Professional Documents
Culture Documents
Farmacocinetica Metformina
Farmacocinetica Metformina
Uploaded by
Norma AlvarezOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Farmacocinetica Metformina
Farmacocinetica Metformina
Uploaded by
Norma AlvarezCopyright:
Available Formats
DOI: 10.1111/j.1464-5491.2005.01769.
Effect of pregnancy on the pharmacokinetics of
Pregnancy
Short Communication
report
Oxford,
Diabetic
DME
Blackwell
0742-3071
22 UK and metformin
Medicine
Publishing, Ltd.pharmacokinetics •R. C. E. Hughes et al.
2005
metformin
R. C. E. Hughes*†, S. J. Gardiner*‡, E. J. Begg*‡ and M. Zhang‡
Abstract
*Department of Clinical Pharmacology, Aims To determine the effects of pregnancy on metformin pharmacokinetics.
Christchurch Hospital, Christchurch, †Department
of Medicine, National Women’s Hospital, Auckland Methods Seven women with Type 2 diabetes mellitus taking metformin throughout
and ‡Department of Medicine, Christchurch School pregnancy were studied on two occasions, once at 28–36 weeks gestation and once
of Medicine, Christchurch, New Zealand
at least 8 weeks postpartum. Serum metformin concentrations were determined
Accepted 4 May 2005 across a dosing interval using high-performance liquid chromatography.
The areas under the serum concentration-time curve from 0 to 4 h post-dose
(AUC0 − 4) and 0 to 8 h post-dose (AUC0 − 8) where possible, were compared in
the pregnant and non-pregnant state.
Results Metformin concentrations were lower in pregnancy in six subjects,
with a mean (95% CI) AUC0 − 4 that was 69% (53.6, 84.8) of the postpartum
value. The AUC0 − 4 of one subject was higher in pregnancy at 142% of the
postpartum value. Overall, the mean (95% CI) AUC0 − 4 during pregnancy for all
seven subjects was 80% (51.3, 107.8) of the postpartum value (P = 0.053,
two-tailed t-test; P = 0.027, one-tailed t-test).
Conclusion These results are consistent with our hypothesis that the clearance
of metformin increases in pregnancy as a result of enhanced renal elimination.
A larger study is required to establish whether metformin dose adjustments are
required in late pregnancy to maintain therapeutic effect.
Diabet. Med. 23, 323–326 (2006)
Keywords metformin, pharmacokinetics, diabetes mellitus, pregnancy
Abbreviations AUC, area under the concentration time curve; GFR, glomerular
filtration rate; Type 2 DM, Type 2 diabetes mellitus
Metformin is a small basic compound (molecular weight
Introduction 129 Da) that is ionized at physiological pH. Oral availability
Metformin improves insulin sensitivity and glucose metabolism (50 – 60%) is inversely related to dose ingested, suggesting
in insulin-resistant states [1,2] such as Type 2 diabetes (Type 2 saturable absorption [8]. The extent of absorption is influenced
DM) and polycystic ovary syndrome. Increasingly, women are by food (which decreases metformin concentrations by ∼20%
conceiving on metformin with some continuing it throughout compared with the fasting state [8,9]) and gastrointestinal transit
pregnancy [3–6]. In other cases, metformin is initiated in time (propantheline slows gut motility and increases concentra-
pregnancy as an adjunct or alternative to insulin. While data tions by ∼20% [10]). Metformin has negligible plasma protein
suggest metformin is not overtly teratogenic [7], little is known binding and a moderately large apparent volume of distribu-
about the effect of pregnancy on metformin pharmacokinetics. tion of 63–276 l. It is eliminated unchanged in urine, the renal
clearance (27–31 l / h) exceeding glomerular filtration rate (GFR,
∼5.4 l/ h) indicating active tubular secretion [8] probably via
Correspondence to: Dr Ruth Hughes, Department of Clinical Pharmacology,
Christchurch Hospital, Private Bag 4710, Christchurch, New Zealand. organic cation transporters such as OCT2 [11,12]. The physi-
E-mail: ruth.hughes@xtra.co.nz ological changes of pregnancy, such as reduced gastrointestinal
© 2006 Diabetes UK. Diabetic Medicine, 23, 323–326 323
324 Pregnancy and metformin pharmacokinetics • R. C. E. Hughes et al.
motility [13,14] and the 40 –50% increase in GFR by the second The samples were analysed for metformin in triplicate using
trimester [15,16], could significantly alter metformin high-performance liquid chromatography [18] and the mean
pharmacokinetics. This rise in GFR may enhance the renal concentration used in subsequent analyses. The standard curve
clearance of metformin as has been reported for some β-lactam was linear (r 2 > 0.99) over the range 20 – 4000 µg / l and intra-
antibiotics [17]. and inter-day coefficients of variation were less than 9% at the
concentrations of 62.5, 250, 1000 and 4000 µg / l. The limit of
The aim of this study was to determine the effects of
detection (signal/noise 3 : 1) was 20 µg / l.
pregnancy on metformin pharmacokinetics by comparing the
The AUC from 0 to 4 h (AUC0 − 4) and 0 to 8 h (AUC0 − 8) were
area under the concentration time curves (AUC) for metformin determined using GraphPad Prism version 4.00 for Windows
in pregnancy and the non-pregnant state. To our knowledge [GraphPad Software, San Diego, CA, USA (www.graphpad.
this is the first study to describe the effect of pregnancy on the com)]. Student’s t-test (paired) was performed for comparison
pharmacokinetics of metformin. of the AUC0 – 4 in pregnancy and postpartum. Use of the one-
tailed test was justified on the basis of our hypothesis that the
clearance of metformin would increase in pregnancy as a result
Patients and methods of increased GFR. The level of significance was set at P < 0.05.
Subjects were recruited from the antenatal clinic at National
Womens’ Hospital, a tertiary referral centre serving the
multiethnic community of central Auckland, New Zealand.
Results
Women eligible for inclusion had: Type 2 DM treated with Nine subjects were enrolled during the time period available to
metformin prenatally; decided to continue metformin dur- the project. Two subjects were subsequently excluded, subject
ing pregnancy independently of this study; a pre-pregnancy or 1 had postpartum metformin intolerance and subject 6 became
early pregnancy creatinine clearance ≥ 90 ml /min (using the pregnant a second time before completion of the study. The
Cockcroft and Gault equation); and were not taking any
remaining seven subjects ranged in age from 31 to 41 years and
medicines known to interact pharmacokinetically with
were from diverse ethnic backgrounds (four Polynesian, one
metformin. Approval was obtained from the Auckland ethics
committee and informed written consent was obtained from
Caucasian, one Asian and one Indian). Subjects were studied at
each participant. a median (range) of 34 weeks gestation (29 – 36) and at 10 weeks
Subjects were studied in an inpatient ward at the National postpartum (8 –11). The median (range) pregnancy and
Womens’ Hospital or in their own homes. Each subject was postpartum weights were 108.4 kg (88–118.5) and 99 kg (74 –
studied on two occasions, once at 28–36 weeks gestation (the 104.6), respectively. No formal measure of GFR was under-
time of maximal pregnancy-related increase in GFR), and once taken and the Cockcroft and Gault equation has not been
in the postpartum period at least 8 weeks after delivery (when validated in pregnancy. However, mean (SEM) serum creatinine
GFR is expected to have returned to baseline). On the study concentrations were lower in pregnancy 0.05 (0.003) mmol/ l
days, the subjects ingested their usual dose of metformin with vs. 0.07 (0.002) mmol / l postpartum (P = 0.0015, two-tailed
meals (low glycaemic, low fat) prepared by the hospital or
t-test). Concurrent drug therapy over the study period included
homemade. The exact time of metformin administration was
insulin, sulphonylureas, aspirin, vitamins/minerals, fluoxetine,
recorded and serial blood samples (5 ml) were collected into
plain tubes via an indwelling venous cannula. Blood samples
oxprenolol and depot progesterone.
were taken prior to the first daily dose (at 0 h) and then at 1, 2, Valid data points for a full AUC0−8 could not be collected in
4, 8 and 12 h post-dose if these time points occurred within the all subjects therefore, the AUC0−4 was calculated for seven
dose interval. Blood samples were centrifuged immediately at subjects and AUC0−8 for the four subjects with sufficient data
2000 g for 10 min and the serum stored at −20°C until analysis. points (Table 1). Concentration-time profiles for two subjects
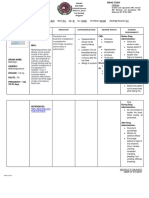
Table 1 Dosing data and AUC for metformin during pregnancy (28–36 weeks gestation) and postpartum
Creatinine Ratio of AUC0 − 4
clearance† AUC0 − 4 (mg / l)h AUC0 − 8 (mg / l)h to AUC0 − 8
Subject Metformin* dose Non-pregnant Pregnant Postpartum Pregnant Postpartum Pregnant Postpartum
2 1000 mg twice daily 90 3.962 2.799 6.524 4.579 1.65 1.70
3 850 mg twice daily 93 3.502 5.838 — — — —
4 850 mg thrice daily 92 3.654 5.247 — — — —
5 500 mg twice daily 100 3.025 3.865 4.821 6.295 1.59 1.63
7 500 mg twice daily 94 3.595 3.833 — — — —
8 1000 mg twice daily 100 2.978 5.585 5.028 10.18 1.69 2.02
9 850 mg twice daily 114 3.162 5.261 5.064 8.469 1.60 1.61
*Metformin (Metomin, Pacific Pharmaceuticals, Christchurch, New Zealand) was a plain release formulation.
†Calculated in ml/min using the Cockcroft and Gault equation (note this may underestimate renal function in the Polynesian volunteers (subjects 2–4
and 7).
© 2006 Diabetes UK. Diabetic Medicine, 23, 323–326
Short report 325
Figure 1 Steady-state serum concentration-time curves for subjects 4 and 5 who were on a metformin dosing regimen of 850 mg thrice daily and 500 mg
twice daily, respectively. Closed squares represent the pregnant state and closed triangles represent the non-pregnant state.
are shown in Fig. 1. With the exception of subject 2, all sub- undergone little research. Variable long-term compliance with
jects had a smaller AUC0 − 4 during pregnancy compared with metformin may be responsible for the incongruent results of
the postpartum AUC0 − 4. In these six subjects, the AUC0 − 4 was subject 2 who, after completing the study, was admitted with
a mean of 69% (95% CI 53.6, 84.8) of the postpartum value, collapse and poor glycaemic control. It is possible therefore
while that of subject 2 was 142%. Overall, including data from that the serum concentrations of metformin were not at a
all seven subjects, the AUC0−4 during pregnancy was a mean steady state for the second part of the study and thus a rise in
(95% CI) of 80% (51.3, 107.8) of the postpartum value the AUC was not seen as predicted. Alternatively, the disparate
(P = 0.053, two-tailed t-test; P = 0.027, one-tailed t-test) (the result may be secondary to factors such as genetic variation in
Mann–Whitney U-test gave identical results to the paired t-test). OCT2 and in the renal clearance of metformin [19], or variable
The AUC0−8 was a mean (95% CI) of 1.63-fold (1.56, 1.70) and food ingestion on study days (although food composition may
1.74-fold (1.54, 1.84) higher than the corresponding AUC0−4 not significantly influence absorption [20]).
in pregnancy and postpartum, respectively. There was excellent The observed decrease in the AUC of metformin in preg-
correlation (r 2 = 0.97) between the AUC0 − 4 and AUC0 − 8 in sub- nancy may have clinical implications with respect to dosing.
jects where both were calculated suggesting that the AUC0 − 4 is The renal clearance of metformin is expected to peak at the
a valid index of relative interdose metformin exposure. time of maximal pregnancy induced insulin resistance. From
Observed peak serum concentrations were at 1–2 h post- a pharmacokinetic point of view, this may necessitate a ≥ 20%
dose in all subjects during pregnancy and postpartum. Peak increase in metformin dose to maintain a given therapeutic
serum concentrations in pregnancy were 81.0% (mean; 95% effect which may ultimately delay the need to commence or
CI 47.3, 114.8%) of the postpartum value (P = 0.077, two- increase insulin in some patients. A larger study incorporating
tailed) (data not shown). measures to assess patient compliance is required to confirm
our findings before specific recommendations can be made on
metformin dosing in pregnancy.
Discussion
In all but subject 2, a marked decrease in the AUC 0 − 4 for
metformin was seen in pregnancy, the magnitude of which was
Competing interests
in keeping with our hypothesis that the renal clearance of met- None declared.
formin would increase by 40–50% secondary to the pregnancy
associated increase in GFR. This is supported by the observed
decrease in serum creatinine concentrations in all subjects. References
Enhanced active tubular secretion of metformin during preg- 1 Kirpichnikov D, McFarlane SI, Sowers JR. Metformin: an update.
nancy may also be a contributing factor, although this has Ann Intern Med 2002; 137: 25–33.
© 2006 Diabetes UK. Diabetic Medicine, 23, 323–326
326 Pregnancy and metformin pharmacokinetics • R. C. E. Hughes et al.
2 Hundal RS, Inzucchi SE. Metformin: new understandings, new uses. 11 Dressler MJ, Xiao G, Leabman MK, Gray AT, Giacomini KM.
Drugs 2003; 63: 1879–1894. Interactions of n-tetraalkylammonium compounds and biguanides
3 Glueck CJ, Goldenberg N, Pranikoff J, Loftspring M, Sieve L, with a human renal organic cation transporter (hoct2). Pharm Res
Wang P. Height, weight, and motor-social development during the 2002; 19: 1244–1247.
first 18 months of life in 126 infants born to 109 mothers with poly- 12 Wang DS, Jonker JW, Kato Y, Kusuhara H, Schinkel AH, Sugiyama Y.
cystic ovarian syndrome who conceived on and continued metformin Involvement of organic cation transporter 1 in hepatic and intestinal
through pregnancy. Hum Reprod 2004; 19: 1323–1330. distribution of metformin. J Pharmacol Exp Ther 2002; 302: 510–
4 Glueck CJ, Wang P, Kobayashi S, Phillips H, Sieve-Smith L. 515.
Metformin therapy throughout pregnancy reduces the development 13 Parry E, Shields R, Turnbull AC. Transit time in the small intestine in
of gestational diabetes in women with polycystic ovary syndrome. pregnancy. J Obstet Gynaecol Br Commonw 1970; 77: 900–901.
Fertil Steril 2002; 77: 520–525. 14 Davison JS, Davison MC, Hay DM. Gastric emptying time in late
5 Glueck CJ, Goldenberg N, Wang P, Loftspring M, Sherman A. pregnancy and labour. J Obstet Gynaecol Br Commonw 1970; 77:
Metformin during pregnancy reduces insulin, insulin resistance, 37–41.
insulin secretion, weight, testosterone and development of gestational 15 Dunlop W, Davison JM. Renal haemodynamics and tubular function
diabetes: Prospective longitudinal assessment of women with in human pregnancy. Baillieres Clin Obstet Gynaecol 1987; 1: 769–
polycystic ovary syndrome from preconception throughout pregnancy. 787.
Hum Reprod 2004; 19: 510–521. 16 Davison JM, Dunlop W. Renal hemodynamics and tubular function
6 Coetzee EJ, Jackson WP. Metformin in management of pregnant in normal human pregnancy. Kidney Int 1980; 18: 152–161.
insulin-independent diabetics. Diabetologia 1979; 16: 241–245. 17 Heikkila A, Erkkola R. Review of beta-lactam antibiotics in preg-
7 Gutzin SJ, Kozer E, Magee LA, Feig DS, Koren G. The safety of nancy. The need for adjustment of dosage schedules. Clin Pharma-
oral hypoglycemic agents in the first trimester of pregnancy: a meta- cokinet 1994; 27: 49–62.
analysis. Can J Clin Pharmacol 2003; 10: 179–183. 18 Zhang M, Moore GA, Lever M, Gardiner SJ, Kirkpatrick CMJ, Begg
8 Scheen AJ. Clinical pharmacokinetics of metformin. Clin Pharma- EJ. A rapid and simple hplc assay for the determination of metformin
cokinet 1996; 30: 359–371. in human plasma and breast milk. J Chromatogr B Analyt Technol
9 Sambol NC, Brookes LG, Chiang J, Goodman AM, Lin ET, Liu CY Biomed Life Sci 2002; 766: 175–179.
et al. Food intake and dosage level, but not tablet vs solution dosage 19 Leabman MK, Giacomini KM. Estimating the contribution of genes
form, affect the absorption of metformin hcl in man. Br J Clin and environment to variation in renal drug clearance. Pharmacoge-
Pharmacol 1996; 42: 510–512. netics 2003; 13: 581–584.
10 Marathe PH, Wen Y, Norton J, Greene DS, Barbhaiya RH, Wilding 20 Saffar F, Aiache JM, Andre P. Influence of food on the disposition of
IR. Effect of altered gastric emptying and gastrointestinal motility on the antidiabetic drug metformin in diabetic patients at steady-state.
metformin absorption. Br J Clin Pharmacol 2000; 50: 325–332. Methods Find Exp Clin Pharmacol 1995; 17: 483–487.
© 2006 Diabetes UK. Diabetic Medicine, 23, 323–326
You might also like
- Biohack by Parth Goyal Class 12 2023 by Education Learn AcademyDocument151 pagesBiohack by Parth Goyal Class 12 2023 by Education Learn AcademyHasmukh Ravat90% (82)
- Solution Manual For Understanding Human Sexuality 14th Edition Janet Hydejohn DelamaterDocument37 pagesSolution Manual For Understanding Human Sexuality 14th Edition Janet Hydejohn DelamaterMarieHughesebgjp100% (82)
- Elementary Science Grade 5 Lesson PlanDocument348 pagesElementary Science Grade 5 Lesson PlanSheila Roxas86% (50)
- Obstetrics and Gynaecology History Taking TemplateDocument4 pagesObstetrics and Gynaecology History Taking TemplateMaruti100% (3)
- Menorrhagia History Taking Notes 1Document7 pagesMenorrhagia History Taking Notes 1Slh SfiNo ratings yet
- Pathophysiology of Ectopic PregnancyDocument3 pagesPathophysiology of Ectopic PregnancyJulienne Sanchez-Salazar100% (1)
- 17Document7 pages17silvanaNo ratings yet
- Preclinical Evaluation of Pharmacokinetic-Pharmacodynamic Rationale For Oral CR Metforminnext Termprevious Termformulationnext TermDocument9 pagesPreclinical Evaluation of Pharmacokinetic-Pharmacodynamic Rationale For Oral CR Metforminnext Termprevious Termformulationnext TermPv KhoiNo ratings yet
- Metformin in The Management of Diabetes During Pregnancy and LactationDocument21 pagesMetformin in The Management of Diabetes During Pregnancy and LactationShaiful BachriNo ratings yet
- Review ArticleDocument14 pagesReview ArticlemelisaberlianNo ratings yet
- I J R P S: Metformin Compared To Insulin For The Management of Gestational DiabeticDocument5 pagesI J R P S: Metformin Compared To Insulin For The Management of Gestational DiabeticAbed AlhaleemNo ratings yet
- Evaluation of Label Drug in The Treatment Polycystic Ovary SyndromeDocument4 pagesEvaluation of Label Drug in The Treatment Polycystic Ovary SyndromeYeni LagaNo ratings yet
- Tugas Individu FarmakoekonomiDocument9 pagesTugas Individu FarmakoekonomiMarisa NurlitaNo ratings yet
- Bioequivalence of Ertugliflozin - Metformin Fixed-Dose Combination Tablets and Coadministration of Respective Strengths of Individual ComponentsDocument12 pagesBioequivalence of Ertugliflozin - Metformin Fixed-Dose Combination Tablets and Coadministration of Respective Strengths of Individual ComponentsAdelNo ratings yet
- Trivedi. Post Laparascopic Treatment of Endometriosis With DYDDocument5 pagesTrivedi. Post Laparascopic Treatment of Endometriosis With DYDRuth RachmawatyNo ratings yet
- Ectopic PregnancyDocument7 pagesEctopic PregnancyAlex BelinschiiNo ratings yet
- The Following Abstracts of Articles From Leading Journals Have Been Selected On The Basis of Their Importance To The Practice of Obstetrics and GynecologyDocument3 pagesThe Following Abstracts of Articles From Leading Journals Have Been Selected On The Basis of Their Importance To The Practice of Obstetrics and GynecologythereberryNo ratings yet
- ArtículoDocument8 pagesArtículo014100700jNo ratings yet
- Pharmaco DynamicsDocument2 pagesPharmaco DynamicsSunil DeshpandeNo ratings yet
- Jurnal PCOSDocument11 pagesJurnal PCOSCinthya ayu MerithaNo ratings yet
- Comparative Pharmacokinetic Study Between Metformin Alone and Combined With Orlistat in Healthy Mexican VolunteersDocument7 pagesComparative Pharmacokinetic Study Between Metformin Alone and Combined With Orlistat in Healthy Mexican Volunteersintan kusumaningtyasNo ratings yet
- Comparison Between Vaginal and Sublingual Misoprostol 50 UgDocument6 pagesComparison Between Vaginal and Sublingual Misoprostol 50 Ugidris setyadi lubisNo ratings yet
- Etg Gonzales Chamorro Diego PDFDocument4 pagesEtg Gonzales Chamorro Diego PDFDiego GonzalesNo ratings yet
- Low-Dose Mifepristone in Treatment of Uterine Leiomyoma: A Randomised Double-Blind Placebo-Controlled Clinical TrialDocument8 pagesLow-Dose Mifepristone in Treatment of Uterine Leiomyoma: A Randomised Double-Blind Placebo-Controlled Clinical TrialAlrick GonzalezNo ratings yet
- Anatomical and Physiological Alterations of PregnancyDocument15 pagesAnatomical and Physiological Alterations of PregnancyMateo BermeoNo ratings yet
- Embarazo EctópicoDocument7 pagesEmbarazo EctópicomariNo ratings yet
- METFORMINDocument11 pagesMETFORMINsalsabila JacobNo ratings yet
- Therapeutic Drug Monitoring Part 2 PDFDocument23 pagesTherapeutic Drug Monitoring Part 2 PDFChandra AvicennaNo ratings yet
- Metformin Vs Insulin in Gestational DiabetesDocument17 pagesMetformin Vs Insulin in Gestational Diabetesmiguel alejandro zapata olayaNo ratings yet
- Acta Obstet Gynecol Scand - 2015 - Abu Hashim - Combined Metformin Clomiphene in Clomiphene Resistant Polycystic OvaryDocument10 pagesActa Obstet Gynecol Scand - 2015 - Abu Hashim - Combined Metformin Clomiphene in Clomiphene Resistant Polycystic Ovarymed2dianavNo ratings yet
- s10549 005 5701 XDocument11 pagess10549 005 5701 XJIAQI MagicNo ratings yet
- JurnalDocument5 pagesJurnalkadekNo ratings yet
- Jurding AulDocument5 pagesJurding AulRizky AuliaNo ratings yet
- 2049 9752 4 1Document5 pages2049 9752 4 1Nasrull BinHzNo ratings yet
- Capecitabine: A Review: Christine M. Walko, Pharmd, and Celeste Lindley, PharmdDocument22 pagesCapecitabine: A Review: Christine M. Walko, Pharmd, and Celeste Lindley, PharmdOsmond BobbyNo ratings yet
- Feig 2017Document13 pagesFeig 2017Lembaga Pendidikan dan PelayananNo ratings yet
- Promethazine Compared WithDocument51 pagesPromethazine Compared WithsprimalNo ratings yet
- Predictive Factors of Methotrexate Treatment Success in Ectopic Pregnancy A Single Center Tertiary StudyDocument5 pagesPredictive Factors of Methotrexate Treatment Success in Ectopic Pregnancy A Single Center Tertiary StudyRizka AdiNo ratings yet
- Effect of Fish OilDocument9 pagesEffect of Fish Oilmuniraj patelNo ratings yet
- Metformin Versus Acarbose Therapy in Patients With Polycystic Ovary Syndrome (PCOS) : A Prospective Randomised Double-Blind StudyDocument9 pagesMetformin Versus Acarbose Therapy in Patients With Polycystic Ovary Syndrome (PCOS) : A Prospective Randomised Double-Blind StudyIam MaryamNo ratings yet
- International Journal of Gynecology and ObstetricsDocument5 pagesInternational Journal of Gynecology and ObstetricsFake_Me_No ratings yet
- Metformina Preeclampsia Temprana, Prolongacion de FPPDocument10 pagesMetformina Preeclampsia Temprana, Prolongacion de FPPGaudy Francheska Alvarado GutierrezNo ratings yet
- Metformin Monotherapy in Lean Women With Polycystic Ovary SyndromeDocument5 pagesMetformin Monotherapy in Lean Women With Polycystic Ovary SyndromeQuratul AyunNo ratings yet
- 256 FullDocument7 pages256 FullAngga M RahmanNo ratings yet
- 4784 17639 1 PB PDFDocument6 pages4784 17639 1 PB PDFbaidyanath kumarNo ratings yet
- Efficacy and Safety of Setmelanotide, An MC4R AgonDocument11 pagesEfficacy and Safety of Setmelanotide, An MC4R Agongipokratik5No ratings yet
- Ppoly Olycystic O Cystic Ovary Syndrome: Metformin in Women Vary Syndrome: Metformin in Women Not Planning Pregnancy Not Planning PregnancyDocument20 pagesPpoly Olycystic O Cystic Ovary Syndrome: Metformin in Women Vary Syndrome: Metformin in Women Not Planning Pregnancy Not Planning PregnancyMixkscel SokopNo ratings yet
- 10 1016@j Ajog 2016 03 013Document7 pages10 1016@j Ajog 2016 03 013Fernando CruzNo ratings yet
- Wu 2022Document12 pagesWu 2022Walaa YousefNo ratings yet
- 2 SOP Pengadaan Sediaan Farmasi Dan Alkes DLM ApotikDocument8 pages2 SOP Pengadaan Sediaan Farmasi Dan Alkes DLM Apotikibnu an nafisNo ratings yet
- Biowaiver ApproachDocument11 pagesBiowaiver Approachmarco hernandezNo ratings yet
- January 2003: East African Medical Journal 51Document5 pagesJanuary 2003: East African Medical Journal 51simoncktNo ratings yet
- 2028-Article Text-9832-3-10-20131105Document3 pages2028-Article Text-9832-3-10-20131105HMC ProcurementNo ratings yet
- 07 Dosage RegimenDocument44 pages07 Dosage Regimenzetttttttttt100% (3)
- A Randomised Clinical Trial Comparing Myoinositol and Metformin in PCOSDocument7 pagesA Randomised Clinical Trial Comparing Myoinositol and Metformin in PCOSAtika NajlaNo ratings yet
- Zaharah KurniawatiDocument6 pagesZaharah KurniawatiIhdina Hanifa Hasanal IbrahimNo ratings yet
- Dosing Interval Between Mifepristone and Misoprostol in Second and Third Trimester TerminationDocument5 pagesDosing Interval Between Mifepristone and Misoprostol in Second and Third Trimester TerminationWILMER HUANGANo ratings yet
- LailaDocument10 pagesLailatettyzoebaedah4321No ratings yet
- TCI Propofol ClearanceDocument9 pagesTCI Propofol ClearanceJoanna GlezNo ratings yet
- Review Metformin in Cancer: Translational ChallengesDocument13 pagesReview Metformin in Cancer: Translational ChallengesliMvuxNo ratings yet
- Ni Hms 58309Document5 pagesNi Hms 58309zuhrahgiatamahNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument3 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyFaradibha Maysarah HasibuanNo ratings yet
- 2.5 Implementation Considerations: Eligible Children Aged 6 YearsDocument45 pages2.5 Implementation Considerations: Eligible Children Aged 6 YearsSibaraniNo ratings yet
- Metformin and Digestive DisordersDocument7 pagesMetformin and Digestive Disorders-Yohanes Firmansyah-No ratings yet
- Complementary and Alternative Medical Lab Testing Part 10: ObstetricsFrom EverandComplementary and Alternative Medical Lab Testing Part 10: ObstetricsNo ratings yet
- Clinical Pharmacology During PregnancyFrom EverandClinical Pharmacology During PregnancyDonald MattisonNo ratings yet
- Adult Office Hours Telehealth Triage Guidelines (Protocols) : Schmitt-Thompson Clinical ContentDocument31 pagesAdult Office Hours Telehealth Triage Guidelines (Protocols) : Schmitt-Thompson Clinical ContentMassimo RiserboNo ratings yet
- From Death To Life Ethical IsDocument7 pagesFrom Death To Life Ethical IsAfiatur RohimahNo ratings yet
- Step-by-Step Approach For Nerve-Sparing Reduction ClitoroplastyDocument1 pageStep-by-Step Approach For Nerve-Sparing Reduction ClitoroplastyKevin YonathanNo ratings yet
- Case Study For Uterine-CancerDocument9 pagesCase Study For Uterine-CancerGabbii CincoNo ratings yet
- Natural Law Case AnalysisDocument1 pageNatural Law Case AnalysisSheila Mae AsuelaNo ratings yet
- Acute Abdomen During Pregnancy 2014 PDFDocument584 pagesAcute Abdomen During Pregnancy 2014 PDFlula gestiana taufan100% (1)
- Year 5 Puberty Changes Lesson PlanDocument4 pagesYear 5 Puberty Changes Lesson PlanArlan DayligNo ratings yet
- Xhand - UrgentDocument1 pageXhand - UrgentMaimoona AimanNo ratings yet
- OFFER LETTER April Mae Lidres Aguilar APP8976078242645304 VERSION 1Document5 pagesOFFER LETTER April Mae Lidres Aguilar APP8976078242645304 VERSION 1rjaylidreslimbosNo ratings yet
- Childhood and Adolescence: Voyages in Development, 7e: Chapter 5: Infancy: PhysicalDocument50 pagesChildhood and Adolescence: Voyages in Development, 7e: Chapter 5: Infancy: PhysicalNUR HUMAIRA ROSLINo ratings yet
- Lee Endocrine SystemDocument3 pagesLee Endocrine SystemLouise Mica LeeNo ratings yet
- 14 06 sIUGR Florence 2 PDFDocument19 pages14 06 sIUGR Florence 2 PDFMeycha Da FhonsaNo ratings yet
- Acute AbdomenDocument45 pagesAcute AbdomenVeronikaNo ratings yet
- METHIRGINEDocument2 pagesMETHIRGINEChoox PriiNo ratings yet
- Placenta Previa Case StudyDocument59 pagesPlacenta Previa Case Studyjuel_navarro88% (33)
- Health Sector ReformDocument12 pagesHealth Sector ReformBritney ApasNo ratings yet
- SOLVED Recalls April 2018 and PreviousDocument256 pagesSOLVED Recalls April 2018 and PreviousNQ ZNo ratings yet
- Surgery of The AppendixDocument5 pagesSurgery of The AppendixJoseph De JoyaNo ratings yet
- Rectal Palpation Harry MomontDocument2 pagesRectal Palpation Harry MomontMaksar Muhuruna LaodeNo ratings yet
- Iron Deficiency Anemia Study DesignDocument43 pagesIron Deficiency Anemia Study DesignDrPriyanka Prashant PawsheNo ratings yet
- The Role of Husband in Assisting Wife Who Suffer Anemia in PregnancyDocument8 pagesThe Role of Husband in Assisting Wife Who Suffer Anemia in Pregnancyyudistira chairinaNo ratings yet
- Endocrine SystemmmDocument3 pagesEndocrine SystemmmTricia GorozaNo ratings yet
- Drug Treatment of Hypertension in PregnancyDocument15 pagesDrug Treatment of Hypertension in PregnancytetriNo ratings yet
- Situation 1 - Mr. Ibarra Is Assigned To The Triage Area and While On Duty, He Assesses The Condition of Mrs. Simon WhoDocument52 pagesSituation 1 - Mr. Ibarra Is Assigned To The Triage Area and While On Duty, He Assesses The Condition of Mrs. Simon Whogerald_ichigoNo ratings yet