Professional Documents
Culture Documents
PRS Heart Neck Vessels
Uploaded by
Ira Velle ViosOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PRS Heart Neck Vessels
Uploaded by
Ira Velle ViosCopyright:
Available Formats
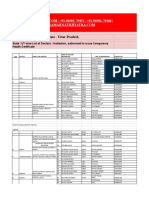
XAVIER UNIVERSITY
PERFORMANCE RATING SCALE
ASSESSING THE HEART & NECK VESSELS
SCALE DESCRIPTION INDICATORS
4 Very Good Student performs behaviors/tasks reflecting the highest level of
performance: consistent, independent, effective
3 Good Student performs behaviors/tasks reflecting mastery of performance with
minimal supervision
2 Fair Student performs behaviors/tasks reflecting development and movement
towards mastery of performance with help or direct supervision in some
aspect
1 Needs Student performs behaviors/tasks reflecting beginning level of
Improvement performance; tasks not done properly majority of the time but demonstrate
understanding of concepts involved with tasks
PROCEDURE 4 3 2 1 REMARKS
1. Perform hand hygiene and put on PPE, if indicated.
2. Iden9fy the pa9ent.
3. Explain the procedure to the client/pa9ent.
Neck Vessels: Inspec?on
4. Observe the jugular venous pulse. Inspect the jugular venous
pulse by standing on the right side of the client. The client should be
in a supine posi9on with the torso elevated 30 to 45 degrees. Make
sure the head and torso are on the same plane. Ask the client to turn
the head slightly to the leJ. Shine a tangen9al light source onto the
neck to increase visualiza9on of pulsa9ons as well as shadows. Next
inspect the suprasternal notch or the area around the clavicles for
pulsa9ons of the internal jugular veins.
5. Evaluate jugular venous pressure. Evaluate jugular venous
pressure by watching for disten9on of the jugular vein. It is normal
for the jugular veins to be visible when the client is supine; to
evaluate jugular vein disten9on, posi9on the client in a supine
posi9on with the head of the bed elevated 30, 45, 60, and 90
degrees. At each increase of the eleva9on, have the client’s head
turned slightly away from the side being evaluated. Using tangen9al
ligh9ng, observe for disten9on, protrusion, or bulging.
Ausculta?on and Palpa?on
6. Auscultate the caro?d arteries. Aus- cultate the caro9d arteries if
the client is middle-aged or older or if you suspect cardiovascular
disease. Place the bell of the stethoscope over the caro9d artery and
ask the client to hold his or her breath for a moment so breath
sounds do not conceal any vascular sounds.
7. Palpate the caro?d arteries. Palpate each caro9d artery
alternately by placing the pads of the index and middle fingers medial
to the sternocleidomastoid muscle on the neck. Note amplitude and
contour of the pulse, elas9city of the artery, and any thrills.
8. Palpate the caro?d arteries individually because bilateral
palpa9on could result in reduced cerebral blood flow.
PROCEDURE 4 3 2 1 REMARKS
Heart (Precordium)
17. Inspect pulsa?ons. With the client in supine posi9on with the
head of the bed elevated between 30 and 45 degrees, stand on the
client’s right side and look for the apical impulse and any abnormal
pulsa9ons.
Palpa?on
18. Palpate the apical impulse. Remain on the client’s right side and
ask the client to remain supine. Use the palmar surfaces of your hand
to palpate the apical impulse in the mitral area (4th or 5th intercostal
space at the midclavicular line). AJer loca9ng the pulse, use one
finger pad for more accurate palpa9on.
19. Palpate for abnormal pulsa?ons. Use your palmar surfaces to
palpate the apex, leJ sternal border, and base.
Ausculta?on
20. Auscultate heart rate and rhythm. Place the diaphragm of the
stethoscope at the apex and listen closely to the rate and rhythm of
the apical impulse.
21. If you detect an irregular rhythm, auscultate for a pulse rate
deficit. This is done by palpa9ng the radial pulse while you auscultate
the apical pulse. Count for a full minute.
22. Auscultate to iden?fy S1 and S2. Auscultate the first heart sound
(S1 or “lub”) and the second heart sound (S2 or “dubb”). Remember
these two sounds make up the cardiac cycle of systole and diastole.
S1 starts systole, and S2 starts diastole. The space, or systolic pause,
be- tween S1 and S2 is of short dura9on (thus S1 and S2 occur very
close together), whereas the space, or diastolic pause, between S2
and the start of another S1 is of longer dura9on.
23. Listen to S1. Use the diaphragm of the stethoscope to best hear
S1
24. Listen to S2. Use the diaphragm of the stethoscope. Ask the client
to breath regularly.
25. Auscultate for extra heart sounds. Use the diaphragm first then
the bell to aus- cultate over the en9re heart area. Note the
characteris9cs (e.g., loca9on, 9ming) of any extra sound heard.
Auscultate during the systolic pause (space heard between S1 and S2).
26. Auscultate during the diastolic pause (space heard between end
of S2 and the next S1).
27. Auscultate for murmurs. A murmur is a swishing sound caused by
turbulent blood flow through the heart valves or great vessels.
Auscultate for murmurs across the en9re heart area. Use the di-
aphragm and the bell of the stethoscope in all areas of ausculta9on
because murmurs have a variety of pitches. Also auscultate with the
client in different posi9ons as described below because some
murmurs occur or subside accord- ing to the client’s posi9on.
28. Auscultate with the client assuming other posi?ons. Ask the
client to assume a leJ lateral posi9on. Use the bell of the
stethoscope and listen at the apex of the heart.
29. Ask the client to sit up, lean forward, and exhale. Use the
diaphragm of the stethoscope and listen over the apex and along the
leJ sternal border
21. Document findings & refer if necessary.
Actual Score/Total Score x 100
A (92 – 100)
A- (84 – 91.99)
B (76 – 83.99)
B- (68 – 75.99)
C (60 – 67.99)
F (< 60 Student’s Signature: _____________________
C.I.’s Signature: _____________________
You might also like
- Respiratory Examination GuideDocument4 pagesRespiratory Examination Guiderhea100% (2)
- Mind and Emotions: A Universal Treatment For Emotional DisordersDocument9 pagesMind and Emotions: A Universal Treatment For Emotional DisordersNew Harbinger Publications100% (7)
- Anesthesiology Resident Manual of Procedures: A Step-by-Step GuideFrom EverandAnesthesiology Resident Manual of Procedures: A Step-by-Step GuideNo ratings yet
- Informative Speech TextDocument2 pagesInformative Speech TextadzwinjNo ratings yet
- Nursing of Clients With Gastrointestinal DisordersDocument228 pagesNursing of Clients With Gastrointestinal DisordersLane Mae Magpatoc Noerrot100% (1)
- The Impact of Computer Based Test On Senior Secondary School StudentsDocument46 pagesThe Impact of Computer Based Test On Senior Secondary School StudentsOrlanshilay100% (18)
- Benson - Hammer 2Document9 pagesBenson - Hammer 2Steven MontgomeryNo ratings yet
- Nebosh: Management of Health and Safety Unit Ig1Document5 pagesNebosh: Management of Health and Safety Unit Ig1TFIBER PROGRESSNo ratings yet
- PRS Thorax Lungs by WeberDocument3 pagesPRS Thorax Lungs by WeberIra Velle ViosNo ratings yet
- Heart and Peripheral VasculatureDocument79 pagesHeart and Peripheral VasculatureEreka LoretoNo ratings yet
- PE CompreDocument5 pagesPE Comprejustme12345mNo ratings yet
- AOP AdultDocument93 pagesAOP AdultKvothe EdemaRuhNo ratings yet
- 16 - Esteban, Shiro S.Document7 pages16 - Esteban, Shiro S.SHIRO ESTEBANNo ratings yet
- Cardiovascular RD ScriptDocument9 pagesCardiovascular RD ScriptMary Joy Anne LucasNo ratings yet
- Heart and Central VesselsDocument3 pagesHeart and Central VesselsSiege DiamondsNo ratings yet
- Cardiovascular Assessment - RDDocument2 pagesCardiovascular Assessment - RDANGELICA CLAIRE BARECUATRONo ratings yet
- Checklist Assessing The Neurological System: S.No Steps YES NODocument9 pagesChecklist Assessing The Neurological System: S.No Steps YES NOpramod kumawat100% (1)
- Procedure Checklist Chapter 19: Assessing The Heart and Vascular SystemDocument2 pagesProcedure Checklist Chapter 19: Assessing The Heart and Vascular SystemjthsNo ratings yet
- PRS Breast Lymphatic SystemDocument2 pagesPRS Breast Lymphatic SystemIra Velle ViosNo ratings yet
- H&P Cardio-Pul-Abd Checklist 2006Document6 pagesH&P Cardio-Pul-Abd Checklist 2006lindseyNo ratings yet
- Pa2 and Pa3 2Document14 pagesPa2 and Pa3 2Roger ViloNo ratings yet
- Mental Status AssessmentDocument16 pagesMental Status Assessmentnokolip100% (1)
- Assessing The Neurological System PDFDocument7 pagesAssessing The Neurological System PDFYousuf Azhar AlamiaNo ratings yet
- PRS Nose Throat SinusesDocument2 pagesPRS Nose Throat SinusesIra Velle ViosNo ratings yet
- HA Procedures Respi Heart and PeripheralDocument10 pagesHA Procedures Respi Heart and Peripheralako at ang exoNo ratings yet
- Perception and Coordination 2Document58 pagesPerception and Coordination 2Jhensczy Hazel Maye AlbaNo ratings yet
- Assessing NeuroDocument7 pagesAssessing NeuroRoldan BalangyaoNo ratings yet
- Assessment of Heart and Neck Vessels - Student's ChecklistDocument3 pagesAssessment of Heart and Neck Vessels - Student's ChecklistRosette Malenab de AsisNo ratings yet
- Assessment of The Head and NeckDocument10 pagesAssessment of The Head and NeckAngela BaldozaNo ratings yet
- Neurological System: (Health Assessment)Document33 pagesNeurological System: (Health Assessment)Kristil ChavezNo ratings yet
- Emergency Treatment of Head InjuriesDocument5 pagesEmergency Treatment of Head InjuriesMasaal VadaiNo ratings yet
- How To Auscultate For Heart Sounds in Adults: Evidence & PracticeDocument3 pagesHow To Auscultate For Heart Sounds in Adults: Evidence & Practiceangela mamauagNo ratings yet
- 2 Neck AssessmentDocument3 pages2 Neck AssessmentAbsalon, J. A. (2201986)No ratings yet
- Head To Toe Physical AssessmentDocument9 pagesHead To Toe Physical Assessmentthe studentNo ratings yet
- Thorax and LungsDocument3 pagesThorax and LungsSiege DiamondsNo ratings yet
- PE ChecklistDocument9 pagesPE Checklist2F PEÑAREDONDO, Achiele, AlcanzoNo ratings yet
- Clin Med Practicals HEENTChest and Lungs and CardioDocument21 pagesClin Med Practicals HEENTChest and Lungs and Cardiohelen joy cuareNo ratings yet
- Health Assessment ChecklistDocument14 pagesHealth Assessment ChecklistLindy JaneNo ratings yet
- Skill: Assessing The Neurological System: LanguageDocument9 pagesSkill: Assessing The Neurological System: LanguageAlmira GamaoNo ratings yet
- Evaluative Tool For NRG 105 Assessing The AbdomenDocument18 pagesEvaluative Tool For NRG 105 Assessing The AbdomenKhim BalcitaNo ratings yet
- Physical Assessment Guide THORAX and LUNGSDocument5 pagesPhysical Assessment Guide THORAX and LUNGSJasmine Kate PatenioNo ratings yet
- Midterm Procedures With RationaleDocument8 pagesMidterm Procedures With RationaleAisha CorobongNo ratings yet
- The Thorax and Lungs Assessment (Autosaved)Document49 pagesThe Thorax and Lungs Assessment (Autosaved)Arlyn Mendenilla100% (4)
- Assessment of The Eyes and The EarsDocument4 pagesAssessment of The Eyes and The EarsAllyssa Mae NacionNo ratings yet
- Neurological Assessment: By, Ms - Keerthana.B Assistant Professor PSG College of NursingDocument54 pagesNeurological Assessment: By, Ms - Keerthana.B Assistant Professor PSG College of NursingKeerthana BNo ratings yet
- Assessing A Peripheral Pulse by AuscultationDocument1 pageAssessing A Peripheral Pulse by AuscultationSIR ONENo ratings yet
- Objective Structured Clinical Examinatio1Document10 pagesObjective Structured Clinical Examinatio1anu aaNo ratings yet
- Head-Toe AssessmentDocument6 pagesHead-Toe AssessmentLamirah ThomasNo ratings yet
- Cardiovascular System (Heart) : 2 - Done Correctly and Completely 1 - Done But Incorrectly or Incompletely 0 - Not DoneDocument3 pagesCardiovascular System (Heart) : 2 - Done Correctly and Completely 1 - Done But Incorrectly or Incompletely 0 - Not DoneVhince Norben Pisco100% (1)
- Clinical SkilllllllllllllllDocument12 pagesClinical SkilllllllllllllllAlmira Putri100% (1)
- Neurological System AssessmentDocument12 pagesNeurological System AssessmentGian Karlo GarridoNo ratings yet
- Physical Assessment Mid-Term Evaluation Fall23Document6 pagesPhysical Assessment Mid-Term Evaluation Fall23Anna DrakeNo ratings yet
- NeuroDocument8 pagesNeurokrezeltayaNo ratings yet
- Cardio ExamDocument8 pagesCardio ExamMark GuirguisNo ratings yet
- Retdem GuideDocument3 pagesRetdem GuideOrtezz RachNo ratings yet
- Assessing The Heart and Central Vessels: Return Demonstration Evaluation Tool ForDocument3 pagesAssessing The Heart and Central Vessels: Return Demonstration Evaluation Tool ForAlexandra DelizoNo ratings yet
- Neurological AssessmentDocument48 pagesNeurological AssessmentSamrat RoyNo ratings yet
- PERFORMANCE-EVALUATION-CHECKLIST-HEADDocument4 pagesPERFORMANCE-EVALUATION-CHECKLIST-HEADHaydi Pineda MedinaNo ratings yet
- Cardiopulmonary Resuscitation (C.P.R) With AED: Procedure Done Not Done Student's Score Notes Correct IncorrectDocument3 pagesCardiopulmonary Resuscitation (C.P.R) With AED: Procedure Done Not Done Student's Score Notes Correct IncorrectBarrak AldosaryNo ratings yet
- LEARNING GUIDE OF PEDIATRIC EMERGENCY-1.revisiDocument4 pagesLEARNING GUIDE OF PEDIATRIC EMERGENCY-1.revisiPutri NoviyantiNo ratings yet
- Assessing Pulse RateDocument4 pagesAssessing Pulse RateJan Jamison ZuluetaNo ratings yet
- Basic LifeDocument33 pagesBasic LifetmschppmNo ratings yet
- Manguiat, Reyes Head and Neck AssessmentDocument4 pagesManguiat, Reyes Head and Neck AssessmentCiara Manguiat100% (1)
- Skill: Assessing The Heart and Central VesselsDocument2 pagesSkill: Assessing The Heart and Central VesselsDr. Abiola KomolafeNo ratings yet
- Apex BeatDocument22 pagesApex BeatdanielNo ratings yet
- Active Rom Exercise - ViosDocument6 pagesActive Rom Exercise - ViosIra Velle ViosNo ratings yet
- PRS EAR INSTILLATION - ViosDocument4 pagesPRS EAR INSTILLATION - ViosIra Velle ViosNo ratings yet
- PRS Nose Throat SinusesDocument2 pagesPRS Nose Throat SinusesIra Velle ViosNo ratings yet
- PRS - Oral Care For Unresponsive Client - ViosDocument2 pagesPRS - Oral Care For Unresponsive Client - ViosIra Velle ViosNo ratings yet
- PRS - Oral Care For Unresponsive Client - ViosDocument2 pagesPRS - Oral Care For Unresponsive Client - ViosIra Velle ViosNo ratings yet
- PRS - Eyes Nose Ear Care - ViosDocument5 pagesPRS - Eyes Nose Ear Care - ViosIra Velle Vios100% (1)
- Nursing Interview Guide - HA - VIOSDocument9 pagesNursing Interview Guide - HA - VIOSIra Velle ViosNo ratings yet
- Leggings and DrapingsDocument1 pageLeggings and DrapingsIra Velle ViosNo ratings yet
- NCM 106 - DRUG and IVF CALCULATIONS - VIOSDocument3 pagesNCM 106 - DRUG and IVF CALCULATIONS - VIOSIra Velle ViosNo ratings yet
- Assignment On Antibiotics - ViosDocument8 pagesAssignment On Antibiotics - ViosIra Velle ViosNo ratings yet
- NCM 105 NC - Nutrition and Diet Therapy - Activity 2-Heat Me Out - ViosDocument1 pageNCM 105 NC - Nutrition and Diet Therapy - Activity 2-Heat Me Out - ViosIra Velle ViosNo ratings yet
- ANS Discussion-Topics VIOSDocument7 pagesANS Discussion-Topics VIOSIra Velle ViosNo ratings yet
- NCM 105 - Calculating Diet Meal Planning Activity - VIOSDocument5 pagesNCM 105 - Calculating Diet Meal Planning Activity - VIOSIra Velle ViosNo ratings yet
- Artwork ViosDocument1 pageArtwork ViosIra Velle ViosNo ratings yet
- Jas08 4Document3 pagesJas08 4krishna saiNo ratings yet
- Scholarship ApplicationDocument5 pagesScholarship ApplicationANDREASNo ratings yet
- Tork Catalogue UkiDocument102 pagesTork Catalogue UkiBirdsNo ratings yet
- Survey Method Statement For Construction Under PASSDocument28 pagesSurvey Method Statement For Construction Under PASSMustakim AnsaryNo ratings yet
- Anti-Aging Checklist - Cheat SheetDocument5 pagesAnti-Aging Checklist - Cheat SheetdrissNo ratings yet
- API BGD DS2 en Excel v2 4685979Document339 pagesAPI BGD DS2 en Excel v2 4685979Areesha KamranNo ratings yet
- A Visit To The Doctor - EnfermeriaDocument4 pagesA Visit To The Doctor - EnfermeriaSILVIA MARIELA LLAMOCA LIMACHENo ratings yet
- Differences in Tear Secretion Before and After Phacoemulsification Surgery Using Schirmer I TestsDocument4 pagesDifferences in Tear Secretion Before and After Phacoemulsification Surgery Using Schirmer I TestsKris AdinataNo ratings yet
- Al-Okshi Et Al 2019Document9 pagesAl-Okshi Et Al 2019Ayman AlOkshiNo ratings yet
- NDCT Rules, 2019Document118 pagesNDCT Rules, 2019ShwetaNo ratings yet
- Diarrhea New Edited 2Document82 pagesDiarrhea New Edited 2bharathNo ratings yet
- 5-Minute Exercises To Make Your Belly Fat Melt Like SnowDocument6 pages5-Minute Exercises To Make Your Belly Fat Melt Like Snowmelbe5jane5quiamcoNo ratings yet
- Uttar PradeshDocument7 pagesUttar PradeshPawani Gupta100% (1)
- Fundamentals of Nursing Transes 3Document4 pagesFundamentals of Nursing Transes 3Louise TorresNo ratings yet
- Colisage ProduitsDocument6 pagesColisage ProduitsBerriche MohamedNo ratings yet
- Medical Surgical Ward Carry Out Order GroupDocument50 pagesMedical Surgical Ward Carry Out Order GroupKheeney AlvarezNo ratings yet
- The Problem and Background of The StudyDocument6 pagesThe Problem and Background of The StudyAileen ElegadoNo ratings yet
- Oxymixer High Flow Without Monitor - BrochureDocument6 pagesOxymixer High Flow Without Monitor - BrochureochaNo ratings yet
- Multidimensional PovertyDocument2 pagesMultidimensional PovertyJohn ClarenceNo ratings yet
- PCR My - Wan Nur Afiyah - 8mayDocument1 pagePCR My - Wan Nur Afiyah - 8mayEvie SuriNo ratings yet
- J Clinic Periodontology - 2018 - Caton - A New Classification Scheme For Periodontal and Peri Implant Diseases andDocument8 pagesJ Clinic Periodontology - 2018 - Caton - A New Classification Scheme For Periodontal and Peri Implant Diseases andVõ Thị Mỹ NhungNo ratings yet
- Name: Date: - Year/Section:: Task 1: PAR-Q and YOU Questionnaire (Prior To The Activity Test)Document3 pagesName: Date: - Year/Section:: Task 1: PAR-Q and YOU Questionnaire (Prior To The Activity Test)Angela Louise Smiths0% (1)
- Shaukat Khanum Memorial Cancer Hospital & Research Centre: Coagulation ProfileDocument1 pageShaukat Khanum Memorial Cancer Hospital & Research Centre: Coagulation ProfileSyed Muhammad Zubair TariqNo ratings yet
- Definition of Terms: Service RadiusDocument11 pagesDefinition of Terms: Service RadiusSamuel ValentineNo ratings yet