Professional Documents
Culture Documents
Infecciones Por Arbovirus - Continuum
Uploaded by
Neurología RebagliatiCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Infecciones Por Arbovirus - Continuum
Uploaded by
Neurología RebagliatiCopyright:
Available Formats
Review Article
Arbovirus Infections
Address correspondence to
Dr J. David Beckham, University
of Colorado School of Medicine,
Departments of Medicine and
J. David Beckham, MD; Kenneth L. Tyler, MD, FAAN Neurology, 12700 East 19th Ave,
B168, Aurora, CO 80045,
David.beckham@ucdenver.edu.
Relationship Disclosure:
ABSTRACT Dr Beckham receives research
funding from the National
Purpose of Review: Arbovirus (arthropod-borne virus) infections are increasingly Institute of Allergy and
important causes of neurologic disease in the United States through both endemic Infectious Diseases and the
transmission and travel-associated infections. This article reviews the major arbovirus University of Colorado
Neurosciences Institute. Dr Tyler
infections that can cause neurologic disease likely to be encountered in the United States. has served on the scientific
Recent Findings: West Nile virus continues to be an important cause of epidemic advisory boards of Biogen;
encephalitis, while emerging arbovirus infections such as dengue and chikungunya have Genentech, Inc; F. Hoffman-La
Roche Ltd; and Janssen
rapidly expanded their geographic distribution. As emerging arboviruses expand in new Pharmaceuticals, Inc; on the
geographic regions, neurologic abnormalities are reported in new patient populations. data and safety monitoring
Summary: Emerging arbovirus infections are increasingly important causes of neurologic board of Lpath Incorporated;
and as a member of the
disease throughout the world and in the United States. While no US Food and Drug Progressive Multifocal
Administration (FDA)Yapproved therapy is yet available for these infections, prompt Leukoencephalopathy
recognition and diagnosis from the consulting neurologist will ensure appropriate Consortium. Dr Tyler has
served as associate editor of the
supportive care for the patient. Journal of NeuroVirology and
Neurology Today and on the
Continuum (Minneap Minn) 2015;21(6):1599–1611. editorial boards of Annals of
Neurology, Apoptosis,
Experimental Neurology, JAMA
Neurology, The Journal of
Infectious Diseases, Microbial
INTRODUCTION FLAVIVIRIDAE Pathogenesis, and Virology.
With the spread of West Nile virus across West Nile Virus Dr Tyler has received research
support from the National
the United States, the evaluation of an Most arboviruses maintain an enzootic Multiple Sclerosis Society, the
National Institute of Allergy
acute febrile patient with neurologic ab- (animal) cycle that does not involve hu- and Infectious Diseases, the
normalities commonly includes arbo- man infection. West Nile virus is main- National Institute of Neurological
tained in an enzootic cycle between Disorders and Stroke, and the
virus infections in the differential. The US Department of Veterans
term arbovirus (arthropod-borne virus) mosquitos such as Culex pipiens and Affairs Merit Program and
includes several families of viruses that passerine (perching) bird species such receives royalties from Elsevier
B.V. and McGraw-Hill Education.
are spread by arthropod vectors, most as jays and finches. After an infected Unlabeled Use of
commonly mosquitoes, ticks, and sand mosquito bites a human, the virus rep- Products/Investigational
Use Disclosure:
flies.1 The families of viruses included licates in dendritic cells and macrophages Drs Beckham and Tyler discuss
in the arbovirus group are Flaviviridae, in local tissue and lymph nodes, result- the unlabeled/investigational
use of corticosteroids,
Togaviridae, Bunyaviridae, and Reoviridae ing in viremia that eventually dissem- humanized monoclonal
(Table 3-1). These large families of vi- inates virus to end organs, including antibodies, interferon alfa, and
IVIg for the treatment of West
ruses have a common feature, an RNA the central nervous system (CNS).2 Of Nile virus.
genome that allows these viruses to rap- note, West Nile viremia in humans is * 2015, American Academy
idly adapt to ever-changing host and not high enough or sustained enough of Neurology.
environmental conditions. Thus, these to support subsequent transmission to
virus families are largely responsible for mosquitoes, so humans are dead-end
the recent growth in geographic range hosts. The ability of an arbovirus to
of emerging viruses such as West Nile invade the CNS (neuroinvasiveness) is
virus, dengue virus, and chikungunya determined by multiple viral and host
virus. This article reviews the epide- factors.3,4 Proposed routes of arboviral
miology, presentation, and diagnosis of CNS entry include penetration of the
arbovirus infections and therapeutic ap- cerebral microvasculature after infec-
proaches to treat them. tion of endothelial cells, diapedesis
Continuum (Minneap Minn) 2015;21(6):1599–1611 www.ContinuumJournal.com 1599
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Arbovirus Infections
TABLE 3-1 Epidemiologic and Clinical Characteristics of Arboviruses
Geographic Clinical At-Risk
Family/Virus Vector Distribution Presentation Populations Diagnosis
Flaviviridae/West Mosquito: Continental Fever, myalgia, Elderly and Serology and
Nile virus Culex pipiens United States, meningismus, immunocompromised, CSF IgM, PCR of
southern Europe altered mental seasonal exposure nucleic acid in
status immunocompromised
Flaviviridae/dengue Mosquito: Worldwide in Fever, myalgia, Children and travelers Clinical presentation,
virus Aedes aegypti tropics and arthralgia acute and convalescent
subtropics serology
Flaviviridae/St Louis Mosquito: Southeastern Fever, myalgia, Elderly, seasonal Serology and CSF IgM
encephalitis virus C. pipiens United States meningismus, exposure
altered mental
status
Flaviviridae/ Tick: Ixodes Northern central Fever, headache, Outdoor exposure, Serum and CSF IgM
Powassan virus species and eastern vomiting, seasonal exposure antibody production
United States meningismus, to ticks
altered mental
status
Togaviridae/eastern Mosquito: Eastern seaboard Fever, Geographic exposure Acute and convalescent
equine encephalitis Culex and of United States, meningismus, during epidemic cycle serology, IgM-positive
virus Aedes species swamplands altered mental serum, CSF IgM
status, cranial
neuropathies
Togaviridae/ Mosquito: Central America Fever, headache, Geographic exposure Acute and convalescent
Venezuelan Aedes and and South America sore throat, during epidemic cycle serology, IgM-positive
equine encephalitis Culex species altered mental serum, CSF-positive
virus status IgM, PCR for viral
nucleic acid
Togaviridae/ Mosquito: Worldwide in Fever, headache, Geographic exposure Acute and convalescent
Chikungunya virus A. aegypti tropics and gastrointestinal serology, CSF IgM,
subtropics symptoms, PCR for viral nucleic
myalgia, arthralgia, acid in serum and CSF
arthritis
Bunyaviridae/La Mosquito: Midwestern Fever, headache, Children Acute and convalescent
Crosse virus Aedes species United States vomiting, altered serology, CSF IgM
mental status,
seizures
CSF = cerebrospinal fluid; IgM = immunoglobulin M; PCR = polymerase chain reaction.
(movement of infected blood cells across induced neuron cell death and CNS
brain capillary walls) of infected leu- injury.6Y11 Immune responses also con-
kocytes, passage through the choroid tribute to clearance of virus but contrib-
plexus, or passage through fenestrated ute to immune-mediated neuronal cell
endothelial cells in the vasculature of death as well.12Y17
specific regions in the CNS.2 West Nile virus infection is now the
After crossing the blood-brain barrier, most common cause of epidemic viral
many arboviruses can directly infect and encephalitis in the United States. Since
cause death of neurons.5 Several studies its emergence in New York City in 1999,
have shown that apoptosis is an im- over 40,000 cases of West Nile virus
portant mechanism of West Nile virusY infection have been reported in the
1600 www.ContinuumJournal.com December 2015
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINTS
United States, with over 17,000 cases clude chorioretinitis,28 myositis,29 and h Less than 1% of West
(42%) of neuroinvasive disease and 1700 autonomic nerve dysfunction.30 Nile virusYinfected
(4%) deaths.18 The epidemics of West Neuroinvasive disease most com- individuals develop
Nile virus in 2003 and 2012 were the monly occurs in older individuals (over neuroinvasive disease.
largest outbreaks of neuroinvasive viral 60 years of age). In one study, the odds h West Nile virus
infections ever reported in the Western ratio (95% confidence interval) of de- neuroinvasive disease
Hemisphere.19,20 veloping encephalitis was 2.2 (1.6 to can manifest as
Almost all cases of West Nile virus dis- 3.1) in individuals older than 64 years.31 meningitis, encephalitis,
ease are caused by transmission through Additional identified risk factors for acute flaccid paralysis,
a mosquito bite. In most areas of the encephalitis include hypertension and or a combination
diabetes mellitus.31,32 Patients who are of syndromes.
United States, the majority of cases oc-
immunocompromised, including organ h West Nile virus
cur between June and October, reflect-
transplant recipients, are at high risk of neuroinvasive disease
ing the peak activity period of biting
developing severe West Nile virus dis- is more common in
mosquitoes. Occasional cases of West ease. Specific genetic factors in humans individuals older than
Nile virus disease also occur follow- shown to enhance susceptibility to se- 60 years of age.
ing transplantation of West Nile virusY rious West Nile virus disease include h CSF from patients
infected organs,21 breast-feeding,22 and single nucleotide polymorphisms in the with West Nile virus
blood transfusions from asymptom- oligoadenylate synthetase gene, which neuroinvasive
atic West Nile virusYinfected individ- encodes an interferon-inducible en- disease may exhibit a
uals.23 Currently, donor organs and zyme involved in antiviral innate immu- neutrophil-predominant
blood products are screened for West nity,33 and a genetic deficiency of the pleocytosis.
Nile virus nucleic acids to prevent iat- chemokine receptor CCR5, which may
rogenic transmission. inhibit trafficking of West Nile virusY
Following transmission of West Nile specific CD8+ T cells into the CNS.34
virus, most infections (approximately West Nile virus meningitis is charac-
80%) are asymptomatic. Approximately terized by the abrupt onset of fever,
20% of infected individuals develop an headache, meningeal signs, photopho-
acute febrile flulike illness (West Nile bia, and phonophobia. Patients have
fever), characterized by fever, headache, a CSF pleocytosis with an average of
fatigue, anorexia, nausea, myalgia, and 226 cells/HL, mildly elevated protein,
lymphadenopathy. A maculopapular rash and normal glucose. In one study, neu-
involving the trunk and limbs occurs trophils, rather than lymphocytes, were
in 25% to 50% of cases.24 Less than 1% found to predominate in the CSF in
of West Nile virusYinfected individuals approximately 50% of patients with
develop neuroinvasive disease, which West Nile virus meningitis.35 In some
can manifest as meningitis, encephalitis, cases of West Nile virus neuroinvasive
acute flaccid paralysis, or a combination disease, very atypical-appearing mono-
of these clinical syndromes.19,25 The symp- cytes are noted in the CSF similar to
tomatology reflects the common pre- Mollaret cells noted in cases of recur-
dilection for the virus to injure the basal rent meningitis. In cases of West Nile
ganglia, thalamus, upper brainstem, and virus meningitis, neuroimaging studies
cerebellum as well as the anterior horns are unremarkable, and the EEG is
of the spinal cord. An estimated 30% to usually normal.
40% of patients with neuroinvasive West West Nile virus encephalitis is dis-
Nile virus infection develop meningitis, tinguished from meningitis by the pres-
50% to 60% develop encephalitis, and ence of signs and symptoms of brain
5% to 10% develop acute flaccid paraly- parenchymal involvement on exami-
sis.26,27 Other reported syndromes in- nation or diagnostic testing including
Continuum (Minneap Minn) 2015;21(6):1599–1611 www.ContinuumJournal.com 1601
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Arbovirus Infections
KEY POINTS
h West Nile virus neuroimaging or EEG. Results from mul- echo and fluid-attenuated inversion re-
encephalitis most tiple studies suggest that patients with covery (FLAIR) sequences. When pres-
commonly causes MRI West Nile virus encephalitis present with ent, MRI abnormalities typically involve
T2-signal abnormalities fever (70% to 100%), headache (50% to the thalamus, basal ganglia, and brain-
in the deep gray nuclei. 100%), and altered mental status (45% to stem (Figure 3-1). CT is considerably less
h West Nile virus 100%).36 Signs common in West Nile sensitive than MRI and is usually normal.
neuroinvasive disease virus encephalitis but unusual in other West Nile virus can also cause a po-
is often diagnosed by forms of viral encephalitis include tremor, liomyelitislike acute flaccid paralysis that
measurement of CSF IgM. parkinsonism, and myoclonus (20% to results from viral injury to motor neu-
40%).26,37 Weakness is common and may rons in the anterior horns of the spinal
be of a lower motor neuron type as- cord.40 Patients typically develop acute
sociated with hypotonia and areflexia, onset of asymmetric limb paralysis as-
with preserved sensation. Cranial neu- sociated with decreased or absent re-
ropathies, most commonly involving uni- flexes and preserved sensation. Weakness
lateral or bilateral peripheral facial palsy, may be associated with respiratory im-
occur in approximately 20%. pairment from diaphragm or intercostal
The prevalence of tremors due to muscle paralysis. Electrophysiology stud-
West Nile virus neuroinvasive disease ies obtained acutely show reduction in
ranges from 12% to nearly 100%.38 When amplitude or absence of compound
present, tremors are described as coarse muscle action potentials with relatively
and isolated to the upper extremities preserved sensory nerve action poten-
and have postural and kinetic compo- tials. EMG studies obtained 2 to 3 weeks
nents.39 Parkinsonian features also oc- after onset show characteristic features
cur with variable frequency and include of denervation, including increased in-
signs of bradykinesia, cogwheel rigidity, sertional activity and fasciculations. In
hypomimia, and postural instability.38,39 contrast to Guillain-Barré syndrome, no
Myoclonus can resemble that seen in evidence of significant demyelination
prion diseases, and usually involves the (slowed conduction velocities or con-
upper extremities and face. Cerebellar duction block) is seen. In most, but not
abnormalities including incoordination all, cases of West Nile virus, acute flac-
and gait ataxia occur in a variable per- cid paralysis is associated with clinical
centage of cases.26,37,38 signs and symptoms of systemic infec-
Patients with West Nile virus infec- tion, and the syndrome may occur in
tion have a normal complete blood association with meningitis or enceph-
count or mild leukocytosis.1 The CSF alitis. Patients typically have CSF features
findings in patients with West Nile virus similar to the features seen in meningo-
encephalitis are almost identical to the encephalitis. MRI of the spinal cord may
findings with meningitis, including pleo- show increased signal in the anterior
cytosis (mean 227 cells/HL), elevated horns on T2 and FLAIR sequences.
protein, and normal glucose. Neutro- West Nile virus neuroinvasive disease
phils predominate rather than lympho- is usually diagnosed by demonstration
cytes in 37% of cases (Case 3-1).35 MRI of West Nile virusYspecific IgM in CSF
is abnormal in approximately 50% to by enzyme-linked immunosorbent assay
70% of West Nile virus encephalitis cases, (ELISA).41 In some patients, CSF West
with the frequency of positive MRI find- Nile virus IgM may persist for 1 year or
ings increasing with imaging later in longer, and it may be necessary to per-
the course of disease (more than 7 days form serial studies of serum and CSF IgG
after symptom onset) and increased sen- and IgM to definitively distinguish acute
sitivity with use of T2-weighted fast spin from remote infection. CSF polymerase
1602 www.ContinuumJournal.com December 2015
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Case 3-1
A 64-year-old woman who lived in western Nebraska was brought to the emergency department in
August by her family for increasing confusion and altered mental status. The patient’s husband stated
that the patient was in her usual state of good health until she developed fever and fatigue 3 days prior to
presentation. Over the next 2 days, she developed nausea, vomiting, and diarrhea associated with
increasing headache. The morning of presentation, the patient was confused and unable to respond to
questions. On examination, she was febrile (39.2-C [102.5-F]), and awake but unable to follow commands
or respond purposefully. Her breathing was rapid, shallow, and labored. In the emergency department,
the patient was intubated, blood cultures were obtained, CT of the head was negative, and a lumbar
puncture was performed. Lumbar puncture showed an opening pressure of 15 cm water, a CSF pleocytosis
of 620 cells/HL (55% neutrophils, 40% lymphocytes), glucose concentration of 42 mg/dL, and protein
concentration of 114 mg/dL. The CSF Gram stain was negative, as were the CSF culture and blood cultures.
MRI of the brain showed T2-signal hyperintensity in the thalamus (bilaterally), midbrain, basal ganglia,
and left medial temporal lobe (Figure 3-1). CSF testing for West Nile virus IgM was positive. Her
hospital course was complicated by cardiac arrest and progressive loss of response to stimuli. The
patient died on hospital day 14.
FIGURE 3-1 Axial T2-weighted fast spin echo MRI of a patient with West Nile virus encephalitis. Increased signal intensity in
the thalamus bilaterally and in the right caudate nucleus (A), the substantia nigra (B), and the midbrain and
left medial temporal lobe (C ).
Comment. The presentation of acute altered mental status in an otherwise healthy individual is
concerning for severe encephalitis or severe bacterial meningitis. In cases such as this, the goal is to initiate
therapy for acute bacterial meningitis and herpes simplex encephalitis as soon as possible. Lumbar
puncture is the key diagnostic test. In this case, the CSF exhibited a neutrophil pleocytosis that is more
commonly found in bacterial meningitis but can be found in up to 50% of West Nile virus neuroinvasive
cases. The subsequent MRI findings are characteristic of West Nile virus. In particular, involvement of
deep gray matter in regions such as the basal ganglia, thalamus, and brainstem are characteristic of
central nervous system infection by a Flavivirus such as West Nile virus. Advanced age and intubation are
predictors of poor outcome in patients with neuroinvasive West Nile virus infection.
chain reaction (PCR) for West Nile virus before antibody responses have fully
is highly specific, but less sensitive than evolved, and in immunocompromised
serologic studies. CSF PCR may be individuals who may have delayed or
particularly useful early in infection, absent seroconversion.41 Antibodies
Continuum (Minneap Minn) 2015;21(6):1599–1611 www.ContinuumJournal.com 1603
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Arbovirus Infections
KEY POINT
h Dengue virus infections reacting with West Nile virus antigens in 18 months of follow-up.44 Up to 50% of
are associated with ELISA tests may occur as a result of West Nile virus encephalitis survivors
encephalitis and peripheral heterologous cross-reactions induced report cognitive problems, decreased
nerve syndromes. by infection with or vaccination against motor speed, and diminished dexterity
other flaviviruses, including St Louis 3 months after the initial infection.44
encephalitis virus, yellow fever virus,
and Japanese encephalitis virus. In Other Flaviviridae
some cases, it may be necessary to According to the World Health Orga-
confirm ELISA results by plaque- nization (WHO), dengue virus causes
reduction neutralization assays. Neu- approximately 50 million cases of dis-
tralization antibody titers are typically ease annually throughout the world and
highest against the inciting virus com- continues to expand its geographic dis-
pared with cross-reacting species. tribution throughout tropical and sub-
No specific therapy of proven ben- tropical regions. Dengue virus isolates
efit for West Nile virus infection exists. are divided into four different serotypes
Isolated case reports and small series and are maintained in endemic cycles
describe both benefit and lack of effect between humans and the Aedes aegypti
from treatment with IVIg containing mosquito. Dengue virus infection causes
high-titer anti-West Nile virus antibodies an acute self-limited febrile syndrome
and with interferon alfa. A multicenter characterized by headache, retroorbital
randomized controlled trial of a high- pain, rash, nausea, vomiting, diarrhea,
titer antiYWest Nile virus IVIg prepara- myalgia, and arthralgia. In individuals
tion was conducted by the Collaborative with prior exposure to dengue virus,
Antiviral Study Group (CASG) and did reexposure to another serotype places
not show evidence of a therapeutic the individual at increased risk for den-
benefit.42 A phase 2/3 trial to evaluate gue hemorrhagic fever, characterized by
the safety and efficacy of a humanized increased vascular permeability, throm-
monoclonal antibody directed against bocytopenia, hypotension, and hemor-
an epitope on the West Nile virus en- rhagic manifestations.
velope glycoprotein was closed because Acute dengue virus infections are
of low enrollment (NCT00515385). Iso- rarely associated with CNS involvement,
lated reports of use of corticosteroids and direct dengue virus infection of the
in patients with West Nile virus acute nervous system remains controversial.45
flaccid paralysis and brainstem dis- A 2014 study in India and Nepal found
ease do not permit any conclusions that 9.2% of dengue infections were
about efficacy.43 associated with a neurologic complica-
Mortality from West Nile virus neuro- tion.45 Of the 45 patients in a prospective
invasive disease is approximately 12% cohort study with neurologic manifesta-
and occurs almost exclusively in the tions associated with dengue virus infec-
subsets of patients with severe en- tion, encephalitis was the most common
cephalitis or severe acute flaccid paral- presentation at 33%.45 Other associated
ysis. The frequency and severity of neurologic abnormalities include en-
sequelae are still not well understood.44 cephalopathy (22%), myelitis, Guillain-
Six months after the acute infection, Barré syndrome, myositis, and neuralgic
40% of patients with movement disor- amyotrophy.45 The diagnosis of dengue
ders such as myoclonus, parkinsonism, is often clinical in endemic locations.
or tremors have residual symptoms, Diagnosis can be supported with serol-
and 20% have ongoing symptoms at ogy using acute and convalescent serum
1604 www.ContinuumJournal.com December 2015
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINT
for antibody to the dengue virus envelope can result in significant numbers of h Cases of eastern equine
protein. No known therapy exists for affected individuals. encephalitis virus and
acute dengue virus infection. Among Venezuelan
other problems, the development of Eastern Equine Encephalitis Virus equine encephalitis
dengue hemorrhagic fever with recur- Eastern equine encephalitis virus is virus encephalitis occur
rent infection from new serotypes has an alphavirus that causes a sporadic during localized
hampered the development of effica- mosquito-borne viral infection endemic epidemic transmission.
cious vaccination strategies. in the eastern United States and
Powassan virus is a rare tick-borne Caribbean. Four lineages of eastern
flavivirus maintained in an enzootic cycle equine encephalitis virus exist; group I
between Ixodes ticks and small mam- causes most disease in humans, whereas
mals.46 Powassan virus causes rare spo- groups IIA, IIB, and III cause primarily
radic cases of neurologic disease in equine disease in Central America and
humans. In the United States, Powassan South America.48Y50 Eastern equine
virus has been reported in the north- encephalitis virus is maintained in an
eastern and north central states.46 Symp- enzootic cycle with avian species after
toms of infection vary from mild fever a bite from a mosquito vector, Culiseta
and myalgia to acute flaccid paralysis, melanura.49 Birds serve as the primary
encephalitis, and death.46,47 reservoir hosts and amplifying hosts,
St Louis encephalitis virus is another and humans are incidentally infected
member of the Flaviviridae family, spread by various mosquito bridging vectors,
by mosquito vectors in southern Midwest including Culex, Culiseta, and Aedes
states. Cases of St Louis encephalitis species.51 In the United States, most
have rapidly decreased with the ex- cases are along the eastern seaboard,
pansion of West Nile virus. According and cases are found sporadically along
to Centers for Disease Control and the Gulf Coast, typically within 5 miles
Prevention (CDC) data, two cases of of swamplands or marshlands. Approx-
neuroinvasive St Louis encephalitis were imately 1 in 30 individuals exposed to
reported in the District of Columbia eastern equine encephalitis virus devel-
in 2010. St Louis encephalitis causes ops disease.52 Eastern equine encepha-
neuroinvasive disease in a minority of litis virus causes sporadic infections in
patients, with very similar clinical pat- human populations during the sum-
terns compared to West Nile virus. mer months and occasional larger epi-
demic outbreaks.
TOGAVIRIDAE (ALPHAVIRUSES) Patients infected with eastern equine
The family Togaviridae is composed of encephalitis virus develop nonspecific
enveloped single-stranded positive-sense symptoms common to other causes of
RNA viruses. In North America, eastern viral encephalitis, including fever, chills,
equine encephalitis virus is the most malaise, and myalgia. The prodrome
important member of this group caus- is followed by either recovery without
ing encephalitis and is, fortunately, neurologic illness or the onset of en-
rare. Chikungunya virus has recently cephalitis characterized by severe head-
emerged as the cause of massive epi- ache, confusion, nausea, and vomiting.
demics of a febrile arthralgic illness that, Seizures, focal neurologic deficits such
in rare cases, is associated with neu- as cranial nerve palsies or focal weak-
rologic manifestations. However, since ness, and meningismus are common
some epidemics can involve millions findings.53 Brainstem involvement is com-
of infected cases, even low-incidence mon and is associated with gaze palsies,
involvement of the nervous system nystagmus, and pupillary abnormalities.
Continuum (Minneap Minn) 2015;21(6):1599–1611 www.ContinuumJournal.com 1605
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Arbovirus Infections
Mortality is about 33% but increases to poor outcome,53 but a longer prodro-
50% in patients older than 60 years of mal period was associated with a bet-
age. Moderate to severe sequelae occur ter prognosis. Sequelae may be more
in one-third of survivors.53 common and generally more severe
Similar to the flaviviruses above, MRI in children.53
abnormalities occur predominantly in
the thalamus, basal ganglia, and brain- Venezuelan Equine
stem.53 EEG is typically diffusely slow, Encephalitis Virus
with some severely ill patients having Venezuelan equine encephalitis virus is
burst suppression or diffuse high-voltage an Alphavirus that was originally isolated
delta-wave slowing.54 Laboratory studies from the brains of dead horses.55
may show a peripheral leukocytosis with Venezuelan equine encephalitis virus
a neutrophil predominance in 69% and circulates between a mosquito vector,
hyponatremia in 60% of patients.53 CSF Culex melanoconion, and forest-
typically shows a significant pleocytosis dwelling small mammals and birds in
with a mean cell count of 370 leuko- Central America and South America.
cytes/2L in one study53 and 940 leuko- It emerges during epizootic outbreaks
cytes/2L in another.54 Approximately to infect horses and humans via bridge
60% of eastern equine encephalitis virus vectors such as Aedes taeniorhynchus.
cases will display a neutrophil predom- Epidemics typically occur in northern
inance in the CSF with a median neu- South America, but have extended as
trophil proportion of 70% of nucleated far north as Mexico and Texas.56 In
cells.53,54 CSF protein is often elevated areas of sylvatic (forest) activity, human
(median 97 mg/dL), and 90% of patients seroprevalence can be 50%. In contrast
have CSF glucose concentrations less to many encephalitic arbovirus infec-
than 60% of coincident serum values. tions, Venezuelan equine encephalitis
CSF red blood cells are common, re- viremia in humans is sufficient to trans-
flecting the necrotic and hemorrhagic mit virus to mosquitos for approxi-
features of the encephalitis pathologically. mately 72 hours.57 However, humans
Diagnosis is typically made by dem- are not likely to play an important role
onstration of IgM antibodies in CSF by in spread; instead, epizootic strains of
capture ELISA, demonstration of serum Venezuelan equine encephalitis virus
IgM antibodies, or a fourfold increase are dependent on equine amplifica-
in IgG antibodies between acute and tion for epidemic spread. Forty percent
convalescent sera. No proven antiviral of patients with Venezuelan equine en-
therapy exists for eastern equine en- cephalitis virus have virus in the pharynx,
cephalitis virus, and treatment is fo- suggesting that direct spread between
cused on supportive care and managing humans may be possible, although
complications such as seizures and in- human-to-human spread has never
creased intracranial pressure. No com- been proven.58
mercial vaccine for eastern equine Symptomatic Venezuelan equine en-
encephalitis virus exists, but standard cephalitis virus infection results in neu-
precautions to prevent mosquito bites rologic disease in a minority of cases
may help to prevent infection. In eval- following a viral prodrome of fever,
uating laboratory and imaging studies headache, photophobia, conjunctival in-
for prognostic value, one study found jection, myalgia, arthralgia, nausea, and
that CSF leukocytosis greater than dizziness. Pharyngeal inflammation,
500 cells/HL and hyponatremia less painful cervical lymphadenopathy, som-
than 130 mEq/L were predictive of a nolence, and tremulousness may occur.59
1606 www.ContinuumJournal.com December 2015
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
KEY POINTS
CSF analysis reveals lymphocytic pleocy- Chikungunya virus infection of the h Chikungunya virus is a
tosis, elevated protein, and a normal CNS is rare but has been reported. As- rapidly emerging virus
CSF glucose. Few reports of neuroim- sociated neurologic clinical manifesta- with rare associations
aging studies exist. CT scans are usually tions of chikungunya virus have included with neurologic disease.
normal. EEG typically shows diffuse meningitis, encephalitis, and encepha- h Chikungunya virus is
slowing, although some cases have focal lomyeloradiculitis.64Y66 Diagnosis of associated with
temporal slowing similar to that seen in chikungunya virus infection can be made meningitis and
herpes simplex virus encephalitis. with serology using acute and convales- encephalitis during
Venezuelan equine encephalitis virus cent serum, and cases of chikungunya acute infection.
infection is diagnosed by detection of virusYassociated CNS disease have been
specific IgM antibody in the CSF or confirmed following detection of antiY
serum, and fatality rates range from chikungunya virus IgM in the CSF.67 No
0.2% to 1% of symptomatic Venezuelan known efficacious therapy or vaccine
equine virusYinfected patients without exists for chikungunya virus.
symptoms of encephalitis and increases
to 10% to 25% in patients with enceph-
alitis. No antiviral therapy or human BUNYAVIRIDAE
vaccine has shown proven benefit. California Encephalitis Group
California encephalitis virus, La Crosse
Chikungunya Virus virus, Jamestown Canyon virus, and
Recently, an emerging alphavirus called Tahyna virus are the major causes of
chikungunya virus has rapidly spread encephalitis in the California encephalitis
across the tropical and subtropical re- group within the family of Bunyaviridae
gions around the globe. The name ‘‘chik- and genus Bunyavirus. Of these viruses,
ungunya’’ is derived from the Makonde La Crosse virus, California encephalitis
language of Tanzania and means ‘‘that virus, and Jamestown Canyon virus are
which bends up.’’ Over 1 million cases causes of disease in the United States,
of chikungunya virus disease were re- and Tahyna virus is predominantly a
ported in recent epidemics in India.60 cause of encephalitis in Russia. La Crosse
The virus rapidly spread west and now virus is the most common cause of
disease in the California encephalitis
is endemic in the Caribbean islands,
group. It was originally described in
South America, Central America, and
1965 after a postmortem examination
recently the southeastern United
of a child who died of encephalitis in
States.61,62 Chikungunya virus has rap-
La Crosse, Wisconsin.68 La Crosse virus
idly adapted to multiple mosquito-
is transmitted in an enzootic pattern be-
mammal transmission cycles depending tween squirrels and chipmunks by the
on the geographic region.63 An urban mosquito Aedes triseriatus in areas of
cycle between the mosquito vector, the Mississippi and Ohio River basins.69
A. aegypti, and humans is thought to Recent outbreaks of La Crosse virus have
support much of the recent epidemic demonstrated a shift in incidence to the
spread. Following the bite of an infected Appalachian region and West Virginia.70
mosquito, chikungunya virus causes a Human exposure is often associated with
characteristic febrile syndrome mani- camping or other recreational activities
fested by headache, rash, and severe in wooded areas in endemic regions.
arthralgia. Patients can develop a poly- California encephalitis virus was ori-
articular large-joint arthritis during acute ginally isolated in 1941, but it is rare.
infection, and symptoms of joint pain Most human cases occur in the western
can linger for months following infection. United States and Canada. The ratio of
Continuum (Minneap Minn) 2015;21(6):1599–1611 www.ContinuumJournal.com 1607
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Arbovirus Infections
KEY POINTS
h La Crosse virus causes asymptomatic to symptomatic infections CONCLUSION
cases of encephalitis is 1000:1.71 Arbovirus infections are increasingly
in children. Although La Crosse and California common throughout the United States
encephalitis viruses mostly cause dis- and the world. Cases of arbovirus in-
h Mortality following
infection from the
ease in children, with a mean age of fections will continue to challenge physi-
California encephalitis La Crosse virus infection in children cians to match the constellation of
group of viruses is low, of 7.5 years, Jamestown Canyon virus findings on examination, laboratory
and outcomes are affects predominantly elderly individuals studies, and neuroimaging with likely
typically favorable. in regions of the northern United States, viral causes. Thus, it is important to
with seroprevalence in some areas understand the characteristic presen-
reaching 10%.72 A recent report of a tations of arbovirus infections so the
Jamestown Canyon virus infection in appropriate testing can be completed
Montana underscores continued low- and patients can be provided with the
level transmission in the northern con- specific prognostic information for a
tinental United States.73 specific virologic diagnosis. Although
Symptoms of La Crosse virus ence- no approved therapies exist for arbo-
phalitis include fever, headache, vomit- virus infections, the diagnostic and prog-
ing in 70%, seizures in 46%, and altered nostic information provided by these
mental status in 42% of cases.71 Focal investigations can be very important
neurologic signs include hemiparesis, for patients and families.
aphasia, dysarthria, and chorea. About
10% of patients develop increased intra- REFERENCES
cranial pressure, and, rarely, cerebral 1. Davis LE, Beckham JD, Tyler KL. North
herniation can occur.71 Jamestown Can- American encephalitic arboviruses. Neurol
yon virus has similar clinical features. Clin 2008;26(3):727Y757, ix. doi:10.1016/
CSF analysis for the California en- j.ncl.2008.03.012.
cephalitis virus group reveals a lym- 2. Petersen LR, Brault AC, Nasci RS. West Nile
phocytic pleocytosis of approximately virus: review of the literature. JAMA 2013;
310(3):308Y315. doi:10.1001/jama.2013.8042.
600 cells/HL and normal glucose. An
increased CSF protein is found in 30% 3. Wang P, Bai F, Zenewicz LA, et al. IL-22
signaling contributes to West Nile encephalitis
of patients with encephalitis.71 Periph- pathogenesis. PLoS One 2012;7(8):e44153.
eral leukocytosis and hyponatremia sec- doi:10.1371/journal.pone.0044153.
ondary to syndrome of inappropriate 4. Dai J, Wang P, Bai F, et al. Icam-1 participates
secretion of antidiuretic hormone in the entry of west nile virus into the central
(SIADH) are common. IgM detection nervous system. J Virol 2008;82(8):4164Y4168.
doi:10.1128/JVI.02621-07.
in the CSF or a fourfold increase in
5. Samuel MA, Morrey JD, Diamond MS. Caspase
paired sera for IgG is considered diag-
3-dependent cell death of neurons
nostic for infection. contributes to the pathogenesis of West Nile
No antiviral therapy currently exists virus encephalitis. J Virol 2007;81(6):
for the California encephalitis group 2614Y2623. doi:10.1128/JVI.02311-06.
of viruses, and no vaccine is available. 6. Melian EB, Edmonds JH, Nagasaki TK, et al.
West Nile virus NS2A protein facilitates
Mortality from La Crosse encephalitis
virus-induced apoptosis independently of
is approximately 1% to 3%, and most interferon response. J Gen Virol 2013;94
survivors return to normal function. (pt 2):308Y313. doi:10.1099/vir.0.047076-0.
Ribavirin treatment for La Crosse 7. Yang MR, Lee SR, Oh W, et al. West Nile
encephalitis in children is not recom- virus capsid protein induces p53-mediated
apoptosis via the sequestration of
mended because of problems with phar-
HDM2 to the nucleolus. Cell Microbiol
macokinetics, toxicity at higher doses, 2008;10(1):165Y176. doi:10.1111/j.
and penetration into the CNS.74 1462-5822.2007.01027.x.
1608 www.ContinuumJournal.com December 2015
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
8. Medigeshi GR, Lancaster AM, Hirsch AJ, et al. Dallas, Texas, 2012. Diagn Microbiol Infect
West Nile virus infection activates the Dis 2014;78(2):132Y136. doi:10.1016/
unfolded protein response, leading to CHOP j.diagmicrobio.2013.11.006.
induction and apoptosis. J Virol 2007;81(20): 21. Iwamoto M, Jernigan DB, Guasch A, et al.
10849Y10860. doi:10.1128/JVI.01151-0.
Transmission of West Nile virus from an organ
9. Kleinschmidt MC, Michaelis M, Ogbomo H, donor to four transplant recipients. N Engl J
et al. Inhibition of apoptosis prevents West Med 2003;348(22):2196Y2203. doi:10.1056/
Nile virus induced cell death. BMC Microbiol NEJMoa022987.
2007;7:49. doi:10.1186/1471-2180-7-49. 22. Centers for Disease Control and Prevention
10. Parquet MC, Kumatori A, Hasebe F, et al. (CDC). Possible West Nile virus transmission to
West Nile virus-induced bax-dependent an infant through breast-feedingVMichigan,
apoptosis. FEBS Lett 2001;500(1Y2):17Y24. 2002. MMWR Morb Mortal Wkly Rep
doi:10.1016/S0014-5793(01)02573-X. 2002;51(39):877Y878.
11. Beatman E, Oyer R, Shives KD, et al. West Nile 23. Biggerstaff BJ, Petersen LR. Estimated risk of
virus growth is independent of autophagy West Nile virus transmission through blood
activation. Virology 2012;433(1):262Y272. transfusion during an epidemic in Queens,
doi:10.1016/j.virol.2012.08.016. New York City. Transfusion 2002;42(8):1019Y1026.
12. Samuel MA, Whitby K, Keller BC, et al. doi:10.1046/j.1537-2995.2002.00167.x.
PKR and RNase L contribute to protection 24. Watson JT, Pertel PE, Jones RC, et al. Clinical
against lethal West Nile Virus infection by characteristics and functional outcomes of
controlling early viral spread in the periphery West Nile Fever. Ann Intern Med 2004;141(5):
and replication in neurons. J Virol 2006;80(14): 360Y365. doi:10.7326/0003-4819-141-5-
7009Y7019. doi:10.1128/JVI.00489-06. 200409070-00010.
13. Sitati EM, Diamond MS. CD4+ T-cell 25. Bode AV, Sejvar JJ, Pape WJ, et al. West Nile
responses are required for clearance of virus disease: a descriptive study of
West Nile virus from the central nervous 228 patients hospitalized in a 4-county
system. J Virol 2006;80(24):12060Y12069. region of Colorado in 2003. Clin Infect Dis
doi:10.1128/JVI.01650-06. 2006;42(9):1234Y1240. doi:10.1086/503038.
14. Suthar MS, Ma DY, Thomas S, et al. IPS-1 is 26. Sejvar JJ, Haddad MB, Tierney BC, et al.
essential for the control of West Nile virus Neurologic manifestations and outcome of
infection and immunity. PLoS Pathog West Nile virus infection. JAMA 2003;290(4):
2010;6(2):e1000757. doi:10.1371/journal.
511Y515. doi:10.1001/jama.290.4.511.
ppat.1000757.
27. Sejvar JJ, Leis AA, Stokic DS, et al. Acute
15. Thompson BS, Moesker B, Smit JM, et al. A flaccid paralysis and West Nile virus infection.
therapeutic antibody against west nile virus Emerg Infect Dis 2003;9(7):788Y793.
neutralizes infection by blocking fusion within
doi:10.3201/eid0907.030129.
endosomes. PLoS Pathog 2009;5(5):e1000453.
doi:10.1371/journal.ppat.1000453. 28. Bains HS, Jampol LM, Caughron MC, Parnell
JR. Vitritis and chorioretinitis in a patient
16. Zhang B, Chan YK, Lu B, et al. CXCR3 mediates with West Nile virus infection. Arch
region-specific antiviral T cell trafficking within Ophthalmol 2003;121(2):205Y207.
the central nervous system during West Nile
doi:10.1001/archopht.121.2.205.
virus encephalitis. J Immunol 2008;180(4):
2641Y2649. doi:10.4049/jimmunol.180.4.2641. 29. Smith RD, Konoplev S, DeCourten-Myers G,
Brown T. West Nile virus encephalitis with
17. Clarke P, Leser JS, Quick ED, et al. myositis and orchitis. Hum Pathol 2004;35(2):
Death receptor-mediated apoptotic 254Y258. doi:10.1016/j.humpath.2003.09.007.
signaling is activated in the brain following
infection with West Nile virus in the 30. Fratkin JD, Leis AA, Stokic DS, et al. Spinal
absence of a peripheral immune response. cord neuropathology in human West Nile
J Virol 2014;88(2):1080Y1089. doi:10. virus infection. Arch Pathol Lab Med
1128/JVI.02944-13. 2004;128(5):533Y537.
18. Centers for Disease Control and Prevention. 31. Jean CM, Honarmand S, Louie JK, Glaser CA.
West Nile virus. www.cdc.gov/westnile/ Risk factors for West Nile virus neuroinvasive
index.html. Updated February 12, 2015. disease, California, 2005. Emerg Infect Dis
2007;13(12):1918Y1920. doi:10.3201/
Accessed October 2, 2015.
eid1312.061265.
19. Kramer LD, Li J, Shi PY. West Nile virus.
32. Nash D, Mostashari F, Fine A, et al. The
Lancet Neurol 2007;6(2):171Y181.
outbreak of West Nile virus infection in
doi:10.1016/S1474-4422(07)70030-3.
the New York City area in 1999. N Engl J
20. Racsa L, Gander R, Chung W, et al. Clinical Med 2001;344(24):1807Y1814. doi:10.1056/
features of West Nile virus epidemic in NEJM200106143442401.
Continuum (Minneap Minn) 2015;21(6):1599–1611 www.ContinuumJournal.com 1609
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
Arbovirus Infections
33. Yakub I, Lillibridge KM, Moran A, et al. USA. Emerg Infect Dis 2013;19:(9).
Single nucleotide polymorphisms in genes for doi:10.3201/eid1909.121846.
2¶-5¶-oligoadenylate synthetase and RNase L 47. Tavakoli NP, Wang H, Dupuis M, et al. Fatal
in patients hospitalized with West Nile virus case of deer tick virus encephalitis. N Engl J
infection. J Infect Dis 2005;192(10):1741Y1748. Med 2009;360(20):2099Y2107. doi:10.1056/
doi:10.1086/497340. NEJMoa0806326.
34. Lim JK, Louie CY, Glaser C, et al. Genetic 48. Centers for Disease Control and Prevention
deficiency of chemokine receptor CCR5 is a (CDC). Eastern equine encephalitisVNew
strong risk factor for symptomatic West Nile Hampshire and Massachusetts,
virus infection: a meta-analysis of 4 cohorts August-September 2005. MMWR Morb
in the US epidemic. J Infect Dis 2008;197(2): Mortal Wkly Rep 2006;55(25):697Y700.
262Y265. doi:10.1086/524691.
49. Loftin KC, Diallo AA, Herbert MW, et al.
35. Tyler KL, Pape J, Goody RJ, et al. CSF findings Five-year surveillance of West Nile and eastern
in 250 patients with serologically confirmed equine encephalitis viruses in Southeastern
West Nile virus meningitis and encephalitis. Virginia. J Environ Health 2006;68(9):33Y40.
Neurology 2006;66(3):361Y365. doi:10.1212/
01.wnl.0000195890.70898.1f. 50. Unnasch RS, Sprenger T, Katholi CR, et al.
A dynamic transmission model of eastern
36. Beckham JD, Tyler KL. Neuro-intensive care equine encephalitis virus. Ecol Modell
of patients with acute CNS infections. 2006;192(3Y4):425Y440. doi:10.1016/
Neurotherapeutics 2012;9(1):124Y138. j.ecolmodel.2005.07.011.
doi:10.1007/s13311-011-0086-5.
51. Mitchell CJ, Niebylski ML, Smith GC, et al.
37. Debiasi RL, Tyler KL. West Nile virus Isolation of eastern equine encephalitis virus
meningoencephalitis. Nat Clin Pract Neurol from Aedes albopictus in Florida. Science 1992;
2006;2(5):264Y275. doi:10.1038/ncpneuro0176. 257(5069):526Y527. doi:10.1126/science.1321985.
38. Davis LE, DeBiasi R, Goade DE, et al. West 52. Goldfield M, Taylor BF, Welsh JN, et al. The
Nile virus neuroinvasive disease. Ann Neurol persistence of eastern encephalitis serologic
2006;60(3):286Y300. doi:10.1002/ana.20959. reactivity following overt and inapparent
39. Sejvar JJ, Marfin AA. Manifestations of West human infectionVan eight year follow-up.
Nile neuroinvasive disease. Rev Med Virol Am J Epidemiol 1968;87(1):50Y57.
2006;16(4):209Y224. doi:10.1002/rmv.501. 53. Deresiewicz RL, Thaler SJ, Hsu L, Zamani AA.
40. Sejvar JJ. West Nile virus and ‘‘poliomyelitis’’. Clinical and neuroradiographic manifestations
Neurology 2004;63(2):206Y207. doi:10.1212/ of eastern equine encephalitis. N Engl J
01.WNL.0000130361.62281.69. Med 1997;336(26):1867Y1874.
41. Shi PY, Wong SJ. Serologic diagnosis of West 54. Przelomski MM, O’Rourke E, Grady GF, et al.
Nile virus infection. Expert Rev Mol Diagn Eastern equine encephalitis in Massachusetts:
2003;3(6):733Y741. doi:10.1586/14737159. a report of 16 cases, 1970-1984. Neurology
3.6.733. 1988;38(5):736Y739.
42. Hart J Jr, Tillman G, Kraut MA, et al. West 55. Beck CE, Wyckoff RW. Venezuelan equine
Nile virus neuroinvasive disease: neurological encephalomyelitis. Science 1938;88(2292):530.
manifestations and prospective longitudinal 56. Griffin DE, Levine B, Tyor WR, Irani DN. The
outcomes. BMC Infect Dis 2014;14:248. immune response in viral encephalitis. Semin
doi:10.1186/1471-2334-14-248. Immunol 1992;4(2):111Y119.
43. Pyrgos V, Younus F. High-dose steroids in the 57. Wang E, Bowen RA, Medina G, et al. Virulence
management of acute flaccid paralysis due and viremia characteristics of 1992 epizootic
to West Nile virus infection. Scand J Infect subtype IC Venezuelan equine encephalitis
Dis 2004;36(6Y7):509Y512. doi:10.1080/
viruses and closely related enzootic subtype
00365540410020659.
ID strains. Am J Trop Med Hyg 2001;65(1):64Y69.
44. Sejvar JJ. The long-term outcomes of human
58. Weaver SC, Salas R, Rico-Hesse R, et al.
West Nile virus infection. Clin Infect Dis
Re-emergence of epidemic Venezuelan
2007;44(12):1617Y1624. doi:10.1086/518281.
equine encephalomyelitis in South America.
45. Sahu R, Verma R, Jain A, et al. Neurologic VEE Study Group. Lancet 1996;348(9025):
complications in dengue virus infection: a 436Y440. doi:10.1016/S0140-6736(96)02275-1.
prospective cohort study. Neurology 2014;
59. Molina OM, Morales MC, Soto ID, et al.
83(18):1601Y1609. doi:10.1212/WNL.
Venezuelan equine encephalitis. 1995
0000000000000935.
outbreak: clinical profile of the case with
46. Sung S, Wurcel AG, Whittier S, et al. Powassan neurologic involvement. Rev Neurol
meningoencephalitis, New York, New York, 1999;29(2):296Y298.
1610 www.ContinuumJournal.com December 2015
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
60. Pialoux G, Gauzere BA, Jaureguiberry S, 67. Robin S, Ramful D, Le Seach’ F, et al. Neurologic
Strobel M. Chikungunya, an epidemic manifestations of pediatric chikungunya
arbovirosis. Lancet Infect Dis 2007;7(5): infection. J Child Neurol 2008;23(9):1028Y1035.
319Y327. doi:10.1016/S1473-3099(07)70107-X. doi:10.1177/0883073808314151.
61. Prince HE, Seaton BL, Matud JL, Batterman HJ. 68. Thompson WH, Kalfayan B, Anslow RO.
Chikungunya virus RNA and antibody testing Isolation of California encephalitis group
at a national reference laboratory since the virus from a fatal human illness. Am J
emergence of Chikungunya in the Americas. Epidemiol 1965;81:245Y253.
Clin Vaccine Immunol 2015;22(3):291Y297. 69. Rust RS, Thompson WH, Matthews CG, et al.
doi:10.1128/CVI.00720-14. La Crosse and other forms of California
encephalitis. J Child Neurol 1999;14(1):1Y14.
62. Lindsey NP, Prince HE, Kosoy O, et al.
doi:10.1177/088307389901400101.
Chikungunya virus infections among
travelersVUnited States, 2010-2013. 70. Haddow AD, Bixler D, Odoi A. The spatial
Am J Trop Med Hyg 2015;92(1):82Y87. epidemiology and clinical features of reported
doi:10.4269/ajtmh.14-0442. cases of La Crosse virus infection in West
Virginia from 2003 to 2007. BMC Infect Dis
63. Tsetsarkin KA, Weaver SC. Sequential adaptive
2011;11:29. doi:10.1186/1471-2334-11-29.
mutations enhance efficient vector switching
by Chikungunya virus and its epidemic 71. McJunkin JE, de los Reyes EC, Irazuzta JE,
emergence. PLoS Pathog 2011;7(12): et al. La Crosse encephalitis in children.
e1002412. doi:10.1371/journal.ppat.1002412. N Engl J Med 2001;344(11):801Y807.
doi:10.1056/NEJM200103153441103.
64. Nelson J, Waggoner JJ, Sahoo MK, et al.
Encephalitis caused by Chikungunya virus in 72. Mayo D, Karabatsos N, Scarano FJ, et al.
a traveler from the Kingdom of Tonga. J Clin Jamestown Canyon virus: seroprevalence
Microbiol 2014;52(9):3459Y3461. in Connecticut. Emerg Infect Dis
doi:10.1128/JCM.01288-14. 2001;7(5):911Y912.
65. Chusri S, Siripaitoon P, Hirunpat S, Silpapojakul K. 73. Centers for Disease Control and Prevention
Case reports of neuro-Chikungunya in (CDC). Human Jamestown canyon virus
southern Thailand. Am J Trop Med Hyg 2011; infectionVMontana, 2009. MMWR Morb
85(2):386Y389. doi:10.4269/ajtmh.2011.10-0725. Mortal Wkly Rep 2011;60(20):652Y655.
66. Ganesan K, Diwan A, Shankar SK, et al. 74. McJunkin JE, Nahata MC, De Los Reyes EC,
Chikungunya encephalomyeloradiculitis: et al. Safety and pharmacokinetics of
report of 2 cases with neuroimaging and ribavirin for the treatment of la crosse
1 case with autopsy findings. AJNR Am J encephalitis. Pediatr Infect Dis J
Neuroradiol 2008;29(9):1636Y1637. 2011;30(10):860Y865. doi:10.1097/
doi:10.3174/ajnr.A1133. INF.0b013e31821c922c.
Continuum (Minneap Minn) 2015;21(6):1599–1611 www.ContinuumJournal.com 1611
Copyright © American Academy of Neurology. Unauthorized reproduction of this article is prohibited.
You might also like
- Global Perspectives on the Transmission of Zoonotic RNA Viruses from Wild Animal Species to Humans: Zoonotic, Epizootic, and Anthropogenic Viral PathogensFrom EverandGlobal Perspectives on the Transmission of Zoonotic RNA Viruses from Wild Animal Species to Humans: Zoonotic, Epizootic, and Anthropogenic Viral PathogensNo ratings yet
- Noor2016 PDFDocument13 pagesNoor2016 PDFBilel DhaouadiNo ratings yet
- Critical Care For Multiple Organ Failure SecondaryDocument20 pagesCritical Care For Multiple Organ Failure SecondarysazaperdanaNo ratings yet
- Infecciones Virales Del SNCDocument246 pagesInfecciones Virales Del SNCpediatria hncase100% (1)
- HHS Public Access: Varicella Zoster Virus InfectionDocument41 pagesHHS Public Access: Varicella Zoster Virus InfectionRiskaNo ratings yet
- Zika VirusesssDocument5 pagesZika Virusesssanes noerNo ratings yet
- Review: OnlineDocument13 pagesReview: OnlineEllenaEllenNo ratings yet
- Guillain-Barré Syndrome. 2023Document30 pagesGuillain-Barré Syndrome. 2023Arbey Aponte PuertoNo ratings yet
- Newcastle Disease VirusDocument10 pagesNewcastle Disease VirusFidelito Nascimento FloraNo ratings yet
- Dechlorane Plus and Related Compounds in Peregrine Falcon (Falco Peregrinus) Eggs From Canada and SpainDocument6 pagesDechlorane Plus and Related Compounds in Peregrine Falcon (Falco Peregrinus) Eggs From Canada and SpainlacosNo ratings yet
- Anez - Et - Al - Evolutionary Dynamics - of - West - Nile - Virus in - The - United - States - pntd.0002245Document12 pagesAnez - Et - Al - Evolutionary Dynamics - of - West - Nile - Virus in - The - United - States - pntd.0002245San JamesNo ratings yet
- Review of Flavivirus EditedDocument9 pagesReview of Flavivirus Editedapi-318473384No ratings yet
- 1 s2.0 S1473309916303851 MainDocument11 pages1 s2.0 S1473309916303851 Mainliz zuñigaNo ratings yet
- Infectious EndocarditisDocument49 pagesInfectious EndocarditisDennisFrankKondoNo ratings yet
- Perspective Discovery of Antivirals Against SmallpDocument16 pagesPerspective Discovery of Antivirals Against SmallpLuthfi ZahluqiNo ratings yet
- West Nile Virus: Review of The LiteratureDocument8 pagesWest Nile Virus: Review of The LiteratureJere AyerbeNo ratings yet
- هرووبیماری جدید تکرارDocument16 pagesهرووبیماری جدید تکرارkaveh.azizi24No ratings yet
- Virology, Ecology, Epidemiology, Pathology, and Treatment of EasternDocument10 pagesVirology, Ecology, Epidemiology, Pathology, and Treatment of EasternCamila Volpini CardosoNo ratings yet
- DrugAINReview 2Document11 pagesDrugAINReview 2Kanaya ChinguNo ratings yet
- Boef Efo Jaef Ajfoef32Document13 pagesBoef Efo Jaef Ajfoef32Bush HsiehNo ratings yet
- Marine Natural Products in The Battle Against Dengue, ZikaDocument17 pagesMarine Natural Products in The Battle Against Dengue, ZikaBeatriz HenkelsNo ratings yet
- Mosquito Salivary Proteins and Arbovirus InfectionDocument16 pagesMosquito Salivary Proteins and Arbovirus InfectionSumera ShaikhNo ratings yet
- Jawaban Farkom 4 ZikaDocument26 pagesJawaban Farkom 4 Zikaastri rahayuNo ratings yet
- Emerging Vector-Borne Diseases: Sioux Falls, South DakotaDocument7 pagesEmerging Vector-Borne Diseases: Sioux Falls, South DakotaHakiki Oksan SaputraNo ratings yet
- Solignat Et Al. - 2009 - Replication Cycle of Chikungunya A Re-Emerging ArbovirusDocument15 pagesSolignat Et Al. - 2009 - Replication Cycle of Chikungunya A Re-Emerging ArbovirusLaise Eduarda Paixão de MoraesNo ratings yet
- Viral Encephalitis: Etiology, Clinical Features, Diagnosis and ManagementDocument13 pagesViral Encephalitis: Etiology, Clinical Features, Diagnosis and ManagementVidinikusumaNo ratings yet
- Epd-323209-54355-Common Infectious and Parasitic Diseases As A Cause of Seizures Geographic Distribution and Contribution To The Burden of Epile-ADocument26 pagesEpd-323209-54355-Common Infectious and Parasitic Diseases As A Cause of Seizures Geographic Distribution and Contribution To The Burden of Epile-ALucas MarzanoNo ratings yet
- Arthropod-Borne Encephalitides - UpToDateDocument21 pagesArthropod-Borne Encephalitides - UpToDateBhargav YagnikNo ratings yet
- Infectivev EndocarditisDocument53 pagesInfectivev EndocarditisMoises Zagala100% (1)
- C. Peter N. Watson, Anne A. Gershon, Michael N. Oxman (Eds.) - Herpes Zoster - Postherpetic Neuralgia and Other Complications - Focus On Treatment and Prevention (2017, ADIS) PDFDocument447 pagesC. Peter N. Watson, Anne A. Gershon, Michael N. Oxman (Eds.) - Herpes Zoster - Postherpetic Neuralgia and Other Complications - Focus On Treatment and Prevention (2017, ADIS) PDFJulianm8888No ratings yet
- Water-Borne Dengue: A Mosquito DiseaseDocument16 pagesWater-Borne Dengue: A Mosquito DiseaseJaylive AnziaNo ratings yet
- Czlonkowska 2019 WDDocument44 pagesCzlonkowska 2019 WDMartinaAstMonNo ratings yet
- Correspondence on Defining COVID-19 Neurological AssociationsDocument2 pagesCorrespondence on Defining COVID-19 Neurological AssociationsMudassar SattarNo ratings yet
- Malignant Transformation of Hymenolepis Nana in A Human HostDocument9 pagesMalignant Transformation of Hymenolepis Nana in A Human HostvictoriaNo ratings yet
- The Causes and Long-Term Consequences of Viral EncephalitisDocument19 pagesThe Causes and Long-Term Consequences of Viral Encephalitismukhlis akmalNo ratings yet
- Ebola Virus Disease PDFDocument31 pagesEbola Virus Disease PDFBibiqnaNo ratings yet
- Epidemiology of EncephalitisDocument2 pagesEpidemiology of EncephalitisFarhan Royan PermanahadiNo ratings yet
- 1995 - Hantaviruses Clinical, Microbiologic, and Epidemiologic AspectsDocument40 pages1995 - Hantaviruses Clinical, Microbiologic, and Epidemiologic AspectsFlorin BranisteNo ratings yet
- 01 Cir 98 25 2936Document13 pages01 Cir 98 25 2936Ikhsan Amadea9969No ratings yet
- Enfermedades Neuroinfecciosas Tropicales - ContinuumDocument23 pagesEnfermedades Neuroinfecciosas Tropicales - ContinuumNeurología RebagliatiNo ratings yet
- Varicella ZozterDocument2 pagesVaricella ZozterPinkan J. LintongNo ratings yet
- 1 s2.0 S2213260020302435 MainDocument6 pages1 s2.0 S2213260020302435 MainranauliafkNo ratings yet
- Whitley1991 Article HerpesSimplexVirusInfectionsOfDocument22 pagesWhitley1991 Article HerpesSimplexVirusInfectionsOfjaspforeverNo ratings yet
- Sphingomonas KoreensisDocument11 pagesSphingomonas KoreensisSMIBA MedicinaNo ratings yet
- Infectious and Autoimmune Causes of Encephalitis in ChildrenDocument11 pagesInfectious and Autoimmune Causes of Encephalitis in ChildrenFandi ArgiansyaNo ratings yet
- The Aspects of Gene TherapyDocument7 pagesThe Aspects of Gene TherapyKian Shane MedollarNo ratings yet
- Introduction to Individual Viruses and VirologyDocument1 pageIntroduction to Individual Viruses and VirologywilliamsbarriosNo ratings yet
- Cacar 2Document18 pagesCacar 2seorangaziNo ratings yet
- Dengue Vaccine Short ComingsDocument9 pagesDengue Vaccine Short Comingsmuhammad attiqueNo ratings yet
- Clinical Microbiology and Infection: A. Mailles, J.-P. Stahl, K.C. BlochDocument7 pagesClinical Microbiology and Infection: A. Mailles, J.-P. Stahl, K.C. BlochgugicevdzoceNo ratings yet
- Caly Etal 2015Document12 pagesCaly Etal 2015Fernando Alexis Gonzales ZubiateNo ratings yet
- Historical Overview of The Cephalosporin Spectrum: Four Generations of Structural EvolutionDocument8 pagesHistorical Overview of The Cephalosporin Spectrum: Four Generations of Structural EvolutionBagus FitraNo ratings yet
- Exploring The Intricacies of Encephalitis in Mosquito Borne Diseases Through Vector Host Pathogen Interactions A Critical ReviewDocument10 pagesExploring The Intricacies of Encephalitis in Mosquito Borne Diseases Through Vector Host Pathogen Interactions A Critical ReviewAthenaeum Scientific PublishersNo ratings yet
- MicroDocument5 pagesMicroJara AmargoNo ratings yet
- Polyomaviruses and Human DiseasesDocument383 pagesPolyomaviruses and Human Diseasessaby abbyNo ratings yet
- 2021_Risk factors promoting external ventricular drain infections in adult neurosurgical patients at the intensive care unit—a retrospective study. Frontiers in Neurology, 2021Document13 pages2021_Risk factors promoting external ventricular drain infections in adult neurosurgical patients at the intensive care unit—a retrospective study. Frontiers in Neurology, 2021Olga Manco GuzmánNo ratings yet
- Fmicb 10 02668Document25 pagesFmicb 10 02668Leonela SánchezNo ratings yet
- Definisi Klasifikasi Etiologi Dan ManifeDocument11 pagesDefinisi Klasifikasi Etiologi Dan ManifenatassyamarizNo ratings yet
- Seminar: Olli Ruuskanen, Elina Lahti, Lance C Jennings, David R MurdochDocument12 pagesSeminar: Olli Ruuskanen, Elina Lahti, Lance C Jennings, David R MurdochChika AmeliaNo ratings yet
- Fungal Infections of The Central Nervous SystemDocument17 pagesFungal Infections of The Central Nervous SystemHabib G. Moutran BarrosoNo ratings yet
- Boef Efo Jaef Ajfoef32Document13 pagesBoef Efo Jaef Ajfoef32Bush HsiehNo ratings yet
- Herpes Simplex Virus Infections of The CentralDocument10 pagesHerpes Simplex Virus Infections of The CentralCristian Delgado BáezNo ratings yet
- Enfermedad Por PrionesDocument27 pagesEnfermedad Por PrionesWasaCaballereNo ratings yet
- Herpesvirus Infections of The Nervous SystemDocument21 pagesHerpesvirus Infections of The Nervous SystemMarcela Garzon O VelezNo ratings yet
- NeurosyphilisDocument15 pagesNeurosyphilisJose Algomas KnorecuerdoNo ratings yet
- Tuberculosis of The Central Nervous SystemDocument17 pagesTuberculosis of The Central Nervous Systemnight.shadowNo ratings yet
- P(A) = 0.3, P(B) = 0.4, find P(A ∪ B) when A and B are mutually exclusive or independentDocument2 pagesP(A) = 0.3, P(B) = 0.4, find P(A ∪ B) when A and B are mutually exclusive or independentJose David KastilloNo ratings yet
- Are Viruses AliveDocument7 pagesAre Viruses AliveMarco GNo ratings yet
- Open Book Exam - Renal Dz. 2019Document2 pagesOpen Book Exam - Renal Dz. 2019Ahmed AliNo ratings yet
- HL BIO IB Extended EssayDocument39 pagesHL BIO IB Extended EssayRachel Tan Hui MinNo ratings yet
- MCQs IN MEDICINEDocument150 pagesMCQs IN MEDICINERITESH SINGHNo ratings yet
- Neural Control and Co-Ordination - Biology Notes For NEET - AIIMS - JIPMERDocument24 pagesNeural Control and Co-Ordination - Biology Notes For NEET - AIIMS - JIPMERlegal eagleNo ratings yet
- Past Paper Questions and AnswersDocument61 pagesPast Paper Questions and AnswerssophiaNo ratings yet
- Vaccines Calling The ShotsDocument2 pagesVaccines Calling The ShotsAngelica SimmonsNo ratings yet
- The Morphology of Blood CellsDocument20 pagesThe Morphology of Blood CellsLita EffendiNo ratings yet
- Anal Condyloma and HIVDocument13 pagesAnal Condyloma and HIVpologroNo ratings yet
- Fundamental of Microbiology Notes FinalDocument111 pagesFundamental of Microbiology Notes Finalshi vaniNo ratings yet
- Cefixime OS DS PIfinalDocument10 pagesCefixime OS DS PIfinalfiqrifahruroziaNo ratings yet
- Case Study: CNS Infection (Meningitis)Document18 pagesCase Study: CNS Infection (Meningitis)Nap Ich50% (2)
- Interleukin 6 in Exhaustive Exercises and Its Correlation To Bacteremia A Pilot StudyDocument9 pagesInterleukin 6 in Exhaustive Exercises and Its Correlation To Bacteremia A Pilot StudyAbdullah ElgeddawyNo ratings yet
- DFDFDFDFDocument10 pagesDFDFDFDFkclaportNo ratings yet
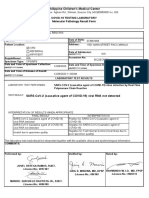
- Philippine Children's Medical Center: Covid-19 Testing Laboratory Molecular Pathology Result FormDocument1 pagePhilippine Children's Medical Center: Covid-19 Testing Laboratory Molecular Pathology Result FormRica RegorisNo ratings yet
- Summary Compassionate Use Remdesivir Gilead - enDocument43 pagesSummary Compassionate Use Remdesivir Gilead - enlelaniaNo ratings yet
- Class 12 Biology Lab Manual Practical Content 2023-24-1Document14 pagesClass 12 Biology Lab Manual Practical Content 2023-24-1Geetanjali Saraswat100% (4)
- Abcam MOM IgG1,2a, 3 Linker Ordering InfoDocument2 pagesAbcam MOM IgG1,2a, 3 Linker Ordering InfoqinggaoiNo ratings yet
- MutationDocument52 pagesMutationIlovecats AndmeNo ratings yet
- Autophagy Provides A Conceptual Therapeutic Framework For Bone Metastasis From Prostate CancerDocument8 pagesAutophagy Provides A Conceptual Therapeutic Framework For Bone Metastasis From Prostate CancerAnnisa RahmaNo ratings yet
- Kyle LiDocument12 pagesKyle Liapi-407846283No ratings yet
- Dermatology Exam 2023Document159 pagesDermatology Exam 2023Syed NoorNo ratings yet
- Microbial Toxins PDFDocument11 pagesMicrobial Toxins PDFAnonymous OPix6Tyk5INo ratings yet
- Brucellosis Brucellosis: Professor Abdelrahman A Mokhtar Internal Medicine Dept Mansoura University 2014Document94 pagesBrucellosis Brucellosis: Professor Abdelrahman A Mokhtar Internal Medicine Dept Mansoura University 2014Abdelrahman MokhtarNo ratings yet
- Please Circle Tests Needed and Provide Relevant ICD10 CodesDocument1 pagePlease Circle Tests Needed and Provide Relevant ICD10 CodesDjdjjd SiisusNo ratings yet
- AAHA Canine Vaccination GuidelinesDocument23 pagesAAHA Canine Vaccination GuidelinesRaniah DahlanNo ratings yet
- Hepatitis - Seminary WorkDocument15 pagesHepatitis - Seminary WorkDraganaNo ratings yet
- June 2013 QP - Unit 2 OCR Biology A-LevelDocument24 pagesJune 2013 QP - Unit 2 OCR Biology A-LevelIrrationaities324No ratings yet