Professional Documents
Culture Documents
Copd - NCP
Uploaded by
Monique Sacherow BacherOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Copd - NCP
Uploaded by
Monique Sacherow BacherCopyright:
Available Formats
Tyerman: Lewis's Medical-Surgical Nursing in Canada, 5th Edition
Chapter 31: Nursing Management: Obstructive Pulmonary Diseases
Care Plans - Customizable
NCP 31-2: Nursing Care Plan: Patient With Chronic Obstructive Pulmonary Disease
(COPD)
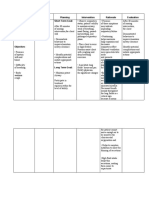
NURSING DIAGNOSIS Ineffective breathing pattern related to body position
that inhibits lung expansion, fatigue, respiratory
muscle fatigue as evidenced by use of three-point
position, pursed-lip breathing, use of accessory
muscles to breathe
Expected Patient Outcomes Nursing Interventions and Rationales
• Returns to baseline respiratory Ventilation Assistance
function • Monitor respiratory and oxygenation status to
• Demonstrates an effective rate, assess need for intervention.
rhythm, and depth of respirations • Auscultate breath sounds, noting areas of
decreased or absent ventilation and presence of
adventitious sounds, to obtain ongoing data on
patient’s response to therapy.
• Encourage slow, deep breathing; turning; and
coughing to promote effective breathing
techniques and secretion mobilization.
• Administer medications (e.g., bronchodilators,
inhalers) that promote airway patency and gas
exchange.
• Position to minimize respiratory efforts (i.e.,
elevate head of the bed and provide overbed
table for patient to lean on) to save energy for
breathing and promote chest expansion.
Copyright © 2023 Elsevier Inc. All rights reserved.
Care Plans - Customizable 31-2
• Monitor for respiratory muscle fatigue to detect a
need for ventilatory assistance.
• Initiate a program of respiratory muscle strength
and/or endurance training to establish effective
breathing patterns and techniques.
NURSING DIAGNOSIS Ineffective airway clearance related to excessive
mucus, retained secretions as evidenced by ineffective
cough, absence of cough, diminished breath sounds
Expected Patient Outcomes Nursing Interventions and Rationales
• Has normal breath sounds for the • Facilitate deep breathing by sitting the patient
patient up to maximize the use of the diaphragm and to
• Demonstrates effective coughing prolong the expiratory phase.
• Reports decreased dyspnea • Ensure adequate hydration (oral intake
• Maintains clear airway approximately 2–3 L/day, humidified ambient
air) to liquefy secretions for easier
expectoration.
• Teach effective cough techniques to minimize
the extent of airway collapse and to enhance
airway clearance.
• Assist with inhaled bronchodilator
administration to facilitate clearance of
retained secretions.
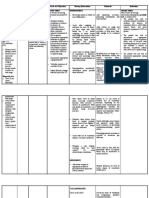
NURSING DIAGNOSIS Impaired gas exchange (related to alveolar
hypoventilation, as evidenced by headache on
awakening, PaCO2 ≥ 45 mm Hg and abnormal for
patient’s baseline, PaO2 <60 mm Hg, or SaO2 <90% at
rest)
Expected Patient Outcomes Nursing Interventions and Rationales
• Has PaCO2 of 35–45 mm Hg or • Monitor respiratory and oxygenation status to
usual compensated baseline assess the need for intervention.
value • Teach pursed-lip breathing to prolong the
Copyright © 2023 Elsevier Inc. All rights reserved.
Care Plans - Customizable 31-3
• Experiences return of PaO2 to expiratory phase and slow the respiratory rate.
normal range for patient • Assist the patient to assume a position of
• Reports improved mental status comfort (e.g., tripod position, elevated back
• Reports decreased dyspnea rest, support of upper extremities to fix shoulder
• Performs ADLs girdle) to maximize respiratory excursion.
• Administer and teach the appropriate use of
bronchodilators to open the airways.
• Teach signs, symptoms, and consequences of
hypercapnia (e.g., confusion, somnolence,
headache, irritability, decrease in mental acuity,
increase in respiration, facial flush, diaphoresis)
to recognize the problem early and initiate
treatment.
• Teach avoidance of central nervous system
depressants because they further depress
respirations.
• Administer O2 if appropriate, to increase SaO2
saturation.
• Select O2 supply systems and devices (e.g.,
nasal cannula, mask) that are appropriate for the
patient’s ADLs (rest, sleep, exercise) to
minimize the effect on preferred lifestyle.
NURSING DIAGNOSIS Imbalanced nutrition: less than body requirements
related to insufficient dietary intake, inability to ingest
food (decreased energy level, shortness of breath,
gastric distention) as evidenced by food intake less
than recommended daily allowance
Expected Patient Outcomes Nursing Interventions and Rationales
• Maintains body weight within • Monitor caloric intake, weight, and serum
normal range for sex, height, and albumin and protein levels to determine
age adequacy of intake.
Copyright © 2023 Elsevier Inc. All rights reserved.
Care Plans - Customizable 31-4
• Has normal serum protein and • Provide menu suggestions for high-protein,
albumin levels high-calorie foods to ensure maintenance of
weight.
• Give patient high-protein, high-calorie liquid
supplements if necessary to provide adequate
calories and protein to prevent weight loss and
muscle wasting.
• Plan periods of rest before and after food intake
to assist with controlling fatigue and to
compensate for blood flow diversion to the
gastro-intestinal tract for digestion.
• Refer to agency for financial and nutritional
assistance as necessary (e.g., Meals-On-Wheels,
home care) to ensure nutritional adequacy after
discharge.
• Discuss the benefit of five to six small meals
throughout the day because this reduces
bloating.
NURSING DIAGNOSIS Disturbed sleep pattern related to nonrestorative sleep
pattern (dyspnea, orthopnea, paroxysmal nocturnal
dyspnea) as evidenced by unintentional awakening,
feeling unrested
Expected Patient Outcomes Nursing Interventions and Rationales
• Sleeps at least 5 hr over a 24-hr • Identify usual sleep habits and elicit reasons for
period difficulty sleeping to provide baseline data.
• Reports improved sleep pattern • Monitor the patient’s sleep pattern, and note
• Reports feeling rejuvenated on physical circumstances (e.g., that causes fear or
awakening anxiety) that interrupt sleep to initiate
appropriate interventions.
• Observe for signs and symptoms of sleep apnea
Copyright © 2023 Elsevier Inc. All rights reserved.
Care Plans - Customizable 31-5
such as frequent awakenings at night, excessive
daytime sleepiness, or a partner that complains
of the patient’s snoring or gasping for air to
initiate appropriate diagnostic tests and
interventions.
• Identify patient-specific methods of relaxation,
and teach patient relaxation methods to foster
sleep.
• Encourage exercise and activity during daylight
hours to ensure improved sleep at night.
• Provide the patient with activity that promotes
wakefulness to limit daytime sleep.
• Instruct the patient in arranging surroundings
(e.g., clothing, temperature, position, noise
level) to produce an environment conducive to
sleep.
• Teach the patient to avoid alcoholic beverages,
caffeine products, or other stimulants before
bedtime to reduce interference with sleep.
NURSING DIAGNOSIS Risk for infection as evidenced by insufficient
knowledge to avoid exposure to pathogens, smoking,
malnutrition, stasis of body fluid (increased secretions)
Expected Patient Outcomes Nursing Interventions and Rationales
• Uses behaviours that minimize • Monitor for systemic and localized signs and
the risk of infection. symptoms of infection to determine whether an
• Experiences fewer or no infection is present.
respiratory infections. • Teach the patient to assess indicators of
infection: changes in sputum colour, quantity,
odour, and viscosity; an increase in cough and
dyspnea; the experience of fever, chills,
Copyright © 2023 Elsevier Inc. All rights reserved.
Care Plans - Customizable 31-6
diaphoresis, or excessive fatigue; an increase in
respiratory rate; and abnormal breath sounds
(gurgles, wheezing) to determine whether an
infection is present.
• Teach the patient to use good handwashing and
hygiene techniques and to avoid contact (when
possible) with people with respiratory
infections to minimize sources of infection.
• Encourage the patient to obtain vaccination for
influenza and pneumococcal pneumonia to
decrease the occurrence or severity of influenza
or pneumonia.
• Teach proper care and cleaning of home
respiratory equipment to eliminate this source
of infection.
• Instruct the patient to seek medical attention for
manifestations of early infection to initiate
treatment promptly.
• Teach the patient to follow the plan of care for
managing exacerbations (e.g., increase fluid
intake, initiate antibiotics and oral
corticosteroid) to initiate appropriate self-care
promptly.
ADLs, activities of daily living; PaCO2, partial pressure of arterial carbon dioxide; PaO2, partial
pressure of arterial oxygen; SaO2, arterial oxygen saturation.
Copyright © 2023 Elsevier Inc. All rights reserved.
You might also like
- PTB 01Document2 pagesPTB 01Dianne ParungaoNo ratings yet
- Nursing Care PlansDocument7 pagesNursing Care PlansJayson Sumampong100% (1)
- Case Pres Ncps FinalDocument13 pagesCase Pres Ncps FinalMariejoy YadaoNo ratings yet
- Nursing Diagnosis Nursing Intervention Rationale Breathing PatternDocument7 pagesNursing Diagnosis Nursing Intervention Rationale Breathing PatternJinaan MahmudNo ratings yet
- Ineffective Breathing Pattern Related To HyperventilationDocument4 pagesIneffective Breathing Pattern Related To HyperventilationVanessa Charlotte LagunayNo ratings yet
- Nursing Diagnosis Nursing Intervention Rationale Breathing PatternDocument8 pagesNursing Diagnosis Nursing Intervention Rationale Breathing PatternJinaan MahmudNo ratings yet
- Hronic Bstructive Ulmonary Isease: C O P DDocument17 pagesHronic Bstructive Ulmonary Isease: C O P DĂhlă ZădjăĹỉăNo ratings yet
- Nursing Care Plan Sample 3Document2 pagesNursing Care Plan Sample 3anon-333251No ratings yet
- Breathing RetrainingDocument39 pagesBreathing RetrainingAishwarya PanchalNo ratings yet
- NCP Lung CancerDocument2 pagesNCP Lung CancerAnn Pauline GoducoNo ratings yet
- Nursing Care PlanDocument8 pagesNursing Care Planalexander abasNo ratings yet
- Bukidnon State University: Subjective: Short Term: Short TermDocument1 pageBukidnon State University: Subjective: Short Term: Short TermSimbo Ralph JulesNo ratings yet
- Nursing Diagnosis Nursing Intervention Rationale Airway ClearanceDocument8 pagesNursing Diagnosis Nursing Intervention Rationale Airway ClearanceJinaan MahmudNo ratings yet
- Nursing Diagnosis Nursing Intervention Rationale Airway ClearanceDocument7 pagesNursing Diagnosis Nursing Intervention Rationale Airway ClearanceJinaan MahmudNo ratings yet
- NCP 3Document3 pagesNCP 3James Francisco GarcesaNo ratings yet
- 6 Pleural Effusion Nursing Care PlansDocument8 pages6 Pleural Effusion Nursing Care Plansmonisha100% (2)
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument4 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationTrisha SuazoNo ratings yet
- Nursing Intervention RationaleDocument2 pagesNursing Intervention RationaleLyca Mae AurelioNo ratings yet
- Chapter 027Document7 pagesChapter 027Diamonique95No ratings yet
- Asthma NCPDocument4 pagesAsthma NCPMonique Sacherow BacherNo ratings yet
- Cu 4Document3 pagesCu 4Paul SahagunNo ratings yet
- DX Resp Failure PDFDocument5 pagesDX Resp Failure PDFSherree HayesNo ratings yet
- Nursing Interventions - RespiratoryDocument4 pagesNursing Interventions - Respiratorymanager.intelligentsolutionsNo ratings yet
- Management of DysarthriaDocument12 pagesManagement of DysarthriaSherin Manoj100% (1)
- Nursing Care Plan in Pedia Ward: Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument3 pagesNursing Care Plan in Pedia Ward: Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationCharlynne AraojoNo ratings yet
- Nursing Assessment Nursing Diagnosis Goal Planning Rationale Implementation Evaluation Subjective DataDocument5 pagesNursing Assessment Nursing Diagnosis Goal Planning Rationale Implementation Evaluation Subjective DataDimpal Choudhary100% (1)
- Funda Notes Nca MidtermDocument9 pagesFunda Notes Nca MidtermAICEL A. ABILNo ratings yet
- PneumothoraxDocument33 pagesPneumothoraxjamil aldasriNo ratings yet
- Week 3 - Ms1 Course Task - Cu 3Document2 pagesWeek 3 - Ms1 Course Task - Cu 302 - DIMAYUGA, BRYANNo ratings yet
- Sample Chapter PDFDocument93 pagesSample Chapter PDFAlma AidhaNo ratings yet
- NCP FinalDocument5 pagesNCP FinalYoongiNo ratings yet
- NCP Acute BronchitisDocument9 pagesNCP Acute BronchitisCarl Simon CalingacionNo ratings yet
- Week 3 - MS1 COURSE TASK - CU 3Document2 pagesWeek 3 - MS1 COURSE TASK - CU 302 - DIMAYUGA, BRYANNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument9 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationYzel Vasquez AdavanNo ratings yet
- Actaul Drug StudyDocument2 pagesActaul Drug Studyjasper pachingelNo ratings yet
- Kel 7 - Nursing Care PlanDocument3 pagesKel 7 - Nursing Care PlanWahda PrameswariNo ratings yet
- Materi Nursing Care PlanDocument1 pageMateri Nursing Care PlanSiti nur Kholifatus samsiyahNo ratings yet
- NCP SciDocument3 pagesNCP SciJaylord VerazonNo ratings yet
- Myrna CruzDocument3 pagesMyrna CruzChris Opal NamocatcatNo ratings yet
- NCP PesebreDocument2 pagesNCP PesebreFrancoise Nicolette PesebreNo ratings yet
- NCP2Document2 pagesNCP2Aura Salve Ildefonso AllasNo ratings yet
- 6 Pleural Effusion Nursing Care PlansDocument7 pages6 Pleural Effusion Nursing Care PlansjamieboyRN87% (62)
- 6 Pleural Effusion Nursing Care PlansDocument7 pages6 Pleural Effusion Nursing Care PlansShaina Fe RabaneraNo ratings yet
- Ineffective Airway ClearanceDocument10 pagesIneffective Airway ClearanceHannah VueltaNo ratings yet
- NANDA DefinitionDocument5 pagesNANDA DefinitionAngel_Liboon_388No ratings yet
- NCP For Tuberculosis.Document7 pagesNCP For Tuberculosis.Kirstie ClaireNo ratings yet
- Group5 NCPDocument24 pagesGroup5 NCPAkira AtomarNo ratings yet
- Time Chart: Data Action ResponseDocument2 pagesTime Chart: Data Action ResponseAziil Liiza100% (2)
- COPD Care PLAN PDFDocument2 pagesCOPD Care PLAN PDFVanessaMUeller100% (1)
- Nursing Care Paln of Mrs Richard (Clinical Scenario-3)Document20 pagesNursing Care Paln of Mrs Richard (Clinical Scenario-3)Axsa AlexNo ratings yet
- Manila Doctors College: Pres. Diosdado Macapagal BLVD., Metropolitan Park, Pasay CityDocument3 pagesManila Doctors College: Pres. Diosdado Macapagal BLVD., Metropolitan Park, Pasay CityNichole CastleNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanRachelleNo ratings yet
- Pneumonia PATHOPHYSIOLOGYDocument3 pagesPneumonia PATHOPHYSIOLOGYElle RosalesNo ratings yet
- MSU-Iligan Institute of TechnologyDocument3 pagesMSU-Iligan Institute of TechnologyYuvi Rociandel LUARDONo ratings yet
- NCP For Scenario BreathingDocument4 pagesNCP For Scenario Breathingmy moznNo ratings yet
- Nursing Care Plans of Bronchial AsthmaDocument8 pagesNursing Care Plans of Bronchial AsthmaKannanNo ratings yet
- Goal:: Ineffective Airway Clearance Related To Cumulation of SecretionDocument4 pagesGoal:: Ineffective Airway Clearance Related To Cumulation of SecretionWyen CabatbatNo ratings yet
- The Basic Breathwork Book: A Fundamental Guide to Enhancing Health, Performance and MindfulnessFrom EverandThe Basic Breathwork Book: A Fundamental Guide to Enhancing Health, Performance and MindfulnessNo ratings yet
- Report 8b3a3101Document11 pagesReport 8b3a3101Pooja AgarwalNo ratings yet
- Test Bank For Health and Physical Assessment in Nursing 4th Edition by FenskeDocument33 pagesTest Bank For Health and Physical Assessment in Nursing 4th Edition by FenskeHeriberto Murray100% (37)
- Internship ReportDocument103 pagesInternship ReportMusnoon Ansary MoonNo ratings yet
- CMS MLN Cognitive Assessment and Care Plan Services CPT Code 99483Document4 pagesCMS MLN Cognitive Assessment and Care Plan Services CPT Code 99483Salomon GreenNo ratings yet
- Ro10 Bukidnon Provincial Medical Center Malaybalay CityDocument37 pagesRo10 Bukidnon Provincial Medical Center Malaybalay Citycaleb castilloNo ratings yet
- HemivaginaDocument3 pagesHemivaginafitriamarizkaNo ratings yet
- SBIL - Health QuestionnaireDocument2 pagesSBIL - Health QuestionnaireKrishna GBNo ratings yet
- Diet HistoryDocument2 pagesDiet HistoryBea Lou SabadoNo ratings yet
- Formularium Obat Viva Generik Kebraon: AntibiotikDocument8 pagesFormularium Obat Viva Generik Kebraon: AntibiotikLahar SatryaNo ratings yet
- Comfort, Effectiveness, AND Self-Awareness AS Criteria OF Improvement IN Psychotherapy"2Document10 pagesComfort, Effectiveness, AND Self-Awareness AS Criteria OF Improvement IN Psychotherapy"2Ilaria PacificoNo ratings yet
- 01-44-3 Efficacy of Self-Examination Therapy in The Treatment of Generalized Anxiety DisordersDocument7 pages01-44-3 Efficacy of Self-Examination Therapy in The Treatment of Generalized Anxiety DisordersAnisa FitrianiNo ratings yet
- Typhoid FeverDocument20 pagesTyphoid FeverKylie GolindangNo ratings yet
- Workshop ReportDocument42 pagesWorkshop ReportSushila PaudelNo ratings yet
- Uterine Therapeutics: by Henry MintonDocument48 pagesUterine Therapeutics: by Henry MintonSravs Pandu100% (1)
- Pre and Post Operative Care: To: DR - Biniyam.G By: Biniam.MDocument55 pagesPre and Post Operative Care: To: DR - Biniyam.G By: Biniam.MBini JaminNo ratings yet
- Motivational Interviewing Theoretical EssayDocument6 pagesMotivational Interviewing Theoretical EssayDanelleHollenbeckNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanSiena KaleiNo ratings yet
- Swot GileadDocument9 pagesSwot GileadMutia Poetry MandelaNo ratings yet
- 封面Document5 pages封面xiaoxin zhang100% (1)
- Medical Services Division: Hi-Precision Diagnostics (V Luna Branch)Document1 pageMedical Services Division: Hi-Precision Diagnostics (V Luna Branch)Ren RenNo ratings yet
- NCP For Dizziness and HeadacheDocument4 pagesNCP For Dizziness and Headachekarthi karthi100% (1)
- 1st Term .Jss3 PheDocument17 pages1st Term .Jss3 Phesamuel joshuaNo ratings yet
- Addiction Counsellors Guide To Working With Alcohol and Drug UsersDocument193 pagesAddiction Counsellors Guide To Working With Alcohol and Drug Usersxiejie22590100% (1)
- Potential Health Benefits of Garlic Allium SativumDocument26 pagesPotential Health Benefits of Garlic Allium SativumAlyssa SagarioNo ratings yet
- Counterfeit DrugsDocument2 pagesCounterfeit DrugsfreeBlidaman0967% (3)
- 1st Grading Exam MAPEHDocument4 pages1st Grading Exam MAPEHSherlita Vargas Mainit DurogNo ratings yet
- Music and Health June 2020utasv PDFDocument4 pagesMusic and Health June 2020utasv PDFPayneOgden54No ratings yet
- 2014 Resume - Adam SavineDocument1 page2014 Resume - Adam SavineAdamSavineNo ratings yet
- Activity 11 Cardiac Tamponade NCPDocument3 pagesActivity 11 Cardiac Tamponade NCPCloe CorpuzNo ratings yet
- Kidney PainDocument2 pagesKidney PainAulia Abdillah RamadhanNo ratings yet