Professional Documents
Culture Documents
Ventricular Pressure-Volume Relationship Preload, Afterload, Stroke Volume, Wall Stress & Frank-Starling's Law - ECG & ECHO
Uploaded by
Alagusundaram LakshminarayananOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ventricular Pressure-Volume Relationship Preload, Afterload, Stroke Volume, Wall Stress & Frank-Starling's Law - ECG & ECHO
Uploaded by
Alagusundaram LakshminarayananCopyright:
Available Formats
ECG ECHO Sign in Sign up
Back to Book/course Clinical Echocardiography Left ventricular systolic funct…
Clinical SECTION 4, CHAPTER 3
Echocardiography
Ventricular Pressure-
Introduction to echocardio… 12 Chapters
Volume Relationship:
Preload, Afterload,
Principles of hemodynamics 5 Chapters
Stroke Volume, Wall
The echocardiographic exa… 3 Chapters
Stress & Frank-
Starling’s law
Left ventricular systolic fun… 11 Chapters
Chapter contents [ Show ]
Left Ventricular Function
Ventricular Pressure-Volume
Myocardial Mechanics: Structure an…
Relationship
Ventricular Pressure-Volume Relatio…
Left ventricular pressure-volume relationship
Assessing left ventricular systolic fu… can be described by a loop diagram with volume
depicted on the x-axis and left ventricular
Left ventricular mass and volume (si… pressure on the y-axis. If left ventricular
pressure and volume are measured continuously
Ejection fraction (EF): Physiology, M… during a single cardiac cycle, the loop diagram
shown in Figure 1 is obtained.
Fractional shortening for estimation …
Strain, strain rate and speckle tracki…
Left Ventricular Segments for Echoc…
The Coronary Arteries
Regional Myocardial Contractile Fun…
Left ventricular diastolic fun… 3 Chapters
Figure 1. Left ventricular pressure-volume
relationship during a single cardiac cycle.
In Figure 1 we begin in diastole, when the mitral
valve opens. When the mitral valve opens, blood
flows into the left ventricle. This results in a
rapid increase in left ventricular volume, but only
a small increase in left ventricular pressure. This
is explained by the fact that the left ventricle is
capable of relaxing and expanding rapidly during
diastole. The term complianceis used to
describe the ability of the left ventricle to relax
during diastole. Compliance is fundamental to
diastolic function. High compliance is desireable
and means that the ventricle is capable of filling
rapidly while operating at low end-diastolic
pressure.
EDV (End Diastolic Volume) denotes the
volume in the left ventricle, just before
contraction commences. Left ventricular
pressure increases when the contracting starts,
and when left ventricular pressure exceeds left
atrial pressure, the mitral valve closes. Upon
closing of the mitral valve, left ventricular
pressure increases rapidly while both the aortic
valve and the mitral valve are closed. This phase
is called isovolumetric contraction (IVC;
Figures 1 and 2).
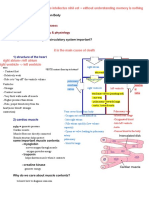
Relationshipbetweenpressure,volumeandECG
Systole Diastole
ejection filling
IVR
ECG
Aorticvalve
;closes
120+ Aorticvalve
opens
Pressure(mmHg)
80 Aorticpressure
40 Mitralvalve Mitralvalve
closes opens Leftventricularpressure
Leftatrialpressure
-EDV Leftventricular
130+ volume
ng
Filli
Eje
90-
Volume
c ti
on
50- ESV
Contraction Relaxation
Filling
Figure 2. Left ventricular pressure-volume
relationship and ECG waveforms during systole
and diastole.
When left ventricular pressure exceeds diastolic
pressure in the aorta, the aortic valve opens and
blood is ejected into the aorta. Left ventricular
volume decreases as the ventricle contracts and
pumps blood into the aorta. After the maximum
pressure is reached, the ventricle relaxes, which
results in diminished left ventricular pressure.
The aortic valve closes when aortic pressure
exceeds left ventricular pressure.
ESV (End Systolic Volume) is defined as left
ventricular volume at the closure of the aortic
valve. Upon aortic valve closure, the ventricle
relaxes and pressure drops rapidly, without any
significant changes in volume. This phase is
referred to as isovolumetric relaxation (IVR;
Figures 1 and 2). When the ventricular pressure
is less than left atrial pressure, the mitral valve
opens and the cycle is repeated.
Stroke volume (SV) and stroke
work (SW)
Stroke volume (SV) is defined as the difference
between ESV and EDV, which is equivalent to the
width of the loop in Figure 1. The area within the
loop is the stroke work (SW), which is
discussed below.
The pressure-volume loop in Figure 1 can be
moved along the black lines called EDPVR and
ESPVR. EDPVR (End-Diastolic Pressure-
Volume Relationship) shows the relationship
between ESV and left ventricular volume. The
EDPVR curve shows that the left ventricle can
withstand large pressure increases but at a
certain threshold, pressure rises rapidly with
further increases in volume. This is explained by
the existence of an upper limit for ventricular
compliance. The greater the left ventricular
compliance, the less steep the slope of the
EDPVR curve, and vice versa.
ESPVR (End-Systolic Pressure-Volume
Relationship) shows how maximum pressure
varies with volume. The smaller the EDV, the
lower the maximum generated pressure, and the
smaller the stroke volume. Thus, low preload
leads to low EDV, which results in lower
generated pressure and ultimately smaller
stroke volume.
Two-dimensional (2D) and three-dimensional
(3D) echocardiography allows for the calculation
of stroke volume. The drawback of stroke
volume as a measure of left ventricular function
is that it ignores the ability of the ventricle to
generate pressure. This is evident from Figure 1,
which demonstrates that stroke volume is the
difference between ESV and EDV, which can be
calculated without considering pressure (the y-
axis). Moreover, stroke volume also ignores the
ability of the ventricle to shorten. These
drawbacks become clear when examining
patients with dilated cardiomyopathy (DCM).
These patients may have normal stroke volumes,
due to their large ventricular volumes, despite
severe impairment of left ventricular function.
The ability to generate pressure can be
calculated by estimating stroke work (SW).
Stroke work (SW)
In physics, work is equivalent to the product of
power (f) and distance (d). The work required to
move an object is the product of the force
needed to move the object and the distance the
object is moved. With regards to the left
ventricle, the object is blood, and the force is the
pressure generated by the left ventricle. Stroke
work is the work performed to move blood from
the ventricle into the aorta.
Stroke work is represented by the area within the
pressure-volume loop in Figure 1. In vivo
measurement of stroke work requires
continuous measurement of ventricular pressure
and volume during the cardiac cycle, which is
not technically feasible. However, stroke work
can be approximated as the product of stroke
volume and mean arterial pressure (MAP). This
does, however, result in an underestimation of
stroke work.
Cardiac work
Cardiac work (CW) is the product of heart rate
(HR) and stroke work (SW):
CW = HR • SW
(SW = SV • MAP)
Frank-Starling's law
(mechanism)
Stroke volume is greater in the supine position,
as compared with an upright position. This is
because venous return increases in the supine
position. More blood flows back to the heart,
leading to increased ventricular filling (EDV). The
left ventricle responds to increased EDV by
automatically increasing stroke volumes. It
follows that the heart can adapt its stroke
volumes to variations in left ventricular filling.
This phenomenon is called Frank-Starling's
mechanism (law).
Figure 3. Frank-Starling's mechanism.
Frank and Starling discovered that an increase in
Left Ventricular End Diastolic Pressure
(LVEDP) leads to stronger contractions and
greater stroke volumes. This mechanism is
independent of neurohumoral stimuli, although
such stimuli can adjust the intensity of the
mechanism. As evident in Figure 3, the Frank-
Starling curve is modified by afterload and
inotropy of the myocardium.
A rather simple cellular mechanism seems to
explain Frank-Starling's mechanism. When
ventricular filling is increased, the myocardial
fibers and their sarcomeres, are stretched. This
results in troponin C becoming more sensitive to
calcium (sensitivity depends on sarcomere
length), which accelerates the interaction
between actin and myosin, and ultimately
produces more force.
The difference between
contractility and contractile
function
There is a discreet difference between
contractility and contractile function.
Contractility describes the intrinsic ability of
the myocardium to contract, regardless of
preload and afterload. Contractility is the ability
of individual muscle fibers to shorten.
Contractility is not studied with
echocardiography.
Contractile function describes the ability of
the myocardium, in a given hemodynamic state
(at certain preload and afterload conditions).
This is synonymous with systolic function and
can be estimated by echocardiography.
Preload
Preload is the force that stretches myocardial
fibers during diastole. Stretching can be
described by end-diastolic pressure, end-
diastolic volume or end-diastolic diameter.
However, neither pressure, volume, nor diameter
is normalized. Therefore, preference should be
given to preload adjusted for the surface area of
the ventricle, which is equivalent to end-
diastolic wall tension (discussed below).
Preload reserve is an important parameter. It
indicates how much reserve there is in preload.
A ventricle with a large preload reserve can
receive a larger volume of blood (i.e increase its
LVDP). In upright position, all healthy individuals
have a large preload reserve, which becomes
useful during physical activity. In the supine
position, however, preload reserve is small. This
is because venous return increases so much in
the supine position, that the ventricle is already
stretched and operates at or close to its reserve.
Afterload
Afterload is the force that the myocardium
generates during systole. Afterload can also be
described in terms of wall tension, which means
that the force is adjusted for surface area.
Afterload depends on the thickness of the
myocardium. Individuals with high blood
pressure (high afterload) often develop a
compensatory hypertrophy, which may
normalize afterload per surface area.
Wall tension
Wall tension is the force applied to the wall of the
ventricle. The force should be adjusted for the
ventricular surface area, resulting in wall tension
per surface area (σ):
σ = (p·r)/2·t
p = transmural pressure; r = ventricular
radius; t = wall thickness.
Transmural pressure (p) is the pressure in the
left ventricle. It can be approximated; this is
done by approximating p to systolic pressure
(measured as conventional blood pressure).
Start learning ECG Start now
You might also like
- Curva de Presion y Volumen Cardiaco CicloDocument5 pagesCurva de Presion y Volumen Cardiaco CicloMauricio P�rez Mac�asNo ratings yet
- CV 2 Heart As A Pump Notes CopyrightDocument7 pagesCV 2 Heart As A Pump Notes Copyrightmaxwell amponsahNo ratings yet
- Fukuta 2008Document11 pagesFukuta 2008redactor 1No ratings yet
- Section VII - Cardiac Pressure TracingsDocument4 pagesSection VII - Cardiac Pressure TracingsFayon JamesNo ratings yet
- K Sembulingam Essentials of Medical Physiology 6th 105 PDFDocument11 pagesK Sembulingam Essentials of Medical Physiology 6th 105 PDFBlerta Deari100% (2)
- Murmur and Cardiac Cycle PDFDocument17 pagesMurmur and Cardiac Cycle PDFAlesisNo ratings yet
- CARDIAC CYCLE New For StudentDocument54 pagesCARDIAC CYCLE New For StudentDavi DzikirianNo ratings yet
- Cardiac EventsDocument3 pagesCardiac Eventshannahangella5949No ratings yet
- Kasus 6 (ADHF Grade II + NSTEMI + HHD + Dislipidemia) - Blok CVS - Tingkat 2 - NRP 1910211099 - REZA RAMADHANSYAHDocument34 pagesKasus 6 (ADHF Grade II + NSTEMI + HHD + Dislipidemia) - Blok CVS - Tingkat 2 - NRP 1910211099 - REZA RAMADHANSYAHReza RamadhansyahNo ratings yet
- w2 Part 1Document30 pagesw2 Part 1farahafiqahNo ratings yet
- Cardiovascular PhysiologyDocument49 pagesCardiovascular PhysiologyAndreea ŞtefănescuNo ratings yet
- 04-The Cardiac Cycle - Wigger's Diagram (J Swanevelder)Document6 pages04-The Cardiac Cycle - Wigger's Diagram (J Swanevelder)Patrick WilliamsNo ratings yet
- CARDIAC CYCLE New For StudentDocument54 pagesCARDIAC CYCLE New For StudentDavi DzikirianNo ratings yet
- Pressure-Volume Relationships in Right Ventricle: by Robert R. Lafontant, B.S., Harold Feinberg, PH.D.Document3 pagesPressure-Volume Relationships in Right Ventricle: by Robert R. Lafontant, B.S., Harold Feinberg, PH.D.Kate udeshiNo ratings yet
- Physiology (Code) - Year 2Document20 pagesPhysiology (Code) - Year 2bgj9cddvxhNo ratings yet
- Cardiac Cycle: Blood Pressure Heartbeat Heart RateDocument6 pagesCardiac Cycle: Blood Pressure Heartbeat Heart RateSUDIPTA SHOWNo ratings yet
- Cardiac Cycle JVPDocument70 pagesCardiac Cycle JVPAstrid PramudyaaNo ratings yet
- Cardiac Cycle - WikipediaDocument13 pagesCardiac Cycle - WikipediaHarshal GaikwadNo ratings yet
- CIE OL Bio Cardiac CycleDocument16 pagesCIE OL Bio Cardiac Cyclevqnygxb8fvNo ratings yet
- Cardiac CycleDocument37 pagesCardiac CycleEltika utariNo ratings yet
- Health Assessment: Cardiac Conduction System DisordersDocument2 pagesHealth Assessment: Cardiac Conduction System DisordersLeigh ProsyneNo ratings yet
- THE Cardiac Cycle: Physiology DepartmentDocument55 pagesTHE Cardiac Cycle: Physiology DepartmentmariacalNo ratings yet
- Cardiac PhysioDocument9 pagesCardiac Physiosakuragi jakeNo ratings yet
- Presentation 5Document5 pagesPresentation 5mahnoorcollection20No ratings yet
- Student ProtocolDocument14 pagesStudent ProtocolLaura Camila Bermeo PeraltaNo ratings yet
- Chapter 18 AHP215Document3 pagesChapter 18 AHP215gielduqueNo ratings yet
- DR Najeeb Cardiac CycleDocument5 pagesDR Najeeb Cardiac Cycleعلي. احمد100% (1)
- ECG & Heart Sounds: Student HandoutDocument7 pagesECG & Heart Sounds: Student HandoutPatrick Joshua PascualNo ratings yet
- AQA A-Level Biology The Cardiac CycleDocument7 pagesAQA A-Level Biology The Cardiac CycleMina BeeNo ratings yet
- ECG & Heart Sounds: Student HandoutDocument7 pagesECG & Heart Sounds: Student HandoutROHITNo ratings yet
- Activity 1 - Circulatory SystemDocument25 pagesActivity 1 - Circulatory Systemisabellamarie.castillo.crsNo ratings yet
- HSCI 103 LAB 2 ECG & Heart Sounds Worksheet - SP 2021Document10 pagesHSCI 103 LAB 2 ECG & Heart Sounds Worksheet - SP 2021MatthewFlecknoeNo ratings yet
- Ecg Heart Sounds Laboratory HandoutDocument7 pagesEcg Heart Sounds Laboratory HandoutShashank SahuNo ratings yet
- LO Dan WO Cardio Week 5Document60 pagesLO Dan WO Cardio Week 5Alan Dwi SetiawanNo ratings yet
- Cardiovascular PhysiologyDocument287 pagesCardiovascular Physiologyarshamboss4No ratings yet
- 10 1016@j Echo 2018 11 011Document19 pages10 1016@j Echo 2018 11 011Jose Ignacio Tarton SisimitNo ratings yet
- Cardiac Cycle & Heart Sounds Flashcards - QuizletDocument11 pagesCardiac Cycle & Heart Sounds Flashcards - QuizletRadijska Postaja KoprivnicaNo ratings yet
- Physiology of The HeartDocument20 pagesPhysiology of The HeartmendozaleannejoyceNo ratings yet
- Physiology (Code) - Year 2Document20 pagesPhysiology (Code) - Year 2bgj9cddvxhNo ratings yet
- Diastole and AnesthesiaDocument16 pagesDiastole and AnesthesiadrsubramanianNo ratings yet
- Cardiovascular SystemDocument50 pagesCardiovascular Systemkintan kamila100% (1)
- Cardiovascular Physiology: Lawrence A. Olatunji ReaderDocument46 pagesCardiovascular Physiology: Lawrence A. Olatunji ReaderMaryam Ogunade0% (1)
- 22cardiac PV Loop Cardiac PhysiologyDocument19 pages22cardiac PV Loop Cardiac PhysiologyJaydave PatelNo ratings yet
- Heart ChambersDocument14 pagesHeart Chambersberniebernie20No ratings yet
- DR Rahimah Zakaria Dept of PhysiologyDocument31 pagesDR Rahimah Zakaria Dept of PhysiologyChokJunHoongNo ratings yet
- Study Guide For Lecture Exam 3. Heart.: Pulmonary CirculationDocument4 pagesStudy Guide For Lecture Exam 3. Heart.: Pulmonary CirculationmakNo ratings yet
- Preload and AfterloadDocument4 pagesPreload and AfterloadNeranga SamaratungeNo ratings yet
- Cardiac Cycle - Atrial Contraction (Phase 1) : A-V Valves Open Semilunar Valves ClosedDocument10 pagesCardiac Cycle - Atrial Contraction (Phase 1) : A-V Valves Open Semilunar Valves ClosedFatima KhanNo ratings yet
- Physiology: Zhao Chun-ling (赵春玲) Email: Phone:18683073667Document62 pagesPhysiology: Zhao Chun-ling (赵春玲) Email: Phone:18683073667Akshay ChaudharyNo ratings yet
- Icu BookDocument1,054 pagesIcu BookqsychoNo ratings yet
- Cardiac Cycle: Himawan WDocument46 pagesCardiac Cycle: Himawan WaprinaNo ratings yet
- Cardiovascular Physiology MCQDocument11 pagesCardiovascular Physiology MCQJessi ObibiNo ratings yet
- The Cardiac Cycle and The Physiologic Basis of Left Ventricular Contraction, Ejection, Relaxation, and FillingDocument13 pagesThe Cardiac Cycle and The Physiologic Basis of Left Ventricular Contraction, Ejection, Relaxation, and FillingFanindya HadamuNo ratings yet
- The 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsFrom EverandThe 12-Lead Electrocardiogram for Nurses and Allied ProfessionalsNo ratings yet
- 01 - Cardiac CycleDocument4 pages01 - Cardiac CycleEhtiram HuseynovNo ratings yet
- Dr. Alurkur's Book On Cardiology - 2Document85 pagesDr. Alurkur's Book On Cardiology - 2Bhattarai ShrinkhalaNo ratings yet
- Kami Export - Cardiovascular System Lecture Outline 1st PeriodDocument16 pagesKami Export - Cardiovascular System Lecture Outline 1st PeriodJada NovakNo ratings yet
- Mechanical Circulatory Support in ST-Elevation Myocardial InfarctionDocument21 pagesMechanical Circulatory Support in ST-Elevation Myocardial InfarctionDiana Marcela Franco SanchezNo ratings yet
- Sample ChapterDocument14 pagesSample ChaptercpfredNo ratings yet
- Gel Polish and Dry Manicure Manual EDITABLEDocument56 pagesGel Polish and Dry Manicure Manual EDITABLECristina Gradinari100% (1)
- KLP 3 - Ebp Telaah Artikel Terapi Musik Klasik Pada Lansia Dengan HipertensiDocument12 pagesKLP 3 - Ebp Telaah Artikel Terapi Musik Klasik Pada Lansia Dengan HipertensiIfah KaharNo ratings yet
- SonoAce R5 Reference Manual P PDFDocument150 pagesSonoAce R5 Reference Manual P PDFNeto Infomab MedNo ratings yet
- The Effect of Hydrotherapy On Blood Pressure of DOIDocument4 pagesThe Effect of Hydrotherapy On Blood Pressure of DOIPhocachinnoNo ratings yet
- Care of Clients With Problems in OxygenationDocument5 pagesCare of Clients With Problems in OxygenationSkyla FiestaNo ratings yet
- Circulatory SystemDocument44 pagesCirculatory SystemAdonai Jireh Dionne BaliteNo ratings yet
- Free Nclex QuestionsDocument161 pagesFree Nclex QuestionspadmaNo ratings yet
- Perloff 2012 Chapter PdaDocument28 pagesPerloff 2012 Chapter PdaMuhammad IrfanNo ratings yet
- 20 Soal Litbing 1 FixDocument7 pages20 Soal Litbing 1 FixRizky AzhariNo ratings yet
- Current Concepts in Adult Criti - Park MD FACS FCCM, Pauline KDocument224 pagesCurrent Concepts in Adult Criti - Park MD FACS FCCM, Pauline KdobiNo ratings yet
- Dysrhythmia Interpretation Modules 1-6 June 2012Document126 pagesDysrhythmia Interpretation Modules 1-6 June 2012Jess Varose100% (3)
- Omssat2008 (1) (1) 1Document253 pagesOmssat2008 (1) (1) 1Ganga Hospital100% (2)
- Cardiac Cycle by Dr. RoomiDocument71 pagesCardiac Cycle by Dr. RoomiMudassar Roomi100% (3)
- Full Test of Neet 2024 Part 2Document26 pagesFull Test of Neet 2024 Part 2bhavyakhandelwal2302100% (1)
- Pulse Contour Cardiac Output Learning Package PDFDocument17 pagesPulse Contour Cardiac Output Learning Package PDFNurse PractitionerNo ratings yet
- Technology Integration Lesson Plan 1Document4 pagesTechnology Integration Lesson Plan 1api-320427440No ratings yet
- 28-31 Cardiovascular ProblemsDocument34 pages28-31 Cardiovascular ProblemsdelarakrishnafaithpNo ratings yet
- Pengangkutan: TransportationDocument22 pagesPengangkutan: TransportationsuhanaNo ratings yet
- Therapy FINAL PDFDocument102 pagesTherapy FINAL PDFManushi HenadeeraNo ratings yet
- Hepatic Vein FlowDocument14 pagesHepatic Vein FlowJORGENo ratings yet
- The Human Heart and Circulatory SystemDocument36 pagesThe Human Heart and Circulatory SystemLindiwe GoweNo ratings yet
- Human Physiology From Cells To Systems 7th Edition Sherwood Test Bank Cells To Systems 7th Edition Sherwood Test BankDocument16 pagesHuman Physiology From Cells To Systems 7th Edition Sherwood Test Bank Cells To Systems 7th Edition Sherwood Test Bankteresamckenzieafvo100% (13)
- ManuscriptDocument8 pagesManuscript킴춘자No ratings yet
- AMBOSS and RX NotesDocument21 pagesAMBOSS and RX NotesBatool Aldaher100% (1)
- On Exam QuestionsDocument302 pagesOn Exam QuestionsMD Luthfy LubisNo ratings yet
- 3-CVS-Valvular Diseases-Prof. Magdy-Student-Final (Compatibility Mode)Document11 pages3-CVS-Valvular Diseases-Prof. Magdy-Student-Final (Compatibility Mode)أميرةNo ratings yet
- Review Article: Management of Cardiac Tamponade After Cardiac SurgeryDocument10 pagesReview Article: Management of Cardiac Tamponade After Cardiac SurgeryJanuar Alfred PoliNo ratings yet
- Chapter 31: Structure and Function of The Cardiovascular and Lymphatic SystemsDocument12 pagesChapter 31: Structure and Function of The Cardiovascular and Lymphatic SystemsMelissa WrightNo ratings yet
- Chapter08 PDFDocument30 pagesChapter08 PDFEnfermeriaAncamNo ratings yet
- Cath Lab Essentials: Basic Hemodynamics For The Cath Lab and ICUDocument38 pagesCath Lab Essentials: Basic Hemodynamics For The Cath Lab and ICUDr. TomNo ratings yet