Professional Documents
Culture Documents
Blood - BLD 2022 018896 Main
Uploaded by
Rana RaedOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Blood - BLD 2022 018896 Main
Uploaded by
Rana RaedCopyright:
Available Formats
Letters to Blood
TO THE EDITOR:
Validation of the Molecular International Prognostic
Scoring System in patients with myelodysplastic
syndromes
Tariq Kewan,1,2, * Waled Bahaj,1, * Arda Durmaz,1, 3 Mai Aly,1,4 Olisaemeka D. Ogbue,1 Hetty E. Carraway,1 Mikkael A. Sekeres,5
Downloaded from http://ashpublications.org/blood/article-pdf/141/14/1768/2042286/blood_bld-2022-018896-main.pdf by Omar Fahmy on 07 April 2023
Valeria Visconte,1 Carmelo Gurnari,1,6, † and Jaroslaw P. Maciejewski1,†
1
Department of Translational Hematology and Oncology Research, Taussig Cancer Institute, Cleveland Clinic, Cleveland, OH; 2 Department of Hematology and
Oncology, Yale University, New Haven, CT; 3 Systems Biology and Bioinformatics Department, School of Medicine, Case Western Reserve University,
Cleveland, OH; 4 Faculty of Medicine, Assiut University, Assiut, Egypt; 5 Department of Hematology and Oncology, University of Miami, Miami, FL; and
6
Department of Biomedicine and Prevention, University of Rome Tor Vergata, Rome, Italy
Myelodysplastic syndrome (MDS) represents a heterogeneous very-high-risk (15% vs 17%) categories (supplemental
group of disorders encompassing a wide range of pathologi- Figure 1A). MDS-EB1/2 cases were enriched among high-risk
cally distinct subtypes associated with different outcomes. Until (28%, 60/214) and very-high-risk (42%, 81/193) IPSS-M groups
recently, clinical and cytogenetic features have dominated the (supplemental Figure 1B, upper panel). Bone marrow blasts
pathological classification and the prognostication of MDS.1-3 percentage followed an incremental pattern from very-low-risk
The wide use of next-generation sequencing and subsequent to very-high-risk subgroups (supplemental Figure 1B, lower
molecular studies have examined the impact of different panel). However, 60% (770/1281) of the patients were treated
genetic alterations on the pathogenetic derivation, diagnostic during the disease course with hypomethylating agents (HMA),
assignment, and disease prognosis.4-9 The latest contribution to allogeneic hematopoietic stem cell transplantation (HSCT), or
the task of adopting molecular features into the clinical prog- lenalidomide (supplemental Figure 1C). Among the patients in
nostic scheme is represented by the Molecular International the low-risk subgroup (n = 336), 38% were treated with HMA at
Prognostic Scoring System (IPSS-M), a product of the Interna- one point of their disease (usually at progression), 16% were
tional Working Group for Prognosis in MDS (IWG-PM).10 Here, treated with lenalidomide, and 14% underwent allogeneic
we took advantage of a large cohort of patients with MDS (n = HSCT. Overall, 59% of the patients treated with HMA (n = 624)
1281, supplemental Methods, available on the Blood website) were assigned to moderate-high-risk, high-risk, or very-high-risk
to validate the novel IPSS-M and to compare the score with the groups. To that end, disease-modifying treatment included
well-established revised IPSS (IPSS-R). To present our clinical HMA, lenalidomide, and allogeneic HSCT similar to what was
experience, we used a cohort of treated and untreated patients reported in the original IWG cohort.10
with MDS. Informed consent was obtained according to the
protocols approved by the institutional review board of the Our higher-risk groups (high and very high, n = 407) were
Cleveland Clinic Foundation and in accordance with the ethical enriched in cases harboring complex karyotype (75%), TP53MT
principles set forth by the Declaration of Helsinki. (75%), RUNX1MT (64%), and NRASMT (65%), and lower-risk
groups showed higher frequencies of normal karyotype (59%,
Overall, MDS–single-lineage dysplasia (SLD) and MDS– 367/620), SF3B1MT (61%, 92/151), and JAK2MT (67%, 66/98)
multilineage dysplasia (MLD) were the most common World (supplemental Figure 1D). Nearly all carriers of biallelic TP53MT
Health Organization 2016 subtypes (477/1281, 37%), whereas (96%, 55/57) were assigned to the very-high-risk group, similar
MDS–excess blasts 1/2 (EB1/2) represented 20% (253/1281) of to the original cohort (91%) (supplemental Figure 2).
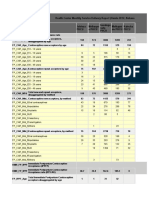
the cohort. The median age was 70 years (interquartile range: Overall, IPSS-M resulted in restratification of 579 (46%) patients
62-77), and 58% (740/1281) of patients were male (Figure 1A). in our cohort (Figure 1B). Of these, 70% were upstaged and
Somatic mutations along with karyotypic abnormalities were 30% were downstaged, paralleling the results of the IWG-PM
similar to the ones analyzed in the IWG-PM cohort. As study (Figure 1A), in which 46% of the cases were restratified.
expected, our cohort did not significantly vary from the IWG-PM The highest rate of restaging was among patients originally
cohort, but we had a higher percentage of treated patients assigned to high-risk IPSS-R (59% [109/186] vs 62% in the
(60% vs 30% in the IWG-PM cohort).10 According to IPSS-R, original cohort). Remarkably, 85% (159/188) of restratified low-
cases (n = 1281) were assigned to very-low-risk (20%, 261), risk IPSS-R patients were upstaged to higher-risk groups per
low-risk (34%, 439), intermediate-risk (17%, 222), high-risk (15%, IPSS-M (Figure 1C).
186), and very-high-risk (14%, 173) categories. When applying
IPSS-M algorithm to our cohort vs the IWG-PM, patients With a median follow-up time of 2.4 years, the 3-year overall
were restratified at similar rates: very-low-risk (14% vs 14%), survival (OS) rate was 51% (95% confidence interval [CI]: 47.6-
low-risk (30% vs 33%), moderate-low-risk (13% vs 11%), 53.8). The 3-year leukemia-free survival (LFS) and progression-
moderate-high-risk (12% vs 11%), high-risk (16% vs 14%), and free survival (PFS) rates were 47% (95% CI: 44-50) and 65%
1768 6 APRIL 2023 | VOLUME 141, NUMBER 14
A
CC IWG-PM J-MDS
Cohort
N=1281 N=2957 N=754
Age in years 70 (60,77) 72 (63,78) 71 (64,78)
Male sex 740 (58%) 1776 (66%) 539 (71%)
Marrow blast % 2 (1,4) 3 (1,6) 5 (1,10)
Hb median (IQR), g/dl 10 (8,11) 10 (8,11) 8 (7,10)
Plt median (IQR), x109/l 98 (45,215) 130 (69,236) 81 (41,146)
IPSS-R risk category
Very Low 261 (20%) 489 (17%) 48 (6%)
Low 439 (34%) 1078 (36%) 161 (22%)
Intermediate 222 (17%) 562 (19%) 160 (22%)
High 186 (15%) 355 (12%) 144 (20%)
Very High 173 (14%) 269 (9%) 223 (30%)
Downloaded from http://ashpublications.org/blood/article-pdf/141/14/1768/2042286/blood_bld-2022-018896-main.pdf by Omar Fahmy on 07 April 2023
Missing 0 (0%) 204 (7%) 0
IPSS-M risk category&
Very Low 178 (14%) 381 (14%) 43 (6%)
Low 384 (30%) 889 (33%) 136 (18%)
Moderate Low 164 (13%) 302 (11%) 80 (11%)
Moderate High 152 (12%) 281 (11%) 78 (10%)
High 214 (16%) 379 (14%) 145 (19%)
Very High 193 (15%) 469 (17%) 272 (36%)
Re-stratification$ 579 (45%) 1232 (46%) 306 (42%)
Up-staged 404 (32%) 911 (34%) -
Down-staged 175 (14%) 312 (12%) -
WHO subtype
MDS-EB1/2 253 (20%) 887 (31%) 415 (55%)
MDS-SLD/MLD 477 (37%) 921 (32%) 246 (33%)
MDS-RS-SLD/MLD 121 (9%) 461 (16%) 37 (4.9%)
MDS-del5q 37 (3%) 142 (4.9%) 9 (1.2%)
MDS-U 29 (2%) 85 (3%) 19 (2.5%)
CMML 137 (11%) 272 (9.5%) 14 (1.9%)
MDS/MPN-RS-T 5 (0.4%) 42 (1.5%) 4 (0.5%)
MDS/MPN-U 190 (15%) 51 (1.8%) 10 (1.3%)
Other 0 (0%) 10 (0.3%) 0 (0%)
Missing 32 (2%) 86 (3%) 0 (0%)
Treated patient# 770 (60%) 894 (30%) 232 (31%)
&: The denominator for the IPSS-M categories for IWG-PM cohort is 2701 patients. $: The denominator for the re-stratified
IWG-PM cohort is 2678 patients. #: Treatment includes hypomethylating agents, lenalidomide, allogeneic hematopoietic stem
cell transplant and chemotherapy.
B C
IPSSM Downstaged
60 Upstaged
Very Low 143 29 2 0 0
Percent (%)
Low 100 251 32 1 0
40
Moderate Low 8 81 64 11 0
Moderate High 10 43 48 46 5 20
High 0 32 56 77 49
0
Very High 0 3 20 51 119
te
h
w
h
ig
ig
Lo
Lo
ia
H
ed
ry
IPSSR
Very Low
Low
Intermediate
High
Very High
y
m
r
Ve
Ve
er
t
In
IPSSR
Figure 1. Baseline characteristics of the validation cohort. (A) Characteristics of the validation cohort as compared with the original and the validation cohorts of the IPSS-M
study. (B) Cross heat map for distribution of patients with MDS according to the IPSS-R (x-axis) and the IPSS-M (y-axis) scores. (C) Bar histogram shows the total percentage of
patients restratified (upstaged or downstaged) according to the IPSS-M. CC, Cleveland Clinic cohort; CMML, chronic myelomonocytic leukemia; EB, MDS with excess blast; Hb,
hemoglobin; IQR, interquartile range; IWG-M, International Working Group for the Prognosis of MDS Cohort; J-MDS, Japanese validation cohort; MLD, multilineage dysplasia;
MPN, myeloproliferative neoplasm; Plt, platelet; RS-T, ring sideroblast-thrombocytosis; SLD, single lineage dysplasia; U, unspecified; WHO, World Health Organization.
LETTERS TO BLOOD 6 APRIL 2023 | VOLUME 141, NUMBER 14 1769
A OS LFS PFS
1.00
0.75
Probability
0.50
0.25
0.00
0 50 100 150 0 50 100 150 0 50 100 150
Time (months) Time (months) Time (months)
No. at risk
VL 150 71 38 21 150 69 37 20 149 65 36 20
L 373 161 71 17 371 153 69 15 368 146 64 14
ML 159 47 20 4 159 47 20 4 158 43 16 3
MH 147 51 22 7 147 48 20 7 146 42 18 7
Downloaded from http://ashpublications.org/blood/article-pdf/141/14/1768/2042286/blood_bld-2022-018896-main.pdf by Omar Fahmy on 07 April 2023
H 207 36 14 5 207 30 11 4 204 26 10 4
VH 181 25 9 3 181 17 6 1 178 13 3 1
B LFS OS PFS
1.0
0.9
Concordance
0.8
0.7
0.6
0.5
Full F M ≥60 <60 Yes No Full F M ≥60 <60 Yes No Full F M ≥60 <60 Yes No
Sex Age (Y) Treatment Sex Age (Y) Treatment Sex Age (Y) Treatment
IPSSM IPSSR
C Cumulative AUC Difference
0.1
0.05
OS
–0.05
–0.1
0.3
0.2
'AUC
LFS
0.1
0.2
0.1
PFS
–0.1
t<10 t<25 t<40 t<55 t<70 t<85 t<100 t<115 t<130
Time (months)
Figure 2. Comparison of the IPSS-M and IPSS-R. (A) Stratification of our cohort based on IPSS-M for OS, LFS, and PFS. (B) Model discrimination measured by the
concordance index via bootstrapping for the IPSS-R (light blue) and the IPSS-M system (red) across all the 3 outcomes end points (LFS, OS, and PFS) for the full cohort, treated
vs untreated patients, males vs females, and ≥60 vs <60 years old. (C) The cumulative AUC differences (ΔAUC) based on IPSS-M between treated and untreated patients
(y-axis) is plotted against the follow-up time intervals of 10 months (x-axis).
1770 6 APRIL 2023 | VOLUME 141, NUMBER 14 LETTERS TO BLOOD
(95% CI: 61-68), respectively (supplemental Table 2). Both IPSS- within the same risk group was significant, especially for certain
M and IPSS-R risk scores showed significant differences in all infrequent but impactful molecular alterations. Remarkably, in
outcomes (supplemental Table 1, Figure 2A, and supplemental our study upstaging was registered mainly in the low-risk IPSS-R
Figure 3). Since IPSS-M aims at improving the IPSS-R with the group, which is a cohort of clinical interest that needs long-term
incorporation of molecular features, we also analyzed differ- follow-up to monitor for AML transformation.
ences in all outcomes in patients originally assigned to the same
IPSS-R group. We noticed meaningful differences in patients Our comprehensive validation could not find significant differ-
assigned to very-low-risk, low-risk, and intermediate-risk groups ences between IPSS-R and IPSS-M when calculating C-indices
(supplemental Figure 4). Performing reverse analysis, IPSS-R did or time-dependent ROC for clinical outcomes. The significant
not significantly restratify patients within the same IPSS-M added prognostic value of IPSS-M in the original study10 was
subgroups in all clinical end points except for LFS in the very- likely a result of the substantial fraction (two-thirds) of untreated
high-risk group and PFS in the IPSS-M high-risk group patients included, which might not accurately represent an
(supplemental Figure 5). actual clinical practice of more treated patients (62% in our
cohort). It is unlikely that a significant proportion of low-risk
Downloaded from http://ashpublications.org/blood/article-pdf/141/14/1768/2042286/blood_bld-2022-018896-main.pdf by Omar Fahmy on 07 April 2023
To quantify the prognostic power of IPSS-M and IPSS-R, we patients does not eventually progress, and under current
used Harrell C-index bootstrapping on OS, LFS, and PFS practice standards they will receive disease-modifying therapy.
(Figure 2B). IPSS-R and IPSS-M showed similar C-indices, This is in contrast to historical cohorts in which treatment
regardless of treatment in our cohort. The C-indices of IPSS-M options were limited.1,2 The information on patients who never
for LFS (0.73 vs 0.75) and OS (0.69 vs 0.74) for all patients in received treatment is useful to assess the need for treatment
our cohort vs the IWG-PM cohort were comparable. In terms of but relatively less helpful in terms of real prognosis under cur-
LFS and OS, we noticed 2.0- and 2.8-point increases, respec- rent clinical standard. This emphasizes the importance of vali-
tively, in the C-index from IPSS-R to IPSS-M, as compared with dating the IPSS-M into independent cohorts to ensure
5-point increase for all clinical end points in the IWG-PM cohort. reproducibility in different clinical settings. In conclusion, MDS
Similar observations were made when the cohort was stratified patients should be stratified based on clinical and molecular
for age (≥60 vs <60) and sex (male vs female) (supplemental features to establish appropriate prognostication and AML
Figure 6). However, a general increase in C-index was progression risk. IPSS-M score provided similar concordance
observed in the untreated group, indicating that both IPSS-M indices to IPSS-R in our well-annotated cohort of patients with
and IPSS-R can provide more precise stratification in a treat- sufficient follow-up time. Particularly, IPSS-M better stratified
ment-naïve scenario. To better quantify the differences of IPSS- low-risk patients assigned within previously similar risk groups.
M performance based on treatment, we used a time-dependent Multiple validation studies can further assess the novel score in
receiver operating characteristic (ROC) analysis and observed a clinical practice and ensure reproducibility for future application
global increase of area under the curve (AUC) for LFS in the in clinical trials.
untreated (never treated) cases as compared with the treated
cases. A time-dependent increase of AUC in PFS was also
noticed. Nevertheless, no difference was observed for OS Acknowledgment
estimation between both groups (Figure 2C). The differences in Carmelo Gurnari is a PhD candidate in Immunology, Molecular Medicine
model fit based on treatment status quantified by the C-index and Applied Biotechnology, University of Rome Tor Vergata,
persisted across relevant clinical stratifications, using sex and Rome, Italy, and this work is submitted in partial fulfillment of the
requirement for a PhD.
age (Figure 2C). Remarkably, no major changes in C-index for
all clinical end points between IPSS-R and IPSS-M were noticed
as compared with the IWG-PM study. Finally, we repeated the
time-dependent ROC analysis to better quantify the differences Authorship
in IPSS-R and IPSS-M and noticed nonsignificant differences Contribution: T.K. and W.B. collected and analyzed clinical and
between the cumulative AUCs for all outcomes (supplemental molecular data, interpreted results, and wrote the manuscript; A.D.
applied statistical methods, analyzed the data, interpreted the results,
Figure 7). and wrote the manuscript; M.A. and O.D.O. collected clinical data and
edited the manuscript; V.V., H.E.C., and M.A.S. edited the manuscript
The IPSS/IPSS-R have been the standard tools for MDS prog- and provided helpful insights to the manuscript; C.G. and J.P.M.
nostication in the last 2 decades.1,2 The new IPSS-M scheme generated and conceived the study, provided invaluable help to the
manuscript preparation, designed figures, and wrote the manuscript;
recently released by the IWG-PM may establish a new standard
and all authors participated in the critical review of the final paper and
to be used in a more rational way by assigning patients to submission.
appropriate treatment modalities and clinical trials based on
genomic features. Aside from the potential usefulness of IPSS-
Conflict-of-interest disclosure: The authors declare no competing
M, a meticulous validation in diverse clinical scenarios is financial interests.
necessary to assure validity, facilitating its wide adoption in
clinical practice. When IPSS-R is used as a benchmark, IPSS-M ORCID profiles: T.K., 0000-0003-4651-5125; A.D., 0000-0001-8394-
algorithm in the original study improves the accuracy of the 600X; M.A., 0000-0002-3926-6856; H.E.C., 0000-0001-5241-3614;
prediction (C-index) of 5 points for all considered outcomes. C.G., 0000-0001-6829-5544.
However, in our cohort both IPSS-R and IPSS-M showed a
Correspondence: Jaroslaw P. Maciejewski, Department of Translational
similar C-index at all end points. Despite a persisting impact of
Hematology and Oncology Research, Taussig Cancer Institute, 9620
clinical features on prognosis,2,11 our findings show that the Carnegie Ave, N Building, Building NE6-250, Cleveland, OH 44106;
ability of IPSS-M to further discriminate outcomes of patients email: maciejj@ccf.org.
LETTERS TO BLOOD 6 APRIL 2023 | VOLUME 141, NUMBER 14 1771
5. Haferlach T, Nagata Y, Grossmann V, et al. Landscape of genetic lesions
Footnotes in 944 patients with myelodysplastic syndromes. Leukemia. 2014;28(2):
Submitted 28 October 2022; accepted 17 January 2023; prepublished 241-247.
online on Blood First Edition 30 January 2023.
6. Bejar R, Stevenson K, Abdel-Wahab O, et al. Clinical effect of point
*T.K. and W.B. contributed equally to the work. mutations in myelodysplastic syndromes. N Engl J Med. 2011;364(26):
2496-2506.
†C.G. and J.P.M. contributed equally to the work. 7. Cazzola M. Myelodysplastic Syndromes. N Engl J Med. 2020;383(14):
1358-1374.
Requests for additional information not provided in the main text or
supplementary material should be sent to maciejj@ccf.org. 8. Nagata Y, Makishima H, Kerr CM, et al. Invariant patterns of clonal
succession determine specific clinical features of myelodysplastic
The online version of this article contains a data supplement. syndromes. Nat Commun. 2019;10(1):5386.
9. Makishima H, Yoshizato T, Yoshida K, et al. Dynamics of clonal evolution
REFERENCES in myelodysplastic syndromes. Nat Genet. 2017;49(2):204-212.
Downloaded from http://ashpublications.org/blood/article-pdf/141/14/1768/2042286/blood_bld-2022-018896-main.pdf by Omar Fahmy on 07 April 2023
1. Greenberg P, Cox C, LeBeau MM, et al. International scoring system for
evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89(6): 10. Bernard E, Tuechler H, Greenberg PL, et al. Molecular International
2079-2088. Prognostic Scoring System for myelodysplastic syndromes. NEJM
Evidence. 2022;1(7):EVIDoa2200008.
2. Greenberg PL, Tuechler H, Schanz J, et al. Revised international
prognostic scoring system for myelodysplastic syndromes. Blood. 2012; 11. Nazha A, Narkhede M, Radivoyevitch T, et al. Incorporation of molecular
120(12):2454-2465. data into the Revised International Prognostic Scoring System in treated
patients with myelodysplastic syndromes. Leukemia. 2016;30(11):
3. Voso MT, Gurnari C. Have we reached a molecular era in myelodysplastic
2214-2220.
syndromes? Hematology Am Soc Hematol Educ Program. 2021;2021(1):
418-427.
https://doi.org/10.1182/blood.2022018896
4. Nagata Y, Zhao R, Awada H, et al. Machine learning demonstrates that
somatic mutations imprint invariant morphologic features in
myelodysplastic syndromes. Blood. 2020;136(20):2249-2262. © 2023 by The American Society of Hematology
TO THE EDITOR:
Monoclonal gammopathy of
thrombotic/thrombocytopenic significance
Adam J. Kanack,1, * Jordan K. Schaefer,2, * Meera Sridharan,3, * Noah P. Splinter,1 Mindy C. Kohlhagen,1 Bandana Singh,1
Silvana B. De Lorenzo,1 Emily E. Mauch,1 Maen A. Hussein,4 Marwan Shaikh,5 Shaji Kumar,3 Renren Wen,6 Demin Wang,6
David Murray,1 and Anand Padmanabhan1
1
Department of Laboratory Medicine and Pathology, Mayo Clinic, Rochester, MN; 2 Department of Medicine, University of Michigan, Ann Arbor, MI;
3
Department of Medicine, Mayo Clinic, Rochester, MN; 4 Florida Cancer Specialists, Orlando, FL; 5 Department of Medicine, Mayo Clinic, Jacksonville, FL; and
6
Department of Microbiology and Immunology, Versiti Blood Research Institute and Medical College of Wisconsin, Milwaukee, WI
Anti–platelet factor 4 (PF4) antibodies have a central role in the to be frequently decreased during these hospitalizations
pathophysiology of thrombosis and thrombocytopenia in (<150 × 109/L; Figure 1A). He had a history of thrombosis in the
heparin-induced thrombocytopenia (HIT)1,2 and vaccine- absence of heparin administration, breakthrough thrombosis
induced immune thrombotic thrombocytopenia (VITT).3-7 even while on anticoagulation (apixaban/warfarin), as well
Here, we present the case of a patient with recurrent throm- as adverse reactions to heparin on occasions when it was used,
bosis and thrombocytopenia, secondary to a persistent anti- as noted in supplemental Materials. Investigation for HIT
PF4/polyanion monoclonal antibody due to an underlying revealed positive PF4/polyanion HIT enzyme-linked immuno-
neoplastic condition, which we refer to as monoclonal gam- sorbent assay (ELISA) (1.983 optical density) and serotonin
mopathy of thrombotic/thrombocytopenic significance (MGTS). release assay (SRA) (95% serotonin release).
The implications of these findings for the investigation of
unexplained thrombophilia are discussed. Platelet counts were available for almost a decade prior to
presentation, and nadir counts were above the lower limit of the
A 64-year-old man presented for evaluation of recurrent normal reference range until ~4 years prior to presentation
thrombotic episodes. His medical history included segmental (Figure 1A). Periodic infusions of intravenous immunoglobulin
and subsegmental pulmonary emboli, portal vein thrombosis, were associated with transient increases in platelet counts
non-ST elevation myocardial infarction, splenic infarction, and (supplemental Figure 1). One of the intravenous immunoglob-
ST elevation myocardial infarction (Figure 1A). Extensive ulin infusions was used in the setting of splenic infarction, and
investigations performed did not support a thrombophilia others were administered due to concern for thrombosis in the
diagnosis (supplemental Table 1 and supplemental Materials; setting of worsening thrombocytopenia. Four years prior, he
available on the Blood website). His platelet counts were noted was noted to have an immunoglobulin G (IgG) κ monoclonal
1772 6 APRIL 2023 | VOLUME 141, NUMBER 14 LETTERS TO BLOOD
You might also like
- E Cacy of Emergency Severity Index (ESI) in Early Identi Cation of Patients With Sepsis and Septic Shock at TriageDocument10 pagesE Cacy of Emergency Severity Index (ESI) in Early Identi Cation of Patients With Sepsis and Septic Shock at Triageputujunidtd13No ratings yet
- Letters: Characteristics of Hospitalized Adults With COVID-19 in An Integrated Health Care System in CaliforniaDocument3 pagesLetters: Characteristics of Hospitalized Adults With COVID-19 in An Integrated Health Care System in CaliforniaDr. Asif RahmanNo ratings yet
- Barbuit T TE Blood 2012Document7 pagesBarbuit T TE Blood 2012amara.ablaNo ratings yet
- Lucrare StintificaDocument8 pagesLucrare StintificaAndreiMunteanuNo ratings yet
- v058p00377 PDFDocument6 pagesv058p00377 PDFAnne Ruth OlinNo ratings yet
- Biol Blood Marrow Transplant 2020 26 10 1828-32Document5 pagesBiol Blood Marrow Transplant 2020 26 10 1828-32Fernando SousaNo ratings yet
- FTPDocument5 pagesFTPHaya RihanNo ratings yet
- 345 FullDocument5 pages345 FullNadiah Umniati SyarifahNo ratings yet
- A Retrospective Multicentre Evaluation of The Outcomes and Management of CHDDocument1 pageA Retrospective Multicentre Evaluation of The Outcomes and Management of CHDRoxana Ioana DumitriuNo ratings yet
- Analysis of Several Loci From Genome-Wide Association Studies inDocument4 pagesAnalysis of Several Loci From Genome-Wide Association Studies inunicum78No ratings yet
- S974 Abstract Book ESTRO 2022: Variable N (%)Document1 pageS974 Abstract Book ESTRO 2022: Variable N (%)andresNo ratings yet
- Preoperative Anemia in Colorectal Cancer RelationsDocument12 pagesPreoperative Anemia in Colorectal Cancer RelationsNahlannisa hubbalillahNo ratings yet
- CML PresentationDocument55 pagesCML PresentationИван НегарэNo ratings yet
- Benzi+Cipelli+Et+Al +proof+1 14Document60 pagesBenzi+Cipelli+Et+Al +proof+1 14adan_infowars0% (1)
- Pima Indians Diabetes Database AnalysisDocument15 pagesPima Indians Diabetes Database AnalysispoppyNo ratings yet
- 1989-The Relationship Between Anemia in PregnancyDocument9 pages1989-The Relationship Between Anemia in Pregnancydw21541No ratings yet
- Dark - Field Microscopic Analysis On The Blood of 1,006 Symptomatic Persons After Anti-Covid Mrna Injections From Pfizer/Biontech or ModernaDocument60 pagesDark - Field Microscopic Analysis On The Blood of 1,006 Symptomatic Persons After Anti-Covid Mrna Injections From Pfizer/Biontech or Modernasum wunNo ratings yet
- Jurnal 4Document11 pagesJurnal 4Kholifatu UlfaNo ratings yet
- Correos Electrónicos jgc-16-12-880Document5 pagesCorreos Electrónicos jgc-16-12-880G RamirezNo ratings yet
- Pathophysiology of COVID-19: Why Children Fare Better Than Adults?Document10 pagesPathophysiology of COVID-19: Why Children Fare Better Than Adults?dilekNo ratings yet
- 2022 - Effect of Polymerised Type I Collagen On Hyperinflammation of AdultDocument8 pages2022 - Effect of Polymerised Type I Collagen On Hyperinflammation of AdultSaid UrbinaNo ratings yet
- Dark - Field Microscopic Analysis On The Blood of 1,006 Symptomatic Persons After Anti-COVID mRNA Injections From Pfizer/BioNtech or ModernaDocument60 pagesDark - Field Microscopic Analysis On The Blood of 1,006 Symptomatic Persons After Anti-COVID mRNA Injections From Pfizer/BioNtech or ModernaJim Hoft100% (2)
- Rituximab For Severe Membranous Nephropathy: A 6-Month Trial With Extended Follow-UpDocument11 pagesRituximab For Severe Membranous Nephropathy: A 6-Month Trial With Extended Follow-UpNarinder SharmaNo ratings yet
- Stroke Among Cancer Patients: ArticleDocument8 pagesStroke Among Cancer Patients: Articlevinit sharmaNo ratings yet
- Clinical Presentation and Outcome in Diabetic Foot Cases: A Prospective Study in A Tertiary Care Teaching Hospital of Uttarakhand, IndiaDocument4 pagesClinical Presentation and Outcome in Diabetic Foot Cases: A Prospective Study in A Tertiary Care Teaching Hospital of Uttarakhand, IndiaNaily Nuzulur RohmahNo ratings yet
- 1 s2.0 S0006497121006340 MainDocument13 pages1 s2.0 S0006497121006340 Mainresi silviaNo ratings yet
- 1382-Article Text-5022-1-10-20180430 PDFDocument4 pages1382-Article Text-5022-1-10-20180430 PDFFadillNo ratings yet
- Validation of The Electronic Version of The Hester Davis ScaleDocument1 pageValidation of The Electronic Version of The Hester Davis ScaleAMIANo ratings yet
- Dr. Atif Sher ASCVD CardioConDocument21 pagesDr. Atif Sher ASCVD CardioConwali ahmedNo ratings yet
- BMJ m3249 FullDocument15 pagesBMJ m3249 Fullvuongquynh290900No ratings yet
- Kaya 2012Document6 pagesKaya 2012didingNo ratings yet
- 576 Friday, 15 June 2018 Scientific AbstractsDocument2 pages576 Friday, 15 June 2018 Scientific AbstractsDanna Carvajal GaitanNo ratings yet
- THR-fast Starters, Slow Starters - Late DippersDocument12 pagesTHR-fast Starters, Slow Starters - Late DippersMohan DesaiNo ratings yet
- Genetic Association Between IL-21 Polymorphisms and Cryptorchidism in A Chinese Han PopulationDocument4 pagesGenetic Association Between IL-21 Polymorphisms and Cryptorchidism in A Chinese Han PopulationHugo AlvesNo ratings yet
- Clinico-Etiological Spectrum of Pancytopenia in Hospitalized ChildrenDocument4 pagesClinico-Etiological Spectrum of Pancytopenia in Hospitalized ChildrenNurul Huda KowitaNo ratings yet
- In Silico/in Vivo Analysis of High-RiskDocument22 pagesIn Silico/in Vivo Analysis of High-RiskDyahNo ratings yet
- The Influence of Body Mass Index On The Long-Term Survival of Patients With Renal Cell Carcinoma After Tumour NephrectomyDocument6 pagesThe Influence of Body Mass Index On The Long-Term Survival of Patients With Renal Cell Carcinoma After Tumour NephrectomyRania AnisNo ratings yet
- IntroduccionTFGJUL 2024Document5 pagesIntroduccionTFGJUL 2024Julia Urquiza LandaluceNo ratings yet
- THALASSEMIADocument5 pagesTHALASSEMIADiego Ferney Guerrero GuerreroNo ratings yet
- Paper Comparativa Sobrevida de PV, TE y MFP ComplementoDocument4 pagesPaper Comparativa Sobrevida de PV, TE y MFP ComplementoDani HaindlNo ratings yet
- Huang 2022 LD 220195 1661882443.12746Document4 pagesHuang 2022 LD 220195 1661882443.12746isrealvirgin763No ratings yet
- A New Classification To Identify Risk of ReintubationDocument3 pagesA New Classification To Identify Risk of ReintubationvillaboyNo ratings yet
- Comparison of qSOFA and SOFA scores for predicting mortality in sepsis patientsDocument4 pagesComparison of qSOFA and SOFA scores for predicting mortality in sepsis patientsBapak Sunaryo SPBUNo ratings yet
- Defining Community Acquired Pneumonia Severity On Presentation To Hospital: An International Derivation and Validation StudyDocument6 pagesDefining Community Acquired Pneumonia Severity On Presentation To Hospital: An International Derivation and Validation StudyAlirio BastidasNo ratings yet
- Pharmaceutical Sciences: Recent Advances and Treatments of Childhood Nephrotic SyndromeDocument3 pagesPharmaceutical Sciences: Recent Advances and Treatments of Childhood Nephrotic SyndromeiajpsNo ratings yet
- A Study of Haematological Profile of Malaria in A Tertiary Care Centre of Western Uttar Pradesh, IndiaDocument5 pagesA Study of Haematological Profile of Malaria in A Tertiary Care Centre of Western Uttar Pradesh, IndiaramperoughNo ratings yet
- Gaptg 6Document3 pagesGaptg 6DIKE NOVELLA -No ratings yet
- SAH 2Document11 pagesSAH 2mutia nur rahmiNo ratings yet
- High antibody response to mRNA COVID-19 vaccine in dialysis patientsDocument3 pagesHigh antibody response to mRNA COVID-19 vaccine in dialysis patientsBala MuraliNo ratings yet
- The Burden of Hydrocephalus Treatment Devices - Survey Perspectives From 562 PatientsDocument11 pagesThe Burden of Hydrocephalus Treatment Devices - Survey Perspectives From 562 PatientsIan ZelkoNo ratings yet
- StrokeDocument12 pagesStrokeM TabishNo ratings yet
- JNMA-61-258-115Document4 pagesJNMA-61-258-115Nicolás Mosso F.No ratings yet
- Doh Hiv Art RegistryDocument7 pagesDoh Hiv Art Registryrommel mendoza100% (1)
- IJSRMDocument11 pagesIJSRMjaya kumarNo ratings yet
- Scientific Letter: Archivos de Bronconeumología 58 (2022) 520-522Document3 pagesScientific Letter: Archivos de Bronconeumología 58 (2022) 520-522johannaNo ratings yet
- Journal Pone 0106203 PDFDocument7 pagesJournal Pone 0106203 PDFAnonymous 4vrma12QgbNo ratings yet
- Genetic DiagnosaDocument6 pagesGenetic DiagnosaIfany oschaliaNo ratings yet
- Clinical Significance of Tacrolimus Intra Patient Variability On Kidney Transplant Outcomes According To Pre Transplant Immunological RiskDocument9 pagesClinical Significance of Tacrolimus Intra Patient Variability On Kidney Transplant Outcomes According To Pre Transplant Immunological RiskBhanu KumarNo ratings yet
- Immunophenotyping For HematologistDocument139 pagesImmunophenotyping For HematologistMantavya PurohitNo ratings yet
- Evaluation of Thrombin Activatable Fibrinolysis Inhibitor (TAFI) in Patients with β-ThalassemiaDocument6 pagesEvaluation of Thrombin Activatable Fibrinolysis Inhibitor (TAFI) in Patients with β-ThalassemiaRana RaedNo ratings yet
- Kanavaki 2009Document5 pagesKanavaki 2009Rana RaedNo ratings yet
- PDF 1202Document18 pagesPDF 1202Rana RaedNo ratings yet
- 3 Dfa 6 DC 7 Ec 55 F 9 CCDocument7 pages3 Dfa 6 DC 7 Ec 55 F 9 CCRana RaedNo ratings yet
- MedJBabylon164340-534105 145010Document6 pagesMedJBabylon164340-534105 145010Rana RaedNo ratings yet
- Course of FCDocument2 pagesCourse of FCRana RaedNo ratings yet
- Acute Leukemia The Scientist's Perspective and ChallengeDocument438 pagesAcute Leukemia The Scientist's Perspective and ChallengemedskyqqNo ratings yet
- Course of FCDocument2 pagesCourse of FCRana RaedNo ratings yet
- Sensory Integration Therapy and Auditory Integration TrainingDocument10 pagesSensory Integration Therapy and Auditory Integration TrainingMuskaan KhannaNo ratings yet
- Jurnal NilamDocument7 pagesJurnal NilamSofia ChaeroniNo ratings yet
- Adult AdhdDocument10 pagesAdult AdhdJose SilvaNo ratings yet
- CPCL Instrumentation 8 May PaperDocument37 pagesCPCL Instrumentation 8 May PaperNitish KumarNo ratings yet
- Collaborative Working RelationshipsDocument15 pagesCollaborative Working RelationshipsMadhabi MondalNo ratings yet
- Antony and Sony (2019)Document25 pagesAntony and Sony (2019)Daniele dos Reis PereiraNo ratings yet
- Hilti Firestop Submittal - Balamand UniversityDocument32 pagesHilti Firestop Submittal - Balamand UniversitybasbousrNo ratings yet
- Sprayspheres SC (SC BL Ve 1103 S)Document3 pagesSprayspheres SC (SC BL Ve 1103 S)asetaldehit yıldırımNo ratings yet
- Return To Work After Work Related Injury in The Construction Sector: A Scoping ReviewDocument21 pagesReturn To Work After Work Related Injury in The Construction Sector: A Scoping ReviewchizitarankwoparaNo ratings yet
- 6month Report NewDocument123 pages6month Report NewEmag YonisNo ratings yet
- Tracking Tool 2018Document149 pagesTracking Tool 2018Fred TNo ratings yet
- The Mental Status Exam (MSE)Document5 pagesThe Mental Status Exam (MSE)Huma IshtiaqNo ratings yet
- Natural Health: SolutionsDocument8 pagesNatural Health: SolutionsLakeshore PublicationNo ratings yet
- Kudori Therapy - Updated 9th Dec17Document32 pagesKudori Therapy - Updated 9th Dec17Manickavasagam RengarajuNo ratings yet
- Pengaruh Keselamatan Dan Kesehatan Kerja KaryawanDocument8 pagesPengaruh Keselamatan Dan Kesehatan Kerja KaryawanJernihNo ratings yet
- Optometry and Vision Science Handbook - Department of Optometry (PDFDrive)Document48 pagesOptometry and Vision Science Handbook - Department of Optometry (PDFDrive)هدهد رحاب100% (1)
- HSE L151 - 2014 - Explosives Regulations 2014 Guidance On Regulations - Security ProvisionsDocument68 pagesHSE L151 - 2014 - Explosives Regulations 2014 Guidance On Regulations - Security ProvisionsKris WilochNo ratings yet
- 10 AmperDocument54 pages10 AmperPy LabNo ratings yet
- B. Choose The Word That Has Different Stress From Others.: Test 6 Part I: Phonetics: (2Pt)Document3 pagesB. Choose The Word That Has Different Stress From Others.: Test 6 Part I: Phonetics: (2Pt)Ngọc VươngNo ratings yet
- 2019 Clinical Performance of Direct Anterior Composite Restorations A Systematic Literature Review and Critical AppraisalDocument19 pages2019 Clinical Performance of Direct Anterior Composite Restorations A Systematic Literature Review and Critical Appraisalmaroun ghalebNo ratings yet
- Saudi License Exam - SLE (DENTAL Test Papers) Set-1Document108 pagesSaudi License Exam - SLE (DENTAL Test Papers) Set-1Adeel Ahmad86% (22)
- LESSON: The Discipline of Counseling ObjectivesDocument6 pagesLESSON: The Discipline of Counseling ObjectivesREYMARK PERALTANo ratings yet
- RENR MOCK EXAMINATION 2 2018. Question SheetDocument24 pagesRENR MOCK EXAMINATION 2 2018. Question SheetSasha UterNo ratings yet
- E4 SubtypesDocument26 pagesE4 SubtypesJuliaNo ratings yet
- Bed Spray Material Safety Data SheetDocument4 pagesBed Spray Material Safety Data SheetKikuta LeeNo ratings yet
- Chain SawsDocument2 pagesChain Sawsابو محمد عليNo ratings yet
- Kahel: Dishwashing Liquid From Orange PeelingsDocument16 pagesKahel: Dishwashing Liquid From Orange PeelingsRussel AloceljaNo ratings yet
- Petroleum Engineering Handbook For The Practicing Engineer Vol. 1 by M. A.Document5 pagesPetroleum Engineering Handbook For The Practicing Engineer Vol. 1 by M. A.ashishNo ratings yet
- Roughdraft AllenDocument5 pagesRoughdraft Allenapi-318349384No ratings yet
- Advanced Cardiovascular Life Support ACLS Emergency Crash Cart CardsDocument1 pageAdvanced Cardiovascular Life Support ACLS Emergency Crash Cart CardsMenGuitarNo ratings yet