Professional Documents
Culture Documents
Acute Cellular Rejection: Transplantation
Uploaded by
ronaldthakorOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acute Cellular Rejection: Transplantation
Uploaded by
ronaldthakorCopyright:
Available Formats
transplantation
Acute Cellular Rejection
Mini review
Mohammad-Reza Ganji,1 Behrooz Broumand2
1Department of Nephrology, Shariati Hospital, Tehran University of Medical Sciences, Tehran, Iran 2Department of Nephrology, Rasoul-e-Akram Hospital, Iran University of Medical Sciences, Tehran, Iran Keywords. kidney transplantation, graft rejection, cellular immunity, immunosuppression
The incidence of acute rejection of the kidney allograft in the world has been around 15% during the period between 2001 and 2003. It is clinically defined as an elevation in the level of serum creatinine by more than 0.3 mg/dL and is diagnosed by kidney biopsy. On pathologic examination, the interstitium of the allograft is diffusely edematous and infiltrated by CD4 and CD8 lymphocytes. Tubulitis occurs when the lymphocytes and monocytes extend into the walls and lumina of the tubules. Presence of leukocytes determines infection or antibody-mediated rejection. Typically C4d staining is negative. Other causes of acute allograft dysfunction included prerenal factors, interstitial nephritis, infection, acute tubular necrosis, toxicity by drugs, and obstruction in the urinary tract. The primary diagnostic assessments include history, especially adherence to immunosuppressive therapy, physical examination, blood and urine laboratory tests, measurement of the serum levels of the drugs, and ultrasonography. Diagnosis of acute cellular rejection depends on biopsy, CD20 staining for refractory cases, negative C4d staining, presence of markers of activating lymphocyte, and proteomic study. Treatment of acute cellular rejection in kidney transplant recipients include pulse steroid for the first rejection episode. It can be repeated for recurrent or resistant rejection. Thymoglobulin and OKT3 are used as the second line of treatment if graft function is deteriorating. Changing the protocol from cyclosporine to tacrolimus or adding mycophenolate mofetil or sirolimus might be effective. Prognosis depends on number of rejection episodes, the use of potent drugs, time of rejection from transplantation, and response to treatment.
IJKD 2007;1:54-6 www.ijkd.org
Acute rejection (AR) remains a major complication after kidney transplantation. Although the incidence of AR has declined with the advent of new immunosuppressive drugs, it is still around 15% worldwide.1 Acute rejection usually manifests as an increase in serum creatinine, and less often, with hematuria, graft tenderness, and fever. Diagnosis can be made only by allograft biopsy. Other causes of acute allograft dysfunction include prerenal factors such as reduced effective arterial blood volume, transplant renal artery stenosis, interstitial nephritis,
infections (bacterial and viral), acute tubular necrosis, recurrent or de novo glomerular diseases, calcineurin-inhibitor-induced toxicity, and urinary tract obstruction. 1 Assessment of acute allograft dysfunction includes history taking with especial attention to adherence to immunosuppressive treatment, physical examination, examination of the serum levels of immunosuppressive drugs, imaging studies by B-mode and Doppler ultrasonography, and blood and urine laboratory tests. The short-term graft survival after treatment of
54
Iranian Journal of Kidney Diseases | Volume 1 | Number 2 | October 2007
Acute Cellular RejectionGanji and Broumand
AR has been improved; however, the long-term outcome is not promising and AR remains a major risk factor for chronic allograft dysfunction. 2,3 Donor age, donor-recipient human leukocyte antibody mismatch, panel reactive antibodies (PRA), ethnicity, and delayed graft function have been shown to be associated with the risk of rejection.4 The majority of graft lost cases after 4 to 6 months posttransplant are due to volume depletion, immunosuppressives, and urinary tract infection. Prompt diagnosis of pyelonephritis is mandatory, especially after the first year due to its strong association with graft loss.5 There are 2 types of AR that could occur either separately or together: cellular and humoral (antibody mediated). Alloreactive immune response is initiated at the interface of the grafts endothelium and the hosts CD4, CD8, and natural killer cells. 6,7 Subsequently, type 1 helper T cells and CD8 lymphocytes release interferon- and interleukin-2 on alloantigen contact and augment the cellular immune response that leads to the activation of cytotoxic T lymphocytes, natural killer cells, and monocytes that infiltrate the graft. The type 2 helper T cells response triggers the humoral response and formation of antibodies that bind to the endothelium and induce complement activation and tissue injury. Acute cellular rejection (ACR) is characterized by tubulitis that occurs when the lymphocytes and monocytes extend into the walls and lumina of the renal tubules, with associated degenerative changes of the epithelial cells. In cell-mediated vascular rejection that can be seen with tubulointerstitial rejection, the lymphocytes and monocytes undermine the swollen arterial endothelium, and with more advanced alloreactivity, arterial wall necrosis can occur. The activated T cells which mediate the AR can be shown to have upregulated expression of T-cell activating genes.8 Interestingly, induction with alemtuzumab has been associated with a predominantly monocytic ACR and poor response to pulse steroids.9 Antibody-mediated rejection (AMR) is associated with neutrophilic margination in peritubular and glomerular capillaries and is typically C4d-positive on fluoroimmunoassay or immunochemistry. The importance of differentiating humoral rejection from ACR was illustrated by many studies 10,11; Mauiyyedi and colleagues studied on patients
diagnosed with ACR and found that half of them had a mild ACR that responded to pulse steroid treatment and the other half had a more severe ACR responded to OKT3 or antilymphocyte globulin. Graft survival at 6 months for patients in the two groups was 97%.10 However, patients diagnosed as AMR had a 78% graft survival rate at 6 months. Treatment of the AMR has been successful with different combinations of mycophenolate mofetil, tacrolimus, plasmapheresis, anti-CD20, and intravenous immunoglobulin.11 Diagnosis of ACR depends on the pathology of specimens obtained by kidney allograft biopsy and different histologic examinations of the kidney tissue, including C4d staining. Noninvasive diagnosis of AR is not currently available. There are a few reports on the association of a positive staining for CD20 in refractory cases that may prompt treatment with Anti-CD20 antibody. 12 Furthermore, several other biomarkers in serum and urine have been proposed for prediction or diagnosis of AR, some with specification for ACR, none used in practice yet. The following are a summary of these markers: urine levels of chemokines CXCL9, CXCL10, and CXCL11 and their ligands, CXCR3, on activating T cells13,14; serum levels of indolamine 2,3-dioxygenase activity 15; transcription factors, T-bet, Fas ligand receptor, and costimulatory CD152 molecule16; serum levels of pretransplant interleukin-12 and interleukin-1017; urine mRNA of perforin, granzyme, and Fas ligand18; and serum levels of soluble CD30 and CD44.19 Concerning the treatment, sucbclinical ACR should be considered as well as clinical ACR. Subclinical rejection describes a morphologic pattern of ACR that may occur in up to 30% of the patients without clinical signs and symptoms of rejection that are diagnosed with protocol biopsy. There are studies that suggest these cases should be treated as clinical ACR. 20 Treatment of ACR includes pulse steroid therapy (methyl prednisolone, 125 mg to 1000 mg, for 3 to 5 days) which can reverse 75% of the first rejection episodes. It can be repeated for recurrent or resistant rejections. Thymoglobulin and OKT3 are used as the second line of treatment for steroid-resistant ACR and for Banff type IIB AR or greater; with refractory rejection, a second course can be administered in selected patients with 40% to 50% success of long term graft function. Changing the maintenance
Iranian Journal of Kidney Diseases | Volume 1 | Number 2 | October 2007
55
Acute Cellular RejectionGanji and Broumand
RS. Association of CD20+ infiltrates with poorer clinical outcomes in acute cellular rejection of renal allografts. Am J Transplant. 2005;5:2248-52. 13. Hu H, Aizenstein BD, Puchalski A, Burmania JA, Hamawy MM, Knechtle SJ. Elevation of CXCR3-binding chemokines in urine indicates acute renal-allograft dysfunction. Am J Transplant. 2004;4:432-7. 14. Abdi R, Tran TB, Sahagun-Ruiz A, et al. Chemokine receptor polymorphism and risk of acute rejection in human renal transplantation. J Am Soc Nephrol. 2002;13:754-8. 15. Friedrich R. Novel biomarkers of allograft rejection: omics approaches start to deliver. Curr Opin Organ Transplant. 2005;10:295-300. 16. Galante NZ, Camara NO, Kallas EG, Salomao R, Pacheco-Silva A, Medina-Pestana JO. Noninvasive immune monitoring assessed by flow cytometry and real time RT-PCR in urine of renal transplantation recipients. Transpl Immunol. 2006;16:73-80. 17. Fitzgerald JT, Johnson JR, Perez RV. Pre-transplant elevations of interleukin-12 and interleukin-10 are associated with acute rejection after renal transplantation. Clin Transplant. 2004;18:434-9. 18. Yannaraki M, Rebibou JM, Ducloux D, et al. Urinary cytotoxic molecular markers for a noninvasive diagnosis in acute renal transplant rejection. Transpl Int. 2006;19:75968. 19. Ayed K, Abdallah TB, Bardi R, Abderrahim E, Kheder A. Plasma levels of soluble CD30 in kidney graft recipients as predictors of acute allograft rejection. Transplant Proc. 2006;38:2300-2. 20. Nankivell BJ, Chapman JR. The significance of subclinical rejection and the value of protocol biopsies. Am J Transplant. 2006;6:2006-12. 21. Meier-Kriesche HU, Ojo AO, Hanson JA, et al. Increased impact of acute rejection on chronic allograft failure in recent era. Transplantation. 2000;70:1098-100. 22. Leggat JE Jr, Ojo AO, Leichtman AB, et al. Long-term renal allograft survival: prognostic implication of the timing of acute rejection episodes. Transplantation. 1997;63:1268-72. Correspondence to: Mohammad-Reza Ganji, MD Department of Nephrology, Shariati Hospital, Jalal-e-Al-e-Ahmad Hwy, Tehran, Iran Tel: +98 21 8883 3769 Fax: +98 21 8884 3348 E-mail: mreza@ganji.ir Received May 2007 Revised August 2007
agents from cyclosporine to tacrolimus or adding mycophenolate mofetil or sirolimus may also be effective. Recurrent rejections,21 ARs with potent immunosuppressive drugs, ARs beyond 6 months posttransplantation, and resistance to therapy are poor prognosis signs and portend poor graft outcome.22
REFERENCES
1. Djamali A, Samaniego M, Muth B, et al. Medical care of kidney transplant recipients after the first posttransplant year. Clin J Am Soc Nephrol. 2006;1:623-40. 2. Hariharan S, Johnson CP, Bresnahan BA, Taranto SE, McIntosh MJ, Stablein D. Improved graft survival after renal transplantation in the United States, 1988 to 1996. N Engl J Med. 2000;342:605-12. 3. Almond PS, Matas A, Gillingham K, et al. Risk factors for chronic rejection in renal allograft recipients. Transplantation. 1993;55:752-6. 4. Chertow GM, Milford EL, Mackenzie HS, Brenner BM. Antigen-independent determinants of cadaveric kidney transplant failure. JAMA. 1996;276:1732-6. 5. Abbott KC, Swanson SJ, Richter ER, et al. Late urinary tract infection after renal transplantation in the United States. Am J Kidney Dis. 2004;44:353-62. 6. Denton MD, Geehan CS, Alexander SI, Sayegh MH, Briscoe DM. Endothelial cells modify the costimulatory capacity of transmigrating leukocytes and promote CD28-mediated CD4(+) T cell alloactivation. J Exp Med. 1999;190:555-66. 7. DElios MM, Josien R, Manghetti M, et al. Predominant Th1 cell infiltration in acute rejection episodes of human kidney grafts. Kidney Int. 1997;51:1876-84. 8. Segerer S, Cui Y, Eitner F, et al. Expression of chemokines and chemokine receptors during human renal transplant rejection. Am J Kidney Dis. 2001;37:518-31. 9. Zhang PL, Malek SK, Prichard JW, et al. Acute cellular rejection predominated by monocytes is a severe form of rejection in human renal recipients with or without Campath-1H (alemtuzumab) induction therapy. Am J Transplant. 2005;5:604-7. 10. Mauiyyedi S, Crespo M, Collins AB, et al. Acute humoral rejection in kidney transplantation: II. Morphology, immunopathology, and pathologic classification. J Am Soc Nephrol. 2002;13:779-87. 11. Crespo M, Pascual M, Tolkoff-Rubin N, et al. Acute humoral rejection in renal allograft recipients: I. Incidence, serology and clinical characteristics. Transplantation. 2001;71:652-8. 12. Hippen BE, DeMattos A, Cook WJ, Kew CE 2nd, Gaston
56
Iranian Journal of Kidney Diseases | Volume 1 | Number 2 | October 2007
You might also like
- 93 TreaTmenT of AcuTe and Chronic RejecTionDocument12 pages93 TreaTmenT of AcuTe and Chronic RejecTionAbdulRehmanKhanNo ratings yet
- Caplacizumab Treatment For Acquired Thrombotic Thrombocytopenic PurpuraDocument12 pagesCaplacizumab Treatment For Acquired Thrombotic Thrombocytopenic PurpuraRobin Devassy MNo ratings yet
- Renal Transplantation An OverviewDocument58 pagesRenal Transplantation An OverviewSony's TechNo ratings yet
- Nej MR A 0902927Document12 pagesNej MR A 0902927Pepita GonzalesNo ratings yet
- Rejeksi AllograftDocument10 pagesRejeksi AllograftIndra kusuma mardiaNo ratings yet
- Understanding Transfusion Reactions in Oncology by NurseDocument6 pagesUnderstanding Transfusion Reactions in Oncology by NursefitriNo ratings yet
- The Pathophysiology of Pure Red Cell Aplasia: Implications For TherapyDocument9 pagesThe Pathophysiology of Pure Red Cell Aplasia: Implications For TherapyPhương NhungNo ratings yet
- Review Article: Antibody-Mediated Rejection in Kidney Transplantation: A ReviewDocument10 pagesReview Article: Antibody-Mediated Rejection in Kidney Transplantation: A ReviewXavier JonazNo ratings yet
- Nej Mo A 1806311Document12 pagesNej Mo A 1806311Hugo PicciottoNo ratings yet
- Jco 2001 19 18 3852Document9 pagesJco 2001 19 18 3852Luis SanchezNo ratings yet
- Biology of Blood and Marrow TransplantationDocument6 pagesBiology of Blood and Marrow TransplantationFrankenstein MelancholyNo ratings yet
- Management and Outcomes For Patients With TTP: Analysis of 100 Cases at A Single InstitutionDocument6 pagesManagement and Outcomes For Patients With TTP: Analysis of 100 Cases at A Single InstitutionBilly Shan LastKagerooboroNo ratings yet
- Acute Leukaemia Presentation 1Document20 pagesAcute Leukaemia Presentation 1Vaibhav KrishnaNo ratings yet
- Reactive and Clonal Thrombocytosis: Cytokines and Acute Phase ReactantsDocument6 pagesReactive and Clonal Thrombocytosis: Cytokines and Acute Phase ReactantsIvana MilanovicNo ratings yet
- Pyruvate Kinase MalariaDocument6 pagesPyruvate Kinase Malariajeff c100% (2)
- Nihms 396194Document15 pagesNihms 396194miR 125bNo ratings yet
- Cytomegalovirus:: Clinical Virological Correlations in Renal Transplant RecipientsDocument10 pagesCytomegalovirus:: Clinical Virological Correlations in Renal Transplant RecipientsRaffaharianggaraNo ratings yet
- Acute Immune Thrombocytopenic Purpura in Children: Abdul RehmanDocument11 pagesAcute Immune Thrombocytopenic Purpura in Children: Abdul RehmanApriliza RalasatiNo ratings yet
- Platelet Transfusion Refractoriness How Do IDocument6 pagesPlatelet Transfusion Refractoriness How Do IJuan Manuel Cano CalderónNo ratings yet
- Prognostic Factors in Acute Myeloid Leukaemia 4: Bob LoèwenbergDocument11 pagesPrognostic Factors in Acute Myeloid Leukaemia 4: Bob LoèwenbergStephania SandovalNo ratings yet
- Pyruvate Kinase Deficiency and Malaria: Brief ReportDocument6 pagesPyruvate Kinase Deficiency and Malaria: Brief ReportErlangga Perwira NegaraNo ratings yet
- Chronic Myeloid Leukemia Dissertation ThesisDocument8 pagesChronic Myeloid Leukemia Dissertation ThesisHelpWithFilingDivorcePapersCanada100% (2)
- Anemia Aplastic JournalDocument13 pagesAnemia Aplastic JournalGenoveva Maditias Dwi PertiwiNo ratings yet
- Clonorchis Sinensis Induced CCADocument3 pagesClonorchis Sinensis Induced CCARyznar FaisalNo ratings yet
- 1 s2.0 S0006497121069950 MainDocument12 pages1 s2.0 S0006497121069950 MainSALEHA HASSANNo ratings yet
- Uso de Plasmaféresis en Unidades de Pacientes CríticosDocument8 pagesUso de Plasmaféresis en Unidades de Pacientes CríticosElena Garcia LueizaNo ratings yet
- Minimal Residual Disease in Acute Lymphoblastic Leukemia: Dario CampanaDocument6 pagesMinimal Residual Disease in Acute Lymphoblastic Leukemia: Dario CampanaJAIR_valencia3395No ratings yet
- Urinary Tract Infection With CKDDocument12 pagesUrinary Tract Infection With CKDbookreader_998No ratings yet
- An Overview of The Mechanisms of HIV-related ThrombocytopeniaDocument17 pagesAn Overview of The Mechanisms of HIV-related ThrombocytopeniaMesay AssefaNo ratings yet
- 4 U1.0 B978 1 4557 4617 0..00062 5..DOCPDFDocument11 pages4 U1.0 B978 1 4557 4617 0..00062 5..DOCPDFCamiloTrimiñoNo ratings yet
- Acute Allograft Rejection in Liver Transplant Recipients: Incidence, Risk Factors, Treatment Success, and Impact On Graft FailureDocument12 pagesAcute Allograft Rejection in Liver Transplant Recipients: Incidence, Risk Factors, Treatment Success, and Impact On Graft Failurenathalialusman98No ratings yet
- Literature AbdoDocument20 pagesLiterature AbdothestaffforpediatricptNo ratings yet
- Late Onset Thrombosis in A Case of Severe Protein S Deficiency Due To Compound Heterozygosity For PROS1 MutationsDocument3 pagesLate Onset Thrombosis in A Case of Severe Protein S Deficiency Due To Compound Heterozygosity For PROS1 Mutationsgabriela ciolpanNo ratings yet
- Rodrguez Vicente 2013Document14 pagesRodrguez Vicente 2013Jose AbadiaNo ratings yet
- Abnormalities of RUNX1, CBFB, CEBPA, and NPM1 Genes in Acute Myeloid LeukemiaDocument10 pagesAbnormalities of RUNX1, CBFB, CEBPA, and NPM1 Genes in Acute Myeloid LeukemiaAndikhaNo ratings yet
- Chronic Lymphocytic Leukemia: A Clinical and Molecular Heterogenous DiseaseDocument14 pagesChronic Lymphocytic Leukemia: A Clinical and Molecular Heterogenous DiseaseCallisthenisLeventisNo ratings yet
- Sepsis Si CoagulareDocument8 pagesSepsis Si CoagulareCorina DavidNo ratings yet
- Citología UrinariaDocument6 pagesCitología UrinariaCarla Véjar DíazNo ratings yet
- Chronic Lymphocytic Leukemia (CLL) - Then and Now: Critical ReviewDocument11 pagesChronic Lymphocytic Leukemia (CLL) - Then and Now: Critical ReviewJose Angel AbadíaNo ratings yet
- Cytologic Diagnosis of Malignant Pleural EffusionDocument4 pagesCytologic Diagnosis of Malignant Pleural EffusionSilva ApryllNo ratings yet
- Retinal Vein Thrombosis in A Patient With Metastatic Colon Cancer Receiving XELOX Chemotherapy Combined With Bevacizumab Pre-Hepatic ResectionDocument4 pagesRetinal Vein Thrombosis in A Patient With Metastatic Colon Cancer Receiving XELOX Chemotherapy Combined With Bevacizumab Pre-Hepatic ResectionmaryNo ratings yet
- Day 21 Bone Marrow Findings Incorrectly Designate Residual Leukaemi - 2024 - PatDocument8 pagesDay 21 Bone Marrow Findings Incorrectly Designate Residual Leukaemi - 2024 - PatLuis GómezNo ratings yet
- Immunological Effects of A Single Hemodialysis TreatmentDocument14 pagesImmunological Effects of A Single Hemodialysis TreatmentBintiNo ratings yet
- ASH Guidlines On Platelet RefractorinessDocument6 pagesASH Guidlines On Platelet RefractorinessM Asif NaveedNo ratings yet
- Combining Immunotherapy and Radiation For Prostate Cancer: ReviewDocument9 pagesCombining Immunotherapy and Radiation For Prostate Cancer: ReviewitontNo ratings yet
- Diagnosis and Management For UrosepsisDocument8 pagesDiagnosis and Management For UrosepsisanggaNo ratings yet
- Immune Dysfunction and Risk of Infection in CKD - 2019Document8 pagesImmune Dysfunction and Risk of Infection in CKD - 2019Lú VillalobosNo ratings yet
- 976 FullDocument7 pages976 FullFirda PotterNo ratings yet
- 263-270 RemuzziDocument8 pages263-270 Remuzzimishrak20No ratings yet
- TMP 9 B42Document6 pagesTMP 9 B42FrontiersNo ratings yet
- Ojim 2016091213324550Document10 pagesOjim 2016091213324550rianmg21No ratings yet
- The Effect of HLADocument9 pagesThe Effect of HLAMihai PerescuNo ratings yet
- JCM 08 01175 v2 PDFDocument28 pagesJCM 08 01175 v2 PDFAs'har AnwarNo ratings yet
- 8329 31380 2 PBDocument3 pages8329 31380 2 PBAshan BopitiyaNo ratings yet
- Non-Onvasive Diagnosis of Acrd Current OpinionDocument9 pagesNon-Onvasive Diagnosis of Acrd Current Opinionnathalialusman98No ratings yet
- Respiratory and Pulmonary Medicine: ClinmedDocument3 pagesRespiratory and Pulmonary Medicine: ClinmedGrace Yuni Soesanti MhNo ratings yet
- Best Practice & Research Clinical HaematologyDocument11 pagesBest Practice & Research Clinical HaematologyStephania SandovalNo ratings yet
- Ma Ramica 2019Document4 pagesMa Ramica 2019NausheenNo ratings yet
- Thrombocytopenia in Plasmodium Falciparum MalariaDocument3 pagesThrombocytopenia in Plasmodium Falciparum MalariaArja' WaasNo ratings yet
- Exercise - Initiating and Maintaining - PcnaDocument1 pageExercise - Initiating and Maintaining - PcnaronaldthakorNo ratings yet
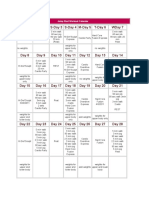
- Master Rotation Plan 2nd Year B.Sc. NursingDocument2 pagesMaster Rotation Plan 2nd Year B.Sc. Nursingronaldthakor100% (1)
- Master Rotation Plan 2nd Year B.Sc. NursingDocument2 pagesMaster Rotation Plan 2nd Year B.Sc. Nursingronaldthakor100% (1)
- Guidelines For The Special Scheme of Faculty Development Programme For Colleges For The Twelfth Plan (2012-2017)Document19 pagesGuidelines For The Special Scheme of Faculty Development Programme For Colleges For The Twelfth Plan (2012-2017)deepak4evolutionNo ratings yet
- Bed MakingDocument44 pagesBed Makingronaldthakor100% (1)
- Types of MattresssDocument1 pageTypes of MattresssronaldthakorNo ratings yet
- ServiceDocument1 pageServiceronaldthakorNo ratings yet
- FInal TOBACCO PamphletDocument2 pagesFInal TOBACCO PamphletronaldthakorNo ratings yet
- 3 - ANNA Scope and StandardsDocument14 pages3 - ANNA Scope and StandardsronaldthakorNo ratings yet
- Ot DesignDocument1 pageOt DesignronaldthakorNo ratings yet
- Decision MakingDocument22 pagesDecision MakingronaldthakorNo ratings yet
- Physiology of MenstruationDocument3 pagesPhysiology of MenstruationMIKAELA DAVIDNo ratings yet
- Autonomic DrugsDocument4 pagesAutonomic DrugsSabrinaNo ratings yet
- A ThingDocument3 pagesA ThingIsaiah Perez0% (1)
- Trauma MaksilofacialDocument69 pagesTrauma MaksilofacialgedepambudiNo ratings yet
- Ectopia Lentis PDFDocument7 pagesEctopia Lentis PDFBeerappaJanpetNo ratings yet
- Neural Signal Processing: ELEC 548 - Fall 2015 Tuesday/Thursday 09:25AM - 10:40AM BRC 284Document31 pagesNeural Signal Processing: ELEC 548 - Fall 2015 Tuesday/Thursday 09:25AM - 10:40AM BRC 284marcaumggNo ratings yet
- N C by Dr. Mohamed Baraka: Ausea AND Vomiting Onstipation AND DiarrheaDocument72 pagesN C by Dr. Mohamed Baraka: Ausea AND Vomiting Onstipation AND DiarrheaIbrahim Mahmoud AliNo ratings yet
- Gabriel Axel - Master Thesis - Vision The Art of Evolution (2010)Document41 pagesGabriel Axel - Master Thesis - Vision The Art of Evolution (2010)gabrielaxelNo ratings yet
- Circulation 1979 Hennekens 486 9Document5 pagesCirculation 1979 Hennekens 486 9Dwi Putri CNo ratings yet
- FandAC - 2017 - Hamid - Chronic Rupture of Peroneal TendonsDocument8 pagesFandAC - 2017 - Hamid - Chronic Rupture of Peroneal TendonsJacob DoughertyNo ratings yet
- Alingatong Plants?Document3 pagesAlingatong Plants?nancy urrizaNo ratings yet
- Development of Media and Automated Liquid Fermentation Methods To Produce Desiccation-Tolerant Propagules of Trichoderma HarzianumDocument8 pagesDevelopment of Media and Automated Liquid Fermentation Methods To Produce Desiccation-Tolerant Propagules of Trichoderma HarzianumcarloscarinelliNo ratings yet
- Chapter 30 - HypertensionDocument70 pagesChapter 30 - HypertensionSakaC.TanayaNo ratings yet
- Module 1 Cells As The Basis of Life NotesDocument17 pagesModule 1 Cells As The Basis of Life NotesNicholas MichailouNo ratings yet
- Medical Certificate: San Isidro Elementary School Provincial Rd. Brgy. San IsidroDocument2 pagesMedical Certificate: San Isidro Elementary School Provincial Rd. Brgy. San IsidroKevin WhiteNo ratings yet
- Advanced Trauma Life SupportDocument452 pagesAdvanced Trauma Life Supportnatalia100% (7)
- Mitosis Meiosis NotesDocument7 pagesMitosis Meiosis NotesSophia Cook100% (1)
- Endocrinology Learning Goals - IPHY 4440Document9 pagesEndocrinology Learning Goals - IPHY 4440Geline Joy D. SamillanoNo ratings yet
- Transitional EpitheliumDocument7 pagesTransitional EpitheliumsakuraleeshaoranNo ratings yet
- Mental Health Nursing Practice Test 11Document5 pagesMental Health Nursing Practice Test 11Dr. Jayesh Patidar100% (2)
- Workout CalendarDocument2 pagesWorkout CalendarKatie Bonick-ColbreseNo ratings yet
- Nutrition Part Fat-Soluble Vitamin Deficiency: UMFA2053 General Pathology (JAN) Lan Yen MinDocument68 pagesNutrition Part Fat-Soluble Vitamin Deficiency: UMFA2053 General Pathology (JAN) Lan Yen MinAliLeeNo ratings yet
- Serum Iron and Iron-Binding Capacity in Clinical Diagnosis: Emanuel E. MandelDocument12 pagesSerum Iron and Iron-Binding Capacity in Clinical Diagnosis: Emanuel E. MandelTanveerNo ratings yet
- Lesson TemplateDocument6 pagesLesson TemplateAnonymous 9p23ZapzNo ratings yet
- Dna StructureDocument23 pagesDna Structureapi-315792432No ratings yet
- Handbook of The Assisted Reproduction LaboratoryDocument412 pagesHandbook of The Assisted Reproduction LaboratoryRinda Puspasari100% (5)
- VanPutte Seeleys Essentials 11e Chap07 PPT AccessibleDocument140 pagesVanPutte Seeleys Essentials 11e Chap07 PPT AccessibleCyrille Aira AndresaNo ratings yet
- Clinical Hemodynamic Correlation in Mitral StenosisDocument82 pagesClinical Hemodynamic Correlation in Mitral StenosisHristo MateevNo ratings yet
- Cardiac Auscultation - Rediscovering The Lost ArtDocument83 pagesCardiac Auscultation - Rediscovering The Lost ArtBrainy-Paykiesaurus Luminirex100% (1)
- Barry. Perception and Visual Communication TheoryDocument16 pagesBarry. Perception and Visual Communication TheoryKosta Hoekstra50% (2)