Professional Documents
Culture Documents
Effectiveness of QICs in LMICs-SystRev
Uploaded by
Bili RubinCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Effectiveness of QICs in LMICs-SystRev
Uploaded by
Bili RubinCopyright:
Available Formats
RESEARCH ARTICLE
The effectiveness of the quality improvement
collaborative strategy in low- and middle-
income countries: A systematic review and
meta-analysis
Ezequiel Garcia-Elorrio ID1*, Samantha Y. Rowe ID2,3, Maria E. Teijeiro4,
Agustı́n Ciapponi5‡, Alexander K. Rowe ID2‡
1 Healthcare quality and safety department, Instituto de Efectividad Clı́nica y Sanitaria (IECS-CONICET),
a1111111111
Buenos Aires, Argentina, 2 Malaria Branch, Division of Parasitic Diseases and Malaria, Center for Global
a1111111111 Health, Centers for Disease Control and Prevention, Atlanta, Georgia, United States of America, 3 CDC
a1111111111 Foundation, Atlanta, Georgia, United States of America, 4 Quality Department, Fundación para la Lucha
a1111111111 contra las Enfermedades Neurológicas de la Infancia (FLENI), Escobar, Buenos Aires Province, Argentina,
a1111111111 5 Argentine Cochrane Centre, Instituto de Efectividad Clı́nica y Sanitaria (IECS-CONICET), Buenos Aires,
Argentina
‡ AC and AKR are joint senior authors on this work.
* egarciaelorrio@iecs.org.ar
OPEN ACCESS
Citation: Garcia-Elorrio E, Rowe SY, Teijeiro ME,
Ciapponi A, Rowe AK (2019) The effectiveness of
Abstract
the quality improvement collaborative strategy in
low- and middle-income countries: A systematic
review and meta-analysis. PLoS ONE 14(10): Background
e0221919. https://doi.org/10.1371/journal.
pone.0221919
Quality improvement collaboratives (QICs) have been used to improve health care for
decades. Evidence on QIC effectiveness has been reported, but systematic reviews to date
Editor: Wisit Cheungpasitporn, University of
Mississippi Medical Center, UNITED STATES
have little information from low- and middle-income countries (LMICs).
Received: February 7, 2019
Objective
Accepted: August 16, 2019
To assess the effectiveness of QICs in LMICs.
Published: October 3, 2019
Copyright: This is an open access article, free of all
copyright, and may be freely reproduced,
Methods
distributed, transmitted, modified, built upon, or We conducted a systematic review following Cochrane methods, the Grading of Recom-
otherwise used by anyone for any lawful purpose.
mendations Assessment, Development, and Evaluation (GRADE) approach for quality of
The work is made available under the Creative
Commons CC0 public domain dedication.
evidence grading, and the Preferred Reporting Items for Systematic Reviews and Meta-
analyses (PRISMA) statement for reporting. We searched published and unpublished stud-
Data Availability Statement: Supplementary Data
are available at the Open Science Framework DOI
ies between 1969 and March 2019 from LMICs. We included papers that compared usual
10.17605/OSF.IO/U3DHF. practice with QICs alone or combined with other interventions. Pairs of reviewers indepen-
Funding: This work was supported by the HQSS
dently selected and assessed the risk of bias and extracted data of included studies. To esti-
Secretariat -Bill and Melinda Gates Foundation, mate strategy effectiveness from a single study comparison, we used the median effect size
grant Kruk/OPP1161450 to EGE and grant (MES) in the comparison for outcomes in the same outcome group. The primary analysis
OPP52730 to AKR. In addition, this work was
evaluated each strategy group with a weighted median and interquartile range (IQR) of MES
supported by the World Bank–Netherlands
Partnership Program grant P098685 to AKR. The values. In secondary analyses, standard random-effects meta-analysis was used to esti-
funders had no role in study design, data collection mate the weighted mean MES and 95% confidence interval (CI) of the mean MES of each
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 1 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
and analysis, decision to publish, or preparation of strategy group. This review is registered with PROSPERO (International Prospective Regis-
the manuscript. ter of Systematic Reviews): CRD42017078108.
Competing interests: The authors have declared
that no competing interests exist. Results
Twenty-nine studies were included; most (21/29, 72.4%) were interrupted time series stud-
ies. Evidence quality was generally low to very low. Among studies involving health facility-
based health care providers (HCPs), for “QIC only”, effectiveness varied widely across out-
come groups and tended to have little effect for patient health outcomes (median MES less
than 2 percentage points for percentage and continuous outcomes). For “QIC plus training”,
effectiveness might be very high for patient health outcomes (for continuous outcomes,
median MES 111.6 percentage points, range: 96.0 to 127.1) and HCP practice outcomes
(median MES 52.4 to 63.4 percentage points for continuous and percentage outcomes,
respectively). The only study of lay HCPs, which used “QIC plus training”, showed no effect
on patient care-seeking behaviors (MES -0.9 percentage points), moderate effects on non-
care-seeking patient behaviors (MES 18.7 percentage points), and very large effects on
HCP practice outcomes (MES 50.4 percentage points).
Conclusions
The effectiveness of QICs varied considerably in LMICs. QICs combined with other inven-
tion components, such as training, tended to be more effective than QICs alone. The low
evidence quality and large effect sizes for QIC plus training justify additional high-quality
studies assessing this approach in LMICs.
Introduction
Major failures in health care have been reported elsewhere but are most evident in low- and
middle-income countries (LMICs). An evaluation of the health-related Millennium Develop-
ment Goals (MDGs) found that, in 2015, when they were to be achieved, major health care
quality gaps still were present in LMICs, which ignited a strong demand for quality improve-
ment [1]. The MDGs have now been replaced by the Sustainable Development Goals (SDGs),
instituted by the United Nations with the aim to contribute to the achievement of universal
health coverage with quality care for all [2]. Concurrently in 2017, The Lancet Global Health
Commission on High-Quality Health Systems in the SDG Era was established to review cur-
rent knowledge, conduct new focused research, and propose policies for measuring and
improving health care quality to reach new levels of performance in LMICs. This Commission
advocated for a revision of methods that could contribute to the advance of the field of quality
of care worldwide [3].
Among the several quality improvement strategies available, quality improvement collabo-
ratives (QICs) (also known as collaborative improvement and learning collaboratives) have
been used to improve health care for several decades [4]. However, reporting on specific com-
ponents of QICs has been imprecise [5].
Formal QICs involve the use of healthcare teams from different sites to improve perfor-
mance on a specific topic by collecting data and testing ideas with improvement cycles (usually
plan-do-study-act cycles, involving planning a change, trying it, observing the results, and act-
ing upon what is learned) supported by coaching and learning sessions [6]. QICs are supported
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 2 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
by the concept that district managers and networks of facilities can be harnessed into learning
systems that accelerate improvement in health care performance with the potential to achieve
results at large scale for scale. The district level of the health system is well positioned to facili-
tate systematic group learning among facilities of similar types and across tiers of the health
system. District-led area-based learning and planning bring together providers and adminis-
trators responsible for a catchment area to solve clinical and system problems, harmonize
approaches, maximize often limited resources and create better communication and referral
between facilities [7].
The use of QICs has increased rapidly despite the absence of strong evidence for effective-
ness, cost-effectiveness or long-term impact. Published systematic reviews on QICs, which
predominantly include studies from high-income countries, show modest improvements, par-
ticularly when addressing straightforward aspects of care where there is a clear gap between
recommended and actual practice. There is still limited information from LMICs, unpublished
studies, or non-English studies [8–10].
Recently, an extensive systematic review has been published characterizing the effectiveness
of a wide array of strategies to improve health care provider (HCP) performance in LMICs
(the Health Care Provider Performance Review, or HCPPR) [11]. Although this review
includes QICs, thus far, these strategies have been analyzed under the broader strategy cate-
gory of “group problem solving,” which includes other, non-QIC, strategies. Additionally, the
most recent literature search for the HCPPR was conducted in May 2016.
The objective of this work was to particularly estimate the effectiveness of QICs in LMICs
using data from the HCPPR and results of studies from an updated literature search. We
aimed to inform decisions about whether to use QIC, how best to implement them, and to
identify knowledge gaps on QICs in LMICs and provide direction on future evaluations of this
strategy.
Materials and methods
We conducted a systematic review following Cochrane Collaboration methods and the Pre-
ferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement for
reporting [12, 13]. The study protocol was registered in PROSPERO International prospective
register of systematic reviews (registration number CRD42017078108).
Study eligibility criteria
Type of study designs. Studies meeting the Cochrane Effective Practice and Organisation
of Care (EPOC) Review Group for inclusion in a systematic review of interventions [14]:
a. Randomized controlled trials (RCTs)
b. Controlled before- and- after trials (CBA)
c. Interrupted time series (ITS) designs with at least 3 data points before and after the inter-
vention, with or without comparison groups
Types of participants. HCPs (and patients that they care for) from LMICs (defined as
countries with a low or middle-income economy, according to the World Bank at the time of
the literature search) [15]. HCPs included hospital-, clinic-, and community-based health
workers, pharmacists, and medicine vendors.
Type of intervention. Studies were included if they had an intervention arm exposed to
QIC with or without other strategy components (e.g., training) compared to a non-exposed
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 3 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
control group (or historical controls, for ITS studies) that could be defined as usual practice.
QIC was defined as a strategy with the following core elements: a) a team of experts (in clinical
care and quality improvement) involved in bringing together the scientific evidence, practical
contextual knowledge and quality improvement methods, usually within a “change package”
or toolkit; b) multiple teams from multiples sites that chose to participate; c) a model or frame-
work for improvement that included measurable aims, data collection, implementation and
evaluation of small tests of change; and d) a set of structured activities that promoted a collabo-
rative process to learn and share ideas, innovations, and experiences (e.g. face-to-face or virtual
meetings; visits to other sites; visits by experts or facilitators; web-based activities to report
changes, results and comparisons with other teams; and coaching and feedback by improve-
ment experts). The comparator was non-exposed control groups that represent usual practice.
Type of outcomes. There was no restriction on outcome type. Outcomes were grouped
into the following categories.
• Facilitators (i.e., elements that facilitate HCP performance, such as supplies and HCP
knowledge)
• Health worker practices (i.e., processes of care, such as correct treatment)
• Patient health outcomes
• Patient behaviors related to care-seeking or use of health services
• Other patient behaviors (i.e., those not related to care-seeking, such as adherence to treat-
ment regimen)
Effect sizes were based on primary outcomes, with the following exclusions.
• For outcomes expressed as a percentage, effect sizes based on <20 observations per study
group and time point, for a given comparison
• Effect sizes based on a simulation study and not actually observed data
• Effect sizes for which baseline and follow-up measures in the intervention group were both
100%, as this indicates that HCP performance in the intervention group had no room for
improvement and did not worsen over time. Similarly, for HCP practice outcomes expressed
as a percentage, we excluded effect sizes based on a baseline value of 95% or greater, as there
was little room for improvement.
• Effect sizes based on outcome measures that were not taken at comparable times between
study groups. For example, if the outcome for a control group was measured at –1 month, 3
months, and 9 months since the intervention began, and the outcome for an intervention
group was measured at –1 month, 3 months, and 21 months since the intervention began,
the effect size based on the 9-month and 21-month outcome measures would be ineligible.
• Outcomes from ITS studies for which the time series was highly unstable and thus could not
be reliably modeled, and outlier outcome measures that probably did not represent the true
trend in HCP performance.
Search strategy
The literature search was conducted in two phases (see S1 File for details). In summary, we
first searched results of the HCPPR, which is a comprehensive systematic review of the effec-
tiveness of strategies to improve health worker performance in LMICs. The HCPPR study
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 4 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
team searched 52 electronic databases for published studies and 58 document inventories for
unpublished studies from 1960s–2016, screened personal libraries, asked colleagues for unpub-
lished studies, and performed hand searches of 854 bibliographies from previous reviews. Sec-
ond, we updated the HCPPR literature search with a focus on studies of QICs (search date was
March 15, 2019). This update involved the search of electronic databases (S1 File, page 14),
screening bibliographies of included study reports (referred to as “reports from additional
sources” in Fig 1), and seeking reports from colleagues. There were no language restrictions.
Data collection
In the first phase of the review, a team of researchers assessed study eligibility, and each
researcher screened studies independently. Before the screening began, concordance testing
was conducted against a “gold standard” list of reports until at least 80% was identified by each
researcher. In the second phase of the review, a pair of investigators (MET, EGE) indepen-
dently assessed study eligibility, and discrepancies were reconciled in consultation with a third
team member (AC). The study eligibility process was conducted using Covidence© from the
Cochrane collaboration. Also, two investigators (AKR, SYR) assessed the eligibility of study
reports that we received from colleagues. Data were extracted from the included studies inde-
pendently by a pair of investigators (SYR, AKR) or researchers using a standardized form, and
discrepancies were resolved through discussion. Before beginning data extraction, concor-
dance testing of all data abstractors was conducted until the percent agreement between indi-
vidual abstractors and a gold standard set of abstracted data (based on consensus by
investigators SYR, AKR) was at least 80%. Data from each study were entered into a Microsoft
Access database (Microsoft Inc., Redmond, Washington). Data elements included: study set-
ting (where, when, HCP types, other contextual factors), study design, health conditions
addressed, strategy description, outcome description, outcome measurements, the timing of
outcome measurements in relation to the implementation of the strategy, effect sizes, sample
sizes, sampling details, and data elements needed to assess risk of bias (RoB). If details regard-
ing study characteristics or the QIC intervention were not available in study reports, we con-
tacted study authors. Except for the purpose of meta-analysis, missing data were not imputed.
For meta-analysis, we used estimates of standard errors of effect sizes that were available from
the HCPPR database. A small proportion of the standard error estimates for percentage out-
comes from the HCPPR database were based on imputed data (usually because sample size
data were missing). Effect sizes with missing standard errors were excluded from meta-
analysis.
Risk of bias (quality) assessment
We categorized RoB with methods based on guidance from the Cochrane EPOC Group [16].
RoB at the study level was categorized as low, moderate, high, or very high. We assessed the
following RoB domains: number of clusters per study arm, completeness of dataset, balance in
baseline outcome measurements, balance in baseline characteristics, reliability of outcomes,
adequacy of concealment of allocation (where relevant), intervention unlikely to affect data
collection, intervention plausibly independent of other changes, and number of data points
before and after the intervention.
We used the Recommendations Assessment, Development, and Evaluation (GRADE)
approach to assess the quality of evidence related to each of the key outcomes [17]. For assess-
ments of the overall quality of evidence for each outcome, randomized studies, ITS studies,
and other non-randomized studies started at “high quality”, “moderate quality” and “low qual-
ity” of evidence, respectively. Although the traditional approach is to start non-randomized
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 5 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
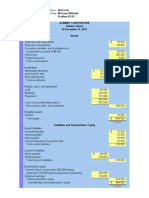
Fig 1. Flow diagram.
https://doi.org/10.1371/journal.pone.0221919.g001
studies as “low quality” [18], ITS studies with multiple periods and measurements during each
period with no other limitations may constitute “moderate quality” of evidence [19, 20]. We
downgraded the study one or two levels depending on the extent of violation across the follow-
ing criteria: study limitations (RoB); indirectness of evidence; inconsistency; imprecision of
effect estimates; or publication bias. If we did not find study limitations, we upgraded the eval-
uation of the quality of the evidence when the pooled estimates revealed negligible concerns
about confounders, a strong dose-response gradient, or a large magnitude of effect. Consider-
ing a mean baseline health worker performance level at 40% for a process-of-care outcome
expressed as a percentage, an absolute increase of 40% or more, representing a relative risk >2,
allowed us to upgrade the quality of evidence by one level.
Data synthesis
Effect sizes were defined as absolute percentage-point differences; positive values meant
improvement.
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 6 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
In non-ITS studies with pre- and post-intervention outcome measures, for outcomes that
were dichotomous or expressed as a percentage, the effect size was calculated with Eq 1.
effect size ¼ ðfollowup baselineÞintervention ðfollowup baselineÞcontrol ð1Þ
In non-ITS studies with pre- and post-intervention outcome measures, for outcomes that
were continuous but not obviously bounded (e.g., a mortality rate), the effect size was calcu-
lated with Eq 2.
�� � � � �
followup baseline followup baseline
effect size ¼ 100% ð2Þ
baseline intervention baseline control
For ITS studies, segmented linear regression modeling was performed to estimate a sum-
mary effect size that incorporated both the level and trend effects. The summary effect size was
the outcome level at the mid-point of the follow-up period as predicted by the regression
model minus a predicted counterfactual value that equals the outcome level based on the pre-
intervention trend extended to the mid-point of the follow-up period. This summary effect
size was used because it allows the results of ITS studies to be combined with those of non-ITS
studies.
To estimate strategy effectiveness from a single study comparison, the effect size was
defined as the median of all effect sizes (MES) in the comparison for outcomes in the same out-
come category. Results were stratified by HCP type (health facility-based vs. lay or community
HCP).
For the primary analysis, we reported median, interquartile range, minimum, and maxi-
mum MES. The median effect size has been used in other systematic reviews of strategies to
improve HCP performance [21, 22]. Median MES for strategy groups that were based on
fewer than five study comparisons were not weighted, as weighting with small samples might
cause the median to be a poor measure of central tendency when outliers are present. Median
MES for strategy groups with five or more study comparisons were weighted, where the
weight = 1 + the natural logarithm of the number of HCPs or (if the number of HCPs in a
study was not reported) the number of service provision sites (e.g., health facilities) or (if the
number of service provision sites was not reported) the number of administrative areas (e.g.,
districts) in the study. Strategy groups tested by at least three study comparisons were consid-
ered to have enough evidence to form generalizations—although caution is increasingly war-
ranted as the minimum of three comparisons is approached. Strategy groups tested by only
one or two study comparisons were interpreted separately.
In a secondary analysis, standard random-effects meta-analysis was used to estimate the
weighted mean MES and 95% confidence interval (CI) of the mean MES of each strategy
group. We used I2 as a measure of consistency for each meta-analysis, considering low hetero-
geneity <30%, moderate heterogeneity 30–60%, and high heterogeneity >60% [23]. We con-
ducted a meta-analysis on one median effect size per study comparison for each outcome
group, and we performed a sensitivity analysis considering all effect sizes individually to test
consistency of the results.
Publication bias was assessed using Funnel Bias Assessment plots to conduct visual inspec-
tion for asymmetry for strategy-outcome groups with at least 10 studies.
Results
During the first phase of the literature search, 216,477 citations were identified (S1 File). After
screening and assessing eligibility, 46 reports from 25 studies were included (left side of Fig 1).
In the second phase, which updated the search through 15 March 2019, 3207 articles were
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 7 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
identified, and seven more reports from four studies were included after removing duplicates.
Altogether, 53 reports from 29 studies with 30 study comparisons were included for this sys-
tematic review (Fig 1).
Description of included studies
The included studies were published between 2008 and 2019, from 12 LMICs in four conti-
nents. Most studies (24/29, 82.7%) were from Africa, three were from the Russian Federation,
and one each was from Georgia and Mexico (Table 1). Most studies were ITS studies without
controls (19/29, 72.4%), two were CBAs with randomized controls, three were CBAs with
non-randomized controls, two were post-only CRTs, and one was an ITS study with controls.
Fig 2 presents the RoB of included studies individually by specific domains. Most studies
(25/29, 86.2%) had a high or very high RoB. Two studies had a moderate RoB and two had a
low RoB. The 30 study comparisons from 29 studies tested six different strategies that included
QICs (Table 2). The most commonly tested QIC intervention had no additional strategy com-
ponents (21 study comparisons). Other QIC interventions that were tested usually combined
QIC with training, with or without additional components. The median study follow-up time
was about one year.
In our assessment of publication bias, no strategy-outcome group had the minimum of 10
studies. However, for the one strategy-outcome group with the most studies (QIC interven-
tion, health worker practice outcomes expressed as a percentage, n = 9 studies), the funnel plot
revealed no evidence of asymmetry (S2 File).
Effect of interventions
The findings are summarized in Table 3, which presents QIC intervention effectiveness in
terms of median MES (left column) and mean MES (right column and S2 File) from the ran-
dom effects meta-analysis. Individual effect sizes are presented in Table 1. We had five main
findings. First, for the “QIC only” strategy, effectiveness varied highly across outcome groups.
For patient behaviors not related to care-seeking, the effect was moderate (median MES: 17.6
percentage points) (Table 3, row 3). For patient health outcomes, there was essentially no effect
(0.3 and 1.4 percentage points for percentage and continuous outcomes, respectively). The
results ranged from modestly to highly effective for health worker practice outcomes (30.2 to
44.2 percentage points) and patient care-seeking outcomes (7.7 to 62.2 percentage points).
Second, for the “QCI + training” strategy for health facility-based HCPs, although there
were only 4 studies, effectiveness was very high: MES 52.4 to 63.4 percentage points for health
worker practice outcomes, 111.6 percentage points for patient health outcomes, and 87.7 per-
centage points for non-care-seeking patient behaviors (Table 3, rows 6–8). An additional study
on a similar strategy (QIC + training + other management techniques) also found very high
effectiveness (101.1 percentage points) for its one outcome on care-seeking patient behaviors.
Third, for the “QIC + training + strengthening infrastructure (bicycles for facilitators)
+ supervision + other management techniques (group process between HCP and commu-
nity)” strategy, the one study found essentially no effect (MES 0.1 percentage points, for patient
health outcomes) (Table 3, row 10). Fourth, for the “QIC + strengthening infrastructure
(report cards) + regulation and governance (community scorecards)” strategy, the effective-
ness from two studies ranged from essentially no effect (-2.8 percentage points, for non-care-
seeking patient behaviors) to modest effect (9.5 percentage points, for care-seeking patient
behaviors) (Table 3, rows 11–12).
Finally, the one study of lay health workers found highly variable results, ranging from
essentially no effect (-0.9 percentage points, for care-seeking patient behaviors) to moderately
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 8 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
Table 1. Characteristics of included studies.
Study ID Country Study Intervention Outcomes Effect
design size ± standard
error
N’Guessan 2011 Cote ITS QIC % of patients lost to follow-up during antiretroviral 3.4±8.6
[27,28] d’Ivoire treatment
% of HIV-exposed infants who were tested for HIV 15.5±20.7
% of patients’ files with complete documentation 44.8±10.2
for antiretroviral treatment
% of patients’ files with complete documentation 76.7±3.8
for prevention of mother to child transmission of
HIV
Chitashvili 2017 Georgia CBA QIC % of hospital pediatric patients with antibiotic 31.0±26.3
[29–34] (NRC) prescription who received appropriate first-line
antibiotic for pneumonia
% of clinic pediatric patients with antibiotic 64.0±9.2
prescription for whom antibiotic was justified for
respiratory tract infection
% of clinic pediatric patients with antibiotic 68.0±8.7
prescription who received appropriate first-line
antibiotic for respiratory tract infection
Singh 2013 [35–38] Ghana ITS QIC Mean % of deliveries attended by a skilled birth -3.6±26.1
attendant defined as a doctor, nurse or midwife per
HF
Mean % of newborns who received follow-up post- 28.9±27.1
natal care on day 6 or 7 after birth per HF
Mean % of newborns who received post-natal care 29.0±30.6
within 48 hours of birth per HF
Mean % of infants attending child wellness clinics 116.1±71.3
who were low weight for age per HF
Singh 2016–1 [36– Ghana ITS QIC Mean % of antenatal care registrants in the first -0.997±3.8
38–41] trimester at the time of registration per HF
Mean % of total deliveries that are attended by 10.5±4.8
skilled personnel per HF catchment area
Mean % of 1- to 11-month-old child welfare clinics 20.4±45.6
attendees who were < 60% weight for age
(moderately or severely underweight) per HF
Singh 2016–2 [36– Ghana ITS QIC Mean % of antenatal care registrants in the first -5.4±4.0
38–41] trimester at the time of registration per HF
Mean % of total deliveries that are attended by 16.4±5.5
skilled personnel per HF catchment area
Mean % of 1- to 11-month-old child welfare clinics 71.7±60.8
attendees who were < 60% weight for age
(moderately or severely underweight) per HF
Singh 2016–3 [36– Ghana ITS QIC Mean % of antenatal care registrants in the first 7.0±8.1
38–41] trimester at the time of registration per HF
Mean % of total deliveries that are attended by 12.7±9.4
skilled personnel per HF catchment area
Colbourn 2013 [42– Malawi CBA (RC) QIC Maternal mortality rate per 100000 livebirths -27.4b
44]a Perinatal mortality rate per 1000 births (stillbirths 3.0b
and early neonatal deaths)
Neonatal mortality rate per 1000 livebirths 22.9b
(Continued )
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 9 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
Table 1. (Continued)
Study ID Country Study Intervention Outcomes Effect
design size ± standard
error
Barceló 2010 [45] Mexico POS-CRT QIC % of patients who received eye examination 68.5±14.2
% of patients who received foot examination 73.8±13.5
% of patients with blood pressure < = 140/90 5.8±18.4
mmHg
% of patients with A1c <7% (good diabetes 11.4±19.2
control)
% of patients with cholesterol <200mg/dL 17.9±18.9
Average triglycerides per patient (mg/dL) 0.8b
Average body mass index per patient (kg/m2) 2.0b
Crigler 2012 [46– Niger ITS QIC Number of deliveries assisted by skilled health -25.8±81.0
47] workers per 100 expected pregnancies
Contraceptive prevalence rate (number of women 131.3±231.0
who accepted contraceptive use at HF per 100
women of reproductive age in catchment area)
% of HCPs with an adequate job description 47.2±139.0
% of HCPs adhering to norms for essential 8.1±24.1
newborn care at birth
Osibo 2017 [48–50] Nigeria POS-CRT QIC % of HIV positive pregnant women who attended 3.0±12.8
6-month postpartum visit and did not miss any
previous scheduled visit by more than 30 days
Catsambas 2008–4 Russian ITS QIC % of deliveries to women with no pregnancy 34.3±9.9
[51–57] Federation induced hypertension out of all deliveries per
month
Catsambas 2008–5 Russian ITS QIC % of women who were pregnant this month with 49.7±26.4
[51–57] Federation pregnancy induced hypertension of any severity for
whom pregnancy induced hypertension protocol
was implemented
Outcome on diagnostic accuracy: ratio of number 3.4±6.1
of deliveries to women with no pregnancy induced
hypertension to number of all deliveries per month
(x100%)
Outcome on diagnostic accuracy: % of deliveries to 5.2±2.2
women with no edema out of all deliveries per
month
Decrease = improvement: ratio of number of -75.3±63.9
women hospitalized this month for pregnancy
induced hypertension complications to number of
women who completed pregnancy this month with
pregnancy induced hypertension of any severity
(x100%)
Catsambas 2008–6 Russian ITS QIC % of patients with hypertension who were taken 10.3±7.0
[52,53,55,57] Federation under observation in the first stage of disease
% of patients with hypertension who were taken 12.5±1.1
under observation who performed non-drug
treatment recommendations
number of patients with hypertension identified -28.2±45.0
for the first time per 1000 residents of HF
catchment areas
% of patients with hypertension who were taken -15.0±9.8
under observation who have consistently reduced
blood pressure
(Continued )
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 10 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
Table 1. (Continued)
Study ID Country Study Intervention Outcomes Effect
design size ± standard
error
Catsambas 2008–7 Rwanda ITS QIC % of women who enrolled for antenatal care -1.5±35.0
[52,54,55,57,58] consultations and were tested for HIV whose male
partners were also tested for HIV
% of women who enrolled for antenatal care 44.6±29.0
consultations and were tested for HIV who
returned for their results the same day of testing
Ngidi 2013 [59] South CITS QIC mean number of antenatal clients referred for -4.7b
Africa antiretroviral therapy per HF per month
mean number of antenatal clients initiated on 172.9 b
antiretroviral therapy per HF per month
Catsambas 2008–9 Tanzania ITS QIC % of women who tested positive for HIV who -10.1±11.7
[52,54,55,57] attended antenatal care consultations and were
enrolled in Care and Treatment Center per month
% of HIV patients on antiretroviral therapy seen at 9.2±1.7
clinic according to their scheduled appointments
who were not lost to follow-up for at least 3
consecutive months
% of HIV patients in general care or on -3.8±1.8
antiretroviral therapy seen at clinic within past
month who were assessed for active tuberculosis at
every visit within past month
% of estimated number of HIV-exposed infants 21.3±34.2
born in this month who received antiretroviral
prophylaxis per month
% of HIV patients on antiretroviral therapy who 27.2±16.6
were seen in clinic within past month who had
documented contact tracing information for 2
cohorts
% of HIV patients in general care seen at clinic 34.6±21.2
within past 6 months who had CD4 test once
during those 6 months
% of estimated number of HIV-exposed infants 59.2±44.6
born in preceding 12 months who started receiving
cotrimoxazole within 2 months of age
Catsambas 2008–10 Uganda ITS QIC % of HIV patients on antiretroviral therapy seen at 26.2±7.5
[52,54,55,57,58] clinic within past month who were adherent to
95% or more of prescribed doses of antiretroviral
medicines
% of HIV patients in general care or on 19.6±13.8
antiretroviral therapy seen at clinic within past
month who were assessed for active tuberculosis at
every visit within past month
Catsambas 2008–11 Uganda ITS QIC % of HIV patients on antiretroviral therapy seen at 17.6±3.6
[52,54,55,57,60] clinic within past month who were adherent to
95% or more of prescribed doses of antiretroviral
medicines
% of HIV patients on antiretroviral therapy for past 0.3±8.5
6 months seen at clinic who showed clinical
improvement (weight steady or increasing,
ambulatory or better, no opportunistic illnesses)
Catsambas 2008–12 Uganda ITS QIC % of HIV patients in general care or on 14.3±12.5
[52,54,55,57,60] antiretroviral therapy seen at clinic within past
month who were assessed for active tuberculosis at
every visit within past month
(Continued )
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 11 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
Table 1. (Continued)
Study ID Country Study Intervention Outcomes Effect
design size ± standard
error
Jaribu 2018 pilot Tanzania ITS QIC Median number of facility deliveries per facility per 85.7±55.4
[61] month
Jaribu 2018 Tanzania ITS QIC Median number of deliveries in which partographs 135.2±120.4
implementation with 4 assessment indicators completed per facility
[61–62] per month
Median number of facility deliveries per facility per 7.1±13.4
month
Catsambas 2008–1 Niger ITS QIC + training + poster for HCP % of live births delivered vaginally in the maternity 78.7±3.9
[52,55,57,63,64] for which immediate breastfeeding within one
hour after birth occurred
% of acute management of third stage of labor 46.3±3.9
standards met among total number of acute
management of third stage of labor standards
expected on the partographs analyzed
% of newborns whose temperature was measured 60.9±7.7
% of standards observed in essential newborn care 71.0±7.3
among total criteria expected in cases analyzed
% of vaginal deliveries performed in the maternity 91.4±2.6
where the three elements of active management of
third stage of labor were applied
Decrease = improvement: number of stillbirths per 16.9±22.4
1000 births in maternity (vaginal and cesarean)
Decrease = improvement: Number of neonatal 39.7±52.9
deaths by time of discharge from hospital per 1000
children born at home or in the maternity (vaginal
and cesarean)
Decrease = improvement: number of women who 96.0±20.1
suffered from postpartum hemorrhages per 1000
women who delivered vaginally in the maternity
Decrease = improvement: Number of all-cause 110.2±31.9
maternal deaths per 1000 births (vaginal or
cesarean) in the maternity
Decrease = improvement: Number of maternal 122.5±61.1
deaths due to postpartum hemorrhages per 1000
women who delivered vaginally in the maternity
Catsambas 2008–2 Niger ITS QIC + training + poster for HCP % of live births delivered vaginally in the maternity 96.7±2.2
[52,55,57,63,64] for which immediate breastfeeding within one
hour after birth occurred
% of standards observed in essential newborn care 85.7±24.9
among total criteria expected in cases analyzed
% of vaginal deliveries performed in the maternity 89.6±29.6
where the three elements of active management of
third stage of labor were applied
% of newborns whose temperature was measured 96.5±2.9
Decrease = improvement: number of stillbirths per 32.3±210.7
1000 births in maternity (vaginal and cesarean)
Decrease = improvement: Number of neonatal 221.9±227.4
deaths by time of discharge from hospital per 1000
children born at home or in the maternity (vaginal
and cesarean)
Catsambas 2008–3 Niger ITS QIC + training + poster for HCP % of pre-eclampsia and eclampsia case 35.3±10.3
[52,55,57,63,64] management criteria that were followed
(Continued )
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 12 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
Table 1. (Continued)
Study ID Country Study Intervention Outcomes Effect
design size ± standard
error
Westercamp 2017 Uganda ITS QIC + training + patient recording form % of all-field completeness (number of malaria 60.1±6.7
[65–67] records with all fields complete/number of malaria
records)
% of records with clinically relevant fields 61.6±2.6
completed (number of malaria records with
clinically-relevant fields complete/number of
malaria records)
% of discordance in malaria case reporting 47.4±66.1
(number of cases in outpatient registry minus
number reported in monthly report divided by
number of cases in registry)
% of discordance in test-positivity rate reporting 57.4±24.5
(test-positivity rate in lab register minus test-
positivity rate in report divided by test-positivity
rate of lab register)
Horwood 2017 [68– South CBA (RC) QIC + training + other printed job aid % of mothers who attended postnatal care within 7 -0.9±4.3
69] Africa (predominantly focused on LHW) days of delivery at HF
% of women who reported exclusive breastfeeding 18.7±6.0
for first 6 weeks after birth
% of women who reported being visited by HCP in 45.8±5.8
the first month after birth
% of women who reported being visited by HCP 55.1±5.7
during pregnancy
Webster 2012 [70] South ITS QIC + training + HCP deployment Monthly Highly Active Antiretroviral Treatment 101.1±21
Africa Initiations (number of HIV positive patients who
needed and were initiated on Highly Active
Antiretroviral Treatment)
Waiswa 2017–2 Uganda CBA QIC + health services performance % of women who reported delivering at a HF -3.0±6.1
[71–76] (NRC) reporting + community scorecard during their most recent pregnancy (within the
past 12 months)
% of births in which a uterotonic was administered 8.0±0.8
within 1 minute of delivery
% of women who reported immediate -6.0±5.6
breastfeeding within 1 hour of delivery during
most recent pregnancy (within past 12 months)
% of women who knew all three critical danger -2.0±6.4
signs in pregnancy reported during most recent
pregnancy (within past 12 months)
Waiswa 2017–1 Tanzania CBA QIC + health services performance % of women who reported delivering at a HF 7.0±7.1
[71–78] (NRC) reporting + community scorecard during their most recent pregnancy (within the
past 12 months)
% of births in which a uterotonic was administered 26.0±0.8
within 1 minute of delivery
% of women who reported immediate -7.0±7.1
breastfeeding within 1 hour of delivery during
most recent pregnancy (within past 12 months)
% of women who knew all three critical danger 4.0±7.4
signs in pregnancy reported during most recent
pregnancy (within past 12 months)
(Continued )
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 13 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
Table 1. (Continued)
Study ID Country Study Intervention Outcomes Effect
design size ± standard
error
Colbourn 2013 [42– Malawi CBA (RC) QIC + training + group process HCP Maternal mortality rate per 100000 livebirths -7.6b
44,79]a community + non-medical commodity Neonatal mortality rate per 1000 livebirths 0.1b
supply + non-performance- financial
incentive + printed materials for HCP Perinatal mortality rate per 1000 births (stillbirths 14.2b
+ supervision and early neonatal deaths)
CBA (NRC): Controlled Before-After study with non-randomized controls; CBA (RC): Pre-post study with randomized controls; CITS: Controlled interrupted time
series (with non-randomized controls); HCP: Health care provider; HF: Health facility; ITS: Interrupted time series; LHW: Lay or community health workers;
POS-CRT: Post-only study-cluster randomized trial; QIC: Quality improvement collaborative.
a
Colbourn 2013 is presented in two rows to indicate two different interventions from the same study.
b
Standard error not available.
https://doi.org/10.1371/journal.pone.0221919.t001
large effects (18.7 percentage points, for non-care-seeking patient behaviors) to very large
effects (50.4 percentage points, for health worker practice outcomes) (Table 3, rows 13–15).
p
Fig 2. Risk of bias of included studies: Summary and by domain item. Yes/done; Unclear; X No/not done; NA Not Applicable. CBA (NRC): Controlled Before-
After study with non-randomized controls; CBA (RC): Pre-post study with randomized controls; CITS: Controlled interrupted time series (with non-randomized
controls); HCPFI: Health Care Professional-directed financial incentives; ITS: Interrupted time series; OMT: Other management techniques; POS-CRT: Post-only
study-Cluster randomized trial; QIC: Quality Improvement Collaborative; R&G: Regulation and governance; S: Supervision; SI: Strengthening infrastructure; TR:
Training.
https://doi.org/10.1371/journal.pone.0221919.g002
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 14 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
Table 2. Number of comparisons and risk of bias by quality improvement collaborative strategy.
Strategy No. of Median follow-up time HCP type Risk of bias distribution
comparisons (months)
QIC only (no other strategy components) 21 11.1 HF-based 1 low, 1 moderate, 9 high, 10
HCPs very high
QIC + training 4 8.9 HF-based 1 moderate, 1 high, 2 very high
HCPs
QIC + strengthening infrastructurea + regulation and 2 11.0 HF-based 2 very high
governanceb HCPs
QIC + training + other management techniquesc 1 13.3 HF-based 1 high
HCPs
QIC + training + strengthening infrastructured + supervision 1 13.5 HF-based 1 high
+ other techniquese HCPs
QIC + training 1 14.5 LHWs 1 low
Total 30
HCP = Health care provider, HF = health facility, LHW = lay or community health workers, QIC = quality improvement collaborative.
a
Report cards (based on household and HF surveys) that summarized data on maternal and newborn health given to HFs and health managers.
b
Community scorecard to improve accountability.
c
Reorganization of HCP deployment (HCPs rotated to high-volume HFs when high staff turnover and absenteeism were affecting patient care).
d
Non-medical commodity supply (bicycles for group facilitators who worked with the community).
e
Group process between HCP and community.
https://doi.org/10.1371/journal.pone.0221919.t002
Both the random effects meta-analysis considering one median effect size per study com-
parison for each outcome (Table 3), and the sensitivity analysis considering all effect sizes indi-
vidually (S3 File) were consistent with the primary analysis. The certainty of the evidence
according to GRADE criteria was low or very low for all strategy-outcome combinations,
except for the effect of QIC + training on health worker practice outcomes for lay health work-
ers (moderate certainty). However, as the result for this last group is based on only a single
study, the generalizability is extremely limited.
Discussion
This systematic review and meta-analysis on QICs in LMICs showed variable effectiveness
across different outcomes and strategies. The quality of the evidence was mainly low or very
low [17]. We found consistent results using different statistical approaches.
In summary, among studies of health facility-based HCPs, for the “QIC only” strategy,
effectiveness varied highly across outcome groups, with no effect for patient health outcomes.
For the “QIC + training” strategy, effectiveness might be very high for patient health outcomes,
HCP practice outcomes, and care-seeking. Adding other management techniques to this strat-
egy might also be highly effective for patient care-seeking behaviors. The effect of “QIC + train-
ing + strengthening infrastructure + supervision + other management techniques” or “QIC
+ strengthening infrastructure + regulation and governance” strategies seemed small to
modest.
The only study assessing lay health workers showed effects that varied from essentially no
effect on care-seeking patient behaviors to a large effect on non-care-seeking patient behaviors
and HCP practice outcomes.
The main limitations of our systematic review were low quality of the evidence, scarce data
on long-term effects, and heterogeneous outcomes. Also, some included studies came from
unpublished gray literature, and several were conducted by the same group of authors. We
attempted to address any potential imbalance in the quality of these studies by applying the
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 15 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
Table 3. Summary of findings.
Population: Multidisciplinary healthcare teams (and patients that they care for) Settings: Health facilities or communities in LMICs
Intervention: Quality Improvement Collaborative / additional strategies—Comparison: Usual care
Outcomes Median MES (IQR / range) No. of studies GRADE a Mean MES from random effects meta-
/comparisons Certainty analysis
(No. of effect of the (95% CI; No. of comparisons; I2)e
sizes) evidence
Quality improvement collaborative only (HF-based HCPs; median follow-up 11.5 months)
Patient health outcomes %f 0.3 (no IQR / -15.0 to 11.4) 3 / 3 (5) Lowb -2.7 (-16.4 to 10.9; 3; 0%)
f h
Cont. 1.4 (no IQR / -75.3 to 3.0) 3 / 3 (6) Non-evaluable
Patient behaviors related to care-seeking % 7.7 (3.9 to 15.9 / -0.5 to 28.9) 8 / 8 (15) Lowb 5.9 (1.4 to 10.4; 8; 0%)
Cont. 62.2 (20.4 to 85.7 / 7.1 to 6 / 6 (7) 17.6 (-5.9 to 41.4; 6; 0%)
116.1)
Patient behaviors not related to care- % 17.6 (no IQR / 12.5 to 26.2) 3 / 3 (3) Very low 16.0 (9.9 to 22.1; 3; 59%)
seekingg b,c
Health worker practice outcomes % 30.2 (19.6 to 49.7 / 8.1 to 9 / 9 (19) Very lowb,d 36.3 (22.5 to 50.2; 9; 61%)
71.2) Lowb
Cont. 44.2 (no IQR / -28.2 to 4 / 4 (6) 4.2 (-3.7 to 12.1; 3; 0%)
135.2)
Facilitators (e.g., % of HW with job % 47.2 (no IQR or range) 1 / 1 (1) Low b Non-evaluable
description)
Quality improvement collaborative + training (HF-based HCPs; median follow-up 8.9 months)
Patient health outcomes Cont. 111.6 (no IQR / 96.0 to 2 / 2 (7) Lowb 96.4 (51.6 to 141.3; 2; 0%)
127.1)
Patient behaviors not related to care- % 87.7 (no IQR / 78.7 to 96.7) 2 / 2 (2) Very lowb,d 88.0 (70.3 to 105.6; 2; 94%)
seekingg
Health worker practice outcomes % 63.4 (no IQR / 35.3 to 89.6) 4 / 4 (10) Very lowb,d 60.9 (48.4 to 73.3; 4; 72%)
Cont. 52.4 (no IQR or range) 1 / 1 (2) Non-evaluable
Quality improvement collaborative + training + other management techniques (HF-based HCPs; median follow-up 13.3 months)
Patient behaviors related to care-seeking Cont. 101.1 (no IQR or range) 1 / 1 (1) Lowb Non-evaluable
Quality improvement collaborative + training + strengthen infrastructure + supervision + other management techniques (HF-based HCPs; median follow-up 13.5
months)
Patient health outcomes Cont. 0.1 (no IQR or range) 1 / 1 (3)i Very low b Non-evaluable
Quality improvement collaborative + strengthen infrastructure + regulation and governance (HF-based HCPs; median follow-up 11.0 months)
Patient behaviors related to care-seeking % 9.5 (no IQR / 2.5 to 16.5) 2 / 2 (4)i Very lowb,d 9.3 (-4.4 to 23.0; 2; 82%)
Patient behaviors not related to care- % -2.8 (no IQR / -4.0 to -1.5) 2 / 2 (4)i Very low b -3.0 (-11.0 to 5.1; 2; 0%)
seekingg
Quality improvement collaborative + training (focused predominantly on lay/community health workers; median follow-up 14.4 months)
Patient behaviors related to care-seeking % -0.9 (no IQR or range) 1 / 1 (1)i Low Non-evaluable
i
Patient behaviors not related to care- % 18.7 (no IQR or range) 1 / 1 (1) Low Non-evaluable
seekingf
(Continued )
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 16 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
Table 3. (Continued)
Health worker practice outcomes % 50.4 (no IQR or range) 1 / 1 (2)i Moderate Non-evaluable
MES: median effect size per comparison; 95% CI: 95% confidence interval; HF-based HCPs: health facility-based health care providers; IQR: Interquartile range
a
GRADE: The certainty evidence for RCTs, ITS studies, and other non-randomized studies started at high, moderate, and low, respectively.
High certainty: Very good indication of the likely effect. The likelihood that the effect will be substantially different is low.
Moderate certainty: Good indication of the likely effect. The likelihood that the effect will be substantially different is moderate.
Low certainty: Some indication of the likely effect. However, the likelihood that it will be substantially different is high.
Very low certainty: Not a reliable indication of the likely effect. The likelihood that the effect will be markedly different is very high.
b
Certainty evidence was downgraded 1 level for serious risk of bias.
c
Certainty evidence was downgraded 1 level for serious inconsistency.
d
Certainty evidence was downgraded 2 levels for very serious inconsistency.
e
Meta-analysis could only be performed if the number of median effect sizes was > 1 and their standard errors were available.
f
%: outcome expressed as a percentage, Cont.: outcome expressed as continuous and unbounded.
g
For example, patient adherence to treatment regimen.
h
Three out of 6 effect sizes were from controlled before-after study.
i
All effect sizes from were controlled before-after studies.
https://doi.org/10.1371/journal.pone.0221919.t003
same risk-of-bias assessment to all included studies. Furthermore, the random effects meta-
analysis in this review was limited by the low quality of studies and wide diversity of outcomes.
However, we believe meta-analysis as a secondary analysis tool provided useful complemental
information about the direction, magnitude, and precision of intervention effects. Strengths of
our review were that it was based on an extensive literature review from multiple sources, it
used a single analytic framework with comparable effect sizes (as opposed to reporting differ-
ent effect sizes, such as odds ratios and risk differences, from different studies), and it focused
on LMIC settings. Its results can inform decision-making for health programs and interven-
tion implementers with regards to which QIC-based interventions are most effective for
improving which aspects of health systems in LMICs. Considering the small number of studies
for each main comparison and the low quality of evidence, this review also highlights substan-
tial evidence gaps and important opportunities for improvement in the conduct of future QIC
studies.
Previous systematic reviews have approached the topic of QIC effectiveness in different
ways and did not include several studies captured by our work [8–10]; nevertheless, they
found similar effects and evidence gaps. Numerous potential determinants of QIC success
were evaluated in a systematic review that did not include any of the primary studies included
in our review, and only a few related to empirical effectiveness [24]. For example, some aspects
of teamwork and participation in specific collaborative activities seem to improve short-term
success, while sustainability of teams and continued data gathering enhanced the chances of
long-term success. In a study currently underway, the impact of district-led learning on clini-
cal practice and patient outcomes, communication, HCP motivation, and team dynamics are
being explored [25, 26]. It would be desirable for future studies to examine what core compo-
nents of QICs are related to patient- and provider-level outcomes.
Our findings clearly show that there is still not a solid evidence base on the effect of QICs in
LMICs, although our results suggest that there are situations in which QICs could be consid-
ered. QICs are not static structures–rather, they have been implemented and adapted in a
number of ways to achieve their stated aims. Some common adaptations include their use for
generating new ideas and for empowering HCPs. Although based on relatively few studies, our
review’s results suggest that combining QICs with training might be the most effective
approach for implementing QICs.
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 17 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
Finally, on the recommendation for additional studies on QICs, we think that the ideal
study design would be an interrupted time series with a randomized control group. The justifi-
cation is that such a design would allow for an overall evaluation of intervention effectiveness
as well as an evaluation of heterogeneity of effectiveness among sites. The design would also
allow for a characterization of the effect over time. Other attributes include a follow-up time of
at least 12 months, an objective data source for the evaluation (i.e., not only data collected by
the QI teams unless the data quality is reasonably good and data quality does not change over
time), a sample size that reflects real-world QICs (i.e., at least 20 facilities per study arm), quali-
tative and process evaluation components to describe how the intervention worked, a costing
and economic evaluation, and an assessment of whether the intervention had any negative
effects (e.g., drawing health workers’ attention to one aspect of care that decreases quality for
other aspects of care).
In conclusion, the overall quality of the evidence on the effectiveness of QICs in LMICs was
low. Based on the large and variable effect sizes seen in some outcome groups, additional
research with high-quality studies is warranted to provide a more reliable and precise estima-
tion of the effect of this promising intervention.
Supporting information
S1 Checklist. PRISMA checklist.
(PDF)
S1 File. Details of the search strategy.
(PDF)
S2 File. Meta-analysis results, forest plots, and funnel plots.
(PDF)
S3 File. Sensitivity analysis and list of excluded studies.
(PDF)
Acknowledgments
This study was performed as part of the Lancet Global Health Commission on High Quality
Health Systems in the SDG Era, which the authors thank. We also thank the HCPPR team
members and Daniel Comandé and Cintia Spira from IECS for their assistance. This article is
based upon information in the Health Care Provider Performance Review, a joint program of
CDC, Harvard Medical School, World Health Organization, Management Sciences for Health,
Johns Hopkins University, and the CDC Foundation.
Disclaimer: the findings and conclusions presented in this report are those of the authors
and do not necessarily reflect the official position of the Centers for Disease Control and Pre-
vention and the CDC Foundation.
Author Contributions
Conceptualization: Ezequiel Garcia-Elorrio, Agustı́n Ciapponi, Alexander K. Rowe.
Data curation: Samantha Y. Rowe.
Formal analysis: Ezequiel Garcia-Elorrio, Samantha Y. Rowe, Maria E. Teijeiro, Agustı́n Ciap-
poni, Alexander K. Rowe.
Funding acquisition: Ezequiel Garcia-Elorrio.
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 18 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
Investigation: Ezequiel Garcia-Elorrio, Agustı́n Ciapponi, Alexander K. Rowe.
Methodology: Ezequiel Garcia-Elorrio, Samantha Y. Rowe, Agustı́n Ciapponi, Alexander K.
Rowe.
Project administration: Ezequiel Garcia-Elorrio, Agustı́n Ciapponi.
Resources: Samantha Y. Rowe, Maria E. Teijeiro, Alexander K. Rowe.
Software: Samantha Y. Rowe, Agustı́n Ciapponi.
Supervision: Ezequiel Garcia-Elorrio.
Validation: Samantha Y. Rowe, Maria E. Teijeiro, Agustı́n Ciapponi, Alexander K. Rowe.
Writing – original draft: Ezequiel Garcia-Elorrio, Agustı́n Ciapponi, Alexander K. Rowe.
Writing – review & editing: Ezequiel Garcia-Elorrio, Samantha Y. Rowe, Maria E. Teijeiro,
Agustı́n Ciapponi, Alexander K. Rowe.
References
1. The Millennium Development Goals Report 2015. New York: United Nations; 2015.
2. Sachs JD. From millennium development goals to sustainable development goals. Lancet. 2012; 379
(9832):2206–11. https://doi.org/10.1016/S0140-6736(12)60685-0 PMID: 22682467
3. Kruk ME, Gage AD, Arsenault C, Jordan K, Leslie HH, Roder-DeWan S, et al. High-quality health sys-
tems in the Sustainable Development Goals era: time for a revolution. Lancet Glob Health. 2018; 6(11):
e1196–e252. https://doi.org/10.1016/S2214-109X(18)30386-3 PMID: 30196093
4. Ovretveit J, Bate P, Cleary P, Cretin S, Gustafson D, McInnes K, et al. Quality collaboratives: lessons
from research. Quality & Safety in Health Care. 2002; 11(4):345–51.
5. Nadeem E, Olin SS, Hill LC, Hoagwood KE, Horwitz SM. Understanding the components of quality
improvement collaboratives: a systematic literature review. Milbank Q. 2013; 91(2):354–94. https://doi.
org/10.1111/milq.12016 PMID: 23758514
6. Institute for Healthcare Improvement. The Breakthrough Series: IHI’s Collaborative Model for Achieving
Breakthrough Improvement. Cambridge, Massachusetts: Institute for Healthcare Improvement. 2003.
7. Kruk ME, Pate M, Mullan Z. Introducing The Lancet Global Health Commission on High-Quality Health
Systems in the SDG Era. Lancet Glob Health. 2017; 5(5):e480–e1. https://doi.org/10.1016/S2214-109X
(17)30101-8 PMID: 28302563
8. Schouten LM, Hulscher ME, van Everdingen JJ, Huijsman R, Grol RP. Evidence for the impact of quality
improvement collaboratives: systematic review. BMJ. 2008; 336(7659):1491–4. https://doi.org/10.
1136/bmj.39570.749884.BE PMID: 18577559
9. de Silva D. Improvement collaboratives in health care. London: Health Foundation, 2014.
10. Wells S, Tamir O, Gray J, Naidoo D, Bekhit M, Goldmann D. Are quality improvement collaboratives
effective? A systematic review. BMJ Qual Saf. 2018; 27(3):226–40. https://doi.org/10.1136/bmjqs-
2017-006926 PMID: 29055899
11. Rowe AK, Rowe SY, Peters DH, Holloway KA, Chalker J, Ross-Degnan D. Effectiveness of strategies
to improve health-care provider practices in low-income and middle-income countries: a systematic
review. The Lancet Global Health. 2018; 6(11):e1163–e75. https://doi.org/10.1016/S2214-109X(18)
30398-X PMID: 30309799
12. Higgins J, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0
[updated March 2011]. Chichester: The Cochrane Collaboration 2011.
13. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement
for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions:
explanation and elaboration. BMJ. 2009; 339:b2700. https://doi.org/10.1136/bmj.b2700 PMID:
19622552
14. Cochrane Effective Practice and Organization of Care (EPOC). What study designs should be included
in an EPOC review? EPOC Resources for review authors. 2017 [23 January, 2018]. Available from:
http://epoc.cochrane.org/resources/epoc-resources-review-authors
15. World Bank Country and Lending Groups Washington, DC. 2018 [07/01/2018]. Available from: https://
datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 19 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
16. Cochrane Effective Practice and Organization of Care (EPOC). Suggested risk of bias criteria for EPOC
reviews. EPOC Resources for review authors. 2017 [updated January 2018]. Available from: http://
epoc.cochrane.org/resources/epoc-resources-review-authors.
17. Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-
GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011; 64(4):383–94 https://
doi.org/10.1016/j.jclinepi.2010.04.026 PMID: 21195583
18. Schünemann H, Brożek J, Guyatt G, Oxman A, (editors). Handbook for grading the quality of evidence
and the strength of recommendations using the GRADE approach. 2013 [updated October 2013]. Avail-
able from: http://gdt.guidelinedevelopment.org/app/index.html.
19. Harder T, Abu Sin M, Bosch-Capblanch X, Bruno C, de Carvalho Gomes H, Duclos P, et al. Towards a
framework for evaluating and grading evidence in public health. Health Policy. 2015; 119(6):732–6.
https://doi.org/10.1016/j.healthpol.2015.02.010 PMID: 25863647
20. Schunemann HJ, Cuello C, Akl EA, Mustafa RA, Meerpohl JJ, Thayer K, et al. GRADE guidelines: 18.
How ROBINS-I and other tools to assess risk of bias in nonrandomized studies should be used to rate
the certainty of a body of evidence. J Clin Epidemiol. 2018.
21. Ivers N, Jamtvedt G, Flottorp S, Young JM, Odgaard-Jensen J, French SD, O’Brien MA, Johansen M,
Grimshaw J, Oxman AD. Audit and feedback: effects on professional practice and healthcare out-
comes. Cochrane Database of Systematic Reviews 2012, Issue 6. Art. No.: CD000259. https://doi.org/
10.1002/14651858.CD000259.pub3 PMID: 22696318
22. Holloway KA, Ivanovska V, Wagner AK, Vialle-Valentin C, D. R-D. Have we improved use of medicines
in developing and transitional countries and do we know how to? Two decades of evidence. Tropical
Medicine and International Health. 2013; 18:656–64. https://doi.org/10.1111/tmi.12123 PMID:
23648177
23. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ
(Clinical research ed.). 2003; 327(7414), 557–560. https://doi.org/10.1136/bmj.327.7414.557 PMID:
12958120
24. Hulscher ME, Schouten LM, Grol RP, Buchan H. Determinants of success of quality improvement col-
laboratives: what does the literature show? BMJ Qual Saf. 2013; 22(1):19–31. https://doi.org/10.1136/
bmjqs-2011-000651 PMID: 22879447
25. Magge H, Chilengi R, Jackson EF, Wagenaar BH, Kante AM. Tackling the hard problems: implementa-
tion experience and lessons learned in newborn health from the African Health Initiative. BMC health
services research. 2017; 17(Suppl 3):829. https://doi.org/10.1186/s12913-017-2659-4 PMID:
29297352
26. Magge H, Garcia-Elorrio E, Liljestrand J, Hirschhorn L, Twum-Danso N, Roder-DeWan S, et al. From
Spread to QI Institutionalization: The Adaptation of Improvement Collaborative Design and Aims in
LMICs (in press).
27. N’Guessan J, Franco LM, Ackah A, Kouassi V, Gondwe T. Effects of collaborative improvement on
PMTCT and ART indicators in Cote d’Ivoire: a comparative study. Bethesda, MD: University Research
Co., LLC (URC), 2011.
28. N’Guessan J, Traore V, Boucar M, Ackah A, Dosso Y, Kouassi V, et al. Results from the pilot phase of
an ART/PMTCT improvement collaborative in Cote d’Ivoire. Bethesda, MD: University Research Co.,
LLC (URC), 2011.
29. Chitashvili T, editor Addressing rational use of medication in pediatric patients with respiratory tract
infections (RTI) through improvement collaborative in Georgia. Third Global Symposium on Health Sys-
tems Research; 2014 30 September to 3 October 2014; Cape Town, South Africa.
30. Chitashvili T. Rationale for improving integrated service delivery: reduced cost and improved care in
Georgia. International Journal of Integrated Care. 2015; 15(8).
31. Chitashvili T. Scaling Up, sustaining and institutionalizing better health care in Georgia: results and stra-
tegic recommendations from USAID support for improving quality of priority clinical conditions during
2012–2015. Technical Report. 2015.
32. Chitashvili T, Cherkezishvili E. Improving quality of care for respiratory tract infections in children: the
role of capacity building and coaching in supporting one multi-facility improvement team in Samtredia
district, Georgia. Submitted to a journal for publication to Lancet of Infectious Diseases 2017:22.
33. Chitashvili T CE, Broughton E, Chkhaidze I, Shengelia N, Hill K, Massoud MR, Ruadze E. Improving
antibiotic prescription practices for pediatric respiratory tract infections in Georgia. Forthcoming (submit-
ted in 2017 for publication to Lancet Infectious Diseases). 2017.
34. USAID. USAID ASSIST Project: Applying Science to Strengthen and Improve Systems (ASSIST) Proj-
ect. Georgia Country Report FY14. Bethesda, MD: University Research Co., LLC (URC), 2014.
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 20 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
35. Singh K, Speizer I, Handa S, Boadu RO, Atinbire S, Barker PM, et al. Impact evaluation of a quality
improvement intervention on maternal and child health outcomes in Northern Ghana: early assessment
of a national scale-up project. Int J Qual Health Care. 2013; 25(5):477–87. https://doi.org/10.1093/
intqhc/mzt054 PMID: 23925506; PubMed Central PMCID: PMC3888142.
36. Twum-Danso NA, Akanlu GB, Osafo E, Sodzi-Tettey S, Boadu RO, Atinbire S, et al. A nationwide qual-
ity improvement project to accelerate Ghana’s progress toward Millennium Development Goal Four:
design and implementation progress. Int J Qual Health Care. 2012; 24(6):601–11. https://doi.org/10.
1093/intqhc/mzs060 PMID: 23118097.
37. Twum-Danso NA, Dasoberi IN, Amenga-Etego IA, Adondiwo A, Kanyoke E, Boadu RO, et al. Using
quality improvement methods to test and scale up a new national policy on early post-natal care in
Ghana. Health Policy Plan. 2014; 29(5):622–32. https://doi.org/10.1093/heapol/czt048 PMID:
23894073.
38. Cofie LE, Barrington C, Akaligaung A, Reid A, Fried B, Singh K, et al. Integrating community outreach
into a quality improvement project to promote maternal and child health in Ghana. Glob Public Health.
2014; 9(10):1184–97. https://doi.org/10.1080/17441692.2014.952656 PMID: 25204848; PubMed Cen-
tral PMCID: PMC4310571.
39. Singh K, Brodish P, Speizer I, Barker P, Amenga-Etego I, Dasoberi I, et al. Can a quality improvement
project impact maternal and child health outcomes at scale in northern Ghana? Health Res Policy Syst.
2016; 14(1):45. https://doi.org/10.1186/s12961-016-0115-2 PMID: 27306769; PubMed Central PMCID:
PMC4910198.
40. Afari H, Hirschhorn LR, Michaelis A, Barker P, Sodzi-Tettey S. Quality improvement in emergency
obstetric referrals: qualitative study of provider perspectives in Assin North District, Ghana. BMJ Open.
2014; 4(5):e005052. https://doi.org/10.1136/bmjopen-2014-005052 PMID: 24833695; PubMed Central
PMCID: PMC4025473.
41. Speizer IS, Story WT, Singh K. Factors associated with institutional delivery in Ghana: the role of deci-
sion-making autonomy and community norms. BMC Pregnancy Childbirth. 2014; 14:398. https://doi.
org/10.1186/s12884-014-0398-7 PMID: 25427853; PubMed Central PMCID: PMC4247879.
42. Colbourn T, Nambiar B, Bondo A, Makwenda C, Tsetekani E, Makonda-Ridley A, et al. Effects of quality
improvement in health facilities and community mobilization through women’s groups on maternal, neo-
natal and perinatal mortality in three districts of Malawi: MaiKhanda, a cluster randomized controlled
effectiveness trial. Int Health. 2013; 5(3):180–95. https://doi.org/10.1093/inthealth/iht011 PMID:
24030269; PubMed Central PMCID: PMC5102328.
43. Colbourn T, Pulkki-Brannstrom AM, Nambiar B, Kim S, Bondo A, Banda L, et al. Cost-effectiveness and
affordability of community mobilisation through women’s groups and quality improvement in health facil-
ities (MaiKhanda trial) in Malawi. Cost Eff Resour Alloc. 2015; 13(1):1. https://doi.org/10.1186/s12962-
014-0028-2 PMID: 25649323; PubMed Central PMCID: PMC4299571.
44. Colbourn T, Nambiar B, Costello A, MaiKhanda A. Final Evaluation Report. The impact of quality
improvement at health facilities and community mobilisation by women’s groups on birth outcomes: an
effectiveness study in three districts of Malawi. 2013.
45. Barcelo A, Cafiero E, de Boer M, Mesa AE, Lopez MG, Jimenez RA, et al. Using collaborative learning
to improve diabetes care and outcomes: the VIDA project. Prim Care Diabetes. 2010; 4(3):145–53.
https://doi.org/10.1016/j.pcd.2010.04.005 PMID: 20478753.
46. Crigler L, Boucar M, K. S, Abdou S, Djibrina S, Saley Z. The Human Resources Collaborative: Improv-
ing Maternal and Child Care in Niger. Final Report. 2012.
47. USAID. USAID Health Care Improvement Project. Strengthening human resources for health to
improve maternal care in Niger’s Tahoua region. Bethesda, MD: University Research Co., LLC (URC),
2011.
48. Oyeledun B, Phillips A, Oronsaye F, Alo OD, Shaffer N, Osibo B, et al. The Effect of a Continuous Qual-
ity Improvement Intervention on Retention-In-Care at 6 Months Postpartum in a PMTCT Program in
Northern Nigeria: Results of a Cluster Randomized Controlled Study. J Acquir Immune Defic Syndr.
2017; 75 Suppl 2:S156–S64. https://doi.org/10.1097/QAI.0000000000001363 PMID: 28498185.
49. Osibo B, Oronsaye F, Alo OD, Phillips A, Becquet R, Shaffer N, et al. Using small tests of change to
improve PMTCT services in Northern Nigeria: Experiences from implementation of a continuous quality
improvement and breakthrough series program. Journal of Acquired Immune Deficiency Syndromes.
2017; 75:S165–S72. https://doi.org/10.1097/QAI.0000000000001369 PMID: 28498186
50. Oyeledun B, Oronsaye F, Oyelade T, Becquet R, Odoh D, Anyaike C, et al. Increasing retention in care
of HIV-positive women in PMTCT services through continuous quality improvement-breakthrough
(CQI-BTS) series in primary and secondary health care facilities in Nigeria: a cluster randomized con-
trolled trial. The Lafiyan Jikin Mata Study. J Acquir Immune Defic Syndr. 2014; 67 Suppl 2:S125–31.
https://doi.org/10.1097/QAI.0000000000000320 PMID: 25310118.
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 21 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
51. USAID Health Care Improvement Project. The Improvement Collaborative: An Approach to Rapidly
Improve Health Care and Scale Up Quality Services. Bethesda, MD: University Research Co., LLC
(URC), 2008 June 2008. Report No.
52. Massoud M. Applying modern quality improvement methodology to maternal and child health in Tver
Oblast, Russian Federation. QA Brief. 2001; 9(2):28–32.
53. Abdallah H, Chernobrovkinam O, Korotkova A, Massoud R, Burkhalter B. Improving the quality of care
for women with pregnancy-induced hypertension reduces costs in Tver, Russia. Operations Research
Results 2(4). Bethesda, MD: Agency for International Development (USAID), 2002.
54. Ethier K. Developing evidence-based standards for pregnancy-induced hypertension in Russia. Quality
Assurance Project Case Study. Bethesda, MD: Agency for International Development (USAID), 2001.
55. Catsambas TT, Franco LM, Gutmann M, Knebel E, Hill P, Lin Y-S, et al. Evaluating health care collabo-
ratives: the experience of the Quality Assurance Project. Bethesda, MD: University Research Co., LLC
(URC), 2008.
56. Franco L, Marquez L, Ethier K, Balsara Z, Isenhower W. Results of collaborative improvement: effects
on health outcomes and compliance with evidence-based standards in 27 applications in 12 countries.
2009.
57. Franco LM, Marquez L. Effectiveness of collaborative improvement: evidence from 27 applications in
12 less-developed and middle-income countries. BMJ Quality & Safety. 2011; 20(8):658–65. https://doi.
org/10.1136/bmjqs.2010.044388 PMID: 21317182.
58. Furth R, Gass R, Kagubare J. Rwanda human resources assessment for HIV/AIDS services scale up:
summary report. Operations Research Results. 2006.
59. Ngidi W, Reddy J, Luvuno Z, Rollins N, Barker P, Mate KS. Using a campaign approach among health
workers to increase access to antiretroviral therapy for pregnant HIV-infected women in South Africa. J
Acquir Immune Defic Syndr. 2013; 63(4):e133–9. https://doi.org/10.1097/QAI.0b013e318291827f
PMID: 23514955.
60. Wittcoff A, Furth R, Nabwire J, Crigler L. Baseline assessment of HIV service provider productivity and
efficiency in Uganda. Technical Report. 2010.
61. Jaribu J, Penfold S, Manzi F, Schellenberg J, Pfeiffer C. Improving institutional childbirth services in
rural Southern Tanzania: a qualitative study of healthcare workers’ perspective. BMJ Open. 2016; 6(9):
e010317. Epub 2016/09/24. https://doi.org/10.1136/bmjopen-2015-010317 PMID: 27660313; PubMed
Central PMCID: PMC5051329.
62. Jaribu J, Penfold S, Green C, Manzi F, Schellenberg J. Improving Tanzanian childbirth service quality.
Int J Health Care Qual Assur. 2018; 31(3):190–202. Epub 2018/04/25. https://doi.org/10.1108/IJHCQA-
10-2015-0122 PMID: 29687759; PubMed Central PMCID: PMC5974692.
63. Broughton E, Saley Z, Boucar M, Alagane D, Hill K, Marafa A, et al. Cost-effectiveness of a quality
improvement collaborative for obstetric and newborn care in Niger. International Journal of Health Care
Quality Assurance. 2013; 26(3):250–61. https://doi.org/10.1108/09526861311311436 PMID:
23729128.
64. Franco L, Webb L. Niger Site Visit Report. Unpublished report prepared for the U.S. Agency for Interna-
tional Development (USAID) by the USAID Health Care Improvement Project and the Quality Assur-
ance Project. 2008.
65. Westercamp N, Staedke S, Hutchinson E, Naiga S, Nabirye C, Taaka L, et al., editors. Effectiveness
and sustainability of a collaborative improvement method to increase the quality of routine malaria sur-
veillance data in Kayunga District, Uganda. 66th Annual Meeting of the American Society of Tropical
Medicine and Hygiene;; 2017 Nov 5–9; Baltimore, MD.
66. Hutchinson E, Nayiga S, Nabirye C, Taaka L, Westercamp N, Rowe A, et al. Opening the ’Black Box’ of
collaborative improvement: a qualitative evaluation of a pilot intervention to improve quality of surveil-
lance data in public health centres in Uganda. 2017.
67. Fatuma A. The Republic of Uganda, Kayunga District Local Government: 3-year district development
plan, 2010/2011. 2010 Apr 282010.
68. Horwood C, Butler L, Barker P, Phakathi S, Haskins L, Grant M, et al. A continuous quality improvement
intervention to improve the effectiveness of community health workers providing care to mothers and
children: a cluster randomised controlled trial in South Africa. Hum Resour Health. 2017; 15(1):39.
https://doi.org/10.1186/s12960-017-0210-7 PMID: 28610590; PubMed Central PMCID: PMC5470211.
69. Horwood CM, Youngleson MS, Moses E, Stern AF, Barker PM. Using adapted quality-improvement
approaches to strengthen community-based health systems and improve care in high HIV-burden sub-
Saharan African countries. AIDS. 2015; 29 Suppl 2:S155–64. https://doi.org/10.1097/QAD.
0000000000000716 PMID: 26102626.
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 22 / 23
Systematic review on effectiveness of quality improvement collaboratives in LMIC
70. Webster PD, Sibanyoni M, Malekutu D, Mate KS, Venter WDF, Barker PM, et al. Using quality improve-
ment to accelerate highly active antiretroviral treatment coverage in South Africa. BMJ Quality and
Safety. 2012; 21 (4):315–24. https://doi.org/10.1136/bmjqs-2011-000381 PMID: 22438327.
71. Waiswa P, Manzi F, Mbaruku G, Rowe A, Marx M, Tomson G, et al. Effects of collaborative quality
improvement on maternal and newborn health care in Tanzania and Uganda. The Expanded Quality
Management Using Information Power (EQUIP) quasi-experimental study. Implementation Science.
2017;(1).
72. Tancred T, Mandu R, Hanson C, Okuga M, Manzi F, Peterson S, et al. How people-centred health sys-
tems can reach the grassroots: experiences implementing community-level quality improvement in rural
Tanzania and Uganda. Health Policy Plan. 2018; 33(1):e1–e13. https://doi.org/10.1093/heapol/czu070
PMID: 29304250.
73. Marchant T, Schellenberg J, Peterson S, Manzi F, Waiswa P, Hanson C, et al. The use of continuous
surveys to generate and continuously report high quality timely maternal and newborn health data at the
district level in Tanzania and Uganda. Implement Sci. 2014; 9:112. https://doi.org/10.1186/s13012-014-
0112-1 PMID: 25149316; PubMed Central PMCID: PMC4160540.
74. Hanson C, Waiswa P, Marchant T, Marx M, Manzi F, Mbaruku G, et al. Erratum to: Expanded Quality
Management Using Information Power (EQUIP): protocol for a quasi-experimental study to improve
maternal and newborn health in Tanzania and Uganda. Implement Sci. 2015; 10:152. https://doi.org/10.
1186/s13012-015-0343-9 PMID: 26515014; PubMed Central PMCID: PMC4627429.
75. Hanson C, Waiswa P, Marchant T, Marx M, Manzi F, Mbaruku G, et al. Expanded Quality Management
Using Information Power (EQUIP): protocol for a quasi-experimental study to improve maternal and
newborn health in Tanzania and Uganda. Implement Sci. 2014; 9(1):41. https://doi.org/10.1186/1748-
5908-9-41 PMID: 24690284; PubMed Central PMCID: PMC4230245.
76. Hanson C, Marchant T, Waiswa P, Manzi F, Schellenberg J, Willey B, et al. Overcoming low implemen-
tation levels for essential maternal and newborn health interventions: Results from the equip project
using systemic quality improvement in Tanzania and Uganda. International Journal of Gynecology and
Obstetrics. 2015; 131:E331.
77. Baker U, Hassan F, Hanson C, Manzi F, Marchant T, Swartling Peterson S, et al. Unpredictability dic-
tates quality of maternal and newborn care provision in rural Tanzania-A qualitative study of health
workers’ perspectives. BMC Pregnancy Childbirth. 2017; 17(1):55. https://doi.org/10.1186/s12884-017-
1230-y PMID: 28166745; PubMed Central PMCID: PMC5294891.
78. Tancred T, Manzi F, Schellenberg J, Marchant T. Facilitators and Barriers of Community-Level Quality
Improvement for Maternal and Newborn Health in Tanzania. Qual Health Res. 2017; 27(5):738–49.
https://doi.org/10.1177/1049732316638831 PMID: 27022034.
79. The Health Foundation. Process evaluation of community intervention: baseline report on the experi-
ences of women volunteers as women’s group facilitators. In: Centre for International Health & Develop-
ment, Institute of Child Health. UCL (UK)2008. p. 45 p. Report No.: 20080924 (v1.4 Final) WGF
Report.
PLOS ONE | https://doi.org/10.1371/journal.pone.0221919 October 3, 2019 23 / 23
You might also like
- BMC Health Services Research: Evidence Based Practice in Postgraduate Healthcare Education: A Systematic ReviewDocument8 pagesBMC Health Services Research: Evidence Based Practice in Postgraduate Healthcare Education: A Systematic Reviewruba azfr-aliNo ratings yet
- Efectividad de Telepsiquiatría Revisión 2008Document10 pagesEfectividad de Telepsiquiatría Revisión 2008psychforallNo ratings yet
- Kim, 2022 - MADocument26 pagesKim, 2022 - MAAnindya Laksmi LarasatiNo ratings yet
- The Effects of Pay-for-Performance Programs On Health, Health Care Use, and Processes of CareDocument14 pagesThe Effects of Pay-for-Performance Programs On Health, Health Care Use, and Processes of CareMasrun FatanahNo ratings yet
- 1019.fullDocument14 pages1019.fullKelly ChanNo ratings yet
- SkizofreniaDocument20 pagesSkizofreniairfan permanaNo ratings yet
- Characteristics of Case Management in Primary Care PDFDocument11 pagesCharacteristics of Case Management in Primary Care PDFCamila AlmeidaNo ratings yet
- mzq028Document7 pagesmzq028eliamusa981No ratings yet
- Campbell Systematic Reviews - 2022 - Apunyo - Interventions To Increase Youth Employment An Evidence and Gap MapDocument28 pagesCampbell Systematic Reviews - 2022 - Apunyo - Interventions To Increase Youth Employment An Evidence and Gap Mapsantiago maciasNo ratings yet
- Como Hacer Una Guia ClinicaDocument11 pagesComo Hacer Una Guia ClinicamiguelpaillalefgutierrezNo ratings yet
- Role of quality improvement in strengthening health systems in developing countriesDocument7 pagesRole of quality improvement in strengthening health systems in developing countriesChristian Bernard OchiengNo ratings yet
- Sacks Et Al. - 2015 - Teamwork, Communication and Safety Climate A Systematic Review of Interventions To Improve Surgical CultureDocument11 pagesSacks Et Al. - 2015 - Teamwork, Communication and Safety Climate A Systematic Review of Interventions To Improve Surgical CultureEdy Tahir MattoreangNo ratings yet
- Victoria Tzortziou Brown, Martin Underwood, Olwyn M Westwood, Dylan MorrisseyDocument9 pagesVictoria Tzortziou Brown, Martin Underwood, Olwyn M Westwood, Dylan MorrisseyCarolina UrrutiaNo ratings yet
- A Questionnaire Based Study-Assessment of KnowledgDocument5 pagesA Questionnaire Based Study-Assessment of KnowledgAnitha NoronhaNo ratings yet
- Performance Incentives Improve Child Health OutcomesDocument7 pagesPerformance Incentives Improve Child Health OutcomesTheodora Ferminarti JatyNo ratings yet
- Hex 21 41Document16 pagesHex 21 41fadedoyinNo ratings yet
- Murphy 2021Document11 pagesMurphy 2021okNo ratings yet
- J Jid 2017 03 004Document5 pagesJ Jid 2017 03 004lifeofthiru11No ratings yet
- Effect of CDSSDocument20 pagesEffect of CDSSMia Md. RaihanNo ratings yet
- Systematic ReviewDocument6 pagesSystematic ReviewRosa ValenteNo ratings yet
- RoweS - 2022 (HCPPR Supervision Effectiveness)Document12 pagesRoweS - 2022 (HCPPR Supervision Effectiveness)Karen ZamboniNo ratings yet
- Portofolio 1Document8 pagesPortofolio 1pt metaNo ratings yet
- Clinical Nutrition: Xiaoli Ruan, Rena Nakyeyune, Yi Shao, Yi Shen, Chen Niu, Zhaoping Zang, Toni Miles, Fen LiuDocument11 pagesClinical Nutrition: Xiaoli Ruan, Rena Nakyeyune, Yi Shao, Yi Shen, Chen Niu, Zhaoping Zang, Toni Miles, Fen LiushangrilaNo ratings yet
- E20200213 FullDocument11 pagesE20200213 FullFC Mekar AbadiNo ratings yet
- 2013 - Novak - Interventions For Children With CPDocument26 pages2013 - Novak - Interventions For Children With CPFriendlymeNo ratings yet
- Clinical Practice GuidelinesDocument9 pagesClinical Practice Guidelinesmarii de los angelesNo ratings yet
- Clinical Trial Reporting LevelsDocument57 pagesClinical Trial Reporting LevelsJoko WinarnoNo ratings yet
- Kutz (2019) Eating Disorder Screening SCOFF - CompressedDocument9 pagesKutz (2019) Eating Disorder Screening SCOFF - CompressedPatricia LopesNo ratings yet
- Jnu.12274 Sistematik ReviewDocument10 pagesJnu.12274 Sistematik ReviewMastifa HanasitaNo ratings yet
- JCI Whitepaper Cpgs Closing The GapDocument12 pagesJCI Whitepaper Cpgs Closing The GapMathilda UllyNo ratings yet
- Pakyz2014 PDFDocument7 pagesPakyz2014 PDFAMSP IPGMERNo ratings yet
- Introduction to Clinical Effectiveness and Audit in HealthcareFrom EverandIntroduction to Clinical Effectiveness and Audit in HealthcareNo ratings yet
- 1 s2.0 S2214623723000145 MainDocument6 pages1 s2.0 S2214623723000145 Mainfaroukrachid101No ratings yet
- Bright Et Al. - 2012 - Effect of Clinical Decision-Support Systems A Sys PDFDocument64 pagesBright Et Al. - 2012 - Effect of Clinical Decision-Support Systems A Sys PDFBen AllenNo ratings yet
- Novak2013 PDFDocument26 pagesNovak2013 PDFRifa YulitaNo ratings yet
- Stroke AFRDocument9 pagesStroke AFRPrasasti 19No ratings yet
- Monitoring Quality of Care: Observations vs Client InterviewsDocument8 pagesMonitoring Quality of Care: Observations vs Client InterviewsFarhati Umminya AfanNo ratings yet
- Puntis Et Al 2014 Associations Between Continuity of Care and Patient Outcomes in Mental Health Care A Systematic ReviewDocument10 pagesPuntis Et Al 2014 Associations Between Continuity of Care and Patient Outcomes in Mental Health Care A Systematic ReviewbraispmNo ratings yet
- C11 - Basics of Quality in HSDocument6 pagesC11 - Basics of Quality in HSCoordinacion aNo ratings yet
- Prevention Strategies To Reduce Future Impact of Low Back Pain: A Systematic Review and Meta-AnalysisDocument10 pagesPrevention Strategies To Reduce Future Impact of Low Back Pain: A Systematic Review and Meta-AnalysisShivangi SaxenaNo ratings yet
- Fphar 11 572569Document12 pagesFphar 11 572569hainguyen.htalabNo ratings yet
- Novack Etal2013Document43 pagesNovack Etal2013eebook123456No ratings yet
- Implementing An Antibiotic Stewardship Program Guidelines by The Infectious Diseases Society of America and The Society For Healthcare Epidemiology of AmericaDocument27 pagesImplementing An Antibiotic Stewardship Program Guidelines by The Infectious Diseases Society of America and The Society For Healthcare Epidemiology of AmericaEnrique AlonsoNo ratings yet
- Periop Outcomes in PedsDocument9 pagesPeriop Outcomes in Pedsrtaneja92No ratings yet
- Nihms 725929Document11 pagesNihms 725929Mario SerranoNo ratings yet
- 1 s2.0 S0168851020303171 MainDocument12 pages1 s2.0 S0168851020303171 MaindestiaNo ratings yet
- An Overview of Reviews On Interprofessional Collaboration in Primary Care: Barriers and FacilitatorsDocument15 pagesAn Overview of Reviews On Interprofessional Collaboration in Primary Care: Barriers and FacilitatorsGendi CynthiaNo ratings yet
- Mzi040 PDFDocument6 pagesMzi040 PDFselamat parminNo ratings yet
- Mzi040 PDFDocument6 pagesMzi040 PDFselamat parminNo ratings yet
- Development and Validation of PACICDocument9 pagesDevelopment and Validation of PACICKristen LynchNo ratings yet
- cg7 12913 2015 Article 795Document6 pagescg7 12913 2015 Article 795Mihalache Dan StefanNo ratings yet
- Anderson (2018) UK Review of Universal Screening - a-systematic-review-of-effectiveness-and-cost-effectiveness-of-school-based-identification-of-children-and-young-people-at-risk-of-or-currently-experiencingDocument11 pagesAnderson (2018) UK Review of Universal Screening - a-systematic-review-of-effectiveness-and-cost-effectiveness-of-school-based-identification-of-children-and-young-people-at-risk-of-or-currently-experiencingAlex YuenNo ratings yet
- Morello 2012Document9 pagesMorello 2012Anonymous Rv3ahYRNo ratings yet
- DMCN 13653Document17 pagesDMCN 13653Dwi ApriyantiNo ratings yet
- Delerium CEA Systematic ReviewDocument30 pagesDelerium CEA Systematic ReviewK. O.No ratings yet
- SolapsoDocument25 pagesSolapsoAnalía CimolaiNo ratings yet
- Tawfik Et Al., 2019Document14 pagesTawfik Et Al., 2019Ana Isabel Benedicto OrtizNo ratings yet
- Academic Emergency Medicine - 2020 - Ebell - Accuracy of Signs and Symptoms For The Diagnosis of Community AcquiredDocument14 pagesAcademic Emergency Medicine - 2020 - Ebell - Accuracy of Signs and Symptoms For The Diagnosis of Community AcquiredOnilis RiveraNo ratings yet
- Effectiveness of Exercise App With Self-E Cacy To Achieve Recommended Levels of Physical Activity Among Adult: A Systematic ReviewDocument9 pagesEffectiveness of Exercise App With Self-E Cacy To Achieve Recommended Levels of Physical Activity Among Adult: A Systematic ReviewI Kade WijayaNo ratings yet
- Clinical Practice Guidelines On Prostate Cancer: A Critical AppraisalDocument6 pagesClinical Practice Guidelines On Prostate Cancer: A Critical AppraisalJufrialdy AldyNo ratings yet
- Developing Reliable ProcessesDocument5 pagesDeveloping Reliable ProcessesBili RubinNo ratings yet
- Ministry of Finance Department of ExpenditureDocument3 pagesMinistry of Finance Department of ExpenditureBili RubinNo ratings yet
- COVID 19 Exposes A Critical Shortage of Oxygen in Developing Countries PDFDocument5 pagesCOVID 19 Exposes A Critical Shortage of Oxygen in Developing Countries PDFBili RubinNo ratings yet
- Building Improvement Capacity CapabilityDocument3 pagesBuilding Improvement Capacity CapabilityBili RubinNo ratings yet
- User Guide To Vac RegDocument4 pagesUser Guide To Vac RegBili RubinNo ratings yet
- Margcost of Lowgluc 2Document1 pageMargcost of Lowgluc 2Bili RubinNo ratings yet
- Margcost of LowglucosDocument1 pageMargcost of LowglucosBili RubinNo ratings yet
- India Nfhs 2015 Fact SheetDocument8 pagesIndia Nfhs 2015 Fact SheetKiran KumbharNo ratings yet
- What Mideco Should DoDocument1 pageWhat Mideco Should DoBili RubinNo ratings yet
- 5x5 Matrix PDFDocument2 pages5x5 Matrix PDFBili RubinNo ratings yet
- Norm Dist CurDocument2 pagesNorm Dist CurBili RubinNo ratings yet
- APMed Coll List 2018Document3 pagesAPMed Coll List 2018Bili RubinNo ratings yet
- India Nfhs 2015 Fact SheetDocument8 pagesIndia Nfhs 2015 Fact SheetKiran KumbharNo ratings yet
- Quality BookDocument1 pageQuality BookBili RubinNo ratings yet
- A Journal ArticleDocument11 pagesA Journal ArticleBili RubinNo ratings yet
- Vital Statistics Report Analyzes Birth & Death Rates Across IndiaDocument6 pagesVital Statistics Report Analyzes Birth & Death Rates Across IndiaBili RubinNo ratings yet
- 5 X 5 Rmnch+aDocument2 pages5 X 5 Rmnch+aManish Chandra Prabhakar0% (1)
- 5 Books To Help You Build Better HabitsDocument5 pages5 Books To Help You Build Better HabitsBili RubinNo ratings yet
- Week 05 Simulation Using GPSS (1) NEWDocument59 pagesWeek 05 Simulation Using GPSS (1) NEWPutriska RazaniNo ratings yet
- GSV EDU Factbook Apr 13 2012Document127 pagesGSV EDU Factbook Apr 13 2012Innovative Educational Services, CCIUNo ratings yet
- Chapter 3 - Excel SolutionsDocument8 pagesChapter 3 - Excel SolutionsHalt DougNo ratings yet
- Highh Mast LightingDocument6 pagesHighh Mast LightingAsghar KhanNo ratings yet
- Study Guide Rev08242018Document188 pagesStudy Guide Rev08242018chong pak limNo ratings yet
- Motion in A Straight Line: Initial PositionDocument7 pagesMotion in A Straight Line: Initial PositionEngelbert Bicoy AntodNo ratings yet
- Threats: What Trends Could Harm You? What Threats Do Your Weaknesses Expose You To?Document3 pagesThreats: What Trends Could Harm You? What Threats Do Your Weaknesses Expose You To?Rufino Gerard MorenoNo ratings yet
- Media Palnning ProcessDocument3 pagesMedia Palnning ProcessSrinivas KumarNo ratings yet
- PLC Ladder Examples 2021Document18 pagesPLC Ladder Examples 2021JosephNo ratings yet
- Mapua IT LED Display "Boot SequenceDocument10 pagesMapua IT LED Display "Boot SequenceKristine ToledoNo ratings yet
- Q Asgt - Biz Law - A192Document10 pagesQ Asgt - Biz Law - A192otaku himeNo ratings yet
- The Ultimate Press Release Swipe File by Pete Williams - SAMPLEDocument20 pagesThe Ultimate Press Release Swipe File by Pete Williams - SAMPLEPete Williams100% (9)
- 2.4 Static Pressure Spreadsheet 1Document4 pages2.4 Static Pressure Spreadsheet 1Swapnil Pratap SinghNo ratings yet
- DL 57 PDFDocument2 pagesDL 57 PDFmaheshm_erpNo ratings yet
- CS 702 Lec10Document9 pagesCS 702 Lec10Muhammad TausifNo ratings yet
- Lay Up ProcedureDocument21 pagesLay Up ProcedureAmir100% (1)
- Databases 2 Exercise Sheet 4Document2 pagesDatabases 2 Exercise Sheet 4Shivam ShuklaNo ratings yet
- Class 11 Accountancy Part 2Document288 pagesClass 11 Accountancy Part 2Pyngs Ronra ShimrayNo ratings yet
- 9 Principles of Income Tax LawsDocument82 pages9 Principles of Income Tax LawsVyankatesh GotalkarNo ratings yet
- Sas Clinical Data Integration Fact SheetDocument4 pagesSas Clinical Data Integration Fact SheetChandrasekhar KothamasuNo ratings yet
- Oracle Forms Developer 10G Student Guide - 1Document440 pagesOracle Forms Developer 10G Student Guide - 1Jayant Agarwal100% (3)
- Intelligent Platform Management Bus Communications Protocol Specification v1.0Document43 pagesIntelligent Platform Management Bus Communications Protocol Specification v1.0alexchuahNo ratings yet
- SANS10162-4 Design of Cold Formed Stainless SteelDocument83 pagesSANS10162-4 Design of Cold Formed Stainless SteelhenvaswegeNo ratings yet
- Chapter 4 Duality and Post Optimal AnalysisDocument37 pagesChapter 4 Duality and Post Optimal AnalysisMir Md Mofachel HossainNo ratings yet
- SpirentAutomotiveLV124 LV148VDocument38 pagesSpirentAutomotiveLV124 LV148VNiculcea Cristin100% (3)
- 10 - A TFT-LCD Source-Driver IC With Charge-Recycling TechniqueDocument11 pages10 - A TFT-LCD Source-Driver IC With Charge-Recycling Techniquematwan29No ratings yet
- Information Requirements For Welding of Pressure Containing Equipment and PipingDocument20 pagesInformation Requirements For Welding of Pressure Containing Equipment and PipingPramod Athiyarathu100% (1)
- PharmacophoreDocument7 pagesPharmacophoresatheeshpharma6No ratings yet
- Superior Drummer 2 ManualDocument38 pagesSuperior Drummer 2 ManualEmmanuel MarcosNo ratings yet
- Soy Candle ModuleDocument17 pagesSoy Candle ModuleCla Rence0% (2)