Professional Documents
Culture Documents
Unang Yakap
Uploaded by
Leamae Abayon0 ratings0% found this document useful (0 votes)
17 views2 pagesOriginal Title
UNANG-YAKAP
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
17 views2 pagesUnang Yakap
Uploaded by
Leamae AbayonCopyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
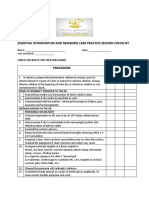
ESSENTIAL INTRAPARTUM AND NEWBORN CARE
PRIOR TO PATIENT’S TRANSFER TO THE DR
Ensure that mother is on her position of choice when in labor.
Ask mother if she wishes to eat/drink.
Communicate with the mother- inform her of progress of labor, give reassurance and
encouragement.
PATIENT ALREADY IN THE DR
Preparing for Delivery
Check temperature in DR area, check for air draft.
Ask patient if patient is comfortable in the semi-upright position which is the default position.
Remove all jewelry.
Wash hands thoroughly observing the proper procedure.
Arrange things in a linear fashion:
Gloves, dry linen, bonnet, oxytocin injection, plastic clamp, instrument clamp, scissors, 2 kidney
basins
Clean the perineum with antiseptic solution.
Wash hands.
Put on 2 pairs of sterile gloves aseptically. (if same worker handles perineum and cord).
At the time Delivery
Encourage woman to push as desired.
Apply perineal support and do controlled delivery of the head.
Call out time of birth and sex of baby.
Inform the mother of outcome.
First 30 seconds
Place the baby on a clean, dry cloth/towel on the mother’s abdomen.
Thoroughly dry baby for at least 30 seconds, starting from the face and head, going down to the
trunk and extremities.
1-3 minutes
Remove wet cloth.
Place baby on skin-to-skin contact on the mother’s abdomen.
Cover the baby with a clean, dry cloth/towel.
Cover baby’s head with a bonnet.
Exclude a 2nd baby by palpating abdomen. Use the wet cloth to wipe the soiled gloves. Give IM
oxytocin within one minute of baby’s birth. Dispose off the wet cloth properly.
Remove the 1st set of gloves.
Decontaminate these properly (by soaking in 0.5% chlorine solution for at least 10 minutes)
Palpate umbilical cord to check for pulsations.
After pulsations stopped, clamp cord using the plastic cord clamp at 2 cm from base.
Place the instrument clamp 5 cm from the base.
Cut near plastic clamp (not midway).
Perfom the remaining steps of the Active Management of Third Stage of Labor:
Wait for strong uterine contractions then apply controlled cord traction and counter traction on
the uterus, continuing until placenta is delivered.
Massage the uterus until it is firm.
Inspect the lower vagina and perineum for lacerations/tears and repaired lacerations/tears if
necessary.
Examine the placenta for completeness and abnormalities.
Clean the mother: flush perineum and apply perineal pad/napkin/cloth
Check baby’s color and breathing; check that mother is comfortable, uterus contracted.
Dispose off the placenta in a leak-proof container or plastic bag.
Decontaminate (soaked in 0.5% chlorine solution) instruments before cleaning; decontaminate 2nd
pair of gloves before disposal.
Advise mother to maintain skin-to-skin contact. Baby should be prone on mother’s chest/in between
the breasts with head turned to one side.
15-90 minutes
Advise mother to observe for feeding cues (cited examples)
Support mother, instruct her on positioning and attachment.
Wait for FULL BREASTFEED to be completed.
After a complete breastfeed, administer eye ointment (first), do thorough physical examination, give
Vit. K, hepatitis B and BCG (simultaneously explain purpose of each intervention).
Advise OPTIONAL/DELAYED bathing of baby (and is able to explain the rationale).
Advise breastfeeding per demand and about Danger Signs for early referral
In the first hour: check baby’s breathing and color; and check mother’s vital signs and massage uterus
every 15 minutes.
In the second hour: check mother-baby dyad every 30 minutes to 1 hour.
Complete all RECORDS: administer eye ointment, vitamin K, hepatitis B and BCG.
You might also like
- ESSENTIAL INTRAPARTUM AND NEWBORN CARE ChecklistDocument2 pagesESSENTIAL INTRAPARTUM AND NEWBORN CARE ChecklistNasriah Macadato88% (26)
- EINC To Be PrintedDocument2 pagesEINC To Be PrintedKathrina Mendoza HembradorNo ratings yet
- Rating Criteria: Prior To Woman'S Transfer To The DRDocument3 pagesRating Criteria: Prior To Woman'S Transfer To The DRPatricia Ann JaringNo ratings yet
- EINCDocument2 pagesEINCmayeNo ratings yet
- Intrapartum and newborn checklistDocument3 pagesIntrapartum and newborn checklistBela MillenaNo ratings yet
- Eesential Intrapartum and Newborn Care Practices - RleDocument2 pagesEesential Intrapartum and Newborn Care Practices - Rleding dutolloNo ratings yet
- Essential Newborn Care Practice ChecklistDocument1 pageEssential Newborn Care Practice ChecklistJeffyNo ratings yet
- Essential Intrapartal and Newborn CareDocument4 pagesEssential Intrapartal and Newborn CareJoycee BoNo ratings yet
- Essential Intrapartum Newborn CareDocument2 pagesEssential Intrapartum Newborn CareKevin LockwoodNo ratings yet
- EINC Checklist - DOHDocument2 pagesEINC Checklist - DOH2A - Nicole Marrie Honrado100% (4)
- EINC Checklist SDRMDocument49 pagesEINC Checklist SDRMloli popNo ratings yet
- EINCDocument9 pagesEINCFLORENCE RIVA MAQUILING GUIMARYNo ratings yet
- 1 Unang YakapDocument3 pages1 Unang Yakapyra capiliNo ratings yet
- Essential Intrapartum and Newborn Care PracticeDocument18 pagesEssential Intrapartum and Newborn Care PracticeCarmel CochingNo ratings yet
- EINC ChecklistDocument3 pagesEINC ChecklistZero TwoNo ratings yet
- EINC Essential Intrapartim NC ChecklistDocument7 pagesEINC Essential Intrapartim NC Checklisthey aadarshaNo ratings yet
- Essential Newborn Care Checklist Ateneo College NursingDocument7 pagesEssential Newborn Care Checklist Ateneo College NursingNur Fatima SanaaniNo ratings yet
- Essential Intrapartum and Newborn Care Suggested Actions Correctly Done Partially Done Not Done RemarksDocument7 pagesEssential Intrapartum and Newborn Care Suggested Actions Correctly Done Partially Done Not Done RemarksSweet BenitezNo ratings yet
- ESSENTIAL INTRAPARTUM NEWBORN CARE (Assisting and Handling Delivery)Document4 pagesESSENTIAL INTRAPARTUM NEWBORN CARE (Assisting and Handling Delivery)Hannah Angelu CabadingNo ratings yet
- EINC ChecklistDocument3 pagesEINC ChecklistShaira Mae Fangon De GuzmanNo ratings yet
- Essential Intrapartum and Newborn Care Practice Session ChecklistDocument3 pagesEssential Intrapartum and Newborn Care Practice Session ChecklistJelaveil De VeraNo ratings yet
- EINC Procedure ChecklistDocument3 pagesEINC Procedure ChecklistKath AngelesNo ratings yet
- EINCDocument16 pagesEINCLea Mee CastroverdeNo ratings yet
- Einc ChecklistDocument9 pagesEinc ChecklistLee Cel100% (1)
- Essential Intrapartal Newborn Care (Einc) Notes By: Yzobelle RedondoDocument11 pagesEssential Intrapartal Newborn Care (Einc) Notes By: Yzobelle RedondoKriztian BorromeoNo ratings yet
- EINC ChecklistDocument3 pagesEINC ChecklistMARK JEFTE BRIONESNo ratings yet
- 3 EINC CHECKLIST HighlightedDocument3 pages3 EINC CHECKLIST HighlightedJohnjohn MarfalNo ratings yet
- Uep - Edu.ph: Nursing AssessmentDocument9 pagesUep - Edu.ph: Nursing AssessmentCzarina Mae Quinones TadeoNo ratings yet
- ENC - at Birth Checklist - Uganda MNCH Facility CollaborativeDocument5 pagesENC - at Birth Checklist - Uganda MNCH Facility CollaborativeadagayNo ratings yet
- 60 Steps to a Normal DeliveryDocument6 pages60 Steps to a Normal DeliveryDrBoen BunawanNo ratings yet
- Conducting A ChildbirthDocument3 pagesConducting A ChildbirthGazala ParveenNo ratings yet
- Delivery Room Rating SheetDocument2 pagesDelivery Room Rating Sheetyabaeve100% (2)
- RD ManualDocument6 pagesRD Manualapple m.No ratings yet
- Unang Yakap 1Document3 pagesUnang Yakap 1Marisse MabutolNo ratings yet
- Einc ScriptDocument3 pagesEinc ScriptJulia Rae Delos SantosNo ratings yet
- RD ManualDocument6 pagesRD Manualapple m.No ratings yet
- Immediate Newborn Care Facilitator GuideDocument58 pagesImmediate Newborn Care Facilitator Guideboinkjilijoy50% (2)
- EINC-checklistDocument3 pagesEINC-checklistSteph VistalNo ratings yet
- NCM 107 SL Semi Final TopicsDocument14 pagesNCM 107 SL Semi Final Topicsmark OrpillaNo ratings yet
- Modul Normal Delivery 2016Document8 pagesModul Normal Delivery 2016Alvin FarhanNo ratings yet
- AMTSL Skills CHKLSTDocument9 pagesAMTSL Skills CHKLSTAliaa HabibNo ratings yet
- Essential Newborn Care StepsDocument9 pagesEssential Newborn Care StepsWeng Maesa MontemayorNo ratings yet
- 4 Core Steps of EincDocument52 pages4 Core Steps of Eincjamaica cabriga100% (1)
- Stages of LaborDocument15 pagesStages of LaborJune DumdumayaNo ratings yet
- Essential Newborn Care PracticesDocument15 pagesEssential Newborn Care PracticesClyde AleczandreNo ratings yet
- Essential Intrapartum Newborn Care 181120082158 PDFDocument19 pagesEssential Intrapartum Newborn Care 181120082158 PDFDorinna Rizada BagaNo ratings yet
- Essential Intrapartum and Newborn CareDocument2 pagesEssential Intrapartum and Newborn CareKia potz100% (1)
- Essential Intrapartum and Newborn CareDocument5 pagesEssential Intrapartum and Newborn Careanjie kamidNo ratings yet
- Essentials of Newborn Care)Document4 pagesEssentials of Newborn Care)Zera Cortez100% (1)
- Handle, Assist, Cord CareDocument2 pagesHandle, Assist, Cord CareMichael Lloyd T. SabijonNo ratings yet
- Essential Intrapartium and Newborn Care Practice (Einc) : Performance Evaluation ChecklistDocument2 pagesEssential Intrapartium and Newborn Care Practice (Einc) : Performance Evaluation ChecklistPam RomeroNo ratings yet
- Infant Care and Feeding Notes 1Document46 pagesInfant Care and Feeding Notes 1Art John CalambaNo ratings yet
- Essential Intrapartum and Newborn Care Practice Session ChecklistDocument28 pagesEssential Intrapartum and Newborn Care Practice Session ChecklistMonica Melchor DoriaNo ratings yet
- Essential Newborn Care ProtocolDocument23 pagesEssential Newborn Care ProtocolKaren Viviene CincoNo ratings yet
- Format APNDocument4 pagesFormat APNRahawarin EllNo ratings yet
- Essential Newborn Care 2013Document145 pagesEssential Newborn Care 2013Ralph Tama Mangacop Benito100% (2)
- Tugas APN 60 Langkah Ristika Wildianti. NDocument9 pagesTugas APN 60 Langkah Ristika Wildianti. NRistikaWildianNo ratings yet
- Emergency Childbirth A Reference Guide for Students of the Medical Self-help Training Course, Lesson No. 11From EverandEmergency Childbirth A Reference Guide for Students of the Medical Self-help Training Course, Lesson No. 11No ratings yet
- 26 - LEAN Weekly Guide - On - October 12Document15 pages26 - LEAN Weekly Guide - On - October 12Andrea CsillaNo ratings yet
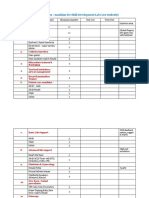
- Republic of The Philippines Department of Education Region VII, Central Visayas Division of BoholDocument4 pagesRepublic of The Philippines Department of Education Region VII, Central Visayas Division of BoholCecille HernandoNo ratings yet
- Certification Exam Candidate Handbook PDFDocument46 pagesCertification Exam Candidate Handbook PDFvetrijNo ratings yet
- Manikins Proposed List For Skill LabDocument3 pagesManikins Proposed List For Skill LabNaren KNo ratings yet
- CRIM 1 Module 5Document8 pagesCRIM 1 Module 5jeffrey PogoyNo ratings yet
- Balkan Bros - Company DeckDocument54 pagesBalkan Bros - Company DeckTutu MosesNo ratings yet
- Pulmonary Tuberculosis - Curitana BSN 2bDocument10 pagesPulmonary Tuberculosis - Curitana BSN 2bDrex CuritanaNo ratings yet
- The Psychiatric Interview - Daniel CarlatDocument473 pagesThe Psychiatric Interview - Daniel CarlatAntonio L Yang96% (26)
- Literature Review On Quality Control SystemDocument6 pagesLiterature Review On Quality Control Systemlsfxofrif100% (1)
- BM POSTER EspDocument1 pageBM POSTER EspAyesha F. SiddiquiNo ratings yet
- Smoking and Alcohol Counselingv2.1Document18 pagesSmoking and Alcohol Counselingv2.1Angelo HuligangaNo ratings yet
- Dwnload Full Introduction To Radiologic and Imaging Sciences and Patient Care 6th Edition Adler Test Bank PDFDocument36 pagesDwnload Full Introduction To Radiologic and Imaging Sciences and Patient Care 6th Edition Adler Test Bank PDFChristopherNortonwqnmc100% (12)
- Child and Adolescent Development Detailed Lesson Plan I. ObjectivesDocument28 pagesChild and Adolescent Development Detailed Lesson Plan I. ObjectivesAndrew Sebi MonsalesNo ratings yet
- VSP - Vision 01Document1 pageVSP - Vision 01api-252555369No ratings yet
- Team 1's Quantitative ApproachesDocument46 pagesTeam 1's Quantitative ApproachesDIANA ALLISON QUINONES JAUREGUINo ratings yet
- Corporate Responsibility: Principles and Perspectives (Mn20445)Document3 pagesCorporate Responsibility: Principles and Perspectives (Mn20445)WilliamArugaNo ratings yet
- Hill, C - Written Assingment 3Document10 pagesHill, C - Written Assingment 3Collin HillNo ratings yet
- January 2024Document1 pageJanuary 2024AmborsiusNo ratings yet
- Ipratropium Salbutamol (DUAVENT)Document2 pagesIpratropium Salbutamol (DUAVENT)Kristine Young100% (2)
- The Mental Health Status of Grade 11 ABM Students During The Online Learning Set Up in Davao CityDocument19 pagesThe Mental Health Status of Grade 11 ABM Students During The Online Learning Set Up in Davao CityALYANNA SARMIENTONo ratings yet
- CASE STUDY ON DEHYDRATIONDocument4 pagesCASE STUDY ON DEHYDRATIONDustin Dela CruzNo ratings yet
- Certificate of Readiness To Enter Higher Surgical Training 2021Document5 pagesCertificate of Readiness To Enter Higher Surgical Training 2021mNo ratings yet
- IELTSFever Academic IELTS Reading Test 163 With Answers - IELTS FeverDocument14 pagesIELTSFever Academic IELTS Reading Test 163 With Answers - IELTS FeverKamalNo ratings yet
- TM 15Document8 pagesTM 15Alfi LafitNo ratings yet
- Anatomy Physiology and Disease Foundations For The Health Professions 1st Edition Roiger Solutions Manual Full Chapter PDFDocument58 pagesAnatomy Physiology and Disease Foundations For The Health Professions 1st Edition Roiger Solutions Manual Full Chapter PDFrelatermotifef4oq100% (10)
- The Outsiders Complete VocabularyDocument4 pagesThe Outsiders Complete VocabularyOsman HuseynliNo ratings yet
- Dr. Warren Morgan's 100-Day Plan For CMSDDocument15 pagesDr. Warren Morgan's 100-Day Plan For CMSDWKYC.comNo ratings yet
- Republic of The Philippines Province of Surigao Del Sur Municipality of HinatuanDocument13 pagesRepublic of The Philippines Province of Surigao Del Sur Municipality of HinatuanGLORIFE RIVERALNo ratings yet
- Situation of Drugs Use Among IDUsDocument52 pagesSituation of Drugs Use Among IDUsSuresh DhunganaNo ratings yet
- PSORIASISDocument9 pagesPSORIASISDianne BernardoNo ratings yet