Professional Documents
Culture Documents
Failure of Physiological Transformation and Spiral
Uploaded by
Ecaterina Sorto de ArgeñalOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Failure of Physiological Transformation and Spiral
Uploaded by
Ecaterina Sorto de ArgeñalCopyright:
Available Formats
Expert Review ajog.
org
Failure of physiological transformation and spiral
artery atherosis: their roles in preeclampsia
Anne Cathrine Staff, MD, PhD; Heidi E. Fjeldstad, MD; Ingrid Knutsdotter Fosheim; Kjartan Moe, MD, PhD;
Gitta Turowski, MD, PhD; Guro Mørk Johnsen, MSc, PhD; Patji Alnaes-Katjavivi, MD, PhD; Meryam Sugulle, MD, PhD
Uterine spiral arteries
The blood to the uterus is supplied by the Physiological transformation with remodeling of the uteroplacental spiral arteries is key to
uterine arteries, arising from the internal a successful placentation and normal placental function. It is an intricate process that
iliac arteries and joined by blood supply involves, but is not restricted to, complex interactions between maternal decidual im-
from the ovarian arteries. The uterine mune cells and invasive trophoblasts in the uterine wall. In normal pregnancy, the
arteries deliver blood to the arcuate smooth muscle cells of the arterial tunica media of uteroplacental spiral arteries are
branches within the myometrium and replaced by invading trophoblasts and fibrinoid, and the arterial diameter increases 5- to
thereafter to the radial arteries, which 10-fold. Poor remodeling of the uteroplacental spiral arteries is linked to early-onset
continue on as spiral arteries.1 The basal preeclampsia and several other major obstetrical syndromes, including fetal growth
arteries branch from the distal ends of restriction, placental abruption, and spontaneous preterm premature rupture of mem-
branes. Extravillous endoglandular and endovenous trophoblast invasions have recently
From the Division of Obstetrics and been put forth as potential contributors to these syndromes as well. The well-
Gynaecology, Oslo University Hospital, Oslo, acknowledged disturbed extravillous invasion of maternal spiral arteries in preeclamp-
Norway (Drs Staff and Fjeldstad, Ms Fosheim, sia is summarized, as are briefly novel concepts of disturbed extravillous endoglandular
and Drs Moe, Johnsen, Alnaes-Katjavivi, and
and endovenous trophoblast invasions.
Sugulle); Faculty of Medicine, University of Oslo,
Oslo, Norway (Drs Staff and Fjeldstad, Ms Acute atherosis is a foam cell lesion of the uteroplacental spiral arteries associated with
Fosheim, and Drs Moe, Turowski, and Sugulle); poor remodeling. It shares some morphologic features with early stages of atheroscle-
Department of Obstetrics and Gynaecology, rosis, but several molecular differences between these lesions have also recently been
Baerum Hospital, Vestre Viken Hospital Trust,
revealed. Acute atherosis is most prevalent at the maternal-fetal interface, at the tip of
Drammen, Norway (Dr Moe); and Department of
Pathology, Oslo University Hospital, Oslo, the spiral arteries. The localization of acute atherosis downstream of poorly remodeled
Norway (Dr Turowski). arteries suggests that alterations in blood flow may trigger inflammation and foam cell
Received June 17, 2020; revised Sept. 4, 2020; development. Acute atherosis within the decidua basalis is not, however, confined to
accepted Sept. 19, 2020. unremodeled areas of spiral arteries or to hypertensive disorders of pregnancy and may
The Research Council of Norway funded part of even be present in some clinically uneventful pregnancies. Given that foam cells of
this acute atherosis work (PATH-study, grant atherosclerotic lesions are known to arise from smooth muscle cells or macrophages
number ref. 230652) as did South-Eastern activated by multiple types of inflammatory stimulation, we have proposed that multiple
Norway Regional Health Authority (the HAPPY-
forms of decidual vascular inflammation may cause acute atherosis, with or without poor
PATH-study, grant number ref. 2014026) (for
A.C.S., G.M.J. and M.S.). Oslo University remodeling and/or preeclampsia. Furthermore, we propose that acute atherosis may
Hospital and University of Oslo provided further develop at different gestational ages, depending on the type and degree of the inflam-
research support. matory insult.
The authors report no conflict of interest. This review summarizes the current knowledge of spiral artery remodeling defects and
A.C.S. has received, in kind, reagents for soluble acute atherosis in preeclampsia. Some controversies will be presented, including
fms-like tyrosine kinase 1 and placental growth endovascular and interstitial trophoblast invasion depths, the concept of 2-stage
factor biomarker analyses from Roche
trophoblast invasion, and whether the replacement of maternal spiral artery endothe-
Diagnostics (Rotkreuz, Switzerland). Roche
Diagnostics had no impact on the planning, lium by fetal endovascular trophoblasts is permanent. We will discuss the role of acute
performance, or other aspects of the biomarker atherosis in the pathophysiology of preeclampsia and short- and long-term health cor-
studies. relates. Finally, we suggest future opportunities for research on this intriguing utero-
This paper is part of a supplement. placental interface between the mother and fetus.
Corresponding author: Anne Cathrine Staff, MD,
Key words: decidua, hypertension, immunology, pathophysiology, placenta, pre-
PhD. uxnnaf@ous-hf.no or a.c.staff@medisin.
uio.no eclampsia, pregnancy, spiral artery
0002-9378
ª 2020 The Author(s). Published by Elsevier Inc. This is
an open access article under the CC BY license (http:// the radial arteries, supplying the basal endometrium undergoes hormone-
creativecommons.org/licenses/by/4.0/).
portion of the endometrium. In contrast, dependent structural changes during the
https://doi.org/10.1016/j.ajog.2020.09.026
the spiral arteries extend beyond the basal menstrual cycle. In pregnancy, this layer
endometrial layer, supplying the outer of the endometrium is transformed into a
functional layer. The outer layer of the “decidua,” destined to “fall off” (from the
FEBRUARY 2022 American Journal of Obstetrics & Gynecology S895
Expert Review ajog.org
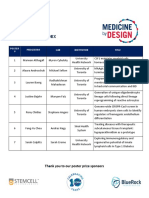
FIGURE 1
The different steps in uterine artery remodeling
The earliest step in vascular remodeling (stage 1) consists of endothelial vacuolation and some swelling in individual muscle cells. Invasion of stromal and
perivascular tissues by interstitial trophoblast is associated with further disorganization of the vascular smooth muscle layer (stage 2). Afterward,
endovascular trophoblast appears (stage 3). Trophoblast becomes embedded intramurally within a fibrinoid layer, which replaces the original vascular
smooth muscle (stage 4). Finally, reendothelialization occurs, which may be accompanied by the appearance of subintimal cushions containing a-actin
immunopositive myointimal cells (stage 5). Reproduced, with permission from the journal Placenta, from Pijnenborg et al.9.
Staff. Failure of physiological transformation and spiral artery atherosclerosis in preeclampsia. Am J Obstet Gynecol 2022.
Latin word “decidere”) at the end of Physiological transformation of higher numbers.5,6 As pregnancy pro-
pregnancy. The spiral arteries, approxi- spiral arteries gresses, uteroplacental blood flow in-
mately 50 to 100 mm in diameter in the Approximately 30 to 60 uterine spiral creases from 45 mL/min to 750 mL/min
nonpregnant state, penetrate the inner arteries are estimated to supply the at term, a dramatic increase in blood
part of the myometrium and the endo- intervillous space of the placenta and flow that is necessary for maintaining
metrium and are nonbranching end ar- maintain uteroplacental perfusion dur- adequate placental function4 and for
teries with a corkscrew shape.2,3 ing pregnancy,4 but other studies suggest meeting the high demands of the
S896 American Journal of Obstetrics & Gynecology FEBRUARY 2022
ajog.org Expert Review
growing fetus. These hemodynamic involves the incorporation of tropho- with decidual NK cells.23 We previously
changes are facilitated by massive phys- blasts into the vessel wall, where a fibri- reported that induction of Tregs
iological transformation of the spiral noid layer replaces the original vascular ameliorated intrauterine growth restric-
arteries,7,8 also known as spiral artery smooth muscle and elastic lamina.9 This tion in a transgenic rat model of pre-
remodeling.9 Expansive remodeling loss of smooth muscle cells converts the eclampsia.24 Recently, in a mouse model,
causes loss of smooth muscle cells and arteries into flaccid conduits.15,16 Stage 5 it was shown that Treg deprivation
their rich autonomic innervation, which involves maternal vascular repair with caused reduced maternal vascular adap-
in turn leads to functional changes in reendothelialization and subintimal tation in pregnancy.25 Insufficient
arterial wall reactivity, enhanced vaso- thickening.9 numbers or impaired function of Tregs is
dilation, and a major decrease in uterine As reviewed previously,17 the local linked to human reproductive disorders,
vascular resistance.4 The physiological uterine lining’s (decidual) immune sys- such as preeclampsia and recurrent im-
remodeling of the spiral arteries into tem is vital to spiral artery remodeling plantation failure or miscarriage.23
highly dilated thin-walled vessels is vital and thereby to successful placentation. Studies in mice have also indicated that
to human pregnancy development. There is increasing evidence for a role of pregnancy imprints Tregs with protec-
At the start of pregnancy, spiral artery both decidual natural killer (NK) cells tive memory to fetal antigens and that
remodeling by endovascular tropho- and T cells (including regulatory T cells these memory Tregs persist and rapidly
blasts has yet to begin.9 Before the [Tregs]) in facilitating uteroplacental accumulate during a subsequent
establishment of the uteroplacental cir- spiral artery remodeling.17 Placental pregnancy.26
culation during the first trimester of extravillous trophoblasts (EVTs) Another important finding is that
pregnancy, uterine glands provide his- invading the uterine spiral arteries are human decidual NK cells also possess
tiotrophic nutrition for the fetus.10 special in that they express only human some features of adaptive immunity. The
Before 9 weeks’ gestation, endovascular leukocyte antigen (HLA)-C among the decidual NK cells develop trained
(extravillous) trophoblast plugs limit classical polymorphic class I HLAs, as “memory” after a first pregnancy and
maternal blood entry into the inter- reviewed by us.18 HLA-C expressed on differ from decidual NK cells from a first
villous chambers. Plugging helps to EVTs is a key molecule that can elicit pregnancy in that they express higher
maintain a state of physiological hypoxia immune responses by both decidual NK levels of some receptors that interact
early in the placentation process, favor- cells and T cells. It is therefore essential with EVTs and growth factors that are
ing cytotrophoblast proliferation rather for a successful pregnancy that maternal- important for spiral artery remodeling,
than differentiation and invasiveness.11 fetal immune tolerance toward HLA-C is potentially promoting more efficient
After the disintegration of these plugs well established. Appropriate remodel- placentation in subsequent pregnan-
around 9 weeks’ gestation, the utero- ing requires successful interaction be- cies.27 Immune cells with pregnancy-
placental spiral arteries start to supply tween these fetal HLA-C proteins, and imprinted memory could be part of the
maternal blood to the intervillous killer cell immunoglobulinlike receptor reason why there is an additional risk of
space.12 (KIR) proteins, expressed on the preeclampsia in first pregnancies.17
The physiological spiral artery maternal decidual NK cells.19 KIR ge- Perhaps the effects of these immune
remodeling process has been divided netics have been shown to impact baby cells with pregnancy memory decline
into 5 stages by Pijnenborg et al9 weight percentiles and preeclampsia over time, which may explain why the
(Figure 1). Stage 1 (decidua-associated rates worldwide.20,21 T cells and the protective benefit of a previous preg-
early vascular remodeling) consists of adaptive immune system are also nancy conceived with the same partner is
endothelial vacuolization and swelling of involved, as HLA-C incompatibility be- lost after a long interpregnancy inter-
individual muscle cells.9 Craven et al13 tween the mother and fetus is associated val.28 However, more research is needed
highlight that initial vascular remodel- with increased T-cell activation and to investigate these hypotheses.
ing occurs in the absence of trophoblast generation of Tregs.22
invasion, whereas others point out that Decidual Tregs are essential to pro- Dysfunctional spiral artery
complete pregnancy-associated spiral moting maternal-fetal immune toler- remodeling in preeclampsia
artery remodeling cannot occur without ance, a mechanism central to ensuring A major contribution to the under-
trophoblasts.9,14 In stage 2, interstitial robust placentation and spiral artery standing of how failed spiral artery
trophoblasts invade stromal and peri- remodeling.23 Tregs contribute to im- transformation contributes to the
vascular tissue and induce further plantation and placental development by development of preeclampsia was made
disorganization of the vascular smooth several mechanisms. These include pre- by Robertson and Brosens. In 1967, they
muscle and weakening of the elastic venting destructive effector T-cell re- reported that preeclampsia is associated
lamina of the arteries. In stage 3, endo- sponses to fetal antigens, regulating with poor placentation, observed as
vascular extravillous trophoblasts enter other decidual immune cells and thus shallow remodeling of the uteroplacental
from the spiral artery lumen into the promoting an anti-inflammatory envi- spiral arteries.29 Some scientific contro-
vessel wall. Stage 4 (labeled by Pijnen- ronment, and by regulating maternal versies remain regarding the dysfunc-
borg as the physiological change) vascular changes through interaction tional nature of spiral artery remodeling
FEBRUARY 2022 American Journal of Obstetrics & Gynecology S897
Expert Review ajog.org
in preeclampsia.9 One controversy has intramurally and the spiral arteries are inadequate trophoblast-associated spiral
been Pijnenborg’s “2-wave” hypothesis reendothelialized by maternal endo- artery remodeling.9,17 Periconceptional
of trophoblast invasion,30 based on hys- thelial cells. In line with this, third- endometrial function, early decidual
terectomy specimens. This hypothesis trimester immunohistochemical find- vascular remodeling (before trophoblast
has been refuted by Lyall,2 who ings show that all spiral artery endo- invasion), and vascular plugging by tro-
concluded based on placental bed find- thelial cells are cytokeratin negative and phoblasts all play a role.11 Obesity and
ings that continuous endovascular therefore unlikely trophoblast derived.9 other risk factors for preeclampsia
migration from decidual to myometrial We35 and others32,39,40 have confirmed affecting the inflammatory state of the
arteries occurs, rather than 2 distinct this finding and further reported that endometrium likely confer risk partly
trophoblast invasion waves. Further- these cells are positive for the endo- through their effects on periconcep-
more, a common misunderstanding is thelial cell markers CD31 and von tional endometrial function17 and spiral
that both the interstitial and endovas- Willebrand factor. artery remodeling.47 Such risk factors
cular depths of trophoblast invasion are The failure of deep endovascular in- may cause defective maturation of
altered in preeclampsia. Interstitial vasion and spiral artery remodeling, as endometrial and decidual NK cells dur-
trophoblast invasion occurs before observed in early-onset preeclampsia, ing the secretory phase and early preg-
endovascular invasion9; however, in was previously assumed to lead to nancy,48 also contributing to poor
preeclampsia, the interstitial trophoblast placental underperfusion41 and thereby placentation.
invasion depth remains normal, whereas chronic hypoxia.42 A 2009 model by
the endovascular trophoblast invasion is Burton et al4 argued that flow volume is Extravillous trophoblast invasion
more shallow than in normotensive minimally affected by unsuccessful spiral failure: affecting more than the
pregnancies, as shown in detailed artery remodeling but that the utero- remodeling of uteroplacental spiral
placental bed studies by Lyall et al.31 placental perfusion has a more pulsatile arteries?
Whether the superficial decidua and higher pressure flow quality than The acknowledged disturbed extra-
basalis spiral arteries in preeclampsia are normally remodeled arteries, partly villous invasion of maternal spiral ar-
also severely affected by poor tropho- because of the remaining contractile teries in preeclampsia is summarized
blast invasion and failure of physiolog- smooth muscle cells. This abnormal flow above. Recent studies have however also
ical transformation, as reported by generates ischemia-reperfusion injury demonstrated extravillous glandular and
Labarrere et al,32 is also debatable. This is and placental oxidative stress rather than extravillous endovenous invasions,
not found in other decidua basalis chronic hypoxia per se.4 Furthermore, occurring early on during
studies.31,33e36 Differences among placental endoplasmic reticulum (ER) placentation.49e51 It is possible that
studies may however result from differ- stress is increased, and the unfolded adverse regulation of these processes
ences in patient selection, tissue collec- protein response is activated by this contributes to several obstetrical syn-
tion techniques (including localization abnormal flow.43 The dysfunctional dromes, including preeclampsia and
of biopsies from the placental bed and placental perfusion results in adverse FGR.
efficiency in spiral artery collection), placental function and release of in-
assessment of smaller nutritional basal flammatory placental factors.42 These The 2-stage model of preeclampsia:
arteries vs wider uteroplacental spiral factors mediate an excessive maternal more than remodeling problems
arteries, and immunohistochemical inflammatory response,42 involving We have proposed that incomplete spiral
markers. endothelial dysfunction and generalized artery remodeling along with other fac-
As Pijnenborg et al9 point out, a vascular inflammation, resulting in the tors contributing to poor placentation is
misconception is that endovascular observed clinical maternal features of 1 of several pathways increasing the risk
trophoblast invasion results in perma- preeclampsia.44 These inflammatory of preeclampsia.44,45 Poor placentation
nent replacement of maternal spiral factors are not fully defined but include increases the risk of early severe placental
artery endothelial cells by invading fetal syncytiotrophoblast microvesicles and dysfunction and “early-onset” pre-
trophoblasts. This concept was derived angiogenic factors, contributing to an eclampsia, with concomitant FGR.
from findings by Zhou et al,37,38 antiangiogenic imbalance in the “Late-onset” preeclampsia, without evi-
showing that endovascular tropho- maternal circulation (eg, elevated solu- dence of poor spiral artery remodeling
blasts normally transform their adhe- ble fms-like tyrosine kinase 1 and low and FGR, may be caused by over-
sion receptor phenotype and begin to placental growth factor [PlGF]),17,45 as crowding of the terminal villi in large
express endothelial markers, whereas observed in early-onset preeclampsia placentas and also by senescent pla-
those in preeclampsia fail to do so. As and fetal growth restriction (FGR), both centas.17,44,45 These pathways are how-
argued by Pijnenborg et al,9 maternal of which are placental syndromes char- ever not mutually exclusive and may
spiral artery endothelial cell replace- acterized by inadequately remodeled interact in causing placental dysfunction
ment by trophoblasts is only temporary spiral arteries.46 with cellular syncytiotrophoblast stress,
(Figure 1, stage 4), as these endovas- Of note, poor placentation and risk of resulting in the maternal syndromic
cular trophoblasts are then embedded preeclampsia involve much more than signs of preeclampsia caused by
S898 American Journal of Obstetrics & Gynecology FEBRUARY 2022
ajog.org Expert Review
FIGURE 2
Decidua basalis identification of spiral arteries and acute atherosis
Slides are stained with (from left to right) hematoxylin and eosin (H & E), desmin and PAS, CK7 and PAS, CD68 and PAS, and MSB. Representative images
of (A) a spiral artery from a normotensive control with complete physiological transformation, characterized by the presence of CK7-positive trophoblasts
and intramural fibrinoid (bright purple on PAS staining, white arrowhead) in the vessel wall, and complete absence of intramural smooth muscle cells (no
desmin stain). B, Spiral artery from a patient with preeclampsia with partial physiological transformation (both intramural fibrinoid and trophoblasts [CK7
positive] and areas with traces of mural smooth muscle cells [desmin positive]). C, Spiral artery with acute atherosis from the same sample as in (B),
lacking bright purple fibrinoid and CK7-positive trophoblasts in the vessel wall. Traces of intramural smooth muscle cells (desmin positive) are seen.
Fibrinoid necrosis is visible as a gray-pink material in the vessel wall (asterisk), which stains red on MSB staining (asterisk). Erythrocytes in the lumen of
the AA artery stain red-brown color on MSB staining. Intramural CD68-positive foam cells are present (black arrowhead). D, Spiral artery from a patient
with preeclampsia with almost complete physiological transformation (lack of desmin-positive smooth muscle cells, presence of CK7-positive tro-
phoblasts), yet acute atherosis lesion present (asterisk; fibrinoid necrosis, black arrowhead; foam cells, white arrowhead; purple physiological fibrinoid).
Reproduced, with permission from the journal Placenta, from Fosheim et al.35
CD68, cluster of differentiation 68; CK7, cytokeratin 7; H & E, hematoxylin and eosin; MSB, martius scarlet blue; PAS, periodic acid-Schiff staining.
Staff. Failure of physiological transformation and spiral artery atherosclerosis in preeclampsia. Am J Obstet Gynecol 2022.
generalized vascular inflammation. that all pathways trigger placental (syn- of preeclampsia accommodates most
Hence, we propose that the pathways to cytiotrophoblast) stress and similar known risk factors, including chronic
early- and late-onset preeclampsia may maternal responses but that FGR is more prepregnancy disease, primiparity, and
differ in the time course and underlying prevalent in early-onset preeclampsia as other pregnancy-related risk factors
causes but that the maternal signs of this preeclampsia form results mainly (including multiples).17 First, maternal
hypertension and other organ dysfunc- from early placental dysfunction with obesity, for instance, is a well-known risk
tion (eg, proteinuria) are the same. This severe adverse effects on fetal factor for both preeclampsia and gesta-
integrative concept takes into account growth.44,45 Our revised 2-stage model tional hypertension,52 a finding that fits
FEBRUARY 2022 American Journal of Obstetrics & Gynecology S899
Expert Review ajog.org
well with our concept of these hyper- inadequate physiological remodeling techniques and diagnostic criteria.59
tensive disorders representing a spec- and less deep endovascular trophoblast Acute atherosis assessment is not part
trum of disease, rather than distinct invasion).57,58 Acute atherosis lesions are of routine clinical practice because of the
entities.17 Second, maternal obesity usually focal,9,33,34 not necessarily need for careful tissue sampling and the
causes chronic inflammation, which affecting all spiral arteries, the entire time-consuming morphologic and
may contribute to reduced periconcep- circumference of a single artery, or its immunohistochemical investigations
tional endometrial function and entire length. Apart from the placental after delivery. Hitherto, there is no
dysfunctional spiral artery remodeling, bed, acute atherosis may be found in the available noninvasive imaging strategy to
in turn resulting in increased early- decidua parietalis,56,58,59 where there is reliably identify uteroplacental acute
onset preeclampsia risk. Third, no physiological transformation of the atherosis.
maternal obesity is also associated with spiral arteries. These lesions are however Various tissue sampling techniques
large placentas and fetal macrosomia,53 not found outside the uterus. Figure 2 have been used to investigate acute
thereby potentially contributing to (reproduced with permission from atherosis, including rare whole uterus
placental overcrowding and late-onset Fosheim35) shows examples of decidual specimens with placenta in situ (from
preeclampsia or gestational hyperten- acute atherosis in serial tissue section postpartum hysterectomies),67 placental
sion risk. In line with this, maternal staining. bed biopsies (including decidual and
obesity is a risk factor for poor spiral The time course of acute atherosis myometrial tissues),31,68 vacuum curet-
artery remodeling across several development is not definitively known, tage of the placental bed (published by us
placental syndromes.47 Incomplete as longitudinal biopsies for histologic in 1999),68e70 biopsies from the basal
spiral artery remodeling and resulting studies are infeasible. Decidual acute plate of the delivered placenta, and
placental dysfunction are however not atherosis has been observed as early as placental membranes (providing
unique to preeclampsia but are associ- the first trimester of pregnancy in decidua parietalis, not the decidua
ated with a spectrum of severe obstet- women with chronic autoimmune dis- basalis of the placental bed).61,68 As
rical outcomes.54 These include eases characterized by excessive inflam- summarized in a state-of-the-art paper
(recurrent) pregnancy loss, FGR, pre- mation (eg, systemic lupus on optimizing sample collection for
term premature rupture of membranes, erythematosus [SLE] with anti- placental research,71 our technique of
intrauterine fetal demise, and placental phospholipid syndrome).60 Delivery of decidual vacuum suction of the placental
abruption.47 Similar to how dysfunc- the placenta is followed by gradual bed during cesarean delivery68e70 rep-
tional spiral artery remodeling may not shedding of the remaining decidual tis- resents the superior sampling method if
be a prerequisite for all forms of pre- sue (where the lesion is most prevalent) one wishes to study the decidua basalis
eclampsia, it is well documented that over a few weeks, and the lesion likely alone.71 Studies examining conventional
FGR and other placental syndromes regresses soon after delivery,18 as placental tissue samples have found a
may occur in the absence of spiral artery confirmed by small autopsy studies.56 higher frequency of acute atherosis in the
remodeling dysfunction. The rate of acute atherosis is elevated fetal membranes, relative to tissue sam-
in preeclampsia compared with that in ples from the maternal surface of the
Acute atherosis: what, where, and normotensive pregnancies but not all placenta.61,72 However, the rate of acute
when? preeclampsia pregnancies are atherosis is lower in fetal membranes
Hertig55 described in 1945 spiral artery affected.34,61e63 Acute atherosis also af- when directly compared with vacuum-
wall lesions characterized by foam cells fects some pregnancies complicated by suctioned decidual tissue from the
and fibrinoid necrosis of the tunica FGR or diabetes mellitus (without placental bed.59 This is not surprising, as
media. This finding was later termed maternal hypertension),34,64 SLE and most acute atherosis lesions are present
acute atherosis by Zeek and Assali56 in antiphospholipid syndrome,65 and even in the decidua basalis.57,58 Advantages
1950. Fibrinoid necrosis and peri- sometimes normotensive uncompli- of the decidual vacuum suction meth-
vascular infiltrate, the features often used cated pregnancies.34,57,63,66 Our decidua odology compared with that of tradi-
to define acute atherosis in addition to basalis studies suggest that the foam cell tional biopsies from the placental bed
foam cells, have themselves been poorly lesions are much rarer in normotensive and maternal surface of the placenta
and heterogeneously defined,34 making uncomplicated pregnancies than in include the following: (1) tissue yield is
comparisons of studies challenging. preeclamptic pregnancies and that the larger; (2) decidual tissue is collected
Acute atherosis usually occurs down- lesions, when present, are smaller and from the whole placental bed in an
stream in inadequately remodeled spiral affect fewer arteries.34 The reported rates unbiased way; and (3) it is easy and
arteries, namely, at their tips, in the of acute atherosis vary from 10% to 52% rapid and does not lead to short- or
decidua basalis. More rarely, acute in preeclampsia and from 0.4% to 11% long-term complications when per-
atherosis is found in the myometrial in normotensive pregnancies.34,61e63 formed by experienced clinicians.68
segments, which is the compartment This huge variation likely reflects dif- One drawback is that the tissue lacks
where the potential spiral artery ferences in the populations investigated orientation, in contrast to placental bed
remodeling problems are seen (eg, and the heterogeneous sampling biopsies. An issue that affects acute
S900 American Journal of Obstetrics & Gynecology FEBRUARY 2022
ajog.org Expert Review
atherosis evaluation irrespective of the We have proposed that acute atherosis clue to its origins. The lesion is found
sampling method is that the diagnostic may be the histologic manifestation of mainly in the tips of the spiral arteries, in
criteria have not always been clear from several decidual inflammatory mecha- the decidual end and is not found in
all studies. Our recently published, nisms leading to arterial damage.18 other maternal arteries outside the
simple, and reproducible set of criteria These underlying mechanisms may uterine wall. We propose that the
have proven useful when comparing the vary in timing and intensity during a decidual spiral artery tips are particularly
rates of acute atherosis across preg- pregnancy, explaining the association of prone to arterial damage because of their
nancy outcome groups and among preeclampsia and a plethora of preg- colocalization with cells from a geneti-
different tissue sources.34,59 Based on nancy complications with the lesion.18 cally distinct fetus, including invading
the ubiquity of perivascular infiltrate This is in line with our 2-stage model extravillous trophoblasts. Dysregulated
and fibrinoid, our simplified definition of the complex preeclampsia syndrome, local maternal tolerization to these allo-
is based on identifying at least 2 adja- including heterogeneous pathways and geneic trophoblasts is likely 1 aspect of
cent foam cells in the spiral artery wall risk factors for both early- and late-onset poor placentation18,76,78 and may also
that are also CD68 positive.34,35,73 preeclampsia (summarized above in play a role in the development of acute
Other researchers, also acknowledging “Extravillous trophoblast invasion fail- atherosis.
that all 3 classically required compo- ure: affecting more than the remodeling Finally, altered hemodynamics may
nents of acute atherosis are not always of uteroplacental spiral arteries?”).17,44,45 lead to acute atherosis. The localization
present, have used the terminology In our model, acute atherosis may not of acute atherosis, usually downstream
decidual vasculopathy for these spiral only be a consequence of placental of unremodeled spiral arteries in the
artery pathologies.62 dysfunction and the result of its under- myometrial part of the spiral arteries, is
lying mechanisms but also be a risk also consistent with hemodynamic risk
Acute atherosis in preeclampsia: factor for placental dysfunction, as factors playing a role in its pathogenesis.
why? illustrated in our 2014 model shown in Altered laminar blood flow caused by
The causes and consequences of acute Figure 3 (reproduced with permission incomplete remodeling likely promotes
atherosis in preeclampsia and other from the American Journal of Obstetrics endothelial shear stress, thus stimu-
obstetrical syndromes mediated by & Gynecology).18 lating foam cell generation. This is
placental dysfunction are not completely The mechanisms mediating placental similar to the formation of atheroscle-
understood. Although more rare and less dysfunction may also cause acute athe- rotic lesions, tending to localize beyond
extensive, the lesion’s presence in clini- rosis; we propose several, potentially arterial branching points in areas of
cally uncomplicated pregnancies34 has synergistic, pathways to acute atherosis altered blood flow patterns.76 We have
also been an enigma. To shed light on the involving inflammatory, immunoge- suggested that the pathways outlined
associations linking acute atherosis and netic, and hemodynamic risks,18,65,76 as above, alone or in combination, may
placental dysfunction, breaking down shown in Figure 4. Firstly, decidual lead to a common endpoint, namely,
the characteristics of the lesion may be inflammation may be a sufficient cause inflammatory stimulation of foam cell
useful. of acute atherosis. We have put forward formation, and thereby acute atherosis
The immunohistochemical hallmark that uteroplacental acute atherosis could lesions.18
of acute atherosis is CD68-positive develop at any stage of pregnancy in the Once present, the acute atherosis le-
subendothelial lipid-filled foam cells. setting of sufficient decidual inflamma- sions may themselves contribute to
CD68 is part of the scavenger receptor tion,18 including in normotensive preg- further placental dysfunction. Acute
family and can bind and internalize nancies. This is in line with findings that atherosis narrows the spiral artery
oxidized low-density lipoprotein some women develop acute atherosis lumina, exacerbating dysfunctional
(LDL). Foam cells themselves are very early in pregnancy, in situations of uteroplacental flow.4,65 The greater the
products of inflammatory stress, typi- excessive prepregnancy and early preg- number of spiral arteries affected in a
cally of the intima, and are character- nancy vascular inflammation, such as in pregnancy, the more likely it is to lead to
istic of early stages of atherosclerosis.74 SLE.60 This is not surprising, as it has exacerbation of placental dysfunction,
In atherosclerosis, foam cells have become widely recognized that immu- with oxidative and ER cellular stress
been shown to derive from both mac- nity and inflammation play a key role in responses,18,76 as seen in preeclampsia.
rophages and smooth muscle cells.75 the pathogenesis of arterial diseases The acute atherosis lesions are also
Foam cells are not, however, specific to affecting all wall layers of the arteries, at associated with an increased rate of
atherosclerosis but may form in several all levels of the arterial tree, including local arterial thrombosis9,34,79,80 and
inflammatory states (as reviewed in smaller vessels,77 where the spiral ar- thereby increased risk of downstream
Staff et al76). Like foam cells, myointi- teries belong to the latter group. placental ischemia and infarctions.29
mal cell proliferation and fibrinoid ne- Secondly, immunologic mechanisms Clinically, acute atherosis lesions in
crosis, the 2 other defining features of are likely important for acute atherosis preeclampsia have been associated with
acute atherosis, are also markers of development. The localization of acute more severe disease forms, including
arterial injury. atherosis is intriguing and may provide a preterm delivery and FGR,59,64,72 both
FEBRUARY 2022 American Journal of Obstetrics & Gynecology S901
Expert Review ajog.org
(acute atherosis only affects the small
FIGURE 3
spiral arteries, in contrast to atheroscle-
A multistage 2014 preeclampsia placenta model rosis affecting much larger arteries), and
artery wall composition. Atherosclerotic
lesions are more complex and develop
plaques that may rupture.
The histologic similarities between
acute atherosis and graft vascular disease
have also been highlighted for several
decades,29,82 although subendothelial
foam cell lesions are less prominent in
the latter. Fibrinoid necrosis and intimal
hyperplasia are however a shared feature,
and both types of lesions involve peri-
vascular lymphocyte infiltration, com-
plement,83 and immunoglobulin
deposits. Strikingly, the arterial lesions of
graft vascular disease and acute atherosis
both occur at the boundaries between
tissues from genetically distinct in-
dividuals, as reviewed by us.18 Both
allograft rejection and preeclampsia
correlate with the presence of circulating
angiotensin II type 1 receptor agonistic
autoantibody (AT1-AA),84 but our study
did not find increased rates of this
autoantibody in preeclampsia with acute
atherosis compared with that of pre-
eclampsia without acute atherosis.85
However, in line with the hypothesis
that acute atherosis shares certain mo-
The model recognizes preplacentation factors leading to poor placentation and suggests utero- lecular pathways with graft vessel disease
placental acute atherosis as part of a multistep pathway of preeclampsia. In this model, acute and acute atherosis, we,83 like others
atherosis may be both a consequence of any form of placental dysfunction and the results of its previously,86 have found presence of
underlying mechanisms, including remodeling problems. Furthermore, the model also proposes that complement around uteroplacental
acute atherosis may represent a risk factor for placental dysfunction and preeclampsia. This is in line decidual spiral arteries afflicted with
with acute atherosis developing very early in women with excessive vascular inflammation, such as acute atherosis.82
in systemic lupus erythematosus, who also have a high risk for developing early-onset preeclampsia. When comparing decidual “tissue”
Reproduced (own figure), with permission from the Journal of Reproductive Immunology, from Staff features of preeclampsia and normo-
et al.18 tensive pregnancies, we previously
Staff. Failure of physiological transformation and spiral artery atherosclerosis in preeclampsia. Am J Obstet Gynecol 2022.
demonstrated excessive tissue inflam-
mation in preeclampsia, with increased
content of lipids (total cholesterol,
well known to further increase the risk partly differing etiologies. We have pre- phospholipids, and triglycerides)70 and
of premature cardiovascular disease af- viously argued that acute atherosis and increased levels of 8-isoprostane,69 a
ter preeclampsia.81 This suggests a link atherosclerosis share inflammatory marker of oxidative stress, and increased
between this short-term manifestation mechanisms for foam cell generation but phospholipase A2 activity decidual tis-
of uteroplacental arterial damage and that acute atherosis likely has additional, sue,87 the latter liberating 8-isoprostane
chronic damage to the systemic pregnancy-specific underlying mecha- from tissue phospholipids. We also
maternal cardiovasculature. nisms.18 As argued by us,18,76 although showed in vitro that 8-isoprostane af-
macrophage-derived foam cells repre- fects trophoblast function, including
Acute atherosis: molecular pathways sent a shared feature of acute atherosis matrix metalloproteinase, NF-kappa B,
Acute atherosis was named after its and atherosclerotic lesions of larger ar- and LOX-1 activities.88,89 Our renin-
morphologic resemblance of early teries, the lesions differ with respect to angiotensin system studies also demon-
atherosclerosis stages, but the lesions time course (long vs short develop- strated its local up-regulation in the
have several differing features and likely ment), the size of the artery affected decidua compared with that in placental
S902 American Journal of Obstetrics & Gynecology FEBRUARY 2022
ajog.org Expert Review
tissues and a 5-fold up-regulation of
FIGURE 4
decidual expression of the angiotensin II
type 1 receptor in preeclampsia
Multiple pathways to the decidua parietalis acute atherosis formation
compared with that of normotensive
pregnancies.84
As for comparing “cellular” features
of acute atherosis and early athero-
sclerosis, we have in our decidual
studies found evidence of both differ-
ences and similarities. Most arterial
injuries begin with endothelial
dysfunction and activation,90 but in
our recent study, immunohistochem-
ical evidence of endothelial activation
was lacking in most decidua basalis
spiral arteries with acute atherosis,
with the absence of intercellular adhe-
sion molecule 1 (ICAM-1) expres-
sion.35 Labarrere et al32 found evidence
of ICAM-1 expression in decidua
basalis spiral arteries with acute athe-
rosis, but the authors studied mainly
nonremodeled arteries, in contrast to
our work.35 We did however find other
evidence of endothelial abnormalities We propose several, potentially synergistic, pathways to acute atherosis, involving inflammatory,
in acute atherosis lesions, character- immunogenetic, and hemodynamic risks.18,65,76
ized by weak CD31 staining, possibly Staff. Failure of physiological transformation and spiral artery atherosclerosis in preeclampsia. Am J Obstet Gynecol 2022.
secondary to cellular stress. Our find-
ings35 and the findings of others66,91 of
fibrinoid necrosis in acute atherosis of pathways lead to decidual acute of cardiovascular death.81 We have sug-
the arterial wall (colored red by Mar- atherosis.18 gested that the subset of women who
tius scarlet blue [MSB] staining and Similarities among the circulating develop acute atherosis lesions in preg-
gray-pink by periodic acid-Schiff biomarkers also exist between acute nancy may have increased risk of
[PAS] staining)35 are consistent with atherosis and atherosclerosis. Another of atherosclerotic disease later in life.18,65
an altered local endothelial phenotype, our recent papers suggests that older Acute atherosis may represent an accel-
likely leaking factors from the maternal women with decidual acute atherosis erated atherosclerotic process, driven by
circulation into the vessel wall, depos- (both preeclamptic and normotensive the dramatic physiological changes that
iting fibrin or fibrinlike (fibrinoid) pregnancies) have a lipidemic profile occur in pregnancy. We have proposed
material. Our recent immunohisto- resembling that of patients with athero- that diagnosing acute atherosis thereby
chemical investigations confirmed that sclerosis, including elevated levels of could aid in better targeting preeclamptic
perivascular infiltrates were not apolipoprotein B and LDL.94 Further- women at higher risk of long-term car-
consistently present or large around all more, we recently showed that the diovascular disease,76 and our findings of
acute atherosis lesions and that adap- presence of decidual acute atherosis or dyslipidemia in the follow-up of older
tive CD4 helper T cells may be other evidences of placental dysfunction pregnant women with acute atherosis
involved, whereas the presence of Tregs (eg, low levels of PlGF) was associated support this notion.94 This concept has
(FOXP3þ) was almost absent,73 again with dysregulated patterns of circulating also been followed up by Veerbeek et al96
demonstrating similarities and dis- cardiovascular diseaseerelated multi- and Stevens et al,97 the latter study
crepancies relative to early atheroscle- plex biomarkers at delivery,95 support- demonstrating an adverse cardiovascular
rosis lesions.92 The recent findings of a ing our model of potentially shared risk profile at 7 months after delivery in
more prevalent proinflammatory mechanisms. women with a history of preeclampsia
macrophage phenotype in the decidua and decidual vasculopathy. However,
basalis with acute atherosis and an Acute atherosis and long-term both short- and long-term studies of
intravascular monocyte source for maternal health acute atherosis are potentially hampered
macrophages in acute atherosis93 sup- Pregnancy is seen as a stress test for future with the challenges in obtaining enough
port our hypothesis that both tissue- maternal health, and preeclampsia is tissue for optimal diagnosis of decidual
based and circulation-based cellular associated with 2- to 8-fold increased risk acute atherosis.59
FEBRUARY 2022 American Journal of Obstetrics & Gynecology S903
Expert Review ajog.org
Early stages of atherosclerosis are genomes. Dissecting its molecular pa- II. Functional and immunological investigations
reversible, and statins have been shown thology and interaction with environ- of the placental bed. Am J Obstet Gynecol
2019;221:457–69.
to confer antiatherogenic and anti- mental and modifiable risk factors is 9. Pijnenborg R, Vercruysse L, Hanssens M.
inflammatory effects in large clinical likely to uncover biologic understanding The uterine spiral arteries in human pregnancy:
trials.98 We have therefore put forward relevant to many human diseases, in facts and controversies. Placenta 2006;27:
that use of statins in established pre- addition to refining our conceptions and 939–58.
eclampsia may ameliorate acute athe- models of preeclampsia. 10. Burton GJ, Watson AL, Hempstock J,
Skepper JN, Jauniaux E. Uterine glands provide
rosis, thereby improving uteroplacental Finally, whether acute atherosis in histiotrophic nutrition for the human fetus during
perfusion and pregnancy outcome.18 In pregnancy truly correlates with exces- the first trimester of pregnancy. J Clin Endocrinol
support of this, small clinical studies of sive cardiovascular risk18,65,96,97 is still Metab 2002;87:2954–9.
statins used in women with anti- an intriguing topic for further 11. Red-Horse K, Zhou Y, Genbacev O, et al.
phospholipid syndrome presenting with investigation. - Trophoblast differentiation during embryo im-
plantation and formation of the maternal-fetal
preeclampsia or FGR have shown interface. J Clin Invest 2004;114:744–54.
promising results with improved utero- ACKNOWLEDGMENTS 12. Jauniaux E, Poston L, Burton GJ.
placental perfusion, although random- The authors would like to express gratitude to Placental-related diseases of pregnancy:
ized trials are lacking.99 Whether Profs Emeriti Chris Redman (Oxford, United involvement of oxidative stress and implica-
postpartum statins or other pharmaco- Kingdom) and Robert Pijnenborg (Leuven, tions in human evolution. Hum Reprod Update
Belgium) for their excellent mentorship and 2006;12:747–55.
logic anti-inflammatory interventions 13. Craven CM, Morgan T, Ward K. Decidual
inspiration and for our joint work in the field of
(eg, metformin) following preeclampsia spiral artery remodelling begins before cellular
preeclampsia and vascular remodeling. Our
or acute atherosis would be useful to long-lasting collaboration with Prof Ralf interaction with cytotrophoblasts. Placenta
women in delaying atherosclerosis pro- Dechend (Berlin, Germany) has been invaluable 1998;19:241–52.
gression and improving long-term car- to our interdisciplinary translational research 14. King A, Loke YW. Placental vascular
work. For their extensive contributions in remodelling. Lancet 1997;350:220–1.
diovascular health is neither known nor 15. Burton GJ, Charnock-Jones DS,
unveiling some of the mysteries of acute athe-
tested. Jauniaux E. Regulation of vascular growth and
rosis, the assistance of all participants of our
research group, in particular Nina Kittelsen function in human placenta. Reproduction
Remaining enigmas of acute Harsem and Gro Leite Størvold, and other col- 2009;138:895–902.
atherosis laborators is greatly appreciated. 16. Harris LK. IFPA Gabor Than Award lecture:
transformation of the spiral arteries in human
We are still far from understanding all pregnancy: key events in the remodelling time-
molecular, immunologic, genetic, and line. Placenta 2011;32(Suppl2):S154–8.
environmental mechanisms leading to REFERENCES 17. Staff AC. The two-stage placental model of
the different clinical presentations of the 1. Boyd JD, Hamilton WJ. The human placenta. preeclampsia: an update. J Reprod Immunol
placental syndromes, including pre- Cambridge, England: Heffner & Sons Ltd; 1970: 2019;134(5):1–10.
253–66. 18. Staff AC, Johnsen GM, Dechend R,
eclampsia and acute atherosis. Areas that
2. Lyall F. The human placental bed revisited. Redman CWG. Preeclampsia and uteropla-
merit more research are preimplantation Placenta 2002;23:555–62. cental acute atherosis: immune and inflamma-
heterogeneity, the decidua-related 3. Brosens I, Benagiano M, Puttemans P, tory factors. J Reprod Immunol 2014;101e2:
(trophoblast-independent) vascular D’Elios MM, Benagiano G. The placental bed 120–6.
remodeling processes, trophoblast inva- vascular pathology revisited: a risk indicator for 19. Robson A, Harris LK, Innes BA, et al. Uterine
cardiovascular disease. J Matern Fetal Neonatal natural killer cells initiate spiral artery remodeling
sion routes (arterial, venous, and glan- in human pregnancy. FASEB J 2012;26:
Med 2019;32:1556–64.
dular), decidual and immune cell 4. Burton GJ, Woods AW, Jauniaux E, 4876–85.
interactions, and cytokine and growth Kingdom JC. Rheological and physiological 20. Nakimuli A, Chazara O, Hiby SE, et al. A KIR
factor production before and during consequences of conversion of the maternal B centromeric region present in Africans but not
trophoblast invasion. The cellular pre- spiral arteries for uteroplacental blood flow dur- Europeans protects pregnant women from pre-
ing human pregnancy. Placenta 2009;30: eclampsia. Proc Natl Acad Sci U S A 2015;112:
cursors of acute atherosis foam cells may 845–50.
473–82.
include trophoblast cells89 in addition to 5. Espinoza J, Romero R, Mee Kim Y, et al. 21. Hiby SE, Apps R, Chazara O, et al. Maternal
activated macrophages and smooth Normal and abnormal transformation of the KIR in combination with paternal HLA-C2 regu-
muscle cells75 and should be further spiral arteries during pregnancy. J Perinat Med late human birth weight. J Immunol 2014;192:
detailed. Emerging studies demon- 2006;34:447–58. 5069–73.
6. Brosens I, Pijnenborg R, Vercruysse L, 22. Tilburgs T, Scherjon SA, van der Mast BJ,
strating accelerated placental aging in
Romero R. The “Great Obstetrical Syndromes” et al. Fetal-maternal HLA-C mismatch is asso-
early-onset preeclampsia and auto- are associated with disorders of deep placen- ciated with decidual T cell activation and induc-
phagy100,101 are worth pursuing, also in tation. Am J Obstet Gynecol 2011;204: tion of functional T regulatory cells. J Reprod
the setting of other placental syndromes 193–201. Immunol 2009;82:148–57.
with remodeling defects. As argued 7. Brosens I, Robertson WB, Dixon HG. The 23. Robertson SA, Care AS, Moldenhauer LM.
physiological response of the vessels of the Regulatory T cells in embryo implantation and
previously,17 preeclampsia represents a the immune response to pregnancy. J Clin Invest
placental bed to normal pregnancy. J Pathol
complex and multifaceted syndrome, as Bacteriol 1967;93:569–79. 2018;128:4224–35.
it involves several genomes; the maternal 8. Harris LK, Benagiano M, D’Elios MM, 24. Przybyl L, Ibrahim T, Haase N, et al. Regu-
(oocyte and uterine), paternal, and fetal Brosens I, Benagiano G. Placental bed research: latory T cells ameliorate intrauterine growth
S904 American Journal of Obstetrics & Gynecology FEBRUARY 2022
ajog.org Expert Review
retardation in a transgenic rat model for pre- 39. Labarrere CA, Faulk WP. Antigenic identifi- birthweight and placental weight. Does maternal
eclampsia. Hypertension 2015;65:1298–306. cation of cells in spiral artery trophoblastic inva- diabetes matter? A population study of 106 191
25. Care AS, Bourque SL, Morton JS, sion: validation of histologic studies by triple- pregnancies. Acta Obstet Gynecol Scand
Hjartarson EP, Robertson SA, Davidge ST. antibody immunocytochemistry. Am J Obstet 2016;95:1162–70.
Reduction in regulatory T cells in early pregnancy Gynecol 1994;171:165–71. 54. Redman CW. Current topic: pre-eclampsia
causes uterine artery dysfunction in mice. Hy- 40. Lyall F, Bulmer JN, Duffie E, Cousins F, and the placenta. Placenta 1991;12:301–8.
pertension 2018;72:177–87. Theriault A, Robson SC. Human trophoblast 55. Hertig AT. Vascular pathology in the hyper-
26. Rowe JH, Ertelt JM, Xin L, Way SS. Preg- invasion and spiral artery transformation. Am J tensive albuminuric toxemias of pregnancy.
nancy imprints regulatory memory that sustains Pathol 2001;158:1713–21. Clinics 1945;4:602–14.
anergy to fetal antigen. Nature 2012;490:102–6. 41. Roberts JM, Redman CW. Pre-eclampsia: 56. Zeek PM, Assali NS. Vascular changes in
27. Gamliel M, Goldman-Wohl D, Isaacson B, more Than pregnancy-induced hypertension. the decidua associated with eclamptogenic
et al. Trained memory of human uterine NK cells Lancet 1993;341:1447–51. toxemia of pregnancy. Am J Clin Pathol
enhances their function in subsequent preg- 42. Redman CW, Sacks GP, Sargent IL. Pre- 1950;20:1099–109.
nancies. Immunity 2018;48:951–62.e5. eclampsia: an excessive maternal inflammatory 57. Meekins JW, Pijnenborg R, Hanssens M,
28. Skjærven R, Wilcox AJ, Lie RT. The interval response to pregnancy. Am J Obstet Gynecol van Assche A, McFadyen IR. Immunohisto-
between pregnancies and the risk of pre- 1999;180:499–506. chemical detection of lipoprotein(a) in the wall of
eclampsia. N Engl J Med 2002;346:33–8. 43. Burton GJ, Yung HW, Cindrova-Davies T, placental bed spiral arteries in normal and severe
29. Robertson WB, Brosens I, Dixon HG. The Charnock-Jones DS. Placental endoplasmic preeclamptic pregnancies. Placenta 1994;15:
pathological response of the vessels of the reticulum stress and oxidative stress in the 511–24.
placental bed to hypertensive pregnancy. pathophysiology of unexplained intrauterine 58. Robertson WB, Brosens I, Dixon G. Utero-
J Pathol Bacteriol 1967;93:581–92. growth restriction and early onset preeclampsia. placental vascular pathology. Eur J Obstet
30. Pijnenborg R, Bland JM, Robertson WB, Placenta 2009;30(SupplA):S43–8. Gynecol Reprod Biol 1975;5:47–65.
Brosens I. Uteroplacental arterial changes 44. Redman CW, Sargent IL, Staff AC. IFPA 59. Alnaes-Katjavivi P, Roald B, Staff AC. Ute-
related to interstitial trophoblast migration in Senior Award Lecture: making sense of pre- roplacental acute atherosis in preeclamptic
early human pregnancy. Placenta 1983;4: eclampsia - two placental causes of pre- pregnancies: rates and clinical outcomes differ
397–413. eclampsia? Placenta 2014;35(Suppl):S20–5. by tissue collection methods. Pregnancy
31. Lyall F, Robson SC, Bulmer JN. Spiral artery 45. Redman CW, Staff AC. Preeclampsia, bio- Hypertens 2020;19:11–7.
remodeling and trophoblast invasion in pre- markers, syncytiotrophoblast stress, and 60. Nayar R, Lage JM. Placental changes in a
eclampsia and fetal growth restriction: relation- placental capacity. Am J Obstet Gynecol first trimester missed abortion in maternal sys-
ship to clinical outcome. Hypertension 2013;62: 2015;213(Suppl4):S9.e1–11. temic lupus erythematosus with antiphospholipid
1046–54. 46. Brosens I, Puttemans P, Benagiano G. syndrome; a case report and review of the liter-
32. Labarrere CA, DiCarlo HL, Bammerlin E, Placental bed research: I. The placental bed: ature. Hum Pathol 1996;27:201–6.
et al. Failure of physiologic transformation of from spiral arteries remodeling to the great 61. Kim YM, Chaemsaithong P, Romero R, et al.
spiral arteries, endothelial and trophoblast cell obstetrical syndromes. Am J Obstet Gynecol The frequency of acute atherosis in normal
activation, and acute atherosis in the basal plate 2019;221:437–56. pregnancy and preterm labor, preeclampsia,
of the placenta. Am J Obstet Gynecol 2017;216: 47. Avagliano L, Bulfamante GP, Morabito A, small-for-gestational age, fetal death and mid-
287.e1–16. Marconi AM. Abnormal spiral artery remodelling trimester spontaneous abortion. J Matern Fetal
33. Meekins JW, Pijnenborg R, Hanssens M, in the decidual segment during pregnancy: from Neonatal Med 2015;28:2001–9.
McFadyen IR, van Asshe A. A study of placental histology to clinical correlation. J Clin Pathol 62. Stevens DU, Al-Nasiry S, Bulten J,
bed spiral arteries and trophoblast invasion in 2011;64:1064–8. Spaanderman ME. Decidual vasculopathy and
normal and severe pre-eclamptic pregnancies. 48. Rabaglino MB, Post Uiterweer ED, adverse perinatal outcome in preeclamptic
Br J Obstet Gynaecol 1994;101:669–74. Jeyabalan A, Hogge WA, Conrad KP. Bioinfor- pregnancy. Placenta 2012;33:630–3.
34. Alnaes-Katjavivi P, Lyall F, Roald B, matics approach reveals evidence for impaired 63. Harsem NK, Roald B, Braekke K, Staff AC.
Redman CW, Staff AC. Acute atherosis in vac- endometrial maturation before and during early Acute atherosis in decidual tissue: not associated
uum suction biopsies of decidua basalis: an pregnancy in women who developed pre- with systemic oxidative stress in preeclampsia.
evidence based research definition. Placenta eclampsia. Hypertension 2015;65:421–9. Placenta 2007;28:958–64.
2016;37:26–33. 49. Moser G, Windsperger K, Pollheimer J, de 64. Khong TY. Acute atherosis in pregnancies
35. Fosheim IK, Alnaes-Katjavivi P, Redman C, Sousa Lopes SC, Huppertz B. Human tropho- complicated by hypertension, small-for-
Roald B, Staff AC, Størvold GL. Acute atherosis blast invasion: new and unexpected routes and gestational-age infants, and diabetes mellitus.
of decidua basalis; characterization of spiral ar- functions. Histochem Cell Biol 2018;150: Arch Pathol Lab Med 1991;115:722–5.
teries, endothelial status and activation. 361–70. 65. Staff AC, Dechend R, Pijnenborg R.
Placenta 2019;82:10–6. 50. Moser G, Weiss G, Sundl M, et al. Extra- Learning from the placenta: acute atherosis
36. Brosens IA, Robertson WB, Dixon HG. The villous trophoblasts invade more than uterine and vascular remodeling in preeclampsia-
role of the spiral arteries in the pathogenesis of arteries: evidence for the invasion of uterine novel aspects for atherosclerosis and future
preeclampsia. Obstet Gynecol Annu 1972;1: veins. Histochem Cell Biol 2017;147:353–66. cardiovascular health. Hypertension 2010;56:
177–91. 51. Windsperger K, Dekan S, Pils S, et al. 1026–34.
37. Zhou Y, Fisher SJ, Janatpour M, et al. Hu- Extravillous trophoblast invasion of venous as 66. Katabuchi H, Yih S, Ohba T, et al. Charac-
man cytotrophoblasts adopt a vascular pheno- well as lymphatic vessels is altered in idiopathic, terization of macrophages in the decidual athe-
type as they differentiate. A strategy for recurrent, spontaneous abortions. Hum Reprod rotic spiral artery with special reference to the
successful endovascular invasion? J Clin Invest 2017;32:1208–17. cytology of foam cells. Med Electron Microsc
1997;99:2139–51. 52. Egeland GM, Klungsøyr K, Øyen N, Tell GS, 2003;36:253–62.
38. Zhou Y, Damsky CH, Fisher SJ. Pre- Næss Ø, Skjærven R. Preconception cardio- 67. Brosens I. How the role of the spiral arteries
eclampsia is associated with failure of human vascular risk factor differences between gesta- in the pathogenesis of preeclampsia was
cytotrophoblasts to mimic a vascular adhesion tional hypertension and preeclampsia: cohort discovered. Hypertens Pregnancy 1996;15:
phenotype. One cause of defective endovas- Norway study. Hypertension 2016;67:1173–80. 143–6.
cular invasion in this syndrome? J Clin Invest 53. Strøm-Roum EM, Tanbo TG, Eskild A. The 68. Harsem NK, Staff AC, He L, Roald B. The
1997;99:2152–64. associations of maternal body mass index with decidual suction method: a new way of
FEBRUARY 2022 American Journal of Obstetrics & Gynecology S905
Expert Review ajog.org
collecting decidual tissue for functional and 80. De Wolf F, Robertson WB, Brosens I. The disorders of pregnancy. Br J Obstet Gynaecol
morphological studies. Acta Obstet Gynecol ultrastructure of acute atherosis in hypertensive 1991;98:648–55.
Scand 2004;83:724–30. pregnancy. Am J Obstet Gynecol 1975;123: 92. Kyaw T, Toh BH, Bobik A. Foxp3þCD4þ
69. Staff AC, Halvorsen B, Ranheim T, 164–74. regulatory T-cell subtypes and atherosclerosis.
Henriksen T. Elevated level of free 8-iso-pros- 81. Staff AC, Redman CW, Williams D, et al. Circ Res 2016;119:1151–3.
taglandin F2alpha in the decidua basalis of Pregnancy and long-term maternal cardiovas- 93. Gill N, Leng Y, Romero R, et al. The immu-
women with preeclampsia. Am J Obstet Gyne- cular health: progress through harmonization of nophenotype of decidual macrophages in acute
col 1999;181:1211–5. research cohorts and biobanks. Hypertension atherosis. Am J Reprod Immunol 2019;81:
70. Staff AC, Ranheim T, Khoury J, Henriksen T. 2016;67:251–60. e13098.
Increased contents of phospholipids, choles- 82. Labarrere CA. Acute atherosis. A histo- 94. Moe K, Alnaes-Katjavivi P, Størvold GL,
terol, and lipid peroxides in decidua basalis in pathological hallmark of immune aggression? et al. Classical cardiovascular risk markers in
women with preeclampsia. Am J Obstet Gyne- Placenta 1988;9:95–108. pregnancy and associations to uteroplacental
col 1999;180:587–92. 83. Hering L, Herse F, Verlohren S, et al. Tro- acute atherosis. Hypertension 2018;72:
71. Burton GJ, Sebire NJ, Myatt L, et al. Opti- phoblasts reduce the vascular smooth muscle 695–702.
mising sample collection for placental research. cell proatherogenic response. Hypertension 95. Lekva T, Sugulle M, Moe K, Redman C,
Placenta 2014;35:9–22. 2008;51:554–9. Dechend R, Staff AC. Multiplex analysis of
72. Stevens DU, Al-Nasiry S, Bulten J, 84. Herse F, Dechend R, Harsem NK, et al. circulating maternal cardiovascular biomarkers
Spaanderman ME. Decidual vasculopathy in Dysregulation of the circulating and tissue- comparing preeclampsia subtypes. Hyperten-
preeclampsia: lesion characteristics relate to based renin-angiotensin system in preeclamp- sion 2020;75:1513–22.
disease severity and perinatal outcome. sia. Hypertension 2007;49:604–11. 96. Veerbeek JH, Brouwers L, Koster MP,
Placenta 2013;34:805–9. 85. Rieber-Mohn AB, Sugulle M, Wallukat G, et al. Spiral artery remodeling and maternal
73. Johnsen GM, Størvold GL, Alnaes- et al. Auto-antibodies against the angiotensin II cardiovascular risk: the spiral artery remod-
Katjavivi PH, et al. Lymphocyte characterization type I receptor in women with uteroplacental eling (SPAR) study. J Hypertens 2016;34:
of decidua basalis spiral arteries with acute acute atherosis and preeclampsia at delivery 1570–7.
atherosis in preeclamptic and normotensive and several years postpartum. J Reprod 97. Stevens DU, Al-Nasiry S, Fajta MM, et al.
pregnancies. J Reprod Immunol 2019;132:42–8. Immunol 2018;128:23–9. Cardiovascular and thrombogenic risk of
74. Tabas I, García-Cardeña G, Owens GK. 86. Labarrere C, Alonso J, Manni J, decidual vasculopathy in preeclampsia. Am J
Recent insights into the cellular biology of Domenichini E, Althabe O. Immunohistochem- Obstet Gynecol 2014;210:545.e1–6.
atherosclerosis. J Cell Biol 2015;209:13–22. ical findings in acute atherosis associated with 98. Sipahi I, Tuzcu EM. Candidate mechanisms
75. Allahverdian S, Chehroudi AC, intrauterine growth retardation. Am J Reprod for regression of coronary atherosclerosis with
McManus BM, Abraham T, Francis GA. Contri- Immunol Microbiol 1985;7:149–55. high-dose statins: insight from intravascular ul-
bution of intimal smooth muscle cells to 87. Staff AC, Ranheim T, Halvorsen B. trasonography trials. Am J Cardiovasc Drugs
cholesterol accumulation and macrophage-like Augmented PLA2 activity in pre-eclamptic 2008;8:365–71.
cells in human atherosclerosis. Circulation decidual tissue—a key player in the patho- 99. Lefkou E, Mamopoulos A, Dagklis T,
2014;129:1551–9. physiology of ‘acute atherosis’ in pre- Vosnakis C, Rousso D, Girardi G. Pravastatin
76. Staff AC, Dechend R, Redman CW. Review: eclampsia? Placenta 2003;24:965–73. improves pregnancy outcomes in obstetric
preeclampsia, acute atherosis of the spiral ar- 88. Staff AC, Ranheim T, Henriksen T, antiphospholipid syndrome refractory to antith-
teries and future cardiovascular disease: two new Halvorsen B. 8-iso-prostaglandin f(2alpha) reduces rombotic therapy. J Clin Invest 2016;126:
hypotheses. Placenta 2013;34(Suppl):S73–8. trophoblast invasion and matrix metalloproteinase 2933–40.
77. Libby P, Hansson GK. Inflammation and activity. Hypertension 2000;35:1307–13. 100. Saito S, Nakashima A. A review of the
immunity in diseases of the arterial tree: players 89. Halvorsen B, Staff AC, Henriksen T, mechanism for poor placentation in early-
and layers. Circ Res 2015;116:307–11. Sawamura T, Ranheim T. 8-iso-prostaglandin onset preeclampsia: the role of autophagy
78. Redman CW. Immunological aspects of F(2alpha) increases expression of LOX-1 in JAR in trophoblast invasion and vascular remod-
pre-eclampsia. Baillieres Clin Obstet Gynaecol cells. Hypertension 2001;37:1184–90. eling. J Reprod Immunol 2014;101e102:
1992;6:601–15. 90. Liao JK. Linking endothelial dysfunction with 80–8.
79. Maqueo M, Chavezazuela J, endothelial cell activation. J Clin Invest 101. Aoki A, Nakashima A, Kusabiraki T, et al.
Dosaldelavega M. Placental pathology in 2013;123:540–1. Trophoblast-specific conditional Atg7 knockout
eclampsia and preeclampsia. Obstet Gynecol 91. Pijnenborg R, Anthony J, Davey DA, et al. mice develop gestational hypertension. Am J
1964;24:350–6. Placental bed spiral arteries in the hypertensive Pathol 2018;188:2474–86.
S906 American Journal of Obstetrics & Gynecology FEBRUARY 2022
You might also like
- EcodopplerDocument7 pagesEcodopplerEnzo German ZampiniNo ratings yet
- 10 1016@j Ajog 2019 07 010 PDFDocument13 pages10 1016@j Ajog 2019 07 010 PDFDaniel GamarraNo ratings yet
- Subinvolution of The Placental Site As An Anatomic Cause of Postpartum Uterine BleedingDocument5 pagesSubinvolution of The Placental Site As An Anatomic Cause of Postpartum Uterine BleedingEnrique RosasNo ratings yet
- Kaufmann-2004-Aspects of Human Fetoplacental V PDFDocument13 pagesKaufmann-2004-Aspects of Human Fetoplacental V PDFNguyễn Cao VânNo ratings yet
- Burton-2009-Rheological and Physiological Cons PDFDocument10 pagesBurton-2009-Rheological and Physiological Cons PDFNguyễn Cao VânNo ratings yet
- Rheological and Physiological Consequences of Conversion of The Maternal Spiral Arteries For Uteroplacental Blood Flow During Human PregnancDocument10 pagesRheological and Physiological Consequences of Conversion of The Maternal Spiral Arteries For Uteroplacental Blood Flow During Human PregnancSherilinne Quiles LópezNo ratings yet
- Boeldt 2016Document40 pagesBoeldt 2016Ryan AndrianNo ratings yet
- Placenta in PreeclampsiaDocument20 pagesPlacenta in PreeclampsiaRania MousaNo ratings yet
- Placenta Accreta Spectrum Disorders: Challenges, Risks, and Management StrategiesDocument13 pagesPlacenta Accreta Spectrum Disorders: Challenges, Risks, and Management StrategiesRahmayantiYuliaNo ratings yet
- Science Direct Cord CareDocument7 pagesScience Direct Cord CareFatma ElzaytNo ratings yet
- Jurnal Puspa 1Document19 pagesJurnal Puspa 1Heri FarnasNo ratings yet
- APJCP - Volume 17 - Issue 7 - Pages 3035-3041Document7 pagesAPJCP - Volume 17 - Issue 7 - Pages 3035-3041Hussain khanNo ratings yet
- Journal - The Physiology of Intrapartum Fetal Compromise at TermDocument10 pagesJournal - The Physiology of Intrapartum Fetal Compromise at TermbedahfkumiNo ratings yet
- Splitting Hairs About Splitting Muscles - YmobDocument1 pageSplitting Hairs About Splitting Muscles - Ymobps.paulayanezNo ratings yet
- A Case of Vasa Previa Diagnosed PrenatallyDocument5 pagesA Case of Vasa Previa Diagnosed PrenatallydeadcorpsesNo ratings yet
- Managingreproduction Emergenciesinthefield: Part 2: Parturient and Periparturient ConditionsDocument39 pagesManagingreproduction Emergenciesinthefield: Part 2: Parturient and Periparturient ConditionsKaren Vanessa Motato ArangonNo ratings yet
- Placental PathologyDocument39 pagesPlacental PathologyconstantinilieNo ratings yet
- Review Endothelial Progenitor Cells in Pregnancy and Obstetric Pathologies 2013 PlacentaDocument6 pagesReview Endothelial Progenitor Cells in Pregnancy and Obstetric Pathologies 2013 PlacentafujimeisterNo ratings yet
- CDH Modern MXDocument11 pagesCDH Modern MXphobicmdNo ratings yet
- PlacentaDocument17 pagesPlacentarizka auliaNo ratings yet
- Diaz Flores 32 1239 1279 2017Document41 pagesDiaz Flores 32 1239 1279 2017María P SNo ratings yet
- Angiogenesis in ImplantationDocument13 pagesAngiogenesis in ImplantationdfdfffffNo ratings yet
- Jsafog 13 137Document5 pagesJsafog 13 137Elizabeth Duprat GaxiolaNo ratings yet
- Pi Is 0002937811009379Document9 pagesPi Is 0002937811009379Mirza FinandarNo ratings yet
- Hum. Reprod. Update 1998 Koninckx 741 51Document11 pagesHum. Reprod. Update 1998 Koninckx 741 51selaturNo ratings yet
- PIIS000293782200535XDocument17 pagesPIIS000293782200535XnataliaNo ratings yet
- Blois Et Al 2011 ProofsDocument8 pagesBlois Et Al 2011 ProofsGabriela BarrientosNo ratings yet
- Linear Correlation of Uterine Artery Pulsatility Index (PI) in Mid Trimester in Pregnant Female With Foetal Birth WeightDocument5 pagesLinear Correlation of Uterine Artery Pulsatility Index (PI) in Mid Trimester in Pregnant Female With Foetal Birth WeightInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 1471 2393 14 80 PDFDocument5 pages1471 2393 14 80 PDFPaula PebriantyNo ratings yet
- Diagnosis of Endometrial Biopsies and Curettings: A Practical ApproachFrom EverandDiagnosis of Endometrial Biopsies and Curettings: A Practical ApproachNo ratings yet
- 89 JNMS.2022 89-312Document6 pages89 JNMS.2022 89-312yaritzaalviarezNo ratings yet
- Placenta: SciencedirectDocument10 pagesPlacenta: SciencedirectFernando Cardenas AriasNo ratings yet
- Regulation of Placental VEGF and PlGF by OxygenDocument9 pagesRegulation of Placental VEGF and PlGF by OxygenFeri ZidaneNo ratings yet
- Early Development of The Human Placenta and Pregnancy ComplicationsDocument9 pagesEarly Development of The Human Placenta and Pregnancy ComplicationsSherilinne Quiles LópezNo ratings yet
- Ijms 22 08622Document24 pagesIjms 22 08622nur aini hidayatinNo ratings yet
- Seminars in Cell & Developmental BiologyDocument10 pagesSeminars in Cell & Developmental BiologyagathapradanaNo ratings yet
- Tenny Parker Change A Reflection of Placental Pathology PDFDocument4 pagesTenny Parker Change A Reflection of Placental Pathology PDFEditors100% (1)
- Mini-Review: Elizabeth Phipps, Devika Prasanna, Wunnie Brima, and Belinda JimDocument12 pagesMini-Review: Elizabeth Phipps, Devika Prasanna, Wunnie Brima, and Belinda JimoneagustinNo ratings yet
- Clinical Implications of Fetal Heart Rate.3Document10 pagesClinical Implications of Fetal Heart Rate.3sabrina shawNo ratings yet
- Disproporsi Kepala PanggulDocument14 pagesDisproporsi Kepala PanggulIntan PermataNo ratings yet
- Severe Preeclampsia Is Associated With Alterations in Cytotrophoblasts of The Smooth ChorionDocument64 pagesSevere Preeclampsia Is Associated With Alterations in Cytotrophoblasts of The Smooth ChorionRicvan Dana Nindrea,MKesNo ratings yet
- 1 s2.0 S2589933323003452 MainDocument10 pages1 s2.0 S2589933323003452 MainimedamNo ratings yet
- MANUAL OF PLACENTAL PATHOLOGY FinaleDocument24 pagesMANUAL OF PLACENTAL PATHOLOGY FinaleAnonymous wE02eRNo ratings yet
- Congenital Diaphragmatic Hernia: Pathogenesis, Prenatal Diagnosis and Management - Literature ReviewDocument7 pagesCongenital Diaphragmatic Hernia: Pathogenesis, Prenatal Diagnosis and Management - Literature ReviewPritariantiNo ratings yet
- The Physiology of Intrapartum Fetal Compromise at TermDocument10 pagesThe Physiology of Intrapartum Fetal Compromise at TermseopyNo ratings yet
- Patent Ductus Arteriosus PathophysiologyDocument6 pagesPatent Ductus Arteriosus PathophysiologyandikaprtmNo ratings yet
- Mini-Review: Elizabeth Phipps, Devika Prasanna, Wunnie Brima, and Belinda JimDocument12 pagesMini-Review: Elizabeth Phipps, Devika Prasanna, Wunnie Brima, and Belinda JimMelisa ClaireNo ratings yet
- Diaz Flores 32 1239 1279 2017Document41 pagesDiaz Flores 32 1239 1279 2017María P SNo ratings yet
- gas053Document11 pagesgas053Angham OuadahNo ratings yet
- Hip Disorders in Children: Postgraduate Orthopaedics SeriesFrom EverandHip Disorders in Children: Postgraduate Orthopaedics SeriesRating: 3 out of 5 stars3/5 (2)
- Nejmra 1513247Document11 pagesNejmra 1513247Franz Huber QueiroloNo ratings yet
- FP Ago 2020 - Mecanismos Moleculares y Mecánicos Que Regulan El Cierre Del Ductus en PrematurosDocument19 pagesFP Ago 2020 - Mecanismos Moleculares y Mecánicos Que Regulan El Cierre Del Ductus en Prematurosjulius castelloNo ratings yet
- Ni Hms 99392Document21 pagesNi Hms 99392dhamar leoNo ratings yet
- Preeclampsia Fisiopatologia 2019Document8 pagesPreeclampsia Fisiopatologia 2019Carlos MirandaNo ratings yet
- Pathology of Preeclampsia (Autosaved) (Autosaved)Document59 pagesPathology of Preeclampsia (Autosaved) (Autosaved)ck4realNo ratings yet
- Hemorragia InterventricularDocument9 pagesHemorragia InterventricularRebeca Tapia RsNo ratings yet
- New Approaches To Rehabilitation After Ectopic PregnancyDocument4 pagesNew Approaches To Rehabilitation After Ectopic PregnancyCentral Asian StudiesNo ratings yet
- Endovascular Trophoblast Invasion: Implications for IUGR and PreeclampsiaDocument7 pagesEndovascular Trophoblast Invasion: Implications for IUGR and PreeclampsiaSarah Saene da Silva NoiaNo ratings yet
- Mini-Review: Elizabeth Phipps, Devika Prasanna, Wunnie Brima, and Belinda JimDocument12 pagesMini-Review: Elizabeth Phipps, Devika Prasanna, Wunnie Brima, and Belinda JimemilyNo ratings yet
- Fitting The Task To The Human A Textbook of Occupational Ergonomics by Grandjean, E. Kroemer, K. H. E.Document414 pagesFitting The Task To The Human A Textbook of Occupational Ergonomics by Grandjean, E. Kroemer, K. H. E.Andy Delos ReyesNo ratings yet
- Necrotizing Enterocolitis (Sultn Aiman NeazyDocument59 pagesNecrotizing Enterocolitis (Sultn Aiman NeazyMohammed ElhashimiNo ratings yet
- Final Reviewer-Science (151-180)Document3 pagesFinal Reviewer-Science (151-180)KAREN BUENAVISTANo ratings yet
- Cardiovascular SystemDocument56 pagesCardiovascular SystemEdwin SilvaNo ratings yet
- Virtual Lab: Muscle Stimulation Post-Lab Quiz and Lab ReportDocument4 pagesVirtual Lab: Muscle Stimulation Post-Lab Quiz and Lab ReportMykaila InmanNo ratings yet
- Module Cardiovascular System Anatomy and PhysiologyDocument9 pagesModule Cardiovascular System Anatomy and PhysiologyPATRICIA KAYE RIONo ratings yet
- Exercise 3 RBC CountDocument6 pagesExercise 3 RBC CountJohn Paul DianNo ratings yet
- Els (Characteristics of Life)Document4 pagesEls (Characteristics of Life)cdcheijdnekjdNo ratings yet
- DATA TARIF LABORATORIUM - OdsDocument4 pagesDATA TARIF LABORATORIUM - OdsData segerNo ratings yet
- Digestive System LabsheetDocument4 pagesDigestive System LabsheetKATHLEEN MAE HERMONo ratings yet
- EAR MCQdoneDocument71 pagesEAR MCQdoneAbdur Raheem QureshiNo ratings yet
- Septum Formation in The VentriclesDocument43 pagesSeptum Formation in The VentriclesAhsan IslamNo ratings yet
- My Answer in Our LaboratoryDocument4 pagesMy Answer in Our LaboratoryKris Marie DelaCruz DomingoNo ratings yet
- Internal Body OrgansDocument8 pagesInternal Body OrgansSangaré soungaloNo ratings yet
- Part 1 Protection (Integumentary Systems)Document25 pagesPart 1 Protection (Integumentary Systems)Muhammad UsamaNo ratings yet
- Donepezil: DR Rashmi SurtiDocument55 pagesDonepezil: DR Rashmi SurtirsurtiNo ratings yet
- Physiological Principles of SotaiDocument13 pagesPhysiological Principles of SotaiBuyu IkkanNo ratings yet
- Lecture Learning Objectives for BIO 210 SystemsDocument14 pagesLecture Learning Objectives for BIO 210 SystemsAmber DavisNo ratings yet
- GAYO C. Revised NCPDocument7 pagesGAYO C. Revised NCPCarl LacambraNo ratings yet
- Tehnologija Vitamina I Hormona: 1. Što Su Vitamini?Document11 pagesTehnologija Vitamina I Hormona: 1. Što Su Vitamini?J.No ratings yet
- Plant Physiology and BiochemistryDocument4 pagesPlant Physiology and BiochemistryShefira TashaNo ratings yet
- 01 Introductory PgyDocument76 pages01 Introductory Pgygbsreg gbsregNo ratings yet
- ZOOL 322 Lecture 1 2019-2020Document10 pagesZOOL 322 Lecture 1 2019-2020Timothy MutaiNo ratings yet
- Soft Tissues PathologyDocument53 pagesSoft Tissues PathologyWz bel DfNo ratings yet
- A Follicular Regulatory Innate Lymphoid Cell Population Impairs Interactions Between Germinal Center TFH and B CellsDocument13 pagesA Follicular Regulatory Innate Lymphoid Cell Population Impairs Interactions Between Germinal Center TFH and B Cellsiva hullNo ratings yet
- Poster Index Symposium 2021Document5 pagesPoster Index Symposium 2021Brien WongNo ratings yet
- Unit f211 1.1 Questions Microscopes Part 2Document41 pagesUnit f211 1.1 Questions Microscopes Part 2Hazel100% (1)
- Chapter-20 Locomotion and Movement: Is The Voluntary Movement of An Individual From One Place ToDocument8 pagesChapter-20 Locomotion and Movement: Is The Voluntary Movement of An Individual From One Place ToLishaNo ratings yet
- Bachelor of Nursing Science Anatomy and Physiology 1 ModuleDocument36 pagesBachelor of Nursing Science Anatomy and Physiology 1 ModuleNORHANANI BINTI BAJURI STUDENT100% (1)
- Prescotts Microbiology 10Th Edition Willey Solutions Manual Full Chapter PDFDocument25 pagesPrescotts Microbiology 10Th Edition Willey Solutions Manual Full Chapter PDFbob.morris579100% (13)