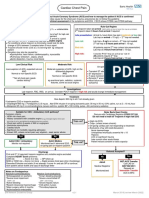
Paediatric Emergency Department
Asthma
Key:
Blue text = 2 - 5 years Some children with
Green text = 5 – 12 years severe asthma do not
Black = all ages appear distressed
Moderate Severe - Any of: Life threatening:
Sats 92% or better Sats < 92% in air Sats < 92% in oxygen
Pulse ≤ 140 or 125 Pulse > 140 or 125 Cyanosis, Silent chest
RR ≤ 40 or 30
Able to talk in sentences RR > 40 or 30 Poor respiratory effort
No severe signs Too breathless to talk / feed Hypotension
Use of accessory muscles Exhaustion / confusion / agitation
No life threatening signs Consider differentials: anaphylaxis, pneumothorax,
inhaled foreign body
Consider Resus Move to Resus
Salbutamol 2 - 10 puffs via spacer Oxygen to achieve sats 94% or above
(1 puff = 5 breaths) Salbutamol 2.5 - 5 mg neb
Reassess after 15 min, repeat as required Prednisolone 20 - 40 mg (2 mg / kg max 60 mg if on po maintenance steroids) OR
Consider Prednisolone 20 - 40 mg Hydrocortisone 50 – 100 mg iv
Better No improvement Life threatening signs
Discharge Criteria: Salbutamol 2.5 - 5 mg neb q20-30min Call Senior ED, Anaesthetic and Paeds
No life threatening signs at any time Add atrovent 125 - 250 mcg neb q20-30min Continue salbutamol neb q20-30min
Stable on 3 - 4 hourly inhalers Consider Magnesium 150 mg neb q20-30min for 1st hour Add atrovent 250 mcg neb q20-30min
Sats 94% or better
Reassess after each treatment. (0-2yrs) Salbutamol 5 mcg/kg iv
PEFR ≥75% predicted or best
If stable after 2 hours wean salbutamol to (2-15yrs) Salbutamol 15 mcg/kg iv
Consider clinical and psychosocial
q1-2h and atrovent to q4-6h (restart inhalers) max 250 mcg iv
risk factors
Prednisolone for at least 3/7 if started followed by infusion: 1 - 2 mcg/kg/min
If no improvement after 3 nebs, consider Max 5 mcg/kg/min up to 45 kg (senior advice)
Written asthma plan / advice leaflet iv salbutamol bolus +/- infusion (see red box) Magnesium 40 - 50 mg/kg (max 2g) iv
Consider regular inhaled steroids
over 30 min
[Beclometasone 100 mcg bd] if:
needing β2 agonist 3 times a week or more
weekly nocturnal symptoms disturbing sleep
Aminophylline 5 mg/kg iv over 20 min
Admit (max 500 mg, omit if on oral theophyllines)
exacerbation(s) requiring oral steroid
Failure to improve with treatment followed by infusion
GP follow-up within 48 hours Clinical and Psychosocial risk factors 1 mg/kg/hour (2 - 12 yrs) or 0.5 – 0.7 mg/kg/hr (> 12 yrs)
Consider paed clinic if 2nd attendance in 12 months Lower threshold for admission at night
Advise against parental smoking Consider HDU if requiring infusions CXR & blood gas (ear lobe / finger)
(venous pCO2 < 6 excludes hypercapnia)
Diagnosis of Asthma
This is based purely on clinical assessment in young children. When using trial of therapy,
Indications for Ventilation:
carefully assess obs and auscultate chest before and after therapy to gauge effect – consider
longer trial of therapy with careful GP follow-up only if asthma likely
Exhaustion
Worsening hypoxia
Likely asthma: RR > 60 despite treatment OR
2 or more symptoms: wheeze, cough, DIB, chest tightness (especially if frequent, recurrent,
worse at night or early morning, occur with triggers eg pets, cold air)
falling RR without clinical
Personal or family history of atopy improvement
Widespread wheeze on auscultation Worsening hypoxia
Symptoms improve with bronchodilator therapy Normal or rising CO2
Unlikely asthma:
Age less than 2 Prepare fluid bolus 20 mL/kg
Isolated cough, moist cough, dizzy, light-headed, peripheral tingling (continue 2/3 maintenance)
Symptoms only with viral URTI Prepare adrenaline bolus 0.1 mL/kg
Symptoms present from birth 1:10,000
Repeatedly normal chest exam / PEFR when symptomatic Induction (consider inhalation):
No response to trial of therapy atropine 20 mcg/kg
Clinical signs of alternative diagnosis eg CF, reflux, immunocompromise, bronchiectasis, TB, suxamethonium 1 - 2 mg/kg
pneumothorax, inhaled foreign body, pneumonia, upper airway disease, mediastinal obstruction ketamine 1 - 2 mg/kg OR
fentanyl 2 - 5 mcg/kg
Ventilation:
Notes on Salbutamol Largest possible / cuffed ETT
Infusion doses in children are higher than adults (max adult dose 20 mcg/min) Permissive hypercapnia: pH > 7.2
Monitor for side effects and signs of toxicity: hypokalaemia, lactic acidosis, tremor, tachycardia Keep PIP < 35 mmHg
Keep Tv 5 - 8 mL/kg
RR 10 – 15, PEEP 5 – 7
Risk factors for fatal asthma
I:E ratio 1:2
Clinical = previous PICU, admission in last year or repeated ED attendances, 3 or more classes
Regular suctioning & chest physio, CXR
of asthma meds, evidence of poor control eg heavy use of β2 agonist, exercise induced or
Sedation:
nocturnal symptoms PLUS
midazolam + ketamine or fentanyl +
Psychosocial = poor compliance with medication or follow-up, psychiatric illness, alcohol or drug
vecuronium as per Paediatric Infusion Protocol
problems, learning difficulties, obesity, NAI, severe domestic stress
PEM Guideline Group v1 January 2017 [review January 2019]
� Paediatric Emergency Department
Asthma
Lead Author
PEM Consultant
Paediatric Consultant
Co-Authors / Collaborators
Reference Documents
British Guideline on the Management of Asthma, BTS / SIGN 153, September 2016
Acute Severe Asthma, CATS, January 2016
British National Formulary for Children
PEM Guideline Group v1 January 2017 [review January 2019]