Professional Documents
Culture Documents
Aging and Bone Metabolism (Pignolo, 2023)
Uploaded by
Evelyn ReCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Aging and Bone Metabolism (Pignolo, 2023)
Uploaded by
Evelyn ReCopyright:
Available Formats
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023].
See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism
Robert J. Pignolo*1,2
ABSTRACT
Changes in bone architecture and metabolism with aging increase the likelihood of osteoporo-
sis and fracture. Age-onset osteoporosis is multifactorial, with contributory extrinsic and intrinsic
factors including certain medical problems, specific prescription drugs, estrogen loss, secondary
hyperparathyroidism, microenvironmental and cellular alterations in bone tissue, and mechani-
cal unloading or immobilization. At the histological level, there are changes in trabecular and
cortical bone as well as marrow cellularity, lineage switching of mesenchymal stem cells to an
adipogenic fate, inadequate transduction of signals during skeletal loading, and predisposition
toward senescent cell accumulation with production of a senescence-associated secretory pheno-
type. Cumulatively, these changes result in bone remodeling abnormalities that over time cause net
bone loss typically seen in older adults. Age-related osteoporosis is a geriatric syndrome due to
the multiple etiologies that converge upon the skeleton to produce the ultimate phenotypic changes
that manifest as bone fragility. Bone tissue is dynamic but with tendencies toward poor osteoblastic
bone formation and relative osteoclastic bone resorption with aging. Interactions with other aging
physiologic systems, such as muscle, may also confer detrimental effects on the aging skeleton.
Conversely, individuals who maintain their BMD experience a lower risk of fractures, disability, and
mortality, suggesting that this phenotype may be a marker of successful aging. © 2023 American
Physiological Society. Compr Physiol 13:4355-4386, 2023.
Didactic Synopsis Introduction
Major teaching points Bone aging most ostensibly results in osteoporosis and the
increased risk of fracture (166). Notably, about 50% of
• Osteoporosis is the loss of mineral content, micro-
women and roughly 25% of men greater than 50 years of
architectural features, and bony matrix composition that
age will have an osteoporosis-associated fracture during
weaken bone and convey increased fracture risk.
their remaining life. Among women, the risk of hip fracture
• In both sexes, peak bone mass is usually obtained before remains very high and is roughly equivalent to the risk of
the fourth decade, with dramatic bone loss surrounding breast, uterine, and ovarian cancers combined. The functional
menopause, and gradual loss of bone mass beginning in impact of osteoporosis-related fracture includes pain, depen-
the sixth decade of life and in both men and women. dence, depression, skeletal deformities (especially in the case
of vertebral fractures), difficulty with bending, lifting, and
• Unbalanced bone formation and resorption coincide with
walking, as well as impairment in basic and instrumental
menopausal onset, accompanied by increased osteoclast
activities of daily living.
activation frequency.
With aging, there are changes in bone structure and
• Estrogen is associated with BMD, bone remodeling, rate metabolism that confer a greater risk of fracture (Figure 1).
of bone loss, and when low, increased fracture risk in older
men; at lower levels, testosterone may also elevate fracture
risk in men.
Correspondence to pignolo.robert@mayo.edu
• With aging, MSC lineage allocation results in recipro-
1 Department of Medicine, Divisions of Geriatric Medicine and
cal adipocyte and osteoblast differentiation in favor of
Gerontology, Endocrinology, and Hospital Internal Medicine,
increased bone marrow adiposity. Mayo Clinic, Rochester, Minnesota, USA
2 The Department of Physiology and Biomedical Engineering, and the
• Important pathways involved in age-related osteoporosis
include the RANK-RANKL-OPG and the Wnt-β-catenin Robert and Arlene Kogod Center on Aging, Mayo Clinic, Rochester,
Minnesota, USA
pathways.
Published online, January 2023 (comprehensivephysiology.com)
• Cellular senescence is a key mechanism that contributes DOI:10.1002/cphy.c220012
to age-related osteoporosis. Copyright © American Physiological Society.
Volume 13, January 2023 4355
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
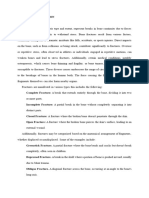
Physiologic and Cellular Histological
Intrinsic extrinsic changes alterations
factors factors
Bone Aging
Personal factors 2° Hyperparathyroidism BMAD Mineral content
Genetic predisposition Estrogen MSCs Microarchitectural deterioration
Skeletal loading Osteocytes Bone quality
Cellular senescence
Figure 1 Factors that contribute to age-related bone loss and their cellular and tissue manifestations. Age-related
osteoporosis is multifactorial and manifests as characteristic cellular and histological changes to bone.
Clinical Considerations 40
Fracture risk (% per decade)
Age
High risk
80
Osteoporosis
Osteoporosis and fractures 30
Moderate
70
60
Osteoporosis can operationally be defined as the loss of min- risk 50
20
eral content, micro-architectural features, and bony matrix
composition (i.e., bone quality) that weaken bone and convey
10
an increased likelihood of fracture. The goal of early identi- Low risk
fication of bone loss and mitigation of further deteriorative
0
changes is reduction in fracture risk. Current treatment of –3 –2.5 –2 –1.5 –1 0 0.5 1
osteoporosis focuses on the management of this risk. BMD (T-score)
The standardization of criteria for the diagnosis of osteo-
porosis relies heavily on quantification of bone mineral Figure 2 The association of BMD with risk of fracture as a function of
density (BMD) at central (hip, lumbar spine) and some- age. Fracture risk approximately doubles with every 1 standard devi-
ation drop in T-score. Intrinsic and extrinsic factors confer additional
times peripheral (distal radius) sites by dual-energy X-ray risk independent of BMD, such that individuals with T-scores in the
absorptiometry (DXA) (257, 378). Although other imaging osteopenic range but with risk factors are at higher likelihood of fracture
modalities exist, they vary in terms of skeletal sites evaluated, than with consideration of BMD alone (e.g., brown shaded area).
time for procedure, radiation exposure, and prediction of
fracture risk. High-resolution imaging by quantitative com- given individual. Low bone density is a strong predictor of
puted tomography and magnetic resonance imaging offer fracture risk, especially in older adults, but it still does not
ways to capture aspects of bone strength independent of carry the same weight as other risk factors or combination of
mineral content (80, 116), but they are not yet standard of risk factors. One solution to this issue has been the creation
care. Most imaging modalities, including DXA, represent of algorithms that predict low bone density and fractures.
BMD and other structural parameters as the number of stan- Age and body weight are factors common to all prediction
dard deviations that a given individual varies from a younger methods. Lifetime exposure to estrogen in women is also
(T-score) and same-aged cohort (Z-score) (183). Generally, strongly weighted in some methods.
a drop in one standard deviation (e.g., from a T-score of A fracture risk assessment tool (FRAX) (http://www.shef
−1 to −2, or from −2 to −3) doubles the risk of fracture .ac.uk/FRAX/) was proposed in 2008 to identify individuals
(Figure 2). Clinically, an incident fracture is diagnostic of at high risk of developing osteoporotic fractures. This tool
osteoporosis, even in the absence of formal testing to quantify estimates the 10-year probability of a major osteoporotic
BMD, or independent of a specific BMD T-score indicative fracture (i.e., fracture of the hip, spine, wrist, or humerus)
of osteoporosis (T-score < −2.5). or hip fracture for untreated patients. FRAX uses BMD and
a combination of risk factors to predict the likelihood of
fractures but has limitations, including no consideration for
Algorithms for risk-factor assessment
fall risk, assignment of prior fracture(s), and glucocorticoid
Most fractures related to bone loss occur in individuals whose intake as dichotomous rather than continuous variables;
BMD measurements are not consistent with osteoporosis use of femoral neck BMD only (underestimating risk of
(372). A major reason for this is that BMD assessment alone fracture due to low lumbar spine BMD and normal femoral
does not account for risk factors that contribute to poor neck BMD); failure to account for competing mortality, and
bone structure and quality (i.e., micro-architectural and bony limited validation among ethnicities. Other tools have been
matrix deterioration). Combining risk factors with BMD developed which account for some of the shortfalls attributed
increases the likelihood of predicting the risk of fracture in a to FRAX (8, 175, 367).
4356 Volume 13, January 2023
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Comprehensive Physiology Aging and Bone Metabolism
Bone remodeling, modeling, and the mechanostat The mechanostat theory (142, 144) explains the adaptation
of bone to its mechanical environment in terms of a feedback
Bone homeostasis and feedback mechanisms are largely loop. Local regions of bone that experience elevated mechan-
mediated by mechanisms of bone remodeling, modeling, ical loads are consolidated, while other regions of bone that
and response to mechanical loading. Discrete groups of experience depressed mechanical loads are resorbed. The
osteoclasts and osteoblasts, together described as basic multi- cell mediator for the mechanostat is the osteocyte and osteo-
cellular or remodeling units (BMUs), are largely responsible cytes are thought to modulate their mechanical properties
for the production of remodeled bone; that is, the process of through processes of rapid and reversible desensitization,
bone resorption followed by formation, which is normally or replacement during bone remodeling, the latter occur-
tightly coupled. These functional units are found in cortical ring over long periods of bone turnover (253). Age-related
bone as Haversian systems or in trabecular bone as How- changes affecting the response to mechanical loading are
ship lacunae (117, 328). Decreased BMUs, increased bone described below in the section titled on “Osteoblasts and
resorption rate, or decreased bone formation rate changes Osteocytes.”
the remodeling balance and promotes loss of bone density
and strength by uncoupling of resorption to formation (193).
Given the relatively shorter lifespans of osteoclasts and Osteoporosis as a geriatric syndrome
osteoblasts compared to the lifespan of BMUs, these cells
must be continually replenished for BMUs to successfully For most system-specific changes with aging, multiple etiolo-
remodel old bone (271). gies are at play, including aging changes in other physiologic
Conversely, formation of bone in the absence of prior systems, co-morbidities, drugs, genetics, and lifestyle. A
resorption, or resorption of bone without subsequent bone description of aging in a single system in isolation perhaps
formation, occurs through the process called “bone model- serves to simplify the task, but it also disguises the nature
ing” (143, 168, 276). In young adults, bone modeling due to of its true complexity. The geriatric syndromes serve as
formation happens during growth and mainly in the meta- examples of the complex interactions often required to
physeal regions. In older adults, bone modeling is mostly fully explain common age-related changes, and bone aging
replaced by remodeling within the BMU. A relative increase is no exception. Geriatric syndromes have been defined
in osteoclast-based resorption predominates without suffi- as multi-factorial, involving more than one organ sys-
cient bone formation by osteoblasts, both in postmenopausal tem, and sharing risk factors such as older age, functional
women and with aging, and leads to net bone loss. Thus, impairment, and impaired mobility (187). Osteoporosis is a
in these settings osteoporosis can be attributed, as least in common geriatric syndrome and from a clinical perspective
part, to osteoclast-related bone modeling. Agents that can is described based on multiple contributory mechanisms
suppress the osteoclast function, for example, antiresorptive (Figure 3).
drugs (111, 314) suppress remodeling-based bone forma- By reference to a funnel analysis, the point of convergence
tion, while modeling-based bone formation is relatively for multiple contributing etiologies of age-related bone loss
unhampered. is the remodeling imbalance. With aging, there is ultimately
On the other hand, osteoporosis treatment using anabolic an uncoupling of bone resorption to bone formation resulting
agents, focused mainly on promoting osteoblast function, in a net loss of bone tissue.
is often lacking in the coupling effect found in the BMU.
Physiologically, parathyroid hormone (PTH) analogs medi-
Falls and risk of fractures
ate their effects by both modeling and remodeling (248),
with the former accounting for about slightly less than a Up to 95% of fractures in hospitalized patients greater than 75
third of its anabolic action. Studies with Romosozumab, years old are related to osteoporosis. On average, about 85%
a neutralizing antibody against sclerostin (Scl-Ab), show of fractures occurring in those aged 60 to 74 years are also
that it works primarily through the modeling process (315). attributable to osteoporosis (2, 3, 236, 427). However, less
Scl-Ab, by activating the Wnt-pathway, suppresses osteoclast than about half of those sustaining recent fragility fractures
function while activating bone lining cells to become active (i.e., those resulting from low-level trauma such as a fall from
osteoblasts (231). Scl-Ab-based bone modeling may also standing height), are evaluated and treated for osteoporosis
suggest a mechanism for bone modeling during mechanical (115). In 2018, the Healthcare Effectiveness Data and Infor-
strain and exercise [i.e., sclerostin (SOST) suppression]. For mation Set (HEDIS) reported that only 51.9% of women
example, exercise suppresses SOST function, which in turn between the ages of 67 and 85 years who had a fracture
activates bone formation (239). With respect to bone remod- were evaluated or treated for osteoporosis, which is a small
eling and modeling, the relative contributions of inadequate improvement from the 2016 report of 47% (https://www
acquisition and excessive loss to osteoporosis pathogenesis .cms.gov/files/document/snp-hedis-2018-report.pdf). This
are variable, with the former more likely with strictly age- is still a suboptimal statistic in light of the risk of future
related bone loss and the latter more relevant with strictly fracture increasing manyfold following a fragility fracture
postmenopausal bone loss. (47, 67, 236).
Volume 13, January 2023 4357
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
Personal factors
Medications
Genetics
Nutrition
Immobility
>55 y.o. ♀
Skeletal
>65 y.o. ♂
unloading
Multifactorial
Functional
Older age
impairment
>1 organ
system Osteoporosis Multimorbidity
involvement
Muscle
Bone
Endocrine
Hematopoietic
Figure 3 Osteoporosis is a geriatric syndrome due to multisystem involvement, and contributions
made by older age, multifactorial risk factors, functional impairment, and multimorbidity.
Types of osteoporotic fractures Bone accrual and maintenance across the lifespan
The most common types of osteoporotic fractures are those Bone accrual and peak bone mass
related to hip, wrist, and thoracolumbar spine. Hip and
The epidemiology of osteoporotic fractures is reviewed by
wrist fractures are most likely to be sustained after a fall.
Harvey et al. (166). In both men and women, peak bone
Vertebral fractures are typically compression fractures with
mass is usually obtained before the fourth decade of life. In
anterior wedging, which with subsequent fractures, especially
women, there is a period of dramatic bone loss surrounding
those above and below the incident fracture, can result in
the menopause, accounting for about a third of the total mass
hyperkyphotic posture, height loss, pulmonary volume loss,
of calcium in the skeleton. This rapid bone loss occurs over
protruding abdomen, and costo-iliac impingement. Vertebral
a perimenopausal period of approximately 8 to 10 years. In
compression fractures can occur spontaneously, or with
men, there is a gradual loss of bone mass beginning in the
sudden or strenuous twisting, turning, bending, or lifting.
sixth decade of life, and in both men and women, age-related
It is important to distinguish between fragility, pathologic,
and high-level traumatic fractures. Pathologic fractures occur bone loss ensues at about the same rate beginning in the
in areas of bone made weak by a variety of detrimental seventh decade of life. Throughout the life span, men gen-
or destructive processes; however, the term is most often erally obtain greater peak bone mass and maintain a greater
applied to indicate fractures caused by neoplastic activity. bone mass compared to women.
In geriatric populations, most pathologic fractures are due
to metastatic lesions from a primary cancer elsewhere in the Gender differences
body. Fragility and traumatic fractures are differentiated by
the mechanism of injury (e.g., low vs. high-level trauma); In women over the age of 50 years, fracture rates double
however, even in high-level trauma, underlying osteoporosis compared to men, owing to the greater incidence of hip,
accounts for much of the observed fracture burden. distal radius, and vertebral fractures, the latter especially
Fragility fractures increase the likelihood of mortality when ascertained from imaging studies rather than history or
(41, 203, 216, 235, 434). The elapsed time from a prior clinical presentation. During the formative years and when
fracture, captured by the concept of “imminent risk” of adjusted for body habitus, males tend to develop thicker
fracture and defined as elevated risk of subsequent fracture cortical bone that may offer a mechanical advantage later in
within the succeeding 1 to 2 years, is now recognized as a life. These early gender differences may partly account for
factor that confers high risk of both subsequent fracture and the lower fracture risk observed in older men. Interestingly,
all-cause mortality (34, 42, 199, 210, 216, 363). Older age trabecular bone accumulation appears to be similar between
superimposes greater risk of imminent fracture (23). young women and men. Generally, age-related bone loss in
4358 Volume 13, January 2023
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Comprehensive Physiology Aging and Bone Metabolism
women and men is similar, with BMD losses occurring at Non-Hispanic Whites
a slower rate in men compared to women and without the Hispanic Americans
Hip fractures
acceleration of bone loss associated with the menopause in
Aging
women.
In the proximal femur and vertebrae of both sexes, trabecu- Native Americans
lar bone loss is initiated in midlife and accelerates thereafter.
African Americans
Trabecular thinning rather than trabecular dropout occurs
Asian Americans
more commonly in men compared to women. With aging,
endocortical bone loss and cortical porosity occur, especially
in long bones, but these alterations may be associated with Asian Americans
Vertebral fractures
a compensatory increase in periosteal bone that serves to Non-Hispanic Whites
preserve at least some bone strength (375).
Aging
Fracture incidence increases exponentially in men as
women, but in men, it begins about 5 to 10 years later.
This earlier onset in combination with longer female life Mexican Americans
expectancy underscores the larger impact of osteoporotic
African Americans
fractures among older women. Only approximately one-fifth
to one-quarter of hip fractures occur in men (318).
Figure 4 Racial differences contribute to the risk of hip and vertebral
The etiologies of osteoporosis in men are more heteroge- fractures. Non-Hispanic whites and Hispanic Americans have the great-
neous compared to women, and multimorbidity is commonly est risk for hip fractures. Asian Americans and non-Hispanic whites have
associated with male osteoporosis. Up to almost 67% of the greatest risk for vertebral fractures.
osteoporotic men have more than two risk factors for bone
loss, including other medical problems, prescription drugs,
and size, and ultimately fracture risk through the lifespan
or lifestyle/behavioral issues that contribute to bone loss and
and in later years (83, 87, 387, 417). Norwegian women have
susceptibility to fracture (16, 318). Identified comorbidities
the greatest incidence of fractures of the hip, while African
include hypogonadism, glucocorticoid use, and alcoholism,
women have the smallest incidence (211). Heterogeneity in
but in a significant proportion of men with osteoporosis,
rates of hip fracture has been reported, even within a single
it remains idiopathic. When added to DXA measurements,
racial group (81). Standardized hip fracture incidence across
risk factors in men increase the likelihood of hip fractures
racial groups in men remains about half of that in women.
(65), including the use of hypoglycemic agents and tricyclic
In the United States, hip fractures are highest in non-
antidepressants, as well as conditions such as Parkinson’s
Hispanic white cohorts, are intermediate or comparable in
disease and poor mobility.
Hispanic groups, and are lowest in African-American and
The relative roles of estrogens, androgens, and sex
Asian populations (26, 269). Vertebral fracture rates are
hormone-binding globulin (SHBG) in male osteoporosis and
highest or similar in Asian-Americans compared to whites
fracture are unsettled (225, 317, 428). Estrogen is important
(26, 48) with African-Americans and Mexican-Americans
for physiological bone development in young men, and
having the lowest rates (28, 48, 190, 415). After adjusting
associated with BMD, bone remodeling, rate of bone loss,
for weight and bone size on BMD, racial differences are
and when low, increased fracture risk in older men (250,
only somewhat mitigated among some groups; among other
283, 446). Testosterone is independently correlated with
racial groups, BMD continues to be influenced by weight
bone formation and resorption, stimulates periosteal bone
and bone size (26, 305, 345). Aging increases the likelihood
(135, 221, 453), and at lower levels may also elevate fracture
of fracture at any location and racial differences in fracture
risk (134). Increased SHBG concentrations have also been
incidence are consistent in older adults (Figure 4).
associated with increased risk of fracture in men (250).
When older men suffer fractures, they are more likely to
suffer morbidity and mortality than older women after a hip
fracture. Although older men have decreased rates of long Structural Alterations in Bone with Aging
bone fracture compared to women (188), vertebral fractures
are more common in men (371) owing to lack of clinical Bone biomechanics
recognition (52, 120) and perhaps higher rates of trauma. For a complete overview of bone biomechanics, excellent
Race and geography appear to influence the epidemiology of reviews are available (422, 423). Briefly, three major compo-
fracture in men. nents dictate whole tissue biomechanical behavior in bone:
amount of tissue (i.e., bone mass or size), geometry, and mate-
rial properties. Bone mass and geometry can be measured
Racial differences
directly or by using imaging modalities. Material proper-
Race contributes to differences in skeletal development, ties can be approximated from trabecular or cortical bone
pubertal onset, and growth, as well as specific skeletal shape samples. Mechanical behavior in the whole bone structure
Volume 13, January 2023 4359
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
represents the combination of all three contributing factors.
In general, mechanical testing is performed by applying an Periosteal apposition Endocortical resorption
increasing load to a bone while recording the displacement
as a function of applied load, which can be axial (tension
or compression), bending, or torsional. Relevant structural
outcome measures such as stiffness and maximum load are
derived values from the load-displacement relationships. The
moment of inertia is a calculated geometric property of a
bone in cross section which quantifies its intrinsic rotational Aging Aging
stiffness.
Overall, there is an age-related reduction in the material
strength and stiffness of bone in both men and women (275).
Between the mid-30s and about 70 years of age, cortical bone Outward cortical
Cortical thickness
displacement
bending strength is decreased by almost 20%, and trabecular Cortical area
bone strength in compression is reduced by about half. In ♀≥♂
addition, with aging bone becomes progressively brittle
and the energy required for fractures is less for any given Cortical porosity
skeletal site. Clinical implications of these changes include Trabecularization
Heterogeneity of mineralized bone
the following: (i) increased risk of fractures with aging;
Ultimate stress
(ii) critical importance of bone size in predicting fracture; ♀≥♂
and (iii) consistency of DXA in predicting fracture risk from
BMD measurements (69). Figure 5 Changes in cortical bone structure with aging. Due to
periosteal apposition in the setting of endocortical resorption, there is
outward cortical displacement with aging resulting in a decrease in cor-
Bone strength tical thickness and area. Concomitant alterations include increases in
cortical porosity, trabecularization, and heterogeneity of mineralized
Individuals who fall do not always fracture and those with bone as well as a decrease in ultimate stress. These changes tend to
only minimal or osteopenic losses in mineral content may occur more prominently in women compared to men.
easily suffer a fracture. Part of the explanation is that imaging
by DXA only provides an areal BMD without capturing
elements of bone microarchitecture that together contribute is less extreme. After mid-life in both sexes, nearly linear
to bone strength. Quantitative CT and MRI-based, high- declines in cortical bone occur, although the cumulative
resolution imaging distinguishes trabecular from cortical losses in women are greater than in men by roughly ten
components, provides volumetric rather than areal BMD, and percent.
identifies microarchitectural features that may contribute to In men and women, age-related endocortical resorption
bone strength. However, two-dimensional DXA images can causes a net decline in cortical area and thickness with
be interrogated using software to assess macroarchitectural outward cortical displacement due to periosteal apposition
features (e.g., of the hip) and derive parameters that estimate occurring in parallel (Figure 5). While increases in bone
bone strength better than BMD alone. The most relevant strength are attributed to this outward displacement, it only
measurement is hip axis length (54, 128), which is associated partially compensates for the decline in bone strength due to
with hip fracture risk in postmenopausal women, independent cortical thinning (327).
of BMD, and based upon length above sex-specific averages. In older women, cortical bone becomes the main source
Although limited reference data for sex-specific averages or of bone loss, showing predominately increased cortical
response to treatment effects are available (256), it never- porosity and so-called trabecularization of cortical bone
theless is another example of how bone structure relates to (53). Continuously high levels of remodeling result in a
strength. more heterogeneously mineralized bone and decreased
strength illustrated by thinning of the cortex and a decline
in the stress at which bone would sustain a fracture (i.e.,
Changes in cortical bone ultimate stress). Thus, as bone undergoes increasing endo-
The menopausal period of accelerated bone loss extends for cortical resorption with age, the amount of bony deposition
up to about 10 years, with loss of approximately one-fifth by periosteal apposition decreases, causing a net decline
to one-third of trabecular bone, but only about 5 to 10% of in cortical thickness. At younger ages, the thinner cortex
cortical bone. After this postmenopausal period, continuous is displaced outwardly, increasing resistance to bend-
bone loss ensues for the remaining life span, with cortical ing, but in postmenopausal women resistance to bending
and trabecular losses occurring at almost equal rates. In decreases secondary to continued endocortical resorption,
men, progressive bone loss also occurs during and past decreased periosteal apposition, and minimal outward
mid-life, but overall loss of both trabecular and cortical bone displacement (404).
4360 Volume 13, January 2023
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Comprehensive Physiology Aging and Bone Metabolism
MSCs from mice lacking expression of OPN (OPN-KO mice)
also support this finding (79) while bone marrow OPN limits
the size of the HSC pool (392).
Aging Aging
Matrix changes
Composition of bony tissue matrix affects bone quality,
Loss of trabecular bone and with aging promotes skeletal fragility related to loss
Thinning of trabecula bone of bone mass (57). Age-related changes in bone mineral,
Trabecular spacing
collagen, and its cross-linked products, and other noncol-
Figure 6 Changes in trabecular bone structure with aging. In women, lagenous matrix proteins likely contribute to anomalies in
there is a loss of trabecular bone with increased trabecular spacing. mineral crystals, including substitutions within the crystal.
In men, there is a thinning of trabecular bone rather than trabecular
bone loss. Enzymatically mediated and nonenzymatically mediated col-
lagen cross-links increase with aging, with the latter making
bone stiffer, more brittle, and more likely to fracture. There
Changes in trabecular bone is an inverse relationship between unbound bone pore water
Beginning at the time of menopause women undergo rapid (i.e., not bound to collagen or mineral) and bone mass such
trabecular bone loss (226), confirmed by both cross-sectional that the former increases with aging-associated bone loss.
and longitudinal QCT studies at the spine, distal radius, and These alterations reduce the capacity of bone to deform in
tibia (350, 351). Changes in the distal forearm are illustrative response to mechanical forces, resulting in increased skeletal
of differences in trabecular bone between women and men fragility and lowered threshold for fracture (57). Although
with aging. Whereas both trabecular bone loss and increased noncollagenous proteins can influence matrix properties and
trabecular spacing occur in older women, men have relatively skeletal remodeling, it is still an area of active investigation
thicker trabeculae and predominately experience thinning of as to whether these change with aging and predispose to
trabecular bone in later life rather than trabecular loss (227) bone fragility. Likewise, other matrix-targeted insults, such
(Figure 6). The trabecular bone score, based on gray-level as oxidative damage, repetitive injury, and glycosylation-
measurements of texture patterns on DXA images of the lum- induced modification, may also contribute to the alterations
bar spine, captures information about trabecular microarchi- in extracellular matrix seen with aging and disease states. It
tecture and is partly independent of clinical risk factors and remains unclear if these alterations are primarily or secon-
BMD in predicting fracture (167). darily due to aging in bone but would likely heterogeneously
affect bone quality.
Changes in the marrow compartment
Hematopoietic stem cells (HSCs) exhibit a variety of alter- Age-related Changes in Bone Cellularity
ations with aging including cell lineage surface marker
expression (148, 161), preference toward myeloid and Mesenchymal stem cells
megakaryocytic cell fates (as opposed to lymphoid bias) Bone-forming osteoblasts and bone marrow adipocytes are
(161, 325), accumulation of DNA damage (309, 361, 365), distinct cell lineage fates that originate from stem cells in
HSC pool expansion (362), and preponderance of dominant bone marrow stroma called MSCs. With aging, there are
clones (152, 178, 191, 281). The HSC compartment relies alterations in MSC lineage allocation resulting in reciprocal
on canonical and noncanonical Wnt pathway signaling for changes in adipocyte and osteoblast differentiation in favor
maintenance and on canonical Wnt signaling for regenera- of increased bone marrow adiposity (BMAT) (Figure 7). Pro-
tion (155, 346). The Wnt signaling pathway has similarly gressive exhaustion of MSC regenerative potential contributes
been implicated in dysregulated bone function with aging to dysfunction in bone homeostasis and metabolism.
(213), suggesting that antagonism of Wnt co-receptors LDL- Early studies focusing on bone marrow changes with aging
receptor protein 5 and 6 (Lrp5/6) by inhibitors SOST (261) identified trabecular bone loss accompanied by increased
and dickkopf1 (Dkk1) (22) in bone contributes to skeletal nonhematopoietic BMAT (201, 337, 399, 413, 414). Detailed
aging. It is thus attractive to hypothesize that loss of Wnt histomorphometric observations have since confirmed this
signals from the skeleton is a primary driver for age-related finding in aged and osteoporotic individuals (159, 461), with a
declines in HSC function. marked increase in BMAT found in postmenopausal females
Osteopontin (OPN), mostly expressed by osteoblastic cells and a more gradual but steady accumulation of BMAT in
(171) and a bony matrix component, may regulate both mes- older males (159).
enchymal stem cell fate determination as well as HSC pool MSC changes with aging may be intrinsic or due to alter-
size (79). OPN influences MSC lineage determination toward ations in the bone microenvironment. Both canonical and
an osteogenic rather than adipocytic cell fate through binding noncanonical Wnt signaling pathways favor osteoblasto-
of integrin heterodimer αVβ1 (CD51/CD29) on MSCs (79). genesis over adipogenesis (406). Adipocyte differentiation
Volume 13, January 2023 4361
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
Normal physiology ♀♂ toward the adipocyte lineage at the exclusion of those com-
mitted toward the osteoblast lineage may be one explanation
OPN Osteoblasts Osteocytes for reciprocal representation of BMAT and new bone for-
TAZ BMPs WNTs mation in the aging skeleton (296). This inverse relationship
bMSC is consistent with results from in vitro experiments on
Adipocytes MSCs demonstrating that pro-adipogenesis factors inhibit
OPN osteoblast differentiation (35, 122), while pro-osteogenesis
Bony matrix
factors inhibit adipocyte differentiation (153, 209). The
balance between MSC differentiation into osteoblastic and
Aging ♀♂ adipocytic cells is tightly controlled by TAZ (transcriptional
Menopause coactivator with PDZ-binding motif) (179), PPARγ2 (9),
Osteoporosis ♀♂ Osteocytes ΔFosB (369), as well as canonical Wnt-β-catenin and non-
DPP4 Osteoblasts canonical Wnt signaling pathways (405). The influence of the
RANKL SOST Mineral apposition bone morphogenetic proteins (BMPs) on BMAT is context
bMSC
PPARγ Mean wall thickness and cell type-specific (49, 184, 208, 308).
C/EBPα/β/σ Adipocytes BMAD Secreted factors with regulatory effects on osteoblas-
SFRP1 togenesis and adipogenesis have been identified on bone
FGF21 Extrinsic marrow preosteoblastic and preadipocytic cells. They include
factors secreted frizzled-related protein 1 (sFRP-1) and delta-like1
Immobilization (preadipocyte factor 1) (Dlk1/Pref-1) (3). When adipogen-
Zero gravity esis is the favored MSC differentiation pathway, reduction
Glucocorticoids in the number of MSCs available for osteoblast differ-
entiation, and subsequent bone formation ensues (360).
Figure 7 Bone MSC (bMSC) lineage switching with aging and osteo-
porosis. There is a substantial increase in bone marrow adiposity with
These observations are supported by experiments in MSC
aging, largely due to the Wnt pathway inhibitor SOST (sclerostin) in the cultures (33, 35, 360), studies in older mice (296), and
context of transcription and other factors that promote adipocyte over in an accelerated aging mouse model (204) where more
osteoblast differentiation of bMSCs. Normal (→), and enhanced (–→)
pathways are indicated; inhibited pathways are noted (||). Upwardly
adipogenesis and less osteoblastogenesis occur in murine
curved arrow indicates renewal and expansion (↻). MSC cultures. Although one report demonstrated that
adipocyte-forming capacity of human MSC does not change
with chronological (donor) age (202), sera derived from
requires the transcription factor peroxisome proliferator- older donors antagonized osteoblast differentiation (2),
activated receptor γ (PPARγ), which is necessary and and promoted adipogenesis in MSC cultures (394). The
sufficient for such differentiation and also plays a role in latter finding is consistent with the notion that age-related
maintaining MSCs in a differentiated state (9, 154). In addi- changes in the bone microenvironment may direct MSC
tion to PPARγ, factors that promote adipocyte differentiation differentiation away from an osteoblastic fate and toward an
include CCAAT enhancer-binding proteins (C/EBPα/β/γ/δ), adipogenic one.
secreted frizzled-related protein 1 (sFRP1), fibroblast growth Reciprocal osteoblast-adipocyte differentiation that occurs
factor 21 (FGF21), SOST, dipeptidyl-peptidase-4 (DPP4) with MSC aging (215, 272) at least in part explains the
inhibitor enzyme, receptor activator of nuclear factor-kappa- decrements in mineral apposition rate and mean wall thick-
B ligand (RANKL), glucocorticoids, glucose, saturated fatty ness as well as the increased BMAT (91, 328) in an older
acids, and reactive oxygen species (ROS). bone microenvironment. The effects of MSC and microen-
The increase in bone marrow fat with aging (56, 201, 364) vironmental aging on functional MSC engraftment and
is associated with the total decrease in bone mass, suggesting lineage determination were studied in carefully performed
a decline in osteoblast and osteocyte numbers. There is also transplantation experiments in mice (381). Using non-
evidence by histomorphometry that these changes occur at myeloablative conditions, old recipients were transplanted
sites of bone loss (286). Similarly, increases in bone marrow with young or old donor MSCs. Age-compatible engraft-
fat are observed in conditions that may only be indirectly (or ment was observed in the bone-lining, marrow, and bony
not at all) related to aging, including immobilization (288), matrix when young MSCs were transplanted into young
exposure to zero gravity (455, 468), ovariectomy (456), or recipients; however, age-compatible engraftment at the
use of high doses of glucocorticoids (137, 441). An inverse same anatomic sites in old donor-old recipient pairs was
relationship between BMAT and osteoblast/osteocyte content far less in aging animals. The fate of transplanted MSCs
implicates cell lineage switching as a viable mechanism predominately tended toward adipocyte versus osteoblast
for primary aging-related and secondary aging-associated differentiation in old recipients regardless of MSC donor
bone loss. age, strongly implying that age-related microenvironmental
It is now clear that both adipocytes and osteoblasts arise changes in bone are sufficient to mediate lineage switching
from marrow-derived MSCs (37, 192). MSCs committed in MSCs (381).
4362 Volume 13, January 2023
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Comprehensive Physiology Aging and Bone Metabolism
Osteoblasts and osteocytes osteoclastic bone resorption further promotes the remodeling
imbalance that leads to net bone loss.
There are extrinsic and intrinsic mechanisms for relative
mechanical unloading of the skeleton, including declines in
physical activity with aging as well as changes in mechan- Osteoclasts
ical transduction largely mediated through WNT signaling,
Age-onset osteoporosis, characterized by low BMD and dete-
respectively (333). Osteocytes are thought to be the primary
riorating microarchitectural features, is generally attributed
mechano-sensors in bone and secrete SOST, which negatively
to osteoblast dysfunction (272, 333). In contrast, bone loss
regulates WNT signaling, ultimately reducing osteoblast
associated with postmenopausal osteoporosis is mostly due to
number and activity. In individuals suffering long-term
increased osteoclast resorption in parallel with loss of estro-
immobilization, increased plasma levels of SOST can be seen
gen in women (1, 302, 330, 344).
(147), while in older women and in mice an age-associated
MSC- and osteoblast-regulated increases of osteoclast
decline in osteocyte number (with concomitant rise in empty
differentiation and resorption activity are important poten-
lacunae) is observed (58, 174). Taken together, these findings
tiators of bone loss (Figure 9). MSCs derived from older
suggest that aging leads to a deficit in mechanical sensing
adults demonstrate age-dependent changes in expression
and/or transduction (Figure 8).
of secreted factors that mediate osteoclast differentiation,
The abundance of osteoblasts and osteocytes, as well as
including increases in RANKL, M-CSF, and a decrease
their MSC precursors, is limited by cellular senescence and
in osteoprotegerin (OPG) expression (86, 307). Likewise,
apoptosis (see below) and are easily demonstrated in aging
osteoblasts from older adults show an age-related elevation in
bone (14, 123). Furthermore, the relative decrease in these
release of pro-osteoclastic cytokines like interleukin-6 (IL-6)
osteogenic cells and progenitors in the setting of continued
and a decrease in OPG expression (86, 307). Furthermore,
the imbalance between bone formation and resorption favors
Wnt Mechanical Osteoblast
Physical activity
Signaling Transduction number and activity
(A) Macrophages
Monocytes
bMSCs Osteoblasts
OPG MCSF
bMSC renewal
and expansion RANKL
Adipocytes
Osteocyte Osteocytes Osteoclasts
(1° mechanosensor)
SOST
Sclerostin Sclerostin BMPs, TGFβs, Bone
IGFs, FGFs Release of factors from bone resorption
Aging (B) Macrophages
Connexin-43 senescent Monocytes
bMSCs Osteoblasts
IL-6 Estrogen
OPG MCSF
RANKL
Adipocytes
Osteocytes Osteoclasts
Estrogen
Activation
SOST Frequency
Schematic bone section showing osteocytes
embedded in bony matrix, sitting in their lacunae. BMPs, TGFβs, Bone
Note the empty lacunae typically seen in aging
bone, resulting in lower osteocyte density. IGFs, FGFs Release of factors from bone resorption
Dendritic processes and canalicular network (not
shown) are also trimmed and disrupted,
respectively, with aging. Figure 9 Bone remodeling imbalance with aging and menopausal
status. (A) Bone remodeling is normally a constant dynamic process that
Figure 8 Aging-related changes in bone mechanical responsiveness. couples bone resorption to bone formation. (B) With aging, bone remod-
Osteocytes are the primary mechanosensors in bone, and with aging, eling becomes uncoupled due to cellular senescence, lineage switching
there is a drop in osteocyte density, loss of osteocyte dendritic pro- that favors adipogenesis over osteogenesis, and a relative increase in
cesses, and disruption of the connectivity of canalicular network. The sclerostin. With postmenopausal status in women (and decreased estro-
loss of connexin-43 is associated with osteocyte cell death, empty gen level in men), there is an increase in osteoclast differentiation and
lacunae, and deteriorative changes in the canalicular network. Wnt activation frequency as well as an enhanced stimulation of sclerostin.
signaling pathway-mediated mechanical transduction is also limited by In both aging and menopause increased levels of RANKL and IL-6 favor
sclerostin inhibition. Dashed arrows (⇢) indicate reduced pathways and osteoclast differentiation. Reduced (⇢), normal (→), and enhanced (—,
solid lines (—) indicate enhanced pathways; inhibited pathways are →) pathways are indicated; inhibited pathways are noted (||); bMSC,
noted (⊢). bone mesenchymal stem cell.
Volume 13, January 2023 4363
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
resorption because of the decrease in osteoblast number and Table 1 Genes Associated with BMD*
function with aging.
In telomere-based models of bone loss in mice, quantifica- Collagen type I alpha 1 (COL1A1)
tion of bone formation (e.g., osteoid, mineralization, mineral Cytochrome P450, family 19, subfamily A, polypeptide 1 (CYP19A1)
apposition rate, and bone formation rate) was significantly
D site of albumin promoter (albumin D-box)-binding protein (DBP)
lower compared to wild-type counterparts (51, 336, 370,
442). Osteoblast dysfunction as a major contributor to the Estrogen receptor 1 (ESR1)
osteoporotic phenotypes seen in these models is further Estrogen receptor 2 (ESR2)
supported by the observation that the number and activity Filamin B (FNLB)
of tartrate-resistant acid phosphatase-positive osteoclasts are
Forkhead box C2 (FOXC2)
relatively unchanged in the young versus older animals (51,
442). As in humans, age-associated bone loss in these models Integrin, alpha 1 (ITGA1)
is primarily due to osteoblast dysfunction in the context of LDL receptor-related protein 4 (LRP4)
minimally altered osteoclast function. LDL receptor-related protein 5 (LRP5)
Major histocompatibility complex (MHC)
5, 10-Methylenetetrahydrofolate reductase (MTHFR)
Multifactorial Nature of Age-associated Parathyroid hormone (PTH)
Osteoporosis Ras homolog gene family, member A (RHOA)
Genetic determinants of bone strength Rho guanine nucleotide exchange factor 3 (ARHGEF3)
The degree of phenotypic variance due to genetic influence, Secreted frizzled-related protein 1 (SFRP1)
or index of heritability, has been applied to BMD and bone Sclerosteosis (SOST)
strength (i.e., fracture) in twin and family studies. Heritability
Secreted phosphoprotein 1 (osteopontin) (SPP1)
of BMD and fracture ranged between 60% and 80% (338,
462) or 25% and 48% (18, 100, 212, 287), respectively. The Tumor necrosis factor ligand superfamily, member 11 (RANKL;
TNFSF11; receptor activator of NF𝜅B)
variance of other heritable markers of bone phenotypes has
also been described, including those of quantitative ultra- Tumor necrosis factor ligand superfamily, member 11a (TNFRSF11A)
sound measurements (181) and bone turnover markers (436). Tumor necrosis factor ligand superfamily, member 11b (OPG;
The search for putative genes related to the development TNFRSF11B)
of osteoporosis has focused mainly on the candidate gene Vitamin D receptor (VDR)
approach and genome-wide studies. Wingless-type MMTv integration site family, member 10B (WNT10B)
The candidate gene approach first selects gene(s) impli-
Zinc finger and BTB domain-containing protein 40 (ZBTB40)
cated in osteoporosis and then compares the frequency of
variants that are in or near those genes between individuals * Identified from candidate genes association studies.
with and without osteoporosis. Candidate gene studies have
identified a number of genes associated with BMD (419),
and examples of these genes are listed in Table 1. Although
simple and straightforward, the candidate gene approach TNFSF11, SOST, and TNFRSF11A) (347, 353), and those
suffers from bias related to the selection of nonosteoporotic variants associated with fracture risk) (found in LRP5, SOST,
persons (who can develop osteoporosis later in life). and TNFRSF11A) (347).
The genome-wide approach makes no assumptions about Advances in whole-genome sequencing (WGS) and whole-
specific gene contributions, but rather provides a represen- exome sequencing (WES) have provided important insights
tation of genes that may contribute to the susceptibility of into relevant genes associated with BMD, fracture risk, and
becoming osteoporotic. Using one genome-wide approach, bone development (397, 398, 473) and together with GWAS
linkage studies have discovered variants based on coseg- have identified genetic variants related to three well-described
regation in families with affected (osteoporotic) members. pathways with roles in bone formation, maintenance, and
For example, the mapping of quantitative trait loci (QTL) remodeling. First, in the RANK-RANKL-OPG pathway
by linkage analyzes has identified bone phenotypes related (TNFRSF11B, TNFRSF11A, TNFSF11), RANK-RANKL
to BMD at multiple locations including the wrist, forearm, binding promotes osteoclast differentiation while OPG
spine, femoral neck, and hip. inhibits this binding and subsequent osteoclast resorption.
Using another genome-wide approach, association stud- Variants within TNFRSF11A, TNFRSF11, and TNFRS11B
ies also overcame the bias of the candidate gene strategy. have been identified and related to BMD and fracture risk
Genome-wide association studies (GWAS) have identified (395, 396). Second, the Wnt-β-catenin pathway (LRP5,
more than 90 genetic variants to date, including those variants LRP4, SOST) regulates aspects of bone formation and frac-
associated with BMD (found in 1p36, ESR1, LRP4, LRP5, ture healing through control of osteoblast differentiation and
4364 Volume 13, January 2023
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Comprehensive Physiology Aging and Bone Metabolism
proliferation. Binding between frizzled receptor proteins and Medical conditions
LRP5/LRP6 initiates nuclear signaling ultimately leading
to gene expression changes in other bone-related pathways. Co-existing or past medical conditions, especially among
LRP5 has been associated with BMD and fracture risk (348) endocrine, rheumatologic, hematologic, and oncological
while SOST, an inhibitor of this pathway by preventing diseases, can predispose older individuals to continued
binding of Wnt to LRP5, is also a candidate gene (396). In bone loss (136). Although older individuals are not a priori
the third pathway, endochondral ossification occurs through excluded from any predisposing condition, they are much
mostly collagenous matrix deposition and then mineralization less likely to present with genetic conditions that otherwise
of a cartilaginous anlagen (88). Genes in this pathway have would present much earlier in life or limit life expectancy.
been implicated in bone loss, including those contributing Conversely, there are medical issues that are more likely
to the cartilage formation (PTHLH, SOX6), endochondral to contribute to osteoporosis due to advanced age, such as
bone, cartilage matrix (SOX9), mineralization (RUNX2), and vitamin D deficiency, postmenopausal status, and chronic
osteoblast differentiation (SP7) (88). kidney disease (CKD) (332).
Knowledge of genetic variants can be applied clinically Special consideration for renal osteodystrophy is deserved
to form the basis for effective prevention as part of an indi- given that the United States Renal Data System estimates
viduated risk assessment. Another potential use for genetic nearly half of all new CKD patients are over the age of 65 and
variants is through pharmacogenetics, to predict the response those with CKD stages 3 and 4 (GFR < 60 mL/min/1.73 m2 )
to therapies for osteoporosis. have risk factors for fracture (255). In one study, among 9931
long-term care residents aged 65 or older, about 40% had a
GFR less than 60 mL/min/1.73 m2 (145).
Personal risk factors, medical conditions, and drugs The National Institute of Diabetes and Digestive and
that contribute to osteoporosis Kidney Diseases (NIDDK) reports that 90% of hemodialysis
patients are affected by renal osteodystrophy. These skeletal
Personal risk factors complications and alterations in bone and mineral metabolism
Many personal risk factors (101, 354) are not modifiable that accompany CKD are associated with increased morbid-
but contribute much toward bone loss and fracture risk, ity, including bone pain, fractures, deformity, myopathy, soft
including older age, personal and family history of metabolic tissue calcification, and tendon rupture, as well as increased
bone disease and fracture, late onset of menses and early mortality (25, 251).
menopause, history of extended bed rest or immobilization, Renal osteodystrophy is typically categorized as osteitis
female sex, and non-Hispanic white or Asian race. They fibrosa, osteomalacia, or adynamic bone disease according
are nevertheless important to consider as part of an accurate to histopathologic features (182). Bone turnover may be
evaluation of an individual’s risk for fracture. By virtue of extremely high in CKD, as identified by elevated levels
their inclusion in multiple algorithms that assess the need for of circulating PTH, or abnormally low, as with “adynamic
BMD testing, age, weight, and lifetime exposure to estro- bone” disease (156) (Figure 10). Mixed pathophysiology
gen in women are among the more predictive risk factors along this spectrum may also be present. All types of renal
(16–21, 59, 60, 151, 238, 268, 374). Lifestyle choices often osteodystrophy cause defects in bone mineralization.
represent modifiable risk factors and should be investigated. Hyperplasia of the parathyroid glands is the major
Smoking, excessive alcohol intake, low intake of calcium mechanism behind high turnover renal osteodystrophy
and vitamin D, excessive caffeine and phosphate intake, and (20). Virtually all individuals with stage V CKD (GFR <
sedentary predisposition have been associated with greater 15 mL/min/1.73 m2 ) will develop secondary hyperparathy-
risk of osteoporosis and fractures (332). Immobilization roidism. In later stages of CKD, phosphorus is retained,
(e.g., bed rest greater than 1 week) is also a significant calcitriol is reduced, and less calcium is absorbed by the
risk factor for bone loss; weightlessness, as experienced by gastrointestinal tract (138, 282). Also, decreased vitamin
astronauts, is an extreme example, but this is approximated D receptor and/or the calcium-sensing receptor expression
on earth by prolonged bed rest, spinal cord injury (SCI), or occurs with parathyroid hyperplasia, further contributing to
stroke. altered calcium homeostasis (62).
Larger skeletons, bone loss starting later in life, slower PTH and calcitriol are important factors in the differentia-
progression, and the absence of a rapid phase of bone loss tion of preosteoclasts during activation of bone remodeling,
(i.e., menopause) make men less likely to suffer from osteo- and they also mediate osteoblast proliferation during bone
porosis and fractures compared to women. However, men formation (320, 400). PTH works in concert with other
have much higher mortality and chronic disability rates growth factors and cytokines (i.e., IGF-1, IL-1, IL-6, IL-11,
after a hip fracture (68). Men are also more likely to have and TNFα) to stimulate the activation of bone remodeling
a secondary cause of bone loss compared to women. These (139). Secondary hyperparathyroidism in CKD eventually
sex differences do not exclude males from being at increased manifests as osteitis fibrosa, with marrow fibrosis and accel-
risk of osteoporosis, especially as they get older and with the erated bone resorption (182). Accumulation of osteoclasts
greater chance of increased age-associated multimorbidity. and increased osteoclast activity are prominent and in cortical
Volume 13, January 2023 4365
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
CKD renal production of calcitriol leads to elevated PTH (368). In
parallel with CKD progression, FGF actions are abated as
Serum 1, 25 (OH)2 Wnt and BMP7 Klotho levels decrease (407).
FGF23
phosphate Vitamin D signaling (osteocytes) As CKD progresses, metabolic acidosis ensues. Dissolu-
tion of the bony matrix occurs as hydrogen ions are buffered
by bone carbonate (241). Acidosis suppresses osteoblast-
Serum calcium
based bone formation and stimulates osteoclast-mediated
Vitamin D bone reportion by altering the effects of PTH and vitamin D
receptor on osteoblasts, and influencing RANKL/OPG, IL-6, and IL-1
PTH
Calcium-sensing effects, respectively (141, 241).
receptor Calcium
Placed in perspective, the overall increased risk of hip frac-
Normal ALP
ture in end-stage renal disease is four to five times that of
PTH general population (12).
Bone Serum Medications
remodeling phosphate
Bone loss attributable to medication use is common (24,
Bone 249), especially in the older adults. Clear etiological roles
High bone turnover
Mineralization remodeling for certain medications are variable. However, certain
bone disease
(osteitis fibrosa) (osteomalacia) (adynamic bone
disease) medications have unequivocal contributions to bone loss.
Glucocorticoid-induced osteoporosis and bone loss due to
Mixed bone disease immunosuppressive therapy after solid organ transplant are
examples of challenging problems (24, 63, 89, 249).
Figure 10 Renal osteodystrophy contributes to age-related bone loss.
Its two most common forms are based on the effects of elevated or
depressed parathyroid hormone (PTH), manifested as osteitis fibrosa Estrogen deficiency and postmenopausal bone loss
(high bone turnover), or adynamic bone disease (low bone turnover).
Defects in bone mineralization are common in all forms of renal There is a strong relationship between low estrogen levels
osteodystrophy but elevated levels of FGF23 are a major inducer of
osteomalacia.
in women and the evolution of postmenopausal osteoporosis
(10). Serum estradiol (E2) levels decrease by about 90%, and
the weaker serum estrone (El) declines by about 70% during
portions of long bones, there is increased porosity as well menopause (222).
as replacement by weaker, woven (nonlamellar) bone (182). Unbalanced bone formation and resorption rates mani-
Osteomalacia can occur in CKD, predominantly the result fest as uncoupled bone remodeling (Figure 9) and coincide
of low bone turnover, increased fibroblast growth factor 23 with menopausal onset. At the level of the so-called “bone-
(FGF23), defective mineralization, and increased osteoid. forming unit,” there is an increase in activation frequency
Adynamic bone disease represents the most likely renal (the rate at which osteoclasts initiate contact with bony
osteodystrophy in those without secondary hyperparathy- surface and begin resorption), prolongation of the resorp-
roidism, those on hemodialysis or peritoneal dialysis, and tion period (186), and shrinkage of the formation period
in those with less common aluminum or other intoxication (271). At menopause, there is roughly a doubling of bone
(139, 182). The deficiency of bone morphogenic protein-7 resorption as compared to formation (146) causing accel-
(i.e., osteogenic protein-1), a growth factor important in erated bone loss, and a net movement of calcium from
osteoblastic cell differentiation, has been implicated in ady- bone tissue to extracellular fluid. Compensatory processes,
namic bone disease (460). Mineralization is depressed and such as increased renal calcium excretion, decreased intesti-
osteoid thickness remains sparse (139, 182, 460). nal calcium resorption, and partial PTH suppression, limit
FGF23 regulates phosphorus and 1,25-dihydroxy vitamin hypercalcemia (149, 349, 463), but also result in a net total
D (calcitriol) metabolism and levels increase progressively, body calcium imbalance (i.e., loss). Estrogen repletion in
likely as a compensatory mechanism to normalize high serum early menopause preserves both renal calcium re-uptake
phosphate levels. In doing so, FGF23 increases phospha- and calcium absorption from the gut (280), suggesting that
turia and decreases calcitriol. FGF23 may thus serve as a these compensatory mechanisms are directly related to
biomarker to identify CKD patients who could benefit from estrogen loss.
more aggressive management (437). FGF23 acts in the kidney The effects of estrogen on osteoblast and osteoclast biol-
via FGF receptor 1 (FGFR1) and its coreceptor Klotho. Its ogy point to regulation of differentiation at the cellular and
phosphate-lowering effects occur by decreasing the expres- molecular level. Estrogen promotes MSC differentiation
sion of type 2a and 2c sodium-phosphate cotransporters toward an osteoblast fate, preosteoblast to an osteoblast lin-
in the renal proximal tubules and by suppressing intestinal eage, and reduces apoptosis of osteoblasts and osteocytes (85,
phosphate absorption (i.e., by reducing calcitriol). Lowering 280, 340). Estrogen also increases the production of IGF-1,
4366 Volume 13, January 2023
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Comprehensive Physiology Aging and Bone Metabolism
transforming growth factor-alpha (TGF-α), and procollagen 375). Cortical bone loss with increases in porosity occurs in
synthesis (119, 319), facilitating osteoblast proliferation, and both postmenopausal women and sex steroid-deficient men
matrix formation. Importantly, estrogen suppresses levels of (469). Other age-induced structural abnormalities include a
the Wnt signaling inhibitor SOST (125, 289, 295). Estrogen decrease in lacunar density (58, 197), affecting intercellular
deficiency confers the opposite effects (Figure 9). Mice with communication via the canalicular network, and dampening
resistance to SOST due to LRP5 mutations have partially anabolic responses to skeletal loading (21, 418). Connexin-43
abrogated ovariectomy-induced bone loss (311), suggesting has been implicated in the maintenance of the canalicular
that estrogen mediates some of its protective effects on the network and its loss is associated with osteocyte cell death,
skeleton by SOST inhibition (219). Other studies demon- empty lacunae, accumulation of osteoclasts, deteriorative
strate that SOST also increases RANKL (a key molecule in changes in bone material properties, and the presence of bony
osteoclast differentiation) and inhibits the RANKL decoy microcracks (95, 430).
receptor OPG (420), increasing antiresorptive effects. Con- BMAT increases with age, causing the development of
versely, Wnt signaling directly inhibits osteoclast formation a yellow fatty marrow (297). As mentioned above, there
(450). Therefore, estrogen may both maintain bone formation is strong inverse correlation between BMD and BMAT
and inhibit bone resorption through its inhibitory effects (377) with increases in BMAT associated with fractures and
on SOST. osteoporosis (30). In an animal MSC transplantation model,
In addition, estrogen has other suppressive effects on MSCs transplanted from young donors into old recipients
bone resorption related to reduced production of RANKL, underwent lineage switching from an osteogenic to an adi-
increased OPG production, as well as reduced production pogenic fate, implicating that age-related microenvironmental
of cytokines [including interleukin-1 (IL-1), IL-6, TNF-α, changes influence red marrow conversion (381). Net bone
M-CSF] and prostaglandins known to play key roles in bone loss occurs when the balance of bone remodeling favors bone
resorption (17, 113, 177, 196, 218, 412). In fact, pharmaco- resorption over bone formation (277, 326); however, unlike
logical blockade of IL-1 or TNF-α can mitigate the expected postmenopausal osteoporosis, aging-related bone loss largely
elevation of bone resorption markers in women newly post- is caused by relatively less bone formation. With aging, there
menopausal (76). While estrogen can inhibit osteoclast is a transcriptional shift from promoting osteoblastogenesis
differentiation, it can also promote cell death of early and to favoring adipogenesis, due to decreases in Runx2 and Osx
mature osteoclasts through apoptotic pathways (274, 304). expression, an increase in PPARγ expression, and reduced
Although follicle-stimulating hormone (FSH) has been WNT signaling (322, 343, 391).
proposed to play a role in postmenopausal bone loss (112, The roles of gonadal sex steroids in regulating skeletal
401), more recent evidence suggests that it does not regulate health are becoming clearer. Current understanding suggests
bone resorption in either women or men participating in estrogen is a key mediator of bone health in both post-
interventional studies (106, 316, 426). The effect of testos- menopausal women and older men (158, 349, 382). There
terone to limit bone resorption at least in part is related is inconsistent evidence for role of testosterone in the main-
to aromatization of testosterone to estrogen (121). In vitro tenance of BMD in men (158, 382), although some studies
evidence suggests that testosterone promotes osteoblast pro- found a direct association between decreasing testosterone
liferation and survival (214, 271), perhaps playing a role in
levels and lower BMD (32, 134) and testosterone clinically
increasing bone formation in women; however, a major role
improves trabecular BMD in the spine (385) Some of these
for testosterone in postmenopausal skeletal maintenance is
positive findings could be explained by the aromatization
unlikely.
of androgens into estrogen and binding to the estrogen
receptor (121).
Compared to postmenopausal women, older men lose
Age-related bone loss about half as much bone and sustain about a third as many
Trabecular bone loss typically begins sometime during fragility fractures (349). Although men do not experience
the third decade of life in both males and females and a menopausal equivalent, biologically available sex steroid
dramatically increases in the perimenopause period (124, levels are sensitive to increasing levels of SHBG levels with
220). As mentioned above, this process is directly affected age (224). Bioavailable free and albumin-associated sex
by declines in estrogen and testosterone levels, leading to steroids decline over the male life span to about half and 65%
osteoporosis (220). Other hormones also affect bone mass, of estrogen and testosterone, respectively (224).
including PTH and corticosteroids (163, 448). For example, Despite testosterone being the predominant sex steroid in
a common age-related phenomenon is secondary hyper- men, cross-sectional and longitudinal studies have demon-
parathyroidism caused by low vitamin D levels and decreased strated that male BMD at multiple skeletal sites better
renal calcium absorption (263). Reproducible alterations in correlates with circulating bioavailable E2 than testosterone
trabecular architecture include loss of trabecular number levels (223, 382, 403). Direct evidence now also suggests that
(more in women than men), loss of trabecular thickness estrogen is the major regulator of bone resorption and bone
(more in men than women), and a loss of connectivity (124, architecture in the aging male skeleton (121, 135).
Volume 13, January 2023 4367
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
Table 2 Selected Preclinical Mouse Models for Age-related Bone Loss
Modela Advantages Disadvantages
Physiological aging No bias as to inducers of bone loss Amount of bone loss varies with genetic background; bone
phenotype takes ≥24 mo to develop
Telomere dysfunction Based on the known cause of senescent cell induction; Must generate G3/G4 animals to see phenotype (i.e.,
human genetic conditions of telomere dysfunction result generations it takes to achieve telomere shortening and
is premature osteoporosis; best phenocopy of human dysfunction comparable to human telomeres)
senile osteoporosis; phenotype occurs in weeks to
several months in G3/G4 animals
Radiation Recapitulates human senile osteoporosis at the histological Predominately a p21 rather than p16 response that drives
level within weeks of focal radiation exposure to bone bone loss; makes assumption that the DDR drives bone
loss with aging
Senescent cell clearance p16 INK-ATTAC model or senolytic compounds ameliorate Genetic models are limited to clearance of p16 or p21
age-onset osteoporosis senescent cells; makes assumption that cellular
senescence is the major driver of age-related bone loss
a Notethat the murine skeleton continues growth after puberty and does not demonstrate osteonal remodeling of cortical bone. However, like
humans, mice show loss of trabecular bone, thinning of cortical bone, and greater cortical porosity with aging.
Abbreviations: G, generation; DDR, DNA damage response.
Models of Age-related Osteoporosis demonstrate that a genetic change is related causally to
age-related bone loss as it occurs physiologically in humans.
Preclinical (animal) models The role of Wrn and Terc genes on aging is well described
(74, 118, 278, 321). In a study by Brennan et al., Terc−/− and
Table 2 compares selected major preclinical mouse models
Wrn−/− Terc−/− mutations in mice caused a bone phenotype
for the study of age-related bone loss. Although many gene
very similar to that seen in age-related human osteoporosis,
knockouts have skeletal phenotypes, this does not necessar-
including osteoblast dysfunction (51).
ily indicate relevance to direct aging mechanisms. There is
Werner syndrome (WS) and dyskeratosis congenita are
strong evidence that the four murine models described below
genetic diseases of premature aging, exhibiting shortened
undergo bone loss by mechanisms that have been implicated
telomeres, and accelerated bone loss. In animals modeling
by primary aging processes.
these conditions, low BMD and age-related bone loss are
seen, as well as shortened osteoblast lifespan and impaired
Physiological aging osteoblast differentiation but with relatively intact osteoclast
Physiologically relevant animal models for age-related osteo- differentiation (336, 442). Furthermore, these models recapit-
porosis have been a challenge. Early models used mouse ulate major structural features of aging-related osteoporosis,
strains with low peak bone mass that developed osteoporosis including decreased trabecular and cortical bone volume as
naturally with older age (36, 64, 131, 279, 329, 409–411). well as increased cortical porosity. These findings were the
The limitation of this approach is that a long time is required first to strongly implicate replicative senescence of osteoblast
to develop characteristic features of bone aging. Other precursors as an important regulator in senile osteoporo-
strategies used ovariectomy, orchiectomy, or bone-marrow sis. Other studies in mice that eliminate only telomerase
ablation (205, 262, 299, 452, 470), which reduced the time reverse transcriptase (TERT) demonstrated low BMD with
to appearance of an osteoporotic phenotype. However, these reduced osteoblast differentiation but elevated osteoclasto-
models better recapitulate secondary causes of osteoporosis genesis (370). The pathway mediating impaired osteoblast
(e.g., sex-hormone deficiency) rather than primary age- differentiation appears to be increased p53/p21 expression
related bone loss. A comprehensive review of mouse models accompanied by cell cycle arrest, apoptosis, and diminished
for the study of bone aging and their appropriateness to Runx2 expression (442). Conversely, overexpression of
human physiologic skeletal aging illustrates the limitations telomerase in MSCs preserves osteogenic differentiation
and potential benefits intrinsic to each model (194). in vitro and promotes bone formation in vivo (160, 380, 465,
466).
Telomerase-based genetic models
Radiation models
Genetically based modification of animals that develop an
osteoporotic phenotype have been described (43, 189, 217, Ionizing radiation (IR) may impart significant energy that
258, 342, 402, 433), but the relevant issue here is how to produces DNA damage through the generation of free radicals
4368 Volume 13, January 2023
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Comprehensive Physiology Aging and Bone Metabolism
and ROS. Therapeutic IR (e.g., for primary or adjuvant cancer and older (i.e., postmenopausal) women also demonstrated
interventions) induces apoptosis, autophagy, or senescence age-related increases in p16INK4A and p21CIP1, as well
in normal and cancerous cells. It is still unknown if there is as a subset of SASP factors (123). Age-dependent increases
an IR threshold effect that differentiates among these cell in RANKL expression in mice have been associated with
fates. Cellular protective mechanisms counter small levels of cortical bone loss (331); however, osteoclast elimination does
IR using antioxidants, catalase, superoxide dismutase, glu- not substantially influence bone loss with aging (229).
tathione peroxidase, and reduced glutathione, but excessive or To evaluate the contribution of senescent cell burden and
cumulative doses of IR may overwhelm these mechanisms to the SASP to aging in general, several approaches have been
induce DNA damage (130). IR-induced single-strand breaks developed (334) and are applicable to bone aging. These
and double-strand breaks (DSBs) in the DNA produce a DNA include a genetic model with the INK-ATTAC transgene
damage response (DDR). The DDR produces a growth arrest containing a FKBPcaspase-8 fusion protein (which is lethal
and if the response is persistent, or with failure to repair to p16+ cells with administration of the drug AP20187) or
damaged DNA, causes an irreversible growth-arrested state a combination of senolytic compounds [i.e., dasatinib and
consistent with cellular senescence. IR-induced senescence is quercetin (D + Q)] that selectively kills senescent cells (127).
accompanied by p21CIP1 and p16INK4A expression and the Both approaches demonstrate partial clearance of senescent
senescence-associated secretory phenotype (SASP). Inter- osteocytes with resultant increases in bone mass, strength,
estingly, cells that express the senescence marker p16Ink4a and microarchitecture compared to control animals. These
but without a DDR do not have a SASP (358), strongly approaches also suppress bone resorption, preserve osteoblast
suggesting that the DDR, and not only the expression of number, and maintain trabecular and cortical bone forma-
senescent markers, is a requirement for induction of the tion (127). The JAK inhibitor (JAKi) ruxolitinib suppresses
complete senescence phenotype. components of the SASP, specifically IL-6, Il-8, and PAI-1
Of the six major DNA repair pathways, nonhomologous (457, 458), which are known to promote osteoclastogenesis
end-joining (NHEJ) secondary to DSBs and homologous and bone resorption (127). JAKi treatment of old mice was
recombination (HR), secondary to DSBs and indirect DNA roughly equivalent to outcomes achieved by the INK-ATTAC
damage effects of IR, are primarily responsible for IR- transgene and pharmacologic senolytics strategies, including
mediated cellular senescence. The DSB component, mediated lower osteoclast number with preserved osteoblast number
by ataxia telangiectasia mutated (ATM), leads to phosphory- (127). In vitro studies where senescent cell-conditioned
lation of γH2AX, and phosphorylated γH2AX then initiates media promotes osteoclastogenesis strongly suggest that
the recruitment of other DDR proteins, including Ku70 and SASP factors may, at least in part, contribute to age-related
DNA-PKC. Nuclear foci of γH2AX corresponds to sites of bone resorption (127).
DSBs, and resolution of DSBs depends on the levels of Ku70 Senescent bone cell types, including osteoprogenitors,
and DNA-PKC following IR. Survival of osteoprogenitors, osteoblasts, and osteocytes no doubt contribute to age-related
osteoblasts, and osteocytes after IR-induced bone damage changes in bone architecture (333, 335), however, the role
depends on stabilization of these proteins by activation of of other senescent cell types (i.e., myeloid-lineage cells)
the cAMP-WNT pathway or by suppression of proteasome- in aging bone tissue is less clear. The presence in vivo of
based degradation (71–73). Unresolved DNA damage in bone senescent osteocytes and osteoblasts and the maintenance
cells results in cellular senescence. Animal models of focal of bone fidelity with aging by clearance of senescent cells
radiation-induced bone damage demonstrate a phenotype provide compelling evidence that cellular senescence and
similar to age-related osteoporosis with the accumulation of the accompanying SASP play key roles in age-related osteo-
senescent cells in the bone microenvironment implicated as porosis (Figure 11). However, clearance of p16+ cells by
the causative etiology (70). another genetic model (i.e., p16-3MR mice), failed to demon-
strate rescue of aging bone features. Compared to studies in
INK-ATTAC mice (127), those in the p16-3MR model did
Models of senescent cell clearance
not eliminate senescent osteocytes but did clear senescent
Senescent cells and their SASP are present in the bone osteoclast progenitors (229). Removal of senescent osteoclast
microenvironment. They can be identified in mice by ele- progenitors did not affect bone microarchitecture of aged
vated p16Ink4a expression, dysfunctional telomeres, and/or p16-3MR mice, supporting that senescent osteocytes are the
the presence of senescence-associated distension of satellites important mediators of age-related bone loss. Superimposed
(SADS) in myeloid cells, B and T cells, osteoblast pro- on the deleterious contribution of senescent bone cells and
genitors, osteoblasts, and osteocytes (123). Although some their SASP, other pathways are likely to be involved in
SASP factors have been identified in osteoblast progenitors, age-related bone loss, including oxidative stress and DNA
osteoblasts, and B and T cells from older animals, myeloid damage linked to ROS (195). Less clear is whether ROS
cells, and osteocytes were the major cell types contributing and DNA damage are indirect influences on bone loss (i.e.,
to the SASP. With aging, mouse osteoprogenitors decline through induction of cellular senescence) or if they mediate
more than half and show markers of DNA damage, increased their effects directly on bone tissue. A similar relationship
p21Cip1, and a SASP (230). Bone biopsies from young may exist in the case of vitamin D insufficiency and its
Volume 13, January 2023 4369
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
association with senescence-associated, age-related bone loss
(339, 459).
HSCs
SASP ?
Accelerated human aging paradigms
Adipocytes BMSC Premature ovarian failure
SASP
In a study limited to females who had bilateral oophorectomy
Osteoclast
at young ages, Rocca et al. (356) demonstrated an elevated
precursors likelihood for 18 conditions associated with age-onset co-
Myeloid cells
morbidities (except cancer). For eight of these conditions,
Senolytics the increased risk was significant and included depression,
SASP modulators SASP
hyperlipidemia, cardiac arrhythmias, coronary artery disease,
Osteoclasts Uncoupling arthritis, asthma, chronic obstructive pulmonary disease,
Senescent
and osteoporosis. After adjustments for social, behavioral,
osteoblasts demographic, and other factors such as age, females who
Aging bone
underwent early oophorectomy developed precocious accu-
mulation of multimorbidity most likely to occur during the
first 6 years after oophorectomy and independent of surgical
Osteocytes Senescent
osteocytes Empty lacunae indication for oophorectomy.
The increased risk for osteoporosis may be related to
P38/
estrogen withdrawal, the increased risk of other conditions
JAK/
STAT mTOR GATA4
associated with osteoporosis (e.g., arthritis), or the increased
risk for a heightened inflammatory state (323, 356, 357).
NF-κB
SASP gene activation
DDR Survivors of childhood cancer
DNA damage
Features of premature aging occur in cancer survivors, includ-
SASP
ing multimorbidity (e.g., secondary cancers, frailty, chronic
Telomere DDR
conditions, cognitive decline), impacting long-term health
dysfunction
p53
outcomes, and quality of life (173, 443). Possible explana-
p16
tions for chemo- and radio- therapy induced precocious aging
p21
have been put forward, implicating telomere dysfunction,
Cyclin D
CDK4/6 Cyclin E cellular senescence, reduced stem cell proliferation, DNA
CDK2
damage, and the DDR, as well as epigenetic phenomena
RB
(443). Estimation of biological age has been proposed in lieu
of chronologic age as the better measure in cancer survivors,
to predict the risk of conditions of accelerated aging, evaluate
Epigenetic modifications
Proteostasis
Mitochondrial dysfunction Dysregulation by miRNAs treatment effects and optimize treatment efficacy.
Nuclear reorganization
In a study of breast cancer survivors without baseline
Figure 11 Cellular senescence in bone aging. Aging disrupts homeo- differences in comorbidities or inflammatory cytokines com-
static processes in bone, causing increased osteoclast resorption and pared to control subjects, cancer survivors had significantly
reduced bone formation and mineralization by osteoblasts. Bone MSCs higher levels of inflammatory cytokines and multimorbidity
(bMSC) produce a reduced number of osteoblasts and preferentially over time (13). In the same study, those survivors treated
undergo adipogenic differentiation. Loss of osteocyte connectivity and
disruption of the canalicular network accompanies osteocyte death and with chemotherapy, surgery, and radiation, acquired more
the accumulation of empty lacunae. Activation of osteoclasts promotes comorbidities and inflammation-associated pain compared to
resorption, leading to bone loss. Senescent osteocytes are prominent in the control group.
the aging bone microenvironment. Important drivers of cellular senes-
cence, in general, include telomere dysfunction and a DDR that induces Among childhood cancer survivors, attainment of peak
cell cycle arrest mediated by p16Ink4a or p21, with subsequent sup- bone mass may be less likely due to cancer treatments, sub-
pression of Cyclin D, CDK4/6, Cyclin E, and CDK2. Activation of NF-κB optimal nutrition or nutritional deficiencies, and less physical
promotes the transcription of pro-inflammatory SASP factors. Mitochon-
drial dysfunction, disruption of protein homeostasis (i.e., proteosta- activity (i.e., less skeletal loading). Early failures to acquire
sis), chromatin modifications, miRNA-regulation of senescence-related adequate BMD during the formative years place survivors
genes, and alterations of the nuclear lamina are among the typical at increased risk for premature osteoporosis and fractures at
features of cellular senescence. Senolytic compounds and senomorphic
agents target senescent cells and the SASP, respectively. Figure is cour- younger ages (432, 451). For example, substantial bone loss
tesy of Abhishek Chandra, PhD, Mayo Clinic College of Medicine. has been reported across the early life span of ALL survivors,
at the time of diagnosis, during therapy, and for decades
posttreatment (164).
4370 Volume 13, January 2023
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Comprehensive Physiology Aging and Bone Metabolism
Immobilization special case of replicative senescence and reflected in culture
as a limited proliferative life span (169, 170). Inducers of
Weight-bearing activities are required for the maintenance cellular senescence include telomere dysfunction/uncapping,
and accrual of BMD and it is well established that lack DNA damage, chromatin alterations, ROS, inappropriate
of physical forces on the skeleton, either by microgravity growth-promoting pathways, and oncogenes among others
or mechanical unloading, accelerates rapid bone loss and (265, 313, 445). Hallmarks of cellular senescence include cell
osteoporosis (4, 77, 94, 240, 408). One study in young indi- cycle arrest, morphologic and functional changes, continued
viduals showed that short-term bed rest on the order of about metabolic activity, apoptosis resistance through senescent
3 weeks resulted in loss of BMD in the lumbar spine and cell antiapoptotic pathways (SCAPs), and the SASP (40, 61,
metacarpal bones by almost 5% and 4%, respectively (310). 99, 230, 233, 416, 440). Characteristic features of cellular
Older adults are particularly prone to prolonged immobility senescence are detailed in Table 3.
secondary to reduced physical activity and weight-bearing In senescence, cell cycle arrest is mainly mediated via
exercise. Immobilization from protracted bed rest (i.e., after two mechanisms: the ATM/p53/p21CIP1 and p16INK4a/
orthopedic injuries, cerebral vascular accident, or systemic retinoblastoma (Rb) signaling pathways. For example, induc-
illness), arthritic pain, fear of falling, or neglect leads to accel- tion of senescence by DNA damage causes kinases such
erated osteoclast-mediated bone resorption and lower bone as ATM to phosphorylate and stabilize p53, upregulating
formation. Unloading of the skeleton decreases osteoblast the expression of the cyclin-dependent kinase inhibitor
recruitment and proliferation; conversely, bed rest results in p21CIP1 and promoting cell cycle arrest (114, 390). In
the accumulation of osteoclasts (408, 424, 425, 438). another example, signaling by ERK and MAPK increases
Studies on rapid bone loss due to weightlessness in zero p16INK4a inhibition of CDK4 and CDK6 leading to phos-
gravity demonstrate immediate elevations in urinary calcium phorylation of Rb and blocking cell cycle progression near
levels with negative calcium balance and an average 1% to 2% G1/S (11, 165). Expression of p16INK4a increases in aging
loss of BMD with each month in space (38). The lumbar ver- cells and tissues and has been used as an aging biomarker
tebrae and legs were the most common locations in astronauts (242). Some evidence suggests that p21CIP1 is important
to be most significantly affected by bone loss (38). for establishing senescence while p16INK4a maintains the
Urinary calcium increases with bed rest and SCI, with net phenotype (390).
calcium imbalance occurring within days, peaking within The roles of p16INK4a and p21CIP1 in establishing and
weeks, and normalizing after 6 to 18 months (359). After maintaining the senescence phenotype are related to both the
normalization of calcium balance, as much as one-third of type of induction and the target cell type (84). It is notewor-
cortical bone and one-half of trabecular bone may be lost thy that cellular senescence is not restricted to proliferating
due to impaired muscle traction on bone and reduced gas- cells but can also be demonstrated in essentially postmitotic
trointestinal absorption of calcium (75, 359). Loss of BMD cells, such as osteocytes (123). The fates of differentiated
is persistent and cumulative (e.g., within 1 year of SCI, BMD and other cell types in response to various insults usually
loss in the femoral neck is 27% and in the distal femur 43%). converge on either senescence or apoptosis. These alternative
These losses continue, with over 50% demineralized bone in cell fates have important implications for tissue renewal
the hip and with about 20% in the upper extremities, 10 years and aging (150, 162). Although tissue repair occurs mostly
postinjury (4, 102, 232). Progression to fracture following through stem cell proliferation and differentiation, these
SCI can be as high as about 30% at 10 years postinjury (4, processes are adversely affected by senescence (421, 447)
102, 232). and result in dysfunctional cells and limited stem cell pools
In contrast, physical activity with sufficient exercise or that drive age-related pathologies.
mechanical loading increases BMD and reduces bone loss
(94, 133, 384). Physical activity and exercise at virtually
any age can still minimize loss or increase BMD and poten- Inducers of cellular senescence and downstream
tially reduce fracture risk with minimal therapeutic harm. pathways
In general, mechanical loading improves bone quality and Several mechanisms for the establishment and maintenance
quantity, especially when exercise strategies allow for ade- of cell senescence have been identified in bone (Figure 11).
quate rest periods between skeletal loads, limit loading cycles Based on knowledge of these pathways, the development of
to avoid bone desensitization, and incorporate low-level strain biomarkers that specifically or preferentially identify senes-
protocols (366, 389, 454). cent cells in hard tissue has also been pursued.
Telomeres are repetitive DNA sequences located at the
chromosome ends, whose length is maintained by the enzyme
Cellular Senescence and Apoptosis telomerase and whose termini are protected or capped by
a complex of proteins. In most somatic cells telomerase
Hallmarks of cellular senescence is absent or diminished and so with each cell division
Cellular senescence was first described as an irreversible telomeres decrease in length, ultimately leading to critically
growth arrest of otherwise viable cells, now referred to as the short and uncapped telomeres (245). Recognition of these
Volume 13, January 2023 4371
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
Table 3 Hallmarks of Cellular Senescence
Hallmark Description
Cell cycle arrest First examined in proliferating cell types; arrest in late G1/S; senescence also demonstrated in postmitotic cell types
Morphological changes Enlarged, flattened, and irregular shape; loss of heterochromatin; nuclear envelop changes (e.g., lamin B1);
decreased telomere length and telomere dysfunction; nucleolar modifications
Functional changes Decreased turnover mechanisms; altered proteostasis; modified lipid and glycoprotein plasma membrane components
Metabolic activity Mitochondrial alterations leading to increased ROS; lipofuscin accumulation; increased NF-𝜅B signaling (i.e.,
inflammatory response)
Apoptosis resistance SCAPs: ephrins/dependence receptors, PI3K/AKT, Bcl-2 (Bcl-xl, Bcl-2, Bcl-w), p53/FOXO4/p21/Serpine (PAI-1&2),
HIF-1α
SASP Signaling factors (e.g., cytokines); proteases (e.g., MMPs); ECM proteins; nonprotein constituents; extracellular
vesicles
Abbreviations: G, gap; S, DNA synthesis; ROS, reactive oxygen species; SCAP, senescent cell apoptosis-resistance pathways; MMPs, matrix
metalloproteinases; SASP, senescence-associated secretory phenotype; ECM, extracellular matrix.
dysfunctional telomeres as double-stranded breaks activates Nucleosome remodeling with aging is reflected by the
the DDR (93), and through the actions of p53/p21CIP1 and complement of histones as well as histone modifications or
p16INK4a facilitates cell cycle withdrawal and transition marks. Overall, there is a net loss of histones with aging,
to the senescent state (29). So-called telomere dysfunction- with changes in the amount of histone variants, their loca-
induced foci (TIFs), detected by the colocalization of DDR tion, and their modifications by methylation, acetylation,
proteins to telomeric DNA, serve as a marker for senescent and phosphorylation (206). There tends to be an increase in
cells and are related to both proliferative and differentiative activating histone marks (e.g., H3K4me3) and a decrease in
capabilities of MSCs and other bone cell types (123, 442). repressive marks (e.g., like H3K9me3) (31); however, these
Interestingly, osteocytes, like muscle cells and neurons, trends are complicated by heterogeneity even among cells
may undergo telomere dysfunction even though they are from the same donor or monozygotic twins (82). MSC studies
postmitotic (324). suggest that heterochromatin dysfunction is associated with
A DDR ensues as the result of exposure to ultraviolet and cellular senescence. In WS progeria, for example, where
IR, as well as ROS and metabolic byproducts. Like telomere mutations are found in the highly conserved helicase (WRN)
dysfunction, the DDR activated by radiation and ROS is involved in DNA repair and telomere maintenance (244,
mediated by stabilization of p53 and cell cycle arrest through 266), MSCs demonstrate premature replicative senescence,
p21CIP1 (114) and secondarily through p16INK4a (123, telomere shortening, DNA damage, and alterations in the
355). Unrepaired DNA damage induces cellular senescence repressive H3K9me3 mark (471).
(200). Concomitant upregulation of the zinc finger transcrip- In another example, the polycomb group (PcG) proteins
tion factor GATA4 stimulates NF-𝜅B and the SASP, further bind to target genes, recruiting EZH2 methyltransferase
reinforcing the senescent state (207). Studies in mice confirm that marks target histones like H3K27me3 (388). EZH2
that DNA damage-induced senescence limit osteoprogenitor methyltransferase plays a role in the regulation of osteoge-
cells and osteoblasts, promote osteoclastogenesis through nesis and bone development (107–109, 172). Conversely,
the SASP, and confer a bone loss phenotype consistent with JMJD3 demethylase unmarks or demethylates H3K27me3,
osteoporosis (78, 230). decreasing PcG complex binding and then resulting in
The loss of heterochromatin with aging has been well- increased p16INK4A expression and senescence (6, 50).
documented across species, including the normally hete- Taken together, these studies illustrate the importance of het-
rochromatic telomere and pericentromeric regions (206). erochromatin alterations in senescence and their association
In senescent cells, new regions of heterochromatin called with limiting MSC pools during bone aging.
senescence-associated heterochromatic foci (SAHF) (291, DNA methylation tends to decrease with aging. In the case
379), are transcriptionally inactive and may facilitate cell of age-related low BMD, for example, Alu hypomethyla-
cycle arrest in some cell types through p16-pathway activation tion was previously demonstrated (198). MSC aging is also
(105, 254, 306, 373, 379). Another chromatin alteration found accompanied by decreased DNA methyltransferases DMNT-
in senescent cells is SADS, which represents uncoiled peri- 1 and DNMT3B expression with concomitant induction of
centromeric satellite heterochromatin. In contrast to SAHF, cell senescence (264, 386). There is an inverse relationship
SADS are not exclusive to either p16Ink4a or p21Cip1 between loss of DMNTs and expression of p16INK4A
pathway activation (180, 383). and p21CIP1 (386). In contrast, increased methylation of
4372 Volume 13, January 2023
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Comprehensive Physiology Aging and Bone Metabolism
promoter-associated CpG islands occurs in genes important promoter by DNA methyltransferase-1 (464). Two miRNAs
for differentiation, cell-type-specific functions, and transcrip- may be involved in MSC fate switching between osteogenesis
tion factors (31, 467) and hypermethylation at CpG sites and adipogenesis or senescence. Downregulation of histone
in MSCs correspond to homeobox family genes related to deacetylase 9 and RPTOR-independent companion of MTOR
differentiation and expression of Runx2 and DLX5, important by the miR-188 complex causes bone loss and fat accumu-
transcription factors for osteogenesis (44). lation (259); miR-363-3p targeted TNF receptor-associated
Mapping of DNA methylation patterns has led to the factor 3 has a similar effect (439). miRNA levels may also
construction of “epigenetic clocks,” in different aging tissues. be useful as biomarkers for osteoporosis (260, 284), with a
Femoral head samples from older women with osteoporosis direct association between miR-29b-3p and bone formation
and osteoarthritis demonstrated that overall methylation (129) where lower levels predict bone fragility, fracture, and
levels at CpG loci were well correlated between the two increased bone turnover in postmenopausal women (237).
conditions (298). However, unique methylation sites linked Downregulation of retinoic acid receptor-related orphan
to cell differentiation and osteogenesis were identified in receptor β (Rorbeta, Rorb) by miR-219a-5p may be another
osteoporotic versus osteoarthritic groups (97). DNA methy- example. Rorb is highly upregulated in aged murine and
lation status as a predictor for osteoporosis also appears to human bone samples and downregulated with osteogenesis,
be very sensitive to the choice of tissue for analysis, with suggesting that miR-219a-5p could be used as a biomarker
bone rather than blood being the much better source from for age-related bone loss (19).
which to make predictions about skeletal aging (132). Chro- Senescent cells have a modified secretome or SASP that
matin modifying enzymes, such as HAT1, KAT5, HDAC6, is composed of signaling factors (e.g., cytokines), proteases
MBD1, and DNMT3A, were all downregulated in a study on (e.g., matrix metalloproteases), extracellular matrix pro-
postmenopausal osteoporosis (435); however, a comparable teins, nonprotein constituents (e.g., ROS), and extracellular
study with age-related osteoporosis is lacking, making it vesicles, some of which contain miRNAs (45, 92). The
uncertain if these changes in epigenetic enzymes in post- specific repertoire of SASP factors varies based on the cell
menopausal women are primarily due to estrogen loss or
type, derivation from cells early or late after the onset of
aging per se.
senescence (96, 176, 270), and type of senescence induction.
At low levels, ROS promote osteoclast differentiation and
The SASP has paracrine and endocrine effects that benefi-
bone resorption in a physiological manner and in balance with
cially (e.g., wound healing, tumor suppression) or negatively
antioxidants (104). Conversely, when ROS levels increase
impacts physiological processes (5, 98, 246, 303, 341, 393).
with aging, they can accelerate cell death in osteoblasts and
In a younger organism, senescent cells are cleared by the
osteocytes and the destruction of bone tissue by increasing
immune system and may promote tissue regeneration through
osteoclast differentiation and activity (7). Human studies
increased stemness of cells in the local microenvironment
confirm the relationships between increases in ROS (or
(300, 352). Transient senescent cells that confer benefit may
decreases in antioxidant levels) and increases in osteoclast
activity, decreases in osteoblast activity, both with aging later mediate deleterious effects as they accumulate with
and with osteoporosis (15, 104, 474). Osteoclasts, due to aging, probably related to chronic production of SASP fac-
their energy requirements for acid production and resorption, tors, especially inflammatory cytokines (140). Longer-term
have abundant mitochondria and NADPH oxidases that are exposure to SASP components can inhibit proliferation and
important sources of ROS. In murine osteoclasts expressing promote senescence and dedifferentiation locally, block
a mitochondria-targeted catalase, decreases in osteoclast tissue regeneration, and confer protumorigenic effects in
formation and survival, as well as elevated BMD, were precancerous cells. That the effects of aging and radiation
observed (27). Mitochondrial defects accumulate with age exposure in bone tissue can be prevented pharmacologically
and drive a senescence phenotype through a complex inter- with drugs that clear senescent cells, or normalize the SASP,
play of mitochondrial dysfunction/ROS production, telomere strongly implicates cellular senescence as a major contributor
shortening, and the DDR, eventually causing disruption of to age-related osteoporosis.
bone and stem cell functions (431). However, in assessing the roles of estrogen deficiency
There are several lines of evidence that suggest an impor- in aging and osteoporosis, there appear to be independent
tant role for micro (mi) RNA regulation of senescence and functions for estrogen that do not overlap with cellular
bone remodeling. Ablation of the RNase III family endori- senescence-related bone loss (126). For example, short-term
bonuclease Dicer, necessary in the maturation process of estrogen therapy in human females fails to affect senescence
many miRNAs, is induced by a senescent state (301). Levels biomarkers or SASP factors (126). In mice, the genetic clear-
of miRNA-195, which targets the 3′ untranslated region ance of p16-positive senescent cells ameliorated age-related
of TERT, become elevated with aging (312). Interestingly, bone loss (127) but did not mitigate ovariectomy-induced
overexpression of miR-195 promotes cell senescence of osteoporosis (126). Additional studies are required to better
MSCs, but its knockdown increases TERT expression and appreciate the associations between gonadal sex hormone
telomere re-lengthening (312). Upregulation of miR-140-3p deficiencies and mechanisms related to cell senescence,
and miR-126 by TNFα relieves inhibition of the RANKL particularly in clinical investigations.
Volume 13, January 2023 4373
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
Muscle-Bone Interactions
Bone loading
Beyond the well-known mechanical interactions between Myogenesis PGE2
Osteocytes
muscle and bone, both tissues likely serve as endocrine, Muscle mass WNTs 3a, 1
Exercise adaptation Osteocalcin
or at least as secretory tissues, that regulate metabolism Muscle Bone Bone
reciprocally in their own systems and with effects on other resorption
physiological systems. The communication between muscle RANKL
Ocyt factor
Aging
and bone appears to be mediated by contraction or load- TGFβ
ing. Myocytes and osteocytes, respectively, may serve as
the predominant “endocrine” cells that produce soluble
factors mediating the crosstalk between muscle and bone. Contraction
Such muscle factors have been identified and include myo-
OC differentiation
statin, irisin, and β-aminoisobutyric acid (BAIBA), a muscle
IL-7 OC activation
metabolite; in bone, soluble factors include osteocalcin, OC recruitment
Myocytes IL-6
transforming growth factor beta (TGFβ), prostaglandin E2
(PGE2), and Wnts. Although these factors may have opposite Myostatin OB differentiation
effects on the complementary tissue, they may be unified by Irisin Bone formation
mediating the beneficial effects of exercise or mechanical BAIBA Ocyt cell death
loading. Empirical evidence supports this hypothesis since BDNF VEGF by OBs
sarcopenia and osteoporosis are delayed or improved by IL-15 Bony matrix formation
exercise and these conditions are often found in the same
individuals (292). Figure 12 Possible age-related changes in muscle-bone interactions.
Factors with beneficial effects are secreted in response to muscle con-
Signaling from muscle tissue has important effects on traction and skeletal loading. RANKL and TGFβ, released during the
bone. For example, myostatin deletion causes animals to have resorptive phase of bone remodeling, have negative effects on muscle,
hypertrophied muscles and enlarged bones. Myostatin also while detrimental effects on both muscle and bone are mediated by myo-
statin. IL-7, IL6, and myostatin contribute to osteoclast differentiation,
inhibits osteoblast differentiation and promotes osteoclast recruitment, and activation, which in turn increases bone resorption.
activation (55). Irisin may facilitate or antagonize bone Dashed lines (- - -) indicate putative age-related changes.
formation (228). BAIBA may limit osteocyte cell death,
preserving both bone and muscle tissue (234). Other factors
that mediate muscle-to-bone crosstalk include brain-derived Exercise
neurotrophic factor (BDNF), which regulates VEGF secre- Genetic BMD
predisposition
tion by osteoblasts (472), IL-6, which recruits osteoclasts Zoledronate
(247), IL-15, which facilitates bony matrix formation (267),
and IL-7, which accelerates osteoclast differentiation (449).
Mortality
Signaling from bone tissue likewise has important effects
Disability Zoledronate
on muscle. Primary osteocytes and MLO-Y4 cells can pro- Fractures
mote C2C12 myoblast differentiation into myotubes (293).
PGE2 is an osteocyte secreted factor that acts as a mimetic Figure 13 Resilience to age-related bone loss confers health and life
to promote myogenesis (294). Wnt factor 3a can promote span advantages. Maintenance of BMD through exercise, genetic pre-
C2C12 differentiation (185). Osteocalcin has beneficial disposition, and/or zoledronate is associated with decreased mortality,
disability, and fractures. Zoledronate, independent of its effects on frac-
pleiotropic effects on muscle mass, function, and exercise ture reduction confers a mortality advantage.
adaptation (285, 376). TGFβ release associated with cancer
metastasis can accelerate muscle weakness (444). RANKL is
inhibitory to accumulation of muscle mass (46, 110). Finally, of age-related osteoporosis and the importance of systems
osteocytes produce unknown factors that potentially mediate biology in geriatric syndromes.
sarcopenia and muscle dysfunction with aging (157).
In summary, factors secreted by muscle and bone have both
positive and negative effects on these complementary tissues Resilience to age-onset bone loss
and probably other tissues. Putative aging-related changes There is growing evidence to suggest that resiliency, or
in muscle-bone interactions may influence sarcopenia and protection against stressors and age-related declines, plays
osteoporosis (Figure 12). Factors with beneficial effects are a key role in conferring successful aging. Resilience to
secreted in response to muscle contraction and skeletal load- specific age-onset disease exists and can be used to identify
ing. RANKL and TGFβ, released during the resorptive phase environmental and genetic factors that confer health span and
of bone remodeling, have negative effects on muscle, while life span benefits. The paradigm of resilience to age-related
detrimental effects on both muscle and bone are mediated bone loss lends itself to this hypothesis (Figure 13). Overall,
by myostatin. These findings add to the multifactorial nature data suggest that faster bone loss over time is associated
4374 Volume 13, January 2023
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Comprehensive Physiology Aging and Bone Metabolism
with mortality risk (273). Older women who maintain their activities of daily living. As a case in point, approximately
BMD experience a lower risk of fractures, disability, and 20% of patients with hip fractures require institutionaliza-
mortality, suggesting that this phenotype may be a marker of tion. Conversely, individuals who maintain BMD do not
successful aging (66). It follows that there may be a subset suffer these consequences and have a substantial mortality
of individuals who have resistance against bone aging, as benefit. Structurally, endocortical resorption with partly
defined by their much greater than expected BMD for their compensatory periosteal apposition produces an outward
age. This is suggested by empirical data where BMD rather cortical displacement with aging, manifesting as decreased
than age remains a very strong predictor of hip fracture even cortical thickness and area. Other cortical bone compromise
at 25 years postbaseline measurements (39). It should be is due to increased cortical porosity, trabecularization, and
possible then, using high-resolution imaging, to ascertain heterogeneity of mineralized bone. Together, these changes
which bone microarchitectural features confer bone strength occur more prominently in women. Loss of trabecular bone
in individuals with resistance to bone aging. These features with increased trabecular spacing is typical in older women;
likely contribute to fracture prevention and consequently thinning of trabecular bone rather than trabecular bone loss
reduce the risk of morbidity and mortality due to fracture and occurs in older men.
perhaps other etiologies. With aging, there are alterations in bone microarchitecture
Those with exceptional BMD will also likely demonstrate and metabolism that promote a higher risk of fracture. Age-
gains in health span and survival. It has been proposed related bone loss is multifactorial, with contributions from
that grip strength is a marker for overall frailty and general genetic and nonhereditary determinants of bone strength,
health and for the adequacy of skeletal loading. In older medical conditions, prescription drugs, estrogen deficiency,
women, regression analysis stratified by exercise indicate secondary hyperparathyroidism, microenvironmental and
that only those who exercise have significant associations cellular changes in bone, and skeletal unloading. At the
of grip strength with BMD and in this cohort grip strength cellular level, there are alterations in bone and marrow cel-
was an independent indicator of general BMD (243). Low lularity, lineage switching to an adipogenic fate, failure to
grip strength in women is associated with low BMD at both adequately transduce mechanical signals, and accumulation
the spine and hip and an increased risk of incident vertebral of senescent cells with production of a SASP. Genetic and
fracture independent of differences in body size or lifestyle molecular approaches have led to the identification of impor-
(103). In men, grip strength appears to be predictive of site tant pathways that mediate aging-related changes in bone,
specific rather than systemic BMD. Thus, surrogate markers, including the RANK-RANKL-OPG pathway and the Wnt-
including grip strength, could be used to assess health span β-catenin pathway that reciprocally regulate bone resorption
in individuals with exceptional BMD. Conversely, preserved and formation, respectively. These aging changes result in
BMD could predict health benefits in disease states, such as the uncoupling of bone resorption from bone formation
diabetes, and perhaps result in a mortality advantage. In a and cause remodeling abnormalities that ultimately lead to
longitudinal study, lower baseline areal BMD in the radius bone deterioration more commonly found in older adults.
was associated with increased all-cause mortality in women The aging skeleton also has important interactions with other
with type 2 diabetes, but not men, independent of other risk systems, most notably the hematopoietic and muscle systems.
factors for death (252). Increasing knowledge of aging bone physiology has lent itself
The identification of environmental factors and genetic fac- to the identification of therapeutic targets and translation of
tors that influence bone mass and longevity may provide a new interventions for the prevention and treatment of age-
roadmap for the development of new drugs and other inter- related osteoporosis. Notable therapeutic interventions based
ventions that target both low bone mass and primary aging. on preclinical studies include the use of senotherapeutic
A corollary of this strategy is that interventions which main- drugs, so-called senolytic compounds that clear senescent
tain or improve system-specific function, such as preservation cells, and senomodulators, agents that normalize the SASP.
of BMD, will also improve health span and/or life span. In Open questions remain regarding various aspects of aging
fact, at least one medication used for the treatment of bone bone physiology. Many of the relationships among bony
loss (zoledronate) conveys a mortality benefit independent of matrix alterations and bone quality are not well-established
preventing fracture, as well as an extension of life span in and are quite speculative as due primarily versus secondarily
an animal model of accelerated aging (90, 429). Also, zole- to aging per se and/or the contribution of disease states. All
dronate was able to extend the lifespan of human mesenchy- preclinical models of age-related bone loss have limitations
mal stem cells by protecting against the accumulation of DNA and a bone loss phenotype does not necessarily recapitulate
damage, an important mechanism of cell aging, and preserv- cellular and molecular mechanisms employed during physio-
ing their ability to proliferate and differentiate in vitro (290).
logical aging in either rodents or humans. In the development
of new models, targeting of already well-established aging
Conclusion mechanisms is likely to be superior to identifying or selecting
for an osteoporosis phenotype which may or may not be
The functional impact of osteoporosis-related fracture can be relevant to aging. The area of muscle-bone crosstalk remains
devastating, with impairments in basic as well as instrumental ripe for discovering common or complementary pathways
Volume 13, January 2023 4375
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
related to bone loss and sarcopenia with aging. Finally, the 13. Alfano CM, Peng J, Andridge RR, Lindgren ME, Povoski SP, Lipari
AM, Agnese DM, Farrar WB, Yee LD, Carson WE 3rd, Kiecolt-Glaser
promise of senotherapeutic agents as a new approach to JK. Inflammatory cytokines and comorbidity development in breast
age-onset bone loss awaits careful translation to human trials, cancer survivors versus noncancer controls: Evidence for accelerated
aging? J Clin Oncol 35: 149-156, 2017.
either as a stand-alone therapy or as combination treatment 14. Almeida M. Aging mechanisms in bone. Bonekey Rep 1: 102, 2012.
with existing therapies. 15. Altindag O, Erel O, Soran N, Celik H, Selek S. Total oxidative/anti-
oxidative status and relation to bone mineral density in osteoporosis.
Rheumatol Int 28: 317-321, 2008.
16. Amin S, Felson DT. Osteoporosis in men. Rheum Dis Clin N Am 27:
19-47, 2001.
Related Articles 17. Ammann P, Rizzoli R, Bonjour JP, Bourrin S, Meyer JM, Vassalli P,
Garcia I. Transgenic mice expressing soluble tumor necrosis factor-
receptor are protected against bone loss caused by estrogen deficiency.
Roles of Parathyroid Hormone and Parathyroid Hormone– J Clin Invest 99: 1699-1703, 1997.
Related Peptide in Calcium Metabolism and Bone Biology: 18. Andrew T, Antioniades L, Scurrah KJ, Macgregor AJ, Spector TD. Risk
of wrist fracture in women is heritable and is influenced by genes that
Biological Actions and Receptors are largely independent of those influencing BMD. J Bone Miner Res
Vitamin D Endocrine System and Calcium and Phosphorus 20: 67-74, 2005.
19. Aquino-Martinez R, Farr JN, Weivoda MM, Negley BA, Onken JL,
Homeostasis Thicke BS, Fulcer MM, Fraser DG, van Wijnen AJ, Khosla S, Monroe
Kidney and Bone: Physiological and Pathophysiological DG. miR-219a-5p regulates rorbeta during osteoblast differentiation
and in age-related bone loss. J Bone Miner Res 34: 135-144, 2019.
Relationships 20. Arnaud CD. Hyperparathyroidism and renal failure. Kidney Int 4:
89-95, 1973.
21. Ashique AM, Hart LS, Thomas CDL, Clement JG, Pivonka P, Carter Y,
Mousseau DD, Cooper DML. Lacunar-canalicular network in femoral
cortical bone is reduced in aged women and is predominantly due to a
Acknowledgements loss of canalicular porosity. Bone Rep 7: 9-16, 2017.
22. Bafico A, Liu G, Yaniv A, Gazit A, Aaronson SA. Novel mechanism
This work was supported by the Robert and Arlene Kogod of Wnt signalling inhibition mediated by Dickkopf-1 interaction with
LRP6/Arrow. Nat Cell Biol 3: 683-686, 2001.
Professorship, National Institutes of Health/National Institute 23. Balasubramanian A, Zhang J, Chen L, Wenkert D, Daigle SG, Grauer
on Aging P01 AG062413, and R25 AG073119-01. The author A, Curtis JR. Risk of subsequent fracture after prior fracture among
older women. Osteoporos Int 30: 79-92, 2019.
has nothing to disclose. 24. Bannwarth B. Drug-induced musculoskeletal disorders. Drug Saf 30:
27-46, 2007.
25. Bardin T. Musculoskeletal manifestations of chronic renal failure. Curr
Opin Rheumatol 15: 48-54, 2003.
References 26. Barrett-Connor E, Siris ES, Wehren LE, Miller PD, Abbott TA, Berger
ML, Santora AC, Sherwood LM. Osteoporosis and fracture risk in
1. Aaron JE, Makins NB, Sagreiya K. The microanatomy of trabecular women of different ethnic groups. J Bone Miner Res 20: 185-194,
bone loss in normal aging men and women. Clin Orthop Relat Res 215: 2005.
260-271, 1987. 27. Bartell SM, Kim HN, Ambrogini E, Han L, Iyer S, Serra Ucer S,
2. Abdallah BM, Haack-Sørensen M, Fink T, Kassem M. Inhibition of Rabinovitch P, Jilka RL, Weinstein RS, Zhao H, O’Brien CA, Manola-
osteoblast differentiation but not adipocyte differentiation of mes- gas SC, Almeida M. FoxO proteins restrain osteoclastogenesis and
enchymal stem cells by sera obtained from aged females. Bone 39: bone resorption by attenuating H2 O2 accumulation. Nat Commun 5:
181-188, 2006. 3773, 2014.
3. Abdallah BM, Kassem M. New factors controlling the balance between 28. Bauer RL, Deyo RA. Low risk of vertebral fracture in Mexican Amer-
osteoblastogenesis and adipogenesis. Bone 50: 540-545, 2012. ican women. Arch Intern Med 147: 1437-1439, 1987.
4. Abdelrahman S, Ireland A, Winter EM, Purcell M, Coupaud S. Osteo- 29. Baxter MA, Wynn RF, Jowitt SN, Wraith JE, Fairbairn LJ, Bellantuono
porosis after spinal cord injury: Aetiology, effects and therapeutic I. Study of telomere length reveals rapid aging of human marrow stro-
approaches. J Musculoskelet Neuronal Interact 21: 26-50, 2021. mal cells following in vitro expansion. Stem Cells 22: 675-682, 2004.
5. Acosta JC, O’Loghlen A, Banito A, Guijarro MV, Augert A, Raguz S, 30. Beekman KM, Veldhuis-Vlug AG, den Heijer M, Maas M, Oleksik
Fumagalli M, Da Costa M, Brown C, Popov N, Takatsu Y, Melamed J, AM, Tanck MW, Ott SM, van t’Hof RJ, Lips P, Bisschop PH, Braven-
d’Adda di Fagagna F, Bernard D, Hernando E, Gil J. Chemokine sig- boer N. The effect of raloxifene on bone marrow adipose tissue and
naling via the CXCR2 receptor reinforces senescence. Cell 133: 1006- bone turnover in postmenopausal women with osteoporosis. Bone 118:
1018, 2008. 62-68, 2019.
6. Agger K, Cloos PA, Rudkjaer L, Williams K, Andersen G, Christensen 31. Benayoun BA, Pollina EA, Brunet A. Epigenetic regulation of ageing:
J, Helin K. The H3K27me3 demethylase JMJD3 contributes to the Linking environmental inputs to genomic stability. Nat Rev Mol Cell
activation of the INK4A-ARF locus in response to oncogene- and Biol 16: 593-610, 2015.
stress-induced senescence. Genes Dev 23: 1171-1176, 2009. 32. Benito M, Gomberg B, Wehrli FW, Weening RH, Zemel B, Wright AC,
7. Agidigbi TS, Kim C. Reactive oxygen species in osteoclast differenti- Song HK, Cucchiara A, Snyder PJ. Deterioration of trabecular archi-
ation and possible pharmaceutical targets of ROS-mediated osteoclast tecture in hypogonadal men. J Clin Endocrinol Metab 88: 1497-1502,
diseases. Int J Mol Sci 20: 3576, 2019. 2003.
8. Ahmed LA, Nguyen ND, Bjornerem A, Joakimsen RM, Jorgensen L, 33. Bennett JH, Joyner CJ, Triffitt JT, Owen ME. Adipocytic cells cultured
Stormer J, Bliuc D, Center JR, Eisman JA, Nguyen TV, Emaus N. from marrow have osteogenic potential. J Cell Sci 99 (Pt1): 131-139,
External validation of the Garvan nomograms for predicting absolute 1991.
fracture risk: The Tromso study. PLoS One 9: e107695, 2014. 34. Bentler SE, Liu L, Obrizan M, Cook EA, Wright KB, Geweke JF,
9. Akune T, Ohba S, Kamekura S, Yamaguchi M, Chung UI, Kubota Chrischilles EA, Pavlik CE, Wallace RB, Ohsfeldt RL, Jones MP,
N, Terauchi Y, Harada Y, Azuma Y, Nakamura K, Kadowaki T, Rosenthal GE, Wolinsky FD. The aftermath of hip fracture: Discharge
Kawaguchi H. PPARgamma insufficiency enhances osteogenesis placement, functional status change, and mortality. Am J Epidemiol
through osteoblast formation from bone marrow progenitors. J Clin 170: 1290-1299, 2009.
Invest 113: 846-855, 2004. 35. Beresford JN, Bennettt JH, Devlin C, Leboyt PS, Owen ME. Evidence
10. Albright F, Smith PH, Richardson AM. Postmenopausal osteoporosis. for an inverse relationship between the differentiation of adipocytic and
J Am Med Assoc 116: 2465-2474, 1941. osteogenic cells in rat marrow stromal cell cultures. J Cell Sci 102: 341-
11. Alcorta DA, Xiong Y, Phelps D, Hannon G, Beach D, Barrett JC. 351, 1992.
Involvement of the cyclin-dependent kinase inhibitor p16 (INK4a) in 36. Bergman RJ, Gazit D, Kahn AJ, Gruber H, McDougall S, Hahn TJ.
replicative senescence of normal human fibroblasts. Proc Natl Acad Age-related changes in osteogenic stem cells in mice. J Bone Miner
Sci U S A 93: 13742-13747, 1996. Res 11: 568-577, 1996.
12. Alem AM, Sherrard DJ, Gillen DL, Weiss NS, Beresford SA, Heckbert 37. Bianco P, Riminucci M, Gronthos S, Robey PG. Bone marrow stromal
SR, Wong C, Stehman-Breen C. Increased risk of hip fracture among stem cells: Nature, biology, and potential applications. Stem Cells 19:
patients with end-stage renal disease. Kidney Int 58: 396-399, 2000. 180-192, 2001.
4376 Volume 13, January 2023
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Comprehensive Physiology Aging and Bone Metabolism
38. Bikle DD, Sakata T, Halloran BP. The impact of skeletal unloading on responsiveness to 1,25-dihydroxyvitamin D. J Biol Chem 277:
bone formation. Gravit Space Biol Bull 16: 45-54, 2003. 30337-30350, 2002.
39. Black DM, Cauley JA, Wagman R, Ensrud K, Fink HA, Hillier TA, Lui 63. Canalis E, Mazziotti G, Giustina A, Bilezikian JP. Glucocorticoid-
LY, Cummings SR, Schousboe JT, Napoli N. The ability of a single induced osteoporosis: Pathophysiology and therapy. Osteoporos Int
BMD and fracture history assessment to predict fracture over 25 years 18: 1319-1328, 2007.
in postmenopausal women: The study of osteoporotic fractures. J Bone 64. Cao J, Venton L, Sakata T, Halloran BP. Expression of RANKL and
Miner Res 33: 389-395, 2018. OPG correlates with age-related bone loss in male C57BL/6 mice.
40. Blagosklonny MV. Cell cycle arrest is not yet senescence, which is J Bone Miner Res 18: 270-277, 2003.
not just cell cycle arrest: Terminology for TOR-driven aging. Aging 65. Cauley JA, Cawthon PM, Peters KE, Cummings SR, Ensrud KE,
(Albany NY) 4: 159-165, 2012. Bauer DC, Taylor BC, Shikany JM, Hoffman AR, Lane NE, Kado
41. Bliuc D, Alarkawi D, Nguyen TV, Eisman JA, Center JR. Risk DM, Stefanick ML, Orwoll ES, Osteoporotic Fractures in Men Study
of subsequent fractures and mortality in elderly women and men Research Group. Risk factors for hip fracture in older men: The
with fragility fractures with and without osteoporotic bone density: osteoporotic fractures in men study (MrOS). J Bone Miner Res 31:
The Dubbo Osteoporosis Epidemiology Study. J Bone Miner Res 30: 1810-1819, 2016.
637-646, 2015. 66. Cauley JA, Lui LY, Barnes D, Ensrud KE, Zmuda JM, Hillier TA,
42. Bonafede M, Shi N, Barron R, Li X, Crittenden DB, Chandler D. Pre- Hochberg MC, Schwartz AV, Yaffe K, Cummings SR, Newman AB,
dicting imminent risk for fracture in patients aged 50 or older with SOF Research Group. Successful skeletal aging: A marker of low
osteoporosis using US claims data. Arch Osteoporos 11: 26, 2016. fracture risk and longevity. The study of osteoporotic fractures (SOF).
43. Bonyadi M, Waldman SD, Liu D, Aubin JE, Grynpas MD, Stanford J Bone Miner Res 24: 134-143, 2009.
WL. Mesenchymal progenitor self-renewal deficiency leads to age- 67. Center JR, Bliuc D, Nguyen TV, Eisman JA. Risk of subsequent frac-
dependent osteoporosis in Sca-1/Ly-6A null mice. Proc Natl Acad Sci ture after low-trauma fracture in men and women. JAMA 297: 387-394,
U S A 100: 5840-5845, 2003. 2007.
44. Bork S, Pfister S, Witt H, Horn P, Korn B, Ho AD, Wagner W. DNA 68. Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA. Mor-
methylation pattern changes upon long-term culture and aging of tality after all major types of osteoporotic fracture in men and women:
human mesenchymal stromal cells. Aging Cell 9: 54-63, 2010. An observational study. Lancet 353: 878-882, 1999.
45. Borodkina AV, Deryabin PI, Giukova AA, Nikolsky NN. “Social life” 69. Chalhoub D, Orwoll ES, Cawthon PM, Ensrud KE, Boudreau R,
of senescent cells: What is SASP and why study it? Acta Nat 10: 4-14, Greenspan S, Newman AB, Zmuda J, Bauer D, Cummings S, Cauley
2018. JA, Osteoporotic Fractures in Men Study Research Group. Areal and
46. Boulanger Piette A, Hamoudi D, Marcadet L, Morin F, Argaw A, Ward volumetric bone mineral density and risk of multiple types of fracture
L, Frenette J. Targeting the muscle-bone unit: Filling two needs with in older men. Bone 92: 100-106, 2016.
one deed in the treatment of duchenne muscular dystrophy. Curr Osteo- 70. Chandra A, Lagnado AB, Farr JN, Monroe DG, Park S, Hachfeld C,
poros Rep 16: 541-553, 2018. Tchkonia T, Kirkland JL, Khosla S, Passos JF, Pignolo RJ. Targeted
47. Bouxsein ML, Kaufman J, Tosi L, Cummings S, Lane J, Johnell O. reduction of senescent cell burden alleviates focal radiotherapy-related
Recommendations for optimal care of the fragility fracture patient bone loss. J Bone Miner Res 35: 1119-1131, 2020.
to reduce the risk of future fracture. J Am Acad Orthop Surg 12: 71. Chandra A, Lin T, Young T, Tong W, Ma X, Tseng WJ, Kramer I,
385-395, 2004. Kneissel M, Levine MA, Zhang Y, Cengel K, Liu XS, Qin L. Suppres-
48. Bow CH, Cheung E, Cheung CL, Xiao SM, Loong C, Soong C, Tan sion of sclerostin alleviates radiation-induced bone loss by protecting
KC, Luckey MM, Cauley JA, Fujiwara S, Kung AW. Ethnic difference bone-forming cells and their progenitors through distinct mechanisms.
of clinical vertebral fracture risk. Osteoporos Int 23: 879-885, 2012. J Bone Miner Res 32: 360-372, 2017.
49. Bowers RR, Lane MD. A role for bone morphogenetic protein-4 in 72. Chandra A, Lin T, Zhu J, Tong W, Huo Y, Jia H, Zhang Y, Liu XS,
adipocyte development. Cell Cycle 6: 385-389, 2007. Cengel K, Xia B, Qin L. PTH1-34 blocks radiation-induced osteoblast
50. Bracken AP, Kleine-Kohlbrecher D, Dietrich N, Pasini D, Gargiulo G, apoptosis by enhancing DNA repair through canonical Wnt pathway.
Beekman C, Theilgaard-Monch K, Minucci S, Porse BT, Marine JC,
Hansen KH, Helin K. The Polycomb group proteins bind throughout J Biol Chem 290: 157-167, 2015.
the INK4A-ARF locus and are disassociated in senescent cells. Genes 73. Chandra A, Rosenzweig A, Pignolo RJ. Osteobiology of aging. In: Pig-
Dev 21: 525-530, 2007. nolo R, Ahn J, editors. Fractures in the Elderly. Cham: Humana Press,
51. Brennan TA, Egan KP, Lindborg CM, Chen Q, Sweetwyne MT, 2018, p. 3-37.
Hankenson KD, Xie SX, Johnson FB, Pignolo RJ. Mouse models of 74. Chang S, Multani AS, Cabrera NG, Naylor ML, Laud P, Lombard D,
telomere dysfunction phenocopy skeletal changes found in human Pathak S, Guarente L, DePinho RA. Essential role of limiting telom-
age-related osteoporosis. Dis Model Mech 7: 583-592, 2014. eres in the pathogenesis of Werner syndrome. Nat Genet 36: 877-882,
52. Briot K, Fechtenbaum J, Roux C. Clinical relevance of vertebral frac- 2004.
tures in men. J Bone Miner Res 31: 1497-1499, 2016. 75. Chantraine A, Heynen G, Franchimont P. Bone metabolism, parathy-
53. Brockstedt H, Kassem M, Eriksen EF, Mosekilde L, Melsen F. Age- roid hormone, and calcitonin in paraplegia. Calcif Tissue Int 27: 199-
and sex-related changes in iliac cortical bone mass and remodeling. 204, 1979.
Bone 14: 681-691, 1993. 76. Charatcharoenwitthaya N, Khosla S, Atkinson EJ, McCready LK,
54. Broy SB, Cauley JA, Lewiecki ME, Schousboe JT, Shepherd JA, Riggs BL. Effect of blockade of TNF-alpha and interleukin-1 action
Leslie WD. Fracture risk prediction by non-BMD DXA measures: The on bone resorption in early postmenopausal women. J Bone Miner Res
2015 ISCD official positions part 1: Hip geometry. J Clin Densitom 22: 724-729, 2007.
18: 287-308, 2015. 77. Chen JS, Cameron ID, Cumming RG, Lord SR, March LM, Sambrook
55. Buehring B, Binkley N. Myostatin—the holy grail for muscle, bone, PN, Simpson JM, Seibel MJ. Effect of age-related chronic immobility
and fat? Curr Osteoporos Rep 11: 407-414, 2013. on markers of bone turnover. J Bone Miner Res 21: 324-331, 2005.
56. Burkhardt R, Kettner G, Böhm W, Schmidmeier M, Schlag R, Frisch 78. Chen Q, Liu K, Robinson AR, Clauson CL, Blair HC, Robbins PD,
B, Mallmann B, Eisenmenger W, Gilg T. Changes in trabecular bone, Niedernhofer LJ, Ouyang H. DNA damage drives accelerated bone
hematopoiesis and bone marrow vessels in aplastic anemia, primary aging via an NF-kappaB-dependent mechanism. J Bone Miner Res 28:
osteoporosis, and old age: A comparative histomorphometric study. 1214-1228, 2013.
Bone 8: 157-164, 1987. 79. Chen Q, Shou P, Zhang L, Xu C, Zheng C, Han Y, Li W, Huang Y,
57. Burr DB. Changes in bone matrix properties with aging. Bone 120: Zhang X, Shao C, Roberts AI, Rabson AB, Ren G, Zhang Y, Wang Y,
85-93, 2019. Denhardt DT, Shi Y. An osteopontin-integrin interaction plays a critical
58. Busse B, Djonic D, Milovanovic P, Hahn M, Puschel K, Ritchie role in directing adipogenesis and osteogenesis by mesenchymal stem
RO, Djuric M, Amling M. Decrease in the osteocyte lacunar density cells. Stem Cells 32: 327-337, 2014.
accompanied by hypermineralized lacunar occlusion reveals failure 80. Chen Y, Guo Y, Zhang X, Mei Y, Feng Y, Zhang X. Bone susceptibility
and delay of remodeling in aged human bone. Aging Cell 9: 1065-1075, mapping with MRI is an alternative and reliable biomarker of osteo-
2010. porosis in postmenopausal women. Eur Radiol 28: 5027-5034, 2018.
59. Cadarette SM, Jaglal SB, Kreiger N, McIsaac WJ, Darlington GA, Tu 81. Cheng SY, Levy AR, Lefaivre KA, Guy P, Kuramoto L, Sobolev B.
JV. Development and validation of the Osteoporosis Risk Assessment Geographic trends in incidence of hip fractures: A comprehensive
Instrument to facilitate selection of women for bone densitometry. literature review. Osteoporos Int 22: 2575-2586, 2011.
CMAJ 162: 1289-1294, 2000. 82. Cheung P, Vallania F, Warsinske HC, Donato M, Schaffert S, Chang
60. Cadarette SM, Jaglal SB, Murray TM, McIsaac WJ, Joseph L, Brown SE, Dvorak M, Dekker CL, Davis MM, Utz PJ, Khatri P, Kuo AJ.
JP. Evaluation of decision rules for referring women for bone densito- Single-cell chromatin modification profiling reveals increased epige-
metry by dual-energy X-ray absorptiometry. JAMA 286: 57-63, 2001. netic variations with aging. Cell 173: 1385-1397 e1314, 2018.
61. Campisi J. Senescent cells, tumor suppression, and organismal aging: 83. Chevalley T, Bonjour JP, van Rietbergen B, Ferrari S, Rizzoli R. Frac-
Good citizens, bad neighbors. Cell 120: 513-522, 2005. tures during childhood and adolescence in healthy boys: Relation with
62. Canaff L, Hendy GN. Human calcium-sensing receptor gene. Vitamin bone mass, microstructure, and strength. J Clin Endocrinol Metab 96:
D response elements in promoters p1 and p2 confer transcriptional 3134-3142, 2011.
Volume 13, January 2023 4377
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
84. Childs BG, Durik M, Baker DJ, van Deursen JM. Cellular senescence R, Westendorf JJ, van Wijnen AJ. Enhancer of zeste homolog 2 (Ezh2)
in aging and age-related disease: From mechanisms to therapy. Nat Med controls bone formation and cell cycle progression during osteogenesis
21: 1424-1435, 2015. in mice. J Biol Chem 293: 12894-12907, 2018.
85. Chow J, Tobias JH, Colston KW, Chambers TJ. Estrogen maintains 108. Dudakovic A, Camilleri ET, Riester SM, Paradise CR, Gluscevic M,
trabecular bone volume in rats not only by suppression of bone resorp- O’Toole TM, Thaler R, Evans JM, Yan H, Subramaniam M, Hawse JR,
tion but also by stimulation of bone formation. J Clin Invest 89: 74-78, Stein GS, Montecino MA, McGee-Lawrence ME, Westendorf JJ, van
1992. Wijnen AJ. Enhancer of zeste homolog 2 inhibition stimulates bone
86. Chung PL, Zhou S, Eslami B, Shen L, LeBoff MS, Glowacki J. Effect formation and mitigates bone loss caused by ovariectomy in skeletally
of age on regulation of human osteoclast differentiation. J Cell Biochem mature mice. J Biol Chem 291: 24594-24606, 2016.
115: 1412-1419, 2014. 109. Dudakovic A, Samsonraj RM, Paradise CR, Galeano-Garces C, Mol
87. Clark EM, Ness AR, Bishop NJ, Tobias JH. Association between bone MO, Galeano-Garces D, Zan P, Galvan ML, Hevesi M, Pichurin O,
mass and fractures in children: A prospective cohort study. J Bone Thaler R, Begun DL, Kloen P, Karperien M, Larson AN, Westendorf JJ,
Miner Res 21: 1489-1495, 2006. Cool SM, van Wijnen AJ. Inhibition of the epigenetic suppressor EZH2
88. Clark GR, Duncan EL. The genetics of osteoporosis. Br Med Bull 113: primes osteogenic differentiation mediated by BMP2. J Biol Chem 295:
73-81, 2015. 7877-7893, 2020.
89. Cohen A, Shane E. Osteoporosis after solid organ and bone marrow 110. Dufresne SS, Boulanger-Piette A, Bosse S, Argaw A, Hamoudi D,
transplantation. Osteoporos Int 14: 617-630, 2003. Marcadet L, Gamu D, Fajardo VA, Yagita H, Penninger JM, Russell
90. Colon-Emeric CS, Mesenbrink P, Lyles KW, Pieper CF, Boonen S, Tupling A, Frenette J. Genetic deletion of muscle RANK or selective
Delmas P, Eriksen EF, Magaziner J. Potential mediators of the mortal- inhibition of RANKL is not as effective as full-length OPG-fc in
ity reduction with zoledronic acid after hip fracture. J Bone Miner Res mitigating muscular dystrophy. Acta Neuropathol Commun 6: 31,
25: 91-97, 2010. 2018.
91. Compston JE. Mechanisms of bone loss and gain in untreated and 111. Duong LT, Pickarski M, Cusick T, Chen CM, Zhuo Y, Scott K, Samad-
treated osteoporosis. Endocrine 17: 21-27, 2002. fam R, Smith SY, Pennypacker BL. Effects of long term treatment with
92. Coppe JP, Patil CK, Rodier F, Sun Y, Munoz DP, Goldstein J, Nelson high doses of odanacatib on bone mass, bone strength, and remodel-
PS, Desprez PY, Campisi J. Senescence-associated secretory pheno- ing/modeling in newly ovariectomized monkeys. Bone 88: 113-124,
types reveal cell-nonautonomous functions of oncogenic RAS and the 2016.
p53 tumor suppressor. PLoS Biol 6: 2853-2868, 2008. 112. Ebeling PR, Atley LM, Guthrie JR, Burger HG, Dennerstein L,
93. d’Adda di Fagagna F, Reaper PM, Clay-Farrace L, Fiegler H, Carr P, Hopper JL, Wark JD. Bone turnover markers and bone density across
Von Zglinicki T, Saretzki G, Carter NP, Jackson SP. A DNA dam- the menopausal transition. J Clin Endocrinol Metab 81: 3366-3371,
age checkpoint response in telomere-initiated senescence. Nature 426: 1996.
194-198, 2003. 113. Eghbali-Fatourechi G, Khosla S, Sanyal A, Boyle WJ, Lacey DL, Riggs
94. Dalsky GP, Stocke KS, Ehsani AA, Slatopolsky E, Lee WC, Birge SJ BL. Role of RANK ligand in mediating increased bone resorption in
Jr. Weight-bearing exercise training and lumbar bone mineral content early postmenopausal women. J Clin Invest 111: 1221-1230, 2003.
in postmenopausal women. Ann Intern Med 108: 824-828, 1988. 114. el-Deiry WS, Tokino T, Velculescu VE, Levy DB, Parsons R, Trent
95. Davis HM, Pacheco-Costa R, Atkinson EG, Brun LR, Gortazar AR, JM, Lin D, Mercer WE, Kinzler KW, Vogelstein B. WAF1, a potential
Harris J, Hiasa M, Bolarinwa SA, Yoneda T, Ivan M, Bruzzaniti A, mediator of p53 tumor suppression. Cell 75: 817-825, 1993.
Bellido T, Plotkin LI. Disruption of the Cx43/miR21 pathway leads to 115. Elliot-Gibson V, Bogoch ER, Jamal SA, Beaton DE. Practice patterns
osteocyte apoptosis and increased osteoclastogenesis with aging. Aging in the diagnosis and treatment of osteoporosis after a fragility fracture:
Cell 16: 551-563, 2017. A systematic review. Osteoporos Int 15: 767-778, 2004.
96. De Cecco M, Ito T, Petrashen AP, Elias AE, Skvir NJ, Criscione SW, 116. Engelke K, Adams JE, Armbrecht G, Augat P, Bogado CE, Bouxsein
Caligiana A, Brocculi G, Adney EM, Boeke JD, Le O, Beausejour C, ML, Felsenberg D, Ito M, Prevrhal S, Hans DB, Lewiecki EM. Clinical
Ambati J, Ambati K, Simon M, Seluanov A, Gorbunova V, Slagboom use of quantitative computed tomography and peripheral quantitative
PE, Helfand SL, Neretti N, Sedivy JM. L1 drives IFN in senescent cells
and promotes age-associated inflammation. Nature 566: 73-78, 2019. computed tomography in the management of osteoporosis in adults:
97. Delgado-Calle J, Fernandez AF, Sainz J, Zarrabeitia MT, Sanudo The 2007 ISCD official positions. J Clin Densitom 11: 123-162, 2008.
C, Garcia-Renedo R, Perez-Nunez MI, Garcia-Ibarbia C, Fraga MF, 117. Epker BN, Frost HM. A histological study of remodeling at the
Riancho JA. Genome-wide profiling of bone reveals differentially periosteal, haversian canal, cortical endosteal, and trabecular endosteal
methylated regions in osteoporosis and osteoarthritis. Arthritis Rheum surfaces in human rib. Anat Rec 152: 129-135, 1965.
65: 197-205, 2013. 118. Epstein CJ, Martin GM, Schultz AL, Motulsky AG. Werner’s syndrome
98. Demaria M, Ohtani N, Youssef SA, Rodier F, Toussaint W, Mitchell a review of its symptomatology, natural history, pathologic features,
JR, Laberge RM, Vijg J, Van Steeg H, Dolle ME, Hoeijmakers JH, de genetics and relationship to the natural aging process. Medicine
Bruin A, Hara E, Campisi J. An essential role for senescent cells in (Baltimore) 45: 177-221, 1966.
optimal wound healing through secretion of PDGF-AA. Dev Cell 31: 119. Ernst M, Heath JK, Rodan GA. Estradiol effects on proliferation, mes-
722-733, 2014. senger ribonucleic acid for collagen and insulin-like growth factor-I,
99. Demidenko ZN, Blagosklonny MV. Growth stimulation leads to cellu- and parathyroid hormone-stimulated adenylate cyclase activity in
lar senescence when the cell cycle is blocked. Cell Cycle 7: 3355-3361, osteoblastic cells from calvariae and long bones. Endocrinology 125:
2008. 825-833, 1989.
100. Deng HW, Chen WM, Recker S, Stegman MR, Li JL, Davies KM, Zhou 120. European Prospective Osteoporosis Study Group, Felsenberg D, Sil-
Y, Deng H, Heaney R, Recker RR. Genetic determination of Colles’ man AJ, Lunt M, Armbrecht G, Ismail AA, Finn JD, Cockerill WC,
fracture and differential bone mass in women with and without Colles’ Banzer D, Benevolenskaya LI, Bhalla A, Bruges Armas J, Cannata JB,
fracture. J Bone Miner Res 15: 1243-1252, 2000. Cooper C, Dequeker J, Eastell R, Felsch B, Gowin W, Havelka S, Hos-
101. Diagnosis and Therapy NIH Consensus Development Panel on Osteo- zowski K, Jajic I, Janott J, Johnell O, Kanis JA, Kragl G, Lopes Vaz
porosis Prevention. Osteoporosis prevention, diagnosis, and therapy. A, Lorenc R, Lyritis G, Masaryk P, Matthis C, Miazgowski T, Parisi
JAMA 285: 785-795, 2001. G, Pols HA, Poor G, Raspe HH, Reid DM, Reisinger W, Schedit-Nave
102. Dionyssiotis Y. Spinal cord injury-related bone impairment and frac- C, Stepan JJ, Todd CJ, Weber K, Woolf AD, Yershova OB, Reeve J,
tures: An update on epidemiology and physiopathological mechanisms. O’Neill TW. Incidence of vertebral fracture in europe: Results from
J Musculoskelet Neuronal Interact 11: 257-265, 2011. the European Prospective Osteoporosis Study (EPOS). J Bone Miner
103. Dixon WG, Lunt M, Pye SR, Reeve J, Felsenberg D, Silman AJ, Res 17: 716-724, 2002.
O’Neill TW, European Prospective Osteoporosis Study Group. Low 121. Falahati-Nini A, Riggs BL, Atkinson EJ, O’Fallon WM, Eastell
grip strength is associated with bone mineral density and vertebral R, Khosla S. Relative contributions of testosterone and estrogen in
fracture in women. Rheumatology (Oxford) 44: 642-646, 2005. regulating bone resorption and formation in normal elderly men. J Clin
104. Domazetovic V, Marcucci G, Iantomasi T, Brandi ML, Vincenzini MT. Invest 106: 1553-1560, 2000.
Oxidative stress in bone remodeling: Role of antioxidants. Clin Cases 122. Falconi D, Oizumi K, Aubin JE. Leukemia inhibitory factor influences
Miner Bone Metab 14: 209-216, 2017. the fate choice of mesenchymal progenitor cells. Stem Cells 25: 305-
105. Donati G, Peddigari S, Mercer CA, Thomas G. 5S ribosomal RNA is 312, 2007.
an essential component of a nascent ribosomal precursor complex that 123. Farr JN, Fraser DG, Wang H, Jaehn K, Ogrodnik MB, Weivoda MM,
regulates the Hdm2-p53 checkpoint. Cell Rep 4: 87-98, 2013. Drake MT, Tchkonia T, LeBrasseur NK, Kirkland JL, Bonewald LF,
106. Drake MT, McCready LK, Hoey KA, Atkinson EJ, Khosla S. Effects of Pignolo RJ, Monroe DG, Khosla S. Identification of senescent cells in
suppression of follicle-stimulating hormone secretion on bone resorp- the bone microenvironment. J Bone Miner Res 31: 1920-1929, 2016.
tion markers in postmenopausal women. J Clin Endocrinol Metab 95: 124. Farr JN, Khosla S. Skeletal changes through the lifespan—from growth
5063-5068, 2010. to senescence. Nat Rev Endocrinol 11: 513-521, 2015.
107. Dudakovic A, Camilleri ET, Paradise CR, Samsonraj RM, Gluscevic 125. Farr JN, Roforth MM, Fujita K, Nicks KM, Cunningham JM, Atkinson
M, Paggi CA, Begun DL, Khani F, Pichurin O, Ahmed FS, Elsayed R, EJ, Therneau TM, McCready LK, Peterson JM, Drake MT, Monroe
Elsalanty M, McGee-Lawrence ME, Karperien M, Riester SM, Thaler DG, Khosla S. Effects of age and estrogen on skeletal gene expression
4378 Volume 13, January 2023
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Comprehensive Physiology Aging and Bone Metabolism
in humans as assessed by RNA sequencing. PLoS One 10: e0138347, 149. Gennari C, Agnusdei D, Nardi P, Civitelli R. Estrogen preserves
2015. a normal intestinal responsiveness to 1,25-dihydroxyvitamin D3 in
126. Farr JN, Rowsey JL, Eckhardt BA, Thicke BS, Fraser DG, Tchkonia oophorectomized women. J Clin Endocrinol Metab 71: 1288-1293,
T, Kirkland JL, Monroe DG, Khosla S. Independent roles of estrogen 1990.
deficiency and cellular senescence in the pathogenesis of osteoporosis: 150. Georgakopoulou E, Evangelou K, Havaki S, Townsend P, Kanavaros P,
Evidence in young adult mice and older humans. J Bone Miner Res 34: Gorgoulis VG. Apoptosis or senescence? Which exit route do epithe-
1407-1418, 2019. lial cells and fibroblasts preferentially follow? Mech Ageing Dev 156:
127. Farr JN, Xu M, Weivoda MM, Monroe DG, Fraser DG, Onken JL, 17-24, 2016.
Negley BA, Sfeir JG, Ogrodnik MB, Hachfeld CM, LeBrasseur NK, 151. Geusens P, Hochberg MC, van der Voort DJ, Pols H, van der Klift M,
Drake MT, Pignolo RJ, Pirtskhalava T, Tchkonia T, Oursler MJ, Kirk- Siris E, Melton ME, Turpin J, Byrnes C, Ross P. Performance of risk
land JL, Khosla S. Targeting cellular senescence prevents age-related indices for identifying low bone density in postmenopausal women.
bone loss in mice. Nat Med 23: 1072-1079, 2017. Mayo Clin Proc 77: 629-637, 2002.
128. Faulkner KG, Cummings SR, Black D, Palermo L, Gluer CC, Genant 152. Gibson CJ, Lindsley RC, Tchekmedyian V, Mar BG, Shi J, Jaiswal S,
HK. Simple measurement of femoral geometry predicts hip fracture: Bosworth A, Francisco L, He J, Bansal A, Morgan EA, Lacasce AS,
The study of osteoporotic fractures. J Bone Miner Res 8: 1211-1217, Freedman AS, Fisher DC, Jacobsen E, Armand P, Alyea EP, Koreth J,
1993. Ho V, Soiffer RJ, Antin JH, Ritz J, Nikiforow S, Forman SJ, Michor
129. Feichtinger X, Muschitz C, Heimel P, Baierl A, Fahrleitner-Pammer F, Neuberg D, Bhatia R, Bhatia S, Ebert BL. Clonal hematopoiesis
A, Redl H, Resch H, Geiger E, Skalicky S, Dormann R, Plachel F, associated with adverse outcomes after autologous stem-cell transplan-
Pietschmann P, Grillari J, Hackl M, Kocijan R. Bone-related circulat- tation for lymphoma. J Clin Oncol 35: 1598-1605, 2017.
ing microRNAs miR-29b-3p, miR-550a-3p, and miR-324-3p and their 153. Gimble JM, Morgan C, Kelly K, Wu X, Dandapani V, Wang CS,
association to bone microstructure and histomorphometry. Sci Rep 8: Rosen V. Bone morphogenetic proteins inhibit adipocyte differen-
4867, 2018. tiation by bone marrow stromal cells. J Cell Biochem 58: 393-402,
130. Fekete N, Erle A, Amann EM, Furst D, Rojewski MT, Langonne A, 1995.
Sensebe L, Schrezenmeier H, Schmidtke-Schrezenmeier G. Effect of 154. Gimble JM, Robinson CE, Wu X, Kelly KA, Rodriguez BR, Kliewer
high-dose irradiation on human bone-marrow-derived mesenchymal SA, Lehmann JM, Morris DC. Peroxisome proliferator-activated
stromal cells. Tissue Eng Part C Methods 21: 112-122, 2015. receptor-gamma activation by thiazolidinediones induces adipogenesis
131. Ferguson VL, Ayers RA, Bateman TA, Simske SJ. Bone development in bone marrow stromal cells. Mol Pharmacol 50: 1087-1094, 1996.
and age-related bone loss in male C57BL/6J mice. Bone 33: 387-398, 155. Goessling W, North TE, Loewer S, Lord AM, Lee S, Stoick-Cooper
2003. CL, Weidinger G, Puder M, Daley GQ, Moon RT, Zon LI. Genetic
132. Fernandez-Rebollo E, Eipel M, Seefried L, Hoffmann P, Strathmann interaction of PGE2 and Wnt signaling regulates developmental speci-
K, Jakob F, Wagner W. Primary osteoporosis is not reflected by fication of stem cells and regeneration. Cell 136: 1136-1147, 2009.
disease-specific DNA methylation or accelerated epigenetic age in 156. Goodman WG, Veldhuis JD, Belin TR, Juppner H, Salusky IB.
blood. J Bone Miner Res 33: 356-361, 2018. Suppressive effect of calcium on parathyroid hormone release in
133. Feskanich D, Willett W, Colditz G. Walking and leisure-time activ- adynamic renal osteodystrophy and secondary hyperparathyroidism.
ity and risk of hip fracture in postmenopausal women. JAMA 288: 2300- Kidney Int 51: 1590-1595, 1997.
2306, 2002. 157. Gorski JP, Huffman NT, Vallejo J, Brotto L, Chittur SV, Breggia A,
134. Fink HA, Ewing SK, Ensrud KE, Barrett-Connor E, Taylor BC, Cauley Stern A, Huang J, Mo C, Seidah NG, Bonewald L, Brotto M. Dele-
JA, Orwoll ES. Association of testosterone and estradiol deficiency tion of Mbtps1 (Pcsk8, S1p, Ski-1) gene in osteocytes stimulates soleus
with osteoporosis and rapid bone loss in older men. J Clin Endocrinol muscle regeneration and increased size and contractile force with age.
Metab 91: 3908-3915, 2006. J Biol Chem 291: 4308-4322, 2016.
135. Finkelstein JS, Lee H, Leder BZ, Burnett-Bowie SA, Goldstein DW, 158. Greendale GA, Edelstein S, Barrett-Connor E. Endogenous sex
Hahn CW, Hirsch SC, Linker A, Perros N, Servais AB, Taylor AP, steroids and bone mineral density in older women and men: The
Webb ML, Youngner JM, Yu EW. Gonadal steroid-dependent effects Rancho Bernardo Study. J Bone Miner Res 12: 1833-1843, 1997.
on bone turnover and bone mineral density in men. J Clin Invest 126: 159. Griffith JF, Yeung DK, Ma HT, Leung JC, Kwok TC, Leung PC. Bone
1114-1125, 2016. marrow fat content in the elderly: A reversal of sex difference seen in
136. Fitzpatrick LA. Secondary causes of osteoporosis. Mayo Clin Proc 77: younger subjects. J Magn Reson Imaging 36: 225-230, 2012.
453-468, 2002. 160. Gronthos S, Chen S, Wang CY, Robey PG, Shi S. Telomerase acceler-
137. Forsén L, Meyer HE, Midthjell K, Edna TH. Diabetes mellitus and ates osteogenesis of bone marrow stromal stem cells by upregulation of
the incidence of hip fracture: Results from the Nord-Trondelag health CBFA1, osterix, and osteocalcin. J Bone Miner Res 18: 716-722, 2003.
survey. Diabetologia 42: 920-925, 1999. 161. Grover A, Sanjuan-Pla A, Thongjuea S, Carrelha J, Giustacchini A,
138. Foster JD. Update on mineral and bone disorders in chronic kidney dis- Gambardella A, Macaulay I, Mancini E, Luis TC, Mead A, Jacob-
ease. Vet Clin North Am Small Anim Pract 46: 1131-1149, 2016. sen SE, Nerlov C. Single-cell RNA sequencing reveals molecular
139. Fournier A, Oprisiu R, Hottelart C, Yverneau PH, Ghazali A, Atik A, and functional platelet bias of aged haematopoietic stem cells. Nat
Hedri H, Said S, Sechet A, Rasolombololona M, Abighanem O, Sarraj Commun 7: 11075, 2016.
A, Esper NE, Moriniere P, Boudailliez B, Westeel P-F, Achard J-M, 162. Guillot C, Lecuit T. Mechanics of epithelial tissue homeostasis and
Pruna A. Renal osteodystrophy in dialysis patients: Diagnosis and treat- morphogenesis. Science 340: 1185-1189, 2013.
ment. Artif Organs 22: 530-557, 1998. 163. Hachemi Y, Rapp AE, Picke AK, Weidinger G, Ignatius A, Tucker-
140. Franceschi C, Campisi J. Chronic inflammation (inflammaging) and its mann J. Molecular mechanisms of glucocorticoids on skeleton and
potential contribution to age-associated diseases. J Gerontol A Biol Sci bone regeneration after fracture. J Mol Endocrinol 61: R75-R90, 2018.
Med Sci 69 (Suppl 1): S4-S9, 2014. 164. Haddy TB, Mosher RB, Reaman GH. Osteoporosis in survivors of acute
141. Frick KK, Bushinsky DA. Metabolic acidosis stimulates RANKL lymphoblastic leukemia. Oncologist 6: 278-285, 2001.
RNA expression in bone through a cyclo-oxygenase-dependent 165. Hall BM, Balan V, Gleiberman AS, Strom E, Krasnov P, Virtuoso
mechanism. J Bone Miner Res 18: 1317-1325, 2003. LP, Rydkina E, Vujcic S, Balan K, Gitlin I, Leonova K, Polinsky
142. Frost HM. Bone “mass” and the “mechanostat”: A proposal. Anat Rec A, Chernova OB, Gudkov AV. Aging of mice is associated with
219: 1-9, 1987. p16(Ink4a)- and beta-galactosidase-positive macrophage accumulation
143. Frost HM. Some ABC’s of skeletal pathophysiology. 6. The growth/ that can be induced in young mice by senescent cells. Aging (Albany
modeling/remodeling distinction. Calcif Tissue Int 49: 301-302, 1991. NY) 8: 1294-1315, 2016.
144. Frost HM. Bone’s mechanostat: A 2003 update. Anat Rec A Discov Mol 166. Harvey N, Curtis EM, Dennison EM, Cooper C. The epidemiology
Cell Evol Biol 275: 1081-1101, 2003. of osteoporotic fractures. In: Bilezikian JP, editor. Primer on the
145. Garg AX, Papaioannou A, Ferko N, Campbell G, Clarke J-A, Ray JG. Metabolic Bone Diseases and Disorders of Mineral Metabolism (9th
Estimating the prevalence of renal insufficiency in seniors requiring ed). Hoboken, NJ: John Wiley & Sons, Inc, 2019, p. 398-404.
long-term care. Kidney Int 65: 649-653, 2004. 167. Harvey NC, Gluer CC, Binkley N, McCloskey EV, Brandi ML,
146. Garnero P, Sornay-Rendu E, Chapuy MC, Delmas PD. Increased bone Cooper C, Kendler D, Lamy O, Laslop A, Camargos BM, Reginster
turnover in late postmenopausal women is a major determinant of JY, Rizzoli R, Kanis JA. Trabecular bone score (TBS) as a new com-
osteoporosis. J Bone Miner Res 11: 337-349, 1996. plementary approach for osteoporosis evaluation in clinical practice.
147. Gaudio A, Pennisi P, Bratengeier C, Torrisi V, Lindner B, Mangiafico Bone 78: 216-224, 2015.
RA, Pulvirenti I, Hawa G, Tringali G, Fiore CE. Increased sclerostin 168. Hattner R, Epker BN, Frost HM. Suggested sequential mode of control
serum levels associated with bone formation and resorption markers of changes in cell behaviour in adult bone remodelling. Nature 206:
in patients with immobilization-induced bone loss. J Clin Endocrinol 489-490, 1965.
Metab 95: 2248-2253, 2010. 169. Hayflick L. The limited in vitro lifetime of human diploid cell strains.
148. Gekas C, Graf T. CD41 expression marks myeloid-biased adult Exp Cell Res 37: 614-636, 1965.
hematopoietic stem cells and increases with age. Blood 121: 4463- 170. Hayflick L, Moorhead PS. The serial cultivation of human diploid cell
4472, 2013. strains. Exp Cell Res 25: 585-621, 1961.
Volume 13, January 2023 4379
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
171. Haylock DN, Nilsson SK. Osteopontin: A bridge between bone and V, Kuo FC, Kluk MJ, Henderson B, Kinnunen L, Koistinen HA, Laden-
blood. Br J Haematol 134: 467-474, 2006. vall C, Getz G, Correa A, Banahan BF, Gabriel S, Kathiresan S, String-
172. Hemming S, Cakouros D, Vandyke K, Davis MJ, Zannettino AC, ham HM, McCarthy MI, Boehnke M, Tuomilehto J, Haiman C, Groop
Gronthos S. Identification of novel EZH2 targets regulating osteogenic L, Atzmon G, Wilson JG, Neuberg D, Altshuler D, Ebert BL. Age-
differentiation in mesenchymal stem cells. Stem Cells Dev 25: 909-921, related clonal hematopoiesis associated with adverse outcomes. N Engl
2016. J Med 371: 2488-2498, 2014.
173. Henderson TO, Ness KK, Cohen HJ. Accelerated aging among cancer 192. Jiang Y, Jahagirdar BN, Reinhardt RL, Schwartz RE, Keene CD, Ortiz-
survivors: From pediatrics to geriatrics. Am Soc Clin Oncol Educ Book: Gonzalez XR, Reyes M, Lenvik T, Lund T, Blackstad M, Du J, Aldrich
e423-e430, 2014. S, Lisberg A, Low WC, Largaespada DA, Verfaillie CM. Pluripotency
174. Heveran CM, Rauff A, King KB, Carpenter RD, Ferguson VL. A new of mesenchymal stem cells derived from adult marrow. Nature 418:
open-source tool for measuring 3D osteocyte lacunar geometries from 41-49, 2002.
confocal laser scanning microscopy reveals age-related changes to 193. Jilka RL. Biology of the basic multicellular unit and the pathophysiol-
lacunar size and shape in cortical mouse bone. Bone 110: 115-127, ogy of osteoporosis. Med Pediatr Oncol 41: 182-185, 2003.
2018. 194. Jilka RL. The relevance of mouse models for investigating age-related
175. Hippisley-Cox J, Coupland C. Derivation and validation of updated bone loss in humans. J Gerontol A Biol Sci Med Sci 68: 1209-1217,
QFracture algorithm to predict risk of osteoporotic fracture in primary 2013.
care in the United Kingdom: Prospective open cohort study. BMJ 344: 195. Jilka RL, Almeida M, Ambrogini E, Han L, Roberson PK, Weinstein
e3427, 2012. RS, Manolagas SC. Decreased oxidative stress and greater bone
176. Hoare M, Ito Y, Kang TW, Weekes MP, Matheson NJ, Patten DA, anabolism in the aged, when compared to the young, murine skeleton
Shetty S, Parry AJ, Menon S, Salama R, Antrobus R, Tomimatsu K, with parathyroid hormone administration. Aging Cell 9: 851-867,
Howat W, Lehner PJ, Zender L, Narita M. NOTCH1 mediates a switch 2010.
between two distinct secretomes during senescence. Nat Cell Biol 18: 196. Jilka RL, Hangoc G, Girasole G, Passeri G, Williams DC, Abrams JS,
979-992, 2016. Boyce B, Broxmeyer H, Manolagas SC. Increased osteoclast devel-
177. Hofbauer LC, Khosla S, Dunstan CR, Lacey DL, Spelsberg TC, opment after estrogen loss: Mediation by interleukin-6. Science 257:
Riggs BL. Estrogen stimulates gene expression and protein production 88-91, 1992.
of osteoprotegerin in human osteoblastic cells. Endocrinology 140: 197. Jilka RL, O’Brien CA. The role of osteocytes in age-related bone loss.
4367-4370, 1999. Curr Osteoporos Rep 14: 16-25, 2016.
178. Holstege H, Pfeiffer W, Sie D, Hulsman M, Nicholas TJ, Lee CC, Ross 198. Johansson AG, Lindh E, Blum WF, Kollerup G, Sørensen OH, Ljung-
T, Lin J, Miller MA, Ylstra B, Meijers-Heijboer H, Brugman MH, hall S. Effects of growth hormone and insulin-like growth factor I in
Staal FJ, Holstege G, Reinders MJ, Harkins TT, Levy S, Sistermans men with idiopathic osteoporosis. J Clin Endocrinol Metab 81: 44-48,
EA. Somatic mutations found in the healthy blood compartment of 1996.
a 115-yr-old woman demonstrate oligoclonal hematopoiesis. Genome 199. Johansson H, Siggeirsdottir K, Harvey NC, Oden A, Gudnason V,
Res 24: 733-742, 2014. McCloskey E, Sigurdsson G, Kanis JA. Imminent risk of fracture after
179. Hong JH, Hwang ES, McManus MT, Amsterdam A, Tian Y, fracture. Osteoporos Int 28: 775-780, 2017.
Kalmukova R, Mueller E, Benjamin T, Spiegelman BM, Sharp PA, 200. Johmura Y, Sun J, Kitagawa K, Nakanishi K, Kuno T, Naiki-Ito
Hopkins N, Yaffe MB. TAZ, a transcriptional modulator of mesenchy- A, Sawada Y, Miyamoto T, Okabe A, Aburatani H, Li S, Miyoshi
mal stem cell differentiation. Science 309: 1074-1078, 2005. I, Takahashi S, Kitagawa M, Nakanishi M. SCF(Fbxo22)-KDM4A
180. Horn HF, Vousden KH. Cooperation between the ribosomal proteins targets methylated p53 for degradation and regulates senescence. Nat
L5 and L11 in the p53 pathway. Oncogene 27: 5774-5784, 2008. Commun 7: 10574, 2016.
181. Howard GM, Nguyen TV, Harris M, Kelly PJ, Eisman JA. Genetic 201. Justesen J, Stenderup K, Ebbesen EN, Mosekilde L, Steiniche T,
and environmental contributions to the association between quantita- Kassem M. Adipocyte tissue volume in bone marrow is increased with
tive ultrasound and bone mineral density measurements: A twin study. aging and in patients with osteoporosis. Biogerontology 2: 165-171,
J Bone Miner Res 13: 1318-1327, 1998.
182. Hruska KA, Teitelbaum SL. Renal osteodystrophy. N Engl J Med 333: 2001.
166-174, 1995. 202. Justesen J, Stenderup K, Eriksen EF, Kassem M. Maintenance of
183. Alexeeva P, Burkhardt P, Christiansen C, Cooper C, Delmas P, osteoblastic and adipocytic differentiation potential with age and
Johnell O, Johnston C, Kanis JA, Lips P, Melton LJ, Meunier P, osteoporosis in human marrow stromal cell cultures. Cacif Tissue Int
Seeman E, Stepan J, and Tosteson A. Assessment of fracture risk and 71: 36-44, 2002.
its application to screening for postmenopausal osteoporosis. Report of 203. Kado DM, Browner WS, Palermo L, Nevitt MC, Genant HK, Cum-
a WHO Study Group. World Health Organ Tech Rep Ser 843: 1-129, mings SR. Vertebral fractures and mortality in older women: A
1994. prospective study. Study of Osteoporotic Fractures Research Group.
184. Huang H, Song T-J, Li X, Hu L, He Q, Liu M, Lane MD, Tang Q- Arch Intern Med 159: 1215-1220, 1999.
Q. BMP signaling pathway is required for commitment of C3H10T1/2 204. Kajkenova O, Lecka-Czernik B, Gubrij I, Hauser SP, Takahashi K,
pluripotent stem cells to the adipocyte lineage. Proc Natl Acad Sci U S A Parfitt AM, Jilka RL, Manolagas SC, Lipschitz DA. Increased adipoge-
106: 12670-12675, 2009. nesis and myelopoiesis in the bone marrow of SAMP6, a murine model
185. Huang J, Romero-Suarez S, Lara N, Mo C, Kaja S, Brotto L, Dallas of defective osteoblastogenesis and low turnover osteopenia. J Bone
SL, Johnson ML, Jahn K, Bonewald LF, Brotto M. Crosstalk between Miner Res 12: 1772-1779, 1997.
MLO-Y4 osteocytes and C2C12 muscle cells is mediated by the 205. Kalu DN. Evaluation of the pathogenesis of skeletal changes in ovariec-
Wnt/beta-catenin pathway. JBMR Plus 1: 86-100, 2017. tomized rats. Endocrinology 115: 507-512, 1984.
186. Hughes DE, Dai A, Tiffee JC, Li HH, Mundy GR, Boyce BF. Estro- 206. Kane AE, Sinclair DA. Epigenetic changes during aging and their
gen promotes apoptosis of murine osteoclasts mediated by TGF-beta. reprogramming potential. Crit Rev Biochem Mol Biol 54: 61-83, 2019.
Nat Med 2: 1132-1136, 1996. 207. Kang C, Xu Q, Martin TD, Li MZ, Demaria M, Aron L, Lu T, Yankner
187. Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: BA, Campisi J, Elledge SJ. The DNA damage response induces inflam-
Clinical, research, and policy implications of a core geriatric concept. mation and senescence by inhibiting autophagy of GATA4. Science
J Am Geriatr Soc 55: 780-791, 2007. 349: aaa5612, 2015.
188. Ismail AA, Pye SR, Cockerill WC, Lunt M, Silman AJ, Reeve J, Banzer 208. Kang Q, Song W-X, Luo Q, Tang N, Luo J, Luo X, Chen J, Bi Y, He
D, Benevolenskaya LI, Bhalla A, Bruges Armas J, Cannata JB, Cooper B-C, Park JK, Jiang W, Tang Y, Huang J, Su Y, Zhu G-H, He Y, Yin
C, Delmas PD, Dequeker J, Dilsen G, Falch JA, Felsch B, Felsenberg D, H, Hu Z, Wang Y, Chen L, Zuo G-W, Pan XL, Shen J, Vokes T, Reid
Finn JD, Gennari C, Hoszowski K, Jajic I, Janott J, Johnell O, Kanis JA, RR, Haydon RC, Luu HH, He T-C. A comprehensive analysis of the
Kragl G, Lopez Vaz A, Lorenc R, Lyritis G, Marchand F, Masaryk P, dual roles of BMPs in regulating adipogenic and osteogenic differen-
Matthis C, Miazgowski T, Naves-Diaz M, Pols HA, Poor G, Rapado A, tiation of mesenchymal progenitor cells. Stem Cells Dev 18: 545-558,
Raspe HH, Reid DM, Reisinger W, Scheidt-Nave C, Stepan J, Todd C, 2009.
Weber K, Woolf AD, O’Neill TW. Incidence of limb fracture across 209. Kang S, Bennett CN, Gerin I, Rapp LA, Hankenson KD, Macdougald
Europe: Results from the European Prospective Osteoporosis Study OA. Wnt signaling stimulates osteoblastogenesis of mesenchymal
(EPOS). Osteoporos Int 13: 565-571, 2002. precursors by suppressing CCAAT/enhancer-binding protein α and
189. Ito CY, Li CY, Bernstein A, Dick JE, Stanford WL. Hematopoietic peroxisome proliferator. J Biol Chem 282: 14515-14524, 2007.
stem cell and progenitor defects in Sca-1/Ly-6A-null mice. Blood 101: 210. Kanis JA, Cooper C, Rizzoli R, Abrahamsen B, Al-Daghri NM, Brandi
517-523, 2003. ML, Cannata-Andia J, Cortet B, Dimai HP, Ferrari S, Hadji P, Har-
190. Jacobsen SJ, Cooper C, Gottlieb MS, Goldberg J, Yahnke DP, Melton vey NC, Kraenzlin M, Kurth A, McCloskey E, Minisola S, Thomas
LJ 3rd. Hospitalization with vertebral fracture among the aged: A T, Reginster JY, European Society for Clinical and Economic Aspects
national population-based study, 1986-1989. Epidemiology 3: 515-518, of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases. Identi-
1992. fication and management of patients at increased risk of osteoporotic
191. Jaiswal S, Fontanillas P, Flannick J, Manning A, Grauman PV, Mar BG, fracture: Outcomes of an ESCEO expert consensus meeting. Osteo-
Lindsley RC, Mermel CH, Burtt N, Chavez A, Higgins JM, Moltchanov poros Int 28: 2023-2034, 2017.
4380 Volume 13, January 2023
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Comprehensive Physiology Aging and Bone Metabolism
211. Kanis JA, Oden A, McCloskey EV, Johansson H, Wahl DA, Cooper C, 235. Klop C, van Staa TP, Cooper C, Harvey NC, de Vries F. The epi-
IOF Working Group on Epidemiology and Quality of Life. A systematic demiology of mortality after fracture in England: Variation by age, sex,
review of hip fracture incidence and probability of fracture worldwide. time, geographic location, and ethnicity. Osteoporos Int 28: 161-168,
Osteoporos Int 23: 2239-2256, 2012. 2017.
212. Kannus P, Palvanen M, Kaprio J, Parkkari J, Koskenvuo M. Genetic 236. Klotzbuecher CM, Ross PD, Landsman PB, Abbott TA 3rd, Berger M.
factors and osteoporotic fractures in elderly people: Prospective 25 year Patients with prior fractures have an increased risk of future fractures:
follow up of a nationwide cohort of elderly Finnish twins. BMJ 319: A summary of the literature and statistical synthesis. J Bone Miner Res
1334-1337, 1999. 15: 721-739, 2000.
213. Karner CM, Long F. Wnt signaling and cellular metabolism in 237. Kocijan R, Muschitz C, Geiger E, Skalicky S, Baierl A, Dormann R,
osteoblasts. Cell Mol Life Sci 74: 1649-1657, 2017. Plachel F, Feichtinger X, Heimel P, Fahrleitner-Pammer A, Grillari
214. Kasperk CH, Wergedal JE, Farley JR, Linkhart TA, Turner RT, Baylink J, Redl H, Resch H, Hackl M. Circulating microRNA signatures in
DJ. Androgens directly stimulate proliferation of bone cells in vitro. patients with idiopathic and postmenopausal osteoporosis and fragility
Endocrinology 124: 1576-1578, 1989. fractures. J Clin Endocrinol Metab 101: 4125-4134, 2016.
215. Kassem M, Marie PJ. Senescence-associated intrinsic mechanisms of 238. Koh LK, Sedrine WB, Torralba TP, Kung A, Fujiwara S, Chan SP,
osteoblast dysfunctions. Aging Cell 10: 191-197, 2011. Huang QR, Rajatanavin R, Tsai KS, Park HM, Reginster JY. A simple
216. Katsoulis M, Benetou V, Karapetyan T, Feskanich D, Grodstein F, tool to identify asian women at increased risk of osteoporosis. Osteo-
Pettersson-Kymmer U, Eriksson S, Wilsgaard T, Jorgensen L, Ahmed poros Int 12: 699-705, 2001.
LA, Schottker B, Brenner H, Bellavia A, Wolk A, Kubinova R, 239. Kontulainen S, Sievanen H, Kannus P, Pasanen M, Vuori I. Effect
Stegeman B, Bobak M, Boffetta P, Trichopoulou A. Excess mortality of long-term impact-loading on mass, size, and estimated strength of
after hip fracture in elderly persons from Europe and the USA: The humerus and radius of female racquet-sports players: A peripheral
CHANCES project. J Intern Med 281: 300-310, 2017. quantitative computed tomography study between young and old
217. Kawaguchi H, Manabe N, Miyaura C, Chikuda H, Nakamura K, Kuro-o starters and controls. J Bone Miner Res 17: 2281-2289, 2002.
M. Independent impairment of osteoblast and osteoclast differentiation 240. Krall EA, Dawson-Hughes B. Walking is related to bone density and
in klotho mouse exhibiting low-turnover osteopenia. J Clin Invest 104: rates of bone loss. Am J Med 96: 20-26, 1994.
229-237, 1999. 241. Krieger NS, Frick KK, Bushinsky DA. Mechanism of acid-induced
218. Kawaguchi H, Pilbeam CC, Vargas SJ, Morse EE, Lorenzo JA, Raisz bone resorption. Curr Opin Nephrol Hypertens 13: 423-436, 2004.
LG. Ovariectomy enhances and estrogen replacement inhibits the activ- 242. Krishnamurthy J, Torrice C, Ramsey MR, Kovalev GI, Al-Regaiey K,
ity of bone marrow factors that stimulate prostaglandin production in Su L, Sharpless NE. Ink4a/Arf expression is a biomarker of aging.
cultured mouse calvariae. J Clin Invest 96: 539-548, 1995. J Clin Invest 114: 1299-1307, 2004.
219. Khastgir G, Studd J, Holland N, Alaghband-Zadeh J, Fox S, Chow J. 243. Kritz-Silverstein D, Barrett-Connor E. Grip strength and bone mineral
Anabolic effect of estrogen replacement on bone in postmenopausal density in older women. J Bone Miner Res 9: 45-51, 1994.
women with osteoporosis: Histomorphometric evidence in a longitudi- 244. Kudlow BA, Kennedy BK, Monnat RJ Jr. Werner and Hutchinson-
nal study. J Clin Endocrinol Metab 86: 289-295, 2001. Gilford progeria syndromes: Mechanistic basis of human progeroid
220. Khosla S. Pathogenesis of age-related bone loss in humans. J Gerontol diseases. Nat Rev Mol Cell Biol 8: 394-404, 2007.
A Biol Sci Med Sci 68: 1226-1235, 2013. 245. Kuilman T, Michaloglou C, Mooi WJ, Peeper DS. The essence of
221. Khosla S. New insights into androgen and estrogen receptor regulation senescence. Genes Dev 24: 2463-2479, 2010.
of the male skeleton. J Bone Miner Res 30: 1134-1137, 2015. 246. Kuilman T, Michaloglou C, Vredeveld LC, Douma S, van Doorn R,
222. Khosla S, Atkinson EJ, Melton LJ 3rd, Riggs BL. Effects of age and Desmet CJ, Aarden LA, Mooi WJ, Peeper DS. Oncogene-induced
estrogen status on serum parathyroid hormone levels and biochemical senescence relayed by an interleukin-dependent inflammatory network.
markers of bone turnover in women: A population-based study. J Clin Cell 133: 1019-1031, 2008.
Endocrinol Metab 82: 1522-1527, 1997. 247. Kurihara N, Bertolini D, Suda T, Akiyama Y, Roodman GD. IL-6 stim-
223. Khosla S, Melton LJ 3rd, Atkinson EJ, O’Fallon WM. Relationship ulates osteoclast-like multinucleated cell formation in long term human
of serum sex steroid levels to longitudinal changes in bone density in marrow cultures by inducing IL-1 release. J Immunol 144: 4226-4230,
young versus elderly men. J Clin Endocrinol Metab 86: 3555-3561, 1990.
2001. 248. Langdahl B, Ferrari S, Dempster DW. Bone modeling and remodeling:
224. Khosla S, Melton LJ 3rd, Atkinson EJ, O’Fallon WM, Klee GG, Riggs Potential as therapeutic targets for the treatment of osteoporosis. Ther
BL. Relationship of serum sex steroid levels and bone turnover markers Adv Musculoskelet Dis 8: 225-235, 2016.
with bone mineral density in men and women: A key role for bioavail- 249. Lawson J. Drug-induced metabolic bone disorders. Semin Muscu-
able estrogen. J Clin Endocrinol Metab 83: 2266-2274, 1998. loskelet Radiol 6: 285-297, 2002.
225. Khosla S, Oursler MJ, Monroe DG. Estrogen and the skeleton. Trends 250. LeBlanc ES, Nielson CM, Marshall LM, Lapidus JA, Barrett-Connor
Endocrinol Metab 23: 576-581, 2012. E, Ensrud KE, Hoffman AR, Laughlin G, Ohlsson C, Orwoll ES,
226. Khosla S, Riggs BL. Pathophysiology of age-related bone loss and Osteoporotic Fractures in Men Study Group. The effects of serum
osteoporosis. Endocrinol Metab Clin N Am 34: 1015-1030, xi, 2005. testosterone, estradiol, and sex hormone binding globulin levels on
227. Khosla S, Riggs BL, Atkinson EJ, Oberg AL, McDaniel LJ, Holets M, fracture risk in older men. J Clin Endocrinol Metab 94: 3337-3346,
Peterson JM, Melton LJ 3rd. Effects of sex and age on bone microstruc- 2009.
ture at the ultradistal radius: A population-based noninvasive in vivo 251. Leinau L, Perazella MA. Hip fractures in end-stage renal disease
assessment. J Bone Miner Res 21: 124-131, 2006. patients: Incidence, risk factors, and prevention. Semin Dial 19: 75-79,
228. Kim H, Wrann CD, Jedrychowski M, Vidoni S, Kitase Y, Nagano K, 2006.
Zhou C, Chou J, Parkman VA, Novick SJ, Strutzenberg TS, Pascal BD, 252. Lenchik L, Register TC, Hsu FC, Xu J, Smith SC, Carr JJ, Freedman
Le PT, Brooks DJ, Roche AM, Gerber KK, Mattheis L, Chen W, Tu H, BI, Bowden DW. Bone mineral density of the radius predicts all-cause
Bouxsein ML, Griffin PR, Baron R, Rosen CJ, Bonewald LF, Spiegel- mortality in patients with type 2 diabetes: Diabetes heart study. J Clin
man BM. Irisin mediates effects on bone and fat via alphaV integrin Densitom 21: 347-354, 2018.
receptors. Cell 175: 1756-1768.e17, 2018. 253. Lerebours C, Buenzli PR. Towards a cell-based mechanostat theory of
229. Kim HN, Chang J, Iyer S, Han L, Campisi J, Manolagas SC, Zhou bone: The need to account for osteocyte desensitisation and osteocyte
D, Almeida M. Elimination of senescent osteoclast progenitors has no replacement. J Biomech 49: 2600-2606, 2016.
effect on the age-associated loss of bone mass in mice. Aging Cell 18: 254. Lessard F, Igelmann S, Trahan C, Huot G, Saint-Germain E, Mignacca
e12923, 2019. L, Del Toro N, Lopes-Paciencia S, Le Calve B, Montero M, Deschenes-
230. Kim HN, Chang J, Shao L, Han L, Iyer S, Manolagas SC, O’Brien Simard X, Bury M, Moiseeva O, Rowell MC, Zorca CE, Zenklusen D,
CA, Jilka RL, Zhou D, Almeida M. DNA damage and senescence in Brakier-Gingras L, Bourdeau V, Oeffinger M, Ferbeyre G. Senescence-
osteoprogenitors expressing Osx1 may cause their decrease with age. associated ribosome biogenesis defects contributes to cell cycle arrest
Aging Cell 16: 693-703, 2017. through the Rb pathway. Nat Cell Biol 20: 789-799, 2018.
231. Kim SW, Lu Y, Williams EA, Lai F, Lee JY, Enishi T, Balani DH, 255. Levey AS. National kidney foundation practice guidelines for chronic
Ominsky MS, Ke HZ, Kronenberg HM, Wein MN. Sclerostin antibody kidney disease: Evaluation, classification, and stratification. Ann Intern
administration converts bone lining cells into active osteoblasts. J Bone Med 139: 137-147, 2003.
Miner Res 32: 892-901, 2017. 256. Lewiecki EM. Clinical vignettes: Using non-BMD measurements in
232. Kiratli BJ, Smith AE, Nauenberg T, Kallfelz CF, Perkash I. Bone min- clinical practice. Clin Rev Bone Miner Metab 14: 50-54, 2016.
eral and geometric changes through the femur with immobilization due 257. Lewiecki EM, Binkley N, Morgan SL, Shuhart CR, Camargos BM,
to spinal cord injury. J Rehabil Res Dev 37: 225-233, 2000. Carey JJ, Gordon CM, Jankowski LG, Lee JK, Leslie WD, International
233. Kirkland JL, Tchkonia T, Zhu Y, Niedernhofer LJ, Robbins PD. The Society for Clinical Densitometry. Best practices for dual-energy X-ray
clinical potential of senolytic drugs. J Am Geriatr Soc 65: 2297-2301, absorptiometry measurement and reporting: International Society for
2017. Clinical Densitometry Guidance. J Clin Densitom 19: 127-140, 2016.
234. Kitase Y, Vallejo JA, Gutheil W, Vemula H, Jahn K, Yi J, Zhou J, Brotto 258. Li B, Boast S, de los Santos K, Schieren I, Quiroz M, Teitelbaum SL,
M, Bonewald LF. Beta-aminoisobutyric acid, l-BAIBA, is a muscle- Tondravi MM, Goff SP. Mice deficient in Abl are osteoporotic and have
derived osteocyte survival factor. Cell Rep 22: 1531-1544, 2018. defects in osteoblast maturation. Nat Genet 24: 304-308, 2000.
Volume 13, January 2023 4381
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
259. Li CJ, Cheng P, Liang MK, Chen YS, Lu Q, Wang JY, Xia ZY, Zhou 284. Meng J, Zhang D, Pan N, Sun N, Wang Q, Fan J, Zhou P, Zhu W,
HD, Cao X, Xie H, Liao EY, Luo XH. MicroRNA-188 regulates age- Jiang L. Identification of miR-194-5p as a potential biomarker for post-
related switch between osteoblast and adipocyte differentiation. J Clin menopausal osteoporosis. PeerJ 3: e971, 2015.
Invest 125: 1509-1522, 2015. 285. Mera P, Laue K, Ferron M, Confavreux C, Wei J, Galan-Diez M,
260. Li H, Wang Z, Fu Q, Zhang J. Plasma miRNA levels correlate with Lacampagne A, Mitchell SJ, Mattison JA, Chen Y, Bacchetta J,
sensitivity to bone mineral density in postmenopausal osteoporosis Szulc P, Kitsis RN, de Cabo R, Friedman RA, Torsitano C, McGraw
patients. Biomarkers 19: 553-556, 2014. TE, Puchowicz M, Kurland I, Karsenty G. Osteocalcin signaling
261. Li X, Zhang Y, Kang H, Liu W, Liu P, Zhang J, Harris SE, Wu D. in myofibers is necessary and sufficient for optimum adaptation to
Sclerostin binds to LRP5/6 and antagonizes canonical Wnt signaling. exercise. Cell Metab 23: 1078-1092, 2016.
J Biol Chem 280: 19883-19887, 2005. 286. Meunier P, Aaron J, Edouard C, Vignon G. Osteoporosis and the
262. Liang CT, Barnes J, Seedor JG, Quartuccio HA, Bolander M, Jeffrey replacement of cell populations of the marrow by adipose tissue: A
JJ, Rodan GA. Impaired bone activity in aged rats: Alterations at the quantitative study of 84 iliac bone biopsies. Clin Orthop Relat Res 80:
cellular and molecular levels. Bone 13: 435-441, 1992. 147-154, 1971.
263. Lips P. Vitamin D deficiency and secondary hyperparathyroidism in 287. Michaelsson K, Melhus H, Ferm H, Ahlbom A, Pedersen NL. Genetic
the elderly: Consequences for bone loss and fractures and therapeutic liability to fractures in the elderly. Arch Intern Med 165: 1825-1830,
implications. Endocr Rev 22: 477-501, 2001. 2005.
264. Liu L, van Groen T, Kadish I, Li Y, Wang D, James SR, Karpf AR, 288. Minaire P, Meunier P, Edouard C, Bernard J, Courpron P, Bourret J.
Tollefsbol TO. Insufficient DNA methylation affects healthy aging and Quantitative histological data on disuse osteoporosis - comparison with
promotes age-related health problems. Clin Epigenetics 2: 349-360, biological data. Calcif Tissue Res 17: 57-73, 1974.
2011. 289. Mirza FS, Padhi ID, Raisz LG, Lorenzo JA. Serum sclerostin levels
265. Liu X, Wan M. A tale of the good and bad: Cell senescence in bone negatively correlate with parathyroid hormone levels and free estrogen
homeostasis and disease. Int Rev Cell Mol Biol 346: 97-128, 2019. index in postmenopausal women. J Clin Endocrinol Metab 95: 1991-
266. Lopez-Otin C, Blasco MA, Partridge L, Serrano M, Kroemer G. The 1997, 2010.
hallmarks of aging. Cell 153: 1194-1217, 2013. 290. Misra J, Mohanty ST, Madan S, Fernandes JA, Hal Ebetino F, Rus-
267. Loro E, Ramaswamy G, Chandra A, Tseng WJ, Mishra MK, Shore sell RG, Bellantuono I. Zoledronate attenuates accumulation of DNA
EM, Khurana TS. IL15RA is required for osteoblast function and bone damage in mesenchymal stem cells and protects their function. Stem
mineralization. Bone 103: 20-30, 2017. Cells 34: 756-767, 2016.
268. Lydick E, Cook K, Turpin J, Melton M, Stine R, Byrnes C. Develop- 291. Misteli T. Higher-order genome organization in human disease. Cold
ment and validation of a simple questionnaire to facilitate identification Spring Harb Perspect Biol 2: a000794, 2010.
of women likely to have low bone density. Am J Manag Care 4: 37-48, 292. Mitchell WK, Williams J, Atherton P, Larvin M, Lund J, Narici M.
1998. Sarcopenia, dynapenia, and the impact of advancing age on human
269. Maggi S, Kelsey JL, Litvak J, Heyse SP. Incidence of hip fractures in skeletal muscle size and strength; a quantitative review. Front Physiol
the elderly: A cross-national analysis. Osteoporos Int 1: 232-241, 1991. 3: 260, 2012.
270. Malaquin N, Martinez A, Rodier F. Keeping the senescence secretome 293. Mo C, Romero-Suarez S, Bonewald L, Johnson M, Brotto M.
under control: Molecular reins on the senescence-associated secretory Prostaglandin E2: From clinical applications to its potential role
phenotype. Exp Gerontol 82: 39-49, 2016. in bone-muscle crosstalk and myogenic differentiation. Recent Pat
271. Manolagas SC. Birth and death of bone cells: Basic regulatory mech- Biotechnol 6: 223-229, 2012.
anisms and implications for the pathogenesis and treatment of osteo- 294. Mo C, Zhao R, Vallejo J, Igwe O, Bonewald L, Wetmore L, Brotto M.
porosis. Endocr Rev 21: 115-137, 2000. Prostaglandin E2 promotes proliferation of skeletal muscle myoblasts
272. Marie PJ, Kassem M. Extrinsic mechanisms involved in age-related via EP4 receptor activation. Cell Cycle 14: 1507-1516, 2015.
defective bone formation. J Clin Endocrinol Metab 96: 600-609, 2011. 295. Modder UI, Roforth MM, Hoey K, McCready LK, Peterson JM, Mon-
273. Marques EA, Elbejjani M, Gudnason V, Sigurdsson G, Lang T, roe DG, Oursler MJ, Khosla S. Effects of estrogen on osteoprogenitor
cells and cytokines/bone-regulatory factors in postmenopausal women.
Sigurdsson S, Aspelund T, Meirelles O, Siggeirsdottir K, Launer L, Bone 49: 202-207, 2011.
Eiriksdottir G, Harris TB. Proximal femur volumetric bone mineral 296. Moerman EJ, Teng K, Lipschitz DA, Lecka-Czernik B. Aging activates
density and mortality: 13 years of follow-up of the AGES-Reykjavik adipogenic and suppresses osteogenic programs in mesenchymal mar-
Study. J Bone Miner Res 32: 1237-1242, 2017. row stroma/stem cells: The role of PPAR-γ2 transcription factor and
274. Martin-Millan M, Almeida M, Ambrogini E, Han L, Zhao H, Weinstein TGF-β/BMP. Aging Cell 3: 379-389, 2004.
RS, Jilka RL, O’Brien CA, Manolagas SC. The estrogen receptor-alpha 297. Moore SG, Dawson KL. Red and yellow marrow in the femur: Age-
in osteoclasts mediates the protective effects of estrogens on cancellous related changes in appearance at MR imaging. Radiology 175: 219-223,
but not cortical bone. Mol Endocrinol 24: 323-334, 2010. 1990.
275. Martin B. Aging and strength of bone as a structural material. Calcif 298. Morris JA, Tsai PC, Joehanes R, Zheng J, Trajanoska K, Soerensen
Tissue Int 53 (Suppl 1): S34-S39; discussion S39-S40, 1993. M, Forgetta V, Castillo-Fernandez JE, Frost M, Spector TD, Chris-
276. Martin TJ, Seeman E. Bone remodelling: Its local regulation and the tensen K, Christiansen L, Rivadeneira F, Tobias JH, Evans DM, Kiel
emergence of bone fragility. Best Pract Res Clin Endocrinol Metab 22: DP, Hsu YH, Richards JB, Bell JT. Epigenome-wide association of
701-722, 2008. DNA methylation in whole blood with bone mineral density. J Bone
277. Martin TJ, Sims NA. Osteoclast-derived activity in the coupling of bone Miner Res 32: 1644-1650, 2017.
formation to resorption. Trends Mol Med 11: 76-81, 2005. 299. Mosekilde L, Danielsen CC, Gasser J. The effect on vertebral
278. Mason PJ, Wilson DB, Bessler M. Dyskeratosis congenita—a disease bone mass and strength of long term treatment with antiresorptive
of dysfunctional telomere maintenance. Curr Mol Med 5: 159-170, agents (estrogen and calcitonin), human parathyroid hormone-(1-38),
2005. and combination therapy, assessed in aged ovariectomized rats.
279. Matsushita M, Tsuboyama T, Kasai R, Okumura H, Yamamuro T, Endocrinology 134: 2126-2134, 1994.
Higuchi K, Higuchi K, Kohno A, Yonezu T, Utani A, Umezawa 300. Mosteiro L, Pantoja C, Alcazar N, Marion RM, Chondronasiou D,
M, Takeda T. Age-related changes in bone mass in the senescence- Rovira M, Fernandez-Marcos PJ, Munoz-Martin M, Blanco-Aparicio
accelerated mouse (SAM). SAM-R/3 and SAM-P/6 as new murine C, Pastor J, Gomez-Lopez G, De Martino A, Blasco MA, Abad M,
models for senile osteoporosis. Am J Pathol 125: 276-283, 1986. Serrano M. Tissue damage and senescence provide critical signals for
280. McKane WR, Khosla S, Burritt MF, Kao PC, Wilson DM, Ory SJ, cellular reprogramming in vivo. Science 354: aaf4445, 2016.
Riggs BL. Mechanism of renal calcium conservation with estrogen 301. Mudhasani R, Zhu Z, Hutvagner G, Eischen CM, Lyle S, Hall LL,
replacement therapy in women in early postmenopause—a clinical Lawrence JB, Imbalzano AN, Jones SN. Loss of miRNA biogenesis
research center study. J Clin Endocrinol Metab 80: 3458-3464, 1995. induces p19Arf-p53 signaling and senescence in primary cells. J Cell
281. McKerrell T, Park N, Moreno T, Grove CS, Ponstingl H, Stephens J, Biol 181: 1055-1063, 2008.
Understanding Society Scientific Group, Crawley C, Craig J, Scott 302. Mullender MG, Tan SD, Vico L, Alexandre C, Klein-Nulend J.
MA, Hodkinson C, Baxter J, Rad R, Forsyth DR, Quail MA, Zeggini Differences in osteocyte density and bone histomorphometry between
E, Ouwehand W, Varela I, Vassiliou GS. Leukemia-associated somatic men and women and between healthy and osteoporotic subjects. Calcif
mutations drive distinct patterns of age-related clonal hemopoiesis. Tissue Int 77: 291-296, 2005.
Cell Rep 10: 1239-1245, 2015. 303. Munoz-Espin D, Canamero M, Maraver A, Gomez-Lopez G, Contr-
282. Mehrotra R. Disordered mineral metabolism and vascular calcification eras J, Murillo-Cuesta S, Rodriguez-Baeza A, Varela-Nieto I, Ruberte
in nondialyzed chronic kidney disease patients. J Ren Nutr 16: 100-118, J, Collado M, Serrano M. Programmed cell senescence during mam-
2006. malian embryonic development. Cell 155: 1104-1118, 2013.
283. Mellstrom D, Vandenput L, Mallmin H, Holmberg AH, Lorentzon M, 304. Nakamura T, Imai Y, Matsumoto T, Sato S, Takeuchi K, Igarashi K,
Oden A, Johansson H, Orwoll ES, Labrie F, Karlsson MK, Ljunggren Harada Y, Azuma Y, Krust A, Yamamoto Y, Nishina H, Takeda S,
O, Ohlsson C. Older men with low serum estradiol and high serum Takayanagi H, Metzger D, Kanno J, Takaoka K, Martin TJ, Chambon
SHBG have an increased risk of fractures. J Bone Miner Res 23: 1552- P, Kato S. Estrogen prevents bone loss via estrogen receptor alpha and
1560, 2008. induction of Fas ligand in osteoclasts. Cell 130: 811-823, 2007.
4382 Volume 13, January 2023
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Comprehensive Physiology Aging and Bone Metabolism
305. Nam HS, Kweon SS, Choi JS, Zmuda JM, Leung PC, Lui LY, Hill 328. Parfitt AM, Villanueva AR, Foldes J, Rao DS. Relations between
DD, Patrick AL, Cauley JA. Racial/ethnic differences in bone mineral histologic indices of bone formation: Implications for the pathogenesis
density among older women. J Bone Miner Metab 31: 190-198, 2013. of spinal osteoporosis. J Bone Miner Res 10: 466-473, 1995.
306. Narita M, Nunez S, Heard E, Narita M, Lin AW, Hearn SA, Spector 329. Perkins SL, Gibbons R, Kling S, Kahn AJ. Age-related bone loss in
DL, Hannon GJ, Lowe SW. Rb-mediated heterochromatin formation mice is associated with an increased osteoclast progenitor pool. Bone
and silencing of E2F target genes during cellular senescence. Cell 113: 15: 65-72, 1994.
703-716, 2003. 330. Pernow Y, Hauge EM, Linder K, Dahl E, Saaf M. Bone histomorphom-
307. Nehlin JO, Jafari A, Tencerova M, Kassem M. Aging and lineage allo- etry in male idiopathic osteoporosis. Calcif Tissue Int 84: 430-438,
cation changes of bone marrow skeletal (stromal) stem cells. Bone 123: 2009.
265-273, 2019. 331. Piemontese M, Almeida M, Robling AG, Kim HN, Xiong J, Thosten-
308. Neumann K, Endres M, Ringe J, Flath B, Manz R, Häupl T, Sittinger son JD, Weinstein RS, Manolagas SC, O’Brien CA, Jilka RL. Old age
M, Kaps C. BMP7 promotes adipogenic but not osteo-/chondrogenic causes de novo intracortical bone remodeling and porosity in mice.
differentiation of adult human bone marrow-derived stem cells in high- JCI Insight 2: e93771, 2017.
density micro-mass culture. J Cell Biochem 102: 626-637, 2007. 332. Pignolo RJ, Al Mukaddam M. Evaluation of bone fragility and fracture
309. Nijnik A, Woodbine L, Marchetti C, Dawson S, Lambe T, Liu C, prevention. In: Pignolo RJ, Ahn J, editors. Fractures in the Elderly:
Rodrigues NP, Crockford TL, Cabuy E, Vindigni A, Enver T, Bell A Guide to Practicalmanagment (2nd ed). Humana Press, 2018, p. 285-
JI, Slijepcevic P, Goodnow CC, Jeggo PA, Cornall RJ. DNA repair 301.
is limiting for haematopoietic stem cells during ageing. Nature 447: 333. Pignolo RJ, Law SF, Chandra A. Bone aging, cellular senescence,
686-690, 2007. and osteoporosis. JBMR Plus 5: e10488, 2021.
310. Nishimura Y, Fukuoka H, Kiriyama M, Suzuki Y, Oyama K, Ikawa S, 334. Pignolo RJ, Passos JF, Khosla S, Tchkonia T, Kirkland JL. Reduc-
Higurashi M, Gunji A. Bone turnover and calcium metabolism during ing senescent cell burden in aging and disease. Trends Mol Med 26:
630-638, 2020.
20 days bed rest in young healthy males and females. Acta Physiol 335. Pignolo RJ, Samsonraj RM, Law SF, Wang H, Chandra A. Targeting
Scand Suppl 616: 27-35, 1994. cell senescence for the treatment of age-related bone loss. Curr Osteo-
311. Niziolek PJ, Bullock W, Warman ML, Robling AG. Missense muta- poros Rep 17: 70-85, 2019.
tions in LRP5 associated with high bone mass protect the mouse skele- 336. Pignolo RJ, Suda RK, McMillan EA, Shen J, Lee SH, Choi Y,
ton from disuse- and ovariectomy-induced osteopenia. PLoS One 10: Wright AC, Johnson FB. Defects in telomere maintenance molecules
e0140775, 2015. impair osteoblast differentiation and promote osteoporosis. Aging Cell
312. Okada M, Kim HW, Matsu-ura K, Wang YG, Xu M, Ashraf M. 7: 23-31, 2008.
Abrogation of age-induced microRNA-195 rejuvenates the senescent 337. Piney A. Anatomy of the bone marrow with special reference to the
mesenchymal stem cells by reactivating telomerase. Stem Cells 34: distribution of red marrow. Br Med J 2: 792-795, 1922.
148-159, 2016. 338. Pocock NA, Eisman JA, Hopper JL, Yeates MG, Sambrook PN, Eberl
313. Olovnikov AM. Principle of marginotomy in template synthesis of S. Genetic determinants of bone mass in adults. A twin study. J Clin
polynucleotides. Dokl Akad Nauk SSSR 201: 1496-1499, 1971. Invest 80: 706-710, 1987.
314. Ominsky MS, Libanati C, Niu QT, Boyce RW, Kostenuik PJ, Wagman 339. Qiao W, Yu S, Sun H, Chen L, Wang R, Wu X, Goltzman D, Miao
RB, Baron R, Dempster DW. Sustained modeling-based bone D. 1,25-Dihydroxyvitamin D insufficiency accelerates age-related
formation during adulthood in cynomolgus monkeys may contribute bone loss by increasing oxidative stress and cell senescence. Am J
to continuous BMD gains with denosumab. J Bone Miner Res 30: Transl Res 12: 507-518, 2020.
1280-1289, 2015. 340. Qu Q, Perala-Heape M, Kapanen A, Dahllund J, Salo J, Vaananen HK,
315. Ominsky MS, Niu QT, Li C, Li X, Ke HZ. Tissue-level mechanisms Harkonen P. Estrogen enhances differentiation of osteoblasts in mouse
responsible for the increase in bone formation and bone volume by bone marrow culture. Bone 22: 201-209, 1998.
sclerostin antibody. J Bone Miner Res 29: 1424-1430, 2014. 341. Rajagopalan S, Long EO. Cellular senescence induced by CD158d
316. Omodei U, Mazziotti G, Donarini G, Gola M, Guella V, Pagani F, reprograms natural killer cells to promote vascular remodeling. Proc
Bugari G, Porcelli T, Giustina A. Effects of recombinant follicle- Natl Acad Sci U S A 109: 20596-20601, 2012.
stimulating hormone on bone turnover markers in infertile women 342. Rasheed N, Wang X, Niu QT, Yeh J, Li B. Atm-deficient mice:
undergoing in vitro fertilization procedure. J Clin Endocrinol Metab An osteoporosis model with defective osteoblast differentiation and
98: 330-336, 2013. increased osteoclastogenesis. Hum Mol Genet 15: 1938-1948, 2006.
317. Orwoll ES. Men, bone and estrogen: Unresolved issues. Osteoporos Int 343. Rauner M, Sipos W, Pietschmann P. Age-dependent Wnt gene expres-
14: 93-98, 2003. sion in bone and during the course of osteoblast differentiation. Age
318. Orwoll ES, Vanderschueren D, Boonen S. Osteoporosis in men: Epi- (Dordr) 30: 273-282, 2008.
demiology, pathophysiology, and clinical characterization. In: Marcus 344. Rehman MT, Hoyland JA, Denton J, Freemont AJ. Age related his-
R, Feldman D, Dempster DW, Luckey M, Cauley JA, editors. Osteo- tomorphometric changes in bone in normal British men and women.
porosis (4th ed). San Diego, CA: Academic Press, 2013, p. 757-802. J Clin Pathol 47: 529-534, 1994.
319. Oursler MJ, Cortese C, Keeting P, Anderson MA, Bonde SK, Riggs 345. Reid IR. Relationships among body mass, its components, and bone.
BL, Spelsberg TC. Modulation of transforming growth factor-beta Bone 31: 547-555, 2002.
production in normal human osteoblast-like cells by 17 beta-estradiol 346. Reya T, Duncan AW, Ailles L, Domen J, Scherer DC, Willert K, Hintz
and parathyroid hormone. Endocrinology 129: 3313-3320, 1991. L, Nusse R, Weissman IL. A role for Wnt signalling in self-renewal of
320. Owen TA, Aronow MS, Barone LM, Bettencourt B, Stein GS, Lian haematopoietic stem cells. Nature 423: 409-414, 2003.
JB. Pleiotropic effects of vitamin D on osteoblast gene expression 347. Richards JB, Kavvoura FK, Rivadeneira F, Styrkarsdottir U, Estrada K,
are related to the proliferative and differentiated state of the bone cell Halldorsson BV, Hsu YH, Zillikens MC, Wilson SG, Mullin BH, Amin
phenotype: Dependency upon basal levels of gene expression, duration N, Aulchenko YS, Cupples LA, Deloukas P, Demissie S, Hofman A,
of exposure, and bone matrix competency in normal rat osteoblast Kong A, Karasik D, van Meurs JB, Oostra BA, Pols HA, Sigurdsson
G, Thorsteinsdottir U, Soranzo N, Williams FM, Zhou Y, Ralston SH,
cultures. Endocrinology 128: 1496-1504, 1991. Thorleifsson G, van Duijn CM, Kiel DP, Stefansson K, Uitterlinden
321. Ozgenc A, Loeb LA. Current advances in unraveling the function of AG, Ioannidis JP, Spector TD, Genetic Factors for Osteoporosis Con-
the Werner syndrome protein. Mutat Res 577: 237-251, 2005. sortium. Collaborative meta-analysis: Associations of 150 candidate
322. Paccou J, Penel G, Chauveau C, Cortet B, Hardouin P. Marrow adipos- genes with osteoporosis and osteoporotic fracture. Ann Intern Med 151:
ity and bone: Review of clinical implications. Bone 118: 8-15, 2019. 528-537, 2009.
323. Pal L, Santoro N. Premature ovarian failure (POF): Discordance 348. Richards JB, Rivadeneira F, Inouye M, Pastinen TM, Soranzo N, Wil-
between somatic and reproductive aging. Ageing Res Rev 1: 413-423, son SG, Andrew T, Falchi M, Gwilliam R, Ahmadi KR, Valdes AM,
2002. Arp P, Whittaker P, Verlaan DJ, Jhamai M, Kumanduri V, Moorhouse
324. Panczyszyn A, Boniewska-Bernacka E, Goc A. The role of telomeres M, van Meurs JB, Hofman A, Pols HA, Hart D, Zhai G, Kato BS, Mullin
and telomerase in the senescence of postmitotic cells. DNA Repair BH, Zhang F, Deloukas P, Uitterlinden AG, Spector TD. Bone min-
(Amst) 95: 102956, 2020. eral density, osteoporosis, and osteoporotic fractures: A genome-wide
325. Pang WW, Price EA, Sahoo D, Beerman I, Maloney WJ, Rossi DJ, association study. Lancet 371: 1505-1512, 2008.
Schrier SL, Weissman IL. Human bone marrow hematopoietic stem 349. Riggs BL, Khosla S, Melton LJ 3rd. A unitary model for involutional
cells are increased in frequency and myeloid-biased with age. Proc Natl osteoporosis: Estrogen deficiency causes both type I and type II osteo-
Acad Sci U S A 108: 20012-20017, 2011. porosis in postmenopausal women and contributes to bone loss in aging
326. Parfitt AM. The coupling of bone formation to bone resorption: A crit- men. J Bone Miner Res 13: 763-773, 1998.
ical analysis of the concept and of its relevance to the pathogenesis of 350. Riggs BL, Melton Iii LJ 3rd, Robb RA, Camp JJ, Atkinson EJ,
osteoporosis. Metab Bone Dis Relat Res 4: 1-6, 1982. Peterson JM, Rouleau PA, McCollough CH, Bouxsein ML, Khosla S.
327. Parfitt AM. Osteonal and hemi-osteonal remodeling: The spatial and Population-based study of age and sex differences in bone volumetric
temporal framework for signal traffic in adult human bone. J Cell density, size, geometry, and structure at different skeletal sites. J Bone
Biochem 55: 273-286, 1994. Miner Res 19: 1945-1954, 2004.
Volume 13, January 2023 4383
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
351. Riggs BL, Melton LJ, Robb RA, Camp JJ, Atkinson EJ, McDaniel 374. Sedrine WB, Chevallier T, Zegels B, Kvasz A, Micheletti MC, Gelas B,
L, Amin S, Rouleau PA, Khosla S. A population-based assessment of Reginster JY. Development and assessment of the osteoporosis index of
rates of bone loss at multiple skeletal sites: Evidence for substantial risk (OSIRIS) to facilitate selection of women for bone densitometry.
trabecular bone loss in young adult women and men. J Bone Miner Res Gynecol Endocrinol 16: 245-250, 2002.
23: 205-214, 2008. 375. Seeman E. Pathogenesis of bone fragility in women and men. Lancet
352. Ritschka B, Storer M, Mas A, Heinzmann F, Ortells MC, Morton 359: 1841-1850, 2002.
JP, Sansom OJ, Zender L, Keyes WM. The senescence-associated 376. Shen H, Grimston S, Civitelli R, Thomopoulos S. Deletion of con-
secretory phenotype induces cellular plasticity and tissue regeneration. nexin43 in osteoblasts/osteocytes leads to impaired muscle formation
Genes Dev 31: 172-183, 2017. in mice. J Bone Miner Res 30: 596-605, 2015.
353. Rivadeneira F, Styrkarsdottir U, Estrada K, Halldorsson BV, Hsu 377. Shen W, Scherzer R, Gantz M, Chen J, Punyanitya M, Lewis CE,
YH, Richards JB, Zillikens MC, Kavvoura FK, Amin N, Aulchenko Grunfeld C. Relationship between MRI-measured bone marrow
YS, Cupples LA, Deloukas P, Demissie S, Grundberg E, Hofman adipose tissue and hip and spine bone mineral density in African-
A, Kong A, Karasik D, van Meurs JB, Oostra B, Pastinen T, Pols American and Caucasian participants: The CARDIA study. J Clin
HA, Sigurdsson G, Soranzo N, Thorleifsson G, Thorsteinsdottir U, Endocrinol Metab 97: 1337-1346, 2012.
Williams FM, Wilson SG, Zhou Y, Ralston SH, van Duijn CM, Spector 378. Shepherd JA, Schousboe JT, Broy SB, Engelke K, Leslie WD. Exec-
T, Kiel DP, Stefansson K, Ioannidis JP, Uitterlinden AG, Genetic Fac- utive summary of the 2015 ISCD position development conference on
tors for Osteoporosis Consortium. Twenty bone-mineral-density loci advanced measures from DXA and QCT: Fracture prediction beyond
identified by large-scale meta-analysis of genome-wide association BMD. J Clin Densitom 18: 274-286, 2015.
studies. Nat Genet 41: 1199-1206, 2009. 379. Shumaker DK, Dechat T, Kohlmaier A, Adam SA, Bozovsky MR,
354. Robbins J, Aragaki AK, Kooperberg C, Watts N, Wactawski-Wende J, Erdos MR, Eriksson M, Goldman AE, Khuon S, Collins FS, Jenuwein
Jackson RD, LeBoff MS, Lewis CE, Chen Z, Stefanick ML, Cauley J. T, Goldman RD. Mutant nuclear lamin A leads to progressive alter-
Factors associated with 5-year risk of hip fracture in postmenopausal ations of epigenetic control in premature aging. Proc Natl Acad Sci
women. JAMA 298: 2389-2398, 2007. U S A 103: 8703-8708, 2006.
355. Robles SJ, Adami GR. Agents that cause DNA double strand breaks 380. Simonsen JL, Rosada C, Serakinci N, Justesen J, Stenderup K, Rattan
lead to p16INK4a enrichment and the premature senescence of normal SI, Jensen TG, Kassem M. Telomerase expression extends the pro-
fibroblasts. Oncogene 16: 1113-1123, 1998. liferative life-span and maintains the osteogenic potential of human
356. Rocca WA, Gazzuola-Rocca L, Smith CY, Grossardt BR, Faubion SS, bone marrow stromal cells. Nat Biotechnol 20: 592-596, 2002.
Shuster LT, Kirkland JL, Stewart EA, Miller VM. Accelerated accumu- 381. Singh L, Brennan TA, Russell E, Kim JH, Chen Q, Brad Johnson F,
lation of multimorbidity after bilateral oophorectomy: A population- Pignolo RJ. Aging alters bone-fat reciprocity by shifting in vivo mes-
based cohort study. Mayo Clin Proc 91: 1577-1589, 2016. enchymal precursor cell fate towards an adipogenic lineage. Bone 85:
357. Rocca WA, Gazzuola Rocca L, Smith CY, Grossardt BR, Faubion SS, 29-36, 2016.
Shuster LT, Kirkland JL, Stewart EA, Miller VM. Bilateral oophorec- 382. Slemenda CW, Longcope C, Zhou L, Hui SL, Peacock M, Johnston
tomy and accelerated aging: Cause or effect? J Gerontol A Biol Sci Med CC. Sex steroids and bone mass in older men. Positive associations
Sci 72: 1213-1217, 2017. with serum estrogens and negative associations with androgens. J Clin
358. Rodier F, Coppe JP, Patil CK, Hoeijmakers WA, Munoz DP, Raza SR, Invest 100: 1755-1759, 1997.
Freund A, Campeau E, Davalos AR, Campisi J. Persistent DNA damage 383. Sloan KE, Bohnsack MT, Watkins NJ. The 5S RNP couples p53 home-
signalling triggers senescence-associated inflammatory cytokine secre- ostasis to ribosome biogenesis and nucleolar stress. Cell Rep 5: 237-
tion. Nat Cell Biol 11: 973-979, 2009. 247, 2013.
359. Rolvien T, Amling M. Disuse osteoporosis: Clinical and mechanistic 384. Smith EL, Gilligan C, McAdam M, Ensign CP, Smith PE. Deter-
insights. Calcif Tissue Int 110: 592-604, 2022. ring bone loss by exercise intervention in premenopausal and
360. Rosen CJ, Ackert-Bicknell C, Rodriguez JP, Pino AM. Marrow fat and postmenopausal women. Calcif Tissue Int 44: 312-321, 1989.
the bone microenvironment: Developmental, functional, and patholog- 385. Snyder PJ, Kopperdahl DL, Stephens-Shields AJ, Ellenberg SS, Cauley
ical implications. Crit Rev Eukaryot Gene Expr 19: 109-124, 2009.
361. Rossi DJ, Bryder D, Seita J, Nussenzweig A, Hoeijmakers J, Weiss- JA, Ensrud KE, Lewis CE, Barrett-Connor E, Schwartz AV, Lee DC,
man IL. Deficiencies in DNA damage repair limit the function of Bhasin S, Cunningham GR, Gill TM, Matsumoto AM, Swerdloff RS,
haematopoietic stem cells with age. Nature 447: 725-729, 2007. Basaria S, Diem SJ, Wang C, Hou X, Cifelli D, Dougar D, Zeldow B,
362. Rossi DJ, Bryder D, Zahn JM, Ahlenius H, Sonu R, Wagers AJ, Bauer DC, Keaveny TM. Effect of testosterone treatment on volumet-
Weissman IL. Cell intrinsic alterations underlie hematopoietic stem ric bone density and strength in older men with low testosterone: A
cell aging. Proc Natl Acad Sci U S A 102: 9194-9199, 2005. controlled clinical trial. JAMA Intern Med 177: 471-479, 2017.
363. Roux C, Briot K. Imminent fracture risk. Osteoporos Int 28: 1765-1769, 386. So AY, Jung JW, Lee S, Kim HS, Kang KS. DNA methyltransferase
2017. controls stem cell aging by regulating BMI1 and EZH2 through
364. Rozman C, Reverter JC, Feliu E, Berga L, Rozman M, Climent C. Vari- microRNAs. PLoS One 6: e19503, 2011.
ations of fat tissue fraction in abnormal human bone marrow depend 387. Solomon L. Osteoporosis and fracture of the femoral neck in the South
both on size and number of adipocytes: A stereologic study. Blood 76: African Bantu. J Bone Joint Surg Br 50: 2-13, 1968.
892-895, 1990. 388. Sparmann A, van Lohuizen M. Polycomb silencers control cell fate,
365. Rube CE, Fricke A, Widmann TA, Furst T, Madry H, Pfreundschuh development and cancer. Nat Rev Cancer 6: 846-856, 2006.
M, Rube C. Accumulation of DNA damage in hematopoietic stem and 389. Srinivasan S, Weimer DA, Agans SC, Bain SD, Gross TS. Low-
progenitor cells during human aging. PLoS One 6: e17487, 2011. magnitude mechanical loading becomes osteogenic when rest is
366. Rubin C, Turner AS, Bain S, Mallinckrodt C, McLeod K. Anabolism. inserted between each load cycle. J Bone Miner Res 17: 1613-1620,
Low mechanical signals strengthen long bones. Nature 412: 603-604, 2002.
2001. 390. Stein GH, Drullinger LF, Soulard A, Dulic V. Differential roles for
367. Rubin KH, Abrahamsen B, Friis-Holmberg T, Hjelmborg JV, Bech M, cyclin-dependent kinase inhibitors p21 and p16 in the mechanisms of
Hermann AP, Barkmann R, Gluer CC, Brixen K. Comparison of differ- senescence and differentiation in human fibroblasts. Mol Cell Biol 19:
ent screening tools (FRAX(R), OST, ORAI, OSIRIS, SCORE and age 2109-2117, 1999.
alone) to identify women with increased risk of fracture. A population- 391. Stevens JR, Miranda-Carboni GA, Singer MA, Brugger SM, Lyons
based prospective study. Bone 56: 16-22, 2013. KM, Lane TF. Wnt10b deficiency results in age-dependent loss of
368. Russo D, Battaglia Y. Clinical Significance of FGF-23 in Patients with bone mass and progressive reduction of mesenchymal progenitor cells.
CKD. Int J Nephrol 2011: 364890, 2011. J Bone Miner Res 25: 2138-2147, 2010.
369. Sabatakos G, Sims NA, Chen J, Aoki K, Kelz MB, Amling M, Bouali 392. Stier S, Ko Y, Forkert R, Lutz C, Neuhaus T, Grunewald E, Cheng T,
Y, Mukhopadhyay K, Ford K, Nestler EJ, Baron R. Overexpression of Dombkowski D, Calvi LM, Rittling SR, Scadden DT. Osteopontin is a
DeltaFosB transcription factor(s) increases bone formation and inhibits hematopoietic stem cell niche component that negatively regulates stem
adipogenesis. Nat Med 6: 985-990, 2000. cell pool size. J Exp Med 201: 1781-1791, 2005.
370. Saeed H, Abdallah BM, Ditzel N, Catala-Lehnen P, Qiu W, Amling 393. Storer M, Mas A, Robert-Moreno A, Pecoraro M, Ortells MC, Di Gia-
M, Kassem M. Telomerase-deficient mice exhibit bone loss owing to como V, Yosef R, Pilpel N, Krizhanovsky V, Sharpe J, Keyes WM.
defects in osteoblasts and increased osteoclastogenesis by inflamma- Senescence is a developmental mechanism that contributes to embry-
tory microenvironment. J Bone Miner Res 26: 1494-1505, 2011. onic growth and patterning. Cell 155: 1119-1130, 2013.
371. Schousboe JT. Epidemiology of vertebral fractures. J Clin Densitom 394. Stringer B, Waddington R, Houghton A, Stone M, Russell G, Foster G.
19: 8-22, 2016. Serum from postmenopausal women directs differentiation of human
372. Schuit SC, van der Klift M, Weel AE, de Laet CE, Burger H, Seeman clonal osteoprogenitor cells from an osteoblastic toward an adipocytic
E, Hofman A, Uitterlinden AG, van Leeuwen JP, Pols HA. Fracture phenotype. Calcif Tissue Int 80: 233-243, 2007.
incidence and association with bone mineral density in elderly men and 395. Styrkarsdottir U, Halldorsson BV, Gretarsdottir S, Gudbjartsson DF,
women: The Rotterdam Study. Bone 34: 195-202, 2004. Walters GB, Ingvarsson T, Jonsdottir T, Saemundsdottir J, Center JR,
373. Sedivy JM, Banumathy G, Adams PD. Aging by epigenetics—a con- Nguyen TV, Bagger Y, Gulcher JR, Eisman JA, Christiansen C, Sig-
sequence of chromatin damage? Exp Cell Res 314: 1909-1917, 2008. urdsson G, Kong A, Thorsteinsdottir U, Stefansson K. Multiple genetic
4384 Volume 13, January 2023
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Comprehensive Physiology Aging and Bone Metabolism
loci for bone mineral density and fractures. N Engl J Med 358: 2355- 419. Tran B, Center JR, Nguyen TV. Translational genetics of osteoporo-
2365, 2008. sis: From population association to individualized assessment. In:
396. Styrkarsdottir U, Halldorsson BV, Gretarsdottir S, Gudbjartsson DF, Bilezikian JP, editor. Primer on the Metabolic Bone Diseases and
Walters GB, Ingvarsson T, Jonsdottir T, Saemundsdottir J, Snorradottir Disorders of Mineral Metabolism. Hoboken, NJ: Wiley-Blackwell,
S, Center JR, Nguyen TV, Alexandersen P, Gulcher JR, Eisman JA, 2019, p. 385-392.
Christiansen C, Sigurdsson G, Kong A, Thorsteinsdottir U, Stefansson 420. Tu X, Delgado-Calle J, Condon KW, Maycas M, Zhang H, Carlesso N,
K. New sequence variants associated with bone mineral density. Nat Taketo MM, Burr DB, Plotkin LI, Bellido T. Osteocytes mediate the
Genet 41: 15-17, 2009. anabolic actions of canonical Wnt/beta-catenin signaling in bone. Proc
397. Styrkarsdottir U, Thorleifsson G, Eiriksdottir B, Gudjonsson SA, Natl Acad Sci U S A 112: E478-E486, 2015.
Ingvarsson T, Center JR, Nguyen TV, Eisman JA, Christiansen C, 421. Turinetto V, Vitale E, Giachino C. Senescence in human mesenchy-
Thorsteinsdottir U, Sigurdsson G, Stefansson K. Two rare mutations mal stem cells: Functional changes and implications in stem cell-based
in the COL1A2 gene associate with low bone mineral density and therapy. Int J Mol Sci 17: 1164, 2016.
fractures in iceland. J Bone Miner Res 31: 173-179, 2016. 422. Turner CH. Biomechanics of bone: Determinants of skeletal fragility
398. Styrkarsdottir U, Thorleifsson G, Sulem P, Gudbjartsson DF, Sigurds- and bone quality. Osteoporos Int 13: 97-104, 2002.
son A, Jonasdottir A, Jonasdottir A, Oddsson A, Helgason A, Mag- 423. Turner CH, Burr DB. Basic biomechanical measurements of bone: A
nusson OT, Walters GB, Frigge ML, Helgadottir HT, Johannsdottir H, tutorial. Bone 14: 595-608, 1993.
Bergsteinsdottir K, Ogmundsdottir MH, Center JR, Nguyen TV, Eis- 424. Uebelhart D, Demiaux-Domenech B, Roth M, Chantraine A. Bone
man JA, Christiansen C, Steingrimsson E, Jonasson JG, Tryggvadottir metabolism in spinal cord injured individuals and in others who have
L, Eyjolfsson GI, Theodors A, Jonsson T, Ingvarsson T, Olafsson I, prolonged immobilisation. A review. Paraplegia 33: 669-673, 1995.
Rafnar T, Kong A, Sigurdsson G, Masson G, Thorsteinsdottir U, Ste- 425. Uhthoff HK, Jaworski ZF. Bone loss in response to long-term immo-
fansson K. Nonsense mutation in the LGR4 gene is associated with bilisation. J Bone Joint Surg Br 60-B: 420-429, 1978.
several human diseases and other traits. Nature 497: 517-520, 2013. 426. Uihlein AV, Finkelstein JS, Lee H, Leder BZ. FSH suppression does
399. Suchacki KJ, Cawthorn WP, Rosen CJ. Bone marrow adipose tissue: not affect bone turnover in eugonadal men. J Clin Endocrinol Metab
Formation, function and regulation. Curr Opin Pharmacol 28: 50-56, 99: 2510-2515, 2014.
2016. 427. van Staa TP, Leufkens HG, Cooper C. Does a fracture at one site predict
400. Suda T, Udagawa N, Nakamura I, Miyaura C, Takahashi N. Modulation later fractures at other sites? A British cohort study. Osteoporos Int 13:
of osteoclast differentiation by local factors. Bone 17: S87-S91, 1995. 624-629, 2002.
401. Sun L, Peng Y, Sharrow AC, Iqbal J, Zhang Z, Papachristou DJ, Zaidi 428. Vanderschueren D, Laurent MR, Claessens F, Gielen E, Lagerquist
S, Zhu LL, Yaroslavskiy BB, Zhou H, Zallone A, Sairam MR, Kumar MK, Vandenput L, Borjesson AE, Ohlsson C. Sex steroid actions in
TR, Bo W, Braun J, Cardoso-Landa L, Schaffler MB, Moonga BS, Blair male bone. Endocr Rev 35: 906-960, 2014.
HC, Zaidi M. FSH directly regulates bone mass. Cell 125: 247-260, 429. Varela I, Pereira S, Ugalde AP, Navarro CL, Suarez MF, Cau P, Cadi-
2006. nanos J, Osorio FG, Foray N, Cobo J, de Carlos F, Levy N, Freije JM,
402. Sun LQ, Lee DW, Zhang Q, Xiao W, Raabe EH, Meeker A, Miao D, Lopez-Otin C. Combined treatment with statins and aminobisphospho-
Huso DL, Arceci RJ. Growth retardation and premature aging pheno- nates extends longevity in a mouse model of human premature aging.
types in mice with disruption of the SNF2-like gene, PASG. Genes Dev Nat Med 14: 767-772, 2008.
18: 1035-1046, 2004. 430. Vashishth D, Verborgt O, Divine G, Schaffler MB, Fyhrie DP. Decline
403. Szulc P, Munoz F, Claustrat B, Garnero P, Marchand F, Duboeuf F, in osteocyte lacunar density in human cortical bone is associated with
Delmas PD. Bioavailable estradiol may be an important determinant of accumulation of microcracks with age. Bone 26: 375-380, 2000.
osteoporosis in men: The MINOS study. J Clin Endocrinol Metab 86: 431. Vasileiou PVS, Evangelou K, Vlasis K, Fildisis G, Panayiotidis MI,
192-199, 2001. Chronopoulos E, Passias PG, Kouloukoussa M, Gorgoulis VG, Havaki
404. Szulc P, Seeman E, Duboeuf F, Sornay-Rendu E, Delmas PD. Bone S. Mitochondrial homeostasis and cellular senescence. Cells 8: 686,
fragility: Failure of periosteal apposition to compensate for increased 2019.
endocortical resorption in postmenopausal women. J Bone Miner Res
21: 1856-1863, 2006. 432. Vassilopoulou-Sellin R, Brosnan P, Delpassand A, Zietz H, Klein MJ,
405. Taipaleenmäki H, Abdallah BM, Al Dahmash A, Saamanen AM, Jaffe N. Osteopenia in young adult survivors of childhood cancer. Med
Kassem M. Wnt signalling mediates the cross-talk between bone Pediatr Oncol 32: 272-278, 1999.
marrow derived pre-adipocytic and pre-osteoblastic cell populations. 433. Vogel H, Lim DS, Karsenty G, Finegold M, Hasty P. Deletion of Ku86
Exp Cell Res 317: 745-756, 2011. causes early onset of senescence in mice. Proc Natl Acad Sci U S A 96:
406. Takada I, Kouzmenko AP, Kato S. Wnt and PPARgamma signaling in 10770-10775, 1999.
osteoblastogenesis and adipogenesis. Nat Rev Rheumatol 5: 442-447, 434. von Friesendorff M, McGuigan FE, Wizert A, Rogmark C, Holmberg
2009. AH, Woolf AD, Akesson K. Hip fracture, mortality risk, and cause of
407. Takashi Y, Fukumoto S. FGF23-Klotho axis in CKD. Renal Replac- death over two decades. Osteoporos Int 27: 2945-2953, 2016.
ment Ther 2: 2-20, 2016. 435. Vrtacnik P, Zupan J, Mlakar V, Kranjc T, Marc J, Kern B, Ostanek
408. Takata S, Yasui N. Disuse osteoporosis. J Med Investig 48: 147-156, B. Epigenetic enzymes influenced by oxidative stress and hypoxia
2001. mimetic in osteoblasts are differentially expressed in patients with
409. Takeda T, Higuchi K, Hosokawa M. Senescence-accelerated mouse osteoporosis and osteoarthritis. Sci Rep 8: 16215, 2018.
(SAM): With special reference to development and pathological 436. Wagner H, Melhus H, Pedersen NL, Michaelsson K. Genetic influ-
phenotypes. ILAR J 38: 109-118, 1997. ence on bone phenotypes and body composition: A Swedish twin study.
410. Takeda T, Hosokawa M, Higuchi K. Senescence-accelerated J Bone Miner Metab 31: 681-689, 2013.
mouse (SAM): A novel murine model of senescence. Exp Gerontol 437. Wahl P, Wolf M. FGF23 in chronic kidney disease. Adv Exp Med Biol
32: 105-109, 1997. 728: 107-125, 2012.
411. Takeda T, Matsushita T, Kurozumi M, Takemura K, Higuchi K, 438. Wang B, Zhang S, Wu XY. Effects of microgravity on the gene expres-
Hosokawa M. Pathobiology of the senescence-accelerated mouse sion and cellular functions of osteoblasts. Space Med Med Eng (Beijing)
(SAM). Exp Gerontol 32: 117-127, 1997. 16: 227-230, 2003.
412. Tanaka S, Takahashi N, Udagawa N, Tamura T, Akatsu T, Stanley 439. Wang D, Cai G, Wang H, He J. TRAF3, a target of microRNA-
ER, Kurokawa T, Suda T. Macrophage colony-stimulating factor is 363-3p, suppresses senescence and regulates the balance between
indispensable for both proliferation and differentiation of osteoclast osteoblastic and adipocytic differentiation of rat bone marrow-derived
progenitors. J Clin Invest 91: 257-263, 1993. mesenchymal stem cells. Stem Cells Dev 29: 737-745, 2020.
413. Tavassoli M. Marrow adipose cells and hemopoiesis: An interpretative 440. Wang E. Senescent human fibroblasts resist programmed cell death, and
review. Exp Hematol 12: 139-146, 1984. failure to suppress bcl2 is involved. Cancer Res 55: 2284-2292, 1995.
414. Tavassoli M, editor. Fatty involution of marrow and the role of adipose 441. Wang GJ, Sweet DE, Reger SI, Thompson RC. Fat-cell changes as
tissue in hematopoiesis. In: Handbook of the Hemopoietic Microenvi- a mechanism of avascular necrosis of the femoral head in cortisone-
ronment. Clifton, NJ: Humana Press, 1989, p. 157-187. treated rabbits. J Bone Joint Surg Am 59: 729-735, 1977.
415. Taylor AJ, Gary LC, Arora T, Becker DJ, Curtis JR, Kilgore ML, Mor- 442. Wang H, Chen Q, Lee SH, Choi Y, Johnson FB, Pignolo RJ. Impair-
risey MA, Saag KG, Matthews R, Yun H, Smith W, Delzell E. Clinical ment of osteoblast differentiation due to proliferation-independent
and demographic factors associated with fractures among older Amer- telomere dysfunction in mouse models of accelerated aging. Aging
icans. Osteoporos Int 22: 1263-1274, 2011. Cell 11: 704-713, 2012.
416. Terzi MY, Izmirli M, Gogebakan B. The cell fate: Senescence or 443. Wang S, Prizment A, Thyagarajan B, Blaes A. Cancer treatment-
quiescence. Mol Biol Rep 43: 1213-1220, 2016. induced accelerated aging in cancer survivors: Biology and assessment.
417. Thandrayen K, Norris SA, Pettifor JM. Fracture rates in urban South Cancers (Basel) 13: 1-15, 2021.
African children of different ethnic origins: The birth to twenty cohort. 444. Waning DL, Mohammad KS, Reiken S, Xie W, Andersson DC, John
Osteoporos Int 20: 47-52, 2009. S, Chiechi A, Wright LE, Umanskaya A, Niewolna M, Trivedi T,
418. Tiede-Lewis LM, Dallas SL. Changes in the osteocyte lacunocanalicu- Charkhzarrin S, Khatiwada P, Wronska A, Haynes A, Benassi MS,
lar network with aging. Bone 122: 101-113, 2019. Witzmann FA, Zhen G, Wang X, Cao X, Roodman GD, Marks AR,
Volume 13, January 2023 4385
10.1002/cphy.c220012, Downloaded from https://onlinelibrary.wiley.com/doi/10.1002/cphy.c220012 by Nova Southeastern University, Wiley Online Library on [06/02/2023]. See the Terms and Conditions (https://onlinelibrary.wiley.com/terms-and-conditions) on Wiley Online Library for rules of use; OA articles are governed by the applicable Creative Commons License
Aging and Bone Metabolism Comprehensive Physiology
Guise TA. Excess TGF-beta mediates muscle weakness associated prevents the telomere shorting and replicative senescence in human
with bone metastases in mice. Nat Med 21: 1262-1271, 2015. osteoblasts. J Bone Miner Res 16: 1453-1464, 2001.
445. Watson JD. Origin of concatemeric T7 DNA. Nat New Biol 239: 197- 466. Yudoh K, Nishioka K. Telomerized presenescent osteoblasts prevent
201, 1972. bone mass loss in vivo. Gene Ther 11: 909-915, 2004.
446. Weber TJ. Battle of the sex steroids in the male skeleton: And the 467. Zampieri M, Ciccarone F, Calabrese R, Franceschi C, Burkle A, Caiafa
winner is. J Clin Invest 126: 829-832, 2016. P. Reconfiguration of DNA methylation in aging. Mech Ageing Dev
447. Wehrwein P. Stem cells: Repeat to fade. Nature 492: S12-S13, 2012. 151: 60-70, 2015.
448. Wein MN, Kronenberg HM. Regulation of bone remodeling by parathy- 468. Zayzafoon M, Gathings WE, McDonald JM. Modeled microgravity
roid hormone. Cold Spring Harb Perspect Med 8: a031237, 2018. inhibits osteogenic differentiation of human mesenchymal stem cells
449. Weitzmann MN, Cenci S, Rifas L, Brown C, Pacifici R. Interleukin-7 and increases adipogenesis. Endocrinology 145: 2421-2432, 2004.
stimulates osteoclast formation by up-regulating the T-cell production 469. Zebaze RM, Ghasem-Zadeh A, Bohte A, Iuliano-Burns S, Mirams M,
of soluble osteoclastogenic cytokines. Blood 96: 1873-1878, 2000. Price RI, Mackie EJ, Seeman E. Intracortical remodelling and poros-
450. Weivoda MM, Ruan M, Hachfeld CM, Pederson L, Howe A, Davey ity in the distal radius and post-mortem femurs of women: A cross-
RA, Zajac JD, Kobayashi Y, Williams BO, Westendorf JJ, Khosla S, sectional study. Lancet 375: 1729-1736, 2010.
Oursler MJ. Wnt signaling inhibits osteoclast differentiation by activat- 470. Zhang J, Pugh TD, Stebler B, Ershler WB, Keller ET. Orchiectomy
ing canonical and noncanonical cAMP/PKA pathways. J Bone Miner increases bone marrow interleukin-6 levels in mice. Calcif Tissue Int
Res 31: 65-75, 2016. 62: 219-226, 1998.
451. Wilson CL, Ness KK. Bone mineral density deficits and fractures in 471. Zhang W, Li J, Suzuki K, Qu J, Wang P, Zhou J, Liu X, Ren R, Xu
survivors of childhood cancer. Curr Osteoporos Rep 11: 329-337, 2013. X, Ocampo A, Yuan T, Yang J, Li Y, Shi L, Guan D, Pan H, Duan
452. Wink CS, Felts WJ. Effects of castration on the bone structure of male S, Ding Z, Li M, Yi F, Bai R, Wang Y, Chen C, Yang F, Li X, Wang
rats: A model of osteoporosis. Calcif Tissue Int 32: 77-82, 1980. Z, Aizawa E, Goebl A, Soligalla RD, Reddy P, Esteban CR, Tang F,
453. Wiren KM, Zhang XW, Olson DA, Turner RT, Iwaniec UT. Androgen Liu GH, Belmonte JC. Aging stem cells. A Werner syndrome stem cell
prevents hypogonadal bone loss via inhibition of resorption mediated model unveils heterochromatin alterations as a driver of human aging.
by mature osteoblasts/osteocytes. Bone 51: 835-846, 2012. Science 348: 1160-1163, 2015.
454. Wiswell RA, Hawkins SA, Dreyer HC, Jaque SV. Maintenance of 472. Zhang Z, Zhang Y, Zhou Z, Shi H, Qiu X, Xiong J, Chen Y. BDNF
BMD in older male runners is independent of changes in training regulates the expression and secretion of VEGF from osteoblasts via
volume or VO(2)peak. J Gerontol A Biol Sci Med Sci 57: M203-M208, the TrkB/ERK1/2 signaling pathway during fracture healing. Mol Med
2002. Rep 15: 1362-1367, 2017.
455. Wronski TJ, Morey-Holton E, Jee WS. Skeletal alterations in rats 473. Zheng HF, Forgetta V, Hsu YH, Estrada K, Rosello-Diez A, Leo PJ,
during space flight. Adv Space Res 1: 135-140, 1981. Dahia CL, Park-Min KH, Tobias JH, Kooperberg C, Kleinman A,
456. Wronski TJ, Walsh CC, Ignaszewski LA. Histologic evidence for Styrkarsdottir U, Liu CT, Uggla C, Evans DS, Nielson CM, Walter
osteopenia and increased bone turnover in ovariectomized rats. Bone K, Pettersson-Kymmer U, McCarthy S, Eriksson J, Kwan T, Jhamai
7: 119-123, 1986. M, Trajanoska K, Memari Y, Min J, Huang J, Danecek P, Wilmot B,
457. Xu M, Palmer AK, Ding H, Weivoda MM, Pirtskhalava T, White TA, Li R, Chou WC, Mokry LE, Moayyeri A, Claussnitzer M, Cheng CH,
Sepe A, Johnson KO, Stout MB, Giorgadze N, Jensen MD, LeBrasseur Cheung W, Medina-Gomez C, Ge B, Chen SH, Choi K, Oei L, Fraser
NK, Tchkonia T, Kirkland JL. Targeting senescent cells enhances J, Kraaij R, Hibbs MA, Gregson CL, Paquette D, Hofman A, Wibom
adipogenesis and metabolic function in old age. elife 4: e12997, 2015. C, Tranah GJ, Marshall M, Gardiner BB, Cremin K, Auer P, Hsu L,
458. Xu M, Tchkonia T, Ding H, Ogrodnik M, Lubbers ER, Pirtskhalava Ring S, Tung JY, Thorleifsson G, Enneman AW, van Schoor NM, de
T, White TA, Johnson KO, Stout MB, Mezera V, Giorgadze N, Jensen Groot LC, van der Velde N, Melin B, Kemp JP, Christiansen C, Sayers
MD, LeBrasseur NK, Kirkland JL. JAK inhibition alleviates the cel- A, Zhou Y, Calderari S, van Rooij J, Carlson C, Peters U, Berlivet
lular senescence-associated secretory phenotype and frailty in old age. S, Dostie J, Uitterlinden AG, Williams SR, Farber C, Grinberg D,
Proc Natl Acad Sci U S A 112: E6301-E6310, 2015. LaCroix AZ, Haessler J, Chasman DI, Giulianini F, Rose LM, Ridker
459. Yang R, Chen J, Zhang J, Qin R, Wang R, Qiu Y, Mao Z, Goltzman D, PM, Eisman JA, Nguyen TV, Center JR, Nogues X, Garcia-Giralt
Miao D. 1,25-Dihydroxyvitamin D protects against age-related osteo- N, Launer LL, Gudnason V, Mellstrom D, Vandenput L, Amin N,
porosis by a novel VDR-Ezh2-p16 signal axis. Aging Cell 19: e13095, van Duijn CM, Karlsson MK, Ljunggren O, Svensson O, Hallmans
2020. G, Rousseau F, Giroux S, Bussiere J, Arp PP, Koromani F, Prince
460. Yeh L-CC, Tsai AD, Lee JC. Osteogenic protein-1 (OP-1, BMP-7) RL, Lewis JR, Langdahl BL, Hermann AP, Jensen JE, Kaptoge S,
induces osteoblastic cell differentiation of the pluripotent mesenchy- Khaw KT, Reeve J, Formosa MM, Xuereb-Anastasi A, Akesson K,
mal cell line C2C12. J Cell Biochem 87: 292-304, 2002. McGuigan FE, Garg G, Olmos JM, Zarrabeitia MT, Riancho JA,
461. Yeung DK, Griffith JF, Antonio GE, Lee FK, Woo J, Leung PC. Osteo- Ralston SH, Alonso N, Jiang X, Goltzman D, Pastinen T, Grundberg
porosis is associated with increased marrow fat content and decreased E, Gauguier D, Orwoll ES, Karasik D, Davey-Smith G, Consortium
marrow fat unsaturation: A proton MR spectroscopy study. J Magn A, Smith AV, Siggeirsdottir K, Harris TB, Zillikens MC, van Meurs
Reson Imaging 22: 279-285, 2005. JB, Thorsteinsdottir U, Maurano MT, Timpson NJ, Soranzo N, Durbin
462. Young D, Hopper JL, Nowson CA, Green RM, Sherwin AJ, Kaymakci R, Wilson SG, Ntzani EE, Brown MA, Stefansson K, Hinds DA,
B, Smid M, Guest CS, Larkins RG, Wark JD. Determinants of bone Spector T, Cupples LA, Ohlsson C, Greenwood CM, Consortium UK,
mass in 10- to 26-year-old females: A twin study. J Bone Miner Res Jackson RD, Rowe DW, Loomis CA, Evans DM, Ackert-Bicknell
10: 558-567, 1995. CL, Joyner AL, Duncan EL, Kiel DP, Rivadeneira F, Richards JB.
463. Young MM, Nordin BE. Calcium metabolism and the menopause. Proc Whole-genome sequencing identifies EN1 as a determinant of bone
R Soc Med 60: 1137-1138, 1967. density and fracture. Nature 526: 112-117, 2015.
464. Yuan L, Chan GC, Fung KL, Chim CS. RANKL expression in myeloma 474. Zhou Q, Zhu L, Zhang D, Li N, Li Q, Dai P, Mao Y, Li X, Ma J, Huang
cells is regulated by a network involving RANKL promoter methy- S. Oxidative stress-related biomarkers in postmenopausal osteoporosis:
lation, DNMT1, microRNA and TNFalpha in the microenvironment. A systematic review and meta-analyses. Dis Markers 2016: 7067984,
Biochim Biophys Acta 1843: 1834-1838, 2014. 2016.
465. Yudoh K, Matsuno H, Nakazawa F, Katayama R, Kimura T. Recon-
stituting telomerase activity using the telomerase catalytic subunit
4386 Volume 13, January 2023
You might also like
- OsteoporosisDocument12 pagesOsteoporosispolog.jm610No ratings yet
- A Review On The Diseases and Treatments That Affect The Bone Physiology and StrengthDocument17 pagesA Review On The Diseases and Treatments That Affect The Bone Physiology and StrengthErnest Gabriel Cruz AdvinculaNo ratings yet
- Lorentz On 2015Document23 pagesLorentz On 2015Sanita AurinNo ratings yet
- JCM 11 06434 v2Document17 pagesJCM 11 06434 v2NeelamNo ratings yet
- Death&Birth 00Document23 pagesDeath&Birth 00kyz79No ratings yet
- Pathophysiology of Bone MetastasesDocument5 pagesPathophysiology of Bone MetastasesdyahNo ratings yet
- Update Osteoporosis Management (Listo)Document18 pagesUpdate Osteoporosis Management (Listo)Jossie AcuñaNo ratings yet
- Shoolar Ederly OsteoDocument9 pagesShoolar Ederly OsteoBayu Surya AwalludinNo ratings yet
- Osteoporosis: Best PracticeDocument7 pagesOsteoporosis: Best PracticePerez Wahyu PurnasariNo ratings yet
- Pathophysiology and Treatment of Osteoporosis: Challenges For Clinical Practice in Older PeopleDocument15 pagesPathophysiology and Treatment of Osteoporosis: Challenges For Clinical Practice in Older PeopleDeddy ZulkarnaenNo ratings yet
- Pathogenesis of Osteoporosis 2: Cli Ord J. RosenDocument13 pagesPathogenesis of Osteoporosis 2: Cli Ord J. RosenRonald TejoprayitnoNo ratings yet
- ARTIGO OsteoporoseDocument25 pagesARTIGO OsteoporoseIndiara Lorena Barros Ribeiro Da SilvaNo ratings yet
- Cagri Karaciklar Fragility Fractures EssayDocument7 pagesCagri Karaciklar Fragility Fractures EssayÇağrıNo ratings yet
- About The Authors: Luisella CianferottiDocument16 pagesAbout The Authors: Luisella CianferottiJamaluddin HaikhahNo ratings yet
- Osteoporosis: Pathophysiolog YDocument42 pagesOsteoporosis: Pathophysiolog YShared LifeNo ratings yet
- 1042 FullDocument9 pages1042 Fulloki harisandiNo ratings yet
- Asupan Mineral, Kadar Kolesterol Total Dan Kepadatan Mineral Tulang Pada LansiaDocument6 pagesAsupan Mineral, Kadar Kolesterol Total Dan Kepadatan Mineral Tulang Pada LansiaLutfia Ardina OFFICIALNo ratings yet
- Bone and The Immune SystemDocument14 pagesBone and The Immune SystemRebecca PinheiroNo ratings yet
- Advanced 3D Magnetic Scaffolds For Tumor-Related BDocument30 pagesAdvanced 3D Magnetic Scaffolds For Tumor-Related BCristina BancilaNo ratings yet
- Osteoporosis in The Aging Male: Treatment Options: BackgroundDocument16 pagesOsteoporosis in The Aging Male: Treatment Options: BackgroundcumbredinNo ratings yet
- Primary Osteoporosis in Postmenopausal WomenDocument5 pagesPrimary Osteoporosis in Postmenopausal WomenAzmi FarhadiNo ratings yet
- FRACTURESDocument35 pagesFRACTURESMichelle DuNo ratings yet
- An Overview of Osteoporosis in The Elderly Population Role of Nutrition and Physical ActivityDocument8 pagesAn Overview of Osteoporosis in The Elderly Population Role of Nutrition and Physical ActivityIJRASETPublicationsNo ratings yet
- Pathophysiology of OsteoarthritisDocument3 pagesPathophysiology of OsteoarthritisHajar ToharNo ratings yet
- BP MecanismDocument14 pagesBP MecanismAdryana StefyNo ratings yet
- OsteoporosisDocument19 pagesOsteoporosisTsedhonNo ratings yet
- Osteoporosis The Evolution in DiagnosisDocument12 pagesOsteoporosis The Evolution in DiagnosisPakistan RevolutionNo ratings yet
- Recent Advances in The Pathogenesis and Treatment of OsteoporosisDocument5 pagesRecent Advances in The Pathogenesis and Treatment of OsteoporosisAnil JohnNo ratings yet
- Westjmed00101 0065Document15 pagesWestjmed00101 0065zarrougonesNo ratings yet
- Normal Bone Formation and RemodelingDocument4 pagesNormal Bone Formation and RemodelingFernando AnibanNo ratings yet
- 13th Lecture OsteoporosisDocument3 pages13th Lecture OsteoporosisMuhammad KhalilNo ratings yet
- Asupan Mineral, Kadar Kolesterol Total Dan Kepadatan Mineral Tulang Pada LansiaDocument6 pagesAsupan Mineral, Kadar Kolesterol Total Dan Kepadatan Mineral Tulang Pada Lansiadwi elma safitriNo ratings yet
- Week 12 Article 1 BrickleyDocument16 pagesWeek 12 Article 1 BrickleyJean-Claude TissierNo ratings yet
- 2018 Update On OsteoporosisDocument16 pages2018 Update On OsteoporosisManel PopescuNo ratings yet
- Osteoporotic Vertebral Compression Fractures and VDocument13 pagesOsteoporotic Vertebral Compression Fractures and VChristopherLawrenceNo ratings yet
- Chapter 23: Osteoporosis of The SpineDocument15 pagesChapter 23: Osteoporosis of The SpineTraian UrsuNo ratings yet
- Task Related To Muscles and Bone ProblemDocument6 pagesTask Related To Muscles and Bone ProblemFOONG YI KUAN MoeNo ratings yet
- Div Class Title Diet Nutrition and The Prevention of Osteoporosis DivDocument17 pagesDiv Class Title Diet Nutrition and The Prevention of Osteoporosis DivLucas Oliveira MouraNo ratings yet
- Osteoporosis Iayu 3Document9 pagesOsteoporosis Iayu 3aanansyoriNo ratings yet
- A Review On Some Physiological Studies Related To OsteoporosisDocument14 pagesA Review On Some Physiological Studies Related To OsteoporosisAndy KumarNo ratings yet
- Fimmu 13 1005665Document14 pagesFimmu 13 1005665sopha seyhaNo ratings yet
- 5 .Document28 pages5 .Dewy Shinta PagalaNo ratings yet
- Screening, Diagnosis and Treatment of Osteoporosis: A Brief ReviewDocument7 pagesScreening, Diagnosis and Treatment of Osteoporosis: A Brief ReviewraffellaNo ratings yet
- mjm11 1p51Document7 pagesmjm11 1p51toaldoNo ratings yet
- Health Teaching Plan - OsteoporosisDocument9 pagesHealth Teaching Plan - OsteoporosisAudrie Allyson Gabales100% (2)
- Osteoporosis Review of EtiologyDocument17 pagesOsteoporosis Review of EtiologyClaudiaGuerreroNo ratings yet
- The Effect of Icariin On Bone Metabolism and Its Potential Clinical ApplicationDocument12 pagesThe Effect of Icariin On Bone Metabolism and Its Potential Clinical ApplicationBrenda MartinsNo ratings yet
- Osteoporosis: Chandraprakash D. Khedkar Gulab Dattarao KhedkarDocument7 pagesOsteoporosis: Chandraprakash D. Khedkar Gulab Dattarao Khedkardafa bintangNo ratings yet
- Secondary Osteoporosis - A Still Neglected ConditionDocument4 pagesSecondary Osteoporosis - A Still Neglected ConditionClaudiaGuerreroNo ratings yet
- Pathophysiology AssignmentDocument12 pagesPathophysiology AssignmentBalqis HyoleeNo ratings yet
- Aging and Bone Loss: New Insights For The Clinician: Oddom Demontiero, Christopher Vidal and Gustavo DuqueDocument16 pagesAging and Bone Loss: New Insights For The Clinician: Oddom Demontiero, Christopher Vidal and Gustavo DuqueNariyyahNo ratings yet
- Pathophysiology of Osteoporosis: Robert P Heaney, MD, Facp, FainDocument6 pagesPathophysiology of Osteoporosis: Robert P Heaney, MD, Facp, FainMaram NurainiNo ratings yet
- OsteoporosisDocument13 pagesOsteoporosisclaudyNo ratings yet
- 2014 OsteoporosisInMen ThematicReport EnglishDocument24 pages2014 OsteoporosisInMen ThematicReport EnglishTatia TsnobiladzeNo ratings yet
- Inflammation, Ageing, and Bone Regeneration: SciencedirectDocument8 pagesInflammation, Ageing, and Bone Regeneration: SciencedirectNileshTipanNo ratings yet
- Osteoporosis JunaidDocument130 pagesOsteoporosis JunaidMohammed JunaidNo ratings yet
- Osteoporosis: Screening, Prevention, and ManagementDocument20 pagesOsteoporosis: Screening, Prevention, and ManagementBernardo RomeroNo ratings yet
- Bone Reports: A A B C C B CDocument9 pagesBone Reports: A A B C C B Caeroforce20No ratings yet
- Breakfast Lunch Dinner: From: UntilDocument4 pagesBreakfast Lunch Dinner: From: UntilOlivi Ioana BolduNo ratings yet
- Polycystic Ovarian Syndrome: Anna Lissa J. Bernadas, M.D., F.P.O.G.SDocument39 pagesPolycystic Ovarian Syndrome: Anna Lissa J. Bernadas, M.D., F.P.O.G.SJerahmeel Sombilon GenillaNo ratings yet
- Renal Function TestsDocument13 pagesRenal Function TestsJennifer CollinsNo ratings yet
- Bharati Report PDFDocument4 pagesBharati Report PDFSachin KothariNo ratings yet
- Frequency DR Hulda Clark ZapperDocument45 pagesFrequency DR Hulda Clark ZapperkwbutterfliesNo ratings yet
- Lab Report Exp 2 - Kidney Function & Physiology (Group 4)Document10 pagesLab Report Exp 2 - Kidney Function & Physiology (Group 4)FARHAH BATRISYIA ABDUL RAHIMNo ratings yet
- Diabetes Technology PresentationDocument13 pagesDiabetes Technology Presentationapi-557588953No ratings yet
- Worksheet 6.1 Mineral Requirement: Module Chapter 6Document7 pagesWorksheet 6.1 Mineral Requirement: Module Chapter 6aeae100% (1)
- Motivation Group B MCQS Fiza Sattar-1Document8 pagesMotivation Group B MCQS Fiza Sattar-1Intzar HussainNo ratings yet
- MenopauseDocument19 pagesMenopauseMuhammad AsmiNo ratings yet
- Endocrine Disorders-1Document52 pagesEndocrine Disorders-1Nathaniel Mbiu TimNo ratings yet
- HDL RandoxDocument4 pagesHDL RandoxJesus Guillermo Caceres FernandezNo ratings yet
- Serum: Levels of Creatine PhosphokinaseDocument2 pagesSerum: Levels of Creatine PhosphokinaseDeepak KumarNo ratings yet
- Project 1: Statistical Analysis: Quantitative MethodsDocument7 pagesProject 1: Statistical Analysis: Quantitative MethodsomNo ratings yet
- Superoksida Dismutase (Sod) Dan Radikal BebasDocument6 pagesSuperoksida Dismutase (Sod) Dan Radikal BebasIvon PalenteNo ratings yet
- Direction: Choose The Letter That Corresponds To The Correct AnswerDocument2 pagesDirection: Choose The Letter That Corresponds To The Correct AnswerjulzhaideNo ratings yet
- First Year B.Sc. Nursing Question Paper 2004Document17 pagesFirst Year B.Sc. Nursing Question Paper 2004Biju Antony100% (1)
- Urine History, Composition, Normal FindingsDocument14 pagesUrine History, Composition, Normal FindingsParas TripathiNo ratings yet
- Hypothyroidism NCLEX ReviewDocument6 pagesHypothyroidism NCLEX ReviewhaleyNo ratings yet
- Uterine Involution and Postpartum Ovarian ActivityDocument8 pagesUterine Involution and Postpartum Ovarian Activityjerry smatt dumtoNo ratings yet
- Cucumber Spray Program With Agritecno ProductsDocument2 pagesCucumber Spray Program With Agritecno ProductsANDRE AURELLIONo ratings yet
- Sepsis and Septic ShockDocument28 pagesSepsis and Septic ShockHayk MinasyanNo ratings yet
- Far Eastern University Institue of Arts and Science Department of Medical Technology Histology 2 SEMESTER AY 2020-2021 Adipose TissueDocument2 pagesFar Eastern University Institue of Arts and Science Department of Medical Technology Histology 2 SEMESTER AY 2020-2021 Adipose TissueKurt EdemNo ratings yet
- BIO202L+Lab+14+ The Urinary SystemDocument9 pagesBIO202L+Lab+14+ The Urinary Systemmyra Thiong'oNo ratings yet
- Principles and Practice of Phytotherapy 2013 Calculos BiliaresDocument8 pagesPrinciples and Practice of Phytotherapy 2013 Calculos BiliaresJose Antonio VenacostaNo ratings yet
- Effects of High TSHDocument3 pagesEffects of High TSHSreream KumarNo ratings yet
- CT KUB CN EditionDocument98 pagesCT KUB CN EditionphoenixibexNo ratings yet
- LAS #1 - EAPP Quarter 1 - Week 1Document2 pagesLAS #1 - EAPP Quarter 1 - Week 1DE JESUS ROBERTO IIINo ratings yet
- Severe Carbamates IntoxicationDocument3 pagesSevere Carbamates IntoxicationFrancieudo SampaioNo ratings yet
- Diabetes MellitusDocument9 pagesDiabetes MellitusglamyposhNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (4)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeFrom EverandThe Twentysomething Treatment: A Revolutionary Remedy for an Uncertain AgeRating: 4.5 out of 5 stars4.5/5 (2)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (38)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (83)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (5)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- I Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionFrom EverandI Shouldn't Feel This Way: Name What’s Hard, Tame Your Guilt, and Transform Self-Sabotage into Brave ActionNo ratings yet
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (267)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (44)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (255)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (61)
- Summary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (11)
- How to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingFrom EverandHow to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingRating: 1 out of 5 stars1/5 (2)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsFrom EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsRating: 4.5 out of 5 stars4.5/5 (39)