100% found this document useful (1 vote)
5K views30 pagesBiochemistry 2nd Year Topical Past Papers 2005-22
This document provides a compilation of past paper questions from 2nd year Biochemistry exams from 2005-2022 at NMU. It covers topics including bioenergetics, carbohydrate metabolism, glycolysis, pyruvate oxidation, the TCA cycle, glycogen metabolism, gluconeogenesis, the pentose phosphate pathway, and fructose, galactose, and diabetes mellitus. The questions are grouped by topic and include multiple choice and explanation questions to test understanding of biochemical pathways and their regulation.
Uploaded by
HussnainCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
100% found this document useful (1 vote)
5K views30 pagesBiochemistry 2nd Year Topical Past Papers 2005-22
This document provides a compilation of past paper questions from 2nd year Biochemistry exams from 2005-2022 at NMU. It covers topics including bioenergetics, carbohydrate metabolism, glycolysis, pyruvate oxidation, the TCA cycle, glycogen metabolism, gluconeogenesis, the pentose phosphate pathway, and fructose, galactose, and diabetes mellitus. The questions are grouped by topic and include multiple choice and explanation questions to test understanding of biochemical pathways and their regulation.
Uploaded by
HussnainCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PDF, TXT or read online on Scribd
- Bioenergetics: Discusses the role of mitochondria in cellular respiration and various hypotheses in oxidative phosphorylation.
- Carbohydrate Metabolism: Covers glycolysis, gluconeogenesis, and the regulation of carbohydrate metabolism.
- TCA Cycle and Glycogen Metabolism: Explores the citric acid cycle's importance and glycogen synthesis and degradation processes.
- Gluconeogenesis and Control of Blood Glucose: Explains the synthesis of glucose from non-carbohydrate sources and its regulation.
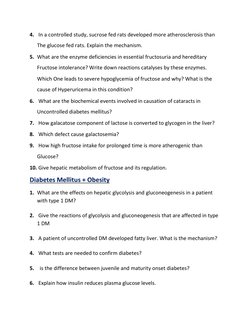
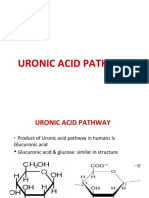
- Pentose Phosphate Pathway and Fructose Metabolism: Details the oxidative phase of pentose phosphate pathway and discusses fructose metabolism's impact on health.
- Diabetes Mellitus and Obesity: Examines biochemical changes in diabetes and obesity and the consequences on metabolism.
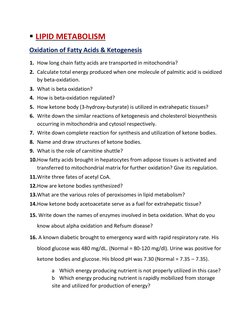
- Lipid Metabolism: Investigates fatty acid oxidation, ketogenesis, and triglyceride regulation.
- Protein and Amino Acid Metabolism: Analyzes protein degradation, urea cycle, and amino acid metabolism.
- Genetics: Explores DNA replication, repair mechanisms, and transcription processes in detail.
- Endocrinology: Discusses hormone functions and regulatory mechanisms in the body.
- Biochemistry of GIT: Focuses on digestion and absorption of nutrients including enzymes in gastrointestinal pathways.
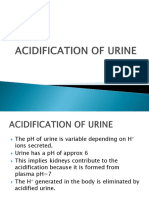
- Water-Electrolyte and Acid-Base Balance: Studies the balance of water and electrolytes in the body and mechanisms of pH regulation.
- Cancer and Xenobiotics: Looks into genetic mutations leading to cancer and the impact of xenobiotics on metabolism.
- Final Page: The page seems to be intentionally left blank or is a separator.