Professional Documents
Culture Documents
CFR Bayes-Genis WEB
Uploaded by
Tran Nguyen ChiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CFR Bayes-Genis WEB
Uploaded by
Tran Nguyen ChiCopyright:
Available Formats
REVIEW
Diagnosis
Biomarkers to Improve Decision-making in Acute Heart Failure
Rafael de la Espriella,1 Gonzalo Núñez-Marín,1 Pau Codina,2 Julio Núñez1,3,4 and Antoni Bayés-Genís2,4,5
1. Department of Cardiology, Hospital Clínico Universitario de Valencia, Valencia, Spain; 2. Heart Institute, Hospital Universitari Germans Trias
i Pujol, Barcelona, Spain; 3. Department of Medicine, Universitat de València, Valencia, Spain; 4. Centro de Investigación Biomédica en Red
en Enfermedades Cardiovasculares, Madrid, Spain; 5. Department of Medicine, Universitat Autònomoa de Barcelona, Barcelona, Spain
Abstract
Acute heart failure (AHF) is a complex clinical syndrome that requires prompt diagnosis, risk stratification and effective treatment strategies
to reduce morbidity and mortality. Biomarkers are playing an increasingly important role in this process, offering valuable insights into the
underlying pathophysiology and facilitating personalised patient management. This review summarises the significance of various biomarkers in
the context of AHF, with a focus on their clinical applications to stratify risk and potential for guiding therapy choices.
Keywords
Acute heart failure, biomarkers, precision medicine
Disclosure: RdlE reports personal fees from AstraZeneca, Novartis, Boehringer Ingelheim and Novo Nordisk (outside the submitted work). GNM reports personal fees
from AstraZeneca and Novo Nordisk (outside the submitted work). PC reports personal fees from AstraZeneca, Novartis, Boehringer Ingelheim and Abbott (outside the
submitted work). JN reports personal fees from AstraZeneca, Novartis, Boehringer Ingelheim, Eli Lilly, Rovi, Novo Nordisk and Vifor Pharma (outside the submitted work).
ABG reports personal fees and/or advisory board from AstraZeneca, Novartis, Boehringer Ingelheim, Abbott, Roche Diagnostics, and Vifor Pharma.
Funding: This work was supported by grants from the Ministry of Economy and Competitiveness, Instituto Carlos III (PI20/00392), CIBER Cardiovascular (16/11/00420 and
16/11/00403).
Received: 3 May 2023 Accepted: 19 June 2023 Citation: Cardiac Failure Review 2023;9:e13. DOI: https://doi.org/10.15420/cfr.2023.08
Correspondence: Antoni Bayés-Genís, Heart Institute, Hospital Universitari Germans Trias i Pujol, Carretera de Canyet, s/n, 08916 Badalona, Barcelona, Spain.
E: abayesgenis@gmail.com
Open Access: This work is open access under the CC-BY-NC 4.0 License which allows users to copy, redistribute and make derivative works for non-commercial
purposes, provided the original work is cited correctly.
The term ‘biomarker’ encompasses a wide-ranging subcategory of objective circulating biomarkers in the context of AHF, focusing on its practical use
biological information, which can be measured accurately and reproducibly in daily clinical care.
and serve as indicators of normal or pathological processes or responses to
therapeutic interventions.1 In the context of acute heart failure (AHF), Biomarkers for the Diagnosis
biomarkers play a crucial role in several aspects of the patient journey, such of Acute Heart Failure
as facilitating prompt and accurate diagnosis, risk stratification, monitoring An accurate and timely diagnosis of AHF in the emergency department
and guiding the initiation or titration of appropriate treatment.2 However, for (ED) is essential to ensure early and appropriate treatment. Some patients
a biomarker to be clinically useful, it should possess several key features: may have a more straightforward presentation with easily identifiable
symptoms or signs on physical examination and imaging, such as chest
• high diagnostic accuracy; X-ray or lung ultrasound, which facilitates an accurate diagnosis. However,
• it should reflect a critical pathophysiological pathway involved in the others may not fit the classic clinical picture or exhibit symptoms or other
disease process; coexisting conditions, which leads to diagnostic uncertainty. In such
• the assays used should be robust and reproducible; cases, combining clinical judgement with the use of biomarkers may
• have a rapid turnaround time to facilitate timely clinical decision- improve diagnostic accuracy, enabling prompt initiation of appropriate
making at the point of care; management.5
• be economically viable; and
• complement clinical judgement in enhancing the understanding of Natriuretic Peptides
diagnosis, prognosis or management.1 Natriuretic peptides (NP) – B-type natriuretic peptide (BNP), N-terminal
proBNP (NT-proBNP) and mid-regional pro-atrial natriuretic peptide (MR-
Therefore, despite the field of biomarkers in heart failure (HF) being proANP) – are by far the most extensively studied and most widely used
dynamic, only a few have translated from initial promise/preclinical use to biomarkers in AHF and current clinical practice guidelines recommend
being integrated into European Society of Cardiology or American College their measurement for early diagnosis or exclusion of AHF, particularly if
of Cardiology/American Heart Association guidelines.3,4 the diagnosis is uncertain and an assay is available at the point of care.3,4
In this article, we will discuss the clinical role of established and emerging Guidelines suggest specific cut-off values for BNP and NT-proBNP to aid in
© The Author(s) 2023. Published by Radcliffe Group Ltd.
www.CFRjournal.com
Intrarenal Venous Flow and Renal Function Trajectory
the initial diagnostic work-up.3,4 In patients with suspected AHF, a cut-off high negative predictive value (rule-out).6 Furthermore, it is common to
concentration of <100 pg/ml BNP and <300 pg/ml NT-proBNP provide an encounter patients with NP values that fall between established diagnostic
excellent negative predictive value to exclude the presence of HF.6 cut-offs for rule-out and rule-in – a grey zone that complicates the
Concentrations above the ruling-in cut-off values support the diagnosis of differentiation between HF and alternative conditions. This scenario is
AHF, particularly if clinical signs and symptoms are consistent.6 The frequently observed in people with obesity who typically exhibit lower NP
age-dependent ruling-in cut-off values for BNP are >400 pg/ml, while the levels than their non-obese counterparts, potentially leading to false-
age-dependent values for NT-proBNP are <50 years: 450 pg/ml, 50–75 negative results and a delay in diagnosis and appropriate treatment.15,16 In
years: 900 pg/ml, and >75 years: 1,800 pg/ml; Figure 1).6 However, it is such scenarios, combining NP measurements with other diagnostic tools,
important to recognise that these cut-off values are not absolute and the such as echocardiography or lung ultrasound, may help improve
diagnostic performance is maximised when NPs are evaluated as diagnostic accuracy.5 Similarly, it is essential to recognise that, when
continuous variables, especially in patients with an intermediate pre-test considering rule-in thresholds, certain patients with chronic HF may
probability. Thus, very low concentrations have a high negative predictive exhibit persistently elevated NP values as a result of structural or
value for excluding the presence of HF. At the other extreme, the higher functional abnormalities rather than necessarily indicating an acute
the NP concentration, the higher the likelihood of an accurate diagnosis haemodynamic change. Familiarity with each patient’s NP concentration
of AHF. under stable conditions – referred to as the ‘dry’ NP concentration –
assists in interpreting these biomarker levels when patients present with
However, despite the strong evidence supporting the use of NPs to assess acute symptoms. A significant increase in NP from dry values (>100%) may
AHF, some considerations should be acknowledged when interpreting indicate a shift in the clinical state, such as worsening HF (Figure 1).7
BNP or NT-proBNP levels in patients presenting with worsening HF
symptoms. Ultimately, it is crucial to adopt a comprehensive approach, using NP
concentrations as one piece of the diagnostic puzzle. Integrating patient
Higher-than-expected Natriuretic Peptide Levels history, clinical presentation and additional diagnostic tools will enable a
NPs are not specific to HF and heart disease.7 Therefore, when faced with more accurate diagnosis and better management of the patient’s
elevated NP levels in the ED, it is crucial to consider alternative conditions condition.
that may lead to increased concentrations of these peptides, particularly
in patients with a low pre-test probability or when an alternative diagnosis Cardiac Troponin
seems more plausible.8 Such conditions include those that result in High-sensitivity cardiac troponin (hs-cTn) testing is commonly conducted
increased myocardial wall stress without a direct association with fluid in patients presenting with AHF syndromes to exclude the presence of
retention, such as AF, acute coronary syndrome, infection, high-output type 1 MI. In this scenario, a significant elevation – >10 times the upper
states and pulmonary embolism, and those related to diminished limit of normal (ULN) – and/or substantial increases within 1–3 hours >100
clearance (renal failure).9–11 Nevertheless, it must be emphasised that ng/l should alert for the possibility of concurrent myocardial ischaemia.3,4
extreme values should not be overlooked because they may identify the In its absence, cardiac troponin elevation should be regarded as a
presence of unrecognised or masked HF and it is essential to acknowledge myocardial injury due to subendocardial stress or myocyte degeneration.
that patients often do not present with a single diagnosis. It is important Notably, elevated hs-cTn levels — regardless of the presence or absence
to contextualise the results according to the patient’s profile and clinical of coronary artery obstruction — prognosticate the risk for progressive
presentation. ventricular remodelling and predict an increased mortality risk.17–20
Lower-than-expected Natriuretic Peptide Levels Biomarkers for Identifying Fluid Overload
Transmural wall stress is the most potent trigger for NP synthesis and The primary therapeutic goal in most patients hospitalised with AHF is to
release.12 In the setting of AHF, the primary factor contributing to optimise their volume status. However, it is important to differentiate
decompensation is either volume overload and/or fluid redistribution in a between volume overload and volume redistribution as the primary cause
heart that cannot adequately accommodate an increase in preload of congestion before initiating decongestive therapies in patients with de
volume, subsequently leading to a pronounced rise in cardiac filling novo or worsening HF. An increasing amount of evidence supports the
pressures.13 As such, most NP release stimuli in AHF are predominantly use of a comprehensive and multiparametric evaluation, including
driven by volume. Laplace’s law governs wall stress and states that for a validated clinical scores, circulating biomarkers and technical
particular intracavitary pressure, wall stress is directly proportional to the assessments, to accurately identify the dominant driver of congestion.
size or radius of the cavity and inversely proportional to the thickness of This integrated approach can aid in effectively addressing this task and
the left ventricular (LV) wall. Therefore, in patients with HF with preserved ensuring appropriate treatment for AHF patients.5,12
LV ejection fraction (HFpEF), the LV chamber size is typically smaller and
thicker, while those with predominantly right-sided HF have a lower Carbohydrate Antigen 125
ventricular mass. As a result, HFpEF and right-sided HF patients often Carbohydrate antigen 125 (CA125), also known as mucin 16 (MUC16) or
exhibit lower NP values for the degree of systemic congestion compared cancer antigen 125, is a complex glycoprotein encoded by the MUC16
with patients with reduced LV ejection fraction (LVEF). Therefore, it is gene in humans.21 This biomarker has been extensively investigated for its
important to consider these factors when interpreting NP levels in patients role in monitoring ovarian cancer. However, elevated CA125 levels have
with different types of HF, as these values may not always reflect the also been observed in other malignancies and non-cancerous conditions,
severity of the condition.14 such as HF.21 Notably, elevated CA125 concentrations have been identified
in nearly two-thirds of patients with AHF, strongly correlating with
Rule-In/Rule-out Cut-off and Baseline Values congestion and fluid overload parameters, particularly markers of tissue
Although both BNP and NT-proBNP have validated rule-out and rule-in congestion and serous effusions.22,23 Furthermore, considering the time
cut-off thresholds, the most robust evidence for NPs in AHF lies in their gap between CA125 upregulation and release (a lagged effect), CA125
CARDIAC FAILURE REVIEW
www.CFRjournal.com
Intrarenal Venous Flow and Renal Function Trajectory
Figure 1: Diagnostic Work-up in Acute Heart Failure
Diagnostic work-up in acute HF
BNP BNP
>500 pg/ml 100–400 pg/ml BNP
NT-proBNP NT-proBNP <100 pg/ml
<50 years >450 pg/ml <50 years >300–450 pg/ml NT-proBNP
50–75 years >900 pg/ml 50–75 years >300–900 pg/ml <300 pg/ml
>75 years >1,800 pg/ml >75 years >300–1,800 pg/ml
AHF likely Grey zone AHF unlikely
Exclude causes of elevated Additional testing required:
NP levels other than primary Echo, lung ultrasound,
diagnosis of AHF chest X-ray, VExUS
Confirm AHF diagnosis
Assess the predominant
clinical profile: ADHF,
acute pulmonary oedema,
right-sided HF,
cardiogenic shock
ADHF = acute decompensated heart failure; AHF = acute heart failure; BNP = B-type natriuretic peptide; Echo = echocardiogram; HF = heart failure; NPs: natriuretic peptides; NT-proBNP = N-terminal
proBNP; VExUS = venous excess ultrasound.
may also aid in estimating the chronicity of the fluid overload process. As gradual clinical onset with predominantly systemic congestion/serous
such, patients with progressive and long-standing fluid retention (volume effusion and may benefit more from an intensive diuretic approach (Figure
overload phenotype) are more likely to exhibit elevated CA125 plasma 2). In contrast, those with more acute onset, with pulmonary redistribution
levels than those with a more acute onset.24 as the dominant congestion phenotype, often have higher NP plasma
levels and normal or mildly abnormal CA125 and bio-ADM values. Such
Bio-adrenomedullin patients may benefit more from the modulation of vascular tone rather
Adrenomedullin (ADM) is involved in various biological processes, with its than aggressive decongestive strategies (Figure 2). In between, varying
primary function being the preservation of vascular integrity, regulation of degrees of overlap may exist, which warrant a multiparametric
vascular tone and permeability barrier function. ADM can freely diffuse assessment.
through the vascular barrier, exerting different effects on vascular
endothelial cells (primarily stabilisation of the barrier) and vascular smooth Biomarkers for Monitoring Diuretic Response
muscle cells (vasodilation). These functions of ADM make it an essential and Decongestion During Admission
molecule for maintaining vascular homeostasis and it has been studied Achieving complete decongestion before hospital discharge is an
for its potential therapeutic use in cardiovascular diseases.25 In situations important therapeutic goal in AHF.29 However, accurately assessing a
characterised by endothelial dysfunction, such as AHF, increased plasma patient’s response to decongestive therapies and determining the optimal
levels of the bioactive form of ADM (bio-ADM) may be interpreted as a time to discontinue these treatments remains a significant challenge.
compensatory attempt to limit vascular leakage by stabilising the Although weight loss and clinical scores based on physical examination
endothelial barrier function.25 Current evidence supports the use of bio- are frequently used to evaluate the congestion status, both have limited
ADM as a surrogate marker of congestion and fluid accumulation in value and often require additional biomarkers and imaging modalities to
HF.26,27 For instance, in patients hospitalised for AHF, bio-ADM is positively provide a more comprehensive assessment.
associated with the severity of clinical congestion scores upon admission
and correlates positively with surrogates of high intravascular pressure Urinary Sodium
(pulmonary capillary wedge pressure, mean right atrial pressure and NT- In the setting of congestion with volume overload, measuring a spot urine
proBNP).28 Thus, bio-ADM may reflect an integrated assessment of both sodium content 1–2 hours following loop diuretic administration has
vascular and tissue congestion. shown to be an excellent marker to predict the initial diuretic response.29
A spot urine sodium content of <50–70 mEq/l generally identifies a patient
Combining CA125 and bio-ADM with the clinical examination and NPs at risk of poor diuretic response for whom doubling the initial loop diuretic
makes it possible to get an overall picture of the severity, temporality and dose is recommended.3,29 Multiple studies have demonstrated that low
distribution of congestion in most patients. In general, patients presenting urinary sodium early after the first loop diuretic dose is associated with
with elevated CA125 and bio-ADM plasma levels often exhibit a more adverse outcomes, irrespective of fluid loss.30–32 However, interpreting
CARDIAC FAILURE REVIEW
www.CFRjournal.com
Intrarenal Venous Flow and Renal Function Trajectory
Figure 2: Biomarkers for Identifying the Predominant Congestion Phenotype
NPs
NPs
CA125 Low High Low High CA125 Low High CA125
bioADM NPs bioADM bioADM
• More acute clinical onset • Gradual clinical onset • Gradual clinical onset
• Predominantly left-sided HF • Combined left- and right-sided HF • Predominantly right-sided HF
• Intravascular congestion/ • Mixed intravascular and tissue • Systemic/tissue congestion
pulmonary redistribution congestion • May benefit more from an
• May benefit more from • May benefit from both modulation intensive diuretic approach
modulation of the vascular of the vascular tone and
tone and less aggressive aggressive diuretic regimen
diuretic regimen
bioADM = bioactive form of adrenomedullin; CA125 = carbohydrate antigen 125; HF = heart failure; NPs = natriuretic peptides.
spot urine sodium necessitates a comprehensive approach, considering Several strategies have been proposed to reduce the burden of early
its relationship with factors, such as diuretic dose, time gap between post-discharge events on patients and healthcare systems, with a
diuretic administration and urinary sodium measurement, the patient’s targeted approach being a potentially cost-effective solution.35 This
fluid volume status (the lower the volume, the lower sodium excretion, strategy involves discharging low-risk patients with less intensive post-
i.e., braking phenomenon) and neurohormonal activity.29 For instance, it is discharge monitoring and providing high-risk patients with comprehensive
possible to encounter patients in whom urinary sodium decreases in-hospital and post-discharge care, potentially promoting a more efficient
‘physiologically’ in parallel with decongestion and others in whom it distribution of scarce healthcare resources. However, accurately
remains stable or even increases during the subsequent days of admission identifying patient subgroups at varying risk levels and predicting events
as a reflection of the persistence of a positive sodium balance.33 such as hospital readmissions remains a significant clinical challenge.
Biomarkers can play an essential role as objective tools for short-term
Haemoconcentration post-discharge risk stratification, and several promising prognostic
Haemoconcentration, which is the increase in the concentration of red biomarkers are currently available that might assist clinicians in assessing
blood cells and plasma proteins due to intravascular volume contraction, post-discharge risk prediction on top of traditional clinical models.
can be used as an indicator of effective intravascular decongestion.12 This
process seems to identify patients who have undergone aggressive Natriuretic Peptides
decongestion and has been associated with better post-discharge Although the NP concentration at admission for AHF strongly predicts
survival. However, since most of the excess volume in patients with AHF inpatient mortality, the absolute discharge value and the percentage
resides in the interstitial compartment, haemoconcentration may only change in levels from admission to discharge seem to be better predictors
indicate that the plasma refill rate has been exceeded even in the of short-term post-discharge outcomes.36–39 For instance, an individual
presence of extravascular volume expansion, which indicates the removal patient data meta-analysis of seven prospective cohort studies, including
of intravascular fluid at a rate faster than it can be refilled from 1,301 patients discharged with NT-proBNP measurements available at
extravascular stores. As a result, haemoconcentration alone does not admission and discharge, showed that the 180-day cumulative mortality
inform total body volume status. In fact, an early haemoconcentration with rate varies significantly with different NT-proBNP absolute discharge
subsequent haemodilution is not associated with clinical benefit as it may levels: 4.1% for <1,500 pg/ml, 10% for 1,500–5,000 pg/ml, 24% for 5,001–
indicate that diuretics may have been de-escalated too early before the 15,000 pg/ml, and 41% for >15,000 pg/ml (Figure 4).38 A similar pattern
complete elimination of extravascular volume expansion, resulting in the was observed when using the reduction percentage, showing that
recurrence of intravascular volume overload – a rebound effect (Figure patients with a ≤30% reduction in NT-proBNP levels have twice the 180-
3).34 Conversely, a late and sustained increase in haematocrit/ day cumulative mortality and composite event rate (all-cause mortality
haemoconcentration in parallel with the patient’s clinical improvement and/or first readmission for a cardiovascular reason) compared to those
may be more informative about the equilibration of extravascular and with a >30% reduction in NT-proBNP levels (Figure 4).38 Likewise, long-
intravascular volume (Figure 3).34 term repeated measurements following the index hospitalisation for AHF
have also been shown to be independently associated with the risk of
Biomarkers for Improving Recognition death.40 A descending kinetic pattern identified those at lower risk of
and Management of High-risk Patients at death, although the ability of serial measurements to predict survival
Discharge and During the Transitional Phase seems to be blunted at longer follow-up periods.40
The transitional phase following admission for AHF is a critical period in a
patient’s care trajectory, requiring meticulous surveillance and While reductions in NT-proBNP levels generally mirror improved central
management. During this period, which comprises the initial week post- cardiac haemodynamic and cardiomyocyte stress, indicating successful
discharge, patients have the highest risk for readmission and adverse response to treatment, there are some clinical scenarios in which NP
outcomes.35 Multiple factors contribute to this heightened vulnerability, values do not significantly decline despite optimal treatment and warrant
with residual congestion and inadequate post-discharge care coordination further evaluation.41 First, a persistently elevated absolute NP
emerging as the most critical elements to address. concentration at discharge in a euvolemic patient may represent their
CARDIAC FAILURE REVIEW
www.CFRjournal.com
Intrarenal Venous Flow and Renal Function Trajectory
Figure 3: Interpreting Haemoconcentration and Haemodilution During Decongestion
Admission Early hospitalisation Late hospitalisation Early hospitalisation Late hospitalisation
Haemodilution Early haemoconcentration with Progressive and sustained
subsequent haemodilution haemoconcentration
Created with BioRender.com.
Figure 4: Biomarkers for Improving Recognition and Management of High-risk Patients
Biomarkers for improving recognition and management of high-risk patients
at discharge and during the transitional phase
Natriuretic peptides CA125 sST2
30 days after
Absolute discharge levels Admission
discharge
30 days after
High risk Discharge
discharge
>15,000 pg/ml High–high
Adverse
U-curve
CA125 U/ml
event zone
sST2 level
5,000–15,000 pg/ml Adverse
event zone
1,500–5,000 pg/ml
High–inter
<1,500 pg/ml Free J-curve
21 event zone
Free High–low
Low risk event zone
Time
Low–low
High risk: ∆ change
admission – discharge ≤30% High risk: ∆ change
admission – discharge ≤15%
Time
CA125 = carbohydrate antigen 125; sST2 = soluble ST2.
‘dry’ NP level, identifying that they may have advanced disease, such as In summary, patients who experience a substantial decrease in NP levels
persistent cardiomyocyte stress. after AHF treatment are more likely to have favourable early post-discharge
outcomes and a less stringent follow-up may be deemed appropriate. On
Another possible scenario involves a patient with predominant right-sided the other hand, those with higher or non-decreasing concentrations might
HF and significant systemic congestion/third-space fluid accumulation require closer monitoring and advanced interventions. The evidence in
who may need a longer diuretic period before achieving a steady patients with AHF and HFpEF and those with lower expected values on
decrease in NP levels.42 In this clinical setting, persistently elevated NP admission is scarce and requires further evaluation.
levels at discharge likely result from fluid mobilisation from the interstitial
compartment to the central circulation, leading to a rebound increase in CA125
cardiac filling pressures once the parenteral diuretic therapy has been One of the most attractive properties of CA125 is its potential role in
stopped. Finally, treatment does not effectively correct the central cardiac monitoring the clinical course following an AHF event.21 Small studies
haemodynamics in some cases, which identifies a treatment-resistant, have indicated that changes in CA125 align with shifts in clinical status.
high-risk patient with a poor prognosis. Other studies have also demonstrated the usefulness of CA125 changes
CARDIAC FAILURE REVIEW
www.CFRjournal.com
Intrarenal Venous Flow and Renal Function Trajectory
Figure 5: Multibiomarker Panel for Identifying the Predominant Heart Failure Phenotype
Predominant right-sided HF Predominant left-sided
Systemic congestion HF Increased left-sided pressures
Elevated CA125 Elevated NPs
Paradoxically low NP values Normal/low CA125
Predominant
HF phenotype
Combined right/left-sided HF Grey zone
Systemic congestion and increased Additional information required for
cardiac filling pressures correct phenotyping
NP vales CA125 values
Renal
Cancer
failure
Infection Non-HF related
hydropic conditions
Anaemia
Treated Pulmonary
HF fibrosis
Obesity MUC16
variants
Lack of
wall stress
Elevated NPs
Elevated CA125 Unexpected high or low
NP/CA125 levels
By combining the info provided by NPs and CA125, we may classify AHF patients as: patients with predominant right-sided HF and systemic fluid overload, mainly extravascular (lower than expected NPs
and high CA125); those with predominant left-sided HF, abrupt onset, and predominant intravascular pulmonary congestion (very high NPs and low CA125); combined left- and right-sided HF with
systemic congestion and increased cardiac filling pressures (high NPs and high CA125); and patients with unexpectedly high or low NPs/CA125 in whom additional information is required for correct
phenotyping. AHF = acute heart failure; CA125 = carbohydrate antigen 125; HF = heart failure; MUC16 = mucin 16; NPs = natriuretic peptides. Created with BioRender.com.
for risk stratification within the first week after discharge.40,43,44 In a cohort 946 consecutive patients discharged for AHF and assessed the long-term
of 293 patients admitted for AHF, CA125 levels decreased to ≤35 U/ml in prognostic impact of repeated CA125 measurements (3,402 observations
52.2% of patients, decreased but remained >35 U/ml in 24.6%, and during an average follow-up of 2.64 years). The outcomes significantly
increased in 23.2% at the first outpatient visit after discharge (median 31 differed based on survival status. A considerable decrease in CA125 levels
days).43 At a median follow-up of 18 months, patients with normalised was observed within the first month after discharge, which identified a
CA125 values had the lowest risk of death.43 In contrast, those with lower-risk subgroup (Figure 4). In contrast, CA125 levels remained high or
decreased but not normalised values and those with increased values increased in patients who died at the end of follow-up (Figure 4).40
had a higher adjusted risk of death. Changes over time showed Moreover, longitudinal measurements of NT-proBNP were also linked to
incremental reclassification indexes compared to a single measurement higher mortality risk. However, unlike the changes in CA125, the magnitude
of CA125 or even changes in NT-proBNP.43 The same categorical changes of these changes was less pronounced and diminished over time. Notably,
proved to be useful for predicting 6-month readmission. Patients who did a shift from high to low or low to high CA125 levels during follow-up was
not have CA125 ≤35 U/ml at the first outpatient visit had a threefold strongly correlated with a decreased or increased risk of death,
increased risk of 6-month HF readmission.43 respectively.40
In a more recent study, the long-term changing patterns of CA125 were The CHANCE-HF trial involved 380 patients discharged for AHF with
found to be independently associated with mortality.40 The study involved high CA125 levels (>35 U/ml). This study compared a CA125-guided
CARDIAC FAILURE REVIEW
www.CFRjournal.com
Intrarenal Venous Flow and Renal Function Trajectory
therapy to the standard of care.45 In brief, the CA125-guided therapy all-cause mortality or readmission for HF during a 1-year follow-up. A
involved intensifying diuretic treatment and monitoring frequency when U-shape sST2 pattern was observed in those with the primary endpoint
CA125 levels increased or remained high during follow-up.45 When – sST2 concentrations increasing before reaching the primary endpoint
CA125 levels decreased below 35 U/ml, the protocol recommended – whereas ST2 stabilised in patients without the primary endpoint during
reducing diuretics and increasing the time between outpatient visits. follow-up – a J-shape sST2 pattern (Figure 4).51
Patients in the CA125-guided strategy experienced a 50% increase in
diuretic dose modifications and up to 21% of them received outpatient Although several new biomarkers also seem to be promising for risk
IV furosemide based on persistently high CA125 levels.45 The guided stratification, such as growth differentiation factor-15 (GDF-15) and
strategy proved superior to the standard of care in reducing the risk of bioADM, optimising the assay methodology remains a major challenge.
the composite 1-year death or AHF readmission. This reduction was Furthermore, only a few new-generation HF biomarkers have fully
achieved by decreasing the risk of the first and recurrent HF automated protocols, while some do not even have Food and Drug
readmissions by 51% at the 1-year follow-up.45 Administration approval or a CE label.52
In summary, current evidence supports the role of CA125 in dynamic risk Multibiomarker Panel: Ready for the Prime Time?
stratification, which is independent and additive to the prognostic In our opinion, a multiparametric approach that considers the key
information provided by traditional proxies of HF severity and NPs.21 pathophysiological mechanisms in AHF is highly relevant. This approach
Patients with elevated CA125 require a comprehensive assessment of should be logistically feasible, widely available, relatively low-cost, highly
congestion and may benefit from intensive diuretic strategies reproducible and not excessively time-consuming. It should also provide
accompanied by closer monitoring. Normalising CA125 values in this additional information to the standard of care to improve diagnosis,
population should be the objective regardless of initial post-discharge monitoring and to guide therapy. In AHF, this panel should ideally include
values.21 Persistently high or non-normalising CA125 levels during the first proxies of LV stretch and pressures (NPs) and information on the
week after discharge may indicate ongoing/residual congestion and an distribution of fluid overload, both regional and compartmental. CA125
increased risk of adverse clinical events (Figure 4).21 appears to be an ideal candidate for assessing the type of fluid overload.
By combining the information provided by NPs and CA125, we can classify
Soluble ST2 AHF patients into four categories based on the predominant type of HF,
ST2, also known as interleukin-1 receptor-like 1 (IL1RL1), belongs to the the onset of symptoms and the type of fluid overload (Figure 5). The
Toll-like/interleukin-1 receptor superfamily and is encoded by the IL1RL1 usefulness of this panel, in conjunction with imaging techniques, is
gene situated on chromosome 2.12 Alternative splicing generates multiple attractive but requires further investigation.
ST2 isoforms, including transmembrane (ST2 ligand or ST2L) and soluble
circulating form (sST2). The latter is a valuable prognostic biomarker in Conclusion
both acute and chronic HF. The biological action of the ST2 protein is Biomarkers in AHF management are critical for enhancing diagnostic
mediated through the extracellular engagement of ST2L with its ligand, accuracy, monitoring therapeutic response and assisting in risk
interleukin-33 (IL-33). While the IL-33/ST2L signalling pathway has anti- stratification during inpatient stays and transitional phases. NPs provide
fibrotic effects, sST2 acts as a decoy receptor, diminishing the net valuable information on cardiac function and help guide diagnosis and
transduction of the favourable effects of IL-33 through ST2L.12 prognostic evaluation in AHF patients. Other biomarkers, such as spot
urine sodium and haemoconcentration, can help predict diuretic response
Single sST2 measurements have consistently demonstrated prognostic and assess effective decongestion. However, due to the multi-layered
and predictive value, as confirmed in two meta-analyses conducted on complexity of HF, relying solely on a single biomarker strategy may not
chronic and acute HF.46,47 However, serial sST2 measurements more offer significant additional benefits. Instead, a multi-biomarker approach
accurately reflect the dynamic and progressive nature of HF compared to is likely to be necessary to reflect the entire disease burden. Therefore,
a single measurement.48 For instance, Boisot et al. demonstrated that we believe there is considerable scope for further research to elucidate
among patients hospitalised with AHF, a failure of sST2 to decrease by at whether these markers accurately mirror specific shifts in disease severity
least 15% during hospitalisation was associated with an increased risk of or comorbidities. In addition, novel biomarkers, such as CA125 and sST2,
death at 90 days (Figure 4).49 Building on this concept, Bayés-Genís et al. can offer additional prognostic information, especially when combined
measured sST2 2 weeks apart in a cohort of outpatients with with NPs. Notably, a multiparametric approach incorporating key
decompensated HF and observed that these patients were at increased pathophysiological mechanisms in AHF and including a panel of
risk of adverse outcomes when sST2 failed to drop by at least 25%.50 biomarkers such as NPs and CA125 could help classify patients into
More recently, van Vark et al. examined the predictive value of frequently distinct categories based on the predominant type of HF, symptom onset
measured sST2 in a population with AHF three times during admission and fluid overload. This classification system could potentially improve
and four more times after discharge at pre-defined time points.51 This diagnosis, monitoring, and therapy guidance in AHF patients. However,
study shows that baseline sST2 and repeated sST2 measurements more research is needed to confirm the use of this panel in conjunction
represent a strong, independent predictor of the composite endpoint of with imaging techniques in routine clinical practice.
1. Biomarkers Definitions Working Group. Biomarkers and doi.org/10.1093/eurheartj/ehab368; PMID: 34447992 updated perspective. Rev Esp Cardiol (Engl Ed) 2023;76:47–
surrogate endpoints: preferred definitions and conceptual 4. Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/ 57. https://doi.org/10.1016/j.rec.2022.07.009;
framework. Clin Pharmacol Ther 2001;69:89–95. https://doi. HFSA guideline for the management of heart failure: PMID: 35934293.
org/10.1067/mcp.2001.113989; PMID: 11240971. executive summary: a report of the American College of 6. Januzzi JL Jr, Chen-Tournoux AA, Christenson RH, et al.
2. Ibrahim NE, Januzzi JL Jr. Established and emerging roles of Cardiology/American Heart Association joint committee on N-terminal pro-B-type natriuretic peptide in the emergency
biomarkers in heart failure. Circ Res 2018;123:614–29. https:// clinical practice guidelines. Circulation 2022;145:e876–94. department: the ICON-RELOADED study. J Am Coll Cardiol
doi.org/10.1161/CIRCRESAHA.118.312706; PMID: 30355136. https://doi.org/10.1161/CIR.0000000000001062; 2018;71:1191–200. https://doi.org/10.1016/j.jacc.2018.01.021;
3. McDonagh TA, Metra M, Adamo M, et al. 2021 ESC PMID: 35363500. PMID: 29544601.
guidelines for the diagnosis and treatment of acute and 5. de la Espriella R, Cobo M, Santas E, et al. Assessment of 7. Mueller C, McDonald K, de Boer RA, et al. Heart Failure
chronic heart failure. Eur Heart J 2021;42:3599–726. https:// filling pressures and fluid overload in heart failure: an Association of the European Society of Cardiology practical
CARDIAC FAILURE REVIEW
www.CFRjournal.com
Intrarenal Venous Flow and Renal Function Trajectory
guidance on the use of natriuretic peptide concentrations. amino-terminal pro-B-type natriuretic peptide model for patients hospitalised for acute decompensated
Eur J Heart Fail 2019;21:715–31. https://doi.org/10.1002/ concentrations in acute heart failure. Eur Heart J Acute heart failure incorporating N-terminal pro-B-type natriuretic
ejhf.1494; PMID: 31222929. Cardiovasc Care 2020;9:437–47. https://doi. peptide levels: a European coLlaboration on Acute
8. Thygesen K, Mair J, Mueller C, et al. Recommendations for org/10.1177/2048872620908033; PMID: 32129669. decompeNsated Heart Failure: ELAN-HF Score. Heart
the use of natriuretic peptides in acute cardiac care: a 24. Lourenço P, Cunha FM, Elias C, et al. CA-125 variation in 2014;100:115–25. https://doi.org/10.1136/
position statement from the Study Group on Biomarkers in acute heart failure: a single-centre analysis. ESC Heart Fail heartjnl-2013-303632; PMID: 24179162.
Cardiology of the ESC Working Group on Acute Cardiac 2022;9:1018–26. https://doi.org/10.1002/ehf2.13758; 39. Eurlings LW, Sanders-van Wijk S, van Kraaij DJ, et al. Risk
Care. Eur Heart J 2012;33:2001–6. https://doi.org/10.1093/ PMID: 34989167. stratification with the use of serial N-terminal pro-B-type
eurheartj/ehq509; PMID: 21292681. 25. Voors AA, Kremer D, Geven C, et al. Adrenomedullin in heart natriuretic peptide measurements during admission and
9. McKie PM, Burnett JC Jr. B-type natriuretic peptide as a failure: pathophysiology and therapeutic application. Eur J early after discharge in heart failure patients: post hoc
biomarker beyond heart failure: speculations and Heart Fail 2019;21:163–71. https://doi.org/10.1002/ejhf.1366; analysis of the PRIMA study. J Card Fail 2014;20:881–90.
opportunities. Mayo Clin Proc 2005;80:1029–36. https://doi. PMID: 30592365. https://doi.org/10.1016/j.cardfail.2014.08.014;
org/10.4065/80.8.1029; PMID: 16092582. 26. Kremer D, Ter Maaten JM, Voors AA. Bio-adrenomedullin as PMID: 25175696.
10. Palmer SC, Yandle TG, Nicholls MG, et al. Regional a potential quick, reliable, and objective marker of 40. Núñez J, Núñez E, Bayés-Genís A, et al. Long-term serial
clearance of amino-terminal pro-brain natriuretic peptide congestion in heart failure. Eur J Heart Fail 2018;20:1363–5. kinetics of N-terminal pro B-type natriuretic peptide and
from human plasma. Eur J Heart Fail 2009;11:832–9. https:// https://doi.org/10.1002/ejhf.1245; PMID: 29932477. carbohydrate antigen 125 for mortality risk prediction
doi.org/10.1093/eurjhf/hfp099; PMID: 19605456. 27. Ter Maaten JM, Kremer D, Demissei BG, et al. Bio- following acute heart failure. Eur Heart J Acute Cardiovasc
11. de la Espriella R, Bayés-Genís A, Llàcer P, et al. Prognostic adrenomedullin as a marker of congestion in patients with Care 2017;6:685–96. https://doi.
value of NT-proBNP and CA125 across glomerular filtration new-onset and worsening heart failure. Eur J Heart Fail org/10.1177/2048872616649757; PMID: 27199489.
rate categories in acute heart failure. Eur J Intern Med 2019;21:732–43. https://doi.org/10.1002/ejhf.1437; 41. Kazanegra R, Cheng V, Garcia A, et al. A rapid test for
2022;95:67–73. https://doi.org/10.1016/j.ejim.2021.08.024; PMID: 30843353. B-type natriuretic peptide correlates with falling wedge
PMID: 34507853. 28. Goetze JP, Balling L, Deis T, et al. Bioactive adrenomedullin pressures in patients treated for decompensated heart
12. Núñez J, de la Espriella R, Rossignol P, et al. Congestion in in plasma is associated with biventricular filling pressures in failure: a pilot study. J Card Fail 2001;7:21–9. https://doi.
heart failure: a circulating biomarker-based perspective. A patients with advanced heart failure. Eur J Heart Fail org/10.1054/jcaf.2001.23355; PMID: 11264546.
review from the Biomarkers Working Group of the Heart 2021;23:489–91. https://doi.org/10.1002/ejhf.1937; 42. Soler M, Miñana G, Santas E, et al. CA125 outperforms
Failure Association, European Society of Cardiology. Eur J PMID: 32558059. NT-proBNP in acute heart failure with severe tricuspid
Heart Fail. 2022;24:1751–66. https://doi.org/10.1002/ 29. Mullens W, Damman K, Harjola VP, et al. The use of diuretics regurgitation. Int J Cardiol 2020;308:54–9. https://doi.
ejhf.2664; PMID: 36039656. in heart failure with congestion – a position statement from org/10.1016/j.ijcard.2020.03.027; PMID: 32209267.
13. Haug C, Metzele A, Kochs M, et al. Plasma brain natriuretic the Heart Failure Association of the European Society of 43. Núñez J, Núñez E, Sanchis J, et al. Antigen carbohydrate
peptide and atrial natriuretic peptide concentrations Cardiology. Eur J Heart Fail 2019;21:137–55. https://doi. 125 and brain natriuretic peptide serial measurements for
correlate with left ventricular end-diastolic pressure. Clin org/10.1002/ejhf.1369; PMID: 30600580. risk stratification following an episode of acute heart failure.
Cardiol 1993;16:553–7. https://doi.org/10.1002/ 30. Brinkley DM Jr, Burpee LJ, Chaudhry SP, et al. Spot urine Int J Cardiol 2012;159:21–8. https://doi.org/10.1016/j.
clc.4960160708; PMID: 8348764. sodium as triage for effective diuretic infusion in an ijcard.2011.02.001; PMID: 21367474.
14. Palazzuoli A, Mullens W. Cardiac congestion assessed by ambulatory heart failure unit. J Card Fail 2018;24:349–54. 44. Miñana Escrivá G, Núñez J, Sanchis J, et al. Carbohydrate
natriuretic peptides oversimplifies the definition and https://doi.org/10.1016/j.cardfail.2018.01.009; antigen 125 serial measurements after an admission for
treatment of heart failure. ESC Heart Fail 2021;8:3453–7. PMID: 29410227. acute heart failure and risk of early readmission. Med Clin
https://doi.org/10.1002/ehf2.13495; PMID: 34255914. 31. Singh D, Shrestha K, Testani JM, et al. Insufficient natriuretic (Barc) 2012;139:479–86 [in Spanish]. https://doi.org/10.1016/j.
15. Wang TJ, Larson MG, Levy D, et al. Impact of obesity on response to continuous intravenous furosemide is medcli.2011.05.029; PMID: 22093405.
plasma natriuretic peptide levels. Circulation 2004;109:594– associated with poor long-term outcomes in acute 45. Núñez J, Llàcer P, Bertomeu-González V, et al. Carbohydrate
600. https://doi.org/10.1161/01.CIR.0000112582.16683.EA; decompensated heart failure. J Card Fail 2014;20:392–9. Antigen-125-Guided therapy in acute heart failure: CHANCE-
PMID: 14769680. https://doi.org/10.1016/j.cardfail.2014.03.006; HF: A randomized study. JACC Heart Fail 2016;4:833–43.
16. Mehra MR, Uber PA, Park MH, et al. Obesity and suppressed PMID: 24704538. https://doi.org/10.1016/j.jchf.2016.06.007; PMID: 27522630.
B-type natriuretic peptide levels in heart failure. J Am Coll 32. Verbrugge FH, Nijst P, Dupont M, et al. Urinary composition 46. Aimo A, Vergaro G, Ripoli A, et al. Meta-analysis of soluble
Cardiol 2004;43:1590–5. https://doi.org/10.1016/j. during decongestive treatment in heart failure with reduced suppression of Tumorigenicity-2 and prognosis in acute
jacc.2003.10.066; PMID: 15120816. ejection fraction. Circ Heart Fail 2014;7:766–72. https://doi. heart failure. JACC Heart Fail 2017;5:287–96. https://doi.
17. Peacock WF 4th, De Marco T, Fonarow GC, et al. Cardiac org/10.1161/CIRCHEARTFAILURE.114.001377; PMID: 25037309. org/10.1016/j.jchf.2016.12.016; PMID: 28189578.
troponin and outcome in acute heart failure. N Engl J Med 33. Biegus J, Zymliński R, Fudim M, et al. Spot urine sodium in 47. Aimo A, Vergaro G, Passino C, et al. Prognostic value of
2008;358:2117–26. https://doi.org/10.1056/NEJMoa0706824; acute heart failure: differences in prognostic value on soluble suppression of Tumorigenicity-2 in chronic heart
PMID: 18480204. admission and discharge. ESC Heart Fail 2021;8:2597–602. failure: A meta-analysis. JACC Heart Fail 2017;5:280–6.
18. O’Connor CM, Fiuzat M, Lombardi C, et al. Impact of serial https://doi.org/10.1002/ehf2.13372; PMID: 33932273. https://doi.org/10.1016/j.jchf.2016.09.010; PMID: 27816512.
troponin release on outcomes in patients with acute heart 34. Testani JM, Brisco MA, Chen J, et al. Timing of 48. Bayés-Genís A, Núñez J, Lupón J. Soluble ST2 for prognosis
failure: analysis from the PROTECT pilot study. Circ Heart Fail hemoconcentration during treatment of acute and monitoring in heart failure: the new gold standard? J Am
2011;4:724–32. https://doi.org/10.1161/ decompensated heart failure and subsequent survival: Coll Cardiol 2017;70:2389–92. https://doi.org/10.1016/j.
CIRCHEARTFAILURE.111.961581; PMID: 21900185. importance of sustained decongestion. J Am Coll Cardiol jacc.2017.09.031; PMID: 29096810.
19. Felker GM, Hasselblad V, Tang WH, et al. Troponin I in acute 2013;62:516–24. https://doi.org/10.1016/j.jacc.2013.05.027; 49. Boisot S, Beede J, Isakson S, et al. Serial sampling of ST2
decompensated heart failure: insights from the ASCEND-HF PMID: 23747773. predicts 90-day mortality following destabilized heart
study. Eur J Heart Fail 2012;14:1257–64. https://doi. 35. Albert NM, Barnason S, Deswal A, et al. Transitions of care failure. J Card Fail 2008;14:732–8. https://doi.org/10.1016/j.
org/10.1093/eurjhf/hfs110; PMID: 22764184. in heart failure: a scientific statement from the American cardfail.2008.06.415; PMID: 18995177.
20. Felker GM, Mentz RJ, Teerlink JR, et al. Serial high Heart Association. Circ Heart Fail 2015;8:384–409. https:// 50. Bayes-Genis A, Pascual-Figal D, Januzzi JL, et al. Soluble
sensitivity cardiac troponin T measurement in acute heart doi.org/10.1161/HHF.0000000000000006; PMID: 25604605. ST2 monitoring provides additional risk stratification for
failure: insights from the RELAX-AHF study. Eur J Heart Fail 36. Fonarow GC, Peacock WF, Phillips CO, et al. Admission outpatients with decompensated heart failure. Rev Esp
2015;17:1262–70. https://doi.org/10.1002/ejhf.341; B-type natriuretic peptide levels and in-hospital mortality in Cardiol 2010;63:1171–8. https://doi.org/10.1016/s1885-
PMID: 26333655. acute decompensated heart failure. J Am Coll Cardiol 5857(10)70231-0; PMID: 20875357.
21. Núñez J, de la Espriella R, Miñana G, et al. Antigen 2007;49:1943–50. https://doi.org/10.1016/j.jacc.2007.02.037; 51. van Vark LC, Lesman-Leegte I, Baart SJ, et al. Prognostic
carbohydrate 125 as a biomarker in heart failure: a narrative PMID: 17498579. value of serial ST2 measurements in patients with acute
review. Eur J Heart Fail 2021;23:1445–57. https://doi. 37. Kociol RD, Horton JR, Fonarow GC, et al. Admission, heart failure. J Am Coll Cardiol 2017;70:2378–88. https://doi.
org/10.1002/ejhf.2295; PMID: 34241936. discharge, or change in B-type natriuretic peptide and long- org/10.1016/j.jacc.2017.09.026; PMID: 29096809.
22. Núñez J, Bayés-Genís A, Revuelta-López E, et al. Clinical term outcomes: data from Organized Program to Initiate 52. Meijers WC, Bayes-Genis A, Mebazaa A, et al. Circulating
role of CA125 in worsening heart failure: a BioStat-CHF Lifesaving Treatment in Hospitalized Patients with Heart heart failure biomarkers beyond natriuretic peptides: review
study subanalysis. JACC Heart Fail 2020;8:386–97. https:// Failure (OPTIMIZE-HF) linked to Medicare claims. Circ Heart from the Biomarker Study Group of the Heart Failure
doi.org/10.1016/j.jchf.2019.12.005; PMID: 32171764. Fail 2011;4:628–36. https://doi.org/10.1161/ Association (HFA), European Society of Cardiology (ESC). Eur
23. Miñana G, de la Espriella R, Mollar A, et al. Factors CIRCHEARTFAILURE.111.962290; PMID: 21743005. J Heart Fail 2021;23:1610–32. https://doi.org/10.1002/
associated with plasma antigen carbohydrate 125 and 38. Salah K, Kok WE, Eurlings LW, et al. A novel discharge risk ejhf.2346; PMID: 34498368.
CARDIAC FAILURE REVIEW
www.CFRjournal.com
You might also like
- Clinical Cases in Chronic Thromboembolic Pulmonary HypertensionFrom EverandClinical Cases in Chronic Thromboembolic Pulmonary HypertensionWilliam R. AugerNo ratings yet
- Biomarkers in Heart FailureDocument6 pagesBiomarkers in Heart Failurekevin ortegaNo ratings yet
- Comments On The 2016 ESC Guidelines For The Diagnosis and Treatment of Acute and Chronic Heart FailureDocument7 pagesComments On The 2016 ESC Guidelines For The Diagnosis and Treatment of Acute and Chronic Heart FailureDian Atillah IkhwaniNo ratings yet
- European Journal of Internal MedicineDocument9 pagesEuropean Journal of Internal MedicinefathiNo ratings yet
- BNP in CKDDocument6 pagesBNP in CKDDedy ShauqiNo ratings yet
- Study of The Role of Plasma Nt-Probnp in The Diagnosis of Heart FailureDocument5 pagesStudy of The Role of Plasma Nt-Probnp in The Diagnosis of Heart FailureMinerva Medical Treatment Pvt LtdNo ratings yet
- Clinical Practice Guideline: Benign Paroxysmal Positional VertigoDocument35 pagesClinical Practice Guideline: Benign Paroxysmal Positional Vertigoapi-19500641No ratings yet
- Hepatic Encephalopathy Update: Reports From The 2012 International Liver ConferenceDocument10 pagesHepatic Encephalopathy Update: Reports From The 2012 International Liver ConferenceMono Yngwie MendozaNo ratings yet
- Nihms 1665920Document19 pagesNihms 1665920jesusNo ratings yet
- 1 s2.0 S0012369219300029 MainDocument22 pages1 s2.0 S0012369219300029 MainbrandusaNo ratings yet
- Life 11 01429Document14 pagesLife 11 01429Genesis PerezNo ratings yet
- Ehu 090Document9 pagesEhu 090Tatiana CumbicosNo ratings yet
- Hypertension Management in Transition From CKD A ERDS 2016Document7 pagesHypertension Management in Transition From CKD A ERDS 2016hemer hadyn calderon alvitesNo ratings yet
- The Recommendations of A Consensus Panel For The Screening, Diagnosis, and Treatment of Neurogenic Orthostatic Hypotension and Associated Supine Hypertension (Journal of Neurology, 2017)Document16 pagesThe Recommendations of A Consensus Panel For The Screening, Diagnosis, and Treatment of Neurogenic Orthostatic Hypotension and Associated Supine Hypertension (Journal of Neurology, 2017)mysticmdNo ratings yet
- Clinical Cardiology - 2022 - Liang - Prognostic Value of RDW Alone and in Combination With NT proBNP in Patients With HeartDocument13 pagesClinical Cardiology - 2022 - Liang - Prognostic Value of RDW Alone and in Combination With NT proBNP in Patients With Heartrizkiyah prabawantiNo ratings yet
- REZUMAT TEZĂ - EnglpetreDocument27 pagesREZUMAT TEZĂ - EnglpetreDaniel StaniloaieNo ratings yet
- 1 5136382648058380752Document11 pages1 5136382648058380752ednasu1No ratings yet
- ANMCO ELAS SIBioC Consensus Document Biomarkers in Heart FailureDocument11 pagesANMCO ELAS SIBioC Consensus Document Biomarkers in Heart FailureLinaNo ratings yet
- Diagnosis and Evaluation of Hypersensitivity Pneumonitis: CHEST Guideline and Expert Panel ReportDocument60 pagesDiagnosis and Evaluation of Hypersensitivity Pneumonitis: CHEST Guideline and Expert Panel Reportjose henaoNo ratings yet
- Evidence-Based Drug Therapy For Chronic Heart Failure: ZannadDocument7 pagesEvidence-Based Drug Therapy For Chronic Heart Failure: ZannadA5BNi Gusti Ketut Purnami Putri AdnyaniNo ratings yet
- Hypertension in ChildrenDocument44 pagesHypertension in ChildrenDsk IndryNo ratings yet
- Ejhf 2206Document10 pagesEjhf 2206Luis Fernando Morales JuradoNo ratings yet
- Physycal Examination On CV SystemDocument21 pagesPhysycal Examination On CV SystemMerellyn Hurtado PachecoNo ratings yet
- FocusDocument9 pagesFocusAdéline NolinNo ratings yet
- Urinary/Kidney Disorders - Health Policy & RegulatoryDocument1 pageUrinary/Kidney Disorders - Health Policy & RegulatoryYehezkiel Nathanael SiahaanNo ratings yet
- Ni Hms 537812Document15 pagesNi Hms 537812maracioNo ratings yet
- 10 5694mja18 00647 PDFDocument7 pages10 5694mja18 00647 PDFandiNo ratings yet
- NIH Public AccessDocument13 pagesNIH Public Accessevi munjayantiNo ratings yet
- Mueller Et Al-2019-European Journal of Heart Failure PDFDocument17 pagesMueller Et Al-2019-European Journal of Heart Failure PDFJANo ratings yet
- Hidrosefalus JournalDocument12 pagesHidrosefalus JournalTrifosa Ika Septiana EryaniNo ratings yet
- CGH:2018 09 13:maravillaDocument3 pagesCGH:2018 09 13:maravillaRachelle MaravillaNo ratings yet
- 2011 - Denicola (Jurnal)Document9 pages2011 - Denicola (Jurnal)Riana HandayaniNo ratings yet
- PE and CHFDocument9 pagesPE and CHFKu Li ChengNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument10 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- MRI & Liver Histology Features in NASHDocument17 pagesMRI & Liver Histology Features in NASHParul SoodNo ratings yet
- Raviele - Europace - PalpitationDocument15 pagesRaviele - Europace - Palpitationnadia shabriNo ratings yet
- BMM 2018 0348Document14 pagesBMM 2018 0348Harpreet SinghNo ratings yet
- Antihypertensives in HDDocument6 pagesAntihypertensives in HDamanyNo ratings yet
- Neutrophil To Lymphocyte Ratio in Diagnosis of Complicated and Non-Complicated AppendicitisDocument7 pagesNeutrophil To Lymphocyte Ratio in Diagnosis of Complicated and Non-Complicated AppendicitisHamza AhmedNo ratings yet
- Debo Ode 2018Document23 pagesDebo Ode 2018MaluNo ratings yet
- Management of Pulmonary Arterial Hypertension (PAH)Document119 pagesManagement of Pulmonary Arterial Hypertension (PAH)caishamNo ratings yet
- 1 s2.0 S0009898118300500 MainDocument8 pages1 s2.0 S0009898118300500 MainMohamed AmineNo ratings yet
- Polypill, Indications and Use 2.1Document12 pagesPolypill, Indications and Use 2.1jordiNo ratings yet
- 2019 EUR J of HF Heart Failure Association of The ESC On The Use of Natriuretic PeptidesDocument17 pages2019 EUR J of HF Heart Failure Association of The ESC On The Use of Natriuretic Peptidessimulacro mirNo ratings yet
- Erp 17 0071Document14 pagesErp 17 0071Jamir PastranaNo ratings yet
- Estado Hemodinamico La Primera Semana de Vida en VLBWDocument7 pagesEstado Hemodinamico La Primera Semana de Vida en VLBWMaluNo ratings yet
- Aao HNSF - BPPVDocument36 pagesAao HNSF - BPPVandiNo ratings yet
- Echocardiography in Hemodynamic MonitoringDocument5 pagesEchocardiography in Hemodynamic MonitoringDr.Biswajit jenaNo ratings yet
- NOAF en Paciente Critico RevisionDocument11 pagesNOAF en Paciente Critico RevisionARTURO YOSHIMAR LUQUE MAMANINo ratings yet
- Uji Klinis 5Document10 pagesUji Klinis 5Verliatesya TugasNo ratings yet
- BNP 3Document9 pagesBNP 3omarfaridtawfikNo ratings yet
- 7.2014 Evidence Based Guideline For The Management of High BP in Adults (JNC 8)Document26 pages7.2014 Evidence Based Guideline For The Management of High BP in Adults (JNC 8)ganda gandaNo ratings yet
- Función Neurocognitiva en El Paciente Con CáncerDocument22 pagesFunción Neurocognitiva en El Paciente Con CáncerMIGUEL MORENONo ratings yet
- Part 2diagnostic of NPH PDFDocument13 pagesPart 2diagnostic of NPH PDFrys239No ratings yet
- Atm 09 20 1587Document14 pagesAtm 09 20 1587Wina Pertiwi 2003113414No ratings yet
- The Prognostic Value of Prognostic Nutritional Index (PNI) and Neutrophil To Lymphocyte Ratio (NLR) For Advanced Non-Small Cell Lung Cancer Treated With Platinum-Based ChemotherapeuticsDocument12 pagesThe Prognostic Value of Prognostic Nutritional Index (PNI) and Neutrophil To Lymphocyte Ratio (NLR) For Advanced Non-Small Cell Lung Cancer Treated With Platinum-Based ChemotherapeuticsWilliamRayCassidyNo ratings yet
- 55421-Gagal JantungDocument21 pages55421-Gagal JantungAngie CouthalooNo ratings yet
- Etm 07 03 0604Document5 pagesEtm 07 03 0604Raissa Metasari TantoNo ratings yet
- Accuracy of Calculated Free Valproate LevelsDocument9 pagesAccuracy of Calculated Free Valproate LevelskelracheltwrNo ratings yet
- Clinical Guideline Diagnosing Syncope Part 1: Value of History, Physical Examination, and ElectrocardiographyDocument8 pagesClinical Guideline Diagnosing Syncope Part 1: Value of History, Physical Examination, and ElectrocardiographyPriya JainNo ratings yet
- Periodontal Accelerated Osteogenic OrthodonticsDocument6 pagesPeriodontal Accelerated Osteogenic Orthodonticsyui cherryNo ratings yet
- Persuasive Speech OutlineDocument5 pagesPersuasive Speech Outlineapi-256458286No ratings yet
- A Chance To Save Millions of Lives by Freeing Up Drug Patents - Advanced PDFDocument5 pagesA Chance To Save Millions of Lives by Freeing Up Drug Patents - Advanced PDFhahahapsuNo ratings yet
- Approach To The Patient in Shock: by James Holencik, DODocument52 pagesApproach To The Patient in Shock: by James Holencik, DOLydia MamurNo ratings yet
- PERDEV DLL Unit 1 - M3 (Developmental Stages Handout)Document4 pagesPERDEV DLL Unit 1 - M3 (Developmental Stages Handout)Leonila MirandaNo ratings yet
- Test Bank For Mosbys Essentials For Nursing Assistants 4th Edition SorrentinoDocument24 pagesTest Bank For Mosbys Essentials For Nursing Assistants 4th Edition Sorrentinozacharymcleanpdqogjyfeb100% (47)
- Surat Permintaan Obat Dinkes BaruDocument21 pagesSurat Permintaan Obat Dinkes BaruHafizh JhunkoNo ratings yet
- TermDocument3 pagesTermapi-308717184No ratings yet
- Health and Wellbeing: AT WORK 2021Document37 pagesHealth and Wellbeing: AT WORK 2021Constantin CiacaruNo ratings yet
- Comparing and Contrasting Lady Macbeth and Ophelia From HamletDocument5 pagesComparing and Contrasting Lady Macbeth and Ophelia From HamletYashika MalhotraNo ratings yet
- Rhomboid Flap For Pilonidal Sinus - Our ExperienceDocument5 pagesRhomboid Flap For Pilonidal Sinus - Our ExperienceKhalidHussainNo ratings yet
- Research Proposal-1Document28 pagesResearch Proposal-1sowsthikaNo ratings yet
- Hizon Interview Group 2Document3 pagesHizon Interview Group 2Dan HizonNo ratings yet
- House Bill 15-1043Document19 pagesHouse Bill 15-1043Michael_Lee_RobertsNo ratings yet
- Class XII Syllabus PDFDocument60 pagesClass XII Syllabus PDFAman SinghNo ratings yet
- Art Comparison Essay ExampleDocument5 pagesArt Comparison Essay Exampleflrzcpaeg100% (2)
- Ebook Electrocardiography For Healthcare Professionals PDF Full Chapter PDFDocument67 pagesEbook Electrocardiography For Healthcare Professionals PDF Full Chapter PDFkenneth.bell482100% (28)
- Anodontia of Permanent Teeth - A Case ReportDocument3 pagesAnodontia of Permanent Teeth - A Case Reportanandsingh001No ratings yet
- BioassayDocument38 pagesBioassayMuhammad Masoom AkhtarNo ratings yet
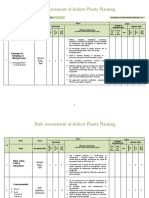
- Risk Assessment of Indoor Plants PlantingDocument5 pagesRisk Assessment of Indoor Plants Plantingطارق رضوانNo ratings yet
- The Peat WhispererDocument85 pagesThe Peat Whispererzarrin77100% (6)
- ARC 360 NGP InstructionManualDocument24 pagesARC 360 NGP InstructionManualLMTNo ratings yet
- Why Is Research Important - NHS GroupDocument8 pagesWhy Is Research Important - NHS GroupRoxan PacsayNo ratings yet
- Complete Holistic Guide To Working Out in The GymDocument218 pagesComplete Holistic Guide To Working Out in The Gympsichi21No ratings yet
- Foundation of Professional Nursing PracticeDocument5 pagesFoundation of Professional Nursing PracticeIvan LouiseNo ratings yet
- Iap Guidelines On Rickettsial Diseases in ChildrenDocument7 pagesIap Guidelines On Rickettsial Diseases in Childrenitaa19No ratings yet
- LENS Skin Disorders 2324Document49 pagesLENS Skin Disorders 2324Zyrille Moira MaddumaNo ratings yet
- Cleft Lip and PalateDocument18 pagesCleft Lip and Palateicywitch100% (1)
- "Rights of Disable Person": Dr. Nazia KhanDocument25 pages"Rights of Disable Person": Dr. Nazia KhanAnonymous tOgAKZ8No ratings yet
- Muhanga District Development Plan 2013-2018-1 01Document116 pagesMuhanga District Development Plan 2013-2018-1 01Joseph Tuseku Officiel100% (1)