Professional Documents
Culture Documents
Tren Kesalahan Pengobatan Dan Efek Dari Faktor Yang Berhubungan Dengan Orang, Terkait Lingkungan Dan Komunikasi Pada Kesalahan Pengobatan Di Rumah Sakit Anak
Uploaded by
Enggar Ardiani TagapOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Tren Kesalahan Pengobatan Dan Efek Dari Faktor Yang Berhubungan Dengan Orang, Terkait Lingkungan Dan Komunikasi Pada Kesalahan Pengobatan Di Rumah Sakit Anak
Uploaded by
Enggar Ardiani TagapCopyright:
Available Formats
doi:10.1111/jpc.
14193
ORIGINAL ARTICLE
Medication error trends and effects of person-related,
environment-related and communication-related factors on
medication errors in a paediatric hospital
Elizabeth Manias ,1,2,3 Noel Cranswick,4,5 Fiona Newall,3,5,6 Ellie Rosenfeld,3 Carlye Weiner,3 Allison Williams,7
Ian CK Wong,8 Narelle Borrott,3 Jerry Lai9 and Sharon Kinney3,6
1
School of Nursing and Midwifery, Centre for Quality and Patient Safety Research, Deakin University, Sydney, New South Wales, 2Department of Medicine,
Royal Melbourne Hospital, 3Melbourne School of Health Sciences, and 6Department of Paediatrics, Royal Children’s Hospital, University of Melbourne,
4
Department of Medicine, Clinical Pharmacology Unit, and 5Murdoch Childrens Research Institute, Royal Children’s Hospital, 7School of Nursing and
Midwifery, Monash University, Melbourne, 9eResearch, Deakin University, Geelong, Victoria, Australia and 8Research Department of Practice and Policy,
School of Pharmacy, University College London, London, United Kingdom
Aim: This study aimed to examine reported medication error trends in an Australian paediatric hospital over a 5-year period and to determine
the effects of person-related, environment-related and communication-related factors on the severity of medication outcomes. In particular, the
focus was on the influence of changes to a hospital site and structure on the severity of medication errors.
Methods: A retrospective clinical audit was undertaken over a 5-year period of paediatric medication errors submitted to an online voluntary
reporting system of an Australian, tertiary, public teaching paediatric hospital. All medication errors submitted to the online system between
1 July 2010 and 30 June 2015 were included.
Results: A total of 3340 medication errors was reported, which corresponded to 0.56% medication errors per combined admissions and presenta-
tions or 5.73 medication errors per 1000 bed days. The most common patient outcomes related to errors requiring monitoring or an intervention to
ensure no harm occurred (n = 1631, 48.8%). A new hospital site and structure had 0.354 reduced odds of producing medication errors causing possible
or probable harm (95% confidence interval 0.298–0.421, P < 0.0001). Patient and family involvement had 1.270 increased odds of identifying medication
errors associated with possible or probable harm compared with those causing no harm (95% confidence interval 1.028–1.568, P = 0.027). Interrupted
time series analyses showed that moving to a new hospital site and structure was associated with a reduction in reported medication errors.
Conclusion: Encouraging child and family involvement, facilitating hospital redesign and improving communication could help to reduce the
harm associated with medication errors.
Key words: family involvement; hospitalised child; interdisciplinary communication; medication error; patient involvement.
What is already known on this topic What this paper adds
1 Children are at high risk of experiencing medication errors. 1 Hospitalised children or family members alerted health professionals
2 Past research has been conducted on identifying the prevalence about the occurrence of medication errors in 15% of occasions.
of medication errors in children; however, little is known about 2 Patient and family involvement was associated with increased odds
the causes, human factors, contributing factors and patient out- of identifying medication errors causing possible or probable harm,
comes of medication errors, as well as the involvement of while a new hospital site and structure was associated with reduced
patients and family members in detecting medication errors. odds of medication errors causing possible or probable harm.
3 Past research shows that common types of medication errors 3 Interrupted time series results showed that a new hospital site
include overdose or under-dose, dose omission, mistakes in adminis- and structure was associated with a reduced percentage of
tration techniques, wrong medication, wrong person and inattention medication errors per combined admissions and presentations
to children’s changing needs, including alterations in body weight. and reduced medication errors per 1000 bed days.
Correspondence: Professor Elizabeth Manias, School of Nursing and
Midwifery, Centre for Quality and Patient Safety Research, Deakin Univer- Children are at high risk of experiencing medication errors.
sity, 221 Burwood Highway, Burwood, Vic. 3125, Australia; email:
They are vulnerable due to their limited ability to communicate,
emanias@deakin.edu.au
especially those who are preverbal and have difficulties in
Conflict of interest: None declared. expressing their needs. Insufficient availability of paediatric for-
Accepted for publication 22 July 2018. mulations contributes to the need for increased medication
Journal of Paediatrics and Child Health (2018) 1
© 2018 The Authors
Journal of Paediatrics and Child Health published by John Wiley & Sons Australia, Ltd on behalf of Paediatrics and Child Health Division (The Royal Australasian College of
Physicians)
This is an open access article under the terms of the Creative Commons Attribution-NonCommercial License, which permits use, distribution and reproduction in any medium,
provided the original work is properly cited and is not used for commercial purposes.
Medication error trends and effects E Manias et al.
compounding, and a lack of information from manufacturers health promotion and prevention programmes. It contains an
about preparing these medications can also lead to medication emergency department, an intensive care unit and a state-wide
errors.1 trauma service. The human research ethics committee of the hos-
Extensive research has been conducted on identifying the pital approved the conduct of the study. A medication error was
prevalence of medication errors in children. Medication error defined as any preventable event that may have caused or led to
rates differ considerably due to varying contexts of care and inappropriate medication use or patient harm while the medica-
methods used for analysis. Variations have ranged between 0.51 tion was in the control of the health professional, patient or fam-
per 1000 bed days2 and 82.9 medication errors per 1000 bed ily member.9
days.3 On 26 October 2011, during the study period, the hospital had
In attempting to reduce medication errors, increased focus moved from an old site to a new building complex. On that day,
has been placed on person-related factors, such as addressing all patients were moved from the old hospital site to the new
how nurses, doctors and pharmacists contribute to these errors. hospital site, including all health professionals involved in provid-
While past research has shown that health professionals can ing their care. Alongside the move, there were structural changes
influence medication errors,4 less is known about how child associated with the new hospital complex. In the new hospital,
and family involvement may prevent and detect medication most hospitalised children were situated in single rooms, with
errors. A retrospective clinical audit conducted in Australia dedicated spaces for family members. These dedicated spaces
demonstrated that, in 8.0% of reported medication errors were created to facilitate family-centred care and engagement
(n = 219), children and family members had alerted health pro- with clinicians. Dedicated medication rooms were developed for
fessionals that a medication error had occurred.5 Further work all wards in the new hospital (Fig. 1). In the old hospital, only
is needed to examine child and family involvement in influenc- one medical ward had a dedicated medication room, whereas in
ing medication errors.
all other wards, the medication room was combined with the
Major causes of medication errors involve communication-
patient treatment room (Fig. 2). In the old hospital, when the
related factors,5,6 with research showing that communication
medication room was combined with the patient treatment room,
problems account for over half of all causes associated with medi-
there was extensive activity, with children undergoing proce-
cation errors.7 Difficulties with written communication feature
dures such as peripheral intravenous cannula insertion, vene-
predominantly, involving illegible and misinterpreted medication
puncture and bladder catheterisation, which sometimes led to
orders. Conversely, details about how communication processes,
distractions from excessive noise and interruptions. In both forms
such as ward rounds and handovers, affect medication errors are
largely missing. of the medication room, whether combined with the treatment
Environment-related factors can have an enormous impact on room in the old hospital or as a stand-alone facility in the new
patient safety. A case study approach was undertaken in the hospital, pharmacists dispensed medications, physicians ordered
USA8 where extensive consultation was sought from architects, medications and nurses prepared and administered medications.
patients, family members, managers and clinicians about what In the new hospital, the nurse–patient ratio was the same, each
they felt was important in designing a new hospital. Through unit had the same staff, and guidelines and policies were
these consultations, a comprehensive checklist was created to the same.
guide the development of the new hospital and enable a culture
of patient safety. In this study, there was no information about
how environment-related factors affected medication errors. The
hospital targeted was an acute care facility with no details about Data collection and procedure
specific provisions for paediatric care.
All medication errors submitted to the online system between
Examining the complexities of diverse factors associated with
1 July 2010 and 30 June 2015 were included. Children’s medical
medication errors can help identify how these factors influence
records were accessed. For many years, hospital management
the severity of harm and ascertain possible strategies for
adopted a no-blame policy, actively encouraging clinicians to sub-
improved patient safety. The aims of the study were to exam-
mit medication errors as they occurred. As a result, reported
ine reported medication error trends in an Australian paediat-
medication errors contained detailed descriptions of medications
ric hospital over a 5-year period and to determine the effects
of person-related, environment-related and communication- errors in the form of free text as well as comprehensive responses
related factors on the severity of medication outcomes. In par- to close-ended questions. A medication safety committee devel-
ticular, the key intent was to focus on the influence of oped the summary data of medication errors, and those with
changes to a hospital site and structure on the severity of severe outcomes were discussed and analysed as they occurred.
medication errors. Feedback was incorporated in online medication error reports on
patient outcomes and in strategies adopted to address recurring
problems and causes.
Methods
The National Coordinating Council for Medication Error
A retrospective clinical audit was undertaken over a 5-year Reporting and Prevention tool was used as the data collection
period of paediatric medication errors submitted to an online vol- instrument.9 This tool provides a structured and standardised
untary reporting system of an Australian, tertiary, public, teach- approach in categorising medication errors. The tool enabled
ing paediatric hospital. The hospital, comprising 334 beds, person-, environment- and communication-related factors to be
provides a comprehensive range of clinical services, tertiary care, systematically classified.
2 Journal of Paediatrics and Child Health (2018)
© 2018 The Authors
Journal of Paediatrics and Child Health published by John Wiley & Sons Australia, Ltd on behalf of Paediatrics and Child Health Division (The Royal Australasian College of
Physicians)
E Manias et al. Medication error trends and effects
Fig. 1 Medication room in the new
hospital.
Fig. 2 Medication room combined
with the patient treatment room in
the old hospital.
Data analysis outcome measure (scores of 1–3 relating to no patient harm and
scores 4–8 relating to possible or probable patient harm).9
Descriptive and inferential data analysis was undertaken using Person-related factors included the individual responsible for the
SPSS, version 23 (IBM Corp., Chicago, IL, USA). Frequency error (nurse/doctor/pharmacist/patient/family member) and
counts and percentage counts were calculated for all variables of patient and family involvement in identifying a medication error
interest. Calculations of medication errors per combined admis- (yes/no). Environment-related factors included: the hospital site
sions and presentations and medication errors per 1000 bed days and structure (new/old) and clinical site of the medication errors.
were obtained from resourcing the statistical data of the hospital’s Communication-related factors included: informal bedside com-
annual reports. These annual reports contained data on the num- munication problem (yes/no), clinical handover problem
ber of patient admissions and presentations and the number of (yes/no) and medical record documentation problem (yes/no).
bed days over the 5-year period and were used for data collection These communication-related factors were selected because they
and analysis. were the most commonly occurring data. Use of the new hospital
Univariate associations with severity of medication errors were site and structure commenced on 26 October 2011. Thus, medi-
examined for all person-related, environment-related and cation errors taking place before 26 October 2011 occurred in the
communication-related factors using cross tabulations and chi old hospital site and structure, while those taking place from
square tests. The outcome or dependent variable was the patient 26 October 2011 onwards occurred in the new hospital site and
Journal of Paediatrics and Child Health (2018) 3
© 2018 The Authors
Journal of Paediatrics and Child Health published by John Wiley & Sons Australia, Ltd on behalf of Paediatrics and Child Health Division (The Royal Australasian College of
Physicians)
Medication error trends and effects E Manias et al.
structure. Binary multiple logistic regression modelling was sub- arbitrarily chosen to safeguard against excluding potentially
sequently undertaken, with factors demonstrating univariate important factors at the univariate level when determining what
associations of less than or equal to P = 0.25. Use of a less strin- factors to test in the binary logistic modelling level.10 Binary
gent P value of 0.25, compared with a P value of 0.05, was logistic regression modelling involved calculating the ability of
various explanatory variables to increase or decrease the odds of
a binary categorical outcome, which can only have two values. In
Table 1 Clinical settings in which medication errors occurred this case, the values of the binary outcome were the presence of
(n = 3340) medication errors causing possible or probable harm and those
causing no harm. The level of significance used for logistic model-
Clinical setting n %
ling was α = 0.05.
Intensive care unit 462 13.8 The impact of the new hospital site and structure was initially
Medical unit 441 13.2 explored through an interrupted time series analysis that
Surgical unit 362 10.8 included both the step-change (hospital site, old = 0; new = 1)
Neonatal intensive care unit 354 10.6 and slope-change (time) components and the interaction term.
Cardiac unit 269 8.1 However, because the contribution of the slope-change and
Psychiatry unit 255 7.6 interaction components was statistically non-significant, our
Oncology unit 192 5.7 final model retained only the step-change component.11 Due to
Neuroscience unit 158 4.7 over-dispersion, all analyses were conducted using the quasi-
Adolescent unit 142 4.3 Poisson model. There was no clear sign of dependencies
Pharmacy department 139 4.2 (i.e. autocorrelation) or seasonality; thus, no further adjust-
Emergency department 128 3.8 ments were made.
Perioperative area 124 3.7
Immunology department 106 3.2
Hospital-in-the-home 79 2.4
Medical short stay 70 2.1 Results
Surgical short stay 44 1.3
During the study period, a total of 3340 medication errors was
Radiology 10 0.3
reported, which corresponded to 0.56% per combined admissions
Outpatient units 5 0.1
and presentations or 5.73 medication errors per 1000 bed days.
In addition, there were 6680 human factors and 4008 causes
Table 2 Patient outcomes of medication errors relating to eight categories of harm (n = 3340 medication errors)
Patient outcome n % Examples of patient outcome
1 Circumstances had the capacity to cause error 14 0.4 Warfarin dose not signed on drug chart
2 Error occurred, but the error did not reach the patient 618 18.5 600 mcg of naloxone was prescribed on the medication
chart instead of 60 mcg – 10× overdose. Patient did
not receive the dose of naloxone
3 Error occurred that reached the patient but did not 979 29.3 Weight recorded as 23 kg when weighed in day surgery
cause patient harm admission; on inspection, the patient obviously
weighed less than this, but issue was not detected until
patient was anaesthetised and after premedication
given comprising midazolam and paracetamol
(acetaminophen)
4 Error occurred that reached the patient and required 1631 48.8 Intravenous order for intravenous ticarcillin + clavulanic
monitoring or intervention to confirm no harm acid in emergency department but not handed over.
Intravenous antibiotics commenced about 14 h late
5 Error occurred that resulted in temporary harm and 89 2.7 Noradrenaline (norepinephrine) found to be
required intervention disconnected following severe hypotension and need
of volume and increase of inotrope requirements
following a bed turn
6 Error occurred that resulted in temporary harm and 8 0.2 Patient’s intravenous antibiotic, flucloxacillin, changed to
required prolonged hospitalisation oral antibiotic but continued to be given as intravenous
form, delaying patient discharge
7 Error occurred that resulted in permanent patient 0 0 Not applicable
harm
8 Error occurred that required intervention necessary to 1 0.1 Patient given overdose of arginine. Patient was
sustain life transferred to paediatric intensive care unit for
hemofiltration and treatment of the overdose
4 Journal of Paediatrics and Child Health (2018)
© 2018 The Authors
Journal of Paediatrics and Child Health published by John Wiley & Sons Australia, Ltd on behalf of Paediatrics and Child Health Division (The Royal Australasian College of
Physicians)
E Manias et al. Medication error trends and effects
Table 3 Causes associated with medication errors (n = 4008 causes) Table 4 Human factors and contributing factors (n = 6680)
Cause of medication error n % Type of factors n %
Communication-related factors, n = 3340 (83.3%) Human factors, n = 3340
Medical record documentation 717 17.9 Performance deficit 1436 21.5
Clinical handover 571 14.2 Knowledge deficit 504 7.5
Informal bedside communication 542 13.5 Inadequate screening of patient 445 6.7
Misinterpretation of order 518 12.9 Miscalculation of dose or infusion rate 341 5.1
Misread or unread order 481 12.0 Failure to activate delivery system properly 173 2.6
Illegible handwriting 235 5.9 Wrong amount of active medication used 126 1.9
Decimal point 107 2.7 Error in stocking 108 1.6
Units of measurement 91 2.3 Wrong diluent used for infusion 69 1.0
Telephone communication 56 1.4 Stress 55 0.8
Ward round 22 0.5 Wrong amount of diluent used 48 0.7
Confusion with medication name, n = 229 (5.7%) Wrong medication added to infusion 27 0.4
Generic name confusion 203 5.1 Intimidating behaviour 8 0.1
Brand name confusion 26 0.6 Contributing factors, n = 3340
Confusion with labelling and reference material, n = 439 (11.0%) Policies and procedures 1619 24.2
Label of dispensed product is wrong 161 4.0 Frequent interruptions and distractions 639 9.6
Problems with reference material 142 3.5 Communication relating to patient 461 6.9
Container of manufacturer similar or 136 3.4 movements
confusing Lack of available trained health 216 3.2
professionals
Inadequate training provided 155 2.3
Insufficient or incorrect counselling offered 126 1.9
identified in the database during the study period. The median to patients or parents
age of children was 4.3 years (interquartile range 4 months, Floor stock 124 1.9
13.5 years), and 30.4% were children aged 12 months or youn-
ger. Of the reported medication errors, 43.5% occurred in female
children. Table 1 shows the clinical settings in which medication
errors occurred. Commonly occurring human factors included performance
Most medication errors occurred during the daytime between deficits (n = 1436, 21.5%) and knowledge deficits (n = 504,
0700 and 1530 (n = 1736, 52.0%). However, considerable medi- 7.5%). Contributing factors that frequently occurred included cli-
cation errors also occurred after business hours and overnight. nicians not adequately following policies and procedures
Medication errors took place predominantly during weekdays, (n = 1619, 24%). Problems with patients’ movements across
but 20.6% of medication errors occurred during weekend days. transitions, such as transfers involving emergency department
The most common patient outcomes related to errors requiring and operating rooms, were also evident (n = 461, 6.9%)
monitoring or an intervention to ensure that no harm occurred (Table 4).
(n = 1631, 48.8%), followed by errors reaching patients that did Bivariate logistic regression modelling identified 10 factors that
not cause patient harm (n = 979, 29.3%) (Table 2). significantly predicted associations with children experiencing
Table 3 shows communication-related factors of medication possible or probable harm versus no harm from medication errors
errors, details about generic and trade name confusion and con- (Table 5). In situations where doctors or pharmacists were
cerns with labelling and reference materials. A total of 4008 responsible for the medication error, there were reduced odds of
causes were attributed to medication errors. The most common a harmful medication error occurring compared to when nurses
communication-related factor was problems with medical record were responsible. Involvement of children and families in identi-
documentation (n = 717, 17.9%), which included health profes- fying medication errors had 1.270 increased odds of harmful
sionals not checking for documented allergies and confusion medication errors occurring compared with those who were not
about children’s actual recorded weight. Labels of dispensed involved. Problems with clinical handover, informal bedside com-
products sometimes had incorrect details documented, but the munication and medical record documentation all increased the
contents of the products were correct (e.g. identification of vehi- odds of harmful medication errors. The new hospital site and
cles on intravenous fluid bags with additives). At other times, the structure showed 0.354 reduced odds in being associated with
labels and the contents were incorrect. Problems with reference harmful medication errors compared with the old hospital site
materials included limitations associated with available medica- and structure. The intensive care unit, oncology unit and emer-
tion resources, leading to delays in administration as clinicians gency department all demonstrated increased odds of having
attempted to obtain further information (n = 142, 3.5%). Exam- harmful medication errors compared to medical units.
ples included availability of injectable guidelines for powder vol- Figure 3 shows the interrupted time series trends for the effect
umes of methylprednisolone for established brands but not for of the new hospital site and structure on reported medication
new brands and the lack of administration instructions for cyclo- errors. The risk of percentage medication errors per combined
phosphamide and mesna. admission and presentation was reduced by 35.4% (relative risk
Journal of Paediatrics and Child Health (2018) 5
© 2018 The Authors
Journal of Paediatrics and Child Health published by John Wiley & Sons Australia, Ltd on behalf of Paediatrics and Child Health Division (The Royal Australasian College of
Physicians)
Medication error trends and effects E Manias et al.
Table 5 Binary logistic regression model for explanatory factors associated with medication errors causing possible or probable harm (n = 3340)
Variable Reference level Comparator level Odds ratio 95% confidence P value
intervals
Person-related factors
Person responsible for the medication error Nurse Doctor 0.571 0.483–0.674 <0.0001
Person responsible for the medication error Nurse Pharmacist 0.410 0.285–0.591 <0.0001
Patient and family involvement in detecting an No Yes 1.270 1.028–1.568 0.027
incident
Environment-related factors
New hospital site and structure Old New 0.354 0.298–0.421 <0.0001
Clinical setting where error occurred Medical ward Intensive care unit 1.516 1.143–2.010 0.004
Clinical setting where error occurred Medical ward Oncology unit 1.794 1.250–2.573 0.002
Clinical setting where error occurred Medical ward Emergency department 1.728 1.131–2.640 0.011
Communication-related factors
Problem with informal bedside communication No Yes 1.360 1.099–1.685 0.005
Problem with medical record documentation No Yes 1.327 1.083–1.625 0.006
Problem with clinical handover No Yes 2.042 1.652–2.523 <0.0001
Fig. 3 Interrupted time series analysis
demonstrating the effect of the new hospital
site and structure on medication errors.
(RR) = 0.598, 95% confidence interval (0.464–0.770)) under the appropriate training in the administration of high-risk medica-
new hospital site and structure and by 36.7% (RR = 0.633 tions in children, and there were reports of nurses having only
(0.492–0.813)) for the number of medication errors per 1000 basic information to help them safely mix and administer intrave-
bed days. nous medications. Nurses were also involved in medication errors
causing harm where patients moved from one clinical setting to
another, which was often compounded by nurses’ busyness in
Discussion
the work area and having to compete with multiple priorities.
The clinical audit demonstrated how person-, environment- and Past research has demonstrated that nurses’ lack of familiarity
communication-related factors affected medication errors in a with medications, the environment, procedures and equipment
paediatric hospital. Implementation of a new hospital site and are common causes of medication errors.7
structure was associated with reduced odds of medication errors Children and family members alerted health professionals
producing possible or probable harm and with a reduction in about medication errors in 15% of cases, particularly about
reported medication errors. Patient and family involvement was those errors associated with possible or probable harm. These
important in identifying medication errors. alerts from children and family members comprised diverse
Doctors and pharmacists had reduced odds in been associated types of medications, including analgesics, antipsychotics, neu-
with medication errors producing possible or probable harm com- rological agents, blood and electrolytes and anti-infective
pared to nurses. In examining the contributing factors affecting agents. Hence, this detection occurred regardless of whether
health disciplines, nurses were subjected to frequent interrup- the child required medication for treatment of an acute or
tions and distractions, especially in relation to errors leading to chronic condition. Family presence possibly contributed to
harm. There were also situations where nurses lacked astute awareness of the safety checks conducted by nurses in
6 Journal of Paediatrics and Child Health (2018)
© 2018 The Authors
Journal of Paediatrics and Child Health published by John Wiley & Sons Australia, Ltd on behalf of Paediatrics and Child Health Division (The Royal Australasian College of
Physicians)
E Manias et al. Medication error trends and effects
monitoring and administering medications. As a result, family Communication-related factors contribute to the occurrence of
members acted as watchful observers to identify deviations medication errors. Implementation of a new hospital site and
from expected routines. structure can have an impact on reducing the severity of medica-
The new hospital site and structure was associated with tion errors, as well as enhancing patient and family contribution
reduced odds of medication errors causing possible or probable in identifying medication errors. Future research should focus on
harm and a reduction of reported medication errors. Past work evaluating strategies for patient and family involvement in reduc-
has shown that spatial designs can increase proximity between ing errors before causing harm. Interventional work involving
health professionals, patients and family members, thereby family-centred configurations of hospital spaces needs to be
enhancing communication.12 It is possible that the new spatial tested for their impact on medication errors.
design was conducive for improved communication as family
members may have been more likely to speak up if they sus- Acknowledgement
pected an actual or possible medication error.13 The presence of
dedicated medication rooms, where health professionals dis- Funding was provided by the Australian Research Council, Dis-
cussed medication decisions with minimal distractions, may have covery Grant Scheme (DP130100221).
also impacted the severity and number of medication errors
occurring. Compared with the old hospital, there was greater
availability of space to enable collaborative decision-making. References
These decisions related to nurses independently checking dose 1 Wong ICK, Ghaleb MA, Franklin BD, Barber N. Incidence and nature of
calculations, preparing parenteral medications for administration dosing errors in paediatric medications – A systematic review. Drug
and discussing options for providing pro re nata ‘as required’ med- Saf. 2004; 27: 661–70.
ications. Decisions also comprised physicians communicating 2 Ross LM, Wallace J, Paton JY. Medication errors in a paediatric teach-
about preferences for medication prescription and specialty per- ing hospital in the UK: Five years operational experience. Arch. Dis.
sonnel, such as diabetic educators, and acute pain clinic nurses Child. 2000; 83: 492–7.
and physicians interacting about treatment options. Pharmacists 3 Wilson DG, McArtney RG, Newcombe RG et al. Medication errors in
also used these rooms to clarify medication orders with physi- paediatric practice: Insights from a continuous quality improvement
approach. Eur. J. Pediatr. 1998; 157: 769–74.
cians, to identify medication supply needs and to organise admis-
4 Ghaleb MA, Barber N, Franklin BD, Wong ICK. The incidence and
sion and discharge counselling sessions.
nature of prescribing and medication administration errors in paediat-
Clinical settings associated with medication errors leading
ric inpatients. Arch. Dis. Child. 2010; 95: 113–8.
to possible or probable harm included intensive care, emer- 5 Manias E, Kinney S, Cranswick N, Williams A. Medication errors in
gency care and oncology care. High-risk medications such as hospitalised children. J. Paediatr. Child Health 2014; 50: 71–7.
intravenous electrolytes, inotropes, opioid analgesics, antico- 6 Sears K, O’Brien-Pallas L, Stevens B, Murphy GT. The relationship
agulants and cytotoxic medications are commonly prescribed between nursing experience and education and the occurrence of
in these environments, which are more likely to cause cata- reported pediatric medication administration errors. J. Pediatr. Nurs.
strophic harm compared with other types of medications.14 In 2016; 31: e283–90.
these settings, health professionals encountered problems 7 Keers RN, Williams SD, Cooke J, Ashcroft DM. Causes of medication
administration errors in hospitals: A systematic review of quantitative
with patient movements. With patient mobility between these
and qualitative evidence. Drug Saf. 2013; 36: 1045–67.
specialty settings and other environments, such as the operat-
8 Reiling J. Creating a culture of patient safety through innovative hos-
ing room and radiology department, hospitalised children
pital design. In: Henriksen K, Battles J, Marks E, Lewin D, eds.
were at increased risk of experiencing a medication error with Advances in Patient Safety: From Research to Implementation, vol. 2.
each transfer. Rockville, MD: Agency for Healthcare Research and Quality;
2005; 1–16.
Limitations 9 National Coordinating Council for Medication Error Reporting and Pre-
vention. About Medication Errors. Rockville, MD: The Council; 2017.
The study comprised a retrospective audit undertaken in one Available from: http://www.nccmerp.org/about-medication-errors
health service. More medication errors may have occurred than [accessed 1 March 2017].
the number documented on the online reporting site. However, 10 Stoltzfus JC. Logistic regression: A brief primer. Acad. Emerg. Med.
2011; 18: 1099–104.
because the hospital had a no-blame reporting policy, and there
11 Lopez Bernal J, Cummins S, Gasparrini A. Interrupted time series
were detailed explanations accompanying many entries, it is
regression for the evaluation of public health interventions: A tutorial.
likely that the prevalence is an accurate reflection of what hap-
Int. J. Epidemiol. 2017; 46: 348–55.
pened in actual practice. At the time of data collection, only 12 Liu W, Manias E, Gerdtz M. The effects of physical environments in
16 months of data were available prior to the hospital move, medical wards on medication communication processes affecting
while 44 months of data were available following the patient safety. Health Place 2014; 26: 188–98.
hospital move. 13 Harris N, Badr LK, Saab R, Khalidi A. Caregivers’ perception of drug
administration safety for pediatric oncology patients. J. Pediatr.
Oncol. Nurs. 2014; 31: 95–103.
Conclusion 14 Grissinger M. Your high-alert medication list is relatively useless
The study showed that children and family members play a sig- without associated risk-reduction strategies. Pharm. Therap.
2016; 41: 598–600.
nificant role in identifying medication errors in clinical practice.
Journal of Paediatrics and Child Health (2018) 7
© 2018 The Authors
Journal of Paediatrics and Child Health published by John Wiley & Sons Australia, Ltd on behalf of Paediatrics and Child Health Division (The Royal Australasian College of
Physicians)
You might also like
- Pediatirc Medical ErrorDocument7 pagesPediatirc Medical ErrorJulls ApouakoneNo ratings yet
- Roughead 2016Document10 pagesRoughead 2016Armando cortezNo ratings yet
- Skin Care For Pediatric2Document7 pagesSkin Care For Pediatric2Sri Nauli Dewi LubisNo ratings yet
- Reducing Medication Errors in HospitalsDocument9 pagesReducing Medication Errors in Hospitalsakko aliNo ratings yet
- Emergency Department Asthma Medication Delivery Program: An Initiative To Provide Discharge Prescriptions and EducationDocument7 pagesEmergency Department Asthma Medication Delivery Program: An Initiative To Provide Discharge Prescriptions and EducationPutra PancasilaNo ratings yet
- Pqs 2 E033Document7 pagesPqs 2 E033Putra PancasilaNo ratings yet
- 2018 - Baraki Et AlDocument8 pages2018 - Baraki Et AlazeemathmariyamNo ratings yet
- Maternal Breast Milk Feeding and Length of Treatment in Infants With Neonatal Abstinence SyndromeDocument7 pagesMaternal Breast Milk Feeding and Length of Treatment in Infants With Neonatal Abstinence SyndromeHariCexinkwaeNo ratings yet
- Written Assignment 5 Corrected Final PaperDocument18 pagesWritten Assignment 5 Corrected Final Paperapi-401934380No ratings yet
- Alexis Fiorello Phase Three Ethics Part TwoDocument7 pagesAlexis Fiorello Phase Three Ethics Part TwoElite TutorsNo ratings yet
- Medication Errors 111765Document7 pagesMedication Errors 111765akko aliNo ratings yet
- Attributable To The Use of Medications (: Near MissesDocument4 pagesAttributable To The Use of Medications (: Near MissesdudijohNo ratings yet
- Pediatric Hospital Adherence To The Standard of Care For Acute GastroenteritisDocument9 pagesPediatric Hospital Adherence To The Standard of Care For Acute GastroenteritisAnggi Apriansyah PNo ratings yet
- Medication Error Patients Admitted To Medical Ward in Primary Hospital, Ethiopia: Prospective Obserbetional StudyDocument18 pagesMedication Error Patients Admitted To Medical Ward in Primary Hospital, Ethiopia: Prospective Obserbetional StudybezieNo ratings yet
- 210 1437 1 PB LibreDocument62 pages210 1437 1 PB Librezozorina21No ratings yet
- Medications and Pregnancy The Role of Community PHDocument15 pagesMedications and Pregnancy The Role of Community PHJaikapil KachhawaNo ratings yet
- Potential Medication Dosing Errors in Outpatient Pediatrics: See Editorial, P 727Document7 pagesPotential Medication Dosing Errors in Outpatient Pediatrics: See Editorial, P 727Tammy Utami DewiNo ratings yet
- First Do No Harm - Avoiding Medication Errors in ChildrenDocument8 pagesFirst Do No Harm - Avoiding Medication Errors in ChildrenAfriska Norma UtamaNo ratings yet
- Final Draft Medication Administration ErrorsDocument13 pagesFinal Draft Medication Administration Errorsapi-466369078100% (1)
- Medication Errors:: Don't Let Them Happen To YouDocument6 pagesMedication Errors:: Don't Let Them Happen To YouPhuong Tran100% (1)
- Drug Induced Birth DefectsDocument5 pagesDrug Induced Birth DefectsAbin ChandrakumarNo ratings yet
- Drug Utilization in The Pediatric Intensive Care UnitDocument9 pagesDrug Utilization in The Pediatric Intensive Care UnitLuciana OliveiraNo ratings yet
- SDOM Promising TherapiesDocument16 pagesSDOM Promising TherapiesdarlingcarvajalduqueNo ratings yet
- Congenital Anomalies Parents Concerns and Opinions To - 2018 - European JournaDocument1 pageCongenital Anomalies Parents Concerns and Opinions To - 2018 - European Journaburak yolcuNo ratings yet
- Editorial: Drugs During Pregnancy and Lactation: New Solutions To Serious ChallengesDocument2 pagesEditorial: Drugs During Pregnancy and Lactation: New Solutions To Serious ChallengesAndri Adma WijayaNo ratings yet
- Factors Influencing Paediatric Nurses' Responses To Medication AdministrationDocument4 pagesFactors Influencing Paediatric Nurses' Responses To Medication AdministrationYuni AstutiNo ratings yet
- Saudi Pharmaceutical JournalDocument5 pagesSaudi Pharmaceutical JournalVictor TabuncicNo ratings yet
- Standard Drug Concentrations and Smart-Pump Technology Reduce Continuous Medication Infusion Errors in Pediatric PatientsDocument7 pagesStandard Drug Concentrations and Smart-Pump Technology Reduce Continuous Medication Infusion Errors in Pediatric PatientsfatimamalmeidaNo ratings yet
- Labio y Paladar Hendido 1Document8 pagesLabio y Paladar Hendido 1Karina HernandezNo ratings yet
- Medication Use During Pregnancy, With Particular Focus On Prescription Drugs: 1976-2008Document8 pagesMedication Use During Pregnancy, With Particular Focus On Prescription Drugs: 1976-2008MARIA KARINA HERNANDEZ PEREZNo ratings yet
- medication errors paper 1Document6 pagesmedication errors paper 1api-739232245No ratings yet
- Final Issues PaperDocument10 pagesFinal Issues Paperapi-619271904No ratings yet
- 2017 - Alomari Et AlDocument18 pages2017 - Alomari Et AlazeemathmariyamNo ratings yet
- Families, Nurses and Organisations Contributing Factors To Medication Administration Error in Paediatrics: A Literature ReviewDocument15 pagesFamilies, Nurses and Organisations Contributing Factors To Medication Administration Error in Paediatrics: A Literature ReviewsabitaNo ratings yet
- Improving Primary Care in Rural Alabama With A Pharmacy InitiativeDocument7 pagesImproving Primary Care in Rural Alabama With A Pharmacy InitiativeBasilharbi HammadNo ratings yet
- EBP Deliverable Module 2Document6 pagesEBP Deliverable Module 2Marian SmithNo ratings yet
- The Role of Pharmacists in Minimizing Medication Errors in The Neonatal Intensive Care Unit: A Systematic ReviewDocument10 pagesThe Role of Pharmacists in Minimizing Medication Errors in The Neonatal Intensive Care Unit: A Systematic ReviewIJAR JOURNALNo ratings yet
- Clinical Reflective JournalDocument4 pagesClinical Reflective Journalapi-547521437No ratings yet
- Medication Errors in An Intensive Care Unit: OriginalresearchDocument10 pagesMedication Errors in An Intensive Care Unit: OriginalresearchFauziah AizulNo ratings yet
- 2019 Article 305 PDFDocument3 pages2019 Article 305 PDFDipyanalarNo ratings yet
- Kohn 2019Document8 pagesKohn 2019Elita RahmaNo ratings yet
- Jong, 2006 - A Survey of The Use of Off-Label and Unlicensed Drugs in A Dutch Childrens HospitalDocument7 pagesJong, 2006 - A Survey of The Use of Off-Label and Unlicensed Drugs in A Dutch Childrens HospitalthuanesgNo ratings yet
- Classification and Management of Feeding Difficulties in Children HO11-004 - E - With - WMDocument2 pagesClassification and Management of Feeding Difficulties in Children HO11-004 - E - With - WMCarlos GonzalezNo ratings yet
- Medication Error Research PaperDocument5 pagesMedication Error Research Paperafeaoebid100% (3)
- NURS4020 AshleyVigne Assessment2 Attemp1Document7 pagesNURS4020 AshleyVigne Assessment2 Attemp1ashleyNo ratings yet
- Institute For Safe Medication PracticesDocument6 pagesInstitute For Safe Medication Practicesadza30No ratings yet
- HOSPITAl PHARMACOEPIDEMIOLOGYDocument6 pagesHOSPITAl PHARMACOEPIDEMIOLOGYDhruvi PatelNo ratings yet
- Medication Error ThesisDocument6 pagesMedication Error Thesisoaehviiig100% (2)
- Artikel 3 Berland 2017Document8 pagesArtikel 3 Berland 2017Eline DebaereNo ratings yet
- JPPR 1345Document6 pagesJPPR 1345Omar Nassir MoftahNo ratings yet
- 2019 - Härkänen Et AlDocument8 pages2019 - Härkänen Et AlazeemathmariyamNo ratings yet
- MederrorpaperDocument6 pagesMederrorpaperapi-642984838No ratings yet
- Medication Errors in Community Pharmacy: An Investigation Into The Types and Potential CausesDocument9 pagesMedication Errors in Community Pharmacy: An Investigation Into The Types and Potential CausesdamiNo ratings yet
- 2017 - BABY BLUESDocument2 pages2017 - BABY BLUESPatrícia BodoniNo ratings yet
- Xylitol Syrup For The Prevention of Acute Otitis Media: PediatricsDocument9 pagesXylitol Syrup For The Prevention of Acute Otitis Media: PediatricsholaNo ratings yet
- 18factores Asociados Al Llamado Por Tto Oncologico Monestime Page 2020Document8 pages18factores Asociados Al Llamado Por Tto Oncologico Monestime Page 2020Milizeth VmNo ratings yet
- Pediatric Integrative PDFDocument21 pagesPediatric Integrative PDFallexyssNo ratings yet
- Medication Errors Their Causative and Preventive Factors2.Doc 1Document11 pagesMedication Errors Their Causative and Preventive Factors2.Doc 1Mary MannNo ratings yet
- Contraception for the Medically Challenging PatientFrom EverandContraception for the Medically Challenging PatientRebecca H. AllenNo ratings yet
- Adminasri, AMBARWATIDocument5 pagesAdminasri, AMBARWATIarikusuma013No ratings yet
- Belajar Memeriksa Ulang Prediksi Model Dari ADocument10 pagesBelajar Memeriksa Ulang Prediksi Model Dari AEnggar Ardiani TagapNo ratings yet
- Asosiasi Antara Doublechecking Dan Obat-ObatanDocument11 pagesAsosiasi Antara Doublechecking Dan Obat-ObatanEnggar Ardiani TagapNo ratings yet
- Apa Yang Kita Lakukan Ketika KitaDocument5 pagesApa Yang Kita Lakukan Ketika KitaEnggar Ardiani TagapNo ratings yet
- Apa Yang Sebenarnya Dideteksi Oleh Rutinitas Pemeriksaan Ulang Penilaian Observasional Dan Analisis Kualitatif Dari Inkonsistensi Yang DiidentifikasiDocument7 pagesApa Yang Sebenarnya Dideteksi Oleh Rutinitas Pemeriksaan Ulang Penilaian Observasional Dan Analisis Kualitatif Dari Inkonsistensi Yang DiidentifikasiEnggar Ardiani TagapNo ratings yet
- Albumin Piggyback Procedure ChecklistDocument3 pagesAlbumin Piggyback Procedure ChecklistAljane VistoNo ratings yet
- Unti 4-6 StudyDocument1 pageUnti 4-6 StudyJennifer Schulze AyscueNo ratings yet
- NCP Normal Spontaneous Delivery Disturbed Sleeping PatternDocument2 pagesNCP Normal Spontaneous Delivery Disturbed Sleeping Patternkaye040389% (28)
- 234-MS1449 - Clinical Fellow FY Equivalent JDDocument21 pages234-MS1449 - Clinical Fellow FY Equivalent JDKeyser SözeNo ratings yet
- Challenges To Implementation of The Pharmaceutical Care Practice in Davao City.Document11 pagesChallenges To Implementation of The Pharmaceutical Care Practice in Davao City.JessieLynMolinaNo ratings yet
- Inhibitorji Protonske ČrpalkeDocument15 pagesInhibitorji Protonske Črpalkeapi-3814389No ratings yet
- Daftar NIE Produk KFTD Jakarta 1Document974 pagesDaftar NIE Produk KFTD Jakarta 1WulanNo ratings yet
- International Travel Health 2010Document264 pagesInternational Travel Health 2010Julyadharma Wangsa DharmaNo ratings yet
- FC Orth (SA) Intermediate Past Papers - 2012 Sept 28-3-2015Document2 pagesFC Orth (SA) Intermediate Past Papers - 2012 Sept 28-3-2015Uhuebor DavidNo ratings yet
- Betadine Irrigation of Breast Implant No UseDocument2 pagesBetadine Irrigation of Breast Implant No Userandomaeiou7273No ratings yet
- Unit 1, Part 4 Clin. PKDocument11 pagesUnit 1, Part 4 Clin. PKshammaNo ratings yet
- Adenovirus: Causes Respiratory Infections in ChildrenDocument6 pagesAdenovirus: Causes Respiratory Infections in ChildrenMuhammad Hifzi IrsadaNo ratings yet
- Combinación de Dosis en Ingredientes FarmaceuticosDocument22 pagesCombinación de Dosis en Ingredientes FarmaceuticosDiana ErasoNo ratings yet
- HEALTH 10 Q1-Mod2 Consumer Health v3Document45 pagesHEALTH 10 Q1-Mod2 Consumer Health v3Macquen Balucio83% (12)
- 210-241 UrinaryDocument34 pages210-241 UrinaryYaj Cruzada100% (1)
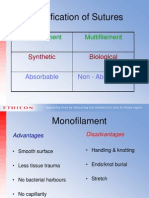
- Classification of Sutures: Monofilament MultifilamentDocument17 pagesClassification of Sutures: Monofilament Multifilamentlina_m354No ratings yet
- Ropivacaine HCL (Naropine)Document23 pagesRopivacaine HCL (Naropine)Dea NandaNo ratings yet
- Medical Certificate For AthletesDocument2 pagesMedical Certificate For AthletesCaitlin PeñeraNo ratings yet
- 24th International Conference On Dental Public Health & Dental HygieneDocument72 pages24th International Conference On Dental Public Health & Dental HygieneAdminNo ratings yet
- EDCDocument7 pagesEDCx7w34TNo ratings yet
- Internship5 12Document7 pagesInternship5 12Jerel MarquezNo ratings yet
- Superstitious BeliefsDocument16 pagesSuperstitious BeliefsLyca EugenioNo ratings yet
- Smart PillDocument2 pagesSmart Pillpappu khanNo ratings yet
- Kamagaju 2013Document26 pagesKamagaju 2013Dessy Erlyani Mugita SariNo ratings yet
- Consensus Guidelines For Delineation of Clinical Target Volume For Intensity-Modulated Pelvic Radiotherapy in Postoperative Treatment of Endometrial and Cervical CancerDocument17 pagesConsensus Guidelines For Delineation of Clinical Target Volume For Intensity-Modulated Pelvic Radiotherapy in Postoperative Treatment of Endometrial and Cervical CancerJaime H. Soto LugoNo ratings yet
- Inspirational StoriesDocument23 pagesInspirational StoriesKalpa R100% (1)
- Lab and Blood Bank Safe DisposalDocument8 pagesLab and Blood Bank Safe DisposalShawqi AlmughniNo ratings yet
- Act 1. PhobiasDocument2 pagesAct 1. PhobiasRoxanne CastilloNo ratings yet
- Antimicrobial Resistance in Campylobacter SPP Isolated FromDocument3 pagesAntimicrobial Resistance in Campylobacter SPP Isolated FromEliud RománNo ratings yet
- SYLABUSDocument6 pagesSYLABUSLarimar Gonzalez LoraNo ratings yet