Professional Documents
Culture Documents
Introduction To Anatomy (Lec 7)
Uploaded by
ehtshamulhaq060 ratings0% found this document useful (0 votes)
13 views32 pagesOriginal Title
Introduction to Anatomy (Lec 7) (1)
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
13 views32 pagesIntroduction To Anatomy (Lec 7)
Uploaded by
ehtshamulhaq06Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 32
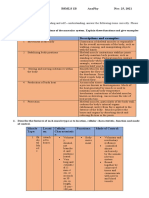
TISSUES OF BODY
Recommended Books:
• Fundamentals of Anatomy & Physiology. Martini F, Nath JL, Bartholomew EF. 10th Edition
• Principles of Anatomy and Physiology. Tortora GJ, Derrickson B. 13th Edition
Tissue Membranes
Tissue membranes are physical barriers of four types: mucous, serous, cutaneous, and synovial.
A tissue membrane forms a physical barrier. There are many different types of anatomical membranes.
Each consists of an epithelium supported by connective tissue. Four such membrane types are found in the body: (1)
mucous membranes, (2) serous membranes, (3) the cutaneous membrane, and (4) synovial membranes
Mucous Membranes
Mucous membranes, or mucosae, line, passageways and chambers that communicate with the exterior, including those in
the digestive, respiratory, reproductive, and urinary tracts. The epithelial surfaces of these passageways must be kept moist
to reduce friction and, in many cases, to facilitate absorption or secretion. The epithelial surfaces are lubricated either by
mucus produced by mucous cells or multicellular glands, or by fluids, such as urine or semen. The areolar tissue
component of a mucous membrane is called the lamina propria. Many mucous membranes contain simple epithelia that
perform absorptive or secretory functions, such as the simple columnar epithelium of the digestive tract. However, other
types of epithelia may be involved. For example, a stratified squamous epithelium is part of the mucous membrane of the
mouth, and the mucous membrane along most of the urinary tract contains a transitional epithelium.
Tissue Membranes
Serous Membranes
Serous membranes line the sealed, internal cavities of the trunk—cavities that are not open to the exterior. These
membranes consist of a mesothelium supported by areolar tissue. The three types of serous membranes are (1) the pleura,
which lines the pleural cavities and covers the lungs; (2) the pericardium, which lines the pericardial cavity and covers
the heart; and (3) the peritoneum, which lines the peritoneal cavity and covers the surfaces of the enclosed organs. Serous
membranes are very thin, but they are firmly attached to the body wall and to the organs they cover. When looking at an
organ such as the heart or stomach, you are really seeing the tissues of the organ through a transparent serous membrane.
The primary function of any serous membrane is to minimize friction between the surfaces that it covers. Each serous
membrane can be divided into a parietal portion, which lines the inner surface of the cavity, and an opposing visceral
portion, or serosa, which covers the outer surfaces of visceral organs. These organs often move or change shape as they
carry out their various functions, and the parietal and visceral surfaces of a serous membrane are in close contact at all
times. Friction between these surfaces is kept to a minimum because mesothelia are very thin and permeable, and tissue
fluids continuously diffuse onto the exposed surfaces, keeping them moist and slippery.
Tissue Membranes
The fluid secreted by the mesothelium of a serous membrane is called serous fluid. Serous fluid prevents friction between
the cavity walls and the surfaces of internal organs. However, after an injury or in certain disease states where there is an
imbalance of hydrostatic and osmotic forces, the volume of serous fluid, now called transudate may increase dramatically.
This change may complicate existing medical problems or produce new ones.
The Cutaneous Membrane
The cutaneous membrane is the skin that covers the surface of your body. It consists of a stratified squamous epithelium
and a layer of areolar tissue reinforced by underlying dense irregular connective tissue. In contrast to serous and mucous
membranes, the cutaneous membrane is thick, relatively waterproof, and usually dry.
Synovial Membranes
Adjacent bones often interact at joints, or articulations. There the two articulating bones are very close together or in
contact. Joints that permit significant amounts of movement are complex structures. Such a joint is surrounded by a
fibrous capsule, and the ends of the articulating bones lie within a joint cavity filled with synovial fluid. The synovial fluid
is produced by a synovial membrane, which lines the joint cavity. A synovial membrane consists of an extensive area of
areolar tissue containing a matrix of interwoven collagen fibers, proteoglycans, and glycoproteins.
Tissue Membranes
An incomplete layer, or sheet, of macrophages and specialized fibroblasts overlies and separates the areolar tissue from the
joint cavity. These cells regulate the composition of the synovial fluid. This incomplete layer of cells is often called an
epithelium, but it differs from true epithelia in four respects: (1) It develops within a connective tissue; (2) no basement
membrane is present; (3) gaps of up to 1 mm may separate adjacent cells; and (4) fluid and solutes are continuously
exchanged between the synovial fluid and capillaries in the underlying connective tissue.
Even though a smooth layer of articular cartilage covers the ends of the bones, the surfaces must be lubricated to keep
friction from damaging the opposing surfaces. Synovial fluid provides the much-needed lubrication. This fluid is similar
in composition to the ground substance in loose connective tissues. Synovial fluid circulates from the areolar tissue into
the joint cavity and percolates through the articular cartilages, supplying oxygen and nutrients to the chondrocytes. Joint
movement is important in stimulating the formation and circulation of synovial fluid: If a synovial joint is immobilized for
long periods, the articular cartilages and the synovial membrane undergo degenerative changes.
Muscle Tissue
Muscle tissues are specialized for contraction and producing movements.
Muscle cells have organelles and properties distinct from other cells.
There are three types of muscle tissue: (1) skeletal muscle, which forms the large muscles that produce gross body
movements; (2) cardiac muscle, found in the heart, is responsible for circulating the blood; and (3) smooth muscle, found in
the walls of visceral organs and a variety of other locations, where it provides elasticity, contractility, and support. The
contraction mechanism is similar in all three types of muscle tissue, but the muscle cells differ in internal organization.
Skeletal Muscle tissue
Skeletal muscle tissue contains very large muscle cells—up to 0.3 m (1 ft) or more in length. The individual muscle cells are
usually called muscle fibers because they are relatively long and slender. Each muscle fiber has several hundred nuclei just
inside the plasma membrane. For this reason, the fibers are described as multinucleate. Skeletal muscle fibers are incapable
of dividing. New muscle fibers are produced instead through the divisions of myosatellite cells (satellite cells), stem cells
that persist in adult skeletal muscle tissue. As a result, skeletal muscle tissue can at least partially repair itself after an injury.
Skeletal muscle fibers also contains actin & myosin filaments however, these filaments are organized into repeating patterns
that give the cells a striated, or banded, appearance. The striations, or bands, are easy to see in light micrographs.
Skeletal muscle fibers do not usually contract unless stimulated by nerves, and the nervous system provides voluntary
control over their activities. Thus, skeletal muscle is called striated voluntary muscle.
Cardiac Muscle tissue
Cardiac muscle tissue is found in the heart. A typical cardiac muscle cell, also known as a cardiocyte, is smaller than a
skeletal muscle cell. A typical cardiac muscle cell has one centrally positioned nucleus, but some cardiocytes have as many
as five. Prominent striations resemble those of skeletal muscle because the actin and myosin filaments are arranged the same
way in the cells of both tissue types. Cardiac muscle tissue consists of a branching network of interconnected cardiac muscle
cells. The cells are connected at specialized regions known as intercalated discs. There the membranes are locked together
by desmosomes, proteoglycans, and gap junctions. Ion movement through gap junctions helps synchronize the contractions
of the cardiac muscle cells, and the desmosomes and proteoglycans lock the cells together during a contraction.
Cardiac muscle tissue has a very limited ability to repair itself. Some cardiac muscle cells do divide after an injury to the
heart, but the repairs are incomplete. Some heart function is usually lost.
Cardiac muscle cells do not rely on nerve activity to start a contraction. Instead, specialized cardiac muscle cells called
pacemaker cells set a regular rate of contraction. The nervous system can alter the rate of pacemaker cell activity, but it does
not provide voluntary control over individual cardiac muscle cells. For this reason, cardiac muscle is called striated
involuntary muscle.
Smooth Muscle tissue
Smooth muscle tissue is found in the walls of blood vessels, around hollow organs such as the urinary bladder, and in layers
around the respiratory, cardiovascular, digestive, and reproductive tracts. A smooth muscle cell is small and spindle-shaped,
with tapering ends and a single, oval nucleus. These cells can divide, so smooth muscle tissue can regenerate after an injury.
The actin and myosin filaments in smooth muscle cells are organized differently from those of skeletal and cardiac muscles.
One result is that smooth muscle tissue has no striations.
Smooth muscle cells may contract on their own, with gap junctions between adjacent cells coordinating the contractions of
individual cells. The contraction of some smooth muscle tissue can be controlled by the nervous system, but contractile
activity is not under voluntary control.
(Imagine the effort you would need to exert conscious control over the smooth muscles along the 8 m [26 ft.] of digestive
tract, not to mention the miles of blood vessels!) Smooth muscle is known as nonstriated involuntary muscle because of its
appearance and the fact that the nervous system usually does not voluntarily control smooth muscle contractions.
Neural or Nervous Tissue
Neural tissue, also known as nervous tissue or nerve tissue, is specialized for the propagation (movement) of electrical
impulses from one region of the body to another. Ninety eight percent of the neural tissue in the body is in the brain and
spinal cord, which are the control centers of the nervous system.
Neural tissue contains two basic types of cells: (1) neurons (neuro, nerve) and (2) several kinds of supporting cells,
collectively called neuroglia, or glial cells (glia, glue).
Our conscious and unconscious thought processes reflect the communication among neurons in the brain. Such
communication involves the propagation of electrical impulses, in the form of reversible changes in the membrane potential.
The frequency and the pattern of the impulses convey information.
Neuroglia support and repair neural tissue and supply nutrients to neurons.
Neurons are the longest cells in your body. Many are as long as a meter (39 in.)! Most neurons cannot divide under normal
circumstances, so they have a very limited ability to repair themselves after injury. A typical neuron has a large cell body
with a large nucleus and a prominent nucleolus. Extending from the cell body are many branching processes (projections or
outgrowths) termed dendrites (DEN-drı.ts; dendron, a tree), and one axon. The dendrites receive information, typically from
other neurons. The axon conducts that information to other cells. Because axons tend to be very long and slender, they are
also called nerve fibers.
Neuron
The Cell Body
The cell body, or soma, contains a large, round nucleus with a prominent nucleolus. The cytoplasm surrounding the nucleus
is the perikaryon (peri, around + karyon, nucleus). The cytoskeleton of the perikaryon contains neurofilaments and
neurotubules, which are similar to the intermediate filaments and microtubules of other types of cells. Bundles of
neurofilaments, called neurofibrils, extend into the dendrites and axon, providing internal support for them. The perikaryon
contains organelles that provide energy and synthesize organic materials, especially the chemical neurotransmitters that are
important in cell-to-cell communication. The numerous mitochondria, free and fixed ribosomes, and membranes of rough
endoplasmic reticulum (RER) give the perikaryon a coarse, grainy appearance. Mitochondria generate ATP to meet the high
energy demands of an active neuron. The ribosomes and RER synthesize proteins. Some areas of the perikaryon contain
clusters of RER and free ribosomes. These regions, which stain darkly, are called Nissl bodies, after the German
microscopist Franz Nissl, who first described them. Nissl bodies give a gray color to areas containing neuron cell bodies—
the gray matter seen in gross dissection of the brain and spinal cord.
Most neurons lack centrioles, important organelles that help to organize the cytoskeleton and the microtubules that move
chromosomes during mitosis. As a result, typical CNS neurons cannot divide. For this reason, they cannot be replaced if lost
to injury or disease.
Neuron
Neural stem cells persist in the adult nervous system, but they are typically inactive except in the nose, where the
regeneration of olfactory (smell) receptors maintains our sense of smell, and in the hippocampus, a part of the brain involved
in storing memories. Researchers are investigating the control mechanisms that trigger neural stem cell activity, with the
goal of preventing or reversing neuron loss due to trauma, disease, or aging.
Dendrites and axons
A variable number of slender, sensitive processes (extensions) known as dendrites extend out from the cell body. Dendrites
play key roles in intercellular communication. Typical dendrites are highly branched, and each branch has fine 0.5- to 1-μm-
long studded processes called dendritic spines.
In the CNS, a neuron receives information from other neurons primarily at the dendritic spines, which represent 80–90
percent of the neuron’s total surface area.
An axon is a long cytoplasmic process capable of propagating an electrical impulse known as an action potential. The
axoplasm or cytoplasm of the axon, contains neurofibrils, neurotubules, small vesicles, lysosomes, mitochondria, and
various enzymes. The axolemma (lemma, husk), a specialized portion of the plasma membrane, surrounds the axoplasm. In
the CNS, the axolemma may be exposed to the interstitial fluid or, it may be covered by the cellular processes of neuroglia.
Neuron
The base, or initial segment, of the axon in a multipolar neuron joins the cell body at a thickened region known as the axon
hillock.
An axon may branch along its length, producing side branches known as collaterals. Collaterals enable a single neuron to
communicate with several other cells. The main axon trunk and any collaterals end in a series of fine extensions called
telodendria (telo-, end + dendron, tree) or terminal branches. The telodendria, in turn, end at axon terminals (also called
synaptic terminals, synaptic knobs, and synaptic boutons), which play a role in communication with another cell.
The structure of the axon terminal varies with the type of postsynaptic cell. A relatively simple, round axon terminal occurs
where the postsynaptic cell is another neuron. At a synapse, the narrow synaptic cleft separates the presynaptic membrane
where neurotransmitters are released, from the postsynaptic membrane, which bears receptors for neurotransmitters. The
axon terminal at a neuromuscular junction is much more structurally complex.
Each axon terminal contains mitochondria and thousands of vesicles filled with neurotransmitter molecules. The axon
terminal reabsorbs breakdown products of neurotransmitters formed at the synapse and reassembles them. It also receives a
continuous supply of neurotransmitters synthesized in the cell body, along with enzymes and lysosomes. These materials
travel the length of the axon on neurotubules, pulled along by protein “molecular motors,” called kinesin and dynein, that
run on ATP.
Neuron
The movement of materials between the cell body and axon terminals is called axoplasmic transport. Some materials travel
slowly, at rates of a few millimeters per day. This transport mechanism is known as the “slow stream.” Vesicles containing
neurotransmitters move much more rapidly, traveling in the “fast stream” at 5–10 mm per hour.
Axoplasmic transport occurs in both directions.
The flow of materials from the cell body to the axon terminal is anterograde (antero-, forward) flow, carried by kinesin.
At the same time, other substances are transported from the axon terminal toward the cell body in retrograde flow (retro,
backward), carried by dynein. If debris or unusual chemicals appear in the axon terminal, retrograde flow soon delivers
them to the cell body. There they may then alter the activity of the cell by turning certain genes on or off.
Structural Classification of Neurons
Anaxonic neurons are small and have numerous dendrites, but no axon. Anaxonic neurons are located in the brain and in
special sense organs. Their functions are poorly understood.
Bipolar neurons have two distinct processes—one dendrite that branches extensively into dendritic branches at its distal tip,
and one axon—with the cell body between the two. Bipolar neurons are rare. They occur in special sense organs, where they
relay information about sight, smell, or hearing from receptor cells to other neurons. Bipolar neurons are small. The largest
measure less than 30 µm from end to end.
In a unipolar neuron, or pseudounipolar neuron, the dendrites and axon are continuous—basically, fused—and the cell
body lies off to one side. In such a neuron, the initial segment lies where the dendrites converge. The rest of the process,
which carries action potentials, is usually considered an axon. Most sensory neurons of the peripheral nervous system are
unipolar. Their axons may extend a meter or more, ending at synapses in the central nervous system. The longest carry
sensations from the tips of the toes to the spinal cord.
Multipolar neurons have two or more dendrites and a single axon. They are the most common neurons in the CNS. All the
motor neurons that control skeletal muscles, for example, are multipolar neurons. The axons of multipolar neurons can be as
long as those of unipolar neurons, and the longest carry motor commands from the spinal cord to small muscles that move
the toes.
Neuroglia of the Central Nervous System
The central nervous system has four types of neuroglia: (1) ependymal cells, (2) astrocytes, (3) oligodendrocytes, and (4)
microglia.
Ependymal Cells
A fluid-filled central passageway extends along the longitudinal axis of the spinal cord and brain. Cerebrospinal fluid (CSF)
fills this passageway and also surrounds the brain and spinal cord. This fluid, which circulates continuously, provides a
protective cushion and transports dissolved gases, nutrients, wastes, and other materials. The diameter of the internal
passageway varies from one region to another. In the spinal cord, this narrow passageway is called the central canal. In
several regions of the brain, the passageway forms enlarged chambers called ventricles. Ependymal cells line the central
canal and ventricles, where they form a simple cuboidal to columnar epithelium known as the ependyma. Unlike other
epithelia, it lacks a basement membrane. Ependymal cells assist in producing, monitoring, and circulating CSF. There are
three types of ependymal cells: ependymocytes, tanycytes, and specialized CSF-producing ependymal cells.
Ependymocytes have motile cilia that aid in the circulation of CSF and also microvilli. In adults, the cilia do not persist in
all areas of the ventricles and central canal. Ependymocytes have long, slender basal processes that branch and make contact
with neuroglia. Tanycytes are specialized, non-ciliated ependymal cells with microvilli on their apical surfaces. They are
found in only one brain ventricle. It is thought that they transport substances between the CSF and the brain.
Neuroglia of the Central Nervous System
Astrocytes
Astrocytes (AS-tro. -sı.ts; astro-, star + -cyte, cell) are the largest and most numerous neuroglia in the CNS.
These cells have a variety of functions, many of them poorly understood:
• Maintaining the Blood–Brain Barrier.
• Creating a Three-Dimensional Framework for the CNS.
• Repairing Damaged Neural Tissue.
• Guiding Neuron Development.
• Controlling the Interstitial Environment.
Oligodendrocytes
Like astrocytes, oligodendrocytes have slender cytoplasmic extensions, but the cell bodies of oligodendrocytes are smaller,
with fewer processes, than astrocytes. The processes of oligodendrocytes generally are in contact with the exposed surfaces
of neurons. The functions of processes ending at the neuron cell body have yet to be determined. Much more is known about
the processes that end on the surfaces of axons. Many axons in the CNS are completely sheathed in these processes, which
insulate them from contact with the extracellular fluid.
Neuroglia of the Central Nervous System
During its maturation, the plasma membrane near the tip of each process of an oligodendrocyte expands to form an
enormous pad, and the cytoplasm there becomes very thin. This flattened “pancake” somehow gets wrapped around the
axolemma, forming concentric layers of plasma membrane. This membranous wrapping, called myelin, serves as electrical
insulation and increases the speed at which an action potential travels along the axon. Many oligodendrocytes cooperate in
forming a myelin sheath along the length of an axon. Such an axon is said to be myelinated. Each oligodendrocyte
myelinates segments of several axons. The fairly large areas of the axon that are wrapped in myelin are called internodes.
Inter nodes are typically 1–2 mm in length. The small gaps of a few micrometers that separate adjacent internodes are called
nodes, or nodes of Ranvier. An axon’s collateral branches originate at nodes.
In dissection, myelinated axons appear glossy white, primarily because of the lipids in the myelin. As a result, regions
dominated by myelinated axons are known as the white matter of the CNS.
Unmyelinated axons are not completely covered by oligodendrocytes. Such axons are common where short axons and
collaterals form synapses with densely packed neuron cell bodies. Areas containing neuron cell bodies, dendrites, and
unmyelinated axons have a dusky gray color, and make up the gray matter of the CNS.
In summary, oligodendrocytes play an important role in structural organization by tying clusters of axons together. They also
improve the functioning of neurons by wrapping axons within a myelin sheath.
Neuroglia of the Central Nervous System
Microglia
The least numerous and smallest neuroglia in the CNS are phagocytic cells called microglia. Their slender processes have
many fine branches. These cells can migrate through neural tissue. Microglia appear early in embryonic development,
originating from mesodermal stem cells related to stem cells that produce monocytes and macrophages. Microglia migrate
into the CNS as the nervous system forms. There they remain, acting as a wandering janitorial service and police force by
engulfing cellular debris, waste products, and pathogens.
Neuroglia of the Peripheral Nervous System
The cell bodies of neurons in the PNS are clustered in masses called ganglia (singular, ganglion). The processes of neuroglia
completely insulate neuronal cell bodies and most axons in the PNS from their surroundings.
The two types of neuroglia in the PNS are satellite cells and Schwann cells.
Satellite cells surround neuron cell bodies in ganglia. They regulate the environment around the neurons, much as astrocytes
do in the CNS.
Schwann cells, or neurilemma cells, either form a thick, myelin sheath or indented folds of plasma membrane around
peripheral axons. Wherever a Schwann cell covers an axon, the outer surface of the Schwann cell is called the neurilemma.
Most axons in the PNS, whether myelinated or unmyelinated, are shielded from contact with interstitial fluids by Schwann
cells. A myelinating Schwann cell can myelinate only one segment of a single axon, whereas an oligodendrocyte in the CNS
may myelinate portions of several adjacent axons. Non-myelinating Schwann cells can enclose segments of several
unmyelinated axons. A series of Schwann cells is required to enclose an axon along its entire length.
You might also like
- Body Tissues: Tissue Matrix MuscleDocument8 pagesBody Tissues: Tissue Matrix Muscle9. Hoàng Mai ChiNo ratings yet
- CCCC C CDocument16 pagesCCCC C CLennon Mars LamsinNo ratings yet
- Muscle TissueDocument10 pagesMuscle TissueHesbone AneneNo ratings yet
- TissuesDocument13 pagesTissuesAvika Bhardwaj100% (1)
- ANATOMY AND PHYSIOLOGY TISSUE NOTESpdfDocument30 pagesANATOMY AND PHYSIOLOGY TISSUE NOTESpdfYego EdwinNo ratings yet
- Histology Notes: Epithelial TissueDocument4 pagesHistology Notes: Epithelial TissueSteph AsideNo ratings yet
- Tissues (Notes)Document11 pagesTissues (Notes)Rezeil CaNo ratings yet
- Lesson 1: Animals' Specialized StructuresDocument58 pagesLesson 1: Animals' Specialized StructuresPhoenixNo ratings yet
- Tugas Self Directed Learning Sains Dan Biomedik DasarDocument7 pagesTugas Self Directed Learning Sains Dan Biomedik DasarApria PratamaNo ratings yet
- Nselec TissueDocument6 pagesNselec TissueClaire funtilarNo ratings yet
- Cell Modifications and TissuesDocument4 pagesCell Modifications and TissuesElla PascuaNo ratings yet
- Human Body Tissues Power PointDocument60 pagesHuman Body Tissues Power PointMaxwell C Jay KafwaniNo ratings yet
- Tissues 2Document48 pagesTissues 2chikwatumilessNo ratings yet
- Cells: Skeletal Muscle Is A Form of Striated Muscle Tissue Existing Under Control of The SomaticDocument11 pagesCells: Skeletal Muscle Is A Form of Striated Muscle Tissue Existing Under Control of The SomaticbloodythornNo ratings yet
- HP I P2 Tissues and MembranesDocument38 pagesHP I P2 Tissues and MembranesNazir RabiuNo ratings yet
- Muscle and Membrane TissuesDocument3 pagesMuscle and Membrane Tissuesamadi3ndessy1260No ratings yet
- Tissue, Glands, and Membranes Epithelial TissueDocument5 pagesTissue, Glands, and Membranes Epithelial TissueMoises MontalboNo ratings yet
- Cell Types TissuesDocument26 pagesCell Types Tissueskurtandreinace04No ratings yet
- Cell SpecializationadpataionDocument67 pagesCell SpecializationadpataionMarc AnthonyNo ratings yet
- 01 Animal TissueDocument8 pages01 Animal TissueRohit SharmaNo ratings yet
- Animal TissuesDocument13 pagesAnimal TissuesYudatami TiaraNo ratings yet
- M 1 PPT-PDF XI Bio CH 7 Structural Organisation in AnimalsDocument39 pagesM 1 PPT-PDF XI Bio CH 7 Structural Organisation in Animalsamarendrar87No ratings yet
- CHAPTER V: Tissues: Epithelial Tissues Connective Tissue Muscular Tissue Nervous TissueDocument10 pagesCHAPTER V: Tissues: Epithelial Tissues Connective Tissue Muscular Tissue Nervous TissueAem TalNo ratings yet
- Class Discussion On TissueDocument2 pagesClass Discussion On TissueKristhine Abegail Manangan-GamiaoNo ratings yet
- The Muscular TissueDocument23 pagesThe Muscular TissueMuhammad Salisu IliyasuNo ratings yet
- Types and Functions of Connective TissuesDocument6 pagesTypes and Functions of Connective TissuesAmmar ShahidNo ratings yet
- Cds Day1Document15 pagesCds Day1Rajkamal ChoudharyNo ratings yet
- Soft Tissue Mechanics: Types and PropertiesDocument14 pagesSoft Tissue Mechanics: Types and PropertiesKripa NNo ratings yet
- Audio 1 Types of TissuesDocument9 pagesAudio 1 Types of TissuesTricia De TorresNo ratings yet
- Tissue - WikipediaDocument42 pagesTissue - WikipediaLumina More100% (1)
- Structural Organisation in AnimalsDocument19 pagesStructural Organisation in AnimalsBiju Mylachal100% (1)
- Epithelial Lab ReportDocument5 pagesEpithelial Lab ReportMadiNo ratings yet
- Human Anatomy - Lec. 2 - GR1Document9 pagesHuman Anatomy - Lec. 2 - GR1bmydwoybx482No ratings yet
- Cuizon Lab Act 3Document18 pagesCuizon Lab Act 3Clarizza Joy J. CuizonNo ratings yet
- GEN BIO Q1M1subtopic WK 4 LectureDocument4 pagesGEN BIO Q1M1subtopic WK 4 LectureDonnalyn Mae EscrupoloNo ratings yet
- Tissue Types and FunctionsDocument36 pagesTissue Types and FunctionsMinan Fahnanza100% (1)
- Sir FayyazDocument49 pagesSir FayyazSara ZaraNo ratings yet
- Tissues (Image) Description and LocationDocument10 pagesTissues (Image) Description and LocationJOHNNY YNo ratings yet
- Connective Tisssue (General)Document29 pagesConnective Tisssue (General)James ChabuNo ratings yet
- TISSUESDocument12 pagesTISSUESMaria Stephanie LabutapNo ratings yet
- ANIMAL TISSUESDocument14 pagesANIMAL TISSUESjitendragandhi250No ratings yet
- MT 100 Lab Notes 1Document11 pagesMT 100 Lab Notes 1Nilo Golosino IIINo ratings yet
- TissuesDocument74 pagesTissuesMonica Sree100% (1)
- General-Biology-module-1-2Document12 pagesGeneral-Biology-module-1-2cabellaNo ratings yet
- Anatomy and Physiology LabDocument12 pagesAnatomy and Physiology Labشهد إياد0% (1)
- Animal Tissues 1. EpithelialDocument3 pagesAnimal Tissues 1. EpithelialRogeimar Claire MangomayaoNo ratings yet
- Tissue (Biology) - Wikipedia PDFDocument37 pagesTissue (Biology) - Wikipedia PDFKissa FrecNo ratings yet
- Body TissuesDocument10 pagesBody TissuesNaanmatha PuspanathanNo ratings yet
- Animal Tissue Hand-Out Bio 101Document3 pagesAnimal Tissue Hand-Out Bio 101Amor Panopio MagtibayNo ratings yet
- Tissue Membranes GuideDocument4 pagesTissue Membranes GuideElleNo ratings yet
- Anatomy and PhysiologyDocument23 pagesAnatomy and Physiologyapi-464344582100% (1)
- Hadba University CollegeتقريرDocument11 pagesHadba University Collegeتقريرtaha1995irqNo ratings yet
- Different Body Tissues: By: Group 4Document25 pagesDifferent Body Tissues: By: Group 4Aisha Mae Cañete JawadNo ratings yet
- MG I S5 - Body Tissues - 2Document4 pagesMG I S5 - Body Tissues - 2Mirela OncioiuNo ratings yet
- Anatomy - TissuesDocument43 pagesAnatomy - TissuesGleceree Filomeno100% (1)
- NCLEX Skeletal Muscle Review: 650 Muscles Work TogetherDocument12 pagesNCLEX Skeletal Muscle Review: 650 Muscles Work TogetherWillington Cuaresma100% (1)
- CartilageDocument33 pagesCartilageRahaf MajadlyNo ratings yet
- Chapter 7 Structural Organisation in AnimalsDocument25 pagesChapter 7 Structural Organisation in Animalsamit lakraNo ratings yet
- المحاضرة الثانية تشريح اسنان م 1Document26 pagesالمحاضرة الثانية تشريح اسنان م 1mfhrluvxxxNo ratings yet
- Dr. Niranjan Murthy H L: Asst. Prof., Dept. of Physiology Sree Siddhartha Medical College & Hospital, TumkurDocument17 pagesDr. Niranjan Murthy H L: Asst. Prof., Dept. of Physiology Sree Siddhartha Medical College & Hospital, Tumkurnirilib100% (1)
- Luminang Muscular System RADocument13 pagesLuminang Muscular System RAJohn Chris LuminangNo ratings yet
- Circulatory System REVIEWERDocument6 pagesCirculatory System REVIEWERClyde BaltazarNo ratings yet
- Histology World MCQDocument43 pagesHistology World MCQAziz100% (6)
- MCQs Nerve and MuscleDocument10 pagesMCQs Nerve and MuscleNo One100% (2)
- SAAOL Medicine With Mech. of ActionDocument58 pagesSAAOL Medicine With Mech. of ActionSusanta RoutNo ratings yet
- Muscle and MovementDocument5 pagesMuscle and MovementRabiaNo ratings yet
- Volibris MOA Storyboard v1 1Document4 pagesVolibris MOA Storyboard v1 1shyamchepurNo ratings yet
- Isradipidine: - NifedipineDocument2 pagesIsradipidine: - NifedipineMahmoud A. ZoghborNo ratings yet
- Muscle Physiology PDFDocument103 pagesMuscle Physiology PDFedabzan234No ratings yet
- Mecanismos de Accion InotropicosDocument8 pagesMecanismos de Accion InotropicosPaola DiazNo ratings yet
- FUNCTIONSDocument1 pageFUNCTIONSCes GarciaNo ratings yet
- ANA205 Muscular Tissue: Lecture Notes by Dr. Taiwo-OlaDocument31 pagesANA205 Muscular Tissue: Lecture Notes by Dr. Taiwo-OlaIbrahim BabatundeNo ratings yet
- FuPap L6 Contractile Mechanisms-2Document39 pagesFuPap L6 Contractile Mechanisms-2Osman MNo ratings yet
- Hollinshead's Functional Anatomy of The Limbs and Back PDFDocument353 pagesHollinshead's Functional Anatomy of The Limbs and Back PDFCarla S Morales Garcia100% (1)
- Basic PhysiologyDocument58 pagesBasic PhysiologyVidit JoshiNo ratings yet
- Lesson PlanDocument13 pagesLesson Planapi-276183071100% (1)
- Iea MSKDocument48 pagesIea MSKAlex WalshNo ratings yet
- Physiology and Pharmacology of The Bladder and Urethra: Gregorio, Frances Mari Mendoza, AlyannaDocument29 pagesPhysiology and Pharmacology of The Bladder and Urethra: Gregorio, Frances Mari Mendoza, AlyannaLic MendozaNo ratings yet
- Official Bank-MusclesDocument27 pagesOfficial Bank-MusclesEbtihal AlharthiNo ratings yet
- CA 2 MedicineDocument15 pagesCA 2 MedicineDimitri Valdes TchuindjangNo ratings yet
- Receptor 1Document1 pageReceptor 1Jeremy WongNo ratings yet
- Smooth & Cardiac Muscles: DR Marlini Muhamad FPSK, Usim Nov 2012Document34 pagesSmooth & Cardiac Muscles: DR Marlini Muhamad FPSK, Usim Nov 2012Harleyquinn96 DrNo ratings yet
- ABSITE CH 16 Critical CareDocument11 pagesABSITE CH 16 Critical CareJames JosephNo ratings yet
- Adrenergic ReceptorsDocument1 pageAdrenergic ReceptorsYavuz Burak KÜÇÜKGÜLNo ratings yet
- Vascular SurgeryDocument38 pagesVascular Surgeryapi-3840195100% (10)
- Science EXPERIMENT For Class 9Document21 pagesScience EXPERIMENT For Class 9HEMRAJ SONINo ratings yet
- Muscle Tissue Differences and Contraction TypesDocument2 pagesMuscle Tissue Differences and Contraction TypesChris CaoagdanNo ratings yet
- Ns Elec 4 - Muscular SystemDocument5 pagesNs Elec 4 - Muscular SystemONGLENGCO WILSON JAKE V.No ratings yet
- 26.pulmonary PharmacologyDocument14 pages26.pulmonary PharmacologyAnggreany AshariNo ratings yet