Professional Documents
Culture Documents
Finals - Cellular Aberrations
Finals - Cellular Aberrations
Uploaded by
Maggay LarsOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Finals - Cellular Aberrations
Finals - Cellular Aberrations
Uploaded by
Maggay LarsCopyright:
Available Formats
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
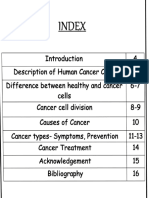
TOPIC OUTLINE: CANCER DESCRIPTION
ALCON, MARY GRACE Cancer is a disease in which some of the body’s cells
AQUINO, JVY MARIE grow uncontrollably and spread to other parts of the
AZUTEN, ZYZA-ZHOLEY body.
BALLESTA, ERIKA Cancer can start almost anywhere in the human body,
BORJA, RIVERT JAMES which is made up of trillions of cells. Normally, human
CARTUJANO, DAZLYNE cells grow and multiply (through a process called cell
CASTERAL, EILEITHIA CHYAVANNA division) to form new cells as the body needs them.
CORPUZ, MARK ANTHONY When cells grow old or become damaged, they die, and
DERY, JOHN BRYAN new cells take their place.
TACCAD, HANNAH Sometimes this orderly process breaks down, and
TALOSIG, KEZIAH abnormal or damaged cells grow and multiply when they
SOMERA, KARLA MAE shouldn’t. These cells may form tumors, which are
lumps of tissue. Tumors can be cancerous(malignant) or
I. CANCER DESCRIPTION not cancerous (benign).
a. Common sites of metastasis Cancerous tumors spread into, or invade, nearby tissues
b. Grading and staging and can travel to distant places in the body to form new
c. General pathophysiology tumors (a process called metastasis). Cancerous tumors
1. Factors that influence cancer development may also be called malignant tumors. Many cancers
2. Prevention form solid tumors, but cancers of the blood, such as
3. Early detection leukemias, generally do not.
4. Warning signs (CAUTION) Benign tumors do not spread into, or invade, nearby
d. Diagnostic tests tissues. When removed, benign tumors usually don’t
1. Biopsy grow back, whereas cancerous tumors sometimes do.
2. Bone marrow examination Benign tumors can sometimes be quite large, however.
3. Chest radiograph Some can cause serious symptoms or be life
4. CBC threatening, such as benign tumors in the brain.
5. MRI
II. PAIN CONTROL COMMON SITES OF METASTASIS
a. Causes
b. Interventions
III. CHEMOTHERAPY
a. Description and classification
b. General nursing responsibilities
IV. RADIATION THERAPY
a. Description and classification
1. Teletherapy Cancer can spread to almost any part of the body,
2. Brachytherapy although different types of cancer are more likely to
b. General nursing responsibilities spread to certain areas than others. The most common
sites for cancers to metastasize include the lungs, liver,
V. COMMON CELLULAR ABERRATIONS bones and brain. Other places include the adrenal
a. Breast cancer gland, lymph nodes, skin and other organs. The
b. Lung cancer following list shows the most common sites of
c. Colon cancer metastasis, not including the lymph nodes, for some
d. Liver cancer common cancers:
e. Cervical cancer
f. Ovarian cancer
g. Prostate cancer
VI. HEMATOLOGIC CELLULAR
ABERRATIONS
a. Leukemia
b. Lymphoma
BSN3A | PBL GROUP 1 1
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
Tumor cells are grouped into 4 types based on their
resemblance to/difference from healthy cells (G1,
G2, G3, G4):
o Well-differentiated tumors (low grade, G1)
generally have a better prognosis than
poorly differentiated tumors (high grade,
G4).
o Poorly differentiated tumors are called
anaplastic.
Tissue markers are helpful if cells of unknown origin
are found:
o Cytokeratin is expressed by carcinomas.
o Vimentin is expressed by sarcomas.
o CD45 is expressed by lymphomas.
Grading is performed for most types of tumors, but there
are specific exceptions.
Prostate cancer: uses the Gleason score ranging
from 2–10
o Based on the growth pattern and degree of
differentiation of tumor cells
o A higher score is associated with disease
outside the prostate.
o A higher score indicates a greater likelihood
of a worse prognosis.
Brain tumors: specific WHO classification
o Uses both genotype and phenotype for
some tumors
o Immunohistochemical data for molecular
genetic alterations are used in addition to
histology.
Breast cancer: uses the Nottingham grading system
o Based on tubule formation of the tumor,
nuclear grade, and mitotic rate
o Each category is scored between 1 and 3,
and a total score is calculated.
o Total score of 3–5 is G1 (low grade; well
differentiated).
o Total score of 6–7 is G2 (intermediate
grade; moderately differentiated).
o Total score of 8–9 is G3 (high grade; poorly
differentiated).
Tumor grading:
Sometimes, a metastasis will be found without a known
primary cancer (point of origin). In this situation, your
Gx = grade cannot be assessed (undetermined
health care provider will search extensively for the
primary cancer source. If none can be found, it’s called grade)
cancer of unknown primary (CUPS). G1 = well differentiated, close similarity to original
tissue (low grade)
G2 = somewhat differentiated malignant tissue
GRADING AND STAGING (intermediate grade)
G3 = poorly differentiated malignant tissue (high
GRADING
grade)
Grading is the histologic assessment of tumor cells G4 = undifferentiated malignant tissue: The original
according to their state of differentiation. tissue that gave rise to the tumor can be determined
Microscopic examination of tumor cells after surgery only by immunohistochemical evaluation or not at all
or biopsy (high grade).
BSN3A | PBL GROUP 1 2
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
STAGING o Cervical and ovarian cancer: International
Federation of Gynecology and Obstetrics
Staging for cancer describes the extent of the disease (FIGO) system
and is used to help communicate with other members of o Breast carcinoma staging uses TNM plus
the medical and surgical team for treatment decisions other factors to determine stage:
and prognosis. For example, with colon cancer, after Grade
surgery and pathologic staging, chemotherapy given to Receptor status: human epidermal
individuals with stage III disease eradicates growth factor receptor(HER)-
micrometastases, reduces the likelihood of disease 2, estrogen receptor (ER),
recurrence, and increases cure rates. and progesterone receptor (PR)
o Lung cancer:
Clinical staging (“c” before the stage) happens before T relates to tumor size but also to
surgery. whether it has invaded nearby
o Physical exam structures.
o Imaging with CT, MRI, or PET scans N of the TNM stage uses the
Pathologic staging (“p” before the stage) is done number of involved nodal stations.
after biopsy or surgical removal. M of the TNM stage is divided
Stages range from localized to widespread: according to whether metastatic
o Stage 0: carcinoma in situ (marked growth disease is limited to the chest or
of abnormal cells that have not spread to single/multiple extrathoracic sites
neighboring tissue but have the potential to of metastasis.
develop into a tumor) o Melanoma uses the TNM staging system;
o Stage I: localized (beyond the basement however:
membrane) Concordance with consensus
o Stage II: early localized advanced reference diagnosis and
o Stage III: late locally advanced reproducibility between
o Stage IV: metastasized to different organs pathologists remains low.
Stage is applied after a tumor is classified using T of the TNM stage takes into
the TNM system. account tumor thickness
o The American Joint Committee on Cancer in mm and the presence or
(AJCC) updates the staging system absence of ulceration.
periodically; currently, the 8th edition is M of the TNM stage takes into
being followed (effective 2018). account the lab LDH levels.
o Relies on anatomic, macroscopic groupings o Colon cancer staging:
of disease with similar prognoses Clinical staging is based on exam,
o T = size and extent of the primary tumor: CT results, and tumor marker
Tx: Primary tumor cannot be carcinoembryonic
measured. (CEA) antigen levels.
T0: absence of primary tumor Pathologic staging is based on
T1–T4: assignment according to TNM.
the specific type of tumor
considering criteria such as size,
invasive depth, and infiltration of
neighboring tissue and organs
o N = involvement of lymph nodes:
Nx: Involvement of
neighboring lymph nodes cannot
be assessed.
N0: no involvement of
neighboring lymph nodes
N1–N3: number and localization
of lymph nodes with cancer
o M = status of metastases:
Mx: Distant metastases cannot be
assessed.
M0: no metastases
M1: distant metastases observed
Staging is specific for each cancer; some deviate
from the commonly used TNM system.
o Lymphoma: Ann Arbor staging
BSN3A | PBL GROUP 1 3
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
Example of T1–T4 staging for tumor in the colon
T1: Tumor invades the submucosa (through the muscularis
mucosa but not into the muscularis propria).
T2: Tumor invades the muscularis propria.
T3: Tumor invades through the muscularis propria into the
surrounding tissues.
T4: Direct extension through the serosa, invading the visceral
peritoneum or adhering to adjacent organs
GENERAL PATHOPHYSIOLOGY
FACTORS THAT INFLUENCE CANCER DEVELOPMENT
Carcinogenesis- Carcinogenesis is the
development of cancer by transforming healthy cells
into cancer cells.
o Molecular Process
Initiation
Promotion
Progression
Proliferative Patterns
o Etiology- Factors implicated or known to
induce carcinogenesis include viruses and
bacteria, physical agents, chemicals,
genetic or familial factors, lifestyle factors,
and hormones. Additional research is
needed for a better understanding of the
relationships among etiologic factors and
cancer.
Viruses and Bacteria- Examples of
these viruses that are known to
cause cancer include human
papillomavirus (HPV) (cervical
and head and neck cancers),
hepatitis B virus (HBV) (liver
cancer), and Epstein–Barr virus
(EBV) (Burkitt lymphoma and
nasopharyngeal cancer).
Examples of bacteria that are
associated with an increased risk
of cancer include: Helicobacter
pylori (stomach cancer),
BSN3A | PBL GROUP 1 4
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
Salmonella enteritidis (colon PREVENTION
cancer), and Chlamydia
trachomatis (ovarian and cervical Eat a healthy diet. Consider the following:
cancers) o Eat plenty of fruits and vegetables and other
Physical Agents- Physical factors foods from plant sources — such as whole
associated with carcinogenesis grains and beans.
include exposure to sunlight, o Drink alcohol only in moderation.
radiation, chronic irritation or o Limit processed meats.
inflammation, tobacco Maintain a healthy weight and be physically
carcinogens, industrial chemicals, active.
and asbestos (ACS, 2019b). Don’t use tobacco. Smoking has been linked to
Chemical Agents (Tobacco, many types of cancer, including cancer of the lung,
Cigarette smoking, Environmental mouth, throat, pancreas, bladder, cervix, and kidney.
tobacco smoke (ETS), otherwise Protect yourself from the sun. Skin cancer is one
known as secondhand smoke. of the most common kinds of cancer and one of the
Other combustible forms of most preventable. Stay out of the sun between 10am
tobacco, such as cigars, pipes, and 4pm when the sun’s rays are the strongest.
roll-your-own products, and water Get vaccinated. Protecting against certain viral
infections can help protect against cancer.
pipes (or hookah), are also Get regular medical care and cancer screening
associated with increased cancer tests. Doing regular self-exams and having
risk (ACS, 2019d). Electronic screening for cancers — such as cancer of the skin,
nicotine delivery systems (ENDS) color, cervix and breast can raise the chances of
including e-cigarettes, e-pens, finding cancer early.
epipes, e-hookah and e-cigars Know yourself, your family history, and your
have gained increased popularity risks.
as an alternative to tobacco.
Smokeless tobacco products, EARLY DETECTION
such as chewing tobacco, snuff
and snus, used most often by Screening tests are used to find cancer before a person
young adults aged 18 to 25 years, has any symptoms.
are associated with an increased Regular screenings can help find and treat pre-cancers
risk of oral, pancreatic, and and cancers early, before they have a chance to spread.
esophageal cancer. The extensive
list of suspected chemical BREAST CANCER
substances continues to grow and
includes aromatic amines and Women ages 40-44 should have the choice to start
aniline dyes; pesticides and annual breast cancer screening with mammogram (x-rays
formaldehydes; arsenic, soot, and of the breast).
tars; asbestos; benzene; Women ages 45-older should get mammograms every
cadmium; chromium compounds; year.
nickel and zinc ores; wood dust; Women should also know how their breasts normally look
beryllium compounds; and and report any breast changes to a health care provider.
polyvinyl chloride. Betel quid,
which are chewed as stimulants in COLON AND RECTAL CANCER AND POLYPS
some cultures, are also included.
The American Cancer Society recommends starting
Genetics and Familial Factors
regular screening at age 45.
Lifestyle Factors (e.g., obesity,
This can be done through a stool-based test, or with an
alcohol intake, poor diet, physical
exam that looks at the colon and rectum (a visual exam).
inactivity)
Hormonal Agents (Prenatal CERVICAL CANCER
exposure to diethylstilbestrol,
Hormonal changes related to the Screening should start at age 25.
female reproductive cycle, Ages 25-65 should get a primary HPV (human
Estrogen, Combination estrogen papilomavirus) test done every 5 years.
and progesterone therapy) Pap-smear test every 3 years.
Role of the Immune System
o Normal Immune Response
o Immune System Evasion
BSN3A | PBL GROUP 1 5
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
ENDOMETRIAL CANCER For instance, in a fine needle aspiration biopsy, the
doctor inserts a very thin, hollow needle through the skin
The American Cancer Society recommends that at the to collect a sample of cells and sometimes fluid for
time of menopause, all women should be told about the examination. This is the most simple type of biopsy. It is
risks and symptoms of endometrial cancer. often used when a mass can be felt through the skin. A
core needle biopsy uses a larger needle to remove a
larger tissue sample than a fine needle biopsy. A vacuum-
Women should report any unexpected vaginal bleeding
assisted biopsy uses a suction device to collect a tissue
or spotting. sample through a specially designed needle. Your doctor
LUNG CANCER can collect multiple or large samples from the same
biopsy site with this method.
Image-guided biopsy. This type of biopsy uses imaging
People at increased risk for lung cancer is recommended
equipment to help your doctor take the sample. You might
to get an annual lung screening test.
have this if your doctor cannot feel a tumor, or it may be
People who currently smoke or have quit in the past 15 deeper inside the body. Sometimes, even if a tumor is
years and have at least a 20 pack-year smoking history large enough to feel, image-guided biopsy can be used to
are required to have a screening test for LDCT scans. help direct the doctor to the right part of the body. This
helps the doctor do the biopsy in the safest way possible.
PROSTATE CANCER The imaging equipment may be:
o Ultrasound
Starting at age 50, men should talk to a health care o Fluoroscopy
provider about the pros and cons of testing. o Computed tomography (CT) scan
Men who have a family history of prostate CA should start o X-ray
at age 45. o Magnetic resonance imaging (MRI) scan
Women should also know how their breasts normally look Surgical (excisional) biopsy. This type of biopsy is
and report any breast changes to a health care provider. done using surgery to remove the tissue your doctor
thinks may be cancer. The surgeon makes an incision
(cut) into the skin to remove the suspicious tissue. The
WARNING SIGNS (CAUTION) complexity of the surgery depends on the area of the body
involved.
Change in bowel or bladder habits Shave biopsy/punch biopsy. For a shave biopsy, the
A sore that does not heal doctor removes some tissue by scraping the surface of
the skin. In a punch biopsy, they use a small circular
Unusual bleeding or discharge
instrument to push through the surface of the skin and
Thickening or lumps take a sample of tissue from below the skin's surface.
Indigestion or difficulty in swallowing These are used most commonly for a skin biopsy.
Obvious change in wart or mole Endoscopic biopsy. An endoscope is a thin, lighted,
Nagging or persistent cough or hoarseness flexible tube with a camera that allows doctors to view the
Unexplained anemia inside of the body, including the esophagus, stomach,
Sudden unexplained weight loss bladder, and joints. The endoscope goes in through the
mouth, nose, or a small incision in the skin. The attached
DIAGNOSTIC TESTS camera helps the doctor see any abnormal areas. Your
doctor can also take tissue samples for a biopsy. Learn
more about the different endoscopic techniques.
Laparoscopic biopsy. Similar to an endoscopic biopsy,
BIOPSY this type of biopsy is used to examine for certain areas of
the body, including the abdomen or pelvis. When used for
In a biopsy, a doctor takes a small amount of tissue from the chest, it is called a thoracoscopy or thoracoscopic
the area of the body where cancer may be present. The biopsy. In this type of biopsy, the doctor inserts a thin tube
tissue is sent to a laboratory and examined under a with a video camera called a laparoscope into the
microscope for cancer cells by a specialist called a abdomen through small incisions. This allows the doctor
pathologist. Other tests can suggest that cancer is in the to see abnormal areas and take tissue samples for
body, but only a biopsy can test to show whether there examination.
are cancer cells. Bone marrow aspiration and biopsy. Bone marrow is
the soft tissue and liquid inside your bones. The
The type of biopsy you have depends on where the
aspiration takes a small sample of the liquid with a needle,
possible cancer is located. while the biopsy takes a sample of solid tissue. A bone
marrow aspiration and biopsy is done to check for a
TYPES OF BIOPSIES
blood disorder or blood cancer, such as leukemia,
lymphoma, or multiple myeloma. Bone marrow aspiration
Needle biopsies. This general category refers to
and biopsy are often taken from the pelvic bone. This is
different biopsies, each using a special needle to collect
on the lower back, near the hip.
cells to test an area for cancer.
Liquid biopsy. Testing a blood sample for cancer is
called a liquid biopsy. You give a small sample of blood,
BSN3A | PBL GROUP 1 6
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
and it is sent to the lab for specific tests. It can also show BONE MARROW EXAMINATION
how cancer is responding to treatment. A liquid
biopsy has less risk than taking a sample of tissue, and crucial when additional information is needed to
your doctor can do it multiple times. However, this type of assess how a patient’s blood cells are being formed
biopsy is still new and it is not done for most types of to assess the quantity and quality of each type of
cancer. There is a lot of research ongoing to expand
cell produced within the marrow
usage of this technique.
GETTING READY FOR BIOPSY results of these tests can be used to document
infection or tumor within the marrow.
You might need to remove your clothing and jewelry and Normal bone marrow: semifluid state and can be
put on a hospital gown after you arrive. aspirated through a special large needle
Ask whether there are restrictions on what you can o Adults
eat or drink before the biopsy. If there are LOCATION of bone marrow
restrictions, ask for how long beforehand. aspiration: iliac crest & sternum
Ask if you should take your regular medications that BONE MARROW ASPIRATE: provides a sample of
day. For certain biopsies, your doctor will want to cells from the more fluid part of the bone marrow
know if you are taking blood thinners or aspirin. Tell BONE MARROW BIOPSY: examines the solid part
your doctor about all medications and supplements of the bone marrow
you are taking. o LOCATION: posterior iliac crest
Tell your doctor about any allergies or other medical o shows the architecture of the bone marrow
conditions you have.
as well as its degree of cellularity
Be sure you understand where the biopsy will take
place. If it is at a different location than your doctor's BEFORE ASPIRATION
office, be sure to talk with that location about your
health insurance coverage for the test. Skin is cleansed using ASEPTIC TECHNIQUE
You will be asked to sign a consent form saying you Small area is anesthesized with LOCAL
understand the benefits and risks and agree to have
ANESTHETIC AGENT thru the skin and
the biopsy. Ask any questions you may have about
SUBCUTANEOUS TISSUE TO THE PERIOSTEUM
this legal form.
OF THE BONE
Being nervous about an upcoming medical test is
common and is sometimes called scanxiety. If you Note: Not possible to anesthesize the bone itself
feel very worried, talk with your health care team Bone marrow is introduced with stylet in place
about ways to cope with these feelings. When the needle moves through the outer cortex of
Ask what to expect about your recovery after the test. bone and enters the marrow cavity, the stylet is
DURING BIOPSY removed, and a syringe is attached
A small volume (5 mL) of blood and marrow is then
Depending on the part of your body being checked, you aspirated.
might lie down or sit up. You might need to hold your Px feel pressure sensation as the needle is
breath or stay still. Your health care team will let you know
advanced
what to expect.
Actual aspiration causes sharp but brief pain
Before the procedure, you may receive a type of
anesthesia to block the awareness of pain. The type o Management: Deep breaths and relaxation
depends on biopsy and where it is done. You may have techniques
local anesthesia to numb the area, conscious sedation, or
general anesthesia. BONE MARROW BIOPSY
AFTER BIOPSY
Uses large special needle
Your recovery period will depend a lot on the type of Skin may be punctured first with a surgical blade to
biopsy done. You might be able to go back to normal make a 3-4 mm incision (advanced to the marrow
activities as soon as the test is over. Or you may need to cavity)
rest at home for some time or stay in the hospital to begin Patient will feel pressure pressure but not pain
your recovery. If your anesthesia includes a sedative, you
need someone to drive you home afterwards. COMPLICATIONS OF BONE MARROW ASPIRATION OR
Talk with your doctor or nurse about how you should take BIOPSY
care of the biopsy area during your recovery. Contact
your doctor’s office if you experience: Bleeding — increased if px platelet count is LOW
o Redness or swelling in the area where the Infection
biopsy was done
o Severe pain AFTER THE BIOPSY
o Fever
o Bleeding After marrow sample is obtained, pressure is
applied to site for several minutes
Site will be covered with sterile dressing
BSN3A | PBL GROUP 1 7
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
Most patients have no discomfort but site of biopsy Note: Tumors appear as a white-grey mass on x-
may ache for 1 to 2 days ray
o Management: warm tub baths and mild
analgesic agent BEFORE CHEST X-RAY
o Do not use aspirin-containing analgesic
agent — may increase risk of bleeding Wear loose and comfortable clothing that does not
o Do not perform rigorous activity or exercise contain metal
Do not wear jewelry.
Ask the radiologist for specific instructions regarding
body piercings.
DURING CHEST X-RAY
change into a medical gown
remove all metal, such as eyeglasses, jewelry or
hairpins
You stand with your chest against the metal plate of
the X-ray machine and your hands on your hips.
This position produces an image of the front of your
chest.
You stand with your side against the metal plate of
the X-ray machine and your arms in the air. This
position creates an image of the side of your chest.
During the chest X-ray, you need to remain very still
and hold your breath. Any movement, even
breathing in and out, can blur the X-ray image.
CBC
for 1 to 2 days A complete blood count (CBC) is a common medical test
that your doctor may recommend to monitor your health.
CHEST RADIOGRAPH In cancer care, this blood test can be used to help
diagnose a cancer or monitor how cancer or its treatment
obtained to determine the size, contour, and is affecting your body. For example, people undergoing
position of the heart, lungs, bronchi, aorta, chemotherapy often receive regular CBCs.
pulmonary arteries, mediastinum, bones of your may be used to evaluate for the presence of anemia.
chest Assessment of tumor markers (blood analysis for antigens
reveals cardiac and pericardial calcifications and indicative of cancer), such as carcinoembryonic antigen
demonstrates physiologic alterations in the (CEA), carbohydrate antigen (CA 19-9), and CA 50 are
pulmonary circulation. monitored to determine the effectiveness of treatment(s)
often the first imaging test a doctor will order if lung Help diagnose some blood cancers, such as leukemia and
or heart disease is suspected lymphoma.
white or gray area: absorbed more radiation (e.g., Helps find out if cancer has spread to bone marrow.
white — bones; gray — lungs)
black: absorbed less radiation (e.g. gases In lungs) HOW IS CBC PERFORMED?
CHEST X-RAY IN DIAGNOSING LUNG CANCERS First, your doctor will order the CBC test be done as
part of your medical care. Then, your blood will be
poor tool in diagnosing lung cancer since tumors drawn for a blood sample. Sometimes you will need
are also seen during advanced stages to avoid eating or taking certain medications before
advanced lung cancer(stage 3b or 4) — more getting a CBC to get the most accurate results. Your
difficult to treat health care provider will let you know if this is the case.
Lung Nodule: spot is 3cm or approx 1.5 inches or After your blood is drawn, the sample is sent to a
less in dm laboratory for analysis. Your health care provider will
Lung mass: spot greater than 3cm let you the results, such as through a phone call or
Lung neoplasm: new growth in the lungs your online patient portal.
Lung lesion: any abnormalities
BSN3A | PBL GROUP 1 8
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
WHAT DO CBC RESULTS MEAN? HOW DOES MRI WORK?
Low white blood cell count. Some cancer An MRI scanner is a long cylinder or tube that holds a
treatments, mainly chemotherapy, can lower your large, very strong magnet. You lie on a table that
white blood cell count. slides into the tube, and the machine surrounds you
Cancers that affect the blood can also lower white with a powerful magnetic field. The machine uses a
blood cell count. These types of cancers include powerful magnetic force and a burst of radiofrequency
leukemia, lymphoma, and multiple myeloma. waves to pick up signals from the nuclei (centers) of
High and low results in the white blood cell hydrogen atoms in your body. A computer converts
differential. Having results that show higher or lower these signals them into a black and white picture.
than normal numbers of certain white blood cells can Contrast materials can be put into the body through a
mean different things. vein to make the images clearer. Once absorbed by
Higher-than-normal numbers of lymphocytes or the body, the contrast speeds up the rate at which
monocytes can indicate the possibility of certain types tissue responds to the magnetic and radio waves. The
of cancer. Some cancers and their treatment may stronger signals give clearer pictures.
cause low numbers of neutrophils, a condition
PAIN CONTROL
called neutropenia. Neutropenia can increase your
chance of a bacterial infection. Not everyone with cancer has cancer pain, but some
Low red blood cell count. Some cancer treatments, do. If you have cancer that's spread or recurred, your
such as chemotherapy and radiation therapy, can chance of having pain is higher.
lower your red blood cell count. This condition is
known as anemia. Cancer pain takes many forms. It can be dull, achy,
Low platelet count. Some cancer treatments, such sharp or burning. It can be constant, intermittent,
as chemotherapy or radiation therapy, can lower mild, moderate or severe. How much pain you feel
platelet count. Cancers that affect the bone marrow depends on a number of factors, including the type
can also lower the platelet count. of cancer you have, how advanced it is, where it's
situated and your pain tolerance.
MRI
Most cancer pain is manageable, and controlling
your pain is an essential part of your treatment.
MRI (also known as magnetic resonance
imaging, magnetic resonance, MR, and nuclear magnetic CAUSES CANCER PAIN
resonance [NMR] imaging) helps doctors find cancer in the
body and look for signs that it has spread. MRI also can Pain can be caused by the cancer itself. Pain could
help doctors plan cancer treatment, like surgery or happen if the cancer grows into or destroys nearby
radiation. MRI is painless and you don’t have to do tissue. As a tumor grows, it can press on nerves,
anything special to get ready for this test. bones or organs. The tumor can also release
chemicals that can cause pain.
WHAT DOES MRI SHOW?
Treatment of the cancer can help the pain in these
MRI creates cross-section pictures of your insides. But situations. However, cancer treatments, including
MRI uses strong magnets to make the images – not surgery, radiation and chemotherapy, also can cause
radiation. An MRI scan takes cross-sectional slices (views) pain.
from many angles, as if someone were looking at a slice
of your body from the front, from the side, or from above SYMPTOMS
your head. MRI creates pictures of soft tissue parts of the
Signs and symptoms caused by cancer will vary depending on
body that are sometimes hard to see using other imaging what part of the body is affected.
tests.
MRI is very good at finding and pinpointing some cancers.
An MRI with contrast dye is the best way to see brain and Some general signs and symptoms associated with, but not
spinal cord tumors. Using MRI, doctors can sometimes tell specific to, cancer, include:
if a tumor is or isn’t cancer.
MRI can also be used to look for signs that cancer may Fatigue
have metastasized (spread) from where it started to Lump or area of thickening that can be felt under the
another part of the body. skin
MRI images can also help doctors plan treatment such as Weight changes, including unintended loss or gain
surgery or radiation therapy. Skin changes, such as yellowing, darkening or
redness of the skin, sores that won't heal, or changes
to existing moles
Changes in bowel or bladder habits
Persistent cough or trouble breathing
BSN3A | PBL GROUP 1 9
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
Difficulty swallowing INTERVENTIONS
Hoarseness A number of treatments are available for cancer pain.
Persistent indigestion or discomfort after eating Your options may depend on what's causing your
Persistent, unexplained muscle or joint pain cancer pain and the intensity of the pain you're
Persistent, unexplained fevers or night sweats feeling. You may need a combination of pain
Unexplained bleeding or bruising treatments to find the most relief.
CAUSES Options include:
Cancer is caused by changes (mutations) to the DNA Over-the-counter pain relievers. For mild and
within cells. The DNA inside a cell is packaged into a moderate levels of pain, pain relievers that don't
large number of individual genes, each of which require a prescription may help. Examples include
contains a set of instructions telling the cell what aspirin, acetaminophen (Tylenol, others) and
functions to perform, as well as how to grow and ibuprofen (Advil, Motrin IB, others).
divide. Errors in the instructions can cause the cell to Medications derived from opium
stop its normal function and may allow a cell to (opioids). Opioids are prescription medications
become cancerous. used to treat moderate to severe pain. Examples of
A gene mutation can instruct a healthy cell to: opioids include morphine (Kadian, Ms Contin, others)
and oxycodone (Oxycontin, Roxicodone, others).
Allow rapid growth. A gene mutation can tell a cell Some opioids are short-acting medicines, so pain relief comes
to grow and divide more rapidly. This creates many quickly but you may need to take them more often. Other
new cells that all have that same mutation. opioid drugs are long-acting medicines, so pain relief takes
Fail to stop uncontrolled cell growth. Normal cells longer but the medicine doesn't need to be taken as often.
know when to stop growing so that you have just the Sometimes short-acting and long-acting opioids are used
right number of each type of cell. Cancer cells lose together.
the controls (tumor suppressor genes) that tell them
when to stop growing. A mutation in a tumor Other prescription medicines. Other types of
suppressor gene allows cancer cells to continue medicine can help relieve pain, including
growing and accumulating. antidepressants, anti-seizure drugs and steroids.
Make mistakes when repairing DNA errors. DNA Procedures to block pain signals. A nerve block
repair genes look for errors in a cell's DNA and make procedure can be used to stop pain signals from
corrections. A mutation in a DNA repair gene may being sent to the brain. In this procedure, a numbing
mean that other errors aren't corrected, leading cells medicine is injected around or into a nerve.
to become cancerous. Integrative therapies. Some people find some pain
relief through acupuncture, massage, physical
These mutations are the most common ones found in cancer. therapy, relaxation exercises, meditation and
But many other gene mutations can contribute to causing hypnosis.
cancer.
Other treatments may be available for your particular
situation. In some places, it may be legal to use medical
CAUSES GENE MUTATION marijuana for cancer pain.
Gene mutations can occur for several reasons, for instance: All pain medicines have side effects. Work with your
doctor to understand the benefits and risks of each pain
treatment and how to manage the side effects. Together
Gene mutations you're born with. You may be
you can decide which treatments may be best for you.
born with a genetic mutation that you inherited from
your parents. This type of mutation accounts for a
small percentage of cancers.
Gene mutations that occur after birth. Most gene CHEMOTHERAPY
mutations occur after you're born and aren't
inherited. A number of forces can cause gene
mutations, such as smoking, radiation, viruses,
DESCRIPTION AND CLASSIFICATION
cancer-causing chemicals (carcinogens), obesity,
hormones, chronic inflammation and a lack of
Chemotherapy is a type of cancer treatment that uses
exercise.
drugs to destroy cancer cells. The drugs work by stopping
Gene mutations occur frequently during normal cell
or slowing the growth of cancer cells, which can help to
growth. However, cells contain a mechanism that
recognizes when a mistake occurs and repairs the shrink tumors or prevent them from spreading to other
mistake. Occasionally, a mistake is missed. This parts of the body. Chemotherapy can be used alone or in
could cause a cell to become cancerous. combination with other treatments such as surgery or
radiation therapy. Chemotherapy drugs work by targeting
rapidly dividing cells, which includes cancer cells.
BSN3A | PBL GROUP 1 10
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
However, they can also affect healthy cells in the body leukemia and multiple myeloma and examples
that divide rapidly, such as those in the bone marrow, hair include prednisone, methylprednisolone and
follicles, and digestive tract. dexamethasone.
One of the most common side effects of chemotherapy is o Mitotic inhibitors: These drugs prevent the mitotic
nausea and vomiting, which can be managed with anti- spindle from forming during cell division, which can
nausea medications. Hair loss is another common side lead to cell death. Mitotic inhibitors include drugs like
effect, but it is usually temporary and hair will usually grow paclitaxel, docetaxel, and vinblastine.
back after treatment has ended. Chemotherapy can also o Hormone therapy: This type of chemotherapy is
weaken the immune system, making patients more used to treat hormone-dependent cancers like breast
susceptible to infections. Patients may need to take and prostate cancer. Hormone therapy drugs block
precautions to avoid exposure to infectious agents and the production or activity of hormones that promote
may require antibiotics or antifungal medications to cancer growth, such as estrogen or testosterone.
prevent or treat infections. Examples of hormone therapy drugs include
Another important consideration in chemotherapy tamoxifen, anastrozole, and leuprolide.
treatment is the timing and dosage of the drugs. o Immunomodulators: These drugs help stimulate
Chemotherapy is usually administered in cycles, with the immune system to attack cancer cells. Examples
each cycle consisting of a period of treatment followed by of immunomodulators include interferon, interleukin-
a period of rest. The length of each cycle and the number 2, and monoclonal antibodies.
of cycles will depend on the type and stage of cancer
GENERAL NURSING RESPONSIBILITIES
being treated, as well as the patient's overall health and
tolerance for chemotherapy. In addition to traditional Chemotherapy is a common cancer treatment that
chemotherapy drugs, there are also targeted therapies involves the use of drugs to destroy cancer cells. As a
that are designed to target specific molecules or nurse, it is important to understand the general nursing
pathways involved in cancer growth. These therapies can responsibilities related to chemotherapy administration to
be more effective and have fewer side effects than ensure patient safety and optimal treatment outcomes.
traditional chemotherapy, but they are often more Here are some of the general nursing responsibilities
expensive and may only be effective for certain types of related to chemotherapy:
cancer. Preparing the patient for chemotherapy: Before the
Chemotherapy drugs can be classified into several patient undergoes chemotherapy, the nurse should
different categories based on their mode of action and the perform a thorough assessment of their physical and
types of cancer they are used to treat: emotional status. The assessment should include a
o Alkylating agents: These drugs work by attaching review of the patient's medical history, current
alkyl groups to DNA strands, which makes it difficult medications, and any allergies or prior reactions to
for cancer cells to divide and grow. Examples of chemotherapy drugs. The nurse should also obtain
alkylating agents include cyclophosphamide, informed consent from the patient and educate them on
cisplatin, and carmustine. the treatment plan, including the benefits and potential
o Antimetabolites: These drugs interfere with the risks. It is important to provide the patient with clear and
synthesis of nucleic acids, which are essential for cell concise information to ensure that they fully understand
division. Antimetabolites include drugs like the treatment plan and can make informed decisions.
methotrexate, 5-fluorouracil, and gemcitabine. Monitoring the patient during chemotherapy:
o Anthracyclines: These drugs work by interfering Chemotherapy drugs can have significant effects on the
with the DNA of cancer cells and preventing them body, including changes in blood pressure, heart rate,
from dividing and growing. Examples include and oxygen saturation. Therefore, it is essential that the
doxorubicin and epirubicin. nurse monitor the patient's vital signs throughout the
o Topoisomerase inhibitors: These drugs prevent
chemotherapy administration process. The nurse should
DNA from unwinding and replicating, which can also be alert for any signs of allergic reactions, such as
cause cancer cells to die. Topoisomerase inhibitors itching, hives, or difficulty breathing, and respond
include drugs like etoposide, irinotecan, and promptly if these occur.
topotecan.
Administering chemotherapy drugs: The nurse should
o Plant alkaloids: Also called mitotic inhibitors, these
follow the prescribed chemotherapy protocol, which
drugs interrupt the M phase of the cell cycle and
includes the correct dosage, timing, and administration
inhibit mitosis. They are used to treat breast and lung
route. Chemotherapy drugs can be administered through
cancers and myeloma, lymphoma, and leukemia.
various routes, including intravenous (IV), intramuscular
Examples of drugs in this class include taxanes such
(IM), and oral. The nurse should be familiar with the
as paclitaxel and docetaxel, vinca alkaloids such as
different administration routes and know how to prepare
vinblastine, vincristine and vinorelbine.
the chemotherapy drugs properly to ensure their efficacy
o Corticosteroids: This drug class includes naturally
and minimize the risk of contamination.
occurring hormones such as the steroid hormones as
Managing chemotherapy side effects: Chemotherapy
well as artificially synthesized analogues of these
can cause a range of side effects, including nausea,
hormones. They are used to treat lymphoma,
BSN3A | PBL GROUP 1 11
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
vomiting, fatigue, hair loss, and anemia. The nurse should WHAT ARE THE GOALS OF RADIATION THERAPY?
educate the patient on the potential side effects of
chemotherapy and provide supportive care to help The goals of radiation therapy depend on your type of cancer
alleviate these symptoms. This may include administering and if and how far it has spread. Radiation therapy can be
anti-nausea medication, providing hydration therapy, and given alone or as a part of a treatment plan that includes
managing pain. It is important to monitor the patient's different treatments. Some of the ways radiation therapy is
response to the supportive care and adjust the treatment used include:
plan as needed.
As the primary treatment. Often, the goal of radiation
Monitoring and managing complications:
therapy is to get rid of all the cancer and keep it from
Chemotherapy can also cause complications such as
coming back.
infections, bleeding, or changes in blood counts. The
nurse should monitor the patient for any signs of Before other treatments. Radiation therapy can be
complications and take appropriate measures to manage given before other treatments, such as surgery, to
them. For example, if the patient develops an infection, shrink a large tumor. This is called "neoadjuvant
the nurse should administer antibiotics and monitor the radiation therapy."
patient closely for any changes in their condition. After other treatments. Radiation therapy can be
Documenting chemotherapy administration and given after other kinds of treatments to destroy any
patient response: The nurse should document the remaining cancer cells. This is called "adjuvant
chemotherapy administration details, including the drug radiation therapy."
name, dose, route of administration, and patient To relieve symptoms. Radiation therapy can be used
response. Documentation is essential for ensuring that to relieve the signs and symptoms of cancer. This is
the patient receives the correct chemotherapy dose and called "palliative radiation therapy."
for tracking the patient's response to treatment. The nurse
TELETHERAPY
should also report any adverse effects or complications
to the healthcare team to ensure that appropriate
Is the most common type of radiation used in the
measures are taken.
treatment of cancer. This type of radiation uses an
Ensuring safety measures: Chemotherapy drugs are external machine away from the body to direct
potent medications that can be hazardous to healthcare radiation towards the area of the body affected by
providers if not handled properly. Therefore, the nurse cancer
should follow safety measures, such as wearing personal
It is a treatment option for patients with low-risk
protective equipment, handling chemotherapy drugs with
prostate cancer; progression-free survival is similar
caution, and disposing of waste materials properly. It is
to that of low-risk patients treated with radical
also important to educate the patient and their family
prostatectomy.
members on safety measures to minimize the risk of
is prescribed by the radiation oncologist for a total
exposure to chemotherapy drugs.
dose over a certain time frame—for example, 28
treatments over 5½ weeks.
In summary, nursing responsibilities related to
chemotherapy involve preparing the patient for treatment, The different types of external-beam radiation therapy
administering chemotherapy drugs, monitoring the are:
patient for complications, managing side effects,
documenting treatment details, and ensuring safety Three-dimensional conformal radiation therapy
measures. By providing safe and effective care, nurses (3D-CRT) – During this type of radiation therapy,
can help improve treatment outcomes and enhance the detailed 3-dimensional pictures of the cancer are
patient's quality of life during cancer treatment. created from computed tomography (CT) or
magnetic resonance imaging (MRI) scans.
RADIATION THERAPY Intensity modulated radiation therapy (IMRT) –
this is a more complex form of radiation therapy. With
IMRT, the intensity of the radiation is varied. This is
DESCRIPTION AND CLASSIFICATION different than conventional 3D-CRT, which uses the
same intensity with each beam. IMRT targets the
Radiation therapy is a cancer treatment that uses tumor and avoids healthy tissue better than
high-energy x-ray or other particles to destroy cancer conventional 3D-CRT.
cells. A doctor who specializes in giving radiation Proton beam therapy – this treatment uses protons
therapy to treat cancer is called a radiation rather than x-rays. Proton therapy is a relatively new
oncologist. treatment that requires special equipment. It is
Radiation therapy can treat many different types of currently only used to treat certain types of cancer.
cancer. It can also be used in combination with other Learn more about proton therapy.
cancer treatments, such as chemotherapy and/or Image-guided radiation therapy (IGRT) – IGRT
surgery. uses imaging during radiation treatment. Images are
BSN3A | PBL GROUP 1 12
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
taken right before and during treatment and radiation. Other skin reactions, referred to as
compared to imaging taken before treatment began. radiodermatitis, occur along a continuum ranging
This helps doctors position the radiation as precisely from erythema and dry desquamation (flaking of
as possible. skin) to moist or wet desquamation (dermis exposed,
Stereotactic radiation therapy (SRT) – this skin oozing serous fluid) to, potentially, ulceration.
treatment delivers a large, precise dose to a small Factors that contribute to the severity of
tumor area. The patient must remain very still. A radiodermatitis include the dose and form of
head frame or individual body molds help limit radiation; use of concurrent chemotherapy,
movement. SRT is often given as a single treatment immunotherapy, or targeted therapy; inclusion of skin
or in fewer than 10 treatments. Some people may folds in the irradiated area; increased age, poor
need more than one course of SRT. nutritional status, chronic sun exposure, current
smoking status, and the presence of medical
comorbidities, such as diabetes or kidney failure.
BRACHYTHERAPY NURSING MANAGEMENT
Is the placement of radioactive sources within or — Nurses anticipate, prevent, and work collaboratively
immediately next to the cancer site in order to with other providers to manage symptoms
provide a highly targeted, intense dose of radiation associated with radiation therapy in order to promote
beyond a dose that is usually provided by EBRT. healing, patient comfort, and quality of life.
This form of radiation delivery helps to spare Symptoms that are not appropriately managed may
exposure to normal surrounding tissue. The radiation lead to poor outcomes as a result of interruptions,
source can be implanted by means of needles or decreased doses, or early cessation of treatment.
rods, seeds, beads, ribbons, or catheters placed into — In particular, advanced age, elevated radiation dose,
body cavities (vagina, abdomen, pleura), lumens and BMI have been associated with greater toxicity
within organs, or interstitial tissue compartments and symptoms.
(breast, prostate). Multiple imaging techniques such — The nature of the relationship between body mass
as ultrasound, CT, or MRI are used to guide index (BMI) and radiation toxicities is less clear. For
placement of radiation sources. example, a decreased BMI was found to be
May be delivered as a temporary or a permanent associated with an increased incidence of toxicities
implant. Temporary applications are delivered as in women with cervical cancer; whereas, an
high-dose radiation (HDR) for short periods of time, increased BMI (obesity) was associated with
while low-dose radiation (LDR) is delivered over a increased incidence of late toxicities in men being
more extended period. treated for prostate cancer. Consequently, the area
of the body being irradiated must be used as the
o ADVANTAGE OF HDR BRACHYTHERAPY focus of nursing assessments of radiation toxicities.
– Treatment time is shorter. — In patients receiving EBRT, the nurse assesses the
– There is reduced exposure to personnel. patient’s skin, nutritional status, and general feelings
– The procedure can be performed on an of well-being throughout the course of treatment.
outpatient basis over several days. — If systemic symptoms such as fatigue occur the
– Can be used for intraluminal, surface, interstitial, nurse explains that these symptoms are a result of
and intracavitary lesions. the treatment and do not represent deterioration or
progression of the disease. The nurse should
TOXICITY recommend evidence-based interventions for the
management of fatigue, which should include
Unfavorable and unintended sign, symptom, or aerobic exercise, which is most effective when
condition associated with cancer treatment. adherence is high.
Toxicities associated with radiation therapy are most
often localized in the region being irradiated and may
PROTECTING CAREGIVERS
be increased if concomitant chemotherapy is given.
Acute or early toxicities most often begin within 2 — Patients receiving internal radiation emit radiation
while the implant is in place; therefore, contact with
weeks of the initiation of treatment and occur when
the health care team is guided by principles of time,
normal cells within the treatment area are damaged
distance, and shielding to minimize exposure of
and cellular death exceeds regeneration. Body
personnel to radiation.
tissues most affected are those that normally
— Specific instructions are provided by the radiation
proliferate rapidly, such as the skin, the epithelial
safety officer from the radiology department and
lining of the gastrointestinal tract, and the bone
specify the maximum time that can be spent safely in
marrow.
the patient’s room, the shielding equipment to be
Altered skin integrity is common and can include
used, and special precautions and actions to be
alopecia (hair loss) associated with whole brain
taken if the implant is dislodged.
BSN3A | PBL GROUP 1 13
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
— Safety precautions used in caring for a patient procedures are followed and all necessary safety
receiving brachytherapy include assigning the measures are in place.
patient to a private room, posting appropriate notices — Nurses handle and dispose of radioactive
about radiation safety precautions, having staff sources used in brachytherapy, which require
members wear dosimeter badges, making sure that careful handling to prevent radiation exposure. They
pregnant staff members are not assigned to the must be trained in handling and disposing of
radioactive materials to ensure the safety of the
patient’s care, prohibiting visits by children or
patient and the healthcare team.
pregnant visitors, limiting visits from others to 30
— Nurses implement safety measures to protect the
minutes daily, and seeing that visitors maintain a 6- patient and healthcare team during the
foot distance from the radiation source. brachytherapy procedure. This includes wearing
— Patients with seed implants typically return home; protective equipment such as lead aprons and
radiation exposure to others is minimal. gloves, as well as implementing procedures to
— Information about any precautions, if needed, is ensure the safe transport of radioactive sources and
provided to the patient and family members to ensure equipment.
safety.
— Depending on the dose and energy emitted by a COMMON CELLULAR ABERRATIONS
systemic radionuclide, patients may or may not
require special precautions or hospitalization. The
nurse should explain the rationale for these
BREAST CANCER
precautions to keep the patient from feeling unduly
isolated. Breast cancer happens when cells in your breast
GENERAL NURSING RESPONSIBILITIES grow and divide in an uncontrolled way, creating a
mass of tissue called a tumor.
Breast cancer is a major health problem in the United
— Patient education: The oncology nurse coordinator
States. Current statistics indicate tha tover a lifetime
educates patients about brachytherapy and what to
(birth to death), a woman’s risk of developing breast
expect during the treatment process. This may
include information about the procedure, potential cancer is about 12%, or one in eight.
side effects, and self-care instructions. Risk of developing breast cancer increases with
— Treatment planning: The nurse coordinator works increasing age. About two of three invasive breast
closely with the radiation oncologist to plan the cancers are found in women 55 years or older. About
brachytherapy treatment, including selecting 5% to 10% of breast cancer cases are thought to be
appropriate radioactive sources and determining the hereditary, resulting directly from gene defects (cell
length and frequency of treatment. mutations) inherited from a biologic parent.
— Coordination of care: The nurse coordinator
coordinates care for the patient, including scheduling TYPES OF BREAST CANCER
appointments, patient assessment and arranging for
any necessary tests or procedures as part of the
cancer care. They may also collaborate with other DUCTAL CARCINOMA IN SITU (DCIS)
healthcare providers, such as radiation therapists
and oncology nurses, to ensure a seamless patient It is characterized by the proliferation of malignant
experience. cells inside the milk ducts without invasion into the
— Support for patients and families: The nurse surrounding tissue.
coordinator provides emotional support to patients Unlike invasive breast cancer, DCIS does not
and their families throughout the cancer treatments, metastasize and a woman generally does not die of
helping them to cope with the stress and uncertainty DCIS unless it develops into invasive breast cancer.
of a cancer diagnosis. DCIS can develop into invasive breast cancer if left
— Follow-up care: The nurse coordinator helps to untreated.
ensure that patients receive appropriate follow-up
care after the brachytherapy treatment is complete, INFILTRATING DUCTAL CARCINOMA
including monitoring for any potential side effects and
70% tp 80% of all cases.
scheduling any necessary imaging or tests.
The most common histologic type of breast cancer.
The tumors arise from the duct system and invade
RADIATION SAFETY the surrounding tissues.
They often form a solid irregular mass in the breast.
— Nurses monitor the patient's exposure to
radiation during the brachytherapy procedure. This Micropapillary invasive ductal carcinoma is a rare
includes calculating the dose of radiation the patient type of aggressive ductal cancer characterized by a
will receive and monitoring the equipment to ensure high rate of axillary node metastasis and skin
the correct amount of radiation is delivered to the involvement.
tumor site. They also work with radiation physicists
and radiation safety officers to ensure the correct INFILTRATING LOBULAR CARCINOMA
BSN3A | PBL GROUP 1 14
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
10% to 15% of breast cancers. RISK FACTORS
The tumors arise from the lobular epithelium and
typically occur as an area of ill-defined thickening in Genetic mutation
the breast. Increasing age
They are often multicentric and can be bilateral. Personal history
Family history
MEDULLARY CARCINOMA Early menarche
Less than 1% of breast cancers and it tends to be Late menopause
diagnosed more often in women younger than 50 Obesity
years. High-fat diet
Alcohol intake
The tumors grow in a capsule inside a duct. They can
become large and may be mistaken for a PREVENTIVE STRATEGIES
fibroadenoma.
The prognosis is often favorable. Long-term Surveillance
Chemoprevention
MUCINOUS CARCINOMA Prophylactic Masectomy
2% of breast cancers and often presents in women
who are postmenopausal and are 75 years and
CLINICAL MANIFESTATIONS
older.
A mucin producer, the tumor is also slow growing; Lesions
thus, the prognosis is more favorable than in many Breast pain
other types.
Skin dimpling
Nipple retractions
TUBULAR CARCINOMA
1% to 5% of breast cancers. Skin ulceration
Because axillary metastases are uncommon with this
histology, prognosis is usually excellent. ASSESSMENT AND DIAGNOSTIC FINDINGS
INFLAMMATORY CARCINOMA Staging
Inflammatory carcinoma is a rare (1% to 5%) and Involves classifying the cancer by the extent of the
aggressive type of breast cancer that has unique disease in the body.
symptoms. It is based on whether the cancer is invasive or
The cancer is characterized by diffuse edema and noninvasive, the size of the tumor, how many lymph
erythema of the skin, often referred to as peau nodes are involved, and if it has spread to other parts
d’orange. of the body.
This is caused by malignant cells blocking the lymph The stage of a cancer is one of the most important
channels in the skin. factors in determining prognosis and treatment
An associated mass may or may not be present; if options.
there is a mass, it is often a large area of indiscrete Other diagnostic tests may be performed before or
thickening. after surgery to help in the staging of the disease.
Inflammatory carcinoma can be confused with an The extent of testing often depends on the clinical
infection because of its presentation. presentation of the disease and may include chest
The disease can spread to other parts of the body x-rays, computed tomography (CT) scan, MRI
rapidly. scan, positron emission tomography (PET) scan,
Chemotherapy often plays an initial role in controlling bone scans, and blood work (complete blood
disease progression, but radiation and surgery may count, comprehensive metabolic panel, and
also follow. tumor markers.
Prognosis
PAGET DISEASE
In general, the smaller the tumor appears, the better
1% to 4% of diagnosed cases of breast cancer; it is
the prognosis.
more common in men than in women.
A tumor starts with a genetic alteration in a single cell
Symptoms typically include a scaly, erythematous,
and takes time to divide and double in size.
pruritic lesion of the nipple.
A carcinoma may double in size 30 times to become
Paget disease often represents DCIS of the nipple
1 cm or larger, at which point it becomes clinically
but may have an invasive component.
apparent.
If no lump can be felt in the breast tissue and the
Prognosis also depends on the extent of spread of
biopsy shows DCIS without invasion, the prognosis
the breast cancer.
is very favorable.
BSN3A | PBL GROUP 1 15
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
The most common route of regional spread is to the LUNG CANCER
axillary lymph nodes.
Other sites of lymphatic spread include the internal Lung cancer is cancer that forms in tissues of the
mammary and supraclavicular nodes. lung, usually in the cells that line the air passages.
It is the leading cause of cancer death in both men
and women.
It is the leading cancer killer among men and women
in the United States, with about 1 out of 4 cancer
deaths from lung cancer; over 135,000 deaths were
estimated in 2018.
PATHOPHYSIOLOGY
The most common cause of lung cancer is inhaled
carcinogens, most often cigarette smoke (>85%);
other carcinogens include radon gas and
occupational and environmental agents.
Lung cancers arise from a single transformed
epithelial cell in the tracheobronchial airways, in
which the carcinogen binds to and damages the
cell’s DNA.
This damage results in cellular changes, abnormal
SURGICAL MANAGEMENT cell growth, and eventually a malignant cell.
As the damaged DNA is passed on to daughter cells,
Modified Radical Mastectomy the DNA undergoes further changes and becomes
Total Mastectomy unstable.
Breast Conservation Treatment With the accumulation of genetic changes, the
Sentinel Lymph Node Biopsy pulmonary epithelium undergoes malignant
NURSING MANAGEMENT transformation from normal epithelium eventually to
invasive carcinoma.
Patients who undergo SLNB in conjunction with Carcinoma tends to arise at sites of previous scarring
breast conservation treatments are generally in the lung.
discharged the same day.
Patients who undergo SLNB with total mastectomy RISK FACTORS
usually stay in the hospital overnight, possibly longer
if breast reconstruction is being performed. Tobacco smoke
The patient must be informed that although frozen- Electronic Nicotine Delivery Systems
section analysis is highly accurate, falsenegative Secondhand Smoke
results can occur. Environmental and Occupational Exposure
A negative sentinel lymph node on frozen-section Genetic Mutations
analysis may show metastatic disease on
subsequent analysis, indicating that ALND is still CLINICAL MANIFESTATIONS
necessary.
The patient should also be reassured that the Chronic cough
radioisotope and blue dye are generally safe. Dyspnea
The nurse informs patients that they may notice a Lung parenchyma
blue-green discoloration in the urine or stool for the
Pleural effusion,
first 24 hours as the blue dye is excreted.
Pneumonia
The incidence of lymphedema, decreased arm
mobility, and seroma formation (collection of serous Hemoptysis
fluid) in the axilla is generally low, but the patient Chest or shoulder pain
should be prepared for these possibilities. Fever
Women who have SLNB alone have neuropathic Dysphagia
sensations similar to those who undergo ALND, Head and neck edema
although the prevalence and severity of these Weakness
sensations and the resulting distress are lower with Anorexia
SLNB. Weight loss
BSN3A | PBL GROUP 1 16
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
blebs or bullae, benign tumors, metastatic malignant
tumors, bronchiectasis, and fungal infections.
ASSESSMENT AND DIAGNOSTIC FINDINGS Pneumonectomy
Removal of an entire lung.
CT Scan
It is performed chiefly for cancer when the lesion
Chest x-ray cannot be removed by a less extensive procedure.
Fiberoptic bronchoscopy It also may be performed for lung abscesses,
Bone scans bronchiectasis, or extensive unilateral tuberculosis.
Abdominal scans The removal of the right lung is riskier than the
Positron Emission Tomography (PET) scan removal of the left, because the right lung has a
Liver ultrasound larger vascular bed and its removal imposes a
Magnetic resonance imaging (MRI) greater physiologic burden.
Mediastinoscopy A posterolateral or anterolateral thoracotomy incision
Endobronchial ultrasound biopsy is made, sometimes with resection of a rib.
The pulmonary artery and the pulmonary veins are
Endoscopy with esophageal ultrasound
ligated and severed.
The main bronchus is divided and the lung removed.
MEDICAL MANAGEMENT
The bronchial stump is stapled, and usually no drains
are used because the accumulation of fluid in the
Surgery
empty hemithorax prevents mediastinal shift.
Radiation and Laser therapy
Chemotherapy
Immunotherapy
Gene therapy
Endoscopic stent placement
SURGICAL MANAGEMENT
Thoracotomy
Creation of a surgical opening into the thoracic
cavity.
Surgery is primarily used for patients with NSCLC, NURSING MANAGEMENT
because SCLC grows rapidly and metastasizes early
and extensively. Patients are typically admitted on the day of surgery.
Surgical resection is the preferred method of treating The nurse in the outpatient surgical clinic setting is
patients with localized NSCLCs without evidence of responsible for performing the preoperative
metastatic spread, and with adequate assessment and education and for alleviating the
cardiopulmonary function. anxiety experienced by the patient and family
members by providing them with anticipatory
Lobectomy guidance.
Removal of a lobe of a lung. Postoperatively, the patient may be managed by the
Lobectomy, which is more common than nurse in the ICU.
pneumonectomy, may be carried out for Successfully managing transitions in care for the
bronchogenic carcinoma, giant emphysematous patient from the ICU to other inpatient acute care
settings (e.g., medical-surgical unit, step-down unit)
BSN3A | PBL GROUP 1 17
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
to the outpatient setting is a key nursing there's an area in a polyp or in the lining of the colon or
responsibility. rectum where the cells look abnormal, but they haven't
A reduction in lung capacity requires a period of become cancer.
physiologic adjustment, and fluids may be given at a
low hourly rate to prevent fluid overload and SIGNS AND SYMPTOMS
pulmonary edema.
A persistent change in your bowel habits, including
After the patient has recovered from anesthesia and
diarrhea or constipation or a change in the consistency of
the vital signs have stabilized, the head of the bed
your stool
may be elevated 30 to 45 degrees.
Rectal bleeding or blood in your stool
Careful positioning of the patient is important.
Persistent abdominal discomforts, such as cramps, gas,
COLON CANCER or pain
A feeling that your bowel doesn't empty completely
Colorectal cancer is a disease in which cells in the colon Weakness or fatigue
or rectum grow out of control. Sometimes it is called colon Unexplained weight loss
cancer, for short. The colon is the large intestine or large
bowel. The rectum is the passageway that connects the CAUSES
colon to the anus.
Sometimes abnormal growths, called polyps, form in the In colon cancer, cells lining your colon and rectum keep
colon or rectum. Over time, some polyps may turn into growing and dividing even when they’re supposed to die.
cancer. These cancerous cells may come from polyps in your
colon.
Medical researchers aren’t sure why some people
develop precancerous colon polyps that become colon
cancer. They do know certain risk factors increase
people’s chances of developing precancerous polyps and
colon cancer.
Inherited conditions, and lifestyle choices
RISK FACTORS
Smoking: Using tobacco products, including chewing
tobacco and e-cigarettes, increases your risk of
developing colon cancer.
Excessive alcohol use: In general, men and people
AMAB should limit beverages containing alcohol to two
servings a day. Women and people AFAB should limit
DIFFERENT TYPES OF POLYPS
beverages containing alcohol to one serving a day. Even
Adenomatous polyps (adenomas): These polyps light alcohol use can increase your risk of developing
sometimes change into cancer. Because of this, cancer.
adenomas are called a pre-cancerous condition. The 3 Having obesity: Eating high-fat, high-calorie foods may
types of adenomas are tubular, villous, and tubulovillous. affect your weight and increase your risk of colon cancer.
Hyperplastic polyps and inflammatory polyps: These Having a diet that includes lots of red meat and
polyps are more common, but in general they are not pre- processed meat: Processed meat includes bacon
cancerous. Some people with large (more than 1cm) sausage and lunchmeat. Healthcare providers
hyperplastic polyps might need colorectal cancer recommend you limit red meat and processed meat to
screening with colonoscopy more often. two servings a week.
Sessile serrated polyps (SSP) and traditional serrated Not exercising: Any kind of physical activity may reduce
adenomas (TSA): These polyps are often treated like your risk of developing colon cancer.
adenomas because they have a higher risk of colorectal
cancer. MEDICAL CONDITIONS THAT INCREASE COLON
Other factors that can make a polyp more likely to contain CANCER RISK
cancer or increase someone’s risk of developing colorectal
Inflammatory bowel disease: People who have
cancer include:
conditions like chronic ulcerative colitis and Crohn’s
If a polyp larger than 1 cm is found colitis, which cause inflammation in their colon lining, may
If more than 3 polyps are found have an increased risk of colon cancer. The risk
If dysplasia is seen in the polyp after it's removed. increases if you have inflammatory bowel disease that
Dysplasia is another precancerous condition. It means lasts more than seven years and affects large parts of
your colon.
BSN3A | PBL GROUP 1 18
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
Inherited conditions: Certain conditions like Lynch Guaiac-based fecal occult blood test (gFOBT): Like
syndrome and familial adenomatous polyposis may the FIT, this test looks for blood in poop that may not be
increase your risk of developing colon cancer. Colon visible.
cancer may happen if you inherit a gene that causes Fecal DNA test: This test looks for signs of genetic
cancer. mutations and blood products in your poop.
A family history of colon and other kinds of cancer: If Flexible sigmoidoscopy: Healthcare providers use a
a close family member has colon cancer, you may have flexible scope called a sigmoidoscope to see inside your
an increased risk of developing the condition. Close lower colon and rectum.
family members include your biological parents, siblings, Virtual colonoscopy: A virtual colonoscopy is an X-ray
and children. Your risk may be higher if any biological that looks for polyps, tumors and ulcers (sores) in your
family member developed colon cancer before age 45. colon and rectum.
A family history of polyps: If your parent, sibling, or
child has an advanced polyp, you may have an increased STAGES OF COLON CANCER
Stage 0: Healthcare providers may refer to this as
risk of getting colon cancer. An advanced polyp may be a carcinoma in situ. When they do, they’re talking about
large polyp. Medical pathologists may characterize a abnormal or precancerous cells in your mucosa, the
polyp as being advanced if they see certain changes in innermost layer of your colon wall.
the polyp when they look at it under a microscope that Stage I: Stage I colorectal cancer has grown into the wall
signs the polyp may contain cancerous cells. of your intestine but hasn’t spread beyond the muscular
Many polyps: People with numerous colon polyps — coat or into close lymph nodes.
including adenomas, serrated polyps, or other types of Stage II: The cancer has spread farther into the wall of
polyps — often have an increased risk of developing your intestine but hasn’t spread to nearby lymph nodes.
polyps and colon cancer. People may inherit a tendency There are three types of Stage II colon cancer:
toward having many colon polyps. o Stage IIA: Cancer has spread through most of your
colon wall but hasn’t grown into the wall’s outer
DIAGNOSIS AND TESTS layer.
o Stage IIB: Cancer has spread into the outer layer of
Healthcare providers use several tests to diagnose colon your colon wall or through the wall.
cancer. Those tests include: o Stage IIC: Cancer has spread to a nearby organ.
Stage III: In this stage, colon cancer has spread to your
Complete blood count (CBC).
lymph nodes. Like Stage II colon cancer, there are three
Comprehensive metabolic panel (CMP). sub-stages of Stage III colon cancer:
Carcinoembryonic antigen (CEA) assay: Cancer o Stage IIIA: There’s cancer in the first or second
cells and normal cells release CEA into your layers of your colon wall and it’s spread to one to
bloodstream. High CEA levels may be a sign of colon four lymph nodes.
cancer. o Stage IIIB: The cancer affects more layers of your
X-rays. colon wall but only affects one to three lymph
Computed tomography (CT) scan. nodes. Cancer that affects fewer colon wall layers
Magnetic resonance imaging (MRI) scan. but has spread to four or more lymph nodes is also
Positron emission tomography (PET) scan. a stage IIIB colon cancer.
Ultrasound. o Stage IIIC: There’s cancer in the outer layer or the
Biopsy. next outermost layer of your colon and in four or
more lymph nodes. Cancer that’s spread into a
THE DIFFERENCE BETWEEN A SCREENING TEST AND nearby organ and one or more lymph nodes is also
TESTS THAT DIAGNOSE COLON CANCER a stage IIIC colon cancer.
Stage IV: Cancer has spread (metastasized) to other
Cancer screening test: checks for cancer when you
areas of your body, such as your liver, lungs, or ovaries:
don’t have any signs or symptoms of cancer. If your
o Stage IVA: In this stage, cancer has spread to one
screening test shows abnormalities, a healthcare provider
organ or to lymph nodes that are farther or more
may recommend additional tests.
distant from your colon.
COMMON COLON CANCER SCREENING TESTS o Stage IVB: Cancer has moved to more than one
distant organ and more lymph nodes.
Colonoscopy is the most common screening test for o Stage IVC: Cancer affects distant organs, lymph
colon cancer. Other tests include: nodes and abdominal tissue.
Fecal immunochemical test (FIT): This test detects
MANAGEMENT AND TREATMENT
hidden blood in your poop. Medical pathologists test
samples of your poop for blood that you may not see just Polypectomy: This surgery removes cancerous polyps.
by looking.
BSN3A | PBL GROUP 1 19
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
Partial colectomy: This is also called colon resection Angiosarcoma, which starts in the blood vessels. This is
surgery. Surgeons remove the section of your colon that a rare type of liver cancer that is more likely to occur in
contains a tumor and some surrounding healthy tissue. people over 70.
They’ll reconnect healthy colon sections in a procedure Secondary cancer in the liver is cancer that started in
called anastomosis. another part of the body but has spread to the liver. If you
Surgical resection with colostomy: Like a colectomy, have secondary cancer in the liver, it may be useful to
surgeons remove the section of your colon that contains read information about primary cancer in conjunction with
a tumor. In this surgery, however, they can’t connect this information or about cancer of unknown primary. A
healthy colon sections. Instead, they do a colostomy. In a secondary cancer is named after the primary site where
colostomy, your bowel is moved to an opening in your it began, for example bowel cancer with liver secondaries.
abdominal wall so your poop is collected in a bag. In this information, we use the term "secondary cancer in
Radiofrequency ablation: This procedure uses heat to the liver" to refer to any cancer type that has spread to
destroy cancer cells. the liver.
Chemotherapy: Healthcare providers may use
chemotherapy drugs to shrink tumors and ease colon
cancer symptoms.
Targeted therapy: This treatment targets the genes,
proteins and tissues that help colon cancer cells grow and
multiply. Healthcare providers often use a type of targeted
therapy called monoclonal antibody therapy. This therapy
uses lab-created antibodies that attach to specific targets
on cancer cells or cells that help cancer cells grow. The
antibodies kill the cancer cells.
PREVENTION
Avoid tobacco. If you smoke and want help quitting, talk
to a healthcare provider about smoking cessation
programs.
Use moderation when you drink beverages
containing alcohol.
Maintain a healthy weight. SIGNS AND SYMPTOMS
Eat a healthy diet. Add fruit and vegetables to your diet
and cut back on red meat processed foods, and high-fat Losing weight without trying
and high-calorie foods. Drinking coffee may lower your Loss of appetite
risk of developing colon cancer. Upper abdominal pain
Keep track of your family medical history. Colon Nausea and vomiting
cancer can run in families. Tell your healthcare provider if General weakness and fatigue
your biological parents, siblings or children have colon
Abdominal swelling
cancer or an advanced polyp or if any of your family has
Yellow discoloration of your skin and the whites of your
cancer before age 45.
eyes (jaundice)
Follow colon cancer screening guidelines. Ask your
White, chalky stools
healthcare provider when you should have colon cancer
screening. If you have chronic irritable bowel disease or HOW DOES LIVER CANCER AFFECT THE BODY?
a family history of colon cancer, your healthcare provider
may recommend you start screening earlier than age 45. Collects and filters blood flowing from your intestines.
Processes and stores nutrients that your intestines
LIVER CANCER
absorb.
Primary liver cancer is a malignant tumor that begins in Changes some nutrients into energy or substances that
the liver. your body needs to build tissue.
Makes bile, a fluid that helps digest fat.
DIFFERENT TYPES OF LIVER CANCER Digests and stores other nutrients from food like sugar,
which makes energy.
Hepatocellular carcinoma (HCC) or hepatoma, is the Makes substances that help your blood to clot.
most common type of primary liver cancer and it starts in
the main cell type in the liver, the hepatocytes RISK FACTORS
Cholangiocarcinoma, or bile duct cancer, starts in the
cells lining the bile ducts (which connect the liver to the Chronic infection with HBV or HCV. Chronic infection with
bowel and gall bladder) the hepatitis B virus (HBV) or hepatitis C virus (HCV)
increases your risk of liver cancer.
BSN3A | PBL GROUP 1 20
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
Cirrhosis. This progressive and irreversible condition Stage II/early stage/stage A: You have a single tumor
causes scar tissue to form in your liver and increases your that measures 5 cm or less or you have more than one
chances of developing liver cancer. tumor that measures less than 3 cm. The tumor may have
Certain inherited liver diseases. Liver diseases that can spread to your blood vessels.
increase the risk of liver cancer include hemochromatosis Stage III/intermediate stage/stage B: In this stage, you
and Wilson's disease. may have more than one tumor and/or a tumor that
Diabetes. People with this blood sugar disorder have a measures more than 5 cm. The tumor may have spread
greater risk of liver cancer than those who don't have to your lymph nodes, large blood vessels or another
diabetes. organ.
Nonalcoholic fatty liver disease. An accumulation of fat in Stage IV/advanced stage/stage C: The cancer has
the liver increases the risk of liver cancer. spread to other places in your body, such as your lungs
Exposure to aflatoxins. Aflatoxins are poisons produced or bones, as well as lymph nodes.
by molds that grow on crops that are stored poorly. Crops,
such as grains and nuts, can become contaminated with
aflatoxins, which can end up in foods made of these MANAGEMENT AND TREATMENT
products.
Healthcare providers have several common treatments
Excessive alcohol consumption. Consuming more than a
for HCC and IHC, including surgery to remove part of your
moderate amount of alcohol daily over many years can
liver, liver transplantation, and liver-directed treatments
lead to irreversible liver damage and increase your risk of
like hepatic arterial embolization and ablation. They may
liver cancer.
also use several types of chemotherapy,
DIAGNOSIS AND TESTS chemoembolization, radiation therapy, radioembolization,
immunotherapy, and targeted therapy.
Blood tests: Healthcare providers may do blood tests for
SURGICAL MANAGEMENT
cancer, such as a liver function test, to check on liver
enzymes, proteins and other substances that show
Surgical resection is the treatment of choice when HCC
whether your liver is healthy or damaged. They may test
is confined to one lobe of the liver and the function of the
for alfa-fetoprotein (AFP). High AFP levels may indicate
remaining liver is considered adequate for postoperative
liver cancer.
recovery.
Ultrasound (sonography): This test provides pictures of
In the case of metastasis, hepatic resection can be
your soft tissue structures. Healthcare providers use
performed if the primary site can be completely excised
ultrasound to look for liver tumors.
and the metastasis is limited. However, metastases to the
Computed tomography (CT) scan: This special type of
liver are rarely limited or solitary. Capitalizing on the
X-ray takes detailed images of your liver, providing
regenerative capacity of the liver cells, some surgeons
information about liver tumor size and location.
have 3786 successfully removed 90% of the liver.
Magnetic resonance imaging (MRI): This test produces However, the presence of cirrhosis limits the ability of the
very clear images of your body using a large magnet, liver to regenerate.
radio waves and a computer. Laparoscopic liver resection for malignant tumors has
Angiogram: This test helps healthcare providers also been described. staging of liver tumors aids in
examine your liver’s blood vessels. During this test, your predicting the likelihood of surgical cure
healthcare provider injects dye into an artery so they can
In preparation for surgery, the patient’s nutritional, fluid,
track blood vessel activity and look for blockages.
and general physical status are assessed, and efforts are
Biopsy: Healthcare providers remove liver tissue to look undertaken to ensure the best physical condition
for signs of cancer. Biopsies are the most reliable way to possible. Extensive diagnostic studies may be performed.
confirm a liver cancer diagnosis. Specific studies may include liver scan, liver biopsy,
Endoscopic retrograde cholangiopancreatography cholangiography, selective hepatic angiography,
(ERCP): ERCP uses an endoscope and a catheter (thin, percutaneous needle biopsy, peritoneoscopy,
flexible tubes) to examine your bile ducts. laparoscopy, ultrasound, CT scan, PET scan, MRI, and
Percutaneous transhepatic cholangiography (PTC): blood tests, particularly determinations of serum alkaline
A PTC creates X-rays of your bile ducts like an ERCP. phosphatase, AST, and GGT and its isoenzymes.
Instead of an endoscope and catheter, your healthcare Lobectomy
provider delivers contrast dye by inserting a needle o Removal of a lobe of the liver is the most
directly into your bile ducts and liver. A PTC is usually only common surgical procedure for excising a
for people who can’t have an ERCP. liver tumor. If it is necessary to restrict blood
flow from the hepatic artery and portal vein
STAGES OF LIVER CANCER
for longer than 15 minutes, it is likely that
hypothermia will be used. For a right-liver
Stage I/very early stage/stage 0: You have a single
lobectomy or an extended right lobectomy
tumor in your liver that measures less than 2 centimeters
(including the medial left lobe), a
(cm). Blood tests show your bilirubin level is normal.
BSN3A | PBL GROUP 1 21
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
thoracoabdominal incision is used. An Cervical cancer begins when healthy cells in the cervix
extensive abdominal incision is made for a develop changes (mutations) in their DNA. A cell's DNA
left lobectomy contains the instructions that tell a cell what to do.
Local Ablation Healthy cells grow and multiply at a set rate, eventually
o In patients who are not candidates for dying at a set time. The mutations tell the cells to grow
resection or transplantation, ablation of and multiply out of control, and they don't die. The
HCC may be accomplished by chemicals accumulating abnormal cells form a mass (tumor).
such as ethanol or by physical means such Cancer cells invade nearby tissues and can break off
from a tumor to spread (metastasize) elsewhere in the
as radiofrequency ablation (most frequently
body.
used local ablative therapy) or microwave
It isn't clear what causes cervical cancer, but it's certain
coagulation. These techniques may be that HPV plays a role. HPV is very common, and most
performed under ultrasound or CT people with the virus never develop cancer. This means
guidance laparoscopically or other factors — such as your environment or your
percutaneously. Radiofrequency ablation is lifestyle choices — also determine whether you'll
becoming a standard mode of treatment; a develop cervical cancer.
tumor up to 5 cm in size can be destroyed
in one session. The most common
complications following ablation are local TYPES OF CERVICAL CANCER
pain or bleeding. Serious complications are
rare. Immunotherapy with interferon may be The type of cervical cancer that you have helps
used after surgical resection for HCC to determine your prognosis and treatment. The main
prevent the recurrence of the lesion in those types of cervical cancer are:
o Squamous cell carcinoma : this type of cervical
patients who have developed the lesion
cancer begins in the thin, flat cells (squamous cells)
related to hepatitis B or C. lining the outer part of the cervix, which projects
Liver Transplantation into the vagina. Most cervical cancers are
o Liver transplantation offers good patient squamous cell carcinomas.
outcomes. Candidates with liver cancer o Adenocarcinoma - this type of cervical cancer
meet stringent selection criteria, including begins in the column-shaped glandular cells that
having small, early-stage lesions. The Milan line the cervical canal.
criteria have been developed to limit Sometimes, both types of cells are involved in cervical
transplantation to patients who are most cancer. Very rarely, cancer occurs in other cells in the
likely to have better outcomes. cervix.
STAGES OF CERVICAL CANCER
COMPLICATION
Stage I - Cancer is found only in your cervix. It hasn't
Bleeding spread and is small.
Infection Stage II - Cancer has spread beyond your cervix and
Rejection uterus but hasn't yet spread to your pelvic wall (the
tissues that line the part of the body between your hips)
PREVENTION or your vagina.
Stage III - Cancer has spread to the lower part of your
Avoid behaviors that lead to cirrhosis. vagina and may have spread to your pelvic wall, ureters
Reach or maintain a healthy weight. (tubes that carry urine) and nearby lymph nodes.
Get a hepatitis B vaccine. This vaccine is safe for nearly Stage IV - Cancer has spread to your bladder, rectum or
everyone. Ask your doctor about the hepatitis A vaccine. other parts of the body like your bones or lungs.
Avoid hepatitis C.
If you have any liver disease, have diabetes, obesity or RISK FACTORS
are a heavy drinker, ask your healthcare provider about
liver cancer screenings. Early childbearing
Exposure to diethylstilbestrol in utero
CERVICAL CANCER
Exposure to human papillomavirus, types 16 and 18
Cervical cancer is a type of cancer that occurs in the Family history of cervical cancer
cells of the cervix — the lower part of the uterus that HIV infection and other causes of immune
connects to the vagina. deficiency
Various strains of the human papillomavirus (HPV), a Low socioeconomic status (may be related to early
sexually transmitted infection, play a role in causing marriage and early
most cervical cancer. childbearing)
Cervical cancer occurs most commonly in women ages Nutritional deficiencies (folate, beta-carotene, and
30 to 45, but it can occur as early as age 18. vitamin C levels are
BSN3A | PBL GROUP 1 22
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
lower in women with cervical cancer than in women including the stage of the disease, your age and general
without it) health, and if you want children in the future.
Overweight status The treatments for cervical cancer are radiation,
Prolonged use of oral contraceptives chemotherapy, surgery, targeted therapy and
Sexual activity: immunotherapy.
o Multiple sex partners o Radiation - Radiation therapy uses energy beams
o Early age (<20 years) at first coitus to kill cancer cells on your cervix. There are two
(exposes the vulnerable young cervix to types of radiation therapy:
potential viruses from a partner) o External beam radiation therapy (EBRT) - Aims
Sexual contact with men whose partners have had high-powered radiation at cancer from a machine
cervical cancer outside your body.
o Brachytherapy - puts the radiation in or just near
Sex with uncircumcised men
cancer.
Smoking and exposure to secondhand smoke
o Chemotherapy - Chemotherapy (chemo) uses
drugs that are injected through your veins or taken
CLINICAL MANIFESTATIONS by mouth to kill cancer cells. It enters your blood
and is effective for killing cells anywhere in your
body. There are several drugs used for chemo and
Early-stage cervical cancer generally produces no signs
or symptoms. they can be combined. Chemo is often given in
cycles. The length of the cycle and the schedule or
Signs and symptoms of more-advanced cervical cancer
frequency of chemotherapy varies depending on the
include:
drug used and where cancer is located.
o Vaginal bleeding after intercourse,
Surgery. Different kinds of surgery are used to treat
between periods or after menopause
cervical cancer. Some of the most common kinds of
o Watery, bloody vaginal discharge that may
surgery for cervical cancer include:
be heavy and have a foul odor
o Laser surgery - This surgery uses a laser beam to
o Pelvic pain or pain during intercourse
o Menstrual periods may be heavier and last burn off cancer cells.
o Cryosurgery - This surgery freezes cancer cells.
longer than normal.
o Cone biopsy - A surgery in which a cone-shaped
If cancer has spread to nearby tissues or organs,
piece of tissue is removed from your cervix.
symptoms may include:
o Simple hysterectomy - This surgery involves the
Difficult or painful urination, sometimes with blood in
removal of your uterus but not the tissue next to
urine.
your uterus. Your vagina and pelvic lymph nodes
Diarrhea, or pain or bleeding from your rectum when aren't removed.
pooping. o Radical hysterectomy with pelvic lymph node
Fatigue, loss of weight and appetite. dissection - With this surgery, your uterus,
A general feeling of illness. surrounding tissue called the parametrium, your
Dull backache or swelling in your legs. cervix, a small portion of the upper part of your
Pelvic/abdominal pain. vagina and lymph nodes from your pelvis are
removed.
o Trachelectomy - This procedure removes your
ASSESSMENT AND DIAGONOSIS cervix and the upper part of your vagina but not
your uterus.
Regular gynecological screenings with a Pap test can o Pelvic exenteration - This is the same as a radical
detect most cases of cervical cancer. hysterectomy but includes your bladder, vagina,
o A Pap test, or Pap smear- this test detects rectum and part of your colon, depending on where
abnormal or irregular cells in your cervix. These cancer has spread.
cells are examined for signs of precancers or other
irregularities.
If your Pap comes back as abnormal, further testing is OVARIAN CANCER
necessary. This could include an HPV test, which is a
specific test that checks the cells of your cervix for HPV Ovarian cancer is a growth of cells that forms in the
infection. Certain types of HPV infection are linked to ovaries. The cells multiply quickly and can invade
cervical cancer. and destroy healthy body tissue.
o HPV test - this test detects the high-risk types of The female reproductive system contains two
HPV infection that are most likely to cause cervical ovaries, one on each side of the uterus. The ovaries
cancer. each about the size of an almond produce eggs
(ova) as well as the hormones estrogen and
progesterone.
MEDICAL MANAGEMENT & TREATMENT It's not clear what causes ovarian cancer, though
doctors have identified things that can increase the
The cervical cancer treatment team includes a risk of the disease.
gynecologic oncologist (a doctor who specializes in
cancers of female reproductive organs). Recommended
treatment for cervical cancer is based on many factors
BSN3A | PBL GROUP 1 23
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
Doctors know that ovarian cancer begins when cells ovarian cancers are caused by genes changes you
in or near the ovaries develop changes (mutations) inherit from your parents.
in their DNA. o Family history of ovarian cancer - If you have
A cell's DNA contains the instructions that tell the blood relatives who have been diagnosed with
cell what to do. The changes tell the cells to grow ovarian cancer, you may have an increased risk of
and multiply quickly, creating a mass (tumor) of the disease.
cancer cells. The cancer cells continue living when o Being overweight or obese - increases the risk of
ovarian cancer.
healthy cells would die. They can invade nearby
o Postmenopausal hormone replacement therapy
tissues and break off from an initial tumor to spread
- taking hormone replacement therapy to control
(metastasize) to other parts of the body menopause signs and symptoms may increase the
risk of ovarian cancer.
TYPES OF OVARIAN CANCER o Endometriosis - is an often painful disorder in
which tissue similar to the tissue that lines the
The type of cell where the cancer begins determines the inside of your uterus grows outside your uterus.
type of ovarian cancer you have and helps your doctor o Age when menstruation started and ended -
determine which treatments are best for you. Ovarian beginning menstruation at an early age or starting
cancer types include: menopause at a later age, or both, may increase
o Epithelial ovarian cancer - this type is the most the risk of ovarian cancer.
common. It includes several subtypes, including o Never having been pregnant - If you've never
serous carcinoma and mucinous carcinoma. been pregnant, you may have an increased risk of
o Stromal tumors - these rare tumors are usually ovarian cancer.
diagnosed at an earlier stage than other ovarian
cancers.
o Germ cell tumors - these rare ovarian cancers ASSESSMENT AND DIAGNOSIS
tend to occur at a younger age.
Despite years of research, experts haven’t yet
developed a successful ovarian cancer screening test.
STAGES OF OVARIAN CANCER For this reason, the condition is often difficult to
diagnose in the early stages.
Stage I—Growth limited to the ovaries. If doctors suspects ovarian cancer, they’ll ask about
Stage II—Growth involves one or both ovaries with symptoms and perform a pelvic exam. During the exam,
pelvic extension. they’ll check for any abnormal growths or enlarged
Stage III—Growth involves one or both ovaries with organs.
metastases outside the pelvis or positive retroperitoneal They may recommend additional tests, including:
or inguinal nodes. o Imaging tests - Providers may use several imaging
Stage IV—Growth involves one or both ovaries with tests, including:
distant metastases. Pelvic ultrasound.
MRI (magnetic resonance imaging).
CT scan (computed tomography).
CLINICAL MANIFESTATIONS PET scan (positron emission tomography).
o Blood tests - Blood tests look for a substance
When ovarian cancer first develops, it might not cause called CA-125. High levels of CA-125 in your blood
any noticeable symptoms. When ovarian cancer can be a sign of cancer. However, CA-125 levels
symptoms happen, they're usually attributed to other, can be normal, even when cancer is present, and
more common conditions. higher in many conditions that aren’t cancer.
Signs and symptoms of ovarian cancer may include: Because of this, providers use blood tests in
o Abdominal bloating or swelling combination with other tests to diagnose ovarian
o Quickly feeling full when eating cancer.
o Weight loss o Surgical evaluation - Providers can diagnose
o Discomfort in the pelvic area ovarian cancer during surgery. Typically, if they find
o Fatigue abnormal growths, they’ll remove them during the
o Back pain same procedure.
o Changes in bowel habits, such as constipation o Laparoscopy - During laparoscopic surgery, a
o A frequent need to urinate surgeon places a thin camera (laparoscope)
through a small cut (incision) made in your
abdomen. Using the scope as a guide, along with
RISK FACTORS additional ports to hold instruments, the surgeon
can assess the cancer, perform staging biopsies
Factors that can increase your risk of ovarian cancer and, in some circumstances, remove ovarian
include: tumors.
o Older age - the risk of ovarian cancer increases as
you age. It's most often diagnosed in older adults.
Inherited gene changes. A small percentage of
BSN3A | PBL GROUP 1 24
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
MEDICAL MANAGEMENT AND TREATMENT father or brother previously diagnosed with prostate
cancer, especially if their relatives were diagnosed at
The goal in treating cancer is to remove as much, if not a young age.
all, cancer from your body as possible. Genes that may be associated with increased risk of
Common ovarian cancer treatments include: prostate cancer include hereditary prostate cancer 1
o Surgery - this typically involves the removal of your (HPC1) and BRCA1 and BRCA2 mutations (Cheng
reproductive organs and any organ that has cancer et al., 2019). The risk of prostate cancer is also
on it. Your surgeon may use laparoscopy (a
greater in men whose diet contains excessive
minimally invasive surgery) or laparotomy (open
surgery that requires an abdominal incision). amounts of red meat or dairy products that are high
o Chemotherapy - provider may recommend in fat (ACS, 2020). Endogenous hormones, such as
chemotherapy either before or after surgery. androgens and estrogens, also may be associated
Chemotherapy are drugs designed to target and kill with the development of prostate cancer.
cancerous cells. Your provider may give you
chemotherapy intravenously (through a vein) or PATHOPHYSIOLOGY
orally (in pill form).
o Targeted therapy - this cancer treatment uses In prostate cancer, the cells of these prostate glands
drugs to identify and attack cancer cells. Targeted mutate into cancer cells. Mutation is majorly in p53
therapy changes the way cancer cells grow and gene, BCL2 and ERK5 or alteration in Akt kinase
divide. signaling contribute toward the development of
o Hormone therapy - some ovarian cancers use prostate cancer. The prostate glands require
hormones to grow. This type of therapy blocks hormones, known as androgens that are involved in
hormones, slowing or stopping the growth of cell survival and apoptosis. Androgens include
cancer. testosterone, dehydroepiandrosterone and
o Radiation therapy - providers rarely use radiation dihydrotestosterone.
therapy for treatment of ovarian cancer.
Initially, small clumps of cancer cells remain confined
to prostate glands, condition known as carcinoma in
PROSTATE CANCER situ or prostatic intraepithelial
neoplasia (PIN). Over time, these cancer cells begin to
multiply and spread to the surrounding prostate tissue
forming a tumor. Eventually, the tumor may grow large
enough to invade nearby organs such as the nearby
lymph nodes or the rectum, or metastasize to bone,
lymphatic system and bladder.
CLINICAL MANIFESTATIONS
The majority of diagnosed patients are identified by
screening for prostate cancer.
Usually asymptomatic in early stages
Prostate cancer is the most common cancer in men Manifestations in later stages:
other than nonmelanoma skin cancer. It is the o Bone pain (most common site of
second most common cause of cancer death in disseminated prostate cancer)
American men, exceeded only by lung cancer, and is o Weakness from spinal-cord compression
responsible for 10% of cancer-related deaths in men. o Weight loss
Among men diagnosed with prostate cancer, 98% o Fatigue
survive at least 5 years, 84% survive at least 10 o Urinary retention
years, and 56% survive 15 years (ACS, 2020). o Hematuria
Prostate cancer is common in the United States and o Erectile dysfunction
northwestern Europe but is rare in Africa, Central o Hydronephrosis
America, South America, China, and other parts of
Asia. African American men have a high risk of ASSESSMENT AND DIAGNOSTIC FINDINGS
prostate cancer; furthermore, they are more than
twice as likely to die of prostate cancer as men of If prostate cancer is detected early, the likelihood of
other racial or ethnic groups cure is high (Brant, 2019). It can be diagnosed
Other risk factors for prostate cancer include through an abnormal finding with the DRE, serum
increasing age; the incidence of prostate cancer PSA, and TRUS with biopsy. Detection is more likely
increases rapidly after the age of 50 years. More than with the use of combined diagnostic procedures.
70% of cases occur in men older than 65 years. A Routine repeated DRE (preferably by the same
familial predisposition may occur in men who have a examiner) is important because early cancer may be
detected as a nodule within the gland or as an
BSN3A | PBL GROUP 1 25
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
extensive hardening in the posterior lobe. The more that can be used to detect either recurrent prostate
advanced lesion is “stony hard” and fixed. DRE also cancer at low PSA levels or metastatic disease
provides useful clinical information about the rectum, (NCCN, 2020b).
anal sphincter, and quality of stool.
The diagnosis of prostate cancer is confirmed by a MEDICAL MANAGEMENT
histologic examination of tissue removed surgically
Principles of treatment
by TURP, open prostatectomy, or ultrasound-guided
Prostate cancer is associated with slow growth and
transrectal needle biopsy. Fine-needle aspiration is a
may not be clinically significant during the lifetime of
quick, painless method of obtaining prostate cells for
a patient.
cytologic examination and determining the stage of
disease. Definitive treatments are associated with substantial
side effects that impact the quality of life.
Most prostate cancers are detected when a man
seeks medical attention for symptoms of urinary Multiple factors are considered in treatment:
obstruction or are found by routine DRE and PSA o Age and life expectancy
testing Cancer detected incidentally when TURP is o Overall health and comorbidities
performed for clinically benign disease and lower o Characteristics of the cancer and risk
urinary tract symptoms occurs in about 1 of 10 cases. stratification
o DRE and PSA testing are important o Patient preferences
Management options
screening procedures because abnormal
o DRE and elevated levels of PSA may Active surveillance:
raise suspicion of prostate cancer. o Deferred treatment with monitoring:
o However, a diagnosis of cancer requires Serial PSA and DREs over regular
confirmation with a prostate biopsy. intervals
TRUS helps detect nonpalpable prostate cancers Repeat biopsies
and assists with staging of localized prostate cancer. MRI
Needle biopsies of the prostate are commonly o Intention to treat for disease progression or
guided by TRUS. The biopsies are examined by a change in patient preference
pathologist to both determine if cancer is present and o Preferred in patients with very low- or low-
to grade the tumor. The most commonly used tumor risk cancer
grading system is the Gleason score. This Radiation therapy (RT):
o External beam RT (EBRT): can cause
erectile dysfunction and radiation proctitis
system assigns a grade of 1 to 5 for the most
o Brachytherapy:
predominant architectural pattern of the glands of the
Radioactive seed implants
prostate and a secondary grade of 1 to 5 to the
Can cause bladder irritation
second most predominant pattern. The Gleason
score is then reported as, for example, 2 + 4; the
combined value can range from 2 to 10. With each
increase in Gleason score, there is an increase in
Surgery (radical prostatectomy):
tumor aggressiveness. Lower Gleason scores
indicate well-differentiated and less aggressive o Options:
tumor cells; higher Gleason scores indicate Open surgery
undifferentiated cells and more aggressive cancer. Laparoscopy with or without
robotic assistance
A total score of 8 to 10 indicates a high-grade cancer
o Removal of the prostate gland, seminal
(Smith et al., 2019; Zhou, Salles, Samarska, et al.,
vesicles, and pelvic lymph nodes, followed
2019).
by reconstruction (reconnecting the bladder
Categorization of low-, intermediate-, and high-risk
neck and the urethra)
prostate cancer is determined by the extent of cancer
o Can cause erectile dysfunction and stress
in the prostate gland, whether or not the cancer is
urinary incontinence
localized to the prostate, the aggressiveness of the
cells, and the spread to the lymph nodes and
Androgen deprivation therapy (ADT):
beyond. Level of risk, in turn, is used to determine
o Luteinizing hormone-releasing hormone
treatment options.
(LHRH) agonists:
Bone scans, skeletal x-rays, and magnetic
Leuprolide acetate, goserelin,
resonance imaging (MRI) may be used to identify
triptorelin, and histrelin
metastatic bone disease. Pelvic computed
Initial release/surge of LH, then ↓
tomography (CT) scans may be performed to
pituitary LH → ↓ testosterone
determine if the cancer has spread to the lymph
o LHRH antagonists:
nodes. The radiolabeled monoclonal antibody
Degarelix, relugolix
capromab pendetide with indium 111 is an antibody
BSN3A | PBL GROUP 1 26
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
↓ Pituitary drive without an initial
Stage II:
surge in LH → ↓ testosterone o Active surveillance
o Antiandrogens: If no symptoms
Androgen receptor antagonists: In the elderly
flutamide, bicalutamide, If serious health issues
apalutamide, and enzalutamide o RT with or without ADT
Androgen synthesis inhibitors: o Surgery with or without EBRT
abiraterone, ketoconazole, and Stage III:
aminoglutethimide o Recurrence after treatment is more likely.
o Surgical castration with simple orchiectomy o EBRT plus ADT: Brachytherapy may be
(removal of the testicles): ↓ testosterone added.
levels o Surgery followed by RT and/or ADT
o General side effects: Stage IV:
Reduced sexual desire o Lymph-node involvement:
Impotence RT plus ADT
Hot flashes In young individuals with minimal
Gynecomastia and breast regional lymph-node spread,
tenderness surgery followed by ADT with or
Depression without RT can be considered.
Chemotherapy: o Metastatic disease: ADT plus
o Docetaxel chemotherapy
o Cabazitaxel o Other options:
ADT-resistant cancer:
Immunotherapy: immunotherapy or PARP
o Sipuleucel-T (Provenge) inhibitors
Vaccine Symptomatic bone metastasis
Made from autologous without visceral disease: radium-
mononuclear cells 223
Induces immunity against prostate Differential Diagnosis
cancer BPH: a condition caused by an increase in the
For metastatic ADT-resistant number of stromal and epithelial cells within the
prostate cancer prostate gland. Patients are usually > 50 years of age
o Pembrolizumab: and present with symptoms of bladder obstruction
Programmed cell death receptor-1 and/or bladder-storage problems. Benign prostatic
ligand (PD-L1) inhibitor hyperplasia can lead to an increase in PSA levels.
For patients lacking the mismatch- Diagnosis is based on history and invasive testing
repair (dMMR) mechanism, and (cystoscopy, urodynamics, transrectal ultrasound
for individuals with high levels of imaging). Management is with medications and/or
microsatellite instability (MSI-H) surgery.
Other therapies: Prostatitis: a group of inflammatory conditions of the
o Targeted therapy prostate gland. Patients may be asymptomatic or
Poly-ADP-ribose polymerase present with urinary symptoms, such as perineal
(PARP) inhibitors pain, increased urinary frequency and urgency,
For patients with germline or urinary obstruction, and fever. The diagnosis is
somatic DNA repair mutation
(BRCA) generally clinical and supported by urinalysis and
o Radium-223 culture data. Management depends on the etiology,
Emits alpha radiation but can include antibiotics in cases of infection.
Prevents complications due to Prostate-specific antigen levels may be elevated. To
bone metastasis differentiate prostatitis from prostate cancer, PSA
levels are remeasured after the treatment of
The following management options are based on prognostic prostatitis.
stage, and should be guided by the age, health, and Erectile dysfunction (ED): the consistent inability to
preferences of the patient: acquire or maintain an erection. Erectile dysfunction
is associated with diabetes mellitus, heart disease,
Stage I: and certain drugs (e.g., antidepressants).
o Active surveillance (preferred) Treatments for prostate cancer (RT, prostatectomy)
o RT or surgery: considered in patients with a can also result in ED. Management is with
high probability of progression
BSN3A | PBL GROUP 1 27
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
phosphodiesterase-5 inhibitors and vacuum- phase of cell development that is halted (i.e., with few
assisted erection devices. leukocytes differentiating beyond that phase).
Urinary incontinence (UI): the involuntary leakage of acute leukemia, the onset of symptoms is abrupt, often
urine. There are many types of incontinence, occurring within a few weeks. Leukocyte development is
including stress, urge, and mixed type. Radical halted at the blast phase, and thus most leukocytes are
prostatectomy can result in stress UI, which presents undifferentiated cells or blasts. Acute leukemia can
as urine leakage with exertion or as gravitational progress rapidly, with death occurring within weeks to
incontinence. Lifestyle intervention (Kegel months without aggressive treatment.
exercises), medical therapy, and surgical procedures chronic leukemia, symptoms evolve over a period of
are options in managing post-surgical UI. months to years, and the majority of leukocytes produced
are mature. Chronic leukemia progresses more slowly;
HEMATOLOGIC CELLULAR ABERRATIONS the disease trajectory can extend for years.
ACUTE MYELOID LEUKEMIA (AML)
LEUKEMIA
originates due to a series of genetic mutations in the
The term leukocytosis refers to an increase of myeloid HSC leading to clonal development of abnormal
leukocytes (WBCs) in the circulation. blast cells
Typically, only one specific cell type is increased. blast cells (i.e., immature leukocytes) continue to
the proportions of several types of leukocytes (e.g., proliferate, they crowd out normal bone marrow
eosinophils, basophils, monocytes) are small, an production resulting in anemia, thrombocytopenia (i.e.,
increase in other types can be great enough to elevate low platelet count), and either low or elevated WBC
the total leukocyte count, particularly the neutrophils or counts (rarely, the WBC may be within normal range).
lymphocytes. There is also impaired development of all myeloid cells:
leukocytosis can be a normal response to increased need monocytes, granulocytes (i.e., neutrophils, basophils,
(e.g., in acute infection), the elevation in leukocytes eosinophils), erythrocytes, and platelets.
should decrease as the physiologic need decreases. AML is the most common form of leukemia, as well as
A prolonged or progressively increasing elevation in most common cause of death from all leukemias.
leukocytes is abnormal and should be evaluated. A
RISK FACTORS
significant cause of persistent leukocytosis is a
hematologic malignancy (i.e., leukemia).
increasing age
The common feature of the leukemias is an unregulated
males have a higher incidence than females
proliferation of leukocytes in the bone marrow
having been exposed to chemicals such as benzene or
In acute forms (or late stages of chronic forms), the
pesticides or exposed to ionizing radiation
proliferation of leukemic cells leaves little room for normal
a history of prior treatment with chemotherapeutic drugs,
cell production.
such as alkylating agents or topoisomerase inhibitors,
There can also be a proliferation of cells in the liver and
tobacco smoking, other blood disorders (e.g.,
spleen (extramedullary hematopoiesis).
myeloproliferative diseases)
With acute forms, there can be infiltration of leukemic
several genetic disorders (e.g., Down syndrome, Trisomy
cells in other organs, such as the meninges, lymph
8, or Fanconi anemia)
nodes, gums, and skin.
The cause of leukemia is not fully known, but exposure to Note: The prognosis and survival rates are highly variable.
radiation or chemicals, certain genetic disorders, and viral Factors influencing a more positive outcome are younger age
infections are known to be risk factors for certain types of at diagnosis, more favorable cytogenetic alterations (which
leukemia. are strongly associated with younger age), and few concurrent
Bone marrow damage from pelvic radiation or certain (or mild) health problems.
types of chemotherapy drugs can cause acute leukemia,
typically occurring years after treatment for another In contrast, patients with significant comorbidities, of older
malignancy age, with cytogenetic features deemed to be adverse, or who
are frail, are more likely to have a poor prognosis.
CLASSIFICATIONS
CLINICAL MANIFESTATIONS
leukemias are commonly classified according to the stem
cell line involved, either lymphoid (referring to stem cells AML often presents, initially, as nonspecific complaints that
that produce lymphocytes) or myeloid (referring to stem can abruptly occur or gradually worsen over time. The signs
cells that produce nonlymphoid blood cells) and symptoms result from inadequate production of normal
They are also classified as either acute or chronic, blood cells, especially as the leukemic cells increasingly
based on the time it takes for symptoms to evolve and the crowd out the bone marrow.
BSN3A | PBL GROUP 1 28
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
Symptoms due to neutropenia (low neutrophil count) consolidation therapy is given to eliminate any residual
include fever and infection. leukemic cells that are not clinically detectable and to
Symptoms related to anemia include pallor, fatigue, reduce the chance for recurrence of leukemia.
weakness, dyspnea on exertion, and dizziness. Allogeneic stem cell transplant is the most common form
Symptoms reflective of thrombocytopenia include of hematopoietic stem cell transplant (HSCT) used in the
ecchymoses (bruises), petechiae (pinpoint red or purple treatment of AML
hemorrhagic spots on the skin), epistaxis (nosebleeds), HSCT is routinely done following induction and
and gingival bleeding. consolidation therapy.
The proliferation of leukemic cells within organs leads to The process of HSCT requires that patients begin by
a variety of additional symptoms: pain from an enlarged receiving high-dose, aggressive chemotherapy,
liver or spleen, hyperplasia of the gums, and bone pain sometimes in tandem with radiation therapy, to destroy
from expansion of marrow the hematopoietic functioning in the bone marrow and to
o Petechia or ecchymoses are common on kill any residual leukemic cells. This process is called
the skin conditioning therapy.
o Occasionally, leukemic infiltrates are seen patient is given human leukocyte antigen (HLA-matched)
o Leukemic cells can also infiltrate the gingiva donor stems cells via intravenous (IV) infusion to
or synovial spaces of joints. reestablish bone marrow functioning and to create a new
Lymphadenopathy (enlargement of lymph immune system
nodes) or splenomegaly. (enlargement of Patients with a poorer prognosis may benefit from early
the spleen) is rare. Fevers may occur and HSCT; those with a good prognosis may not ever require
are not always due to infection. HSCT
Other approaches may include treatment with
ASSESSMENT AND DIAGNOSTIC FINDINGS
enasidenib, a cytarabine-based regimen, along with other
agents (e.g., cladribine, fludarabine, mitoxantrone,
complete blood count (CBC) commonly shows a
etoposide); palliative care; or use of a hypomethylating
decrease in both erythrocytes and platelets
agent (e.g., azacitidine or decitabine).
AML can be further classified into seven different
Supportive care may be the best treatment option to
subgroups, based on cytogenetics, histology, and
consider if the patient has significant comorbidity, such as
morphology of the blasts, as well as the presence of
extremely poor cardiac, pulmonary, renal, or hepatic
genetic mutations.
function; is older and frail; or both.
The actual prognosis varies somewhat between
subgroups and with the extent of cytogenetic COMPLICATIONS
abnormalities and genetic mutations, yet the clinical
course and treatment differ substantially with only bleeding and infection, which are the major causes of
one subtype. death.
The low platelet count can cause ecchymoses and
MEDICAL MANAGEMENT
petechiae.
achieve complete remission of the disease, in which Major hemorrhages also may develop when the platelet
count drops to less than 10,000/mm3.
there is no residual leukemic cells in the bone
marrow or peripheral blood. The most common bleeding sources include
gastrointestinal (GI), pulmonary, vaginal, and intracranial.
chemotherapy treatment is administered in two parts:
induction and consolidation. Disseminated intravascular coagulation (DIC) is
Induction therapy typically involves high doses of common, particularly in patients with the APL subtype
cytarabine and either daunorubicin, idarubicin, or very high WBC count (greater than 100,000/mm3) can
mitoxantrone; etoposide is occasionally added to the cause stasis within the cerebral or pulmonary circulation
regimen. Because of the lack of mature and normal granulocytes
Older patients (especially those older than 70 years) that help fight infection, patients with leukemia are prone
or those unable to tolerate standard therapy (in poor to infection
health) may receive lower-intensity therapy (using Massive leukemic cell destruction from chemotherapy
hypomethylating agents, low doses of cytarabine, or results in the release of intracellular electrolytes and fluids
hydroxyurea), which may extend survival without a into the systemic circulation.
significant increase in toxicity beyond that of the Increases in uric acid levels, potassium, and phosphate
underlying disease are seen; this process is referred to as tumor lysis
syndrome
NOTE: During induction therapy, chemotherapy not only The increased uric acid and phosphorus levels make the
destroys leukemic cells, but also healthy cells, requiring patient vulnerable to renal stone formation and renal
patients to be hospitalized for several weeks (typically 4 to 6 colic, which can progress to acute kidney injury.
weeks) due to severe and potentially life-threatening side Hyperkalemia and hypocalcemia can lead to cardiac
effects, such as neutropenia. arrhythmias; hypotension; neuromuscular effects such as
BSN3A | PBL GROUP 1 29
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
muscle cramps, weakness, and spasm/tetany; and perfusion to the lungs and brain from leukostasis (the
confusion; and seizures may also develop excessive volume of leukocytes inhibits blood flow
Patients require a high fluid intake, and prophylaxis with through the capillaries).
allopurinol or rasburicase to prevent crystallization of uric The patient may have an enlarged, tender spleen, and
acid and subsequent stone formation. occasionally the liver may also be enlarged and tender.
GI problems may result from the infiltration of abnormal Some patients have insidious symptoms, such as
leukocytes into the abdominal organs and from the malaise, anorexia, and weight loss.
toxicity of the chemotherapeutic agents. Anorexia, Lymphadenopathy is uncommon, but if present, indicates
nausea, vomiting, diarrhea, and severe mucositis are late disease and a poor prognosis
common.
MEDICAL MANAGEMENT
NURSING MANAGEMENT
The goal of treatment for CML is to control the disease, either
Emphasize comfort by obtaining remission or by keeping the patient in the chronic
Minimize the adverse effects of chemotherapy phase for as long as possible. CML is not considered to be
Promote preservation of veins curable among older adults despite advances in
Manage complications understanding the pathophysiology of the disease and the
Provide teaching and psychological support advent of new agents.
CHRONIC MYELOID LEUKEMIA the use of tyrosine kinase inhibitors (TKIs) has
significantly improved treatment and long-term survival
Chronic myeloid leukemia (CML) arises from a mutation for patients with CML
in the myeloid stem cell. Medical management is based upon the patient’s age,
CML results from a chromosomal translocation, where a general health, calculation of risk-score (based upon
section of deoxyribonucleic acid (DNA) is shifted from stage of disease and prognosis), and phase of disease.
chromosome 22 to chromosome 9, forming what is known TKIs work by blocking the signals within the leukemic
as a “fusion gene” that is abnormal. cells that express the BCR-ABL protein.
CML accounts for 15% of all new cases of leukemia The TKI imatinib mesylate is considered to be standard
of care for patients with CML.
RISK FACTORS Newer, alternative TKIs approved for first-line (primary)
therapy for patients in the chronic phase of CML include
increasing age, being male, having a history of smoking, dasatinib or nilotinib
and being exposed to high doses of radiation (e.g., atomic
bomb survivors). NOTE: periorbital edema is common with long-term use of
imatinib; dasatinib is very myelosuppressive, and its use
CLINICAL MANIFESTATIONS carries a significant risk for pleural effusion and for causing a
prolonged QT interval; and nilotinib has cardiotoxic effects.
There are three stages in CML that include chronic,
accelerated, and blast crisis Other TKIs approved for second-line therapy (when
During the chronic phase, patients have few symptoms, patients do not respond satisfactorily to the first-line
leukocytosis is detected by a CBC performed for some agents) are bosutinib and ponatinib.
other reason, and complications from the disease itself All TKIs are metabolized by the cytochrome P450
are rare pathway, which means that drug-to-drug interactions are
The accelerated phase can be insidious or rapid; it marks common.
the process of evolution (or transformation) to the acute Drugs that may decrease the effects of the TKI are
form of leukemia (blast crisis). corticosteroids, antiseizure medications, antacids, and
In the accelerated phase of disease, blood counts begin St. John’s wort.
to worsen, new chromosomal changes may be seen on Drugs that may increase the effects of the TKI include
analysis, and symptoms consistent with leukemia may grapefruit juice, certain antibiotics (e.g., clarithromycin),
start to appear, such as fatigue, anemia, splenomegaly, and azole antifungals (e.g., clotrimazole, ketoconazole).
or dyspnea CML is a disease that can potentially be cured with
The patient may complain of bone pain and may report allogeneic HSCT in otherwise healthy patients who are
fevers (without any obvious sign of infection) and weight younger than 65 years.
loss acute form of CML (blast crisis), treatment may resemble
Blast crisis or blast phase of CML is the most advanced induction therapy for acute leukemia, using the same
phase. medications as for AML or acute lymphocytic leukemia.
Patients in this phase exhibit signs and symptoms that Patients whose disease evolves into a “lymphoid” blast
are more like AML than a chronic disease. crisis are more likely to be able to reenter a chronic phase
Patients with extremely high leukocyte counts may be after induction therapy
dyspneic or slightly confused because of decreased
BSN3A | PBL GROUP 1 30
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
NURSING MANAGEMENT Similar to treatment for AML, treatment for ALL can be
grouped into induction, consolidation, and maintenance
Most TKIs are oral agents; therefore, their effectiveness phases.
is dependent upon the patient’s ability and motivation to Because ALL frequently invades the CNS, preventive
adhere to the prescribed treatment regimen (These drugs intrathecal chemotherapy or, less frequently, cranial
may cause side effects that the patient may find difficult irradiation, are also a key part of the treatment plan
to manage, such as fatigue, asthenia (weakness), TKIs (e.g., imatinib) are effective in patients with
pruritus (itching), headache, skin rash, and Philadelphia chromosome-positive ALL; these drugs can
oropharyngeal pain. be used alone or in combination with conventional
It is extremely important for the nurse to educate the chemotherapy
patient about the medication regimen, how to manage Lymphoid blast cells are typically very sensitive to
side effects, drug interactions, and safe handling corticosteroids and to vinca alkaloids; therefore, these
The nurse should also monitor the patient for adverse medications are an integral part of the initial induction
signs and symptoms of therapy, such as decreased therapy
urinary output, changes in the electrocardiogram (ECG; Lymphoid blast cells are typically very sensitive to
TKIs can cause arrhythmias and prolonged QT intervals), corticosteroids and to vinca alkaloids; therefore, these
and myelosuppression (e.g., fevers, chills, changes in the medications are an integral part of the initial induction
CBC). therapy
Typically, an anthracycline is included, sometimes with
ACUTE LYMPHOCYTIC LEUKEMIA
asparaginase.
results from an uncontrolled proliferation of immature Once a patient is in remission, special testing
cells (lymphoblasts) derived from the lymphoid stem cell. (immunophenotyping, immunoglobulin gene
rearrangements, T-cell receptor genes, molecular
The cell of origin is the precursor to the B lymphocyte in
testing) is done to look for residual leukemic cells; these
approximately 75% of ALL cases; Tlymphocyte ALL
tests can detect as few as a single ALL cell among 10,000
occurs in approximately 25% of cases.
to 100,000 normal cells.
For patients with relapsed or refractory B-cell precursor
ALL can occur at any age, but 75% to 80% of all cases
ALL, agents such as blinatumomab or inotuzumab
are found in children, with the median age at diagnosis
ozogamicin have been found to be effective
being 15 years
The development of chimeric antigen receptor (CAR) T
Boys are affected more often than girls; the peak
cells has significantly improved treatment outcomes and
incidence is 4 years of age. After 15 years of age, it is
overall survival in patients with ALL
relatively uncommon, until age 45 when the incidence
again rises NURSING MANAGEMENT
For those over age 45, risk factors for ALL include older
age (especially over 70 years), prior exposure to Emphasize comfort
chemotherapy or radiation therapy, having certain genetic Minimize the adverse effects of chemotherapy
conditions (e.g., especially Down syndrome; also Promote preservation of veins
neurofibromatosis, Klinefelter syndrome, and Fanconi Manage complications
anemia) Provide teaching and psychological support
CLINICAL MANIFESTATIONS
CHRONIC LYMPHOCYTIC LEUKEMIA
may be nonspecific while others have no symptoms Chronic lymphocytic leukemia (CLL) is a common
initially. malignancy of older adults, and the most prevalent type
Manifestations of leukemic cell infiltration into other of adult leukemia in the Western world
organs are more common with ALL than with other forms The average age at diagnosis is 71 years
of leukemia and include pain from an enlarged liver or
CLL is rarely seen in Native Americans and infrequently
spleen as well as bone pain.
among people of Asian descent. Unlike other forms of
The central nervous system (CNS) is frequently a site for leukemia, a strong familial predisposition exists with CLL;
leukemic cells; thus, patients may exhibit cranial nerve the disease can occur in 10% of those with a first- or
palsies or headache and vomiting because of meningeal second-degree relative with the same diagnosis.
involvement. Other extranodal sites include the testes
Veterans of the Vietnam War who were exposed to Agent
and breasts.
Orange may be at risk for developing this disease
MEDICAL MANAGEMENT
PATHOPHYSIOLOGY
obtain remission without excess toxicity and with a rapid
CLL is typically derived from a malignant clone of B
hematologic recovery so that additional therapy can be
lymphocytes.
given if needed.
BSN3A | PBL GROUP 1 31
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
A clone proliferates from a cell of origin so that should be followed, such as for breast, colorectal, lung,
descendent cells are identical to the cell of origin. In and prostate cancer
contrast to the acute forms of leukemia, most leukemic
cells in CLL are fully mature. MEDICAL MANAGEMENT
One possible mechanism that explains this oncogenesis
For patients with no symptoms at the time of diagnosis,
is that these cells can escape apoptosis (programmed
the traditional “watchand-wait” approach is often used
cell death), resulting in an excessive accumulation of the
until progression of disease is noted (which could be
cells in the marrow and circulation
months to years)
CLL is characterized by the progressive accumulation of
Treatment for CLL is variable and can consist of a single
leukemic cells in the bone marrow, blood, and lymphoid
immunotherapy agent administered in combination with
tissues
chemotherapeutic agents, such as an immunotherapeutic
Because the lymphocytes are small, they can easily travel
antibody against the B-lymphocyte antigen CD20 (e.g.,
through the small capillaries within the circulation, and the
rituximab, ofatumumab, obinutuzumab) with
pulmonary and cerebral complications of leukocytosis
chemotherapeutic agents (e.g., fludarabine,
seen with myeloid leukemias are not typically found in
cyclophosphamide, bendamustine, chlorambucil) as
CLL. However, these cells often accumulate within the
initial therapy.
lymph nodes and spleen. When it takes less than 12
The most commonly prescribed first-line
months for the absolute number of lymphocytes to double
chemotherapeutic agent is fludarabine. When the disease
(lymphocyte doubling time), a more aggressive disease
is accompanied by a deletion of the TP53 gene or a
course may ensue. Immunophenotyping of the circulating
mutation of this gene, TKIs such as ibrutinib or idelalisib
B cells is critical to establish the diagnosis by identifying
may be used as either monotherapy or in combination
the presence of a malignant clone of these cells; it is also
with other agents
used to gauge the prognosis
Depending upon the age of the patient (less than or
Beta-2 microglobulin, a protein found on the surface of
greater than 65 years of age) and whether or not the
lymphocytes, can be measured in the serum; an elevated
patient has comorbidities, patients with relapsed or
level correlates with a more advanced clinical stage and
refractory disease may also receive newer agents such
poorer prognosis.
as venetoclax, duvelisib, or acalabrutinib
o Autoimmune complications can occur at
The major side effect of fludarabine is prolonged bone
any stage, as either autoimmune hemolytic
marrow suppression, manifested by prolonged periods of
anemia or idiopathic thrombocytopenic
neutropenia, lymphopenia, and thrombocytopenia, which
purpura. In the autoimmune process, the
puts patients at risk for such infections as Pneumocystis
reticuloendothelial system destroys the
jiroveci, Listeria, mycobacteria, herpes viruses, and
body’s own erythrocytes or platelets.
cytomegalovirus (CMV).
Patients with CLL also have a greater risk
for developing other cancers The monoclonal antibody (MoAb) alemtuzumab is often
used in combination with other chemotherapeutic agents
Approximately 2% to 10% of patients with CLL will
experience transformation of their disease to a very when the disease is refractory to fludarabine, the patient
aggressive lymphoma, known as Richter’s has very poor prognostic markers, or it is necessary to
transformation eradicate residual disease after initial treatment.
Alemtuzumab targets the CD52 antigen commonly found
CLINICAL MANIFESTATIONS on CLL cells, and it is effective in clearing the marrow and
circulation of these cells without affecting the stem cells.
Lymphocytosis (an increased lymphocyte count) is Because CD52 is present on both B and T lymphocytes,
always present. patients receiving alemtuzumab are at significant risk for
The erythrocyte and platelet counts may be normal or, in infection; prophylactic use of antiviral agents and
later stages of the illness, decreased. Lymphadenopathy antibiotics (e.g., trimethoprim–sulfamethoxazole) is
is common; this can be severe and sometimes painful important and needs to continue for several months after
Splenomegaly may also occur treatment ends.
T-cell function is impaired and may be the cause of tumor CMV infection is also common with alemtuzumab,
progression and increased susceptibility to second idelalisib, and duvelisib, and prophylaxis is important;
malignancies and infections. among commonly prescribed antiviral agents, vancyclovir
Viral infections, such as herpes zoster, can become is more effective than acyclovir for treating CMV
widely disseminated. Patients receiving idelalisib or duvelisib have an
Defects in the complement system are also seen, which increased risk of hepatotoxicity, severe diarrhea, colitis,
results in increased risk of developing infection with and pneumonitis. TKIs have been found to increase the
encapsulated organisms (e.g., Haemophilus influenzae). risk of cardiovascular toxicities, including hypertension,
Patients should receive an annual comprehensive skin prolonged QT interval, left ventricular dysfunction, and
examination (as the incidence of skin cancer is higher in heart failure
this group), and screening guidelines for other cancers Ongoing periodic assessment of the CBC, blood
chemistries, ECG, blood pressure, and bowel habits are
BSN3A | PBL GROUP 1 32
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
important parameters to monitor among patients taking PATHOPHYSIOLOGY
these various agents.
Because of the older age of most patients with CLL, Hodgkin lymphoma is unicentric in origin, meaning that it
allogeneic HSCT may not be an option, particularly if initiates in a single node.
significant comorbidities exist. However, allogeneic The disease spreads by contiguous extension along the
HSCT might be considered for some patients with TP53 lymphatic system.
deletions or mutations who otherwise have a poor The malignant cell of Hodgkin lymphoma is the Reed–
prognosis. Morbidity and mortality rates remain high Sternberg cell, a gigantic tumor cell that is
(20%); thus, this treatment modality may be reserved for morphologically unique and thought to be of immature
those patients with high-risk disease, younger age, and lymphoid origin.
high degree of match from the donor These cells arise from the B lymphocyte. They may have
more than one nucleus and often have an owl-like
NURSING MANAGEMENT appearance
The presence of Reed–Sternberg cells is the pathologic
Emphasize comfort
hallmark and essential diagnostic criterion
Minimize the adverse effects of chemotherapy
The World Health Organization (WHO) has classified
Promote preservation of veins Hodgkin lymphoma into five subtypes based on
Manage complications pathologic analyses that reflect the natural history of the
Provide teaching and psychological support disease and suggest the prognosis
LYMPHOMA Four of these subtypes of Hodgkin lymphoma are
recognized as being consistent with classical disease
The lymphomas are neoplasms of cells of lymphoid
SUBTYPES
origin. These tumors usually start in lymph nodes but can
involve lymphoid tissue in the spleen, GI tract (e.g., the
Nodular sclerosis: This is the most common form of
wall of the stomach), liver, or bone marrow
Hodgkin lymphoma, accounting for about 70% of all
CLASSIFICATIONS cases. It is seen most often in the young; among
these patients, the lymph node contains elements of
They are often classified according to the degree of cell fibrous (sclerotic) tissue; approximately 40% of
differentiation and the origin of the predominant malignant patients have B symptoms. This type of Hodgkin
cell. Lymphomas are broadly classified into two lymphoma is highly curable.
categories: Hodgkin lymphoma and NHL. Mixed cellularity: This is the second most common
form of Hodgkin lymphoma, accounting for 20% to
HODGKIN LYMPHOMA 25% of all cases. This subtype is more common in
older adults and in males; it is frequently seen in
Hodgkin lymphoma is a relatively rare malignancy that patients with HIV infection, and B symptoms are
has a high cure rate. frequently reported.
It is somewhat more common in males than in females Lymphocyte-depleted: This form of Hodgkin
and has two peaks of incidence: one from ages 15 to 34 lymphoma is rare; it is characterized by involved
and the other after 60 years of age lymph node(s) with few normal lymphocytes but
numerous Reed–Sternberg cells. B symptoms are
RISK FACTORS
commonly reported
Lymphocyte-rich: This type of Hodgkin lymphoma
The cause of Hodgkin lymphoma is unknown. However,
is also an uncommon form of the disease; the lymph
several risk factors have been identified, which include
node(s) has numerous normal lymphocytes and
age, a history of viral infections (particularly the Epstein–
Reed–Sternberg cells and B symptoms are rare.
Barr virus, human immune deficiency virus [HIV], or
human herpesvirus 8 [HHV8]), having a family history, Nodular lymphocytes predominant Hodgkin
and being exposed to cytotoxic agents. lymphoma (NLPHL): This is the lone type of
Hodgkin lymphoma that is not considered of the
Additionally, Hodgkin lymphoma is seen more commonly
classical type. In NLPHL there are few Reed–
in patients receiving long-term immunosuppressive
Sternberg cells; rather, there is a predominance of
therapy (e.g., organ transplant recipients) and in veterans
lymphocyte cells called “popcorn” cells.
who were exposed to the herbicide Agent Orange (see
o Furthermore, there is minimal involvement of the
Veterans Considerations section in CLL)
lymph nodes as compared to the subtypes that
The 5-year survival rate for Hodgkin lymphoma is about
fall under the four classical Hodgkin types.
92% to 94% for localized/regional disease (stage I or II)
o NLPHL is seen more often in males than
and 78% for those with distant disease (stage IV)
females and the age at diagnosis is more often
between 30 and 50 years.
o Patients tend to present with peripheral
adenopathy and with early-stage disease.
BSN3A | PBL GROUP 1 33
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
o NLPHL is slow growing and highly curable, but staging to help determine the extent of disease as well as
some patients can relapse while others can later for evaluation of response to treatment
transform to an aggressive NHL Laboratory tests include CBC with differential; serum
electrolytes, blood urea nitrogen (BUN) and creatinine;
CLINICAL MANIFESTATIONS ESR; liver and renal function studies;
immunohistochemistry and cytogenetic evaluation; HIV
Hodgkin lymphoma usually begins as an enlargement of
testing; and hepatitis B and C testing.
one or more lymph nodes on one side of the neck.
A multiple-gated acquisition (MUGA) scan and/or ECG
The individual nodes are painless and firm but not hard.
should be performed prior to the start of therapy if the
The most common sites for lymphadenopathy are the
patient is to receive an anthracycline-based treatment
cervical nodes. However, other nodes that can be
regimen, as these chemotherapeutic agents are
affected include the supraclavicular and mediastinal
associated with adverse cardiovascular effects.
nodes; involvement of the iliac or inguinal nodes or spleen
Bone marrow biopsies are not routinely performed unless
is much less common
cytopenias are present and the PET scan is negative
A mediastinal mass may be seen on chest x-ray;
occasionally, the mass is large enough to compress the MEDICAL MANAGEMENT
trachea and cause dyspnea. B symptoms, if present, are
indicative of more advanced disease The goal in the treatment of Hodgkin lymphoma is cure,
Clinical manifestations result from compression of organs as the overall cure rate is about 90%
by the tumor, such as cough and pulmonary effusion Treatment is determined primarily by stage of disease,
(from pulmonary infiltrates), jaundice (from hepatic not histologic type, utilizing the Ann Arbor staging system
involvement or bile duct obstruction), abdominal pain Patients with early disease (stage I-II) may receive one of
(from splenomegaly or retroperitoneal adenopathy), or the following combination chemotherapy regimens:
bone pain (from skeletal involvement). ABVD (doxorubicin [trade name Adriamycin], bleomycin,
A mild anemia is the most common hematologic finding. vinblastine, and dacarbazine) or Stanford V (doxorubicin,
The leukocyte count may be elevated or decreased. vinblastine, mechlorethamine, etoposide, vincristine,
bleomycin, and prednisone)
The platelet count is typically normal, unless the tumor The standard treatment for patients with advanced
has invaded the bone marrow, suppressing disease (stages III to IV) and those with B symptoms is
hematopoiesis. also ABVD chemotherapy, although these patients
Laboratory tests that may be assessed to detect disease typically receive additional cycles of chemotherapy
activity include the serum copper level, which may be treatment.
elevated, and the erythrocyte sedimentation rate (ESR). Other combinations of chemotherapy may be used;
The ESR measures the rate of settling of RBCs; elevation however, these options have more toxic effects.
is indicative of inflammation; it is also called the sed rate. When a patient has a suspected relapse of disease, a
Other symptoms seen in patients with Hodgkin lymphoma biopsy and a PET scan are performed to confirm the
are pruritus, which is common and can be extremely diagnosis and stage of disease.
distressing, fatigue, decreased appetite, abdominal pain, Treatment options for patients with refractory or relapsed
splenomegaly, and although rare, occasional pain in disease include immunotherapeutic agents, such as a
affected lymph node after drinking alcohol monoclonal antibody (MoAb) (e.g., everolimus,
Patients may also have impaired cellular immunity, as brentuximab), or a checkpoint inhibitor (e.g., nivolumab,
evidenced by an absent or decreased reaction to skin pembrolizumab)
sensitivity tests (i.e., Candida, mumps) and increased Treatment for patients with NLPHL in the early stage of
susceptibility to infections, particularly herpes zoster disease may include radiation therapy only
Treatment for patients with NLPHL in the early stage of
ASSESSMENT AND DIAGNOSTIC FINDINGS disease may include radiation therapy only
Patients with stage IB to IIB disease may receive ABVD,
The diagnosis is made by means of an excisional lymph
CHOP (cyclophosphamide, doxorubicin [also less
node biopsy and the presence of Reed–Sternberg cells.
commonly called hydroxydaunorubicin], vincristine [trade
Once the diagnosis is confirmed and the histologic type is
name of Oncovin], and prednisone) or CVP
established, it is necessary to assess the stage of the
(cyclophosphamide, vincristine, and prednisone)
disease
regimens in combination with rituximab.
Physical examination requires a careful, systematic
Those with advanced stage disease are treated with
evaluation of all palpable lymph node chains as well as
these same regimens but with radiation therapy added.
the size of the spleen and liver.
Patients typically feel better following therapy. Late
A chest x-ray and a computed tomography (CT) scan of
effects of treatment, which may occur months to years
the chest, abdomen, and pelvis are crucial to identify the
following treatment, include development of a secondary
extent of lymphadenopathy within these regions. A
malignancy, or cardiovascular disease, hypothyroidism,
positron emission tomography (PET) scan is the most
and infertility
sensitive imaging test and is recommended for initial
BSN3A | PBL GROUP 1 34
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
Secondary malignancies (most common are lung and The incidence increases with each decade of life; the
breast) often develop more than 10 years following median age at diagnosis is 66 years
completion of therapy. This is especially true in females The natural course of the disease is variable and
who received radiation therapy to the chest or axillary dependent upon the type of lymphoma.
areas NHLs can be categorized as indolent (i.e., a slow-
Cardiovascular disease (e.g., coronary artery disease, growing cancer that often remains localized or causes
arrhythmias, and cardiomyopathy) is also seen 10 years few symptoms) or aggressive (i.e., a fast-growing cancer
posttreatment and tends to occur in patients who received that spreads rapidly and causes significant morbidity)
mediastinal radiation or an anthracycline-based
chemotherapeutic agent (e.g., daunorubicin, CLINICAL MANIFESTATIONS
doxorubicin).
Hypothyroidism may occur in about 50% of long-term Symptoms of NHL are highly variable, reflecting the
survivors of Hodgkin lymphoma, particularly in those who diverse nature of the disease. Similar to Hodgkin
received neck or upper mediastinal radiation lymphoma, NHL may start as a painless swelling in one
or more lymph nodes in the neck, axillary region, or groin.
The use of some chemotherapy combinations can lead to
infertility in both males and females. For instance, If the lymphoma is indolent in nature, symptoms may be
females of childbearing years may experience premature absent or very minor
menopause following treatment with alkylating agents Other symptoms depend upon enlarged lymph node site
(e.g., cyclophosphamide, dacarbazine, and size, which can compress organs, compromising
mechlorethamine). function. For example, a mass in the mediastinum can
Other organ dysfunction is also well documented, cause cough, shortness of breath, and chest pain that
including that of the endocrine system. may lead to cardiovascular or respiratory distress.
Persistent fatigue is common in survivors and can be An abdominal mass may compromise the bowel or
exacerbated by depression and other treatment-related ureters, leading to acute kidney injury or bowel
comorbidities obstruction.
Splenomegaly can cause abdominal pain, nausea, early
NURSING MANAGEMENT satiety, and weight loss.
The nurse should encourage patients to reduce ASSESSMENT AND DIAGNOSTIC FINDINGS
factors that increase the risk of developing second
cancers, such as use of tobacco and alcohol and Similar to Hodgkin lymphoma, an incisional or excisional
exposure to environmental carcinogens and lymph node biopsy is required for immunophenotyping
excessive sunlight. and cytogenetic analysis testing
The specific histopathologic type of the disease is used
Screening for late effects of treatment, such as to differentiate the subtype of NHL; it also has important
chemotherapy prognostic implications and is used to determine
the nurse should provide education about relevant appropriate treatment
self-care strategies and disease management.
Flow cytometry is commonly performed to determine the
NON-HODGKIN LYMPHOMAS specific antigen on the malignant cell.
Another test that may be performed is fluorescence in situ
The NHLs are a heterogeneous group of cancers that hybridization (FISH), which analyzes the DNA and RNA
originate from the neoplastic growth of lymphoid tissue. of the biopsy or blood sample for chromosomal
Similar to CLL, the neoplastic cells are thought to arise abnormalities.
from a single clone of lymphocytes; however, in NHL, the Laboratory studies mirror those done for a patient with
cells may vary morphologically. In contrast to Hodgkin Hodgkin lymphoma (see that previous discussion). In
lymphoma, the lymphoid tissues involved are largely addition, there may be testing for viruses (e.g., Epstein–
infiltrated with malignant cells. Barr, HHV8, hepatitis B); polymerase chain reaction
The spread of these malignant lymphoid cells occurs (PCR); CT scans of the chest, abdomen, and pelvis; PET
unpredictably; true localized disease is uncommon. scan; MUGA or ECG (if patient is to receive
Lymph nodes from multiple sites may be infiltrated, as anthracycline-based regimen); and bone marrow biopsy
may sites outside the lymphoid system (i.e., extranodal and aspirate (if marrow involvement is suspected).
tissue; Although the stage of disease is important, often it is not
an accurate predictor of prognosis. Two prognostic
RISK FACTORS classification systems are used: the International
Prognostic Index (IPI) and, for follicular lymphomas, the
NHL is the seventh most common type of cancer
Follicular Lymphoma International Prognostic Index
diagnosed in the United States, accounting for about 4% (FLIPI).
to 5% of all new cancer cases each year. It occurs more
commonly in males.
BSN3A | PBL GROUP 1 35
NCM112 LECTURE
MEDICAL-SURGICAL NURSING
CELLULAR ABERATIONS
Age, performance status, lactate dehydrogenase levels, complication. The fatality rate is 90% and tends to occur
stage of disease, and extranodal involvement are scored within 2 months after the diagnosis is confirmed
to determine risk of failure or death from disease
NURSING MANAGEMENT
MEDICAL MANAGEMENT
Lymphoma is a highly complex constellation of diseases.
The goal of treatment for NHL is to obtain remission of When caring for patients with lymphoma, it is extremely
disease by killing as many of the malignant cells as important for the nurse to know the specific disease type,
possible; in contrast, the goal is cure for Hodgkin stage of disease, treatment history, and current treatment
lymphoma. plan.
Treatment for NHL is based upon the specific subtype of Most of the care for patients with Hodgkin lymphoma or
lymphoma and the stage of disease. NHL takes place in the outpatient setting, unless
If the disease is indolent and localized, the treatment of complications occur (e.g., infection, respiratory
choice may be radiation therapy alone. “Watchful waiting” compromise due to mediastinal mass).
may also be a choice for patients with an indolent form of Patients need to be educated to minimize the risks of
NHL, such as stage I follicular lymphoma, who have no or infection, to recognize signs of possible infection, and to
few symptoms at time of diagnosis. contact their primary provider if such signs develop
For aggressive subtypes of NHL, combination regular follow-up appointments and be screened for the
chemotherapy is typically indicated. One of the most signs and symptoms of possible secondary malignancies.
common combinations is CHOP. Additionally, patients should be evaluated for
A MoAb (e.g., rituximab, obinutuzumab) may be given cardiovascular and fertility concerns with each patient
along with the chemotherapy visit.
Radiation therapy may or may not be added to the
treatment regimen. In some cases, a MoAb may be
conjugated with a radioactive isotope and used for
treatment (e.g., ibritumomab tiuxetan).
CNS involvement is common with some aggressive forms
of NHL; in this situation, cranial radiation or intrathecal
chemotherapy is used in addition to systemic
chemotherapy.
When NHL has relapsed or is refractory to standard
treatments, other single agent or combination
chemotherapy regimens may be used. For instance, the
ICE regimen (i.e., ifosfamide, carboplatin, and etoposide)
may be implemented; or agents such as bendamustine,
brentuximab vedotin, romidepsin, or axicabtagene may
be tried
Autologous HSCT (AuHSCT) is another treatment option
for relapsed or refractory NHL, particularly in patients
younger than 60 years
A rare but potentially life-threatening complication of
chemotherapy is tumor lysis syndrome. Tumor lysis
syndrome occurs when the intracellular content of the
malignant cell breaks down and is released into the
peripheral blood and typically occurs 12 to 72 hours after
initiation of therapy
Reactivation of hepatitis B virus may be seen in patients
with NHL who become immunosuppressed following
chemotherapy. For example, hepatitis B reactivation can
occur in patients treated with rituximab-containing
regimens, even if the patient had tested negative for
hepatitis B prior to start of treatment
Preemptive treatment is recommended, including
antiviral therapy (i.e., lamivudine or entecavir) and close
surveillance in patients at high risk
Symptoms include confusion, motor weakness or poor
motor coordination, and visual and possibly speech
changes. Currently, there is no effective treatment for this
BSN3A | PBL GROUP 1 36
You might also like
- Medical-Surgical (Week 7) : (Sir Laingo-Octobe 07) JayloiseDocument6 pagesMedical-Surgical (Week 7) : (Sir Laingo-Octobe 07) Jayloisejeanylou chachi coronadoNo ratings yet
- Healthcare TransDocument9 pagesHealthcare TransKeihla NiebresNo ratings yet
- CanserDocument50 pagesCansertarek ahmed100% (1)
- 3 1 Neoplasia PDFDocument3 pages3 1 Neoplasia PDFPrabhat GuptaNo ratings yet
- Chapter 6 Neoplasia (2nd Edition)Document42 pagesChapter 6 Neoplasia (2nd Edition)vs7ksgrj8pNo ratings yet
- 1.06 General Pathology - Neoplasia (Part 1) - Dr. Annette SallilasDocument17 pages1.06 General Pathology - Neoplasia (Part 1) - Dr. Annette SallilasCherry RahimaNo ratings yet
- 5 NeoplasiaDocument55 pages5 Neoplasiaadinda kerenNo ratings yet
- Tumors: Benign and Malignant: Cancer Therapy & OncologyDocument3 pagesTumors: Benign and Malignant: Cancer Therapy & OncologyMaria ArifahNo ratings yet
- L2-Principles of Surgical OncologyDocument25 pagesL2-Principles of Surgical OncologyTofeeq101 WaNo ratings yet
- NeoplasiaDocument2 pagesNeoplasiaFayon JamesNo ratings yet
- Cancer Ms LecDocument16 pagesCancer Ms LecJulia Rae Delos Santos100% (1)
- What Is NeoplasmsDocument38 pagesWhat Is NeoplasmsRashid HussainNo ratings yet
- Aberrant Cell GrowthDocument3 pagesAberrant Cell Growthaziz aliNo ratings yet
- Cancer ResearchDocument5 pagesCancer ResearchmelanieNo ratings yet
- Oncology New AdultDocument13 pagesOncology New Adultرافت العواضيNo ratings yet
- OncologyDocument23 pagesOncologyEslam NassarNo ratings yet
- Pharma en OncologyDocument14 pagesPharma en Oncologyyaqoob008No ratings yet
- Understanding CancerDocument5 pagesUnderstanding CancerEunice Villa CuñadaNo ratings yet
- 2.3.1 Cancer Biology Cheat Sheet: by ViaDocument5 pages2.3.1 Cancer Biology Cheat Sheet: by Viaimk_mithunNo ratings yet
- Ovarian Sex Cord-Stromal Tumors Update (IJGC Jan 2021)Document8 pagesOvarian Sex Cord-Stromal Tumors Update (IJGC Jan 2021)Bernadette YapNo ratings yet
- Pathogenesis of Neoplasm PDFDocument3 pagesPathogenesis of Neoplasm PDFTasya Citra KiranaNo ratings yet
- 2 - Fudamentals of Neoplasm 1 - 2022Document33 pages2 - Fudamentals of Neoplasm 1 - 2022noreentamer20No ratings yet
- Outline: 1. Overview 2. NomenclatureDocument30 pagesOutline: 1. Overview 2. NomenclatureAbdullah MuceddidiNo ratings yet
- CancerDocument2 pagesCancermikErlhNo ratings yet
- 3 - Fudamentals of Neoplasm 2022Document32 pages3 - Fudamentals of Neoplasm 2022noreentamer20No ratings yet
- NATIONAL CANCER CONTROL PROGRAMM 2 (Prakash)Document19 pagesNATIONAL CANCER CONTROL PROGRAMM 2 (Prakash)angayarkanni100% (1)
- Cellular AbrasionDocument16 pagesCellular Abrasionmolina ababonNo ratings yet
- Index: DescriptionDocument17 pagesIndex: DescriptionDeepak R SriRamNo ratings yet
- Rishika Vijayvargiya Class XII ADocument21 pagesRishika Vijayvargiya Class XII ARajat PorwalNo ratings yet
- Module 1: Pathophysiologic Concepts in Cellular AberrationsDocument9 pagesModule 1: Pathophysiologic Concepts in Cellular AberrationsJanelle Cabida SupnadNo ratings yet
- PPP of The Malignant Process: Oncology: Nursing Management in Nursing CancerDocument3 pagesPPP of The Malignant Process: Oncology: Nursing Management in Nursing Cancer알파No ratings yet
- Lecture Handouts Oncology NursingDocument12 pagesLecture Handouts Oncology NursingTiffany Luv AdriasNo ratings yet
- They Adhere To Any Part That They Seize In, Similar To A Crab's Behavior. Malignant, As AppliedDocument10 pagesThey Adhere To Any Part That They Seize In, Similar To A Crab's Behavior. Malignant, As AppliedbeylaNo ratings yet
- NeoplasiaDocument11 pagesNeoplasiaعبدالكريم الاسدNo ratings yet
- Pathology NeoplasiaDocument15 pagesPathology NeoplasiaLaiba WarisNo ratings yet
- CELL OVERVIEW PREVENTION Notes 2015Document7 pagesCELL OVERVIEW PREVENTION Notes 2015Alexander LukashenkoNo ratings yet
- Set 3 SBL100 Introduction To Cancer 10nov2023Document66 pagesSet 3 SBL100 Introduction To Cancer 10nov2023dandotiya.yash73No ratings yet
- 7a. Cellular Aberration With PAIN ConceptDocument25 pages7a. Cellular Aberration With PAIN ConceptRENEROSE TORRESNo ratings yet
- Oncology Nursing NotesDocument12 pagesOncology Nursing NotesBavitha BNo ratings yet
- Oncology Nursing NotesDocument12 pagesOncology Nursing Notesjoyrena ochondra100% (7)
- MS CA and EN Ans KeyDocument15 pagesMS CA and EN Ans KeyAydh Dim-Mac RsclNo ratings yet
- Neoplasia ReviewDocument22 pagesNeoplasia ReviewLegnaNo ratings yet
- Cancer Hallmarks of Cancer CellDocument4 pagesCancer Hallmarks of Cancer CellMark James GavinaNo ratings yet
- 2.7 Cell Division Going Wrong - Cancer PDFDocument8 pages2.7 Cell Division Going Wrong - Cancer PDFAntoline Natasha RayappanNo ratings yet
- 212F - Oncology L1 - 2104Document25 pages212F - Oncology L1 - 2104Tyler LiuNo ratings yet
- NeoplasiaDocument150 pagesNeoplasiaDavon Richard Walter Van-VeenNo ratings yet
- Bisc 3150 General Pathology: Neoplasia Wednesday, January 31, 2018 Friday, February 2, 2018 Judy Maloney, PHDDocument62 pagesBisc 3150 General Pathology: Neoplasia Wednesday, January 31, 2018 Friday, February 2, 2018 Judy Maloney, PHDEvan PfeiferNo ratings yet
- NeoplasiaDocument31 pagesNeoplasiaAnin PrakashNo ratings yet
- OncologyDocument38 pagesOncologyNidhi PalNo ratings yet
- Cellular Aberration Lecture 1Document93 pagesCellular Aberration Lecture 1David Dwane Art SilorioNo ratings yet
- Oncology 1Document178 pagesOncology 1SUNIL KUMARNo ratings yet
- Chem. SummativeDocument3 pagesChem. SummativeAngel AticoNo ratings yet
- Cancer OverviewDocument10 pagesCancer Overviewampogison08No ratings yet
- 02.22.1 Neoplasia I Final PDFDocument79 pages02.22.1 Neoplasia I Final PDFSameeha AbbasNo ratings yet
- Neoplasia (I) : Department of Pathology, Sun Yat-Sen UniversityDocument113 pagesNeoplasia (I) : Department of Pathology, Sun Yat-Sen UniversityleyreaNo ratings yet
- Investigatory Project On CANCERDocument15 pagesInvestigatory Project On CANCERSreeja SwainNo ratings yet
- Jamaoncology Patel 2020 PG 200003 1599155176.12055Document1 pageJamaoncology Patel 2020 PG 200003 1599155176.12055Tiara Sekar AyudhipashaNo ratings yet
- Care of Patients With CancerDocument15 pagesCare of Patients With CancerArturo M. Ongkeko Jr.100% (6)
- Notes On Cancer (Class XII)Document2 pagesNotes On Cancer (Class XII)Aryan JaiswalNo ratings yet
- Entrepreneurship Introductory ConceptsDocument21 pagesEntrepreneurship Introductory ConceptsMaggay LarsNo ratings yet
- Restraints StudentsDocument3 pagesRestraints StudentsMaggay LarsNo ratings yet
- Outline S6Document23 pagesOutline S6Maggay LarsNo ratings yet
- Malabsorption SyndromeDocument5 pagesMalabsorption SyndromeMaggay LarsNo ratings yet
- Bio ProjectDocument19 pagesBio Projectpraveen godaraNo ratings yet
- Gastrointestinal MalignanciesDocument478 pagesGastrointestinal MalignanciesdrAlbertoVVNo ratings yet
- Minimally Invasive Surgery in Pediatric Oncology Galazka 2019Document11 pagesMinimally Invasive Surgery in Pediatric Oncology Galazka 2019jonays_0106293No ratings yet
- Clinical Features, Diagnosis, and Staging of Gastric Cancer - UpToDateDocument31 pagesClinical Features, Diagnosis, and Staging of Gastric Cancer - UpToDateCileni NuñezNo ratings yet
- Lung CancerDocument11 pagesLung CancerNader Smadi100% (2)
- Path BooksDocument7 pagesPath BooksbeosroNo ratings yet
- Laryngeal DysplasiaDocument7 pagesLaryngeal DysplasiakarimahihdaNo ratings yet
- 1oral DiagnosisDocument3 pages1oral Diagnosisابو العز100% (1)
- Balian Community College School of Midwifery Balian Pangil, LagunaDocument54 pagesBalian Community College School of Midwifery Balian Pangil, LagunaThriska Ravven ResurreccionNo ratings yet
- Anatomy Nail Biopsy NailDocument7 pagesAnatomy Nail Biopsy Nailaudriant.devarana.putra.wijoyonoNo ratings yet
- Truscreen Cervical Screening SystemDocument39 pagesTruscreen Cervical Screening SystemVyacheslav PilyaevNo ratings yet
- Pamphlet Liver BiopsyDocument8 pagesPamphlet Liver BiopsyManisha ShakyaNo ratings yet
- Breast Cancer PreventionDocument16 pagesBreast Cancer PreventionWindy HardiyantyNo ratings yet
- Utilizing Vitamin C To Treat Malignancies and Cancer: A Special Interview With Dr. Nathan GoodyearDocument42 pagesUtilizing Vitamin C To Treat Malignancies and Cancer: A Special Interview With Dr. Nathan GoodyearRocco LamponeNo ratings yet
- Brauchle - Discharge Paper - Nur 331Document12 pagesBrauchle - Discharge Paper - Nur 331api-405374041No ratings yet
- Pathology of Lung CancerDocument24 pagesPathology of Lung CancerWeiLinNo ratings yet
- W Biod05Document13 pagesW Biod05Эма СэмNo ratings yet
- Physiological Integrity Reduction of Risk PotentialDocument41 pagesPhysiological Integrity Reduction of Risk PotentialAndrew Isiah BonifacioNo ratings yet
- Dr. Lina ChoridahDocument8 pagesDr. Lina ChoridahAgung Kan AkuNo ratings yet
- The International Academy of Cytology Yokohama System For Reporting Breast Fine-Needle Aspiration Biopsy CytopathologyDocument17 pagesThe International Academy of Cytology Yokohama System For Reporting Breast Fine-Needle Aspiration Biopsy Cytopathologyunimo.prgNo ratings yet
- Biliary Tract Cancers: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Document96 pagesBiliary Tract Cancers: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)dragon_huboNo ratings yet
- CancerDocument51 pagesCancerShelly LyonsNo ratings yet
- Amedee 2001Document7 pagesAmedee 2001Hakim naufaldiNo ratings yet
- Oncology Nursing-2 PDFDocument22 pagesOncology Nursing-2 PDFHebsiba PonnayyanNo ratings yet
- Anterior Rhinoscopy-Hanan BakriDocument15 pagesAnterior Rhinoscopy-Hanan BakriMadalina DutanNo ratings yet
- Dermatologic and Cosmetic Procedures in Office Practice, Expert Consult - Online and Print 1st EsDocument48 pagesDermatologic and Cosmetic Procedures in Office Practice, Expert Consult - Online and Print 1st Esprogramgrabber67% (3)
- Surgery Chapter 1 SkinDocument6 pagesSurgery Chapter 1 Skinnandoooo86No ratings yet
- Biopsy TechniquesDocument31 pagesBiopsy Techniqueschouchou124No ratings yet
- Hematology - Oncology GlossaryDocument18 pagesHematology - Oncology GlossaryFran CescaNo ratings yet
- Ccs Sample QuestionsDocument20 pagesCcs Sample Questionscarrie0875% (44)