Professional Documents
Culture Documents
Surgery of The Appendix
Uploaded by
Joseph De JoyaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Surgery of The Appendix
Uploaded by
Joseph De JoyaCopyright:
Available Formats
Surgery: The Appendix o Usually in one of the infarcted areas of the
antimesenteric border
o Just beyond the obstruction and not at the
References: Baby and Mommy Schwartz, 10th Edition
tip
Sequence is NOT inevitable –some episodes
Anatomy and Function spontaneously resolves
Base is attached to the cecum Causes of obstruction
Tip may be retrocecal (most common), pelvic, subcecal, o Fecalith or appendicolith (most common)
preileal, or right pericolic in postion o Foreign bodies
3 taenia coli converge at the junction of cecum and o Intestinal worms
appendix o Trauma
Length may be <1 cm to >30 cm (6-9 cm most common) o Bezoars
Lymphoid tissue, secretes IgA (an integral component of
gut-associated lymphoid tissue [GALT]) Bacteriology
o Function is “not essential” –no immune Principal organisms involved are Escherichia coli (G-,
compromise upon resection facultative, bacilli) and Bacteroides fragilis (G+, anaerobic,
bacilli)
Acute Appendicitis o Both are normal flora of appendix
o Seen in both acute and perforated appendicitis
Historical Background Up to 14 different organisms were identified
Charles McBurney – greatest contributor to treatment Culture – questionable (normal flora predominance)
(1889) o Peritoneal culture reserved for patients who are
o Described McBurney’s point (point of maximum immunosuppressed and PX who develop
tenderness) abscess after treatment
o One-half to two inches inside the right anterior Broad-spectrum antibiotics indicated
spinous process of the ilium on a line drawn to o Non perforated → 24-48 hour-antibiotics
the umbilicus o Perforated → 7-10 days recommended
Semm – widely credited to 1st perform a successful o IV antibiotics given when WBC count is normal
laparoscopic appendectomy (1982) and patient afebrile for 24 hours
Incidence Clinical Manifestations
Lifetime rate: 12%m:25%f – 7% undergoes appendectomy Symptoms
for acute appendicitis o Abdominal pain – prime symptom in acute onset
Seen more frequently in 2nd to 4th decades of life (20-40); Classic presentation: diffusely centered
mean age of 31.3; median age of 22 in lower epigastrium/umbilical area
Male over female predominance – 1.2-1.3m:1f Moderately severe, steady, may have
Rate of misdiagnosis: 15.3% (equivalent to appendiceal superimposed intermittent cramping
rupture) After varying period of 1-12 hours –
o Higher in women – 22.2%:9.3% localizes to RLQ
Negative appendectomy rate for women of reproductive (there are cases where pain starts in
age: 23.2% highest in 40-49 years old RLQ and stays there)
o Highest negative appendectomy rate – women Location of appendix account for
>80 years old variation of pain locus (in the somatic
Etiology and pathogenesis (interpret as 1 will cause 2, 2 phase)
will cause 3…) o Anorexia is almost always present
1. Proximal obstruction Diagnosis is questionable if Px is not
2. Closed loop obstruction (Continuous luminal anorectic
secretion) o Vomiting is present in 75% of cases
3. Distention o Obstipation prior to onset of pain
4. Stimulates visceral afferent stretch fibers o Diarrhea may occur (particularly in children)
5. Pain (vague, dull, and diffuse) in mid/lower o In 95% of cases: Anorexia → abdominal pain →
epigastrium vomiting
6. Cramps (distention aggravates peristaltic waves) If vomiting comes before pain, think
7. Continued distention + multiplication of resident otherwise
bacteria (may cause nausea and vomiting) Signs
8. Pressure exceeds venous pressure o Determined principally by anatomic position of
9. Capillary and venous occlusion, arteriolar inflow appendicitis
continues o Vital signs
10. Engorgement + vascular congestion Temperature elevation rarely exceeds
11. Arteriolar inflow occlusion 1C
12. Involvement of serosa and parietal peritoneum Pulse rate – N to sl↑
13. Pain shifts to RLQ Greater changes in VS indicate
Ultimately, distention + bacterial invasion + vascular complication
compromise + infarction = PERFORATION o General Survey and PE findings
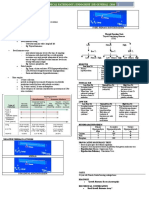
Prefers to lie supine with thighs drawn Alvarado Scale for Diagnosing Appendicitis
up (motion causes pain) Category Manifestation Value
Classic RLQ pain if appendix is anterior Symptoms Migration of pain 1
of cecum Anorexia 1
Tenderness maximal at or near Nausea/Vomiting 1
McBurney’s point Signs RLQ tenderness 2
Direct rebound tenderness Rebound 1
Referred/indirect rebound tenderness Elevated temp 1
may also be present (maximal at RLQ) Lab values Leukocytosis 2
Indicates peritoneal irritation Left shift 1
Rovsing’s sign (+) Total points 10
Palpatory pressure in LLQ
produces pain in RLQ Appendiceal Rupture
Cutaneous hyperesthesia at T10-T12
Immediate appendectomy – standard treatment of acute
Abdominal guarding
appendicitis due to risk of rupture
Psoas sign (+)
25.8% - overall rate of perforated appendicitis
Obturator sign (+)
o Most prevalent in children <5 years old, and
Laboratory Findings
older patients >65 years old
o Mild leukocytosis (10,000-18,000/mm3)
Nonoperative treatment increases morbidiy and mortality
Usually present in acute onset,
risk associated with ruptured appendicitis
uncomplicated cases
Rupture should be suspected in the following
With PMN predominance
o Fever >39C
If WBC > than specified, suspect
o WBC >18,000/mm3
perforation
o Localized rebound/referred tenderness
o Urinalysis useful to rule-out UT as infection
o Ill-defined mass on PE
source
Phlegmon
Bacteriuria not found in catheterized
Periappendiceal abscess
urine specimen in acute cases
Px with mass – longer duration of
symptoms (5-7 days)
Imaging Studies
Of note
Plain radiographic films are rarely helpful
o Phlegmons and small abscesses may be treated
o Useful only to rule-out other pathologies
conservatively with antibiotics
o Acute – abnormal bowel gas pattern –
o Well-localized abscesses – percutaneous
nonspecific finding
drainage
o Fecalith is rarely noted – if present, highly
o Complex abscesses – surgical drainage
suggestive of diagnosis
o Interval appendectomy recommended after 6
Graded compression sonography
weeks following acute event treated
o With maximal compression, appendiceal
nonoperatively or with simple drainage of
diameter is measured in the anteroposterior
abscess
dimension
o Positive – if appendix is noncompressible 6 mm
Differential Diagnosis
or more in anteroposterior direction
Essentially the diagnosis of “acute abdomen”
o Presence of appendicolith establishes diagnosis
o Clinical manifestations are mostly not specific
o Other highly suggestive findings
and therefore may have identical clinical picture
Thickening of appendiceal wall
with a wide variety of acute processes in the
Periappendiceal fluid or mass
abdomen
o When acute appendicitis is excluded, perform
Preoperative diagnosis accuracy of 85% is acceptable
brief survey of the abdominal cavity
o Less than this may result to unnecessary
On CT scan
operations
o Inflamed appendix is dilated
o If consistently greater than 90% - would mean
o Wall thickened
you’re “observing” instead of operating
o Evidence of inflammation with “dirty fat”
Diseases/conditions commonly misdiagnosed as acute
o Thickened mesoappendix
o Obvious phlegmon appendicitis and found to be naught ntraoperatively
(descending order of frequency):
o Fecalith (easily visualized)
o Arrowhead sign (thickening of the cecum, o Acute mesenteric lymphadenitis
o No organic pathologic condition
funnels contrast to the inflamed appendix)
o Acute pelvic inflammatory disease
Laparoscopy
o Twisted ovarian cyst or ruptured graafian follicle
o Both diagnostic and therapeutic approach
o Acute gastroenteritis
o Most useful for females
Differentials depend on four major factors:
Used to differentiate acute
o Anatomic location
appendicitis from acute gynecologic
o Stage of process
pathology
o Px age
o Px sex
Acute Appendicitis in the Young o TB
Diagnosis is more difficult o Lymphoma
Higher morbidity rate due to o Other causes of infectious colitis
o ↑ propensity for rupture Immediate appendectomy is indicated
Underdeveloped tissues and rapid In patients with diarrhea as primary symptom,
progression colonoscopy may be warranted
o Underdeveloped greater omentum Negative appendectomy rate – 5-10%
Lesser ability to contain a rupture o Up to 25% will have AIDS-related entities in
<5 vs. 5-12 years of age respectively operative specimen
o Negative appendectomy rate: 25% vs. <10% CMV
o Appendiceal perforation rate: 45% vs. 20% Kaposi
Treatment regimen includes M. aviumintracellulare
o Perforated – immediate appendectomy and Postoperative morbidity rate higher in Px with perforation
irrigation of peritoneal cavity Hospital stay rate is longer
o Antibiotics
Nonperforated – 24-48 hrs Treatment
Perforated – 7-10 days Preoperative preparations
IV preparations given when Px is o Adequate hydration
afebrile for at least 24 hrs o Electrolyte abnormalities corrected
o Laparoscopic appendectomy – safe and effective o Preexisting conditions should be addressed
Cardiac
Acute Appendicitis in Older Adults Pulmonary
Incidence is lower than young Renal
Morbidity and mortality is higher o Preoperative antibiotics may be considered
High index of suspicion should be observed (lowered infectious complications in trials)
>80 years of age Cefoxitin
o Perforation rate – 49% Cefotetan
o Mortality – 21% Ticarcillin-clavulanic acid
More severe infections
Acute Appendicitis in Pregnancy Carbapenems
Most frequently encountered extrauterine disease Combination therapy with
requiring surgical treatment in pregnancy o 3rd gen
Most frequent during 1st and 2nd trimesters cephalosporin
Diagnosis is inversely related to gestational age o Monobactam
o Due to displacement of appendix latero- Aminoglycoside plus
superiorly o Clindamycin
Nausea and vomiting (or new-onset) after 1st trimester o Metronidazole
may be of consideration for diagnosis Open Appendectomy
Abdominal pain and tenderness may be present but less o Incision is either McBurney (oblique) or Rocky-
guarding (due to abdominal laxity) Davis (transverse) at the point of maximal
tenderness or palpable mass
WBC >15.000-20,000 /uL – PMN predominance
(according to doc Cabredo, Rocky-
Abdominal ultrasound is beneficial
Davis is more common now-a-days)
Laparoscopy may be indicated especially in early
o Abscess suspected → lateral incision for
pregnancy
retroperitoneal drainage
Premature labor risk of 10-15% in appendectomy during
o Diagnosis in doubt → midline incision for better
pregnancy
examination of cavity
Appendiceal perforation – significant factor in fetal and
Relevant in older Px where
maternal death
malignancy/diverticulitis is possible
o Fetal mortality – 3-5% in early appendicitis to
o Localization techniques
20% if with perforation
Follow convergence point of taenia coli
Sweeping lateral to medial motion
Appendicitis in Patients with AIDS or HIV Infection
Limited mobilization of cecum
Presentation of acute appendicitis same as noninfected o Once appendix is identified
persons except for Divide mesoappendix
o Nonmanifestation of absolute leukocytosis (only Ligate appendiceal artery
relative leukocytosis) o Appendiceal stump clearly viable with base of
Increased risk for appendiceal rupture associated to cecum uninvolved in inflammatory process -
o Delay in manifestation managed by:
o Low CD4 count Simple ligation
Differential diagnosis should always include opportunistic Ligation and inversion
infection such as but not limited to
Purse-string stitch
o CMV
Z-string stitch
o Kaposi sarcoma
o Mucosa obliterated to avoid mucocele formation
o Peritoneal cavity irrigated o Associated to added expense and longer
o Wound closed in layers hospitalization
o If perforation or gangrene is found in adults o Initial treatment include
Skin and subcutaneous tissue left open to IV antibiotics
heal by secondary intent (may be closed Bowel rest
after 4-5 days [delayed primary closure]) o Percutaneous or operative drainage of abscess is
o In children primary wound closure is always not considered failure of conservative therapy
indicated
Laparoscopy Prognosis
o Performed under general anesthesia Mortality is steadily decreasing
o Requires 3 ports (or sometimes 4) o Principal factors of mortality include rupture
o Steps before surgical treatment and age of Px
Surgeon in Px’s left Complications occur in 3% of Px with nonperforated vs.
Assitant 1 operates camera 47% in Px with perforations
One trocar in the umbilicus Serious early complication is usually septic (abscess and/or
Another trocar suprapubic wound infection)
3rd trocar variable (usually in LLQ, Complete wound dehiscence rarely occurs in McBurney
epigastrium, or RUQ) type of incision
Abdomen is first thoroughly explored Predilection sites of abscesses
(rule-out other pathology) o Appendiceal fossa
Identify appendix o Pouch of Douglas
Dissection at the base o Subhepatic space
Division of mesentery from o Between intestinal loops
appendiceal base o Rectally bulging abscess (transrectal drainage)
If mesoappendix involved, Fecal fistula may occur as a complication of appendectomy
divide appendix by stapler; o May be due to sloughing of cecal portion inside a
then divide mesoappendix constricting purse-string suture
from appendix o Ligature’s slipping off an appendiceal stump
Base of appendix is not inverted o Necrosis from abscess encroaching on cecum
Appendix removed via trocar site or
within retrieval bag Chronic Appendicitis
Evaluate site for hemostasis An uncommon disease
RLQ irrigated Pain lasts longer but less intense in the same location
Trocars removed Characteristic symptoms
o Should be considered only as an option in thin o Vomiting (lower incidence)
males aged 15-45 o Anorexia
o May be beneficial to obese males o Nausea (occasionally)
o Pregnant women withpresumed appendicitis o Pain with motion
may benefit from diagnostic laparoscopy o Malaise
Leukocyte counts are normal
Laparoscopy vs. Open Appendectomy CT scans are non-diagnostic
Category Laparoscopy Open Laparoscopy is effective
Duration and cost ↑ ↓ Appendectomy is curative
Wound infection ↓ ↑ Px whose symptoms are not cured or recur usually have
Intraabdominal Crohn disease as an underlying diagnosis
↑ ↓
abscess
Pain of 1st Appendiceal Parasites
↓ ↑
postoperative day
Live parasites cause obstruction
Hospital length of
↓ ↑ Ascaris lumbricoides – most common
stay
Others
Benefit to thin
↓ ↑ o E. vermicularis
males (15-45 yo)
o S. stercoralis
Benefit to obese
↑ ↓ o E. granulosis
males
Presence of parasites make appendectomy difficult
Px treated with helminthicide post-operation
Interval Appendectomy
Amebiasis can also cause appendicitis
o Performed on Px with palpable or
o Invasion by trophozoites
radiographically documented mass (abscess or
o Component of more generalized intestinal
phlegmon)
amebiasis
Initial conservative therapy with
o Appendectomy followed by antibiotic therapy
interval appendectomy after 6-10
(metronidazole)
weeks later
o Provides lower morbidity and mortality rates Incidental Appendectomy
than immediate appendectomy
Both appendicitis and appendicitis with perforation are Mucocele
more common in men than women o Leads to progressive enlargement due to
NNT = 36 (36 incidental appendectomies performed to intraluminal accumulation of mucoid substance
prevent the occurrence of 1 appendicitis) o Histologic type dictates course and prognosis of
Indications for incidental appendectomy disease
o Children about to undergo chemotherapy Retention cysts
o Disabled who cannot respond normally to Mucosal hyperplasia
abdominal pain Cystadenomas
o Crohn disease Px in whom cecum is free of Cystadenocarcinomas
macroscopic disease o If benign – simple appendectomy
o Individuals about to travel to remote areas o Pseudomyxoma peritonei
without access to medical/surgical care Rare condition where diffuse
collections of gelatinous fluid are
Tumors associated with mucinous implants on
Extremely rare peritoneal surfaces and omentum
2-3x more common in females than
Incidence of primary appendiceal malignancy is 0.9-1.4%
males
found on appendectomy specimens
Usually present with
<50% of cases diagnosed perioperatively
Abdominal pain
Epidemiology
Distention
o Carcinoid (most common in most series studies)
– greater than 50% of cases Mass
o NCI – SEER reports histologic update Ureteral obstruction and/or venous
Mucinous adenocarcinoma as most obstruction may occur
common (37%) CT scanning is preferred
Carcinoid as second most common Perioperative location of mucinous
(33%) ascites and tumor deposits in women
Carcinoid Right hemidiaphragm
o Appendix most common site of GI carcinoid Right retrohepatic space
Small bowel then rectum Left paracolic gutter
(respectively) Ligament of Treitz
o Carcinoid syndrome rarely associated with Ovaries
appendiceal carcinoid unless metastases are Surgical debulking is mainstay of
present treatment (all gross disease removed)
o The tumor may/may not obstruct the lumen Appendectomy routinely performed
(most common site is apex/tip) Hysterectomy with bilateral salphingo-
o Malignant potential directly proportional to size oophorectomy is performed in women
of tumor Not of benefit
o <1 cm – 78% Ultra-radical surgery
o 1-2 cm – 17% Adjuvant chemo
o >2 cm – 5% Systemic post-op chemo
o Treatment Lumph node and distant mets are
Simple appendectomy most common uncommon
<1 cm with mesoappendiceal Recurrences treated by additional
extension and >1.5 cm – right surgery – although associated with
hemicolectomy Enterotomies, anastomotic
Adenocarcinoma leaks, fistulas
o Rare neoplasm of appendix Lymphoma
o Has three subtypes o Uncommon
Mucinous adenocarcinoma o GIT most frequently involved extranodal site for
Colonic adenocarcinoma non-Hodgkin lymphoma
Adenocarcinoid Burkitt and leukemia also been
o Most commonly presents like an acute reported
appendicitis o Primary lymphoma frequency of 1-3%
May have additional signs like ascites o Presents as acute appendicitis
and/or palpable mass o CT scan finding ≥ 2.5 cm or surrounding soft
Neoplasm may incidentally be tissue thickening prompts suspicion
discovered perioperatively for an o If confined to appendix – appendectomy (w/o
unrelated cause adjuvant therapy
Recommended treatment for all types o Extension of tumor onto cecum or mesentery -
– formal right hemicolectomy right hemicolectomy
o Have propensity for early perforation With postoperative staging workup
o Px are at risk for both synchronous or before adjuvant therapy
metachronous neoplasms
You might also like
- Intussusception TransDocument4 pagesIntussusception TransJames Maravillas100% (1)
- (Surgery) Midterms PediatricsDocument5 pages(Surgery) Midterms Pediatricsalmira.s.mercadoNo ratings yet
- INGUINAL HERNIAS - Short Surgery PresentationDocument11 pagesINGUINAL HERNIAS - Short Surgery Presentationq6hzqsf2hfNo ratings yet
- PottDocument2 pagesPottkimNo ratings yet
- IntussDocument4 pagesIntussemman_abzNo ratings yet
- Spinal Infection: PathologyDocument2 pagesSpinal Infection: Pathologyyoyo06chillinNo ratings yet
- Backup of LO 2 DD HERNIA - Id.en-2Document3 pagesBackup of LO 2 DD HERNIA - Id.en-2dianNo ratings yet
- 6 SURGERY II 6 - Pediatric UrologyDocument6 pages6 SURGERY II 6 - Pediatric UrologyDeann RoscomNo ratings yet
- AppendixDocument2 pagesAppendixMikhail BrionesNo ratings yet
- AppendixyyyDocument2 pagesAppendixyyyAlbert CorderoNo ratings yet
- Book: - RecordingDocument8 pagesBook: - RecordingVon HippoNo ratings yet
- Pediatrics NotesDocument13 pagesPediatrics NotesYsa BonifacioNo ratings yet
- 5 Patho 1 - Lut - Dr. MesinaDocument11 pages5 Patho 1 - Lut - Dr. MesinaRobert Francis DikioNo ratings yet
- HerniasDocument6 pagesHerniasYalin AbouhassiraNo ratings yet
- The Appendix FinalDocument62 pagesThe Appendix FinalLajel S. LachicaNo ratings yet
- Hernia RepairDocument19 pagesHernia RepairdanarfsNo ratings yet
- Surgery 2.01.3 Omentum, Mesentery and Retroperitoneum - Dr. MendozaDocument8 pagesSurgery 2.01.3 Omentum, Mesentery and Retroperitoneum - Dr. MendozaJorge De VeraNo ratings yet
- Primary Review: Psoas Abscess: Case of The LiteratureDocument3 pagesPrimary Review: Psoas Abscess: Case of The LiteratureDung Tran HoangNo ratings yet
- (SURGPATH) 1.01 Gastrointestinal PathologyDocument20 pages(SURGPATH) 1.01 Gastrointestinal PathologyKarl ChavezNo ratings yet
- Anorectal MalformationDocument4 pagesAnorectal MalformationFawzia Haznah Nurul ImaniNo ratings yet
- Pruritus Ani, Hemorroidet EtjDocument4 pagesPruritus Ani, Hemorroidet EtjKreshnik HAJDARINo ratings yet
- 1 - Abdomen 1Document23 pages1 - Abdomen 1noushad aminNo ratings yet
- (Surg2-Trans) 4.01 AppendixDocument7 pages(Surg2-Trans) 4.01 AppendixJake Brandon M. Andal, RNDNo ratings yet
- 2.4.5.2.3.a Bowel ObstructionDocument35 pages2.4.5.2.3.a Bowel ObstructionProject ByNo ratings yet
- PEDTRIC SURGERY Dr. Isabedra - PDF Notes - 201702082201Document25 pagesPEDTRIC SURGERY Dr. Isabedra - PDF Notes - 201702082201deevonc100% (1)
- Esophagus - 1Document27 pagesEsophagus - 1hussain AltaherNo ratings yet
- Undescended Testes: What General Practitioners Need To KnowDocument4 pagesUndescended Testes: What General Practitioners Need To KnowRizka Desti AyuniNo ratings yet
- SGD AppendicitisDocument11 pagesSGD Appendicitisนีล ไบรอันNo ratings yet
- Pelvic Organ ProlapseDocument5 pagesPelvic Organ Prolapsecgao30No ratings yet
- Slide Hernia 2003Document24 pagesSlide Hernia 2003anfaNo ratings yet
- HirschprungDocument13 pagesHirschprungfitra hayatiNo ratings yet
- French 16 - AppendixDocument5 pagesFrench 16 - AppendixPrince VallejosNo ratings yet
- AppendicitisDocument4 pagesAppendicitisRonaldoNo ratings yet
- Worm AppendicitisDocument1 pageWorm AppendicitisNandan.m.pNo ratings yet
- Testis and ScrotumDocument7 pagesTestis and Scrotumyoussef.aziz2020No ratings yet
- 0 Yazan Mini-OSCE PedsDocument60 pages0 Yazan Mini-OSCE Pedsmoyasserayoub78No ratings yet
- Deviriligo Notes 12Document99 pagesDeviriligo Notes 12A Fish100% (1)
- When To Operate On Abdominal Stab Wounds: K. TavilogluDocument4 pagesWhen To Operate On Abdominal Stab Wounds: K. Tavilogluimade candraNo ratings yet
- L7.3-SURG-Colon, Rectum, Anus, and The Appendix (Mar2022)Document3 pagesL7.3-SURG-Colon, Rectum, Anus, and The Appendix (Mar2022)Erald PaderangaNo ratings yet
- Delay in Diagnosis of Congenital Anal ST PDFDocument4 pagesDelay in Diagnosis of Congenital Anal ST PDFJimi Kalvin SarareniNo ratings yet
- Hirschprung's DiseaseDocument26 pagesHirschprung's DiseaseAbdur RaqibNo ratings yet
- Hernias UltrasoundDocument35 pagesHernias UltrasoundRafa Rodríguez AveigaNo ratings yet
- Undescended TestesDocument29 pagesUndescended TestesHillary Bushnell100% (1)
- Inguinal Hernia Review PDFDocument4 pagesInguinal Hernia Review PDFSebastian SetiahardjaNo ratings yet
- Gastrointestinal System DiseasesDocument6 pagesGastrointestinal System DiseasesHazel ConjeNo ratings yet
- Oesophagus - Lecture (1 & 2) SurgeryDocument27 pagesOesophagus - Lecture (1 & 2) Surgeryhussain AltaherNo ratings yet
- Utero-Vaginal Prolapse: BY: Muhammad Anwar Ridzwan Bin Abd HarisDocument47 pagesUtero-Vaginal Prolapse: BY: Muhammad Anwar Ridzwan Bin Abd HarisHizami NorddinNo ratings yet
- Acute Appendicitis: Michael Alan Cole Robert David HuangDocument10 pagesAcute Appendicitis: Michael Alan Cole Robert David HuangandreaNo ratings yet
- Wa0000. 1Document41 pagesWa0000. 1Aditya SinghNo ratings yet
- Gastrointestinal Tract PathologyDocument8 pagesGastrointestinal Tract PathologyMiguel Cuevas Dolot100% (2)
- Appendix DuplicationDocument3 pagesAppendix DuplicationMario TrejoNo ratings yet
- Case Report APDocument48 pagesCase Report APSimon Peter MollanedaNo ratings yet
- Git تجميعاتDocument146 pagesGit تجميعاتMenna SalemNo ratings yet
- Hernia OSCE ExaminationDocument3 pagesHernia OSCE ExaminationkylieverNo ratings yet
- Inguinal Hernia and Hydrocele: Congenital Hydrocele Presents As A Mass in The Scrotum ShortlyDocument3 pagesInguinal Hernia and Hydrocele: Congenital Hydrocele Presents As A Mass in The Scrotum ShortlyBetão AviãoNo ratings yet
- 11 AppendixDocument15 pages11 AppendixOmar MohammedNo ratings yet
- Minilaparoscopic Left Paraduodenal Hernia Repair-A CaseDocument4 pagesMinilaparoscopic Left Paraduodenal Hernia Repair-A CaseAritra PaulNo ratings yet
- Gyne 2.6 - Benign and Malignant Tumors of The Ovaries and Fallopian TubesDocument8 pagesGyne 2.6 - Benign and Malignant Tumors of The Ovaries and Fallopian TubesVon HippoNo ratings yet
- JIndianAssocPediatrSurg203148-2122777 003522Document2 pagesJIndianAssocPediatrSurg203148-2122777 003522Cata santaNo ratings yet
- Hypothyroidism - Harrison Copy-PasteDocument4 pagesHypothyroidism - Harrison Copy-PasteJoseph De Joya100% (1)
- Ust Mock Boards 2017 - Anatomy-1Document10 pagesUst Mock Boards 2017 - Anatomy-1Jason Mirasol100% (1)
- DRUG of CHOICE - InfectiousDocument1 pageDRUG of CHOICE - InfectiousJoseph De JoyaNo ratings yet
- Highlights Citric Acid CycleDocument1 pageHighlights Citric Acid CycleJoseph De JoyaNo ratings yet
- AnaPLEDocument20 pagesAnaPLEMc EstanislaoNo ratings yet
- AnaPLEDocument20 pagesAnaPLEMc EstanislaoNo ratings yet
- Low Free T4 Normal Free T4 High Free T4Document3 pagesLow Free T4 Normal Free T4 High Free T4Joseph De JoyaNo ratings yet
- 1.entamoeba Histolytica - Is The Major Pathogen in This GroupDocument14 pages1.entamoeba Histolytica - Is The Major Pathogen in This GroupJoseph De JoyaNo ratings yet
- Structures of GovernmentDocument6 pagesStructures of GovernmentJoseph De JoyaNo ratings yet
- Introduction To HISDocument20 pagesIntroduction To HISJoseph De JoyaNo ratings yet
- Fundamentals of HISDocument19 pagesFundamentals of HISJoseph De JoyaNo ratings yet
- 3 Dyspnea, Palpitation, CyanosisDocument62 pages3 Dyspnea, Palpitation, CyanosisJoseph De JoyaNo ratings yet
- 5HM04 Module 5.evaluating Healthcare Institution Financial PerformanceDocument21 pages5HM04 Module 5.evaluating Healthcare Institution Financial PerformanceJoseph De JoyaNo ratings yet
- Reporter:: Master in Hospital Management Healthcare Marketing Course OutlineDocument3 pagesReporter:: Master in Hospital Management Healthcare Marketing Course OutlineJoseph De JoyaNo ratings yet
- Evidenced Based MedicineDocument20 pagesEvidenced Based MedicineJoseph De JoyaNo ratings yet
- An Urgency To Improve Nurse's Salary Through PhilHealth's Professional FeeDocument9 pagesAn Urgency To Improve Nurse's Salary Through PhilHealth's Professional FeeJoseph De JoyaNo ratings yet
- Chapter 4Document3 pagesChapter 4aznknight323No ratings yet
- Bates Test Bank Chapter 3 PDFDocument3 pagesBates Test Bank Chapter 3 PDFJoseph De JoyaNo ratings yet
- 3-Tx Appraisal TipsDocument2 pages3-Tx Appraisal TipsJoseph De JoyaNo ratings yet
- Physical Diagnosis CVS BCCM Second Year Lecture MARKMDDocument26 pagesPhysical Diagnosis CVS BCCM Second Year Lecture MARKMDJoseph De JoyaNo ratings yet
- FEVER - FUO - RASH Into To Medicine - First YearDocument93 pagesFEVER - FUO - RASH Into To Medicine - First YearJoseph De JoyaNo ratings yet
- Abdominal Pain, HeadaceDocument22 pagesAbdominal Pain, HeadaceJoseph De JoyaNo ratings yet
- Intro To Medicine: Mark Joseph Cervantes, SAC Dip, MDDocument14 pagesIntro To Medicine: Mark Joseph Cervantes, SAC Dip, MDJoseph De JoyaNo ratings yet
- Porphyrias Henrys 23eDocument2 pagesPorphyrias Henrys 23eJoseph De JoyaNo ratings yet
- Respi Anatomy (Correlative Anatomy)Document7 pagesRespi Anatomy (Correlative Anatomy)Joseph De JoyaNo ratings yet
- Physical Diagnosis SGD 1 CVS Module CaseDocument1 pagePhysical Diagnosis SGD 1 CVS Module CaseJoseph De JoyaNo ratings yet
- Quiz 1 Bates Chapter 1 and 2 Exam Fever, FuoDocument3 pagesQuiz 1 Bates Chapter 1 and 2 Exam Fever, FuoJoseph De JoyaNo ratings yet
- Awsum BrandingDocument18 pagesAwsum Brandingdharam123_904062105No ratings yet
- Shabeer Et Al-2018-Journal of PerinatologyDocument8 pagesShabeer Et Al-2018-Journal of PerinatologyrenataNo ratings yet
- LinkageDocument47 pagesLinkageTony BernardNo ratings yet
- First Communion: You Are The VoiceDocument10 pagesFirst Communion: You Are The VoiceErnesto Albeus Villarete Jr.No ratings yet
- Formulating A Dental Treatment Plan: DR Tashnim BagusDocument33 pagesFormulating A Dental Treatment Plan: DR Tashnim BagustarekrabiNo ratings yet
- Vacon NXP System Drive Hardware Manual DPD01365A UDocument72 pagesVacon NXP System Drive Hardware Manual DPD01365A UTanuTiganu100% (3)
- Sample CV Format (JIMS FORMAT)Document3 pagesSample CV Format (JIMS FORMAT)Elay PedrosoNo ratings yet
- Unika Hole SawDocument21 pagesUnika Hole SawQin DieselNo ratings yet
- Blood Stasis and What Does That MeanDocument2 pagesBlood Stasis and What Does That MeanCarl MacCordNo ratings yet
- Current Issues On Construction Project ManagementDocument2 pagesCurrent Issues On Construction Project ManagementJoyce Abegail De PedroNo ratings yet
- Ccii Proposal EssayDocument4 pagesCcii Proposal Essayapi-456307983No ratings yet
- Arduino CertificationDocument8 pagesArduino Certificationhack reportNo ratings yet
- Reading Passage 1: IELTS Recent Actual Test With Answers Volume 1Document17 pagesReading Passage 1: IELTS Recent Actual Test With Answers Volume 1Amogha GadkarNo ratings yet
- Mem CalcDocument6 pagesMem CalcQruisedNo ratings yet
- Invoice, packing list mẫuDocument2 pagesInvoice, packing list mẫuPHI BUI MINHNo ratings yet
- 150.66-RP4 YcalDocument92 pages150.66-RP4 YcalJosé RamosNo ratings yet
- E560 PSR00 DSDocument4 pagesE560 PSR00 DSSalvador FayssalNo ratings yet
- Social Science Assignment Class 8 CBSEDocument3 pagesSocial Science Assignment Class 8 CBSEgurdeepsarora8738No ratings yet
- Oil Palm Fractions Derivatives Web PDFDocument6 pagesOil Palm Fractions Derivatives Web PDFIan RidzuanNo ratings yet
- Birthday QuotesDocument24 pagesBirthday QuotesArniel CatubigNo ratings yet
- Benefits of SwimmingDocument3 pagesBenefits of Swimmingaybi pearlNo ratings yet
- Unit 1 Marks: 15 Introduction To Micro System and Smart SystemsDocument9 pagesUnit 1 Marks: 15 Introduction To Micro System and Smart SystemsSudarsh KNo ratings yet
- Elecsys T4: Cobas e 411 Cobas e 601 Cobas e 602 English System InformationDocument5 pagesElecsys T4: Cobas e 411 Cobas e 601 Cobas e 602 English System InformationIsmael CulquiNo ratings yet
- Fleming Trio-E Promotional SheetDocument2 pagesFleming Trio-E Promotional SheetRed BarnNo ratings yet
- L23Document29 pagesL23Mary MorseNo ratings yet
- MSDS TSHDocument8 pagesMSDS TSHdwiNo ratings yet
- Volume Booster: YT-300 / YT-310 / YT-305 / YT-315 / YT-320Document1 pageVolume Booster: YT-300 / YT-310 / YT-305 / YT-315 / YT-320SeikatsukaiNo ratings yet
- Organisational Behaviour DEC 2022Document10 pagesOrganisational Behaviour DEC 2022Rajni KumariNo ratings yet
- Alabama Religious Exemption AdvisoryDocument1 pageAlabama Religious Exemption AdvisoryABC 33/40No ratings yet