Professional Documents
Culture Documents
Fluids Electrolytes and Acid Base Balance
Uploaded by
Crazy StrangerOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fluids Electrolytes and Acid Base Balance
Uploaded by
Crazy StrangerCopyright:
Available Formats
FLUIDS – ELECTROLYTES AND ACID- - Promotes cellular chemical
BASE BALANCE function
- Maintains normal body
BODY FLUID COMPARTMENTS temperature
- Eliminates waste products
Intracellular fluid compartment
from the cells
(ICF)
- Fluid found inside the cells FUNCTIONS OF ELECTROLYTES
- It comprises 2/3 (70%) of the
body fluid Promote neuromuscular irritability
Extracellular fluid compartment Maintain body fluid volume and
(ECF) osmolality
- Fluid found outside the cells. Distribute body water between fluid
- It comprises 1/3 (30%) of the compartments
body fluid Regulate acid-base balance
- May be interstitial fluid (in-
NORMAL VALUES
between the cells)
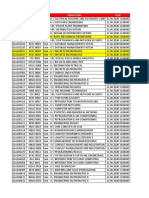
Intravascular fluid ELECTROLYTES NORMAL VALUES
(plasma) SODIUM (Na) 135 – 145 mEg/L
Transcellular fluid POTASSIUM (K) 3.5 – 5 mEg/L
(digestive juices, CALCIUM (Ca) 4.5 – 5.5 mEg/L
pleural fluid, water in PHOSPHATE 1.7 – 2.6 mEg/L
the renal tubules & (HPO4)
CSF CHLORIDE (Cl) 98 – 108 mEg/L
MAGNESIUM (Mg) 1.5 – 2.5 mEg/L
FACTORS OF BODY WATER
DISTRIBUTION
INTERNAL REGULATION OF BODY
In infants, 80% of the body weight is WATER AND ELECTROLYTES
water.
Sodium and water regulation
In males, 60% of the body weight is
Thirst – major control of
water. Males are more muscular
actual fluid intake
than females.
Kidneys – major organs
In females, 50% of the body weight
controlling output
is water. Females have more
ADH – retains water in the
adipose tissue than males.
renal tubules
FUNCTIONS OF WATER RAAS – aldosterone retain
sodium and water (sodium
Extracellular fluid primarily determines
- Maintains blood volume osmolality (concentration) of
- Transports gases, nutrients the body fluids)
and other substances to the
cells RAAS (RENIN – ANGIOTENSIN –
Intracellular fluid ALDOSTERONE SYSTEM)
Potassium Regulation Calcium Regulation
Aldosterone and hydrogen Parathormone,
ions regulate potassium thyrocalcitonin and Vitamin D
levels regulate calcium levels
Aldosterone retains sodium Vitamin D promotes calcium
and excretes potassium absorption from GIT
Alkalosis increases k Calcium promotes
excretion neuromuscular irritability;
(hypokalemia) bone and teeth development
Acidosis decreases k and blood clotting
excretion Parathormone elevates s.
(hyperkalemia) Ca levels by withdrawing
K is the major cation in the calcium from bones (bone
ICF resorption)
K is necessary in the Thyrocalcitonin lowers s.
conduction of nerve impulses Ca levels by depositing Ca in
and promotion of skeletal the bones (bone absorption)
and cardiac muscle activity Calcium and phosphorus
have inverse relationship
HYRDROGEN IN CONENTRATION
MOVEMENTS OF FLUIDS
PASSIVE TRANSPORT
Diffusion – transport of solutes from
area of higher concentration to lower
concentration across semi-
permeable membrane
Osmosis – transport of solvent from
area of lower concentration to higher
concentration across semi- - Examples: D10W, D50W,
permeable membrane D5LR, D5NM
ACTIVE TRANSPORT
Hydrostatic pressure – caused by
the blood pressing against walls of
blood vessels (pushing force)
Colloid Osmotic pressure (oncotic
pressure) – pressure needed to
overcome the pull of CHON. Pull or
absorb fluid from the interstitial
space
TYPES OF SOLUTION
POTASSIUM INSIDE, SODIUM
OUTSIDE
ELECTROLYTE IMBALANCES:
SODIUM IMBALANCES
Hyponatremia (sodium deficit)
- Caused by sodium loss or
water excess
Causes:
Diuretics
Low Na diet
Decreased aldosterone
secretions
TYPES OF INTRAVENOUS FLUIDS Edema
Ascites
ISOTONIC SOLUTION
Burns
- Has the same concentration
Diaphoresis
as the body fluids
- Examples: D5W, NaCl 0.9%
Hypernatremia (Sodium excess,
& Plain ringer’s lactate
edema)
- Sodium and water excess
HYPOTONIC SOLUTION
result to edema
- Has lower concentration than
Causes:
the body fluids
Hyperventilation and diarrhea
- Example: NaCl 0.3%
High sodium intake
Sodium tablets
HYPERTONIC SOLUTION
Water deprivation
- Has HIGHER concentration
than the body fluids
increased neuromuscular
irritability
- Everything is high and fast
Causes:
Decreased ionized calcium
Excess loss of calcium
Inadequate dietary intake of
calcium-rich food
Decreased calcium
absorption
Hypercalcemia
- Decreased cell membrane
permeability which
POTASSIUM IMBALANCES decreases neuromuscular
Hypokalemia (Potassium Deficit) irritability
- Everything is low and slow
- Characterized by decreased
Causes:
neuromuscular irritability
Calcium loss from bones
- Everything is low and slow
Excessive intake of calcium
Causes:
Hyperparathyroidism
Decreased food and fluid
Hypervitaminosis D
intake (starvation)
Steriod therapy
Increased loss of potassium
Shifting of K into the cells MAGNESIUM IMBALANCE
Hyperkalemia (potassium excess) Hypomagnesemia
- Characterized by increased - Magnesium inhibits
neuromuscular irritability acetylcholine release
- Everything is high and fast - In hypomagnesemia, there is
Causes: increased acetylcholine
Excess dietary intake of release which results to
potassium-rich food increased neuromuscular
Excess parenteral irritability
administration of potassium - Everything is high and fast
Decreased excretion of Causes:
potassium Prolonged malnutrition or
Shifting of potassium out of starvation
cells Malabsorption syndromes
Hypercalcemia
CALCIUM IMBALANCES Alcohol withdrawal
syndromes
Hypocalcemia
Draining fistulas
- Increased cell membrane
permeability which results to
Hypermagnesemia
-There is decreased
acetylcholine release which
result to decreased
neuromuscular irritability
- Everything is low and slow
Causes:
Excessive intake of
magnesium-containing
antacids
Renal failure
Diabetic ketoacidosis
If pH is 7 and below or 7.8 and
above, death occurs.
If pH and pCO2 are primarily
affected, respiratory acid-base
imbalances will result
If pH and HCO3 are primarily
affected, metabolic acid – base
imbalances will be experienced.
RESPIRATORY ACIDOSIS (Carbonic
Acid Excess)
Caused by failure of the respiratory
system to remove carbon dioxide
ACID-BASE IMBALANCES from the body fluid as it is produced
in the tissues
Arterial Blood Gas Analysis (ABG) Disorders that lead to
hypoventilation result to retention of
carbon dioxide
Respiratory Alkalosis (Carbonic Acid
Deficit)
Caused by loss of carbon dioxide
from the lungs at a faster rate that it
is produced in the tissues
Disorders that lead to
hyperventilation result to excess loss
of carbon dioxide.
METABOLIC ACIDOSIS (Bicarbonate ARTERIAL BLOOD GAS ANALYSIS
Deficit)
Commonly ordered on the client with
Results from abnormal of fixed acids COPD, pulmonary edema, ARD, MI
or loss of base or PNA.
Assessment: Also used for non-emergencies such
Headache as weaning from ventilator
Mental dullness helpful in the assessment of children
Kussmaul’s breathing who are acutely ill with either
hyperkalemia pulmonary or non pulmonary
disorders who require an artificial
METABOLIC ALKALOSIS (Bicarbonate airway
Excess)
ALLEN’S TEST
Results from loss of hydrogen ions
or addition of base to body fluids. To assess adequacy of blood supply
Assessment to the client’s non-dominant hand.
Hypoventilation STEPS:
Mental confusion 1. Have client open and close
Dizziness fist a few times.
Numbness and tingling of 2. While fist is clenched,
fingers and toes, muscle simultaneously occlude both
twitching radial and ulnar arteries.
Tetany and seizures 3. While arteries are occluded,
ask client to slowly unclench
fist and relax hand. (the palm
should be pale from lack of
arterial blood flow)
4. Then, release the pressure
over the ulnar artery. The
palm should turn pink within
7 to 15 seconds (+ Allen’s
test), indicating that arterial
circulation has resumed. If
that does not happen, you
will need to select another
site.
ACCESSIBLE VESSELS FOR ARTERIAL
PUNCTURE
Radial artery – superficial, easily
compressible and with good
collaterals with ulnar artery. Ideal
vessel for arterial puncture.
Brachial artery
Femoral artery
Temporal artery
Dorsalis pedis artery
You might also like
- NCM 112 - Fluid and Electrolytes (Unit 1)Document2 pagesNCM 112 - Fluid and Electrolytes (Unit 1)Pauline Mae RobertoNo ratings yet
- PHARMACOLOGYDocument19 pagesPHARMACOLOGYKiela Therese LabroNo ratings yet
- Reviewer Chapter 52 FluidsDocument8 pagesReviewer Chapter 52 FluidsKeren GaciasNo ratings yet
- Fluid & ElectrolytesDocument75 pagesFluid & ElectrolytesfaridahuNo ratings yet
- Fluid and ElectrolytesDocument11 pagesFluid and ElectrolytesangelaclaireramosNo ratings yet
- NCM112 MS 1 Week 1Document11 pagesNCM112 MS 1 Week 1Lerry Claire LimosNo ratings yet
- Fluids Electrolytes - Acid-Base BalanceDocument11 pagesFluids Electrolytes - Acid-Base BalanceJhosita Flora Laroco100% (1)
- Fluid and Electrolytes - MTDocument14 pagesFluid and Electrolytes - MTAlliah Polvorido AnaudNo ratings yet
- Fluids and Electrolytes ReviewerDocument4 pagesFluids and Electrolytes ReviewerdverraNo ratings yet
- Fluids and Electrolytes-2Document82 pagesFluids and Electrolytes-2Jem Loterte100% (1)
- Fluids & Electrolytes: Thirst Reflex Triggered byDocument7 pagesFluids & Electrolytes: Thirst Reflex Triggered byGummie Akalal SugalaNo ratings yet
- BODY Weight 100%: Balance/Imbalances & TherapyDocument11 pagesBODY Weight 100%: Balance/Imbalances & TherapyVictoria Castillo TamayoNo ratings yet
- Fluids and Electrolytes A5Document4 pagesFluids and Electrolytes A5FrancheskaNo ratings yet
- Chapter 27: Fluid and Electrolyte BalanceDocument26 pagesChapter 27: Fluid and Electrolyte BalanceMarwan M.No ratings yet
- Fluids & Electrolytes: A. 2 Body CompartmentsDocument5 pagesFluids & Electrolytes: A. 2 Body CompartmentsJULIUS ART VINCENT A. PADINITNo ratings yet
- Fe ConceptDocument177 pagesFe ConceptIvan MaximusNo ratings yet
- Fluid and ElectrolytesDocument13 pagesFluid and ElectrolytesHenry Philip93% (15)
- Fluid & Electrolyte Balance: Part 4: Regulation & MaintenanceDocument40 pagesFluid & Electrolyte Balance: Part 4: Regulation & MaintenanceMy MusicNo ratings yet
- Fluids and ElectrolytesBlood TransfusionDocument6 pagesFluids and ElectrolytesBlood TransfusionMaria Erica Jan MirandaNo ratings yet
- MS - Fluids and ElectrolytesDocument6 pagesMS - Fluids and ElectrolytesJOHN LOYD CASTILLONo ratings yet
- 3.14 Chapter 3 Water and Electrolytes Balance and ImblanceDocument140 pages3.14 Chapter 3 Water and Electrolytes Balance and ImblanceShourav SarkarNo ratings yet
- AC. Nutrition - Water and ElectrolytesDocument81 pagesAC. Nutrition - Water and ElectrolytesAnuchithra Radhakrishnan100% (1)
- CH 39 Acid-Base ElectrolyteDocument16 pagesCH 39 Acid-Base ElectrolyteJonathan EdieNo ratings yet
- Fluids: ElectrolytesDocument56 pagesFluids: ElectrolytesZee Zang100% (1)
- Fluid and ElectrolytesDocument105 pagesFluid and ElectrolytesCarl Elexer Cuyugan Ano100% (3)
- Ecf and Icf PDFDocument55 pagesEcf and Icf PDFChidera EmmanuelNo ratings yet
- Fluids and Electrolytes A5Document70 pagesFluids and Electrolytes A5FrancheskaNo ratings yet
- Body Fluid CompartmentsDocument37 pagesBody Fluid Compartmentsmanu sethiNo ratings yet
- Intranscellular Fluid Interstitial Fluid Transcellular FluidDocument19 pagesIntranscellular Fluid Interstitial Fluid Transcellular FluidCharish Dwayne Bautista PondalesNo ratings yet
- Fe Finals NotesDocument23 pagesFe Finals NoteshanhananicasNo ratings yet
- CCHM 312: Week 4 & 5: Water Balance and ElectrolytesDocument7 pagesCCHM 312: Week 4 & 5: Water Balance and ElectrolytesJanine Alicia VargasNo ratings yet
- Fluid and ElectrolytesDocument21 pagesFluid and ElectrolytesMeryl RamosNo ratings yet
- Fe OverviewDocument5 pagesFe OverviewAngel YuNo ratings yet
- Felixcharlie Electrolyte Homeostasis Part 1Document2 pagesFelixcharlie Electrolyte Homeostasis Part 1Nur Fatima SanaaniNo ratings yet
- Basic of Fluid Therapy ImaDocument69 pagesBasic of Fluid Therapy Imal Made ArtawanNo ratings yet
- Fluids and ElectrolytesDocument71 pagesFluids and ElectrolytesHarold Castillo OrigenesNo ratings yet
- 312 MidDocument60 pages312 MidVALERIANO TRISHANo ratings yet
- Medsurg Lec FeDocument10 pagesMedsurg Lec FeChelsea Faith SarandiNo ratings yet
- Fluids and Electrolytes Intro NotesDocument3 pagesFluids and Electrolytes Intro NotesTricia Joy EspinosaNo ratings yet
- Waterandelectrolyte 170425132238Document50 pagesWaterandelectrolyte 170425132238Sahil SrivastavaNo ratings yet
- Fluid & Electrolyte ImbalancesDocument212 pagesFluid & Electrolyte ImbalancesLane Mae Magpatoc NoerrotNo ratings yet
- 1021 Lecture Question Bank PDFDocument44 pages1021 Lecture Question Bank PDFaskldhfdasjkNo ratings yet
- Mabes Fluid and ElectrolytesDocument9 pagesMabes Fluid and ElectrolytesMabesNo ratings yet
- F and e Imb .... Edu ..Document20 pagesF and e Imb .... Edu ..esakkiammalNo ratings yet
- Electrolytes IDocument4 pagesElectrolytes IRed AnthonyNo ratings yet
- Cairan Biologi: I Gaa. SuartiniDocument52 pagesCairan Biologi: I Gaa. SuartiniAlif Ilham100% (1)
- 3 Fluids and Electrolytes PPDocument112 pages3 Fluids and Electrolytes PPjcodoyNo ratings yet
- Potter & Perry: Fundamentals of Nursing, 7 EditionDocument11 pagesPotter & Perry: Fundamentals of Nursing, 7 Editionmissy23pap100% (1)
- Fluid and Electrolytes BalanceDocument29 pagesFluid and Electrolytes BalanceHachi Nini Shop IINo ratings yet
- Fluid J Electrolyte J and Acid-Base BalanceDocument11 pagesFluid J Electrolyte J and Acid-Base Balancejeraldine marceraNo ratings yet
- Water ElectrolytesDocument2 pagesWater ElectrolytesLyzajoyce SeriozaNo ratings yet
- Fluid, Electrolyte, and Acid-Base BalanceDocument41 pagesFluid, Electrolyte, and Acid-Base BalanceRn nadeenNo ratings yet
- Fe 1Document36 pagesFe 1api-3697326No ratings yet
- Fluid and Electrolyte Imbalance PDFDocument21 pagesFluid and Electrolyte Imbalance PDFShafaq AlamNo ratings yet
- Major ElectrolytesDocument4 pagesMajor Electrolytes6k8rtwgpksNo ratings yet
- Body FluidsDocument46 pagesBody FluidsSidharth BhardwajNo ratings yet
- F&E For Elderly - ModuleDocument163 pagesF&E For Elderly - ModuleArihk NiladaNo ratings yet
- Chapter 17 Fluid Electrolytes and Acid-BDocument23 pagesChapter 17 Fluid Electrolytes and Acid-BKayan L.No ratings yet
- Fluid and Electrolytes Session 1-8Document17 pagesFluid and Electrolytes Session 1-8Angie100% (1)
- Fecal EliminationDocument13 pagesFecal EliminationCrazy StrangerNo ratings yet
- PLANNINGDocument3 pagesPLANNINGCrazy StrangerNo ratings yet
- ASSESSINGDocument3 pagesASSESSINGCrazy StrangerNo ratings yet
- Lydia HallDocument1 pageLydia HallCrazy StrangerNo ratings yet
- Margaret Newman and Rosemarie Rizzo-ParseDocument2 pagesMargaret Newman and Rosemarie Rizzo-ParseCrazy StrangerNo ratings yet
- Imogen KingDocument1 pageImogen KingCrazy StrangerNo ratings yet
- Dorothy JohnsonDocument2 pagesDorothy JohnsonCrazy StrangerNo ratings yet
- 1753-Article Text-39640-3-10-20220815Document9 pages1753-Article Text-39640-3-10-20220815Inah SaritaNo ratings yet
- Detailed Lesson Plan in Science IiiDocument3 pagesDetailed Lesson Plan in Science Iiicharito riveraNo ratings yet
- The Coffee Shop Easy Reading - 152542Document1 pageThe Coffee Shop Easy Reading - 152542Fc MakmurNo ratings yet
- Jetline: Theoretical Working Point Performance ChartDocument1 pageJetline: Theoretical Working Point Performance ChartMohamed GamalNo ratings yet
- API 571 Quick ReviewDocument32 pagesAPI 571 Quick ReviewMahmoud Hagag100% (1)
- 2006 - Dong Et Al - Bulk and Dispersed Aqueous Phase Behavior of PhytantriolDocument7 pages2006 - Dong Et Al - Bulk and Dispersed Aqueous Phase Behavior of PhytantriolHe ZeeNo ratings yet
- MIKE21BW Step by Step GuideDocument124 pagesMIKE21BW Step by Step Guideflpbravo100% (2)
- Fill in The Table by Determining The Functions of The Following ItemsDocument6 pagesFill in The Table by Determining The Functions of The Following ItemsJessabel CandidatoNo ratings yet
- Staff Code Subject Code Subject Data FromDocument36 pagesStaff Code Subject Code Subject Data FromPooja PathakNo ratings yet
- Samsung Bd-p4600 SMDocument101 pagesSamsung Bd-p4600 SMIonel CociasNo ratings yet
- Block-1 BLIS-03 Unit-2 PDFDocument15 pagesBlock-1 BLIS-03 Unit-2 PDFravinderreddynNo ratings yet
- 020 Basketball CourtDocument4 pages020 Basketball CourtMohamad TaufiqNo ratings yet
- Consent For Diagnostic And/or Therapeutic ParacentesisDocument2 pagesConsent For Diagnostic And/or Therapeutic ParacentesisnaveenNo ratings yet
- Stahl - PUDSDocument29 pagesStahl - PUDSsusanasusana_No ratings yet
- EV Connect What Is EVSE White PaperDocument13 pagesEV Connect What Is EVSE White PaperEV ConnectNo ratings yet
- Module III Rural MarketingDocument30 pagesModule III Rural MarketingNikita YadavNo ratings yet
- Handbook (P)Document224 pagesHandbook (P)Joe80% (5)
- 9 Daftar Pustaka VaricelaDocument2 pages9 Daftar Pustaka VaricelaAfrina FaziraNo ratings yet
- EI6704: UNIT 5 NotesDocument19 pagesEI6704: UNIT 5 NotesMadhu MithaNo ratings yet
- Q3 Module 15Document33 pagesQ3 Module 15jovielyn kathley manaloNo ratings yet
- Chapter 4: Palm Oil and Oleochemical Industries.: Presented By: Lovelyna Eva Nur Aniqah Siti MaryamDocument15 pagesChapter 4: Palm Oil and Oleochemical Industries.: Presented By: Lovelyna Eva Nur Aniqah Siti MaryamdaabgchiNo ratings yet
- Itinerary - State 2010Document3 pagesItinerary - State 2010purest123No ratings yet
- Materi B.inggris SMP Kelas 9 Kurikulum 2013Document21 pagesMateri B.inggris SMP Kelas 9 Kurikulum 2013Siti DianurNo ratings yet
- Schrodinger Wave EquationsDocument6 pagesSchrodinger Wave EquationsksksvtNo ratings yet
- Geology and Mineralization of The Maggie Creek DistrictDocument28 pagesGeology and Mineralization of The Maggie Creek DistrictRockstone Research Ltd.No ratings yet
- Jerms B 2109 - 0BDocument10 pagesJerms B 2109 - 0BNothing is ImpossibleNo ratings yet
- Idlers: TRF Limited TRF LimitedDocument10 pagesIdlers: TRF Limited TRF LimitedAjit SarukNo ratings yet
- RA - Ducting WorksDocument6 pagesRA - Ducting WorksResearcherNo ratings yet
- Acoustic Phonetics PDFDocument82 pagesAcoustic Phonetics PDFAnonymous mOSDA2100% (2)
- Mohd Mopti Bin Yassin V Lembaga Kemajuan Perusahaan Pertanian Negeri Pahang (LKPP) Corp SDN BHD & AnorDocument12 pagesMohd Mopti Bin Yassin V Lembaga Kemajuan Perusahaan Pertanian Negeri Pahang (LKPP) Corp SDN BHD & AnorA random humanNo ratings yet