Professional Documents
Culture Documents
Cirrhosis V2-1
Uploaded by
El MaheritoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cirrhosis V2-1
Uploaded by
El MaheritoCopyright:
Available Formats
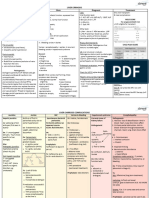
Cirrhosis Pharmacotherapy Summary
Based on the AFP guideline on cirrhosis (2019), AASLD guidelines on portal hypertensive bleeding (2016) and ascites/SBP/HRS (2021), More clinical pearls at pyrls.com
and AASLD/EASL guideline on hepatic encephalopathy (2014)
Overview of Cirrhosis
What is cirrhosis? Cirrhosis
• End-stage of chronic liver disease
• Characterized by advanced fibrosis/scarring Scarring/fibrosis leads to
• Complications include portal hypertension, varices, ascites, increased hepatic resistance
HE, HRS, SBP, liver cancer, and liver failure
• Common causes: alcohol-associated liver disease, chronic Bacterial
viral hepatitis infection, nonalcoholic fatty liver disease Redirection of blood flow Portal Hypertension
translocation
• Diagnosed by liver biopsy (gold standard but invasive) or to collateral veins
clinical findings (imaging, labs, medical history, presentations)
Classification of cirrhosis Spontaneous
Varices Splanchnic Hepatic dysfunction leads to Bacterial
• Child-Turcotte-Pugh (CTP) or Child-Pugh (CP) score vasodilation increase in systemic ammonia Peritonitis
assesses stage and severity of cirrhosis
⚬ Considers total bilirubin, albumin, INR, and degree of
ascites and encephalopathy Activation of endogenous
⚬ Classifies into A (compensated), B (early decompensated), vasoconstrictive systems Hepatic
or C (severely decompensated) (e.g., RAAS) Encephalopathy
• Model for End-Stage Liver Disease (MELD)score assesses
prognosis (3-month mortality) for patients with cirrhosis
Renal vasoconstriction
⚬ 12 or higher predicts increased risk of complications
and sodium retention
Goals of therapy
• Prevent complications of cirrhosis Ascites HE Hepatic encephalopathy
Hepatorenal
• Prevent hepatic decompensation HRS Hepatorenal syndrome
Syndrome
• Reduce mortality SBP Spontaneous bacterial peritonitis
Portal Hypertension (PH) & Varices Spontaneous Bacterial Peritonitis (SBP)
• Scarring of liver impedes blood flow through portal vein, increasing the blood pressure • Often no clear source of infection; mainly Gram-negative bacteria (E. coli, K. pneumoniae)
⚬ Varices = distension in collateral vessels from redirected blood; at risk of variceal hemorrhage but some Gram-positive organisms can be common (S. aureus, E. faecalis, E., faecium)
• PH defined as hepatic venous pressure gradient (HVPG) > 5 mmHg • Diagnosis: polymorphonuclear (PMN) leukocyte > 250/mm3 in the ascitic fluid
⚬ HVPG = difference in pressure between portal vein and hepatic veins • Treatment: antibiotic therapy + IV albumin
⚬ HVPG ≥ 10 mmHg = clinically significant portal hypertension (CSPH) ⚬ Empiric 3rd-gen cephalosporin (e.g., ceftriaxone, cefotaxime) generally recommended
• Primary prophylaxis of variceal hemorrhage ⚬ Broad spectrum agents (e.g., piperacillin/tazobactam) recommended for healthcare-
⚬ A beta-blocker (propranolol 20-40 mg twice daily, nadolol 20-40 mg once daily, or associated or nosocomial infection, those with recent exposure to broad-spectrum
carvedilol 6.25 mg twice daily) continued indefinitely, OR abx, or those admitted with sepsis/septic shock
⚬ Endoscopic variceal ligation (EVL) every 2-8 weeks until variceal eradication ⚬ Add vancomycin if prior MRSA infection or positive MRSA swab
⚬ Add daptomycin for vancomycin-resistant enterococcus
• Treatment of acute variceal hemorrhage ⚬ Meropenem +/- glycopeptide if current or recent exposure to piperacillin/tazobactam
⚬ IV ceftriaxone (1 g/day x max 7 days) + EVL + a vasoactive drug (see below)
⚬ Repeat diagnostic paracentesis 48 hours from initiation; PMN decrease of < 25% from baseline
- Octreotide: 50 mcg bolus → continuous infusion at 50 mcg/hr for 2-5 days, or
may require broadening of antibiotic therapy or investigation of secondary peritonitis
- Vasopressin: continuous infusion at 0.2-0.4 units/min (max 0.8 units/min) for 24 hours
+ concurrent IV nitroglycerin to maintain SBP of 90 mmHg, or • Secondary prevention
- Terlipressin: 2 mg IV every 4 hours during the first 48 hours to control bleeding, ⚬ Long-term prophylaxis with ciprofloxacin 500 mg/day
then 1 mg every 4 hours to prevent rebleeding (total duration 2-5 days) • Primary prevention
• Secondary prophylaxis of variceal hemorrhage ⚬ IV ceftriaxone for patients with variceal hemorrhage (see PH & Varices section)
⚬ A non-selective beta-blocker (propranolol 20-40 mg twice daily or nadolol 20-40 mg ⚬ Generally only needed if high risk of infection present
once daily) continued indefinitely, AND ⚬ Ciprofloxacin for patients with low ascitic fluid protein (< 1.5 g/dL) + and renal dysfunction or liver failure
⚬ EVL every 1-4 weeks until variceal eradication
Hepatorenal Syndrome (HRS)
Ascites • Renal complication due to hemodynamic changes and systemic inflammation
• Accumulation of excess fluid in the abdomen; often the first decompensating event associated with cirrhosis
• Dietary sodium restriction (to 2 g/day) recommended for net fluid loss • Diagnosis of HRS-AKI (acute kidney injury from HRS)
⚬ Cirrhosis with ascites
• Diuretic therapy (aldosterone antagonist + loop diuretic) ⚬ Diagnosis of AKI (↑ SCr by ≥ 0.3 mg/dL in 48 hr OR ≥ 50% ↑ in SCr in the past 7 days)
⚬ Preferred: spironolactone + furosemide ⚬ No response after 2 consecutive days of diuretic withdrawal & plasma volume expansion
⚬ Initially spironolactone 100 mg + furosemide 40 mg per day with albumin infusion
⚬ Titrate to maximum of spironolactone 400 mg + furosemide 160 mg per day ⚬ No current/recent use of nephrotoxic drugs, structural kidney injury, or shock
⚬ At least 72-hour interval needed between dose titrations
⚬ Taper down to the lowest effective dose after fluid is adequately mobilized • Treatment of HRS-AKI
⚬ Vasoconstrictor (terlipressin preferred; norepinephrine also recommended) + albumin
• Monitor daily body weight to assess efficacy of diuretics ⚬ Decrease in SCr to < 1.5 mg/dL or return to baseline within 0.3 mg/dL over
⚬ Up to 0.5 kg/day weight loss is generally appropriate (up to 1 kg/day for those with edema) maximum of 14 days indicates successful response
Hepatic Encephalopathy (HE)
• Believed to be due to ammonia accumulation caused by hepatic dysfunction • Treatment recommended for fully symptomatic overt HE
• Symptoms: impaired memory and motor function, asterixis (“flapping tremor”), ⚬ Lactulose (nonabsorbable disaccharide): preferred treatment
personality changes, coma - 30-45 mL every 1-2 hours until at least 2 soft stools/day are produced
- Thereafter, titrated to maintain 2-3 soft stools/day
• Categorized with West Haven criteria (WHC grades 1 to 4) ⚬ Rifaximin (add-on to lactulose) to prevent HE recurrence after second episode
• Diagnosed by excluding other causes of cognitive dysfunction - 550 mg twice daily
• Short-term protein restriction may be necessary for nitrogen modulation
Reference:
[1] American Association for the Study of Liver Diseases; European Association for the Study of the Liver. Hepatic encephalopathy in chronic liver disease: 2014 practice guideline by the European Association for the Study of the Liver and
the American Association for the Study of Liver Diseases. J Hepatol. 2014 Sep;61(3):642-59. doi: 10.1016/j.jhep.2014.05.042. Epub 2014 Jul 8. Erratum in: J Hepatol. 2015 Oct;63(4):1055.
[2] Biggins SW, Angeli P, et al. Diagnosis, evaluation, and management of ascites, spontaneous bacterial peritonitis and hepatorenal syndrome: 2021 Practice guidance by the American Association for the Study of Liver Diseases. Hepatology.
2021 Aug;74(2):1014-1048. doi: 10.1002/hep.31884.
[3] Garcia-Tsao G, Abraldes JG, et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017
Jan;65(1):310-335. doi: 10.1002/hep.28906. Epub 2016 Dec 1. Erratum in: Hepatology. 2017 Jul;66(1):304.
[4] Smith A, Baumgartner K, et al. Cirrhosis: Diagnosis and management. Am Fam Physician. 2019;100(12):759-770.
® 2023 Cosmas Health, Inc. and/or its affiliates. All rights reserved.
You might also like
- DBT CoachDocument12 pagesDBT CoachTreva100% (1)
- JOE Holder: Teaches Fitness and Wellness FundamentalsDocument30 pagesJOE Holder: Teaches Fitness and Wellness FundamentalsNathaniel LaiNo ratings yet
- ADHD AdultDocument3 pagesADHD AdultCristinaNo ratings yet
- Hematemesis, Melena, HematoscheziaDocument48 pagesHematemesis, Melena, HematoscheziaSyarifah FauziahNo ratings yet
- Infectious Pathology of The Respiratory Tract Zinserling 1 Ed 2021Document256 pagesInfectious Pathology of The Respiratory Tract Zinserling 1 Ed 2021Anna PermyakovaNo ratings yet
- Liver Cirrhosis Pathophysiology and EvaluationDocument91 pagesLiver Cirrhosis Pathophysiology and EvaluationGiorgi PopiashviliNo ratings yet
- Esophageal Varices AMJDocument35 pagesEsophageal Varices AMJAli Al.JuffairiNo ratings yet
- Managing Discomforts During PregnancyDocument3 pagesManaging Discomforts During PregnancyMariana Mikaela AlagarNo ratings yet
- Acute Renal Failure - PPT 1Document36 pagesAcute Renal Failure - PPT 1Jay PaulNo ratings yet
- SOP Feedback Management and Customer Com-PlaintsDocument4 pagesSOP Feedback Management and Customer Com-Plaintslune assongmoNo ratings yet
- Liver Cirrhosis: Etiology Pathogenesis Clinical Features Management PrognosisDocument35 pagesLiver Cirrhosis: Etiology Pathogenesis Clinical Features Management PrognosisMohd Johari Mohd ShafuwanNo ratings yet
- Treatment and Complications of Chronic Liver DiseaseDocument40 pagesTreatment and Complications of Chronic Liver DiseaseRisydaMKhNo ratings yet
- ABDOMINAL DISTENSION CAUSESDocument29 pagesABDOMINAL DISTENSION CAUSESANENA RHODANo ratings yet
- Cirrhosis and Its Complications Part 1 LenchoDocument76 pagesCirrhosis and Its Complications Part 1 Lenchoosman nurNo ratings yet
- L25 CLD-2Document55 pagesL25 CLD-2S sNo ratings yet
- CirrhosisDocument39 pagesCirrhosisC ONo ratings yet
- Portal Hypertension: Pathophysiology, Diagnosis and ManagementDocument11 pagesPortal Hypertension: Pathophysiology, Diagnosis and ManagementXol-TikaNo ratings yet
- Acute Liver Failure-1Document40 pagesAcute Liver Failure-1elizabethNo ratings yet
- DCLDDocument36 pagesDCLDAnonymous uoxEU3mkNo ratings yet
- CIRRHOSIS v1Document41 pagesCIRRHOSIS v1anil sahNo ratings yet
- ABDOMINAL DISTENSION CAUSES AND MANAGEMENTDocument36 pagesABDOMINAL DISTENSION CAUSES AND MANAGEMENTANENA RHODANo ratings yet
- KUIPER Et Al-2007-Alimentary Pharmacology & TherapeuticsDocument11 pagesKUIPER Et Al-2007-Alimentary Pharmacology & TherapeuticsJhonatan Efrain Lopez CarbajalNo ratings yet
- Tutorial Liver FailureDocument59 pagesTutorial Liver FailureNadhrah zulkifliNo ratings yet
- Abd Distension & Ascites-1, All NewDocument34 pagesAbd Distension & Ascites-1, All NewANENA RHODANo ratings yet
- Generally, the prognosis is better for prerenal and postrenal causes compared to intrinsic renal injury. Early recognition and treatment also improves prognosisDocument23 pagesGenerally, the prognosis is better for prerenal and postrenal causes compared to intrinsic renal injury. Early recognition and treatment also improves prognosisrjfeeleyNo ratings yet
- UW Step 2 CK IM GIDocument146 pagesUW Step 2 CK IM GISelena GajićNo ratings yet
- Portal Hypertension and AscitesDocument5 pagesPortal Hypertension and AscitesHưng Nguyễn KiềuNo ratings yet
- Liver Cirrhosis: DR Alex MogereDocument51 pagesLiver Cirrhosis: DR Alex MogereGladys Maina100% (1)
- Liver CirrhosisDocument3 pagesLiver CirrhosisYalin AbouhassiraNo ratings yet
- Liver Curs 2009Document215 pagesLiver Curs 2009Mohammad_Islam87No ratings yet
- Emergency treatment for GI bleedingDocument46 pagesEmergency treatment for GI bleedingzoya shaikhNo ratings yet
- Cirrhosis Hepatic: DinadewisliDocument47 pagesCirrhosis Hepatic: DinadewisliwilmaNo ratings yet
- Portal Hypertension: Gabriel Quah Group 86Document12 pagesPortal Hypertension: Gabriel Quah Group 86bryan-teoh-9027No ratings yet
- Chronic Renal Failure 4-9-18Document27 pagesChronic Renal Failure 4-9-18Muhammad MakkiNo ratings yet
- 8 Cirrhosis NewDocument10 pages8 Cirrhosis Newb_rahman2k39603No ratings yet
- L11 Renal Failure General Approach 230213 002819Document16 pagesL11 Renal Failure General Approach 230213 002819S sNo ratings yet
- Anaesthesia Concerns in CKDDocument34 pagesAnaesthesia Concerns in CKDAbhi JeetNo ratings yet
- Renal Support in Hepatic Patient: by Mohammed Dabbour Lecturer of Anesthesia Ain Shams UniversityDocument36 pagesRenal Support in Hepatic Patient: by Mohammed Dabbour Lecturer of Anesthesia Ain Shams UniversityTrishenth FonsekaNo ratings yet
- Chronic Liver Disease Decompensated N PDFDocument6 pagesChronic Liver Disease Decompensated N PDFmzhao230No ratings yet
- BGD Chronic Hepatitis BDocument6 pagesBGD Chronic Hepatitis BJay Malvin TiaNo ratings yet
- Portal Hypertension: Qbank Session Clinical Sciences LearnedDocument6 pagesPortal Hypertension: Qbank Session Clinical Sciences LearnedMike GNo ratings yet
- Renal Failure: SMF Urologi FK-Unpar / RSUD Dr. Doris SylvanusDocument53 pagesRenal Failure: SMF Urologi FK-Unpar / RSUD Dr. Doris SylvanusClarissa SuheryNo ratings yet
- IPD - SirosisDocument30 pagesIPD - SirosisRahmat AzimiNo ratings yet
- Ascites PresentationDocument19 pagesAscites PresentationDanielle FosterNo ratings yet
- Budd Chiari Syndrome: by DR - Kamran M SaeedDocument41 pagesBudd Chiari Syndrome: by DR - Kamran M SaeeddockmsNo ratings yet
- Jurnal Non Sirotic VEDocument21 pagesJurnal Non Sirotic VEDheajeng Intan MutiarasariNo ratings yet
- Portal Hypertension SPDocument19 pagesPortal Hypertension SPAshish SatyalNo ratings yet
- Liver CirrhosisDocument9 pagesLiver CirrhosismedsmracelisNo ratings yet
- Cirrhosis AndrewDocument33 pagesCirrhosis Andrewlionel andreaNo ratings yet
- Gastroenterology AscitesDocument2 pagesGastroenterology AscitesNour SamadNo ratings yet
- Upper GI BleedingDocument6 pagesUpper GI BleedingMarie Jennifer ParilNo ratings yet
- Chapter 18 - Liver and Biliary TractDocument18 pagesChapter 18 - Liver and Biliary TractAgnieszka WisniewskaNo ratings yet
- Liver Transplant: Gebhard Wagener, MDDocument8 pagesLiver Transplant: Gebhard Wagener, MDAli AftabNo ratings yet
- Fulminant Hepatic Failure: 7 October 2009 Morning Report Christine Williams, MDDocument25 pagesFulminant Hepatic Failure: 7 October 2009 Morning Report Christine Williams, MDAndreas SichoneNo ratings yet
- Compli Cirrhosis RXDocument10 pagesCompli Cirrhosis RXdrgmavmhNo ratings yet
- Liver RebeDocument81 pagesLiver RebeOded YanaNo ratings yet
- Ascites Guide: Causes, Diagnosis & TreatmentDocument86 pagesAscites Guide: Causes, Diagnosis & Treatmentابراهيم عبداللهNo ratings yet
- AscitesDocument5 pagesAscitesEeshuAomNo ratings yet
- HypertensionDocument35 pagesHypertensionMuhammad ZubairNo ratings yet
- Manage Upper GI Bleed in 33yo Hotel ReceptionistDocument42 pagesManage Upper GI Bleed in 33yo Hotel ReceptionistMuhammad Naveed AslamNo ratings yet
- Middle Age Man With Nephrotic Syndrome, Ascitis and Edema: Raika Jamali MDDocument66 pagesMiddle Age Man With Nephrotic Syndrome, Ascitis and Edema: Raika Jamali MDyusnafratilova16No ratings yet
- CirrhosisDocument55 pagesCirrhosisFUTURE DOCTORNo ratings yet
- The Hepatorenal Syndrome: 11 Pathophysiology and Treatment Ofascites andDocument27 pagesThe Hepatorenal Syndrome: 11 Pathophysiology and Treatment Ofascites andJose JulcaNo ratings yet
- Uworld GI NotesDocument17 pagesUworld GI NotesAyodeji SotimehinNo ratings yet
- Approach To Acute Renal FailureDocument40 pagesApproach To Acute Renal FailureMochammad Fariz AmsalNo ratings yet
- UKFP 2024 Applicant HandbookDocument20 pagesUKFP 2024 Applicant HandbookS Abi GunnamNo ratings yet
- SYB Varicose Veins ChecklistDocument2 pagesSYB Varicose Veins ChecklistDrmanzor NwazNo ratings yet
- RRT Declaration Form UpdatedDocument2 pagesRRT Declaration Form UpdatedShayne Jessemae AlmarioNo ratings yet
- Volunteer Handbook 2019Document12 pagesVolunteer Handbook 2019Katharine Tondra100% (1)
- Understanding Acute Leukemia: Signs, Symptoms and TreatmentDocument46 pagesUnderstanding Acute Leukemia: Signs, Symptoms and TreatmentMaica LectanaNo ratings yet
- CaseDocument5 pagesCaseFejlean Angelica AntineoNo ratings yet
- Gary Fending For HimselfDocument3 pagesGary Fending For HimselfPrincess Levie CenizaNo ratings yet
- Week 4 (February 14 - 19) System Life CycleDocument9 pagesWeek 4 (February 14 - 19) System Life CycleChrisanta Joyce Dela Cruz BOCALIGNo ratings yet
- Apgar ScoreDocument2 pagesApgar ScoreVanet100% (1)
- Giraffe Incubator: GE HealthcareDocument2 pagesGiraffe Incubator: GE Healthcarewaludde conradNo ratings yet
- PUDV3134Document1 pagePUDV3134rakesh adamalaNo ratings yet
- Atrial Septal Defect (ASD) : For EducatorsDocument7 pagesAtrial Septal Defect (ASD) : For EducatorsJaven BNo ratings yet
- Article+0202 368 379Document12 pagesArticle+0202 368 379Muhammad Alif Nur FaizinNo ratings yet
- COVID 19 Self Test Throat and Nose InstructionsDocument11 pagesCOVID 19 Self Test Throat and Nose InstructionsonlinregNo ratings yet
- Preparing For Face-To-Face Classes: Better DaysDocument3 pagesPreparing For Face-To-Face Classes: Better DaysMaria Cristina LolosNo ratings yet
- Stroke & Neurological Disease Conference: Ninth AnnualDocument2 pagesStroke & Neurological Disease Conference: Ninth Annualyos_peace86No ratings yet
- 1353 FullDocument15 pages1353 FullmilsaNo ratings yet
- Haloperidol 2mg-ml DropsDocument15 pagesHaloperidol 2mg-ml Dropsddandan_2No ratings yet
- Sister Callista RoyDocument17 pagesSister Callista RoyAbhee CalimagNo ratings yet
- Stroke Prediction System Using ANN (Artificial Neural Network)Document3 pagesStroke Prediction System Using ANN (Artificial Neural Network)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Makabuhay (Tinospora RumphiiDocument4 pagesMakabuhay (Tinospora RumphiiErica Ritz TrainNo ratings yet
- Myanmar Health Assistant Association Vacancy Announcement (VA - 052/2023 MHAA-HR)Document3 pagesMyanmar Health Assistant Association Vacancy Announcement (VA - 052/2023 MHAA-HR)Zawhtet HtetNo ratings yet
- Juvenile DelinquencyDocument34 pagesJuvenile Delinquencyjihan latifahNo ratings yet
- Ncp. Pedia.Document2 pagesNcp. Pedia.Czarina MayoNo ratings yet