upregulation of this pathway may be a hallmark of neuroinflammation.
Research shows that tryptophan is high with tryptophan supplementation (Michael, Drummond et al. 1964) and in some individuals with a high
protein diet (Poesen, Mutsaers et al. 2015). Clinically, high tryptophan is associated with headaches (Curto, Lionetto et al. 2015) and selective
serotonin reuptake inhibitor treatment (Mackay, Forrest et al. 2009).
TREATMENT CONSIDERATIONS: discontinue tryptophan supplementation if side effects are bothersome, these include blurred vision,
dizziness, fatigue, nausea, stomach pain, vomiting, diarrhea and loss of appetite.
SEROTONIN
Serotonin is within reference range. Serotonin has calming effects and contributes to the feelings of well-being. Serotonin elevates mood,
decreases anxiety, appetite, and libido, improves sleep and memory, eases depression, and helps regulate body temperature. Most of serotonin
in the human body is produced in the gastrointestinal tract, where it stimulates gut motility.
5-HIAA
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
8 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
TEST REPORT | Comments continued # D2021 03 17 876 U
5-hydroxyindoleacetic acid (5-HIAA) is within reference range. 5-HIAA is the primary metabolite of serotonin via the actions of monoamine
oxidase and aldehyde dehydrogenase enzymes.
GABA
GABA is within the reference range. The brain's major inhibitory neurotransmitter GABA functions as the off switch in the brain. GABA is
essential to limiting excitation so that input signals are balanced and not overdone. GABA prevents anxiety, improves mood, promotes sleep,
lowers blood pressure, acts as a muscle relaxant, aids in formation and storage of fear memories, increases insulin secretion and decreases
blood glucose levels.
GLYCINE
Glycine is lower than the optimal range, which may be due to depression (self-reported). Although research on urinary levels of glycine is scarce,
levels of glycine in blood are lower in depressed individuals than in controls (Altamura, et. al. 1995).
Glycine is a neurotransmitter and a simple, nonessential (can be made in the body) amino acid that plays a role in the production of DNA,
phospholipids, collagen, creatine, heme and glutathione. Glycine serves as an anti-inflammatory agent, calms aggression, improves sleep
quality, stabilizes blood sugar, improves metabolic parameters and modulates excitatory signals in the brain. Low levels may be indicative of
chronically increased demand for tetrahydrofolate (active folic acid) production, for which glycine serves as a precursor.
Additional research studies show that urinary glycine levels are reduced after intense exercise (Corsetti, et. al. 2016), and in patients with
rheumatoid arthritis (Jones, et. al. 2005), or hypometabolic disorders, such as hypothyroidism (Friedrich, et. al. 2017), obesity (Ahmad, et. al.
2016), and diabetes (Sasaki, et. al. 1988).
THERAPEUTIC CONSIDERATIONS: Glycine supplementation, vitamin B6, serine and MTHF may all support optimal glycine levels.
TAURINE
Taurine is lower than the reference range. Taurine is a semi-essential or conditionally essential sulfur-containing amino acid and an inhibitory
(calming) neurotransmitter. Taurine improves sleep, relieves anxiety, alleviates fatigue, aids with metabolism and digestion, and promotes
glucose control and electrolyte balance.
The main source of taurine is diet (highest in shellfish and poultry (dark meat)). Taurine protects healthy cells and tissues, functions as a potent
antioxidant to reduce oxidative stress, mitigates mitochondrial and endoplasmic reticulum stress, inhibits lipid peroxidation, improves energy
metabolism, regulates gene expression, and participates in detoxification, calcium homeostasis and osmoregulation processes. By fulfilling all
these functions, taurine is therefore protective in cardiovascular health, improves lean body mass and exercise performance. With regard to
brain health, taurine serves a neuroprotective role, promotes neural development in embryonic and adult brain tissues, and is an important factor
in neurogenesis.
Research shows that taurine excretion is low specifically with vegetarian or vegan diets (Rana and Sanders 1986) and with low protein diets in
general (Turner, Brum et al. 1964). Low taurine levels are implicated in diabetes (Sak, Erdenen et al. 2019), hypertension (Sak, Erdenen et al.
2019) and breast cancer (El Agouza, Eissa et al. 2011).
THERAPEUTIC CONSIDERATIONS: taurine is found in most types of meat, shellfish, and fish - increasing intake of these foods may help
restore normal taurine levels. Additionally, taurine supplementation is considered safe and can be tolerated up to 3 g per day without adverse
effects.
EXCITATORY NEUROTRANSMITTERS
GLUTAMATE
Glutamate is low-normal (< 20th percentile). The brain's major excitatory neurotransmitter glutamate functions as the "on" switch in the brain.
Glutamate regulates appetite, thinking, increases gut motility, optimizes learning, modulates memory, improves libido, and decreases sleep. Low
urinary glutamate levels have been reported in patients with migraines (Ragginer et al., 2012). Clinically, lower glutamate levels may contribute
to agitation, depression, chronic fatigue, lack of concentration, low energy levels, and sleep difficulties.
THERAPEUTIC CONSIDERATIONS: L-glutamine may be beneficial to restore glutamate to normal values.
GLUTAMINE
Glutamine is within range. Glutamine is an essential and the most abundant free amino acid in the human body. Glutamine provides fuel for
rapidly dividing cells (lymphocytes, enterocytes and epithelial cells of the intestines), helps balance ammonia levels in the body, improves
immune system function, contributes to biosynthesis of proteins, amino acids, nucleic acids and glutathione, and protects intestinal lining.
Additionally, glutamine increases glutamate and GABA levels in the brain and in the body.
HISTIDINE
Histidine is high-normal (>80th percentile), likely due to supplementation or recent dietary intake. Histidine is a semi-essential amino acid that
gives rise to the neurotransmitter histamine. Histidine protects neurons, assists with making new blood cells, reduces inflammation and oxidative
stress, helps with tissue repair and growth. Histidine also helps ameliorate fatigue, promotes clear thinking and concentration, reduces appetite,
decreases anxiety, improves sleep and glucose homeostasis.
Research shows that histidine excretion is high with histidine administration (Du, Sun et al. 2017), in histidinemia (Auerbach, DiGeorge et al.
1962), and in diabetic nephropathy (Shao, Lu et al. 2020).
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
9 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
TEST REPORT | Comments continued # D2021 03 17 876 U
THERAPEUTIC CONSIDERATIONS: because high histamine has not been linked to adverse symptoms, no therapy is thought to be needed.
HISTAMINE
Histamine is above the optimal range, which may be due to allergies (self-reported). Research shows that individuals with gastrointestinal food
allergies have higher urinary histamine levels (Raithel, et. al. 2015). This study showed that histamine was elevated in both IgE- and non-IgE
food allergy types during consumption of offending foods, but not during the hypoallergenic diet.
This individual concurrently reports having ADHD. Literature suggests that some individuals with ADHD may have food sensitivities, and when
present in diet, these foods could exacerbate symptoms of the disorder. Restriction/elimination diets, excluding artificial food coloring and excess
sugar from diet have been shown by multiple studies to improve symptoms of hyperactivity and inattentiveness (Nigg and Holton, 2014).
Histamine plays a dual role in the body as a neurotransmitter and a modulator of the immune system that has anti-pain properties, plays a
neuroprotective role in the brain, and contributes to optimal maintenance of cognition and memory. Histamine stimulates wakefulness and
decreases sleep, stimulates gastric acid production, increases metabolism, suppresses appetite, and prevents weight gain. Histamine is a
potent vasodilator and a pro-inflammatory agent. Additional research studies show that urinary histamine is elevated in patients with flushing
disorder (Myers et al., 1981), cystitis (el-Mansoury et al., 1994), polycythemia (Horakova et al., 1977), and pregnancy (Harrison et al., 1974).
Clinically, high histamine levels are implicated in depression, headaches, sensitivity to chemicals, and sleep difficulties.
THERAPEUTIC CONSIDERATIONS: Beneficial therapeutic strategies to reduce histamine levels may involve antihistamines and/or a low
histamine diet. High histamine foods include but are not limited to beer, champagne, aged cheeses, eggplant, canned fish, fermented meat, red
and white wine, sauerkraut, and spinach (Maintz and Novak, 2007), however individual food sensitivities ought to be considered as well.
Additionally, flavonoids (green tea extract, quercetin, grape seed extract, gingko biloba, citrus bioflavonoids, bilberry extract, hawthorn extract)
may be beneficial to ease the symptoms of high histamine (Murray et al., 2005).
N-METHYLHISTAMINE
N-Methylhistamine is high. N-Methylhistamine is a major metabolite of the neurotransmitter histamine. Research shows that N-methylhistamine
excretion is elevated with high protein diet (Keyzer, Breukelman et al. 10/1984), in gastrointestinal food allergies (Raithel, Hagel et al. 2015), in
irritable bowel disease (Winterkamp, Weidenhiller et al. 2002), in colitis (Schwab, Hahn et al. 2003), in histidinemia (Imamura, Watanabe et al.
1984), in chronic urticaria (Patel and Divekar 2017), in angioedema (Patel and Divekar 2017), and with interstitial cystitis (el-Mansoury, Boucher
et al. 8/1994).
THERAPEUTIC CONSIDERATIONS: evaluation for food allergy sources may be warranted.
PEA
Phenethylamine or PEA is below the optimal range. Low PEA may contribute to fatigue, depression and decreased attention span. PEA acts as
a "neuro-amplifier" - increasing the actions of dopamine (for wellbeing and feeling pleasure), norepinephrine (the brain's stimulant for
wakefulness, alertness and higher performance), acetylcholine (for improving memory and mental activity), and serotonin (for better mood
emotion and impulse control) (Paterson, et. al. 1990).
Recently, PEA has been recognized as a biomarker in ADHD and research shows that urinary levels of PEA are low in patients with ADHD
(Irsfeld, et. al. 2013). Patients whose symptoms improve in response to treatment, typically show higher PEA levels than patients who do not
experience an improvement in the condition.
Additionally, low PEA has been implicated in a number of psychological disorders, such as depression (Sabelli and Mosnaim, 1974), eating
disorders (bulimia nervosa) (Davis et al., 1994), inattentiveness (Faraone et al., 2014), Parkinson's disease (Wolf and Mosnaim, 1983), and
Tourette's syndrome (Bornstein et al., 1990)
THERAPEUTIC CONSIDERATIONS: when PEA is low, supplementation with vitamin B6 (cofactor) and phenylalanine (precursor) to promote
biosynthesis may be beneficial. Exercise helps increase PEA levels (Szabo, et a. 2001). Additionally, curcumin and passionflower, botanical
MAO inhibitors, may help by preventing rapid PEA metabolism.
TYROSINE
Tyrosine is within range. Tyrosine is obtained from diet (sesame seeds, cheese, soy, meat, nuts and fish) or synthesized in the body from the
amino acid phenylalanine. Tyrosine serves as a constituent of proteins and gives rise to neurotransmitters, like dopamine, norepinephrine and
epinephrine; and the trace-amine tyramine. Additionally, in the thyroid gland, tyrosine can also be iodinated to give rise to thyroid hormones.
Tyrosine enhances cognitive performance, energy, and alertness, and improves memory after sleep deprivation. Tyrosine also prevents the
depletion of central and peripheral catecholamines (dopamine, norepinephrine, epinephrine) induced by acute stress, thereby eliciting protective
effects on behavioral and cardiovascular parameters in the body.
TYRAMINE
Tyramine is within range. Tyramine is a trace amine derived from the amino acid tyrosine that is found naturally in food. Specifically, tyramine is
found in aged, fermented cured or spoiled food where microbes with decarboxylase enzymes convert tyrosine to tyramine. These foods include
aged cheeses, smoked fish, cured meats, wine, and some types of beer. In sensitive individuals, eating high amount of tyramine can trigger
migraines and increase blood pressure.
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
10 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
TEST REPORT | Comments continued # D2021 03 17 876 U
DOPAMINE
Dopamine is low-normal (<20th percentile). Dopamine improves attention, focus, and motivation, helps with decision making, modulates
movement control, promotes lactation, increases blood pressure, urine output and sodium excretion, and allows for feelings of reward and
pleasure. Additionally, the quest for dopamine stimulation plays a central role in the etiology of addiction. Dopamine also serves as the parent
precursor to norepinephrine and epinephrine. Research shows that urinary dopamine levels are reduced in patients with Alzheimer's disease
(Liu et al., 2011), anorexia nervosa (Van Binsbergen et al., 1991), anxiety with depression (Field et al., 2010), fibromyalgia (Riva et al., 2012),
and periodic limb movement disorder (Cohrs et al., 2004). Clinically, low dopamine is also implicated in apathy, cravings, fatigue, impulse control
issues, increased sensitivity to pain, low libido, low mood, memory issues, sleep disturbances, and weight control issues.
THERAPEUTIC CONSIDERATIONS: Supplementation with precursors (tyrosine or L-DOPA) and/or cofactors (iron, vitamin B6, tetrahydrofolate)
to promote biosynthesis may be beneficial.
DOPAC
DOPAC is low-normal (<20th percentile). DOPAC is the primary metabolite of dopamine formed via the actions of monoamine oxidase.
Research shows that DOPAC is reduced in the urine of patients with Alzheimer's disease (Liu et al., 2011). Lower than optimal levels suggest
that dopamine and its upstream precursors L-Dopa or tyrosine may be insufficient. DOPAC may also be lower due to MAO genetic SNPs which
can slow down this enzyme or insufficient vitamin B2 or copper levels. Evaluate this level in combination with dopamine, but also 5HIAA (the
serotonin metabolite) since it also uses the MAO enzyme.
THERAPEUTIC CONSIDERATIONS: Consider supplementing with the building blocks of dopamine (tyrosine and/or l-dopa). L-dopa is found
naturally in the herb mucuna as well as supporting nutritional co-factors used with MAO enzymes.
HVA
Homovanillic acid (HVA) is within reference range. HVA is a dopamine metabolite.
NOREPINEPHRINE
Norepinephrine is within reference range. Norepinephrine functions both as a neurotransmitter and a hormone, participating in the body's "fight
or flight" response. Norepinephrine increases alertness, focuses attention, fine-tunes vigilance, increases blood pressure, heart rate, and blood
sugar, reduces digestive activity, pain, and sleep, prevents bladder emptying, and regulates body temperature. Norepinephrine is very similar in
structure and physiological effects to epinephrine. The adrenal gland produces approximately 20% of the total output with 80% produced by the
sympathetic nerve fibers.
NORMETANEPHRINE
Normetanephrine is within reference range. Normetanephrine is a norepinephrine metabolite formed via the actions of catechol-O-methyl
(COMT) transferase enzyme in response to stress.
EPINEPHRINE
Epinephrine is within reference range. Epinephrine, also called adrenaline, functions both as a neurotransmitter and a hormone, participating in
the body's fight or flight response. Epinephrine increases alertness, focuses attention, fine-tunes vigilance, increases blood pressure, heart rate,
and blood glucose, reduces digestive activity, pain and sleep, prevents bladder emptying, and regulates body temperature.
VMA
Vanillylmandelic acid (VMA) is within reference range. VMA is a norepinephrine and epinephrine metabolite formed via the actions of
monoamine oxidase, catechol-O-methyl transferase (COMT), and aldehyde dehydrogenase.
INFLAMMATORY MARKERS
KYNURENINE
Kynurenine is high-normal (>80th percentile). Kynurenine is a central metabolite of the amino acid tryptophan with vasodilatory properties.
Kynurenine is utilized by the body in the production of niacin (vitamin B3), eventually leading to the formation of NAD+, which plays a pivotal role
in energy metabolism, gene expression, cell death and regulation of calcium homeostasis. More than 90% of the body's tryptophan is
metabolized to the kynurenine pathway.
Kynurenine is synthesized by the enzyme tryptophan dioxygenase, which is expressed primarily but not exclusively in the liver, and indoleamine
2,3-dioxygenase, which is made in many tissues in response to immune activation by interferons and cytokines, or free radicals. In the brain,
approximately ~40% of kynurenine is produced locally, whereas the rest is absorbed from the blood.
Kynurenine degradation generates a series of neuroprotective and neurotoxic compounds that can activate or inhibit N-methyl-d-aspartate
(NMDA) glutamate receptors (see kynurenic acid and 3-OH kynurenine). Upregulation of this pathway may be a hallmark of neuroinflammation
and is associated with certain disorders.
Research shows that kynurenine is high with tryptophan administration (Michael, Drummond et al. 1964), hydrocortisone treatment (Rose and
Braidman 1971), metabolic syndrome (Oh, Seo et al. 2017), with major coronary events (Pedersen, Svingen et al. 9/2013), and in women in
pregnancy (Rose and Braidman 1971). High kynurenine levels have been implicated in disorders like Irritable Bowel Syndrome (Fitzgerald,
Cassidy Eugene et al. 2008), lupus (Akesson, Pettersson et al. 2018), Crohn's disease (Gupta, Thaker et al. 2012), and Alzheimer's Disease
(Chatterjee, Goozee et al. 2018). Additionally, caffeine (Orlikov and Ryzov 1991) and regular black tea (Gostner, Becker et al. 2015)
consumption can elevate kynurenine levels as well.
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
11 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
TEST REPORT | Comments continued # D2021 03 17 876 U
TREATMENT CONSIDERATIONS: reduction of inflammation through diet and supplementation may be beneficial. Glutathione support and
modulation of the NMDA receptor (e.g. magnesium) may help reduce symptoms.
KYNURENIC ACID
Kynurenic acid is within range. Kynurenic acid is a neuroactive metabolite produced from kynurenine. Kynurenine is formed from tryptophan via
the enzyme tryptophan dioxygenase and indoleamine 2,3-dioxygenase; and metabolized along two independent pathways to produce kynurenic
acid via aminotransferases and 3-OH kynurenine.
Kynurenic acid (unless in excess amounts) is regarded to have a neuroprotective role because it inhibits the N-methyl-d-aspartate (NMDA)
glutamate receptor, reduces the neurotransmitter glutamate release and thereby prevents excitotoxicity.
3-HYDROXYKYNURENINE
3-Hydroxykynurenine is high. 3-Hydroxy Kynurenine (3-OH Kynurenine) is a metabolic intermediate of the kynurenine pathway, one of the major
metabolites of tryptophan degradation. Kynurenine is transformed into 3-OH Kynurenine, which acts as a N-methyl-d-aspartate (NMDA)
glutamate receptor agonist and has been demonstrated to exert neurotoxic effects.
Neurotoxicity elicited by 3-OH Kynurenine appears to be also related to generation of oxidative stress produced by reactive radical species,
formed as a result of auto-oxidation. Additionally, 3-OH Kynurenine gives rise to neurotoxic metabolites, such as quinolinic acid, which activate
the NMDA receptor, induce lipid peroxidation and promote oxidative stress.
Research shows that urinary levels of 3-OH Kynurenine are high with hydrocortisone treatment (Rose and Braidman 1971) and in women in
pregnancy (Rose and Braidman 1971). High 3-OH Kynurenine is implicated in vitamin B6 deficiency (Theofylaktopoulou, Ulvik et al. 2014) and
Alzheimer's disease (Schwarz, Guillemin et al. 2013).
TREATMENT CONSIDERATIONS: consider glutathione support and antioxidant support to prevent the oxidative stress produced by 3-
hydroxyhynurenine. Consider B6 supplementation (under 200 mg/day for safety).
XANTHURENIC ACID
Xanthurenic acid is within range. Xanthurenic acid is a metabolite of the kynurenine pathway, formed directly from 3-OH Kynurenine, and serves
as an indirect marker of vitamin B6 status.
URINARY FREE CORTISOL (F) AND CORTISONE (E)
Urinary free cortisol (F) and cortisone (E) are NOT following a normal circadian rhythm and levels are outside the expected reference ranges,
particularly in the first two morning voids. F and E are very high in the first morning void, but drop precipitiously in the second void but begin to
recover to normal reference ranges in the evening and at night before bed. This individual has reported use of a synthetic glucocorticoid,
commonly used topically for treating skin conditions associated with inflammation. Synthetic glucocorticoids that enter the systemic circulation
suppress endogenous cortisol synthesis by negative feedback to the hypothalamic-pituitary-adrenal axis and lower ACTH/cortisol synthesis. The
negative feedback is transient and may result in a rebound with higher synthesis of cortisol several hours afterward. Low second morning
cortisol likely results from use of the synthetic glucocorticoid after collecting the first morning void. As seen in these results cortisol recovers to
expected levels in the evening and at night before bed. A high F and E in the first morning void suggests that levels are high during sleep at night
or rise rapidly just before waking (possible rebound from evening use of the synthetic glucocorticoid).
Overall, these results indicate that endogenous cortisol synthesis is high and is somewhat amplified by use of the topical synthetic
glucocorticoid. Self-reported symptoms (e.g. excessive stress, fatigue, depression, irritability, decreased mental sharpness, weight gain most in
the waist (belly fat), are consistent with overall high cortisol exposure.
While a normal daily adrenal output of cortisol is essential to maintain normal metabolic activity, help regulate steady state glucose levels
(important for brain function and energy production), and optimize immune function, excessive levels of glucocorticoids (natural and synthetic)
can have the opposite effect over time. For information about strategies to support adrenal health and reduce stress(ors) that can lead to excess
or deficient cortisol synthesis, the following books are worth reading: "Adrenal Fatigue", by James L. Wilson, N.D., D.C., Ph.D.; "The Cortisol
Connection", by Shawn Talbott, Ph.D.; "The End of Stress As We Know It" by Bruce McEwen; "The Role of Stress and the HPA Axis in Chronic
Disease Management" by Thomas Guilliams, PhD.
MELATONIN METABOLITE 6-SULFATOXYMELATONIN (MT6s)
The melatonin metabolite 6-sulfatoxymelatonin (MT6s) is not following a normal circadian rhythm. MT6s should be at its highest level in the first
morning void, which is reflective of the dark period (night), but instead is low. Lower MT6s in the first morning void may reflect work during a
night shift or staying up at night with excessive lighting (e.g. watching television). Some sleep (benzodiazepines, barbituates), pain (ibuprofen,
opiates) and blood pressure medications (beta blockers like propranolol) are known to interfere with melatonin production and secretion and
lower the circulating and excreted (MT6s) urinary levels of melatonin. Use of any of these medications at night before bed would result in a lower
melatonin in the first morning void. The second morning void in this individual is also lower than the reference range. MT6s begins to rise
thereafter in the evening and is within normal reference range at night before bed.
In a healthy individual the circadian rhythm of melatonin is inversely related to circulating levels of adrenal cortisol levels, i.e. melatonin rises with
darkness and peaks about 2-3 am, while cortisol falls to its lowest level at this time of day. With morning and onset of light exposure, melatonin
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
12 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
TEST REPORT | Comments continued # D2021 03 17 876 U
drops rapidly and cortisol rises, peaking to its highest level about 30 min to 1 hr after waking (referred to as a Cortisol Awakening Response-
CAR). By mid-afternoon (evening void) with maximal light exposure melatonin reaches a nadir. It then gradually begins to rise again with nightfall
and less light exposure, while cortisol continues to rise. Cortisol and melatonin reach their nadir and peak, respectively, about 2-3 am. Melatonin
synthesis by the pineal gland is controlled by light exposure, while cortisol synthesis is controlled by the hypothalamic-pituitary axis in response
to stressors. While melatonin and cortisol have opposing circadian rhythms neither hormone directly and acutely controls the synthesis of the
other.
Melatonin is known to have many different beneficial effects in the body. For an excellent review of melatonin's many benefits please read:
Pandi-Perumal et.al. Melatonin, Nature's most versatile biological signal. FEBS 273: 2813-2838, 2006. Melatonin has multiple roles in
maintaining health. It helps slow the aging process, is a potent anti-oxidant, regulates the immune system, inhibits formation and growth of
tumors such as breast and prostate cancers, and helps regulate the synthesis of the sex-hormones estradiol and progesterone (melatonin
increases progesterone, decreases estrogens by inhibiting aromatase, and down-regulates cellular estrogen receptors, which diminishes
response of estrogen-sensitive tissues to estrogens). Low melatonin is also thought to contribute to obesity in people with insomnia or those who
do night shift work.
Because of its established role in the regulation of the circadian rhythm, treatment with exogenous melatonin has been found useful in people
with circadian rhythm sleep disorders, such as delayed sleep phase disorder, jet lag, shift worker disorder, and the non-24-hour sleep-wake
disorder most commonly found in totally blind individuals; however, its utility for the treatment of insomnia is not established and remains
controversial.
If melatonin is taken as a supplement (available OTC) to correct low levels or treat a condition, the timing and dosage are important to its
effectiveness, especially as a sleep aid. Response to supplemental melatonin can be very individual. For optimal benefit it is best to work with a
health care provider familiar with melatonin dosage and timing. Excessive dosing can result in spillover of melatonin into daylight hours,
excessive sleepiness during the day, and disruption of the normal melatonin-cortisol circadian rhythms.
For more general information about melatonin please see: http://www.nlm.nih.gov/medlineplus/druginfo/natural/940.html
DIURNAL EPINEPHRINE
Epinephrine is elevated during the night (1st morning), but returns to normal range in the morning (2nd sample), and remains within normal
ranges throughout the day (evening collection) and at night (evening/night sample) before bed. The pooled sample is within range, but the
diurnal results are more accurate for true epinephrine status. Epinephrine, also called adrenaline, functions both as a neurotransmitter and a
hormone, participating in the body's "fight or flight" response. Epinephrine increases alertness, focuses attention, fine-tunes vigilance, increases
blood pressure, heart rate, and blood glucose, reduces digestive activity, pain and sleep, prevents bladder emptying, and regulates body
temperature. It is commonly triggered by stress, fear, blood sugar irregularities or anxiety.
Research shows that urinary epinephrine levels are increased in patients with attention deficit disorder (Faraone et al., 2014), anxiety and
depression (Hughes et al., 2004), bipolar disorder (Koslow et al., 1983), hyperglycemia (Troisi et al., 1991), hyperinsulinemia (Troisi et al., 1991),
obstructive sleep apnea (Kheirandish-Gozal et al., 2013), post-traumatic stress disorder (Yehuda et al., 1992), and stress (Holzman et al., 2009;
Fujiwara et al., 2004). Fluctuating levels throughout the day have been commonly associated with an inverse relationship with cortisol (e.g. high
epi when cortisol is low).
THERAPEUTIC CONSIDERATIONS: Because epinephrine is almost exclusively from the adrenal glands, treatments geared to support normal
adrenal function and calm the sympathetic nervous system may be beneficial. Supplements such as adrenal adaptogens, B vitamins, essential
fatty acids, vitamin C, as well as stress management, blood sugar balance and sleep support may be helpful.
Creatinine is within range throughout the day reflecting normal concentration of urine.
Creatinine levels reflect urine concentration.
Low values suggest overly dilute urine; High values suggest overly concentrated urine.
Extreme low or high values may be induced by kidney or other metabolic disorders, but most values will be due to inadequate hydration (high
creatinine) or excessive water intake in the several hours prior to testing (low creatinine). Creatinine is used to adjust the lab results for kidney
function. No samples were refused due to quality issues.
INHIBITORY NEUROTRANSMITTERS
TRYPTOPHAN
Tryptophan is high likely due to supplementation. The essential amino acid tryptophan originates in diet and serves as a constituent of proteins
and a precursor to neurotransmitters. Only a fraction of tryptophan is used by the GI tract, the vast majority of this amino acid enters portal
circulation and undergoes liver metabolism. The remaining tryptophan pool, together with its liver degradation products, is distributed to
peripheral circulation and transported to tissues such as the brain, heart, and skeletal muscle. Tryptophan not taken up by the upper GI tract is
metabolized by resident microbiota.
Tryptophan is a substrate for two important biosynthetic pathways relevant to the inflammatory neuropsychiatric interface: the generation of the
neurotransmitter serotonin and therefore hormone melatonin, and the formation of kynurenine derivatives and therefore niacin (vitamin B3).
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
13 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
TEST REPORT | Comments continued # D2021 03 17 876 U
Tryptophan hydroxylase initiates the two-step conversion to serotonin, a process that requires tetrahydrobiopterin (BH4), iron and vitamin B6.
Approximately 5-10% of tryptophan is converted to serotonin. Tryptophan dioxygenase and indoleamine 2,3-dioxygenase are the enzymes
responsible for tryptophan's conversion to kynurenine in a copper and iron-dependent manner. In fact, upward of 90-95% of tryptophan is
metabolized to the kynurenine pathway, and upregulation of this pathway may be a hallmark of neuroinflammation.
Research shows that tryptophan is high with tryptophan supplementation (Michael, Drummond et al. 1964) and in some individuals with a high
protein diet (Poesen, Mutsaers et al. 2015). Clinically, high tryptophan is associated with headaches (Curto, Lionetto et al. 2015) and selective
serotonin reuptake inhibitor treatment (Mackay, Forrest et al. 2009).
TREATMENT CONSIDERATIONS: discontinue tryptophan supplementation if side effects are bothersome, these include blurred vision,
dizziness, fatigue, nausea, stomach pain, vomiting, diarrhea and loss of appetite.
SEROTONIN
Serotonin is within reference range. Serotonin has calming effects and contributes to the feelings of well-being. Serotonin elevates mood,
decreases anxiety, appetite, and libido, improves sleep and memory, eases depression, and helps regulate body temperature. Most of serotonin
in the human body is produced in the gastrointestinal tract, where it stimulates gut motility.
5-HIAA
5-hydroxyindoleacetic acid (5-HIAA) is within reference range. 5-HIAA is the primary metabolite of serotonin via the actions of monoamine
oxidase and aldehyde dehydrogenase enzymes.
GABA
GABA is within the reference range. The brain's major inhibitory neurotransmitter GABA functions as the off switch in the brain. GABA is
essential to limiting excitation so that input signals are balanced and not overdone. GABA prevents anxiety, improves mood, promotes sleep,
lowers blood pressure, acts as a muscle relaxant, aids in formation and storage of fear memories, increases insulin secretion and decreases
blood glucose levels.
GLYCINE
Glycine is lower than the reference range. Glycine is a neurotransmitter and a simple, nonessential (can be made in the body) amino acid that
plays a role in the production of DNA, phospholipids, collagen, creatine, heme and glutathione. Glycine serves as an anti-inflammatory agent,
calms aggression, improves sleep quality, stabilizes blood sugar, improves metabolic parameters and modulates excitatory signals in the brain.
Low levels may be indicative of chronically increased demand for tetrahydrofolate (active folic acid) production, for which glycine serves as a
precursor. Research shows that glycine levels are reduced after intense exercise (Corsetti, et. al. 2016) and in patients with rheumatoid arthritis
(Jones, et. al. 2005), hypometabolism, such as hypothyroidism (Friedrich, et. al. 2017), obesity (Ahmad, et. al. 2016), and diabetes (Sasaki, et.
al. 1988).
THERAPEUTIC CONSIDERATIONS: Glycine supplementation has been shown to improve metabolic response - such as cholesterol
parameters and insulin sensitivity, reduce blood pressure, and aid with decreasing the levels of hemoglobin A1C and pro-inflammatory cytokines
(Diaz-Flores, et. al. 2013; Perez-Torres, et. al. 2017). Additionally, vitamin B6, serine support, and MTHF may all support the production of
glycine.
TAURINE
Taurine is lower than the reference range. Taurine is a semi-essential or conditionally essential sulfur-containing amino acid and an inhibitory
(calming) neurotransmitter. Taurine improves sleep, relieves anxiety, alleviates fatigue, aids with metabolism and digestion, and promotes
glucose control and electrolyte balance.
The main source of taurine is diet (highest in shellfish and poultry (dark meat)). Taurine protects healthy cells and tissues, functions as a potent
antioxidant to reduce oxidative stress, mitigates mitochondrial and endoplasmic reticulum stress, inhibits lipid peroxidation, improves energy
metabolism, regulates gene expression, and participates in detoxification, calcium homeostasis and osmoregulation processes. By fulfilling all
these functions, taurine is therefore protective in cardiovascular health, improves lean body mass and exercise performance. With regard to
brain health, taurine serves a neuroprotective role, promotes neural development in embryonic and adult brain tissues, and is an important factor
in neurogenesis.
Research shows that taurine excretion is low specifically with vegetarian or vegan diets (Rana and Sanders 1986) and with low protein diets in
general (Turner, Brum et al. 1964). Low taurine levels are implicated in diabetes (Sak, Erdenen et al. 2019), hypertension (Sak, Erdenen et al.
2019) and breast cancer (El Agouza, Eissa et al. 2011).
THERAPEUTIC CONSIDERATIONS: taurine is found in most types of meat, shellfish, and fish - increasing intake of these foods may help
restore normal taurine levels. Additionally, taurine supplementation is considered safe and can be tolerated up to 3 g per day without adverse
effects.
EXCITATORY NEUROTRANSMITTERS
GLUTAMATE
Glutamate is low-normal (< 20th percentile). The brain's major excitatory neurotransmitter glutamate functions as the "on" switch in the brain.
Glutamate regulates appetite, thinking, increases gut motility, optimizes learning, modulates memory, improves libido, and decreases sleep. Low
urinary glutamate levels have been reported in patients with migraines (Ragginer et al., 2012). Clinically, lower glutamate levels may contribute
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
14 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
TEST REPORT | Comments continued # D2021 03 17 876 U
to agitation, depression, chronic fatigue, lack of concentration, low energy levels, and sleep difficulties.
THERAPEUTIC CONSIDERATIONS:: L-glutamine may be beneficial to restore glutamate to normal values.
GLUTAMINE
Glutamine is lower than the reference range. Glutamine is an essential and should be the most abundant free amino acid in the human body.
Glutamine provides fuel for rapidly dividing cells (lymphocytes, enterocytes and epithelial cells of the intestines), helps balance ammonia levels
in the body, improves immune system function, contributes to biosynthesis of proteins, amino acids, nucleic acids and glutathione, and protects
intestinal lining. Additionally, glutamine increases glutamate and GABA levels in the brain and in the body.
Although the body usually makes enough glutamine to meet all its needs, extreme stress (e.g., strenuous exercise, persistent stress, or injury)
can increase the demand for glutamine beyond the amount naturally manufactured. Research on urinary low glutamine levels is scarce,
however low circulating glutamine levels are reported after intense exercise (Keast, Arstein et al. 1995), in overtraining syndrome (Rowbottom,
Keast et al. 1996), in diabetes (Liu, Zheng et al. 2019), depression (Umehara, Numata et al. 2017), and in autism spectrum disorder (Rolf,
Haarmann et al. 1993, Moreno-Fuenmayor, Borjas et al. 1996). Low glutamine levels are associated with high oxidative stress (Pietzner, Kaul et
al. 2017).
THERAPEUTIC CONSIDERATIONS: consider supplementation with glutamine which comes in capsules or powder. Glutamine is a fairly bland
tasting amino acid and easily goes into smoothies. Glutamine is also high in chicken, fish, cabbage, spinach, diary, tofu and lentils among many
over foods.
HISTIDINE
Histidine is low. Histidine is a semi-essential amino acid that gives rise to the neurotransmitter histamine. Histidine protects neurons, assists with
making new blood cells, reduces inflammation and oxidative stress, helps with tissue repair and growth. Histidine also helps ameliorate fatigue,
promotes clear thinking and concentration, reduces appetite, decreases anxiety, improves sleep and glucose homeostasis.
Research shows that urinary levels of histidine are low in in folate deficiency (Cooperman and Lopez 2002). Low histidine levels are also
implicated in obesity (Niu, Feng et al. 2012), fatigue with MS (Loy, Fling et al. 2019), rheumatoid arthritis (Gerber 1975), obstructive pulmonary
disease (Diao, Labaki et al. 2019), and chronic kidney disease (Watanabe, Suliman et al. 2008).
THERAPEUTIC CONSIDERATIONS: dosages of histidine up to 4 g/day have shown no negative side effects and have been associated with
general improvements. Meat, fish, eggs, soy, and beans are all high in histidine.
HISTAMINE
Histamine is high-normal (>80th percentile). Histamine is both a neurotransmitter and a modulator of the immune system that has anti-pain
properties, plays a neuroprotective role in the brain, and contributes to optimal maintenance of cognition and memory. Histamine stimulates
wakefulness and decreases sleep, stimulates gastric acid production, increases metabolism, suppresses appetite, and prevents weight gain.
Histamine is a potent vasodilator and a pro-inflammatory agent. Research shows that urinary histamine is high in patients with burns (Johansson
et al., 2012), flushing disorder (Myers et al., 1981), food allergies (Raithel et al., 2015), cystitis (el-Mansoury et al., 1994), polycythemia
(Horakova et al., 1977), and pregnancy (Harrison et al., 1974). Clinically, high histamine levels are implicated in allergies, depression,
headaches, migraines, OCD, schizophrenia, sensitivity to chemicals, and sleep difficulties.
THERAPEUTIC CONSIDERATIONS: Therapeutic strategies to reduce histamine levels may involve antihistamines and a low histamine diet.
High histamine foods include but are not limited to beer, champagne, aged cheeses, eggplant, canned fish, fermented meat, red and white wine,
sauerkraut, and spinach (Maintz and Novak, 2007). Additionally, flavonoids (green tea extract, quercetin, grape seed extract, gingko biloba,
citrus bioflavonoids, bilberry extract, hawthorn extract) may be beneficial to ease the symptoms of high histamine (Murray et al., 2005).
N-METHYLHISTAMINE
N-Methylhistamine is high. N-Methylhistamine is a major metabolite of the neurotransmitter histamine. Research shows that N-methylhistamine
excretion is elevated with high protein diet (Keyzer, Breukelman et al. 10/1984), in gastrointestinal food allergies (Raithel, Hagel et al. 2015), in
irritable bowel disease (Winterkamp, Weidenhiller et al. 2002), in colitis (Schwab, Hahn et al. 2003), in histidinemia (Imamura, Watanabe et al.
1984), in chronic urticaria (Patel and Divekar 2017), in angioedema (Patel and Divekar 2017), and with interstitial cystitis (el-Mansoury, Boucher
et al. 8/1994).
THERAPEUTIC CONSIDERATIONS: evaluation for food allergy sources may be warranted.
PEA
PEA is low-normal (< 20th percentile). PEA, also known as phenethylamine, promotes energy, elevates mood, and regulates attention. Low
urinary PEA levels are detected in patients with autism (Kusaga et al., 2002), ADHD, (Kusaga et al., 2002; Baker et al., 1991; Irsfeld et al.,
2013), depression (Sabelli and Mosnaim, 1974), eating disorders (bulimia nervosa) (Davis et al., 1994), inattentiveness (Faraone et al., 2014),
Parkinson's disease (Wolf and Mosnaim, 1983), and Tourette's syndrome (Bornstein et al., 1990). Clinically, low PEA is suspected to contribute
to inability to concentrate, memory issues, and weight control difficulties.
THERAPEUTIC CONSIDERATIONS: Supplementation with PEA, phenylalanine, and cofactors (e.g. B6) that aid with PEA metabolism may be
helpful to increase PEA levels. Additionally, beans, chocolate, cocoa nibs, eggs, Korean natto, and peas are food sources of PEA.
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
15 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
TEST REPORT | Comments continued # D2021 03 17 876 U
TYROSINE
Tyrosine is within range. Tyrosine is obtained from diet (sesame seeds, cheese, soy, meat, nuts and fish) or synthesized in the body from the
amino acid phenylalanine. Tyrosine serves as a constituent of proteins and gives rise to neurotransmitters, like dopamine, norepinephrine and
epinephrine; and the trace-amine tyramine. Additionally, in the thyroid gland, tyrosine can also be iodinated to give rise to thyroid hormones.
Tyrosine enhances cognitive performance, energy, and alertness, and improves memory after sleep deprivation. Tyrosine also prevents the
depletion of central and peripheral catecholamines (dopamine, norepinephrine, epinephrine) induced by acute stress, thereby eliciting protective
effects on behavioral and cardiovascular parameters in the body.
TYRAMINE
Tyramine is within range. Tyramine is a trace amine derived from the amino acid tyrosine that is found naturally in food. Specifically, tyramine is
found in aged, fermented cured or spoiled food where microbes with decarboxylase enzymes convert tyrosine to tyramine. These foods include
aged cheeses, smoked fish, cured meats, wine, and some types of beer. In sensitive individuals, eating high amount of tyramine can trigger
migraines and increase blood pressure.
DOPAMINE
Dopamine is low-normal (<20th percentile). Dopamine improves attention, focus, and motivation, helps with decision making, modulates
movement control, promotes lactation, increases blood pressure, urine output and sodium excretion, and allows for feelings of reward and
pleasure. Additionally, the quest for dopamine stimulation plays a central role in the etiology of addiction. Dopamine also serves as the parent
precursor to norepinephrine and epinephrine. Research shows that urinary dopamine levels are reduced in patients with Alzheimer's disease
(Liu et al., 2011), anorexia nervosa (Van Binsbergen et al., 1991), anxiety with depression (Field et al., 2010), fibromyalgia (Riva et al., 2012),
and periodic limb movement disorder (Cohrs et al., 2004). Clinically, low dopamine is also implicated in apathy, cravings, fatigue, impulse control
issues, increased sensitivity to pain, low libido, low mood, memory issues, sleep disturbances, and weight control issues.
THERAPEUTIC CONSIDERATIONS: Supplementation with precursors (tyrosine or L-DOPA) and/or cofactors (iron, vitamin B6, tetrahydrofolate)
to promote biosynthesis may be beneficial.
DOPAC
DOPAC is low-normal (<20th percentile). DOPAC is the primary metabolite of dopamine formed via the actions of monoamine oxidase.
Research shows that DOPAC is reduced in the urine of patients with Alzheimer's disease (Liu et al., 2011). Lower than optimal levels suggest
that dopamine and its upstream precursors L-Dopa or tyrosine may be insufficient. DOPAC may also be lower due to MAO genetic SNPs which
can slow down this enzyme or insufficient vitamin B2 or copper levels. Evaluate this level in combination with dopamine, but also 5HIAA (the
serotonin metabolite) since it also uses the MAO enzyme.
THERAPEUTIC CONSIDERATIONS: Consider supplementing with the building blocks of dopamine (tyrosine and/or l-dopa). L-dopa is found
naturally in the herb mucuna as well as supporting nutritional co-factors used with MAO enzymes.
HVA
Homovanillic acid (HVA) is within reference range. HVA is a dopamine metabolite.
NOREPINEPHRINE
Norepinephrine is within reference range. Norepinephrine functions both as a neurotransmitter and a hormone, participating in the body's "fight
or flight" response. Norepinephrine increases alertness, focuses attention, fine-tunes vigilance, increases blood pressure, heart rate, and blood
sugar, reduces digestive activity, pain, and sleep, prevents bladder emptying, and regulates body temperature. Norepinephrine is very similar in
structure and physiological effects to epinephrine. The adrenal gland produces approximately 20% of the total output with 80% produced by the
sympathetic nerve fibers.
NORMETANEPHRINE
Normetanephrine is within reference range. Normetanephrine is a norepinephrine metabolite formed via the actions of catechol-O-methyl
(COMT) transferase enzyme in response to stress.
EPINEPHRINE
Epinephrine is within reference range. Epinephrine, also called adrenaline, functions both as a neurotransmitter and a hormone, participating in
the body's fight or flight response. Epinephrine increases alertness, focuses attention, fine-tunes vigilance, increases blood pressure, heart rate,
and blood glucose, reduces digestive activity, pain and sleep, prevents bladder emptying, and regulates body temperature.
VMA
Vanillylmandelic acid (VMA) is within reference range. VMA is a norepinephrine and epinephrine metabolite formed via the actions of
monoamine oxidase, catechol-O-methyl transferase (COMT), and aldehyde dehydrogenase.
INFLAMMATORY MARKERS
KYNURENINE
Kynurenine is high-normal (>80th percentile). Kynurenine is a central metabolite of the amino acid tryptophan with vasodilatory properties.
Kynurenine is utilized by the body in the production of niacin (vitamin B3), eventually leading to the formation of NAD+, which plays a pivotal role
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
16 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
TEST REPORT | Comments continued # D2021 03 17 876 U
in energy metabolism, gene expression, cell death and regulation of calcium homeostasis. More than 90% of the body's tryptophan is
metabolized to the kynurenine pathway.
Kynurenine is synthesized by the enzyme tryptophan dioxygenase, which is expressed primarily but not exclusively in the liver, and indoleamine
2,3-dioxygenase, which is made in many tissues in response to immune activation by interferons and cytokines, or free radicals. In the brain,
approximately ~40% of kynurenine is produced locally, whereas the rest is absorbed from the blood.
Kynurenine degradation generates a series of neuroprotective and neurotoxic compounds that can activate or inhibit N-methyl-d-aspartate
(NMDA) glutamate receptors (see kynurenic acid and 3-OH kynurenine). Upregulation of this pathway may be a hallmark of neuroinflammation
and is associated with certain disorders.
Research shows that kynurenine is high in high with tryptophan administration (Michael, Drummond et al. 1964), hydrocortisone treatment (Rose
and Braidman 1971), metabolic syndrome (Oh, Seo et al. 2017), with major coronary events (Pedersen, Svingen et al. 9/2013), and in women in
pregnancy (Rose and Braidman 1971). High kynurenine levels have been implicated in disorders like Irritable Bowel Syndrome (Fitzgerald,
Cassidy Eugene et al. 2008), lupus (Akesson, Pettersson et al. 2018), Crohn's disease (Gupta, Thaker et al. 2012), and Alzheimer's Disease
(Chatterjee, Goozee et al. 2018). Additionally, caffeine (Orlikov and Ryzov 1991) and regular black tea (Gostner, Becker et al. 2015)
consumption can elevate kynurenine levels as well.
TREATMENT CONSIDERATIONS: reduction of inflammation through diet and supplementation may be beneficial. Glutathione support and
modulation of the NMDA receptor (e.g. magnesium) may help reduce symptoms.
KYNURENIC ACID
Kynurenic acid is within range. Kynurenic acid is a neuroactive metabolite produced from kynurenine. Kynurenine is formed from tryptophan via
the enzyme tryptophan dioxygenase and indoleamine 2,3-dioxygenase; and metabolized along two independent pathways to produce kynurenic
acid via aminotransferases and 3-OH kynurenine.
Kynurenic acid (unless in excess amounts) is regarded to have a neuroprotective role because it inhibits the N-methyl-d-aspartate (NMDA)
glutamate receptor, reduces the neurotransmitter glutamate release and thereby prevents excitotoxicity.
3-HYDROXYKYNURENINE
3-Hydroxykynurenine is high. 3-Hydroxy Kynurenine (3-OH Kynurenine) is a metabolic intermediate of the kynurenine pathway, one of the major
metabolites of tryptophan degradation. Kynurenine is transformed into 3-OH Kynurenine, which acts as a N-methyl-d-aspartate (NMDA)
glutamate receptor agonist and has been demonstrated to exert neurotoxic effects.
Neurotoxicity elicited by 3-OH Kynurenine appears to be also related to generation of oxidative stress produced by reactive radical species,
formed as a result of auto-oxidation. Additionally, 3-OH Kynurenine gives rise to neurotoxic metabolites, such as quinolinic acid, which activate
the NMDA receptor, induce lipid peroxidation and promote oxidative stress.
Research shows that urinary levels of 3-OH Kynurenine are high with hydrocortisone treatment (Rose and Braidman 1971) and in women in
pregnancy (Rose and Braidman 1971). High 3-OH Kynurenine is implicated in vitamin B6 deficiency (Theofylaktopoulou, Ulvik et al. 2014) and
Alzheimer's disease (Schwarz, Guillemin et al. 2013).
TREATMENT CONSIDERATIONS: consider glutathione support and antioxidant support to prevent the oxidative stress produced by 3-
hydroxyhynurenine. Consider B6 supplementation (under 200 mg/day for safety).
XANTHURENIC ACID
Xanthurenic acid is within range. Xanthurenic acid is a metabolite of the kynurenine pathway, formed directly from 3-OH Kynurenine, and serves
as an indirect marker of vitamin B6 status.
URINARY FREE CORTISOL (F) AND CORTISONE (E)
Urinary free cortisol (F) and cortisone (E) are NOT following a normal circadian rhythm and levels are outside the expected reference ranges,
particularly in the first two morning voids. F and E are very high in the first morning void, but drop precipitiously in the second void but begin to
recover to normal reference ranges in the evening and at night before bed. This individual has reported use of a synthetic glucocorticoid,
commonly used topically for treating skin conditions associated with inflammation. Synthetic glucocorticoids that enter the systemic circulation
suppress endogenous cortisol synthesis by negative feedback to the hypothalamic-pituitary-adrenal axis and lower ACTH/cortisol synthesis. The
negative feedback is transient and may result in a rebound with higher synthesis of cortisol several hours afterward. Low second morning
cortisol likely results from use of the synthetic glucocorticoid after collecting the first morning void. As seen in these results cortisol recovers to
expected levels in the evening and at night before bed. A high F and E in the first morning void suggests that levels are high during sleep at night
or rise rapidly just before waking (possible rebound from evening use of the synthetic glucocorticoid).
Overall, these results indicate that endogenous cortisol synthesis is high and is somewhat amplified by use of the topical synthetic
glucocorticoid. Self-reported symptoms (e.g. excessive stress, fatigue, depression, irritability, decreased mental sharpness, weight gain most in
the waist (belly fat), are consistent with overall high cortisol exposure.
While a normal daily adrenal output of cortisol is essential to maintain normal metabolic activity, help regulate steady state glucose levels
(important for brain function and energy production), and optimize immune function, excessive levels of glucocorticoids (natural and synthetic)
can have the opposite effect over time. For information about strategies to support adrenal health and reduce stress(ors) that can lead to excess
or deficient cortisol synthesis, the following books are worth reading: "Adrenal Fatigue", by James L. Wilson, N.D., D.C., Ph.D.; "The Cortisol
Connection", by Shawn Talbott, Ph.D.; "The End of Stress As We Know It" by Bruce McEwen; "The Role of Stress and the HPA Axis in Chronic
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
17 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
TEST REPORT | Comments continued # D2021 03 17 876 U
Disease Management" by Thomas Guilliams, PhD.
MELATONIN METABOLITE 6-SULFATOXYMELATONIN (MT6s)
The melatonin metabolite 6-sulfatoxymelatonin (MT6s) is not following a normal circadian rhythm. MT6s should be at its highest level in the first
morning void, which is reflective of the dark period (night), but instead is low. Lower MT6s in the first morning void may reflect work during a
night shift or staying up at night with excessive lighting (e.g. watching television). Some sleep (benzodiazepines, barbituates), pain (ibuprofen,
opiates) and blood pressure medications (beta blockers like propranolol) are known to interfere with melatonin production and secretion and
lower the circulating and excreted (MT6s) urinary levels of melatonin. Use of any of these medications at night before bed would result in a lower
melatonin in the first morning void. The second morning void in this individual is also lower than the reference range. MT6s begins to rise
thereafter in the evening and is within normal reference range at night before bed.
In a healthy individual the circadian rhythm of melatonin is inversely related to circulating levels of adrenal cortisol levels, i.e. melatonin rises with
darkness and peaks about 2-3 am, while cortisol falls to its lowest level at this time of day. With morning and onset of light exposure, melatonin
drops rapidly and cortisol rises, peaking to its highest level about 30 min to 1 hr after waking (referred to as a Cortisol Awakening Response-
CAR). By mid-afternoon (evening void) with maximal light exposure melatonin reaches a nadir. It then gradually begins to rise again with nightfall
and less light exposure, while cortisol continues to rise. Cortisol and melatonin reach their nadir and peak, respectively, about 2-3 am. Melatonin
synthesis by the pineal gland is controlled by light exposure, while cortisol synthesis is controlled by the hypothalamic-pituitary axis in response
to stressors. While melatonin and cortisol have opposing circadian rhythms neither hormone directly and acutely controls the synthesis of the
other.
Melatonin is known to have many different beneficial effects in the body. For an excellent review of melatonin's many benefits please read:
Pandi-Perumal et.al. Melatonin, Nature's most versatile biological signal. FEBS 273: 2813-2838, 2006. Melatonin has multiple roles in
maintaining health. It helps slow the aging process, is a potent anti-oxidant, regulates the immune system, inhibits formation and growth of
tumors such as breast and prostate cancers, and helps regulate the synthesis of the sex-hormones estradiol and progesterone (melatonin
increases progesterone, decreases estrogens by inhibiting aromatase, and down-regulates cellular estrogen receptors, which diminishes
response of estrogen-sensitive tissues to estrogens). Low melatonin is also thought to contribute to obesity in people with insomnia or those who
do night shift work.
Because of its established role in the regulation of the circadian rhythm, treatment with exogenous melatonin has been found useful in people
with circadian rhythm sleep disorders, such as delayed sleep phase disorder, jet lag, shift worker disorder, and the non-24-hour sleep-wake
disorder most commonly found in totally blind individuals; however, its utility for the treatment of insomnia is not established and remains
controversial.
If melatonin is taken as a supplement (available OTC) to correct low levels or treat a condition, the timing and dosage are important to its
effectiveness, especially as a sleep aid. Response to supplemental melatonin can be very individual. For optimal benefit it is best to work with a
health care provider familiar with melatonin dosage and timing. Excessive dosing can result in spillover of melatonin into daylight hours,
excessive sleepiness during the day, and disruption of the normal melatonin-cortisol circadian rhythms.
For more general information about melatonin please see: http://www.nlm.nih.gov/medlineplus/druginfo/natural/940.html
DIURNAL EPINEPHRINE
Epinephrine is elevated during the night (1st morning), but returns to normal range in the morning (2nd sample), and remains within normal
ranges throughout the day (evening collection) and at night (evening/night sample) before bed. The pooled sample is within range, but the
diurnal results are more accurate for true epinephrine status. Epinephrine, also called adrenaline, functions both as a neurotransmitter and a
hormone, participating in the body's "fight or flight" response. Epinephrine increases alertness, focuses attention, fine-tunes vigilance, increases
blood pressure, heart rate, and blood glucose, reduces digestive activity, pain and sleep, prevents bladder emptying, and regulates body
temperature. It is commonly triggered by stress, fear, blood sugar irregularities or anxiety.
Research shows that urinary epinephrine levels are increased in patients with attention deficit disorder (Faraone et al., 2014), anxiety and
depression (Hughes et al., 2004), bipolar disorder (Koslow et al., 1983), hyperglycemia (Troisi et al., 1991), hyperinsulinemia (Troisi et al., 1991),
obstructive sleep apnea (Kheirandish-Gozal et al., 2013), post-traumatic stress disorder (Yehuda et al., 1992), and stress (Holzman et al., 2009;
Fujiwara et al., 2004). Fluctuating levels throughout the day have been commonly associated with an inverse relationship with cortisol (e.g. high
epi when cortisol is low).
THERAPEUTIC CONSIDERATIONS: Because epinephrine is almost exclusively from the adrenal glands, treatments geared to support normal
adrenal function and calm the sympathetic nervous system may be beneficial. Supplements such as adrenal adaptogens, B vitamins, essential
fatty acids, vitamin C, as well as stress management, blood sugar balance and sleep support may be helpful.
Creatinine is within range throughout the day reflecting normal concentration of urine.
Creatinine levels reflect urine concentration.
Low values suggest overly dilute urine; High values suggest overly concentrated urine.
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
18 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
NeuroAdvanced w Diurnal
TEST REPORT | Comments continued # D2021 03 17 876 U
Extreme low or high values may be induced by kidney or other metabolic disorders, but most values will be due to inadequate hydration (high
creatinine) or excessive water intake in the several hours prior to testing (low creatinine). Creatinine is used to adjust the lab results for kidney
function. No samples were refused due to quality issues.
CLIA Lic # 38D0960950
3/18/2021 9:12:22 AM
The above results and comments are for informational
purposes only and are not to be construed as medical
David T. Zava, Ph.D.
Laboratory Director
Alison McAllister, ND.
(Ordering Provider unless
19 of 19
advice. Please consult your healthcare practitioner for otherwise specified on page 1)
diagnosis and treatment.
© 1998-2021 ZRT Laboratory, LLC. All rights reserved.
You might also like
- Clinical Evaluation of Purified Shilajit On TestosteroneDocument6 pagesClinical Evaluation of Purified Shilajit On TestosteroneAlejandro MüllerNo ratings yet
- 7 Food Timing Hacks For Rapid Fat LossDocument20 pages7 Food Timing Hacks For Rapid Fat LossLennart BjurstromNo ratings yet
- Perfect Health For Dogs and CatsDocument36 pagesPerfect Health For Dogs and CatsKit Cain100% (1)
- Biomarker Ranges Functional Vs StandardDocument3 pagesBiomarker Ranges Functional Vs Standardswetor100% (1)
- Pharmacology Unit 1Document58 pagesPharmacology Unit 1Asif Ali LashariNo ratings yet
- A26 - Walk in Paschim Vihar Ii: NoteDocument2 pagesA26 - Walk in Paschim Vihar Ii: NoteLakshay MahajanNo ratings yet
- Lalpathlab PDFDocument3 pagesLalpathlab PDFTushar Kar0% (1)
- Soal MCQDocument39 pagesSoal MCQRonald Allan Valle SantosNo ratings yet
- Origin of Lymphoid Neoplasms: CLP: BLB: NBC: MC: GC: MZDocument26 pagesOrigin of Lymphoid Neoplasms: CLP: BLB: NBC: MC: GC: MZSri Naharindah NingNo ratings yet
- Profhegde PDFDocument130 pagesProfhegde PDFRahul Pagidala100% (1)
- Case Study ThyroidectomyDocument8 pagesCase Study Thyroidectomyapi-347153077No ratings yet
- Salonga, Rosalina Bartolo 2340043643Document4 pagesSalonga, Rosalina Bartolo 2340043643judeNo ratings yet
- Lcms Saliva Sample ReportDocument6 pagesLcms Saliva Sample ReportDaniNo ratings yet
- 99fbcd52 Da4b 4be2 Bfd8 789c8ffdc7eeDocument7 pages99fbcd52 Da4b 4be2 Bfd8 789c8ffdc7eeG D HEALTH CARENo ratings yet
- L89 - Muzaffar Nagar Cc3 Shop No. 11, Near Dr. Dharampal Singh Sadar Bazar Muzaffarnagar 251001Document4 pagesL89 - Muzaffar Nagar Cc3 Shop No. 11, Near Dr. Dharampal Singh Sadar Bazar Muzaffarnagar 251001shivang ranaNo ratings yet
- Anemico Miriam: IDEXX ServicesDocument1 pageAnemico Miriam: IDEXX ServicesThalia ZuluetaNo ratings yet
- 001 230323583 CB6 117 3Document1 page001 230323583 CB6 117 3waqasjhseNo ratings yet
- SBKRDocument7 pagesSBKRsourabhkhatri131No ratings yet
- Analisis 2Document6 pagesAnalisis 2josé armando ramirezNo ratings yet
- Date 24/dec/2022 08:32AM 03/dec/22 09:33AM 26/nov/22 09:05AM Unit Bio Ref IntervalDocument11 pagesDate 24/dec/2022 08:32AM 03/dec/22 09:33AM 26/nov/22 09:05AM Unit Bio Ref IntervalAmit SinghNo ratings yet
- Mrs. V.DHANALAXMIDocument2 pagesMrs. V.DHANALAXMIAnonymous lSZ9JVNo ratings yet
- Gulapa, Hanah Gracia Besar 2371011421Document3 pagesGulapa, Hanah Gracia Besar 2371011421Hanah GulapaNo ratings yet
- FBCReport Aspx2Document2 pagesFBCReport Aspx2RahulNo ratings yet
- 02dc8e95-538f-43c2-9f8f-54e118503267Document10 pages02dc8e95-538f-43c2-9f8f-54e118503267reenasingh26092004No ratings yet
- TN Widodo 20231204004 - 231204 - 211846Document2 pagesTN Widodo 20231204004 - 231204 - 211846PhjnNo ratings yet
- Surendra KumarDocument2 pagesSurendra KumarUjjwal KumarNo ratings yet
- Cczzst5oiztfamqh0e0xjjeaDocument2 pagesCczzst5oiztfamqh0e0xjjeaUjjwal KumarNo ratings yet
- Max Lab ReportDocument4 pagesMax Lab ReportKallu PrasadNo ratings yet
- PdfText - 2024-03-15T191650.936Document1 pagePdfText - 2024-03-15T191650.936jayanthmahesh0403No ratings yet
- SVLT Lab Report DetailsDocument2 pagesSVLT Lab Report DetailsDaya RaniNo ratings yet
- SVLT Lab Report DetailsDocument1 pageSVLT Lab Report DetailsJaiprakash GuptaNo ratings yet
- SL Report-287060681Document7 pagesSL Report-287060681SubhaNo ratings yet
- PDFDocument4 pagesPDFmelsabaeNo ratings yet
- Muneca Izquierdo 2023 11 01 1529Document1 pageMuneca Izquierdo 2023 11 01 1529ucivetperuNo ratings yet
- 05062023CA6901RDocument1 page05062023CA6901Rasad922No ratings yet
- Bilirubin Total-2303-00945Document1 pageBilirubin Total-2303-00945adiljuttNo ratings yet
- Lucy Toma Vasile 2023 01 25 1056Document3 pagesLucy Toma Vasile 2023 01 25 1056marian vasile tomaNo ratings yet
- ebe62dd8-6966-4e8d-8c16-26e2035aca80Document6 pagesebe62dd8-6966-4e8d-8c16-26e2035aca80ankitkumarpatna482No ratings yet
- 5ded66d6-1410-4590-ac97-cba8de91f7d2Document6 pages5ded66d6-1410-4590-ac97-cba8de91f7d2sahatwarccNo ratings yet
- Final Report Patient Progress Report: Steroid Hormone Tests (Saliva)Document2 pagesFinal Report Patient Progress Report: Steroid Hormone Tests (Saliva)Kaveh EshkoftiNo ratings yet
- BP2023021645715 PDFDocument5 pagesBP2023021645715 PDFzena carterNo ratings yet
- Salonga, Jesus Garcia 2340043644Document3 pagesSalonga, Jesus Garcia 2340043644judeNo ratings yet
- Chemistry - I: TEST(s) Normal UNIT(s)Document1 pageChemistry - I: TEST(s) Normal UNIT(s)Waheed AhmadNo ratings yet
- (CENTRO MEDICO KARAM, C.A. J-29872070-0) (Avenida Urdaneta Edificio Karam Piso 7 Oficina 714 0212.564.79.69)Document1 page(CENTRO MEDICO KARAM, C.A. J-29872070-0) (Avenida Urdaneta Edificio Karam Piso 7 Oficina 714 0212.564.79.69)AnaNo ratings yet
- This Is An Electronic Report & Not: To Be Used For Any Legal PurposesDocument2 pagesThis Is An Electronic Report & Not: To Be Used For Any Legal PurposesAyazNo ratings yet
- Kongamdana: Clinical BiochemistryDocument5 pagesKongamdana: Clinical BiochemistryShariqNo ratings yet
- CASE STUDY FORMAT (Kidney Transplantation)Document12 pagesCASE STUDY FORMAT (Kidney Transplantation)ashnaNo ratings yet
- Mahmoorganj CC - 2 Dr. Lal Path Labs LTD Lanka, Varanasi 221005Document4 pagesMahmoorganj CC - 2 Dr. Lal Path Labs LTD Lanka, Varanasi 221005osmovinodchaubeyNo ratings yet
- 001 200607833 CF7 117 1Document1 page001 200607833 CF7 117 1Umer Bin SalmanNo ratings yet
- Bailey ReportDocument1 pageBailey Reportnithya.amiraNo ratings yet
- 001 240406541 CW8 117 1Document1 page001 240406541 CW8 117 1Wajih FarhanNo ratings yet
- Https WWW - Midas.com - NP Hospital Labreports Reports Reports Index 2079-N36700Document2 pagesHttps WWW - Midas.com - NP Hospital Labreports Reports Reports Index 2079-N36700ABhishek KishanNo ratings yet
- Adobe Scan Jun 07, 2023Document3 pagesAdobe Scan Jun 07, 2023protyushkar1No ratings yet
- Adobe Scan Nov 08, 2022Document11 pagesAdobe Scan Nov 08, 2022artemis 0516No ratings yet
- CQ055945 2349007340 Files indivPDF 2023 3 1 2349007340Document5 pagesCQ055945 2349007340 Files indivPDF 2023 3 1 2349007340mocsNo ratings yet
- Lyphochek Immunoassay Plus Control Levels 1, 2 and 3Document11 pagesLyphochek Immunoassay Plus Control Levels 1, 2 and 3Enrique DuarteNo ratings yet
- Machado PDFDocument4 pagesMachado PDFpm2001No ratings yet
- VS TL - Urine - L2 28565 2112 2Document24 pagesVS TL - Urine - L2 28565 2112 2mnemonicsNo ratings yet
- Daya Lab Report 13703222503202309101Document1 pageDaya Lab Report 13703222503202309101WebkuttanNo ratings yet
- ab28ea20-53df-4b65-8c10-0d19640922c6Document2 pagesab28ea20-53df-4b65-8c10-0d19640922c6Ujjwal KumarNo ratings yet
- L38 - FPSC Gms Road Gms Road, Near Saffron Leaf Hotel DEHRADUN, UK - 248007, Ambiwala B.ODocument5 pagesL38 - FPSC Gms Road Gms Road, Near Saffron Leaf Hotel DEHRADUN, UK - 248007, Ambiwala B.Oanadinath sharmaNo ratings yet
- Mohamad Afify AmbulatorySummary1 2023-01-16 To 2023-01-18 PDFDocument27 pagesMohamad Afify AmbulatorySummary1 2023-01-16 To 2023-01-18 PDFMo AfifyNo ratings yet
- Lyphochek Immunoassay Plus Control Levels 1, 2 and 3: Fecha de Revisión 2021-04-20 Indica Información RevisadaDocument25 pagesLyphochek Immunoassay Plus Control Levels 1, 2 and 3: Fecha de Revisión 2021-04-20 Indica Información RevisadaMariam MangaNo ratings yet
- PDFDocument9 pagesPDFCésar CuadraNo ratings yet
- SVLT Lab Report DetailsDocument1 pageSVLT Lab Report DetailsAnirudh JHA100% (1)
- Stem-Cell Therapy-For-Cardiac-RepairDocument19 pagesStem-Cell Therapy-For-Cardiac-RepairJob MonobeNo ratings yet
- Usos TerapeuticosDocument33 pagesUsos TerapeuticosJob MonobeNo ratings yet
- Artrosis MSCDocument9 pagesArtrosis MSCJob MonobeNo ratings yet
- Diabetes 1 y Celuas Madre 2015Document9 pagesDiabetes 1 y Celuas Madre 2015Job MonobeNo ratings yet
- Positive EmotionsDocument15 pagesPositive EmotionsJob MonobeNo ratings yet
- Mesenchymal Stem Cell Mediated Cancer Therapy CryovidaDocument8 pagesMesenchymal Stem Cell Mediated Cancer Therapy CryovidaJob MonobeNo ratings yet
- Reporte Muestra - Dna MindDocument20 pagesReporte Muestra - Dna MindJob MonobeNo ratings yet
- Jurnal Sains Dan Teknologi Laboratorium MedikDocument6 pagesJurnal Sains Dan Teknologi Laboratorium MedikAfrizal ThezxemoengNo ratings yet
- Throughout The Lesson, The Students Are Expected To:: Movements, Undergone Long Duration of TimeDocument3 pagesThroughout The Lesson, The Students Are Expected To:: Movements, Undergone Long Duration of TimeWinter Summer SmithNo ratings yet
- 2 Toxicokinetics & ToxicodynamicsDocument32 pages2 Toxicokinetics & ToxicodynamicsLaura RodriguezNo ratings yet
- Group Discussion Second Year Cardiovascular SystemDocument2 pagesGroup Discussion Second Year Cardiovascular Systemola nagarNo ratings yet
- Progesterone III: A) Tris (2,2'-Bipyridyl) Ruthenium (II) - Complex (Ru (Bpy) )Document4 pagesProgesterone III: A) Tris (2,2'-Bipyridyl) Ruthenium (II) - Complex (Ru (Bpy) )Jimboreanu György PaulaNo ratings yet
- Diabetes Mellitus in Children 1Document89 pagesDiabetes Mellitus in Children 1Vinay PatilNo ratings yet
- Nejmoa 2111953Document10 pagesNejmoa 2111953Andreea VlădanNo ratings yet
- Frequent OralsDocument91 pagesFrequent Oralsfatma daganeNo ratings yet
- Chemical Coordination and IntegrationDocument17 pagesChemical Coordination and IntegrationHemant KumarNo ratings yet
- Warm-Up Strategies For Sport and Exercise: Mechanisms and ApplicationsDocument25 pagesWarm-Up Strategies For Sport and Exercise: Mechanisms and Applicationsbiciusas the coachNo ratings yet
- 28 - Extracted - Supplementary Material Biology (Revised)Document9 pages28 - Extracted - Supplementary Material Biology (Revised)Mahalaksshmi .DNo ratings yet
- Male Physical and Sexual Changes: Happening To An IndividualDocument2 pagesMale Physical and Sexual Changes: Happening To An IndividualMarian Licuasen Ab-aboNo ratings yet
- SgfsDocument1 pageSgfsjoycechicagoNo ratings yet
- 99.guidelines For Prevention and Management ofDocument11 pages99.guidelines For Prevention and Management oftereNo ratings yet
- Skema Jawapan Struktur Biologi Tingkatan 5Document38 pagesSkema Jawapan Struktur Biologi Tingkatan 5Ler Ming BangNo ratings yet
- Clinical Chemistry BrochureDocument20 pagesClinical Chemistry Brochureyogesh kumarNo ratings yet
- BSC MLT Syllabus 2020 - SeptemberDocument70 pagesBSC MLT Syllabus 2020 - SeptemberDani DanyNo ratings yet
- NURS FPX 6011 Assessment 1 Evidence-Based Patient-Centered Concept MapDocument4 pagesNURS FPX 6011 Assessment 1 Evidence-Based Patient-Centered Concept MapCarolyn HarkerNo ratings yet
- Urinalysis ChecklistDocument7 pagesUrinalysis ChecklistLana LocoNo ratings yet
- Melatonin Gummies: Body Requirement and Effects of MelatoninDocument13 pagesMelatonin Gummies: Body Requirement and Effects of MelatoninmelatoningummiesNo ratings yet
- Clinical Chemistry Lecture KayzardnDocument3 pagesClinical Chemistry Lecture KayzardnHenry QuimbaNo ratings yet
- Dr. Doni Priambodo, SP - PD-KPTI, FINASIM - Immunomodulator and Antioxidant in SepsisDocument22 pagesDr. Doni Priambodo, SP - PD-KPTI, FINASIM - Immunomodulator and Antioxidant in SepsisOlivia DwimaswastiNo ratings yet
- Compilation and Comparison of Medical Camp Data in The Endosulfan Affected Area in KasaragodDocument4 pagesCompilation and Comparison of Medical Camp Data in The Endosulfan Affected Area in KasaragodDr KMSreekumarNo ratings yet
- Graves Basedow DiseaseDocument17 pagesGraves Basedow Diseaseramona_25No ratings yet